Aniridia: Background, Pathophysiology, Epidemiology (original) (raw)
Overview
Background
Aniridia is a congenital, hereditary, bilateral, extreme form of iris hypoplasia that may be associated with other ocular defects. [1, 2, 3, 4] It describes an extreme form of iris hypoplasia in which the iris appears absent on superficial clinical examination; however, gonioscopy shows the presence of the iris root. Aniridia is not just an isolated defect in iris development; it is a panocular disorder with macular and optic nerve hypoplasia, cataract, and corneal changes, anomalies that lead to decreased vision and nystagmus. Visual acuity generally is low but is unrelated to the degree of iris hypoplasia. Glaucoma is a secondary problem causing additional visual loss over time. [5]
Patients with aniridia usually lack a foveal reflex, indicating poor macular development. True aplasia of the optic nerve also can occur. All these patients need specialized management of each individual problem. Because of poor visual acuity and nystagmus, low vision aids are very helpful. Lifelong regular follow-up care is necessary for the early detection of any new problems, especially glaucoma, lens, and systemic problems, so that timely treatment is given. [6] Since the condition has a dominant transmission, proper genetic counseling should be obtained. Aniridia is shown in the images below.
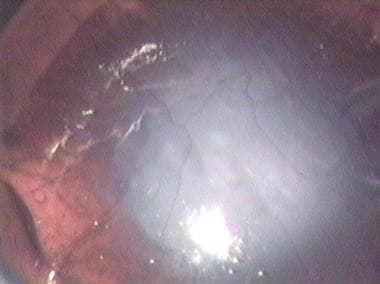
Aniridia with a vascularized corneal opacity in a young patient.
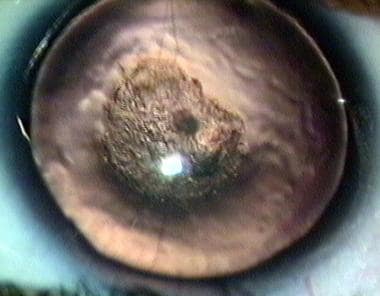
Centrally placed cataractous lens and aniridia in a pediatric patient.
Clinical manifestations
Clinical manifestations include the following:
Isolated aniridia
Aniridia in association with systemic defects
- Wilms tumor (20% of cases) [7, 8, 9]
- Genitourinary abnormalities
- Intellectual disability [10]
- Central nervous system problems such as olfactory and hearing difficulties, cognition and behavioral problems, or developmental delay in patients with isolated aniridia [11]
Aniridia in association with ocular defects [12, 11, 13]
- Albinism
- Ectopia lentis (50%)
- Spontaneous lens dislocation
- Cataract (50-85%)
- Glaucoma (30-50%)
- Nystagmus
- Strabismus
- Optic nerve hypoplasia (75%)
- Optic nerve coloboma
- Aniridia-associated keratopathy (AAK) (20%)
- Foveal hypoplasia
- Bilateral ptosis (%10)
- Meibomian gland dysfunction
- Microcornea
- Persistent pupillary membrane
- Aniridic fibrosis syndrome

Pathophysiology
The pathogenesis of aniridia is attributed to a primary developmental arrest of the neuroectoderm and a secondary alteration of all 3 neural crest waves of the mesenchyme. The functional development of the anterior segment is a complex interrelationship between the neural ectoderm and the neural crest waves of the mesenchyme. The pathogenesis may involve defective formation or excessive regression of various layers of the anterior segment caused by cellular or biochemical aberrations. This explains the combined anterior and posterior segment neural ectodermal and mesenchymal defects. The iris stroma is hypoplastic, indicating an altered third neural crest wave of mesenchyme.
The occurrence of aniridia is classified as the following:
- Autosomal dominant, isolated congenital aniridia without systemic involvement [14]
- Sporadic congenital aniridia; chromosome deletion of the short arm of chromosome 11, including band p13 (WAGR Syndrome) [15]
- Autosomal recessive congenital aniridia (Gillespie Syndrome) [10]
The exact defect in iris morphogenesis giving rise to aniridia is unknown. Because the iris pigment epithelium, the iris musculature, the retina, and the optic nerve are derived from neuroectoderm, there may be a common embryologic origin for these anomalies. As an isolated ocular malformation, aniridia is an autosomal dominant disorder, which is caused by a mutation in the PAX6 (paired box gene family) gene. [16, 17, 18]
Patients with aniridia who have a positive family history are not at an increased risk for Wilms tumor. Two genetic loci for aniridia have been identified: one (AN1) on chromosome arm 2p and one (AN2) on chromosome 11.
Patients with aniridia without a positive family history have a 30% chance of developing Wilms tumor, and they represent new mutations for the autosomal dominant gene. About one third of such patients have a mutation that affects the WT and AN2 loci, causing the patient to develop Wilms tumor; the other two thirds of patients have a mutation of just the AN2 locus. Because of the high mortality from Wilms tumor, those patients with the WT and AN2 mutations have a low probability of reproducing, whereas those with just AN2 mutations have normal fertility and, hence, a 50% risk to pass the aniridia gene mutation to each child.

Epidemiology
Frequency
Aniridia is a rare disease with an incidence of 1.8 per 100,000 live births. [19] The incidence ranges from 1/60,000 to 1/100,000 live births. The autosomal dominant form accounts for about two thirds of cases. The sporadic form accounts for one third of cases. [20]
Mortality/Morbidity
All patients with aniridia are visually handicapped for a lifetime. This already reduced vision is threatened further by such complications as cataract and glaucoma. Patients with Wilms tumor have a reduced span of life.
Race
Aniridia has no racial predisposition.
Age
Congenital glaucoma and aniridia usually are not associated at birth. The glaucoma develops at either the preteen or the teenage level.
Significant cataracts may occur before puberty. The risk for cataract increases with age, with lens opacities observed in 50-85% of patients during the first 2 decades of life.
See Primary Congenital Glaucoma and Secondary Congenital Glaucoma.

Prognosis
The prognosis of aniridia varies from patient to patient.
Unmonitored and untreated elevated intraocular pressure may damage vision.
Cataract may require surgery.
Progressive corneal opacification may need corneal grafting.

Patient Education
Thoroughly educating the patient and parents about aniridia and the associated ocular anomalies and systemic problems is mandatory.

- Hittner HM. Aniridia. Robert ED, Shields MB, et al, eds. The Glaucomas. St. Louis: Mosby; 1989. 869-884.
- Nelson LB, Spaeth GL, Nowinski TS, Margo CE, Jackson L. Aniridia. A review. Surv Ophthalmol. 1984 May-Jun. 28(6):621-42. [QxMD MEDLINE Link].
- Roy FH. Ocular Syndromes and Systemic Disease. 3rd ed. Lippincott Williams & Wilkins; 2002.
- Elsas FJ, Maumenee IH, Kenyon KR, Yoder F. Familial aniridia with preserved ocular function. Am J Ophthalmol. 1977 May. 83(5):718-24. [QxMD MEDLINE Link].
- Grant WM, Walton DS. Progressive changes in the angle in congenital aniridia, with development of glaucoma. Am J Ophthalmol. 1974 Nov. 78(5):842-7. [QxMD MEDLINE Link].
- Jastaneiah S, Al-Rajhi AA. Association of aniridia and dry eyes. Ophthalmology. 2005 Sep. 112(9):1535-40. [QxMD MEDLINE Link].
- Francois J, Coucke D, Coppieters R. Aniridia-Wilms' tumour syndrome. Ophthalmologica. 1977. 174(1):35-9. [QxMD MEDLINE Link].
- Green DM, Breslow NE, Beckwith JB, Norkool P. Screening of children with hemihypertrophy, aniridia, and Beckwith-Wiedemann syndrome in patients with Wilms tumor: a report from the National Wilms Tumor Study. Med Pediatr Oncol. 1993. 21(3):188-92. [QxMD MEDLINE Link].
- Pilling GP. Wilms' tumor in seven children with congenital aniridia. J Pediatr Surg. 1975 Feb. 10(1):87-96. [QxMD MEDLINE Link].
- Nevin NC, Lim JH. Syndrome of partial aniridia, cerebellar ataxia, and mental retardation--Gillespie syndrome. Am J Med Genet. 1990 Apr. 35(4):468-9. [QxMD MEDLINE Link].
- Hingorani M, Hanson I, van Heyningen V. Aniridia. Eur J Hum Genet. 2012 Oct. 20 (10):1011-7. [QxMD MEDLINE Link].
- Schroeder HW, Orth U, Meyer-Konig E, Gal A. [Hereditary foveal hypoplasia - clinical differentiation]. Klin Monbl Augenheilkd. 2003 Aug. 220(8):559-62. [QxMD MEDLINE Link].
- Lee H, Khan R, O'Keefe M. Aniridia: current pathology and management. Acta Ophthalmol. 2008 Nov. 86 (7):708-15. [QxMD MEDLINE Link].
- Pearce WG. Variability of iris defects in autosomal dominant aniridia. Can J Ophthalmol. 1994 Feb. 29(1):25-9. [QxMD MEDLINE Link].
- Riccardi VM, Sujansky E, Smith AC, Francke U. Chromosomal imbalance in the Aniridia-Wilms' tumor association: 11p interstitial deletion. Pediatrics. 1978 Apr. 61(4):604-10. [QxMD MEDLINE Link].
- Glaser T, Walton DS, Maas RL. Genomic structure, evolutionary conservation and aniridia mutations in the human PAX6 gene. Nat Genet. 1992 Nov. 2(3):232-9. [QxMD MEDLINE Link].
- Vincent MC, Pujo AL, Olivier D, Calvas P. Screening for PAX6 gene mutations is consistent with haploinsufficiency as the main mechanism leading to various ocular defects. Eur J Hum Genet. 2003 Feb. 11(2):163-9. [QxMD MEDLINE Link].
- Dharmaraj N, Reddy A, Kiran V, Mandal A, Panicker S, Chakrabarti S. PAX6 gene mutations and genotype-phenotype correlations in sporadic cases of aniridia from India. Ophthalmic Genet. 2003 Sep. 24(3):161-5. [QxMD MEDLINE Link].
- Berlin HS, Ritch R. The treatment of glaucoma secondary aniridia. Mt Sinai J Med. 1981 Mar-Apr. 48 (2):111-5. [QxMD MEDLINE Link].
- Lim HT, Seo EJ, Kim GH, Ahn H, Lee HJ, Shin KH, et al. Comparison between aniridia with and without PAX6 mutations: clinical and molecular analysis in 14 Korean patients with aniridia. Ophthalmology. 2012 Jun. 119 (6):1258-64. [QxMD MEDLINE Link].
- Roy FH. Ocular Differential Diagnosis. 7th ed. Lippincott Williams & Wilkins; 2002.
- Tibrewal S, Ratna R, Gour A, Agarkar S, Dubey S, Ganesh S, et al. Clinical and molecular aspects of congenital aniridia - A review of current concepts. Indian J Ophthalmol. 2022 Jul. 70 (7):2280-2292. [QxMD MEDLINE Link].
- Friedman AL. Wilms' tumor detection in patients with sporadic aniridia. Successful use of ultrasound. Am J Dis Child. 1986 Feb. 140(2):173-4. [QxMD MEDLINE Link].
- Lapid-Gortzak R, Santana NTY, Nieuwendaal CP, Mourits MP, van der Meulen IJE. Topical bevacizumab treatment in aniridia. Int Ophthalmol. 2017 Jun 15. [QxMD MEDLINE Link].
- Wong VW, Lam PT, Lai TY, Lam DS. Black diaphragm aniridia intraocular lens for aniridia and albinism. Graefes Arch Clin Exp Ophthalmol. 2005 May. 243(5):501-4. [QxMD MEDLINE Link].
- Omoto M, Shimmura S, Hatou S, Ichihashi Y, Kawakita T, Tsubota K. Simultaneous deep anterior lamellar keratoplasty and limbal allograft in bilateral limbal stem cell deficiency. Jpn J Ophthalmol. 2010 Nov. 54 (6):537-43. [QxMD MEDLINE Link].
- Holland EJ, Djalilian AR, Schwartz GS. Management of aniridic keratopathy with keratolimbal allograft: a limbal stem cell transplantation technique. Ophthalmology. 2003 Jan. 110 (1):125-30. [QxMD MEDLINE Link].
- Akpek EK, Harissi-Dagher M, Petrarca R, et al. Outcomes of Boston keratoprosthesis in aniridia: a retrospective multicenter study. Am J Ophthalmol. 2007 Aug. 144(2):227-231. [QxMD MEDLINE Link].
- Walton DS. Aniridic glaucoma: the results of gonio-surgery to prevent and treat this problem. Trans Am Ophthalmol Soc. 1986. 84:59-70. [QxMD MEDLINE Link]. [Full Text].
- Fantes JA, Bickmore WA, Fletcher JM, Ballesta F, Hanson IM, van Heyningen V. Submicroscopic deletions at the WAGR locus, revealed by nonradioactive in situ hybridization. Am J Hum Genet. 1992 Dec. 51(6):1286-94. [QxMD MEDLINE Link]. [Full Text].
- Aniridia with superiorly dislocated cataract.
- Aniridia. Close-up of the superior limbus of same patient as in the image above to show pannus.
- Aniridia with a vascularized corneal opacity in a young patient.
- Centrally placed cataractous lens and aniridia in a pediatric patient.
- Aniridia. 3-D image showing absence of the inferior half of the iris and absence of most of the anterior leaf of the iris in the upper half. In the less affected area, the iris is represented mostly by the posterior pigment epithelium. No choroidal coloboma was present.
- Aniridia and aphakia following perforating injury.
- Single piece intraocular lens inside the bag, in a case of aniridia.
- Multipiece intraocular lens inside the bag, in a case of aniridia.
- In-the-bag intraocular lens. The lens has been displaced superiorly.
- Aniridia. A single piece nonfoldable lens has been implanted after placing an endocapsular ring. An endocapsular ring provides better chances of centration.
- Partial traumatic aniridia. The lost iris gap has been covered by the use of a lens optic that is clear in the center and is opaque at the periphery. A scleral fixated lens has been used in this case.


Author
Michael Ross, MD Clinical Instructor, University of British Columbia Faculty of Medicine, Canada
Disclosure: Nothing to disclose.
Coauthor(s)
Kubra Ozdemir Yalcinsoy, MD Cornea, External Disease and Uveitis Observer, Department of Ophthalmology, McGill University Health Center, McGill University Faculty of Medicine, Canada
Disclosure: Nothing to disclose.
Jean Deschênes, MD, FRCSC Professor, Research Associate, Director, Uveitis Program, Department of Ophthalmology, McGill University Faculty of Medicine; Senior Ophthalmologist, Clinical Director, Department of Ophthalmology, Royal Victoria Hospital, Canada
Jean Deschênes, MD, FRCSC is a member of the following medical societies: American Academy of Ophthalmology, Association for Research in Vision and Ophthalmology, Canadian Medical Association, Canadian Ophthalmological Society, International Ocular Inflammation Society, Quebec Medical Association
Disclosure: Nothing to disclose.
Specialty Editor Board
Francisco Talavera, PharmD, PhD Adjunct Assistant Professor, University of Nebraska Medical Center College of Pharmacy; Editor-in-Chief, Medscape Drug Reference
Disclosure: Received salary from Medscape for employment. for: Medscape.
J James Rowsey, MD Former Director of Corneal Services, St Luke's Cataract and Laser Institute
J James Rowsey, MD is a member of the following medical societies: American Academy of Ophthalmology, American Association for the Advancement of Science, American Medical Association, Association for Research in Vision and Ophthalmology, Florida Medical Association, Sigma Xi, The Scientific Research Honor Society, Southern Medical Association, Pan-American Association of Ophthalmology
Disclosure: Nothing to disclose.
Chief Editor
Michael Taravella, MD Director of Cornea and Refractive Surgery, Rocky Mountain Lions Eye Institute; Professor, Department of Ophthalmology, University of Colorado School of Medicine
Michael Taravella, MD is a member of the following medical societies: American Academy of Ophthalmology, American Medical Association, American Society of Cataract and Refractive Surgery, Contact Lens Association of Ophthalmologists, Eye Bank Association of America
Disclosure: Received income in an amount equal to or greater than $250 from: J&J Vision (Consultant)/Proctor
for: Coronet Surgical (Consultant), no income received.
Additional Contributors
Daljit Singh, MBBS, MS, DSc † Professor Emeritus, Department of Ophthalmology, Guru Nanak Dev University; Director, Daljit Singh Eye Hospital, India
Daljit Singh, MBBS, MS, DSc is a member of the following medical societies: All India Ophthalmological Society, American Society of Cataract and Refractive Surgery, Indian Medical Association, International Intra-Ocular Implant Club, Intraocular Implant and Refractive Society, India
Disclosure: Nothing to disclose.
Arun Verma, MD Senior Consultant, Department of Ophthalmology, Dr Daljit Singh Eye Hospital, India
Disclosure: Nothing to disclose.