Hypertension: Practice Essentials, Background, Pathophysiology (original) (raw)
Practice Essentials
High blood pressure (BP), or hypertension, is defined by two levels by the 2017 American College of Cardiology/American Heart Association (ACC/AHA) guidelines [1, 2] : (1) elevated BP, with a systolic pressure (SBP) between 120 and 129 mm Hg and diastolic pressure (DBP) less than 80 mm Hg, and (2) stage 1 hypertension, with an SBP of 130 to 139 mm Hg or a DBP of 80 to 89 mm Hg.
Hypertension is the most common primary diagnosis in the United States. [3] It affects approximately 86 million adults (≥20 years) in the United States [4] and is a major risk factor for stroke, myocardial infarction, vascular disease, and chronic kidney disease.
Signs and symptoms of hypertension
The 2017 ACC/AHA guidelines provide the following definitions and classifications of elevated BP and stages of hypertension [1, 2] :
- Elevated BP with a systolic pressure between 120 and 129 mm Hg and diastolic pressure less than 80 mm Hg
- Stage 1 hypertension, with a systolic pressure of 130 to 139 mm Hg or a diastolic pressure of 80 to 89 mm Hg
- Stage 2 hypertension, with a systolic pressure of 140 mm Hg or greater or a diastolic pressure of 90 mm Hg or greater
Of note, the International Society of Hypertension (ISH) and the European Society of Cardiology (ESC) have a higher BP threshold, defining hypertension as an SBP of 140 mm Hg or greater and/or a DBP of 90 mm Hg or above. [5, 6]
Hypertension may be primary, which may develop as a result of a variety of environmental or genetic causes, or it may be secondary to renal, vascular, and endocrine causes. Primary or essential hypertension accounts for 90-95% of adult cases, and secondary hypertension accounts for 2-10% of adult cases.
See Presentation for more detail.
Diagnosis of hypertension
The evaluation of hypertension involves accurately measuring the patient’s BP, performing a focused medical history and physical examination, and obtaining results of routine laboratory studies. [7, 8] A 12-lead electrocardiogram should also be obtained. These steps can help determine the following [7, 8, 9] :
- Presence of end-organ disease
- Possible causes of hypertension
- Cardiovascular risk factors
- Baseline values for judging biochemical effects of therapy
Other studies may be obtained on the basis of clinical findings or in individuals with suspected secondary hypertension and/or evidence of target-organ disease, such as complete blood cell (CBC) count, basic metabolic panel; chest radiograph, transthoracic echocardiogram; and urine microalbumin. [7]
See Workup for more detail.
Management of hypertension
Many guidelines exist for the management of hypertension. Most groups, including the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood (JNC), the American Diabetes Associate (ADA), and the ACC/AHA recommend lifestyle modification as the first step in managing hypertension.
Lifestyle modifications
JNC 7 recommendations to lower BP and decrease cardiovascular disease risk include the following, with greater results achieved when two or more lifestyle modifications are combined [7] :
- Weight loss (range of approximate SBP reduction, 5-20 mm Hg per 10 kg)
- Limit alcohol intake to no more than 1 oz (30 mL) of ethanol per day for men or 0.5 oz (15 mL) of ethanol per day for women and people of lighter weight (range of approximate SBP reduction, 2-4 mm Hg)
- Reduce sodium intake to no more than 100 mmol/day (2.4 g sodium or 6 g sodium chloride; range of approximate SBP reduction, 2-8 mm Hg) [10]
- Maintain adequate intake of dietary potassium (approximately 90 mmol/day)
- Maintain adequate intake of dietary calcium and magnesium for general health
- Stop smoking and reduce intake of dietary saturated fat and cholesterol for overall cardiovascular health
- Engage in aerobic exercise at least 30 minutes daily for most days (range of approximate SBP reduction, 4-9 mm Hg)
The ACC/AHA recommends a diet that is low in sodium, is high in potassium, and promotes the consumption of fruits, vegetables, and low-fat dairy products for reducing BP and lowering the risk of cardiovascular events. Other recommendations include increasing physical activity (30 minutes or more of moderate intensity activity on a daily basis) and losing weight (persons with overweight and obesity). [1]
The 2018 ESC and the European Society of Hypertension (ESH) guidelines recommend a low-sodium diet (limited to 2 g per day) as well as reducing body-mass index (BMI) to 20-25 kg/m2 and waist circumference (to < 94 cm in men and < 80 cm in women). [11] The 2023 ESH guidelines for managing arterial hypertension indicates a linear reduction in BP with sodium intake limited to as low as 800 mg/day; when dietary sodium intake fell from about 3.6 g/day to around 2.7 g/day, there was an associated 18-26% fall in cardiovascular disease. [6]
Pharmacologic therapy
If lifestyle modifications are insufficient to achieve the goal BP, there are several drug options for treating and managing hypertension. Thiazide diuretics, an angiotensin-converting enzyme inhibitor (ACEI)/angiotensin receptor blocker (ARB), or calcium channel blocker (CCB) are the preferred first-line agents. [1] Often, patients require several antihypertensive agents to achieve adequate BP control.
Compelling indications for specific agents include comorbidities such as heart failure, ischemic heart disease, chronic kidney disease, and diabetes. Drug intolerability or contraindications may also be factors. [7]
The following are drug class recommendations for compelling indications based on various clinical trials [7] :
- Heart failure: Diuretic, beta-blocker, ACE inhibitor/ARB/ARNI, aldosterone antagonist
- Following myocardial infarction: Beta-blocker, ACE inhibitor
- Diabetes: ACE inhibitor/ARB
- Chronic kidney disease: ACE inhibitor/ARB
Although the 2017 ACC/AHA guidelines favor CCBs or thiazide diuretics in the absence of other indications as first-line medications in Black hypertensive populations, [1] reports in relatively recent years have raised questions on the benefits of race or ethnicity-based medication prescribing. [12, 13, 14, 15, 16, 17, 18, 19, 20]
See Treatment and Medication for more details.

Background
Hypertension is the most common primary diagnosis in the United States, [3] and it is one of the most common worldwide diseases afflicting humans. It is a major risk factor for stroke, myocardial infarction, vascular disease, and chronic kidney disease. Despite extensive research over the past several decades, the etiology of most cases of adult hypertension is still unknown, and control of blood pressure (BP) is suboptimal in the general population. Due to the associated morbidity and mortality and cost to society, preventing and treating hypertension is an important public health challenge. Fortunately, relatively recent advances and trials in hypertension research are leading to an increased understanding of the pathophysiology of hypertension and the promise for novel pharmacologic and interventional treatments for this widespread disease.
According to the American Heart Association (AHA), approximately 86 million adults (34%) in the United States are affected by hypertension, which is defined as a systolic BP (SBP) of 130 mm Hg or more or a diastolic BP (DBP) of 80 mm Hg or more, taking antihypertensive medication, or having been told by clinicians on at least two occasions as having hypertension. [1] Substantial efforts have been made to enhance awareness and treatment of hypertension. However, a National Health Examination Survey (NHANES) spanning 2011-2014 revealed that 34% of US adults aged 20 years and older are hypertensive and NHANES 2013-2014 data showed that 15.9% of these hypertensive adults are unaware they are hypertensive; these data have increased from NHANES 2005-2006 data that showed 29% of US adults aged 18 years and older were hypertensive and that 7% of these hypertensive adults had never been told that they had hypertension. [4]
Of those with elevated BP, 78% were aware they were hypertensive, 68% were being treated with antihypertensive agents, and only 64% of treated individuals had controlled hypertension. [4] In addition, previous data from NHANES estimated that 52.6% (NHANES 2009-2010) to 55.8% (NHANES 1999-2000) of adults aged 20 years and older have elevated BP or stage 1 hypertension, defined as an untreated SBP of 120-139 mm Hg or untreated DBP of 80-89 mm Hg. [4] (See Epidemiology.)
Hypertension is the most important modifiable risk factor for coronary heart disease (the leading cause of death in North America), stroke (the third leading cause), congestive heart failure, end-stage renal disease, and peripheral vascular disease. Therefore, healthcare professionals must not only identify and treat patients with hypertension but also promote a healthy lifestyle and preventive strategies to decrease the prevalence of hypertension in the general population. (See Treatment.)
Definition and classification
The definition of abnormally high blood pressure (BP) has varied among guidelines. Nevertheless, the relationship between systemic arterial pressure and morbidity appears to be quantitative rather than qualitative. A level for high BP must be agreed upon in clinical practice for screening patients with hypertension and for instituting diagnostic evaluation and initiating therapy. Because the risk to an individual patient may correlate with the severity of hypertension, a classification system is essential for making decisions about aggressiveness of treatment or therapeutic interventions. (See Presentation.)
Based on recommendations of the 2017 ACC/AHA guidelines, the classification of BP (expressed in mm Hg) for adults aged 18 years or older is as follows [1, 2] :
- Normal: Systolic lower than 120 mm Hg and diastolic lower than 80 mm Hg
- Elevated: Systolic 120-129 mm Hg and diastolic lower than 80 mm Hg
- Stage 1: Systolic 130-139 mm Hg or diastolic 80-89 mm Hg
- Stage 2: Systolic 140 mm Hg or greater or diastolic 90 mm Hg or greater
The classification above is based on the average of two or more readings taken at each of two or more visits after the initial screening. [1] Normal BP with respect to cardiovascular risk is less than 120/80 mm Hg. However, unusually low readings should be evaluated for clinical significance.
From another perspective, hypertension may be categorized as either primary or secondary. Primary (essential) hypertension is diagnosed in the absence of an identifiable secondary cause. Approximately 90-95% of adults with hypertension have primary hypertension, whereas secondary hypertension accounts for about 5-10% of the cases. [21] However, secondary forms of hypertension, such as primary hyperaldosteronism, account for as much as 30% of resistant hypertension (hypertension in which BP is >140/90 mm Hg despite the use of medications from three or more drug classes, one of which is a thiazide diuretic).
Especially severe cases of hypertension, or hypertensive crises, are defined as a BP of more than 180/120 mm Hg and may be further categorized as hypertensive emergencies or urgencies. Hypertensive emergencies are characterized by evidence of impending or progressive target organ dysfunction, whereas hypertensive urgencies are those situations without target organ dysfunction. [7]
Acute end-organ damage in the setting of a hypertensive emergency may include the following [22] :
- Neurologic: hypertensive encephalopathy, cerebral vascular accident/cerebral infarction, subarachnoid hemorrhage, intracranial hemorrhage
- Cardiovascular: myocardial ischemia/infarction, acute left ventricular dysfunction, acute pulmonary edema, aortic dissection, unstable angina pectoris
- Other: acute renal failure/insufficiency, retinopathy, eclampsia, microangiopathic hemolytic anemia
With the advent of antihypertensives, the incidence of hypertensive emergencies has declined from 7% to approximately 1%. [23] In addition, the 1-year survival rate associated with this condition has increased from only 20% (prior to 1950) to more than 90% with appropriate medical treatment. [24] (See Medication.)

Pathophysiology
The pathogenesis of primary hypertension is multifactorial and complex. [25] Multiple factors modulate the blood pressure (BP) including humoral mediators, vascular reactivity, circulating blood volume, vascular caliber, blood viscosity, cardiac output, blood vessel elasticity, and neural stimulation. The pathogenesis of primary hypertension involves multiple factors, including genetic predisposition, excess dietary salt intake, adrenergic tone, and renal sodium and water handling that interact to produce BP elevations. Although genetics contribute, with rare exceptions this condition is polygenic. Emerging evidence suggests a role for immune cell activation and the microbiome in the pathogenesis of hypertension. [26]
The natural history of primary hypertension evolves from occasional to established hypertension. After a long asymptomatic period, persistent hypertension develops into complicated hypertension, in which end-organ damage to the aorta and small arteries, heart, kidneys, retina, and central nervous system is evident.
A general progression of primary hypertension is as follows:
- Prehypertension in persons aged 10-30 years (by increased cardiac output)
- Early hypertension in persons aged 20-40 years (in which increased peripheral resistance is prominent)
- Established hypertension in persons aged 30-50 years
- Complicated hypertension in persons aged 40-60 years
As evident from the above, younger individuals may present with hypertension associated with an elevated cardiac output (high-output hypertension). High-output hypertension results from volume and sodium retention by the kidney, leading to increased stroke volume and, often, with cardiac stimulation by adrenergic hyperactivity. Systemic vascular resistance is generally not increased at such earlier stages of hypertension. As hypertension is sustained, however, vascular adaptations including remodeling, vasoconstriction, and vascular rarefaction occur, leading to increased systemic vascular resistance. In this situation, cardiac output is generally normal or slightly reduced, and circulating blood volume is normal.
Cortisol reactivity, an index of hypothalamic-pituitary-adrenal function, may be another mechanism by which psychosocial stress is associated with future hypertension. [27] In a prospective sub-study of the Whitehall II cohort, with 3 years follow-up of an occupational cohort in previously healthy patients, investigators reported 15.9% of the patient group developed hypertension in response to laboratory-induced mental stressors, and there was an association between cortisol stress reactivity and incident hypertension. [27]
Investigations into the pathophysiology of hypertension, both in animals and humans, have revealed that hypertension may have an immunologic basis. Studies have revealed that hypertension is associated with renal infiltration of immune cells and that pharmacologic immunosuppression (such as with the drug mycophenolate mofetil) or pathologic immunosuppression (such as occurs with human immunovirus [HIV] deficiency) results in reduced BP in animals and humans. Evidence suggests that T lymphocytes and T-cell derived cytokines (eg, interleukin 17, tumor necrosis factor alpha) play an important role in hypertension. [28, 29]
One hypothesis is that prehypertension results in oxidation of lipids such as arachidonic acid that leads to the formation of isoketals or isolevuglandins, which function as neoantigens, which are then presented to T cells, leading to T-cell activation and infiltration of critical organs (eg, kidney, vasculature). [30] This results in persistent or severe hypertension and end-organ damage. Sympathetic nervous system activation and noradrenergic stimuli have also been shown to promote T-lymphocyte activation and infiltration, and contribute to the pathophysiology of hypertension. [31, 32, 33]

Etiology
Hypertension can be primary, which may develop as a result of environmental or genetic causes, or secondary, which has multiple etiologies, including renal, vascular, and endocrine causes. Primary or essential hypertension accounts for 90-95% of adult cases, and a small percentage of patients (2-10%) have a secondary cause. Hypertensive emergencies are most often precipitated by inadequate medication or poor adherence.
Environmental and genetic/epigenetic causes
Hypertension develops secondary to environmental factors, as well as multiple genes, whose inheritance appears to be complex. [24, 34] Furthermore, obesity, diabetes, and heart disease also have genetic components and contribute to hypertension. Epidemiologic studies using twin data and data from Framingham Heart Study families reveal that blood pressure (BP) has a substantial heritable component, ranging from 33% to 57%. [35, 36, 37]
In an attempt to elucidate the genetic components of hypertension, multiple genome wide association studies (GWAS) have been conducted, revealing multiple gene loci in known pathways of hypertension as well as some novel genes with no known link to hypertension as of yet. [38] Further research into these novel genes, some of which are immune-related, will likely increase the understanding of the pathophysiology of hypertension, allowing for increased risk stratification and individualized treatment.
Epigenetic phenomena, such as DNA methylation and histone modification, have also been implicated in the pathogenesis of hypertension. For example, a high-salt diet appears to unmask nephron development caused by methylation. Maternal water deprivation and protein restriction during pregnancy increase renin-angiotensin expression in the fetus. Mental stress induces a DNA methylase, which enhances autonomic responsiveness. The pattern of serine protease inhibitor gene methylation predicts preeclampsia in pregnant women. [39]
Despite these genetic findings, targeted genetic therapy seems to have little impact on hypertension. In the general population, not only does it appear that individual and joint genetic mutations have very small effects on BP levels, but it has not been shown that any of these genetic abnormalities are responsible for any applicable percentage of cases of hypertension in the general population. [40]
Secondary causes of hypertension related to single genes are very rare. They include Liddle syndrome, glucocorticoid-remediable hyperaldosteronism, 11 beta-hydroxylase and 17 alpha-hydroxylase deficiencies, syndrome of apparent mineralocorticoid excess, and pseudohypoaldosteronism type II. [7]
Causes of secondary hypertension
Renal causes (2.5-6%) of hypertension include the renal parenchymal diseases and renal vascular diseases, as follows:
- Polycystic kidney disease
- Chronic kidney disease
- Urinary tract obstruction
- Renin-producing tumor
- Liddle syndrome
- Nephritic syndrome/glomerulonephritis
Renovascular hypertension (RVHT) causes 0.2-4% of cases of hypertension. Since the 1934 seminal experiment by Goldblatt et al, [41] RVHT has become increasingly recognized as an important cause of clinically atypical hypertension and chronic kidney disease—the latter by virtue of renal ischemia. The coexistence of renal arterial vascular (ie, renovascular) disease and hypertension roughly defines this type of secondary hypertension. More specific diagnoses are made retrospectively when hypertension is improved after intravascular intervention.
Vascular causes include the following:
- Coarctation of the aorta
- Vasculitis
- Collagen vascular disease
Endocrine causes may account for the largest proportion of secondary hypertension (10-20%) and include exogenous or endogenous hormonal imbalances. Exogenous causes include administration of steroids. Primary hyperaldosteronism is the most common endogenous hormone abnormality causing hypertension. Approximately 20% of cases of confirmed resistant hypertension are due to primary hyperaldosteronism. Pheochromocytomas and paragangliomas are rare, chromaffin cell tumors, that produce catecholamines. The prevalence of these tumors is 0.01-0.2% in the hypertensive population, but up to 4% in the resistant hypertension population. Cushing syndrome is caused by excess glucocorticoids and can present in a variety of ways, including weight gain, menstrual irregularities, mood disorders, muscle weakness, abdominal striae, and enlargement of the pad fat on the dorsal neck. Small cohort studies suggest a high prevalence of hypertension in patients with Cushing syndrome; further studies are needed for accurate correlation. [42]
Another common endocrine cause of hypertension is oral contraceptive use, likely due to activation of the renin-angiotensin-aldosterone system (RAAS). This is caused by increased hepatic synthesis of angiotensinogen in response to the estrogen component of oral contraceptives. Approximately 5% of women taking oral contraceptives may develop hypertension, which abates within 6 months after discontinuation. The risk factors for oral contraceptive–associated hypertension include coexistent renal disease, familial history of primary hypertension, age older than 35 years, and obesity.
Exogenous administration of steroids used for therapeutic purposes also increases BP, especially in susceptible individuals, mainly by volume expansion. Nonsteroidal anti-inflammatory drugs (NSAIDs) may also have adverse effects on BP. NSAIDs block both cyclooxygenase-1 (COX-1) and COX-2 enzymes. The inhibition of COX-2 can inhibit its natriuretic effect, which, in turn, increases sodium retention. NSAIDs also inhibit the vasodilating effects of prostaglandins and the production of vasoconstricting factors—namely, endothelin-1. These effects can contribute to the induction of hypertension in a normotensive or controlled hypertensive patient.
Endogenous hormonal causes include the following:
- Primary hyperaldosteronism
- Cushing syndrome
- Pheochromocytoma
- Congenital adrenal hyperplasia
Neurogenic causes include the following:
- Brain tumor
- Autonomic dysfunction
- Sleep apnea
- Intracranial hypertension
Drugs and toxins that cause hypertension include the following:
- Alcohol
- Cocaine
- Cyclosporine, tacrolimus
- NSAIDs
- Erythropoietin
- Adrenergic medications
- Decongestants containing ephedrine
- Herbal remedies and candy that contain licorice (including licorice root) or ephedrine (and ephedra)
- Nicotine
Other causes include the following:
- Hyperthyroidism and hypothyroidism
- Hypercalcemia
- Hyperparathyroidism
- Acromegaly
- Obstructive sleep apnea
- Pregnancy
Obstructive sleep apnea (OSA) is a common but frequently undiagnosed sleep-related breathing disorder defined as an average of at least five apneic and hypopneic episodes per sleep hour, with associated symptoms, including excessive daytime sleepiness. [43] Multiple studies have shown OSA to be an independent risk factor for the development of primary hypertension, even after adjusting for age, sex, and degree of obesity.
Approximately half of individuals with hypertension have OSA, and approximately half with OSA have hypertension. Ambulatory BP monitoring normally reveals a "dip" in BP of at least 10% during sleep. However, if a patient is a "nondipper," the chances that the patient has OSA is increased. Nondipping is thought to be caused by frequent apneic/hypopneic episodes that end with arousals associated with marked spikes in BP that last for several seconds. Apneic episodes are associated with striking increases in sympathetic nerve activity and enormous elevations of BP. Individuals with sleep apnea have increased cardiovascular mortality, in part likely related to the high incidence of hypertension.
Although treatment of sleep apnea with continuous airway positive pressure (CPAP) would logically seem to improve cardiovascular outcomes and hypertension, studies evaluating this mode of therapy have been disappointing. A 2016 review of several studies indicated that CPAP either had no effect or a modest BP-lowering effect. [44] Findings from the SAVE (Sleep Apnea Cardiovascular Endpoints) study showed no effect of CPAP therapy on BP above usual care. [45] It is likely that patients with sleep apnea have other etiologies of hypertension, including obesity, hyperaldosteronism, increased sympathetic drive, and activation of the renin/angiotensin system that contribute to their hypertension. Although CPAP remains an effective therapy for other aspects of sleep apnea, it should not be expected to normalize BP in the majority of patients.
Causes of hypertensive emergencies
The most common hypertensive emergency is a rapid unexplained rise in BP in patients with chronic essential hypertension. Most patients who develop hypertensive emergencies have a history of inadequate hypertensive treatment or an abrupt discontinuation of their medications. [46, 47]
Other causes of hypertensive emergencies include the use of recreational drugs, abrupt clonidine withdrawal, post pheochromocytoma removal, and systemic sclerosis, as well as the following:
- Renal parenchymal disease: chronic pyelonephritis, primary glomerulonephritis, tubulointerstitial nephritis (accounts for 80% of all secondary causes)
- Systemic disorders with renal involvement: systemic lupus erythematosus, systemic sclerosis, vasculitis
- Renovascular disease: atherosclerotic disease, fibromuscular dysplasia, polyarteritis nodosa
- Endocrine disease: pheochromocytoma, Cushing syndrome, primary hyperaldosteronism
- Drugs: cocaine, [48] amphetamines, cyclosporine, clonidine (withdrawal), phencyclidine, diet pills, oral contraceptive pills
- Drug interactions: monoamine oxidase inhibitors with tricyclic antidepressants, antihistamines, or tyramine-containing food
- Central nervous system (CNS) factors: CNS trauma or spinal cord disorders, such as Guillain-Barré syndrome
- Coarctation of the aorta
- Preeclampsia/eclampsia
- Postoperative hypertension

Epidemiology
Hypertension is a worldwide epidemic; accordingly, its epidemiology has been well studied. Data from the US National Health and Nutrition Examination Survey (NHANES) spanning 2011-2014 found that of those in the population aged 20 years or older, an estimated 86 million adults had hypertension, with a prevalence of 34%. [4]
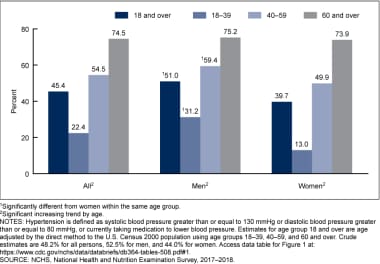
More recently, 2020 data from the Centers for Disease Control and Prevention's (CDC) National Center for Health Statistics (NCHS) spanning 2017-2018 show a 45.4% prevalence of hypertension among those aged 18 and older (see the following image; prevalence by sex and age). [49] Of the US adult population diagnosed with hypertension, a higher prevalence exists in males (51%) relative to females (39.7%).
Hypertension. Prevalence of hypertension among adults aged 18 and older, by sex and age: United States, 2017-2018. Courtesy of the Centers for Disease Control and Prevention (CDC), National Center for Health Statistics (NCHS).
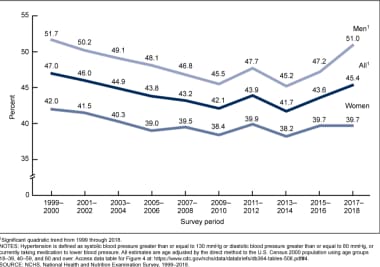
There has been an interesting trend in the prevalence of hypertension, which fell in the early 2000s but began trending upward in 2014 (see the image below, which shows the prevalence of hypertension by year and sex). [49] The prevalence of hypertension declined during the first decade of this century, but it has since increased, particularly in men.
Hypertension. Age-adjusted trends in hypertension among adults aged 18 and older: United States, 1999–2018. Courtesy of the Centers for Disease Control and Prevention (CDC), National Center for Health Statistics (NCHS).
Globally, an estimated 26% of the world’s population (972 million people) has hypertension, and the prevalence is expected to increase to 29% by 2025, driven largely by increases in economically developing nations. [50] The high prevalence of hypertension exacts a tremendous public health burden. For example, as a primary contributor to heart disease and stroke, the first and third leading causes of death worldwide, respectively, high BP was the top modifiable risk factor for disability adjusted life-years lost worldwide in 2013. [51, 52]
Hypertension and sex- and age-related statistics
Females have a lower prevalence of hypertension until the fifth decade of life. Afterward, the prevalence of hypertension is increased in females compared to males. [1]
Hypertension and race and ethnicity
Black adults have among the highest rates of hypertension, with an increasing prevalence, in the United States and globally. [17, 18, 19, 53] Although White adults also have an increasing incidence of high BP, they develop this condition later in life than Black adults and have much lower average BPs. In fact, compared to hypertensive White persons, hypertensive Black individuals have a 1.3-fold higher rate of nonfatal stroke, a 1.8-fold higher rate of fatal stroke, a 1.5-fold higher mortality rate due to heart disease, and a 4.2-fold higher rate of end-stage renal disease (ESRD). [54]
Table 2, below, summarizes age-adjusted prevalence estimates from the National Health Interview Survey (NHIS) and the NCHS according to racial/ethnic groups and diagnosed conditions in individuals aged 18 years and older.
Table 2. NHIS/NCHS Age-Adjusted Prevalence Estimates in Individuals Aged 18 Years and Older in 2015. (Open Table in a new window)
| Race/Ethnic Group | Have Hypertension, % | Have Heart Disease, % | Have Coronary Heart Disease, % | Have Had a Stroke, % |
|---|---|---|---|---|
| White only | 23.8 | 11.3 | 5.6 | 2.4 |
| Black/African American | 34.4 | 9.5 | 5.4 | 3.7 |
| Hispanic/Latino | 23.0 | 8.2 | 5.1 | 2.4 |
| Asian | 20.6 | 7.1 | 3.7 | 1.4 |
| American Indian/Alaska Native | 28.4 | 13.7 | 9.3 | 2.2 (this number is considered unreliable) |
| Source: Summary health statistics: National Health Interview Survey, 2015. Available at: https://ftp.cdc.gov/pub/Health_Statistics/NCHS/NHIS/SHS/2015_SHS_Table_A-1.pdf. Accessed: November 14, 2016.NCHS = National Center for Health Statistics; NHIS = National Health Interview Survey. |

Prognosis
Most individuals diagnosed with hypertension will have increasing blood pressure (BP) as they age. Untreated hypertension is notorious for raising the mortality risk and is often described as a silent killer. Mild to moderate hypertension, if left untreated, may be associated with a risk of atherosclerotic disease in 30% of people and of organ damage in 50% of persons within 8-10 years after onset. Patients with resistant hypertension are also at higher risk for poor outcomes, particularly those with certain comorbidities (eg, chronic kidney disease, ischemic heart disease). [55] Patients with resistant hypertension who have lower BP appear to have a reduced risk for some cardiovascular events (eg, incident stroke, coronary heart disease, or heart failure). [55]
Death from ischemic heart disease or stroke increases progressively as BP increases. For every 20 mm Hg systolic or 10 mm Hg diastolic increase in BP above 115/75 mm Hg, mortality doubles for both ischemic heart disease and stroke. [7]
Hypertensive retinopathy was associated with an increased long-term risk of stroke, even in patients with well-controlled BP, in a report of 2907 adults with hypertension participating in the Atherosclerosis Risk in Communities (ARIC) study. [56, 57] Increasing severity of hypertensive retinopathy was associated with an increased risk of stroke; the stroke risk was 1.35 in the mild retinopathy group and 2.37 in the moderate/severe group.
In a meta-analysis of pooled data from 19 prospective cohort studies involving 762,393 patients, Huang et al reported that, after adjustment for multiple cardiovascular risk factors, prehypertension was associated with a 66% increased risk for stroke, compared with an optimal BP (< 120/80 mm Hg). [58, 59] Patients in the high range of prehypertension (130-139/85-89 mm Hg) had a 95% increased risk of stroke, compared to a 44% increased risk for those in the low range of prehypertension (120-129/80-84 mm Hg). [58, 59]
The morbidity and mortality of hypertensive emergencies depend on the extent of end-organ dysfunction on presentation and the degree to which BP is controlled subsequently. With BP control and medication adherence, the 10-year survival of patients with hypertensive crises approaches 70%. [60]
In the Framingham Heart Study, the age-adjusted risk of congestive heart failure was 2.3 times higher in men and 3 times higher in women when the highest BP was compared to the lowest BP. [61] Multiple Risk Factor Intervention Trial (MRFIT) data showed that the relative mortality risk for coronary artery disease was 2.3 to 6.9 times higher for persons with mild to severe hypertension than it was for persons with normal BP. [62] The relative risk for stroke ranged from 3.6 to 19.2. The population-attributable risk percentage for coronary artery disease varied from 2.3 to 25.6%, whereas the population-attributable risk for stroke ranged from 6.8% to 40%. [62]
The Framingham Heart Study also found a 72% increase in the risk of all-cause death and a 57% increase in the risk of any cardiovascular event in patients with hypertension who were also diagnosed with diabetes mellitus. [63]
Nephrosclerosis is one of the possible complications of long-standing hypertension. The risk of hypertension-induced end-stage renal disease is higher in Black patients, even when BP is under good control. Furthermore, patients with diabetic nephropathy who are hypertensive are also at high risk for developing end-stage renal disease.
Comparative data from the National Health Examination Survey (NHANES) I and III showed a decrease in mortality over time in hypertensive adults, but the mortality gap between hypertensive and normotensive adults remained high. [64]
Clinical trials have demonstrated the following benefits with antihypertensive therapy [7] :
- Average 35-40% reduction in stroke incidence
- Average 20-25% reduction in myocardial infarction
- Average greater than 50% reduction in heart failure
Moreover, it is estimated that 1 death is prevented per 11 patients treated for stage 1 hypertension and other cardiovascular risk factors when a sustained reduction of 12 mm Hg in systolic BP over 10 years is achieved. [7] However, for the same lowering in systolic BP reduction, it is estimated that 1 death is prevented per 9 patients treated when cardiovascular disease or end-organ damage is present. [7]

Patient Education
Hypertension is a lifelong disorder. For optimal control, a long-term commitment to lifestyle modifications and pharmacologic therapy is required. Therefore, repeated in-depth patient education and counseling not only improves compliance with medical therapy but also reduces cardiovascular risk factors.
Various strategies to decrease cardiovascular disease risk include the following:
- Prevention and treatment of obesity: An increase in body mass index (BMI) and waist circumference is associated with an increased risk of developing conditions with high cardiovascular risk, such as hypertension, diabetes mellitus, impaired fasting glucose, and left ventricular hypertrophy [65]
- Appropriate amounts of aerobic physical activity
- Diets low in salt, total fat, and cholesterol
- Adequate dietary intake of potassium, calcium, and magnesium
- Limited alcohol consumption
- Avoidance of cigarette smoking
- Avoidance of the use of illicit drugs, such as cocaine

- [Guideline] Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018 Jun. 71(6):e13-e115. [QxMD MEDLINE Link]. [Full Text].
- Jeffrey S. New ACC/AHA hypertension guidelines make 130 the new 140. Medscape Medical News. November 13, 2017. Available at https://www.medscape.com/viewarticle/888560. Accessed: November 18, 2017.
- Rivera SL, Martin J, Landry J. Acute and chronic hypertension: what clinicians need to know for diagnosis and management. Crit Care Nurs Clin North Am. 2019 Mar. 31(1):97-108. [QxMD MEDLINE Link].
- Benjamin EJ, Blaha MJ, Chiuve SE, et al, for the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics-2017 update: a report from the American Heart Association. Circulation. 2017 Mar 7. 135(10):e146-e603. [QxMD MEDLINE Link]. [Full Text].
- [Guideline] Unger T, Borghi C, Charchar F, et al. 2020 International Society of Hypertension global hypertension practice guidelines. Hypertension. 2020 Jun. 75(6):1334-57. [QxMD MEDLINE Link]. [Full Text].
- [Guideline] Mancia G, Kreutz R, Brunström M, et al, for The Task Force for the management of arterial hypertension of the European Society of Hypertension: Endorsed by the International Society of Hypertension (ISH) and the European Renal Association (ERA). 2023 ESH Guidelines for the management of arterial hypertension. J Hypertens. 2023 Dec 1. 41 (12):1874-2071. [QxMD MEDLINE Link]. [Full Text].
- Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003 Dec. 42(6):1206-52. [QxMD MEDLINE Link].
- Katakam R, Brukamp K, Townsend RR. What is the proper workup of a patient with hypertension?. Cleve Clin J Med. 2008 Sep. 75(9):663-72. [QxMD MEDLINE Link].
- Institute for Clinical Systems Improvement (ICSI). Hypertension diagnosis and treatment. Bloomington, Minn: Institute for Clinical Systems Improvement (ICSI); 2010.
- Whelton PK, Appel LJ, Sacco RL, et al. Sodium, blood pressure, and cardiovascular disease: further evidence supporting the American Heart Association sodium reduction recommendations. Circulation. 2012 Dec 11. 126(24):2880-9. [QxMD MEDLINE Link].
- [Guideline] Williams B, Mancia G, Spiering W, et al, for the ESC Scientific Document Group. 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J. 2018 Sep 1. 39 (33):3021-104. [QxMD MEDLINE Link]. [Full Text].
- Gopal DP, Okoli GN, Rao M. Re-thinking the inclusion of race in British hypertension guidance. J Hum Hypertens. 2022 Mar. 36(3):333-5. [QxMD MEDLINE Link]. [Full Text].
- Gopal DP, Francis R. Does race belong in the hypertension guidelines?. J Hum Hypertens. 2021 Oct. 35(10):940-1. [QxMD MEDLINE Link].
- Holt HK, Gildengorin G, Karliner L, Fontil V, Pramanik R, Potter MB. Differences in hypertension medication prescribing for Black Americans and their association with hypertension outcomes. J Am Board Fam Med. 2022 Jan-Feb. 35(1):26-34. [QxMD MEDLINE Link]. [Full Text].
- Apeles L. Race-based prescribing for Black people with high blood pressure shows no benefit. University of California San Francisco. Available at https://www.ucsf.edu/news/2022/01/422151/race-based-prescribing-black-people-high-blood-pressure-shows-no-benefit. January 18, 2022; Accessed: February 27, 2024.
- Abrahamowicz AA, Ebinger J, Whelton SP, Commodore-Mensah Y, Yang E. Racial and ethnic disparities in hypertension: barriers and opportunities to Improve Blood Pressure Control. Curr Cardiol Rep. 2023 Jan. 25 (1):17-27. [QxMD MEDLINE Link]. [Full Text].
- Hedgepeth C III. Discrimination, high blood pressure, and health disparities in African Americans. Harvard Health Blog. Available at https://www.health.harvard.edu/blog/discrimination-high-blood-pressure-and-health-disparities-in-african-americans-2020092120943. September 21, 2020; Accessed: February 27, 2023.
- Ogunniyi MO, Commodore-Mensah Y, Ferdinand KC. Race, ethnicity, hypertension, and heart disease: JACC focus seminar 1/9. J Am Coll Cardiol. 2021 Dec 14. 78 (24):2460-70. [QxMD MEDLINE Link]. [Full Text].
- Williamson L. The link between structural racism, high blood pressure and Black people's health. Heart.org. Available at https://www.heart.org/en/news/2021/04/15/the-link-between-structural-racism-high-blood-pressure-and-black-peoples-health. April 15, 2021; Accessed: February 27, 2024.
- Flack JM, Buhnerkempe MG. Race and antihypertensive drug therapy: edging closer to a new paradigm. Hypertension. 2022 Feb. 79 (2):349-51. [QxMD MEDLINE Link]. [Full Text].
- Hajjar I, Kotchen TA. Trends in prevalence, awareness, treatment, and control of hypertension in the United States, 1988-2000. JAMA. 2003 Jul 9. 290(2):199-206. [QxMD MEDLINE Link].
- Bianchi S, Bigazzi R, Campese VM. Microalbuminuria in essential hypertension: significance, pathophysiology, and therapeutic implications. Am J Kidney Dis. 1999 Dec. 34(6):973-95. [QxMD MEDLINE Link].
- Shayne PH, Pitts SR. Severely increased blood pressure in the emergency department. Ann Emerg Med. 2003 Apr. 41(4):513-29. [QxMD MEDLINE Link].
- Rhoades R, Planzer R. Human Physiology. 3rd ed. Fort Worth, TX: Saunders College Publishing; 1996.
- Gandhi SK, Powers JC, Nomeir AM, et al. The pathogenesis of acute pulmonary edema associated with hypertension. N Engl J Med. 2001 Jan 4. 344(1):17-22. [QxMD MEDLINE Link]. [Full Text].
- Harrison DG, Coffman TM, Wilcox CS. Pathophysiology of hypertension: the Mosaic Theory and beyond. Circ Res. 2021 Apr 2. 128(7):847-63. [QxMD MEDLINE Link]. [Full Text].
- Hamer M, Steptoe A. Cortisol responses to mental stress and incident hypertension in healthy men and women. J Clin Endocrinol Metab. 2012 Jan. 97(1):E29-34. [QxMD MEDLINE Link].
- Madhur MS, Lob HE, McCann LA, et al. Interleukin 17 promotes angiotensin II-induced hypertension and vascular dysfunction. Hypertension. 2010 Feb. 55(2):500-7. [QxMD MEDLINE Link]. [Full Text].
- Venegas-Pont M, Manigrasso MB, Grifoni SC, et al. Tumor necrosis factor-alpha antagonist etanercept decreases blood pressure and protects the kidney in a mouse model of systemic lupus erythematosus. Hypertension. 2010 Oct. 56(4):643-9. [QxMD MEDLINE Link]. [Full Text].
- Kirabo A, Fontana V, de Faria AP, et al. DC isoketal-modified proteins activate T cells and promote hypertension. J Clin Invest. 2014 Oct. 124(10):4642-56. [QxMD MEDLINE Link]. [Full Text].
- Harrison DG, Guzik TJ, Lob HE, et al. Inflammation, immunity, and hypertension. Hypertension. 2011 Feb. 57(2):132-40. [QxMD MEDLINE Link]. [Full Text].
- Guzik TJ, Hoch NE, Brown KA, et al. Role of the T cell in the genesis of angiotensin II induced hypertension and vascular dysfunction. J Exp Med. 2007 Oct 1. 204(10):2449-60. [QxMD MEDLINE Link].
- Madhur MS, Lob HE, McCann LA, et al. Interleukin 17 promotes angiotensin II-induced hypertension and vascular dysfunction. Hypertension. 2010 Feb. 55(2):500-7. [QxMD MEDLINE Link].
- Rule AD, Fridley BL, Hunt SC, et al. Genome-wide linkage analysis for uric acid in families enriched for hypertension. Nephrol Dial Transplant. 2009 Aug. 24(8):2414-20. [QxMD MEDLINE Link]. [Full Text].
- Jermendy G, Horvath T, Littvay L, et al. Effect of genetic and environmental influences on cardiometabolic risk factors: a twin study. Cardiovasc Diabetol. 2011 Nov 3. 10:96. [QxMD MEDLINE Link]. [Full Text].
- Mitchell GF, DeStefano AL, Larson MG, et al. Heritability and a genome-wide linkage scan for arterial stiffness, wave reflection, and mean arterial pressure: the Framingham Heart Study. Circulation. 2005 Jul 12. 112(2):194-9. [QxMD MEDLINE Link].
- Levy D, DeStefano AL, Larson MG, et al. Evidence for a gene influencing blood pressure on chromosome 17. Genome scan linkage results for longitudinal blood pressure phenotypes in subjects from the framingham heart study. Hypertension. 2000 Oct. 36(4):477-83. [QxMD MEDLINE Link].
- Coffman TM. Under pressure: the search for the essential mechanisms of hypertension. Nat Med. 2011 Nov 7. 17(11):1402-9. [QxMD MEDLINE Link].
- Millis RM. Epigenetics and hypertension. Curr Hypertens Rep. 2011 Feb. 13(1):21-8. [QxMD MEDLINE Link].
- Brown MJ. Hypertension and ethnic group. BMJ. 2006 Apr 8. 332(7545):833-6. [QxMD MEDLINE Link]. [Full Text].
- Goldblatt H, Lynch J, Hanzal RF, Summerville WW. Studies on experimental hypertension: I. The production of persistent elevation of systolic blood pressure by means of renal ischemia. J Exp Med. 1934 Feb 28. 59(3):347-79. [QxMD MEDLINE Link]. [Full Text].
- Carey RM, Calhoun DA, Bakris GL, et al, for the American Heart Association Professional/Public Education and Publications Committee of the Council on Hypertension; Council on Cardiovascular and Stroke Nursing; Council on Clinical Cardiology; et al. Resistant Hypertension: Detection, Evaluation, and Management: A Scientific Statement From the American Heart Association. Hypertension. 2018 Nov. 72(5):e53-e90. [QxMD MEDLINE Link]. [Full Text].
- [Guideline] Kapur VK, Auckley DH, Chowdhuri S, et al. Clinical practice guideline for diagnostic testing for adult obstructive sleep apnea: an American Academy of Sleep Medicine clinical practice guideline. J Clin Sleep Med. 2017 Mar 15. 13(3):479-504. [QxMD MEDLINE Link]. [Full Text].
- Feldstein CA. Blood pressure effects of CPAP in nonresistant and resistant hypertension associated with OSA: A systematic review of randomized clinical trials. Clin Exp Hypertens. 2016. 38(4):337-46. [QxMD MEDLINE Link].
- McEvoy RD, Antic NA, Heeley E, et al, for the SAVE Investigators and Coordinators. CPAP for prevention of cardiovascular events in obstructive sleep apnea. N Engl J Med. 2016 Sep 8. 375(10):919-31. [QxMD MEDLINE Link]. [Full Text].
- Marik PE, Varon J. Hypertensive crises: challenges and management. Chest. 2007 Jun. 131(6):1949-62. [QxMD MEDLINE Link].
- Rodriguez MA, Kumar SK, De Caro M. Hypertensive crisis. Cardiol Rev. 2010 Mar-Apr. 18(2):102-7. [QxMD MEDLINE Link].
- Hollander JE. Cocaine intoxication and hypertension. Ann Emerg Med. 2008 Mar. 51(3 Suppl):S18-20. [QxMD MEDLINE Link].
- Ostchega Y, Fryar CD, Nwankwo T, Nguyen DT. Hypertension prevalence among adults aged 18 and over: United States, 2017-2018. NCHS Data Brief. 2020 Apr. no 364:1-8. [QxMD MEDLINE Link]. [Full Text].
- Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet. 2005 Jan 15-21. 365(9455):217-23. [QxMD MEDLINE Link].
- Forouzanfar MH, Alexander L, Anderson HR, et al, for the GBD 2013 Risk Factors Collaborators. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks in 188 countries, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015 Dec 5. 386(10010):2287-323. [QxMD MEDLINE Link]. [Full Text].
- GBD 2013 Mortality and Causes of Death Collaborators. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015 Jan 10. 385(9963):117-71. [QxMD MEDLINE Link]. [Full Text].
- Saeed A, Dixon DL, Yang E. Racial disparities in hypertension prevalence and management: a crisis control?. American College of Cardiology. Available at https://www.acc.org/Latest-in-Cardiology/Articles/2020/04/06/08/53/Racial-Disparities-in-Hypertension-Prevalence-and-Management. April 6, 2020; Accessed: February 27, 2024.
- Mozaffarian D, Benjamin EJ, Go AS, et al, for the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics--2015 update: a report from the American Heart Association. Circulation. 2015 Jan 27. 131(4):e29-322. [QxMD MEDLINE Link]. [Full Text].
- [Guideline] Carey RM, Calhoun DA, Bakris GL, et al, for the American Heart Association Professional/Public Education and Publications Committee of the Council on Hypertension; Council on Cardiovascular and Stroke Nursing; Council on Clinical Cardiology; et al. Resistant hypertension: detection, evaluation, and management: a scientific statement from the American Heart Association. Hypertension. 2018 Nov. 72(5):e53-e90. [QxMD MEDLINE Link]. [Full Text].
- Ong YT, Wong TY, Klein R, et al. Hypertensive retinopathy and risk of stroke. Hypertension. 2013 Oct. 62(4):706-11. [QxMD MEDLINE Link]. [Full Text].
- Brooks M. Hypertensive retinopathy linked to increased stroke risk. Medscape Medical News. August 16, 2013. Available at https://www.medscape.com/viewarticle/809541. Accessed: August 20, 2013.
- Huang Y, Cai X, Li Y, et al. Prehypertension and the risk of stroke: a meta-analysis. Neurology. 2014 Apr 1. 82(13):1153-61. [QxMD MEDLINE Link].
- Hughes S. Even prehypertension increases stroke risk: meta-analysis. Medscape Medical News. March 14, 2014. Available at https://www.medscape.com/viewarticle/821977. Accessed: March 20, 2014.
- Webster J, Petrie JC, Jeffers TA, Lovell HG. Accelerated hypertension--patterns of mortality and clinical factors affecting outcome in treated patients. Q J Med. 1993 Aug. 86(8):485-93. [QxMD MEDLINE Link].
- Culleton BF, Larson MG, Kannel WB, Levy D. Serum uric acid and risk for cardiovascular disease and death: the Framingham Heart Study. Ann Intern Med. 1999 Jul 6. 131(1):7-13. [QxMD MEDLINE Link].
- Mortality after 10 1/2 years for hypertensive participants in the Multiple Risk Factor Intervention Trial. Circulation. 1990 Nov. 82(5):1616-28. [QxMD MEDLINE Link].
- Chen G, McAlister FA, Walker RL, Hemmelgarn BR, Campbell NR. Cardiovascular outcomes in Framingham participants with diabetes: the importance of blood pressure. Hypertension. 2011 May. 57(5):891-7. [QxMD MEDLINE Link]. [Full Text].
- Ford ES. Trends in mortality from all causes and cardiovascular disease among hypertensive and nonhypertensive adults in the United States. Circulation. 2011 Apr 26. 123(16):1737-44. [QxMD MEDLINE Link].
- Bombelli M, Facchetti R, Sega R, et al. Impact of body mass index and waist circumference on the long-term risk of diabetes mellitus, hypertension, and cardiac organ damage. Hypertension. 2011 Dec. 58(6):1029-35. [QxMD MEDLINE Link]. [Full Text].
- Redon J, Campos C, Narciso ML, Rodicio JL, Pascual JM, Ruilope LM. Prognostic value of ambulatory blood pressure monitoring in refractory hypertension: a prospective study. Hypertension. 1998 Feb. 31(2):712-8. [QxMD MEDLINE Link]. [Full Text].
- Wong TY, Mitchell P. Hypertensive retinopathy. N Engl J Med. 2004 Nov 25. 351(22):2310-7. [QxMD MEDLINE Link].
- Zampaglione B, Pascale C, Marchisio M, Cavallo-Perin P. Hypertensive urgencies and emergencies. Prevalence and clinical presentation. Hypertension. 1996 Jan. 27(1):144-7. [QxMD MEDLINE Link].
- Staykov D, Schwab S. Posterior reversible encephalopathy syndrome. J Intensive Care Med. 2012 Feb. 27(1):11-24. [QxMD MEDLINE Link].
- McCord J, Mundy BJ, Hudson MP, et al, for the Breathing Not Properly Multinational Study Investigators. Relationship between obesity and B-type natriuretic peptide levels. Arch Intern Med. 2004 Nov 8. 164(20):2247-52. [QxMD MEDLINE Link]. [Full Text].
- Mammaro A, Carrara S, Cavaliere A, et al. Hypertensive disorders of pregnancy. J Prenat Med. 2009 Jan. 3(1):1-5. [QxMD MEDLINE Link]. [Full Text].
- Wang IK, Muo CH, Chang YC, et al. Association between hypertensive disorders during pregnancy and end-stage renal disease: a population-based study. CMAJ. 2013 Feb 19. 185(3):207-13. [QxMD MEDLINE Link]. [Full Text].
- American College of Obstetricians and Gynecologists, Task Force on Hypertension in Pregnancy. Hypertension in pregnancy. Report of the American College of Obstetricians and Gynecologists’ Task Force on Hypertension in Pregnancy. Obstet Gynecol. 2013 Nov. 122(5):1122-31. [QxMD MEDLINE Link]. [Full Text].
- Pickering TG, James GD, Boddie C, Harshfield GA, Blank S, Laragh JH. How common is white coat hypertension?. JAMA. 1988 Jan 8. 259(2):225-8. [QxMD MEDLINE Link].
- Stiles S. Framingham criteria predict new hypertension better than prehypertension in young adults. Medscape Medical News. September 20, 2013. Available at https://www.medscape.com/viewarticle/811416. Accessed: September 30, 2013.
- Carson AP, Lewis CE, Jacobs DR Jr, et al. Evaluating the Framingham hypertension risk prediction model in young adults: the Coronary Artery Risk Development in Young Adults (CARDIA) study. Hypertension. 2013 Dec. 62(6):1015-20. [QxMD MEDLINE Link]. [Full Text].
- Koivistoinen T, Lyytikainen LP, Aatola H, et al. Pulse wave velocity predicts the progression of blood pressure and development of hypertension in young adults. Hypertension. 2018 Mar. 71(3):451-6. [QxMD MEDLINE Link]. [Full Text].
- Olin JW, Piedmonte MR, Young JR, DeAnna S, Grubb M, Childs MB. The utility of duplex ultrasound scanning of the renal arteries for diagnosing significant renal artery stenosis. Ann Intern Med. 1995 Jun 1. 122(11):833-8. [QxMD MEDLINE Link].
- US Food and Drug Administration. Information on gadolinium-based contrast agents. Available at https://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/ucm142882.htm. Accessed: February 22, 2012.
- American College of Radiology. ACR manual on contrast media, 2023. Available at https://www.acr.org/-/media/ACR/Files/Clinical-Resources/Contrast_Media.pdf. Accessed: March 4, 2024.
- Cortigiani L, Bigi R, Landi P, Bovenzi F, Picano E, Sicari R. Prognostic implication of stress echocardiography in 6214 hypertensive and 5328 normotensive patients. Eur Heart J. 2011 Jun. 32(12):1509-18. [QxMD MEDLINE Link].
- [Guideline] Qaseem A, Wilt TJ, Rich R, et al, for the Clinical Guidelines Committee of the American College of Physicians and the Commission on Health of the Public and Science of the American Academy of Family Physicians. Pharmacologic treatment of hypertension in adults aged 60 years or older to higher versus lower blood pressure targets: A clinical practice guideline from the American College of Physicians and the American Academy of Family Physicians. Ann Intern Med. 2017 Mar 21. 166(6):430-7. [QxMD MEDLINE Link]. [Full Text].
- [Guideline] ElSayed NA, Aleppo G, Aroda VR, et al, for the American Diabetes Association. Addendum. 3. Prevention or delay of type 2 diabetes and associated comorbidities: standards of care in diabetes-2023. Diabetes Care. 2023 Sep 1. 46 (9):1716-17. [QxMD MEDLINE Link]. [Full Text].
- [Guideline] ElSayed NA, Aleppo G, Aroda VR, et al, for the American Diabetes Association. Addendum. 2. Classification and diagnosis of diabetes: standards of care in diabetes-2023. Diabetes Care. 2023 Sep 1. 46 (9):1715. [QxMD MEDLINE Link]. [Full Text].
- Redon J, Cifkova R, Laurent S, et al. Mechanisms of hypertension in the cardiometabolic syndrome. J Hypertens. 2009 Mar. 27(3):441-51. [QxMD MEDLINE Link].
- [Guideline] American Diabetes Association. Standards of medical care in diabetes-2016 abridged for primary care providers. Clin Diabetes. 2016 Jan. 34(1):3-21. [QxMD MEDLINE Link]. [Full Text].
- Tseng CD, Yen AM, Chiu SY, Chen LS, Chen HH, Chang SH. A predictive model for risk of prehypertension and hypertension and expected benefit after population-based life-style modification (KCIS No. 24). Am J Hypertens. 2012 Feb. 25(2):171-9. [QxMD MEDLINE Link].
- Stiles S. New AHA/ACC cholesterol treatment guideline expands role of LDL targets. Medscape Medical News. November 10, 2018. Available at https://www.medscape.com/viewarticle/904736. Accessed: December 1, 2018.
- [Guideline] Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2019 Jun 25. 73(24):e285-e350. [QxMD MEDLINE Link]. [Full Text].
- [Guideline] Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019 Sep 10. 140(11):e596-e646. [QxMD MEDLINE Link]. [Full Text].
- [Guideline] Jellinger PS, Handelsman Y, Rosenblit PD, et al. American Association of Clinical Endocrinologists and American College of Endocrinology guidelines for management of dyslipidemia and prevention of cardiovascular disease. Endocr Pract. 2017 Apr. 23(suppl 2):1-87. [QxMD MEDLINE Link]. [Full Text].
- Barbato E, Azizi M, Schmieder RE, et al. Renal denervation in the management of hypertension in adults. A clinical consensus statement of the ESC Council on Hypertension and the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur Heart J. 2023 Apr 17. 44(15):1313-30. [QxMD MEDLINE Link]. [Full Text].
- Forman JP, Scheven L, de Jong PE, Bakker SJ, Curhan GC, Gansevoort RT. Association between sodium intake and change in uric acid, urine albumin excretion, and the risk of developing hypertension. Circulation. 2012 Jun 26. 125(25):3108-16. [QxMD MEDLINE Link]. [Full Text].
- Slagman MC, Waanders F, Hemmelder MH, et al. Moderate dietary sodium restriction added to angiotensin converting enzyme inhibition compared with dual blockade in lowering proteinuria and blood pressure: randomised controlled trial. BMJ. 2011 Jul 26. 343:d4366. [QxMD MEDLINE Link]. [Full Text].
- [Guideline] American Diabetes Association. Standards of medical care in diabetes--2011. Diabetes Care. 2011 Jan. 34 Suppl 1:S11-61. [QxMD MEDLINE Link]. [Full Text].
- Aburto NJ, Hanson S, Gutierrez H, Hooper L, Elliott P, Cappuccio FP. Effect of increased potassium intake on cardiovascular risk factors and disease: systematic review and meta-analyses. BMJ. 2013 Apr 3. 346:f1378. [QxMD MEDLINE Link]. [Full Text].
- Ried K, Sullivan T, Fakler P, Frank OR, Stocks NP. Does chocolate reduce blood pressure? A meta-analysis. BMC Med. 2010 Jun 28. 8:39. [QxMD MEDLINE Link]. [Full Text].
- Salaish Kumar S, Mhd Jalil AM, Hussin N, Mat Daud Z', Ismail A. Effects of flavanols and procyanidins-rich cocoa consumption on metabolic syndrome: an update review (2013 to 2023). Biosci Biotechnol Biochem. 2024 Jan 29. [QxMD MEDLINE Link]. [Full Text].
- Amoah I, Lim JJ, Osei EO, et al. Effect of cocoa beverage and dark chocolate consumption on blood Pressure in Those with Normal and elevated blood pressure: a systematic review and meta-analysis. Foods. 2022 Jul 1. 11 (13):1962. [QxMD MEDLINE Link]. [Full Text].
- Ha V, Sievenpiper JL, de Souza RJ, et al. Effect of fructose on blood pressure: a systematic review and meta-analysis of controlled feeding trials. Hypertension. 2012 Apr. 59(4):787-95. [QxMD MEDLINE Link]. [Full Text].
- Blumenthal JA, Babyak MA, Hinderliter A, et al. Effects of the DASH diet alone and in combination with exercise and weight loss on blood pressure and cardiovascular biomarkers in men and women with high blood pressure: the ENCORE study. Arch Intern Med. 2010 Jan 25. 170(2):126-35. [QxMD MEDLINE Link]. [Full Text].
- [Guideline] de Boer IH, Bangalore S, Benetos A, et al. Diabetes and hypertension: a position statement by the American Diabetes Association. Diabetes Care. 2017 Sep. 40(9):1273-84. [QxMD MEDLINE Link]. [Full Text].
- [Guideline] Piercy KL, Troiano RP, Ballard RM, et al. The physical activity guidelines for Americans. JAMA. 2018 Nov 20. 320(19):2020-8. [QxMD MEDLINE Link]. [Full Text].
- [Guideline] 2018 Physical Activity Guidelines Advisory Committee. 2018 Physical Activity Guidelines Advisory Committee Scientific Report. Washington, DC: US Department of Health and Human Services; November 2018. [Full Text].
- Daien V, Duny Y, Ribstein J, et al. Treatment of hypertension with renin-angiotensin system inhibitors and renal dysfunction: a systematic review and meta-analysis. Am J Hypertens. 2012 Jan. 25(1):126-32. [QxMD MEDLINE Link].
- Boggs W. Benazepril plus amlodipine effective for high-risk, stage 2 hypertension. Medscape Medical News. May 3, 2013. Available at https://www.medscape.com/viewarticle/803579. Accessed: May 8, 2013.
- Bakris G, Briasoulis A, Dahlof B, et al, for the ACCOMPLISH Investigators. Comparison of benazepril plus amlodipine or hydrochlorothiazide in high-risk patients with hypertension and coronary artery disease. Am J Cardiol. 2013 Jul 15. 112(2):255-9. [QxMD MEDLINE Link].
- Cushman WC, Evans GW, Byington RP, Goff DC Jr, Grimm RH Jr. Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med. 2010 Apr 29. 362(17):1575-85. [QxMD MEDLINE Link]. [Full Text].
- Jamerson K, Weber MA, Bakris GL, et al, for the ACCOMPLISH Trial Investigators. Benazepril plus amlodipine or hydrochlorothiazide for hypertension in high-risk patients. N Engl J Med. 2008 Dec 4. 359(23):2417-28. [QxMD MEDLINE Link]. [Full Text].
- Chrysant SG, Izzo JL Jr, Kereiakes DJ, et al. Efficacy and safety of triple-combination therapy with olmesartan, amlodipine, and hydrochlorothiazide in study participants with hypertension and diabetes: a subpopulation analysis of the TRINITY study. J Am Soc Hypertens. 2012 Mar-Apr. 6(2):132-41. [QxMD MEDLINE Link].
- Ruggenenti P, Lauria G, Iliev IP, et al, for the DEMAND Study Investigators. Effects of manidipine and delapril in hypertensive patients with type 2 diabetes mellitus: the delapril and manidipine for nephroprotection in diabetes (DEMAND) randomized clinical trial. Hypertension. 2011 Nov. 58(5):776-83. [QxMD MEDLINE Link]. [Full Text].
- O'Riordan M. Spironolactone provides benefit in resistant hypertension, small study shows. Medscape Medical News. June 17, 2013. Available at https://www.medscape.com/viewarticle/806388. Accessed: July 29, 2013.
- Tsimihodimos V, Gonzalez-Villalpando C, Meigs JB, Ferrannini E. Hypertension and diabetes mellitus: coprediction and time trajectories. Hypertension. 2018 Mar. 71(3):422-8. [QxMD MEDLINE Link]. [Full Text].
- [Guideline] ElSayed NA, Aleppo G, Aroda VR, et al, on behalf of the American Diabetes Association. 10. Cardiovascular disease and risk management: standards of care in diabetes-2023. Diabetes Care. 2023 Jan 1. 46(Suppl 1):S158-S190. [QxMD MEDLINE Link]. [Full Text].
- Pancioli AM. Hypertension management in neurologic emergencies. Ann Emerg Med. 2008 Mar. 51(3 Suppl):S24-7. [QxMD MEDLINE Link].
- Slovis CM, Reddi AS. Increased blood pressure without evidence of acute end organ damage. Ann Emerg Med. 2008 Mar. 51(3 Suppl):S7-9. [QxMD MEDLINE Link].
- [Guideline] Flynn JT, Kaelber DC, Baker-Smith CM, et al, for the Subcommittee on Screening and Management of High Blood Pressure in Children and Adolescents. Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics. 2017 Sep. 140(3):[QxMD MEDLINE Link]. [Full Text].
- Blowey DL, Duda PJ, Stokes P, Hall M. Incidence and treatment of hypertension in the neonatal intensive care unit. J Am Soc Hypertens. 2011 Nov-Dec. 5(6):478-83. [QxMD MEDLINE Link].
- [Guideline] James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014 Feb 5. 311(5):507-20. [QxMD MEDLINE Link]. [Full Text].
- Wood S. JNC 8 at last! Guidelines ease up on BP thresholds, drug choices. Heartwire from Medscape. December 18, 2013. Available at https://www.medscape.com/viewarticle/817991. Accessed: December 21, 2013.
- Goto Y, Ishii M, Saruta T, et al, for the JATOS Study Group. Principal results of the Japanese trial to assess optimal systolic blood pressure in elderly hypertensive patients (JATOS). Hypertens Res. 2008 Dec. 31(12):2115-27. [QxMD MEDLINE Link].
- Ogihara T, Saruta T, Rakugi H, et al, for the Valsartan in Elderly Isolated Systolic Hypertension Study Group. Target blood pressure for treatment of isolated systolic hypertension in the elderly: valsartan in elderly isolated systolic hypertension study. Hypertension. 2010 Aug. 56(2):196-202. [QxMD MEDLINE Link]. [Full Text].
- Williamson JD, Supiano MA, Applegate WB, et al, for the SPRINT Research Group. Intensive vs standard blood pressure control and cardiovascular disease outcomes in adults aged ≥75 years: a randomized clinical trial. JAMA. 2016 Jun 28. 315(24):2673-82. [QxMD MEDLINE Link]. [Full Text].
- Kostis JB, Cabrera J, Cheng JQ, et al. Association between chlorthalidone treatment of systolic hypertension and long-term survival. JAMA. 2011 Dec 21. 306(23):2588-93. [QxMD MEDLINE Link]. [Full Text].
- Staessen JA, Fagard R, Thijs L, et al. Randomised double-blind comparison of placebo and active treatment for older patients with isolated systolic hypertension. The Systolic Hypertension in Europe (Syst-Eur) Trial Investigators. Lancet. 1997 Sep 13. 350(9080):757-64. [QxMD MEDLINE Link].
- Cooper CJ, Murphy TP, Cutlip DE, et al, for the CORAL Investigators. Stenting and medical therapy for atherosclerotic renal-artery stenosis. N Engl J Med. 2014 Jan 2. 370(1):13-22. [QxMD MEDLINE Link]. [Full Text].
- Calhoun DA. Advances in resistant hypertension. Ann Transl Med. 2018 Aug. 6(15):294. [QxMD MEDLINE Link]. [Full Text].
- Nishizaka MK, Zaman MA, Calhoun DA. Efficacy of low-dose spironolactone in subjects with resistant hypertension. Am J Hypertens. 2003 Nov. 16(11 Pt 1):925-30. [QxMD MEDLINE Link].
- de la Sierra A, Segura J, Banegas JR, et al. Clinical features of 8295 patients with resistant hypertension classified on the basis of ambulatory blood pressure monitoring. Hypertension. 2011 May. 57(5):898-902. [QxMD MEDLINE Link]. [Full Text].
- Townsend RR, Epstein M. Resistant hypertension: insights on evaluation and management in the post-SPRINT (Systolic Blood Pressure Intervention Trial) era. Hypertension. 2016 Nov. 68(5):1073-80. [QxMD MEDLINE Link]. [Full Text].
- Idorsia Pharmaceuticals. US FDA approves Idorsia’s once-daily TRYVIO (aprocitentan) – the first and only endothelin receptor antagonist for the treatment of high blood pressure not adequately controlled in combination with other antihypertensives [news release]. Available at https://www.idorsia.com/media/news/news-archive/media-release-details?id=3195250. March 20, 2024; Accessed: March 20, 2024.
- Brooks M. FDA okays new drug for resistant hypertension. Medscape Medical News. Available at https://www.medscape.com/viewarticle/fda-okays-new-drug-resistant-hypertension-2024a100058b. March 20, 2024; Accessed: March 20, 2024.
- Schlaich MP, Bellet M, Weber MA, et al, for the PRECISION investigators. Dual endothelin antagonist aprocitentan for resistant hypertension (PRECISION): a multicentre, blinded, randomised, parallel-group, phase 3 trial. Lancet. 2022 Dec 3. 400 (10367):1927-37. [QxMD MEDLINE Link].
- Orciari Herman A, Sadoughi S. Heart group updates guidelines on resistant hypertension. NEJM Journal Watch. September 13, 2018. Available at https://www.jwatch.org/fw114569/2018/09/13/heart-group-updates-guidelines-resistant-hypertension. Accessed: October 2, 2018.
- Krum H, Schlaich M, Whitbourn R, et al. Catheter-based renal sympathetic denervation for resistant hypertension: a multicentre safety and proof-of-principle cohort study. Lancet. 2009 Apr 11. 373(9671):1275-81. [QxMD MEDLINE Link].
- Catheter-based renal sympathetic denervation for resistant hypertension: durability of blood pressure reduction out to 24 months. Hypertension. 2011 May. 57(5):911-7. [QxMD MEDLINE Link].
- Esler MD, Krum H, Sobotka PA, et al. Renal sympathetic denervation in patients with treatment-resistant hypertension (The Symplicity HTN-2 Trial): a randomised controlled trial. Lancet. 2010 Dec 4. 376(9756):1903-9. [QxMD MEDLINE Link].
- Bhatt DL, Kandzari DE, O'Neill WW, et al, for the SYMPLICITY HTN-3 Investigators. A controlled trial of renal denervation for resistant hypertension. N Engl J Med. 2014 Apr 10. 370(15):1393-401. [QxMD MEDLINE Link]. [Full Text].
- Azizi M, Sanghvi K, Saxena M, et al, for the RADIANCE-HTN investigators. Ultrasound renal denervation for hypertension resistant to a triple medication pill (RADIANCE-HTN TRIO): a randomised, multicentre, single-blind, sham-controlled trial. Lancet. 2021 Jun 26. 397(10293):2476-86. [QxMD MEDLINE Link].
- Azizi M, Saxena M, Wang Y, et al, for the RADIANCE II Investigators and Collaborators. Endovascular ultrasound renal denervation to treat hypertension: the RADIANCE II randomized clinical trial. JAMA. 2023 Feb 28. 329(8):651-61. [QxMD MEDLINE Link]. [Full Text].
- Bohm M, Kario K, Kandzari DE, et al, for the SPYRAL HTN-OFF MED Pivotal Investigators. Efficacy of catheter-based renal denervation in the absence of antihypertensive medications (SPYRAL HTN-OFF MED Pivotal): a multicentre, randomised, sham-controlled trial. Lancet. 2020 May 2. 395(10234):1444-51. [QxMD MEDLINE Link].
- Mahfoud F, Kandzari DE, Kario K, et al. Long-term efficacy and safety of renal denervation in the presence of antihypertensive drugs (SPYRAL HTN-ON MED): a randomised, sham-controlled trial. Lancet. 2022 Apr 9. 399(10333):1401-10. [QxMD MEDLINE Link].
- Bisognano JD, Bakris G, Nadim MK, et al. Baroreflex activation therapy lowers blood pressure in patients with resistant hypertension: results from the double-blind, randomized, placebo-controlled rheos pivotal trial. J Am Coll Cardiol. 2011 Aug 9. 58(7):765-73. [QxMD MEDLINE Link]. [Full Text].
- de La Sierra A, Larrousse M, Oliveras A, et al. Abnormalities of vascular function in resistant hypertension. Blood Press. 2012 Apr. 21(2):104-9. [QxMD MEDLINE Link]. [Full Text].
- Mariampillai JE, Eskas PA, Heimark S, et al. Apparent treatment-resistant hypertension - patient-physician relationship and ethical issues. Blood Press. 2017 Jun. 26(3):133-8. [QxMD MEDLINE Link].
- Kronish IM, Woodward M, Sergie Z, Ogedegbe G, Falzon L, Mann DM. Meta-analysis: impact of drug class on adherence to antihypertensives. Circulation. 2011 Apr 19. 123(15):1611-21. [QxMD MEDLINE Link]. [Full Text].
- Fagugli RM, Taglioni C. Changes in the perceived epidemiology of primary hyperaldosteronism. Int J Hypertens. 2011. 2011:162804. [QxMD MEDLINE Link]. [Full Text].
- Pedrosa RP, Drager LF, Gonzaga CC, et al. Obstructive sleep apnea: the most common secondary cause of hypertension associated with resistant hypertension. Hypertension. 2011 Nov. 58(5):811-7. [QxMD MEDLINE Link]. [Full Text].
- Martinez-Garcia MA, Capote F, Campos-Rodriguez F, et al, for the Spanish Sleep Network. Effect of CPAP on blood pressure in patients with obstructive sleep apnea and resistant hypertension: the HIPARCO randomized clinical trial. JAMA. 2013 Dec 11. 310(22):2407-15. [QxMD MEDLINE Link]. [Full Text].
- O'Riordan M. CPAP reduces blood pressure in resistant hypertension. Heartwire from Medscape. December 10, 2013. Available at https://www.medscape.com/viewarticle/817569. Accessed: December 16, 2013.
- Fahey T, Schroeder K, Ebrahim S. Interventions used to improve control of blood pressure in patients with hypertension. Cochrane Database Syst Rev. 2006 Apr 19. CD005182. [QxMD MEDLINE Link]. [Full Text].
- Pezzin LE, Feldman PH, Mongoven JM, McDonald MV, Gerber LM, Peng TR. Improving blood pressure control: results of home-based post-acute care interventions. J Gen Intern Med. 2011 Mar. 26(3):280-6. [QxMD MEDLINE Link]. [Full Text].
- Glynn LG, Murphy AW, Smith SM, Schroeder K, Fahey T. Interventions used to improve control of blood pressure in patients with hypertension. Cochrane Database Syst Rev. 2010 Mar 17. CD005182. [QxMD MEDLINE Link]. [Full Text].
- Bosworth HB, Powers BJ, Olsen MK, et al. Home blood pressure management and improved blood pressure control: results from a randomized controlled trial. Arch Intern Med. 2011 Jul 11. 171(13):1173-80. [QxMD MEDLINE Link]. [Full Text].
- O'Riordan M. New European hypertension guidelines released: goal is less than 140 mm Hg for all. Heartwire from Medscape. June 15, 2013. Available at https://www.medscape.com/viewarticle/806367. Accessed: June 24, 2013.
- [Guideline] Mancia G, Fagard R, Narkiewicz K, et al, for the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension and the European Society of Cardiology. 2013 ESH/ESC practice guidelines for the management of arterial hypertension. Blood Press. 2014 Feb. 23(1):3-16. [QxMD MEDLINE Link]. [Full Text].
- [Guideline] Krist AH, Davidson KW, Mangione CM, et al, for the US Preventive Services Task Force. Screening for hypertension in adults: US Preventive Services Task Force reaffirmation recommendation statement. JAMA. 2021 Apr 27. 325(16):1650-6. [QxMD MEDLINE Link]. [Full Text].
- [Guideline] American Congress of Obstetricians and Gynecologists (ACOG). Well-woman care: assessments & recommendations. Washington, DC: American Congress of Obstetricians and Gynecologists. Available at https://www.acog.org/About-ACOG/ACOG-Departments/Annual-Womens-Health-Care/Well-Woman-Recommendations . 2013; Accessed: May 15, 2016.
- [Guideline] Department of Veterans Affairs and Department of Defense (VA/DoD). Clinical practice guideline for the diagnosis and management of hypertension in the primary care setting. Version 3.0. Available at https://www.healthquality.va.gov/guidelines/CD/htn/VADoDCPGfortheManagementofHTN.pdf . 2014; Accessed: May 15, 2016.
- [Guideline] Rosendorff C, Lackland DT, Allison M, Aronow WS, et al, for the American Heart Association, et al. Treatment of hypertension in patients with coronary artery disease: a scientific statement from the American Heart Association, American College of Cardiology, and American Society of Hypertension. Circulation. 2015 May 12. 131(19):e435-70. [QxMD MEDLINE Link]. [Full Text].
- [Guideline] Go AS, Bauman MA, Coleman King SM, et al, for the American Heart Association, American College of Cardiology, et al. An effective approach to high blood pressure control: a science advisory from the American Heart Association, the American College of Cardiology, and the Centers for Disease Control and Prevention. Hypertension. 2014 Apr. 63(4):878-85. [QxMD MEDLINE Link]. [Full Text].
- [Guideline] Weber MA, Schiffrin EL, White WB, et al. Clinical practice guidelines for the management of hypertension in the community a statement by the American Society of Hypertension and the International Society of Hypertension. J Hypertens. 2014 Jan. 32(1):3-15. [QxMD MEDLINE Link]. [Full Text].
- Wright JT Jr, Williamson JD, Whelton PK, et al, for the SPRINT Research Group. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015 Nov 26. 373(22):2103-16. [QxMD MEDLINE Link]. [Full Text].
- Benavente OR, Coffey CS, Conwit R, et al, for the SPS3 Study Group. Blood-pressure targets in patients with recent lacunar stroke: the SPS3 randomised trial. Lancet. 2013 Aug 10. 382(9891):507-15. [QxMD MEDLINE Link]. [Full Text].
- Oparil S, Lewis CE. Should patients with cardiovascular risk factors receive intensive treatment of hypertension to Circulation. 2016 Nov 1. 134(18):1308-1310. [QxMD MEDLINE Link]. [Full Text].
- Thomopoulos C, Parati G, Zanchetti A. Effects of blood pressure lowering on outcome incidence in hypertension: 7. Effects of more vs. less intensive blood pressure lowering and different achieved blood pressure levels - updated overview and meta-analyses of randomized trials. J Hypertens. 2016 Apr. 34(4):613-22. [QxMD MEDLINE Link].
- O'Riordan M. AHA/ACC/CDC issue 'science advisory' on treating BP. Medscape Medical News. November 15, 2013. Available at https://www.medscape.com/viewarticle/814442. Accessed: November 16, 2013.
- [Guideline] Magee LA, Pels A, Helewa M, Rey E, von Dadelszen P, Canadian Hypertensive Disorders of Pregnancy Working Group. Diagnosis, evaluation, and management of the hypertensive disorders of pregnancy: executive summary. J Obstet Gynaecol Can. 2014 May. 36(5):416-41. [QxMD MEDLINE Link]. [Full Text].
- [Guideline] Goldstein LB, Bushnell CD, Adams RJ, et al, for the American Heart Association Stroke Council, Council on Cardiovascular Nursing, et al. Guidelines for the primary prevention of stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011 Feb. 42(2):517-84. [QxMD MEDLINE Link]. [Full Text].
- [Guideline] Wolf SJ, Lo B, Shih RD, Smith MD, Fesmire FM; American College of Emergency Physicians Clinical Policies Committee. Clinical policy: critical issues in the evaluation and management of adult patients in the emergency department with asymptomatic elevated blood pressure. Ann Emerg Med. 2013 Jul. 62(1):59-68. [QxMD MEDLINE Link]. [Full Text].
- [Guideline] National High Blood Pressure Education Program Working Group. Report of the National High Blood Pressure Education Program Working Group on high blood pressure in pregnancy. Am J Obstet Gynecol. 2000 Jul. 183(1):S1-S22. [QxMD MEDLINE Link].
- [Guideline] American College of Obstetricians and Gynecologists, Task Force on Hypertension in Pregnancy. Hypertension in pregnancy. Report of the American College of Obstetricians and Gynecologists’ Task Force on Hypertension in Pregnancy. Obstet Gynecol. 2013 Nov. 122(5):1122-31. [QxMD MEDLINE Link]. [Full Text].
- [Guideline] Committee on Obstetric Practice. Committee opinion no. 623: emergent therapy for acute-onset, severe hypertension during pregnancy and the postpartum period. Obstet Gynecol. 2015 Feb. 125(2):521-5. [QxMD MEDLINE Link]. [Full Text].
- [Guideline] James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014 Feb 5. 311(5):507-20. [QxMD MEDLINE Link]. [Full Text].
- Leung AA, Wright A, Pazo V, Karson A, Bates DW. Risk of thiazide-induced hyponatremia in patients with hypertension. Am J Med. 2011 Nov. 124(11):1064-72. [QxMD MEDLINE Link].
- Harel Z, Gilbert C, Wald R, et al. The effect of combination treatment with aliskiren and blockers of the renin-angiotensin system on hyperkalaemia and acute kidney injury: systematic review and meta-analysis. BMJ. 2012 Jan 9. 344:e42. [QxMD MEDLINE Link]. [Full Text].
- Cummings DM, Amadio P Jr, Nelson L, Fitzgerald JM. The role of calcium channel blockers in the treatment of essential hypertension. Arch Intern Med. 1991 Feb. 151(2):250-9. [QxMD MEDLINE Link].
- Fryar CD, Ostchega Y, Hales CM, Zhang G, Kruszon-Moran D. Hypertension prevalence and control among adults: United States, 2015-2016. NCHS Data Brief. 2017 Oct. 1-8. [QxMD MEDLINE Link]. [Full Text].
- Stowasser M, Gordon RD. Primary aldosteronism: changing definitions and new concepts of physiology and pathophysiology both inside and outside the kidney. Physiol Rev. 2016 Oct. 96(4):1327-84. [QxMD MEDLINE Link]. [Full Text].
- Briasoulis A, Bakris GL. Current status of renal denervation in hypertension. Curr Cardiol Rep. 2016 Nov. 18(11):107. [QxMD MEDLINE Link].
- Frellick M. Updated hypertension guidelines released by ACP, AAFP. Medscape Medical News. January 17, 2017. Available at https://www.medscape.com/viewarticle/874494. Accessed: November 18, 2017.
- Weinberger MH, Izzo JL Jr, Purkayastha D, Weitzman R, Black HR. Comparative efficacy and safety of combination aliskiren/amlodipine and amlodipine monotherapy in African Americans with stage 2 hypertension and obesity or metabolic syndrome. J Am Soc Hypertens. 2011 Nov-Dec. 5(6):489-97. [QxMD MEDLINE Link].
- Denker MG, Cohen DL, Townsend RR. Catheter-based renal artery denervation for resistant hypertension: promise unfulfilled or unsettled?. Curr Atheroscler Rep. 2015 Oct. 17(10):535. [QxMD MEDLINE Link].
- Qureshi AI, Suri MF, Kirmani JF, Divani AA. Prevalence and trends of prehypertension and hypertension in United States: National Health and Nutrition Examination Surveys 1976 to 2000. Med Sci Monit. 2005 Sep. 11(9):CR403-9. [QxMD MEDLINE Link].
- Cornoni-Huntley J, LaCroix AZ, Havlik RJ. Race and sex differentials in the impact of hypertension in the United States. The National Health and Nutrition Examination Survey I Epidemiologic Follow-up Study. Arch Intern Med. 1989 Apr. 149(4):780-8. [QxMD MEDLINE Link].
- Strong Heart Study Data Book: A Report to American Indian Communities. Bethesda, MD: National Heart, Lung, and Blood Institute, NIH; 2001.
- Grundy SM, Cleeman JI, Daniels SR, et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 2005 Oct 25. 112(17):2735-52. [QxMD MEDLINE Link].
- Aronow WS, Fleg JL, Pepine CJ, et al. ACCF/AHA 2011 expert consensus document on hypertension in the elderly: a report of the American College of Cardiology Foundation Task Force on Clinical Expert Consensus documents developed in collaboration with the American Academy of Neurology, American Geriatrics Society, American Society for Preventive Cardiology, American Society of Hypertension, American Society of Nephrology, Association of Black Cardiologists, and European Society of Hypertension. J Am Coll Cardiol. 2011 May 17. 57(20):2037-114. [QxMD MEDLINE Link]. [Full Text].
- [Guideline] Guidelines Subcommittee. 1999 World Health Organization-International Society of Hypertension guidelines for the management of hypertension. J Hypertens. 1999 Feb. 17(2):151-83. [QxMD MEDLINE Link].
- Abalos E, Duley L, Steyn DW, Henderson-Smart DJ. Antihypertensive drug therapy for mild to moderate hypertension during pregnancy. Cochrane Database Syst Rev. 2007 Jan 24. CD002252. [QxMD MEDLINE Link].
- Abergel E, Chatellier G, Battaglia C, Menard J. Can echocardiography identify mildly hypertensive patients at high risk, left untreated based on current guidelines?. J Hypertens. 1999 Jun. 17(6):817-24. [QxMD MEDLINE Link].
- Matchar DB, McCrory DC, Orlando LA, et al. Systematic review: comparative effectiveness of angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers for treating essential hypertension. Ann Intern Med. 2008 Jan 1. 148(1):16-29. [QxMD MEDLINE Link]. [Full Text].
- ACR Committee on Drugs and Contrast Media. ACR Manual on Contrast Media. Vers. 7. American College of Radiology. 2023. Available at https://www.acr.org/-/media/ACR/Files/Clinical-Resources/Contrast_Media.pdf.
- Anderson CS, Huang Y, Arima H, et al, for the INTERACT Investigators. Effects of early intensive blood pressure-lowering treatment on the growth of hematoma and perihematomal edema in acute intracerebral hemorrhage: the Intensive Blood Pressure Reduction in Acute Cerebral Haemorrhage Trial (INTERACT). Stroke. 2010 Feb. 41(2):307-12. [QxMD MEDLINE Link]. [Full Text].
- Anderson CS, Huang Y, Wang JG, et al, for the INTERACT Investigators. Intensive blood pressure reduction in acute cerebral haemorrhage trial (INTERACT): a randomised pilot trial. Lancet Neurol. 2008 May. 7(5):391-9. [QxMD MEDLINE Link].
- Ault MJ, Ellrodt AG. Pathophysiological events leading to the end-organ effects of acute hypertension. Am J Emerg Med. 1985 Dec. 3(6 Suppl):10-5. [QxMD MEDLINE Link].
- Barton JR. Hypertension in pregnancy. Ann Emerg Med. 2008 Mar. 51 (3 suppl):S16-7. [QxMD MEDLINE Link].
- Brown MJ, McInnes GT, Papst CC, Zhang J, MacDonald TM. Aliskiren and the calcium channel blocker amlodipine combination as an initial treatment strategy for hypertension control (ACCELERATE): a randomised, parallel-group trial. Lancet. 2011 Jan 22. 377(9762):312-20. [QxMD MEDLINE Link].
- Chapman N, Huxley R, Anderson C, et al, for the Writing Committee for the PROGRESS Collaborative Group. Effects of a perindopril-based blood pressure-lowering regimen on the risk of recurrent stroke according to stroke subtype and medical history: the PROGRESS Trial. Stroke. 2004 Jan. 35(1):116-21. [QxMD MEDLINE Link]. [Full Text].
- Cheung AT, Hobson RW 2nd. Hypertension in vascular surgery: aortic dissection and carotid revascularization. Ann Emerg Med. 2008 Mar. 51(3 Suppl):S28-33. [QxMD MEDLINE Link].
- Chrysant SG, Fagan T, Glazer R, Kriegman A. Effects of benazepril and hydrochlorothiazide, given alone and in low- and high-dose combinations, on blood pressure in patients with hypertension. Arch Fam Med. 1996 Jan. 5(1):17-24; discussion 25. [QxMD MEDLINE Link].
- Cushman WC, Bakris GL, White WB, et al. Azilsartan medoxomil plus chlorthalidone reduces blood pressure more effectively than olmesartan plus hydrochlorothiazide in stage 2 systolic hypertension. Hypertension. 2012 Aug. 60(2):310-8. [QxMD MEDLINE Link]. [Full Text].
- Diercks DB, Ohman EM. Hypertension with acute coronary syndrome and heart failure. Ann Emerg Med. 2008 Mar. 51(3 Suppl):S34-6. [QxMD MEDLINE Link].
- Dungan JR, Conley YP, Langaee TY, et al. Altered beta-2 adrenergic receptor gene expression in human clinical hypertension. Biol Res Nurs. 2009 Jul. 11(1):17-26. [QxMD MEDLINE Link]. [Full Text].
- Epstein M. Calcium antagonists and renal disease. Kidney Int. 1998 Nov. 54(5):1771-84. [QxMD MEDLINE Link].
- Faselis C, Doumas M, Kokkinos JP, et al. Exercise capacity and progression from prehypertension to hypertension. Hypertension. 2012 Aug. 60(2):333-8. [QxMD MEDLINE Link]. [Full Text].
- Hansson L, Hedner T, Lund-Johansen P, et al. Randomised trial of effects of calcium antagonists compared with diuretics and beta-blockers on cardiovascular morbidity and mortality in hypertension: the Nordic Diltiazem (NORDIL) study. Lancet. 2000 Jul 29. 356(9227):359-65. [QxMD MEDLINE Link]. [Full Text].
- Heilpern K. Pathophysiology of hypertension. Ann Emerg Med. 2008 Mar. 51(3 Suppl):S5-6. [QxMD MEDLINE Link].
- Hermida RC, Ayala DE, Mojon A, Fernandez JR. Decreasing sleep-time blood pressure determined by ambulatory monitoring reduces cardiovascular risk. J Am Coll Cardiol. 2011 Sep 6. 58(11):1165-73. [QxMD MEDLINE Link]. [Full Text].
- Izzo JL Jr, Weintraub HS, Duprez DA, et al. Treating systolic hypertension in the very elderly with valsartan-hydrochlorothiazide vs. either monotherapy: ValVET primary results. J Clin Hypertens (Greenwich). 2011 Oct. 13(10):722-30. [QxMD MEDLINE Link]. [Full Text].
- Kandzari DE, Bhatt DL, Sobotka PA, et al. Catheter-based renal denervation for resistant hypertension: rationale and design of the SYMPLICITY HTN-3 Trial. Clin Cardiol. 2012 Sep. 35(9):528-35. [QxMD MEDLINE Link]. [Full Text].
- Kaplan NM. Calcium entry blockers in the treatment of hypertension. Current status and future prospects. JAMA. 1989 Aug 11. 262(6):817-23. [QxMD MEDLINE Link].
- [Guideline] Khan NA, McAlister FA, Lewanczuk RZ, et al, for the Canadian Hypertension Education Program. The 2005 Canadian Hypertension Education Program recommendations for the management of hypertension: part II - therapy. Can J Cardiol. 2005 Jun. 21(8):657-72. [QxMD MEDLINE Link].
- Kitiyakara C, Guzman NJ. Malignant hypertension and hypertensive emergencies. J Am Soc Nephrol. 1998 Jan. 9(1):133-42. [QxMD MEDLINE Link].
- Lao D, Parasher PS, Cho KC, Yeghiazarians Y. Atherosclerotic renal artery stenosis--diagnosis and treatment. Mayo Clin Proc. 2011 Jul. 86(7):649-57. [QxMD MEDLINE Link]. [Full Text].
- Lloyd-Jones D, Adams RJ, Brown TM, et al, for the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics--2010 update: a report from the American Heart Association. Circulation. 2010 Feb 23. 121(7):e46-e215. [QxMD MEDLINE Link]. [Full Text].
- Magee LA, Helewa M, Rey E, Hypertension Guidelines Committee, Strategic Training Initiative in Research in the Reproductive Health Sciences (STIRRHS) Scholars. Diagnosis, evaluation, and management of the hypertensive disorders of pregnancy. J Obstet Gynaecol Can. 2008 Mar. 30(3 Suppl):S1-S2. [QxMD MEDLINE Link].
- Furberg CD, Wright JT, Davis BR, et al, for the The ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. Major cardiovascular events in hypertensive patients randomized to doxazosin vs chlorthalidone: the antihypertensive and lipid-lowering treatment to prevent heart attack trial (ALLHAT). ALLHAT Collaborative Research Group. JAMA. 2000 Apr 19. 283(15):1967-75. [QxMD MEDLINE Link]. [Full Text].
- Narkiewicz K. Diagnosis and management of hypertension in obesity. Obes Rev. 2006 May. 7(2):155-62. [QxMD MEDLINE Link].
- National Institutes of Health. Your guide to lowering your blood pressure with DASH. National Heart, Lung, and Blood Institute. April 2006. Available at https://www.nhlbi.nih.gov/health/public/heart/hbp/dash/new_dash.pdf.
- Novartis announces termination of ALTITUDE study with Rasilez/Tekturna in high-risk patients with diabetes and renal impairment [press release]. FiercePharma. December 20, 2011. Available at https://www.fiercepharma.com/pharma/novartis-announces-termination-of-altitude-study-rasilez%C2%AE-tekturna%C2%AE-high-risk-patients. Accessed: February 22, 2012.
- O'Connor PJ, Vazquez-Benitez G, Schmittdiel JA, et al. Benefits of early hypertension control on cardiovascular outcomes in patients with diabetes. Diabetes Care. 2013 Feb. 36(2):322-7. [QxMD MEDLINE Link]. [Full Text].
- O'Riordan M. Olmesartan label to include intestinal problems, FDA says. Medscape Medical News. July 3, 2013. Available at https://www.medscape.com/viewarticle/807289. Accessed: July 8, 2013.
- Pimenta E, Calhoun DA, Oparil S. Sleep apnea, aldosterone, and resistant hypertension. Prog Cardiovasc Dis. 2009 Mar-Apr. 51(5):371-80. [QxMD MEDLINE Link].
- Pleis JR, Lucas JW, Ward BW. Summary health statistics for U.S. adults: National Health Interview Survey, 2008. Vital Health Stat 10. 2009 Dec. No. 242:1-157. [QxMD MEDLINE Link]. [Full Text].
- Podymow T, August P. Antihypertensive drugs in pregnancy. Semin Nephrol. 2011 Jan. 31(1):70-85. [QxMD MEDLINE Link].
- Pollare T, Lithell H, Berne C. A comparison of the effects of hydrochlorothiazide and captopril on glucose and lipid metabolism in patients with hypertension. N Engl J Med. 1989 Sep 28. 321(13):868-73. [QxMD MEDLINE Link].
- Rastan A, Krankenberg H, Muller-Hulsbeck S, et al. Improved renal function and blood pressure control following renal artery angioplasty: the renal artery angioplasty in patients with renal insufficiency and hypertension using a dedicated renal stent device study (PRECISION). EuroIntervention. 2008 Aug. 4(2):208-13. [QxMD MEDLINE Link].
- Roberts CL, Ford JB, Algert CS, et al. Population-based trends in pregnancy hypertension and pre-eclampsia: an international comparative study. BMJ Open. 2011 May 24. 1(1):e000101. [QxMD MEDLINE Link]. [Full Text].
- Shook RP, Lee DC, Sui X, et al. Cardiorespiratory fitness reduces the risk of incident hypertension associated with a parental history of hypertension. Hypertension. 2012 Jun. 59(6):1220-4. [QxMD MEDLINE Link]. [Full Text].
- Svetkey LP, Moore TJ, Simons-Morton DG, et al, for the DASH collaborative research group. Angiotensinogen genotype and blood pressure response in the Dietary Approaches to Stop Hypertension (DASH) study. J Hypertens. 2001 Nov. 19(11):1949-56. [QxMD MEDLINE Link].
- Taubert D, Roesen R, Lehmann C, Jung N, Schomig E. Effects of low habitual cocoa intake on blood pressure and bioactive nitric oxide: a randomized controlled trial. JAMA. 2007 Jul 4. 298(1):49-60. [QxMD MEDLINE Link].
- World Health Organization. The World Health Report 2002 - reducing risks, promoting healthy life. Geneva, Switzerland: WHO; 2002. Available at https://www.who.int/whr/2002/en/. Accessed: February 20, 2012.
- Tymchak W, Armstrong PW, Westerhout CM, et al. Mode of hospital presentation in patients with non-ST-elevation myocardial infarction: implications for strategic management. Am Heart J. 2011 Sep. 162(3):436-43. [QxMD MEDLINE Link].
- Wallach R, Karp RB, Reves JG, Oparil S, Smith LR, James TN. Pathogenesis of paroxysmal hypertension developing during and after coronary bypass surgery: a study of hemodynamic and humoral factors. Am J Cardiol. 1980 Oct. 46(4):559-65. [QxMD MEDLINE Link].
- White WB, Weber MA, Sica D, et al. Effects of the angiotensin receptor blocker azilsartan medoxomil versus olmesartan and valsartan on ambulatory and clinic blood pressure in patients with stages 1 and 2 hypertension. Hypertension. 2011 Mar. 57(3):413-20. [QxMD MEDLINE Link]. [Full Text].
- Wolz M, Cutler J, Roccella EJ, Rohde F, Thom T, Burt V. Statement from the National High Blood Pressure Education Program: prevalence of hypertension. Am J Hypertens. 2000 Jan. 13(1 Pt 1):103-4. [QxMD MEDLINE Link].
- Yakovlevitch M, Black HR. Resistant hypertension in a tertiary care clinic. Arch Intern Med. 1991 Sep. 151(9):1786-92. [QxMD MEDLINE Link].
- Dolan E, O'Brien E. Is it daily, monthly, or yearly blood pressure variability that enhances cardiovascular risk?. Curr Cardiol Rep. 2015 Nov. 17(11):93. [QxMD MEDLINE Link].
- Cau SB, Guimaraes DA, Rizzi E, Ceron CS, Gerlach RF, Tanus-Santos JE. The nuclear factor kappaB inhibitor pyrrolidine dithiocarbamate prevents cardiac remodelling and matrix metalloproteinase-2 up-regulation in renovascular hypertension. Basic Clin Pharmacol Toxicol. 2015 Oct. 117(4):234-41. [QxMD MEDLINE Link]. [Full Text].
- Rosner B, Cook NR, Daniels S, Falkner B. Childhood blood pressure trends and risk factors for high blood pressure: the NHANES experience 1988-2008. Hypertension. 2013 Aug. 62(2):247-54. [QxMD MEDLINE Link]. [Full Text].
- Alam T, Khan S, Gaba B, Haider MF, Baboota S, Ali J. Nanocarriers as treatment modalities for hypertension. Drug Deliv. 2017 Nov. 24(1):358-69. [QxMD MEDLINE Link]. [Full Text].
- Marcuccilli M, Kendrick J, Chonchol M. Sodium and fluid management in the conservative management of chronic kidney disease. Panminerva Med. 2017 Jun. 59(2):116-23. [QxMD MEDLINE Link].
- Clinical implications: hypertension. Hypertension. 2018 Mar 1. 71(3):367. [Full Text].
- Osborn JW, Banek CT. Catheter-based renal nerve ablation as a novel hypertension therapy: lost, and then found, in translation. Hypertension. 2018 Mar. 71(3):383-88. [QxMD MEDLINE Link]. [Full Text].
- Itoh H, Hayashi K, Miyashita K. Pre-emptive medicine for hypertension and its prospects. Hypertens Res. 2019 Mar. 42(3):301-5. [QxMD MEDLINE Link].
- Vemu PL, Yang E, Ebinger J. 2023 ESH hypertension guideline update: bringing us closer together across the pond. American College of Cardiology. Available at https://www.acc.org/Latest-in-Cardiology/Articles/2024/02/05/11/43/2023-ESH-Hypertension-Guideline-Update. February 5, 2024; Accessed: February 27, 2024.
- Whelton PK, Carey RM, Mancia G, Kreutz R, Bundy JD, Williams B. Harmonization of the American College of Cardiology/American Heart Association and European Society of Cardiology/European Society of Hypertension blood pressure/hypertension guidelines: comparisons, reflections, and recommendations. Circulation. 2022 Sep 13. 146 (11):868-77. [QxMD MEDLINE Link]. [Full Text].
Author
Mackenzie Samson, MD Resident Physician, Department of Internal Medicine, Vanderbilt University Medical Center
Disclosure: Nothing to disclose.
Coauthor(s)
Matthew R Alexander, MD, PhD Assistant Professor of Medicine, Department of Medicine, Division of Clinical Pharmacology, Division of Cardiovascular Medicine, Vanderbilt University School of Medicine; Assistant Professor of Molecular Physiology and Biophysics, Vanderbilt University
Matthew R Alexander, MD, PhD is a member of the following medical societies: American Association of Immunologists, American Heart Association, American Physiological Society, Federation of Clinical Immunology Societies, Vanderbilt Institute for Infection, Immunology, and Inflammation
Disclosure: Received income in an amount equal to or greater than $250 from: Idorsia pharmaceuticals.
Meena S Madhur, MD, PhD, FACC, FAHA Associate Professor with Tenure, Division Chief of Clinical Pharmacology, Department of Medicine, Division of Clinical Pharmacology and Division of Cardiology, Adjunct Associate Professor of Anatomy, Cell Biology, and Physiology, Indiana University School of Medicine; Adjunct Associate Professor of Medicine, Vanderbilt University School of Medicine
Meena S Madhur, MD, PhD, FACC, FAHA is a member of the following medical societies: American College of Cardiology, American Heart Association, American Physiological Society, American Society for Clinical Investigation
Disclosure: Nothing to disclose.
David G Harrison, MD Betty and Jack Bailey Professor of Medicine and Pharmacology, Director of Clinical Pharmacology, Vanderbilt University School of Medicine
David G Harrison, MD is a member of the following medical societies: American College of Cardiology, American Heart Association, American Physiological Society, American Society for Clinical Investigation, Association of American Physicians, Central Society for Clinical and Translational Research, American Federation for Clinical Research, Society for Vascular Medicine
Disclosure: Nothing to disclose.
Specialty Editor Board
Gary Edward Sander, MD, PhD, FACC, FAHA, FACP, FASH Professor of Medicine, Director of CME Programs, Team Leader, Root Cause Analysis, Tulane University Heart and Vascular Institute; Director of In-Patient Cardiology, Tulane Service, University Hospital; Visiting Physician, Medical Center of Louisiana at New Orleans; Faculty, Pennington Biomedical Research Institute, Louisiana State University; Professor, Tulane University School of Medicine
Gary Edward Sander, MD, PhD, FACC, FAHA, FACP, FASH is a member of the following medical societies: Alpha Omega Alpha, American Chemical Society, American College of Cardiology, American College of Chest Physicians, American College of Physicians, American Federation for Clinical Research, American Federation for Medical Research, American Heart Association, American Society for Pharmacology and Experimental Therapeutics, American Society of Hypertension, American Thoracic Society, Heart Failure Society of America, National Lipid Association, Southern Society for Clinical Investigation
Disclosure: Nothing to disclose.
Chief Editor
Eric H Yang, MD Associate Professor of Medicine, Director of Cardiac Catherization Laboratory and Interventional Cardiology, Mayo Clinic ArizonA
Eric H Yang, MD is a member of the following medical societies: Alpha Omega Alpha
Disclosure: Nothing to disclose.
Additional Contributors
Kamran Riaz, MD Clinical Assistant Professor, Department of Internal Medicine, Section of Cardiology, Wright State University, Boonshoft School of Medicine
Kamran Riaz, MD is a member of the following medical societies: American College of Cardiology, American College of Physicians, American Society of Echocardiography, Ohio State Medical Association, Royal College of Physicians
Disclosure: Nothing to disclose.
Albert W Dreisbach, MD Associate Professor of Medicine, Division of Nephrology, University of Mississippi Medical Center
Disclosure: Nothing to disclose.
Acknowledgements
George R Aronoff, MD Director, Professor, Departments of Internal Medicine and Pharmacology, Section of Nephrology, Kidney Disease Program, University of Louisville School of Medicine
George R Aronoff, MD is a member of the following medical societies: American Federation for Medical Research, American Society of Nephrology, Kentucky Medical Association, and National Kidney Foundation
Disclosure: Nothing to disclose.
Michael S Beeson, MD, MBA, FACEP Professor of Emergency Medicine, Northeastern Ohio Universities College of Medicine and Pharmacy; Attending Faculty, Akron General Medical Center
Michael S Beeson, MD, MBA, FACEP is a member of the following medical societies: American College of Emergency Physicians, Council of Emergency Medicine Residency Directors, National Association of EMS Physicians, and Society for Academic Emergency Medicine
Disclosure: Nothing to disclose.
Pamela L Dyne, MD Professor of Clinical Medicine/Emergency Medicine, University of California, Los Angeles, David Geffen School of Medicine; Attending Physician, Department of Emergency Medicine, Olive View-UCLA Medical Center
Pamela L Dyne, MD is a member of the following medical societies: American Academy of Emergency Medicine, American College of Emergency Physicians, and Society for Academic Emergency Medicine
Disclosure: Nothing to disclose.
Mert Erogul, MD Assistant Professor of Emergency Medicine, University Hospital of Brooklyn: Consulting Staff, Department of Emergency Medicine, Kings County Hospital Center
Mert Erogul, MD is a member of the following medical societies: American College of Emergency Physicians, American Medical Association, and Society for Academic Emergency Medicine
Disclosure: Nothing to disclose.
Allysia M Guy, MD Staff Physician, Department of Emergency Medicine, State University of New York Downstate Medical Center
Disclosure: Nothing to disclose.
Dawn C Jung, MD Staff Physician, Department of Emergency Medicine, Suny Downstate Medical Center, Kings County Hospital Center
Dawn C Jung, MD is a member of the following medical societies: American College of Emergency Physicians and Society for Academic Emergency Medicine
Disclosure: Nothing to disclose.
Claude Kortas, MD, MEd, FRCP(C) Program Director, Associate Professor, Department of Medicine, University of Western Ontario, Canada
Claude Kortas, MD, Med, FRCP(C) is a member of the following medical societies: American Society of Nephrology, College of Physicians and Surgeons of Ontario, Ontario Medical Association, and Royal College of Physicians and Surgeons of Canada
Disclosure: Nothing to disclose.
Stephen C Morris, MD Resident, Section of Emergency Medicine, Department of Surgery, Yale New Haven Hospital
Stephen C Morris, MD is a member of the following medical societies: American College of Emergency Physicians and American Medical Association
Disclosure: Nothing to disclose.
L Michael Prisant, MD, FACC, FAHA Cardiologist, Emeritus Professor of Medicine, Medical College of Georgia
L Michael Prisant, MD, FACC, FAHA is a member of the following medical societies: American College of Cardiology, American College of Chest Physicians, American College of Clinical Pharmacology, American College of Forensic Examiners, American College of Physicians, American Heart Association, and American Medical Association
Disclosure: Boehringer-Ingelheim Honoraria Speaking and teaching
Assaad J Sayah, MD Chief, Department of Emergency Medicine, Cambridge Health Alliance
Assaad J Sayah, MD is a member of the following medical societies: National Association of EMS Physicians
Disclosure: Nothing to disclose.
Zina Semenovskaya, MD Resident Physician, Department of Emergency Medicine, Kings County Hospital, State University of New York Downstate Medical Center College of Medicine
Disclosure: Nothing to disclose.
Sat Sharma, MD, FRCPC Professor and Head, Division of Pulmonary Medicine, Department of Internal Medicine, University of Manitoba; Site Director, Respiratory Medicine, St Boniface General Hospital
Sat Sharma, MD, FRCPC is a member of the following medical societies: American Academy of Sleep Medicine, American College of Chest Physicians, American College of Physicians-American Society of Internal Medicine, American Thoracic Society, Canadian Medical Association, Royal College of Physicians and Surgeons of Canada, Royal Society of Medicine, Society of Critical Care Medicine, and World Medical Association
Disclosure: Nothing to disclose.
Mark A Silverberg, MD, MMB, FACEP Assistant Professor, Associate Residency Director, Department of Emergency Medicine, State University of New York Downstate College of Medicine; Consulting Staff, Department of Emergency Medicine, Staten Island University Hospital, Kings County Hospital, University Hospital, State University of New York Downstate Medical Center
Mark A Silverberg, MD, MMB, FACEP is a member of the following medical societies: American College of Emergency Physicians, American Medical Association, Council of Emergency Medicine Residency Directors, and Society for Academic Emergency Medicine
Disclosure: Nothing to disclose.
Francisco Talavera, PharmD, PhD Adjunct Assistant Professor, University of Nebraska Medical Center College of Pharmacy; Editor-in-Chief, Medscape Drug Reference
Disclosure: Medscape Salary Employment
Mark Zwanger, MD, MBA Assistant Professor, Department of Emergency Medicine, Jefferson Medical College of Thomas Jefferson University
Mark Zwanger, MD, MBA is a member of the following medical societies: American Academy of Emergency Medicine, American College of Emergency Physicians, and American Medical Association
Disclosure: Nothing to disclose.