Inflammation (original) (raw)
inflammation
[in″flah-ma´shun]
a localized protective response elicited by injury or destruction of tissues, which serves to destroy, dilute, or wall off both the injurious agent and the injured tissue. adj., adj inflam´matory.
The inflammatory response can be provoked by physical, chemical, and biologic agents, including mechanical trauma, exposure to excessive amounts of sunlight, x-rays and radioactive materials, corrosive chemicals, extremes of heat and cold, or by infectious agents such as bacteria, viruses, and other pathogenic microorganisms. Although these infectious agents can produce inflammation, infection and inflammation are not synonymous.
The classic signs of inflammation are heat, redness, swelling, pain, and loss of function. These are manifestations of the physiologic changes that occur during the inflammatory process. The three major components of this process are (1) changes in the caliber of blood vessels and the rate of blood flow through them (hemodynamic changes); (2) increased capillary permeability; and (3) leukocytic exudation.
Hemodynamic changes begin soon after injury and progress at varying rates, according to the extent of injury. They start with dilation of the arterioles and the opening of new capillaries and venular beds in the area. This causes an accelerated flow of blood, accounting for the signs of heat and redness. Next follows increased permeability of the microcirculation, which permits leakage of protein-rich fluid out of small blood vessels and into the extravascular fluid compartment, accounting for the inflammatory edema.
Leukocytic exudation occurs in the following sequence. First, the leukocytes move to the endothelial lining of the small blood vessels (margination) and line the endothelium in a tightly packed formation (pavementing). Eventually, these leukocytes move through the endothelial spaces and escape into the extravascular space (emigration). Once they are outside the blood vessels they are free to move and, by , are drawn to the site of injury. Accumulations of neutrophils and macrophages at the area of inflammation act to neutralize foreign particles by phagocytosis.
Chemical mediators of the inflammatory process include a variety of substances originating in the plasma and the cells of uninjured tissue, and possibly from the damaged tissue. The major kinds of mediators are (1) vasoactive amines, such as and serotonin; (2) plasma endopeptidases that comprise three interrelated systems, the kinin system that produces , the complement system that produces proteins that interact with antigen--antibody complexes and mediate immunologic injury and inflammation, and the clotting system that increases vascular permeability and chemotactic activity for the leukocytes; (3) prostaglandins, which can reproduce several aspects of the inflammatory process; (4) neutrophil products; (5) lymphocyte factors; and (6) other mediators, such as slow-reacting substance of anaphylaxis and endogenous pyrogen.
Hormonal Response. Some hormones, such as , have an action that limits inflammation to a local reaction while others are proinflammatory. Thus, the endocrine system has a regulatory effect on the process of inflammation so that it can be balanced and beneficial in the body's attempts to recover from injury.
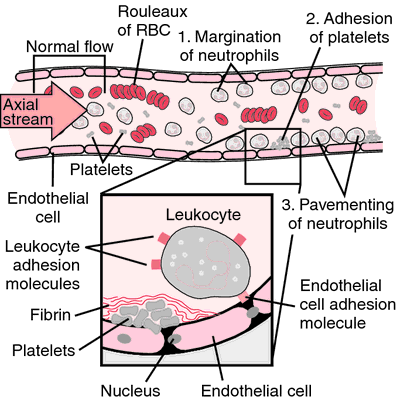
Cellular changes in inflammation. 1, Margination of neutrophils brings these inflammatory cells in close contact with the endothelium. 2, Adhesion of platelets results in the release of mediators of inflammation and coagulation. Fibrin strands are the first signs of clot formation. 3, Pavementing of leukocytes is mediated by adhesion molecules activated by the mediators of inflammation released from platelets and leukocytes. RBC, red blood cells. From Damjanov, 2000.
acute inflammation inflammation, usually of sudden onset, marked by the classical signs of heat, redness, swelling, pain, and loss of function, and in which vascular and exudative processes predominate.
catarrhal inflammation a form affecting mainly a mucous surface, marked by a copious discharge of mucus and epithelial debris.
chronic inflammation prolonged and persistent inflammation marked chiefly by new connective tissue formation; it may be a continuation of an acute form or a prolonged low-grade form.
exudative inflammation one in which the prominent feature is an exudate.
fibrinous inflammation one marked by an exudate of coagulated fibrin.
granulomatous inflammation a form, usually chronic, attended by formation of granulomas.
interstitial inflammation inflammation affecting chiefly the stroma of an organ.
parenchymatous inflammation inflammation affecting chiefly the essential tissue elements of an organ.
productive inflammation (proliferative inflammation) one leading to the production of new connective tissue fibers.
pseudomembranous inflammation an acute inflammatory response to a powerful necrotizing toxin (such asdiphtheria toxin), characterized by formation on a mucosal surface of a false membrane composed of precipitated fibrin, necrotic epithelium, and inflammatory leukocytes.
serous inflammation one producing a serous exudate.
subacute inflammation a condition intermediate between chronic and acute inflammation, exhibiting some of the characteristics of each.
suppurative inflammation one marked by pus formation.
toxic inflammation one due to a poison, e.g., a bacterial product.
traumatic inflammation one that follows a wound or injury.
ulcerative inflammation that in which necrosis on or near the surface leads to loss of tissue and creation of a local defect (ulcer).
Miller-Keane Encyclopedia and Dictionary of Medicine, Nursing, and Allied Health, Seventh Edition. © 2003 by Saunders, an imprint of Elsevier, Inc. All rights reserved.
in·flam·ma·tion
(in'flă-mā'shŭn), Avoid the misspelling inflamation.
A fundamental pathologic process consisting of a dynamic complex of histologically apparent cytologic changes, cellular infiltration, and mediator release that occurs in the affected blood vessels and adjacent tissues in response to an injury or abnormal stimulation caused by a physical, chemical, or biologic agent, including the local reactions and resulting morphologic changes; the destruction or removal of the injurious material; and the responses that lead to repair and healing. The so-called cardinal signs of inflammation are rubor, redness; calor, heat (or warmth); tumor, swelling; and dolor, pain; a fifth sign, functio laesa, inhibited or lost function, is sometimes added. All these signs may be observed in certain instances, but none is necessarily always present.
[L. inflammo, pp. -atus, fr. in, in, + flamma, flame]
Farlex Partner Medical Dictionary © Farlex 2012
inflammation
(ĭn′flə-mā′shən)
n.
1. The act of inflaming or the state of being inflamed.
2. A localized protective reaction of tissue to irritation, injury, or infection, characterized by pain, redness, swelling, and sometimes loss of function.
The American Heritage® Medical Dictionary Copyright © 2007, 2004 by Houghton Mifflin Company. Published by Houghton Mifflin Company. All rights reserved.
inflammation
A response to injury which is characterized by pain, swelling, heat, redness, and/or loss of function. See Round cellinflammation.
McGraw-Hill Concise Dictionary of Modern Medicine. © 2002 by The McGraw-Hill Companies, Inc.
in·flam·ma·tion
(in'flă-mā'shŭn)
A fundamental, stereotyped complex of cytologic and chemical reactions that occur in affected blood vessels and adjacent tissues in response to an injury or abnormal stimulation caused by a physical, chemical, or biologic agent. Redness (rubor), heat (calor), swelling (tumor), and pain (dolor) are signs generally associated with inflammation.
[L. inflammo, pp. -atus, fr. in, in, + flamma, flame]
Medical Dictionary for the Health Professions and Nursing © Farlex 2012
inflammation
The response of living tissue to injury, featuring widening of blood vessels, with redness, heat, swelling and pain-the cardinal signs ‘rubor’, ‘calor’, ‘tumor’ and ‘dolor’ of the first century physician Celsus. Inflammation also involves loss of function and is the commonest of all the disease processes. It is expressed by the ending ‘-itis’. Inflammation involves release of PROSTAGLANDINS which strongly stimulate pain nerve endings. It is, in general, protective and assists the immune system to restore normality, but persistent (chronic) inflammation may lead to the formation of undesirable scar tissue.
Collins Dictionary of Medicine © Robert M. Youngson 2004, 2005
inflammation
a local response to injury or damage, by which HISTAMINES are released that trigger a number of effects including dilation of blood vessels, and the invasion of blood proteins, blood fluid and LEUCOCYTES into the tissues to combat invading bacteria.
Collins Dictionary of Biology, 3rd ed. © W. G. Hale, V. A. Saunders, J. P. Margham 2005
Inflammation
The body's immune reaction to presumed foreign substances like germs. Inflammation is characterized by increased blood supply and activation of defense mechanisms. It produces redness, swelling, heat, and pain.
Mentioned in: Acetaminophen, , Analgesics, Opioid, Ankylosing Spondylitis, , Antiarrhythmic Drugs, Antiasthmatic Drugs, , Antibiotics, Topical, Antigastroesophageal Reflux Drugs, Antimigraine Drugs, Antiprotozoal Drugs, Antiretroviral Drugs, Antirheumatic Drugs, Antispasmodic Drugs, Antiulcer Drugs, Aspirin, , Buerger's Disease, Bursitis, Cancer Therapy, Supportive, Canker Sores, Cellulitis, , Corneal Ulcers, , Costochondritis, Crohn's Disease, Dermatomyositis, , Encephalitis, , Exophthalmos, Fluoroquinolones, , Graft-vs.-Host Disease, Hyperlipoproteinemia, Immunologic Therapies, Immunosuppressant Drugs, Keratitis, Leukocytosis, , Nonsteroidal Anti-Inflammatory Drugs, Periodontal Disease, Physical Allergy, Pleurisy, Pulmonary Fibrosis, Q Fever, Relapsing Polychondritis, Rheumatic Fever, Sulfonamides, Trichinosis, Ulcerative Colitis, Vaginal Pain, Vasculitis
Gale Encyclopedia of Medicine. Copyright 2008 The Gale Group, Inc. All rights reserved.
inflammation
A complex reaction that occurs in response to injury, infection, irritation, toxicity or hypersensitivity. The reaction is characterized by redness, heat, pain and swelling to different degrees. Treatment depends on the cause. See antiinflammatory drug; .
Millodot: Dictionary of Optometry and Visual Science, 7th edition. © 2009 Butterworth-Heinemann
in·flam·ma·tion
(in'flă-mā'shŭn) Avoid the misspelling inflamation.
Fundamental pathologic process consisting of a dynamic complex of histologically apparent cytologic changes, cellular infiltration, and mediator release that occurs in the affected blood vessels and adjacent tissues in response to an injury or abnormal stimulation caused by a physical, chemical, or biologic agent.
[L. inflammo, pp. -atus, fr. in, in, + flamma, flame]
Medical Dictionary for the Dental Professions © Farlex 2012
Patient discussion about Inflammation
Q. What causes inflammation of the knee joint?
A. It depends on many things - the age of the person, other diseases he or she may have, whether he experienced any trauma to the joint, drugs or other substances he or she uses. Generally speaking, it may be caused by an infection (usually after trauma, very painful and abrupt inflammation, necessitates rapid treatment), rheumatologic diseases (such as rheumatoid arthritis or others, reaction to drugs or as a feature of other diseases.
You may read more here: http://en.wikipedia.org/wiki/Arthritis
Q. what is fragments of endocervical glandular mucosa with inflammation and squamous metaplasia fragments of endocervical glandular mucosa
A. It means that part of the mucose on the cervix area has changes from a certain kind of mucose cells to another, and that there is a bit of an inflammation around it. This should be brought to the knowledge of a gynecologist and be monitored by him/her.
Q. Does anyone know how to relieve chronic back pain due to inflammation and arthritis? I have tried OTC arthritis pain meds they don't offer much relief for me. I have had surgery for herniated disc. My doctor says that there is a lot of inflammation and arthritis in my back. You can't get Vioxx anymore. Is there an alternative?
A. there also is a drug called diclofenac(cataflam) ask your DR.
More discussions about Inflammation
This content is provided by iMedix and is subject to iMedix Terms. The Questions and Answers are not endorsed or recommended and are made available by patients, not doctors.