Trends in Antibiotic Prescribing for Adults in the United States—1995 to 2002 (original) (raw)
Abstract
Context
The impact of national efforts to limit antibiotic prescribing has not been fully evaluated.
Objectives
To analyze trends in outpatient visits associated with antibiotic prescription for U.S. adults.
Design
Cross-sectional study of data (1995 to 2002) from the National Ambulatory Medical Care Survey and the National Hospital Ambulatory Medical Care Survey.
Participants
Adults ≥18 years with an outpatient visit to an office- or hospital-based medical practice or to an emergency department. All visits were classified into 1 of 4 diagnostic categories: (1) acute respiratory infection (ARI)—antibiotics rarely indicated, (2) ARI—antibiotics often indicated, (3) nonrespiratory infection—antibiotics often indicated, and (4) all others.
Measurements
Trends in: (1) Proportion of outpatient visits associated with an antibiotic prescription; (2) proportion of antibiotic prescriptions that were broad spectrum; and (3) number of visits and antibiotic prescriptions per 1,000 U.S. adults ≥18 years of age.
Results
From 1995–1996 to 2001–2002, the proportion of all outpatient visits that generated an antibiotic prescription decreased from 17.9% to 15.3% (adjusted odds ratio [OR] 0.84, 95 % confidence interval [CI] 0.76 to 0.92). The entire reduction was because of a decrease in antibiotic prescriptions associated with visits for ARIs where antibiotics are rarely indicated from 59.9% to 49.1% (adjusted OR 0.64 95% CI 0.51 to 0.80). However, the proportion of prescribed antibiotics for these visits that were classified as broad-spectrum antibiotic prescription increased from 41.0% to 76.8%. Overall outpatient visits increased from 1693 to 1986 per 1,000 adults over the 8 years studied, but associated antibiotic prescriptions changed little, from 302 to 304 per 1,000 adults.
Conclusion
During the study period, outpatient antibiotic prescribing for respiratory infections where antibiotics are rarely indicated has declined, while the proportion of broad-spectrum antibiotics prescribed for these diagnoses has increased significantly. This trend resulted in a 15% decline in the total proportion of outpatient visits in which antibiotics were prescribed. However, because outpatient visits increased 17% over this time period, the population burden of outpatient antibiotic prescriptions changed little.
Keywords: antibiotics, prescribing, United States, NAMCS, NHAMCS
Acute respiratory infections (ARIs) are among the most common diagnoses resulting in primary care visits. Although symptomatic respiratory infections are overwhelmingly viral in origin and do not respond to antibiotic therapy,1,2 patients often receive antibiotics for these illnesses. Direct and indirect costs of these ARIs surpass 25 billion dollars yearly and include visits to medical care providers, fees for medications, decreased productivity, and school or work loss.3,4 The increased use of broad-spectrum and newer antimicrobials to “treat” ARIs increases the costs of health care and promotes antibiotic resistance.3–5 McCaig et al.5 demonstrated increasing prescription rates of antimicrobials in the United States during the 1980s. In 1997, Gonzales et al.6 reported that 50 to 70% of adult ARI visits generated an antibiotic prescription. Steinman et al.7,8 and Mainous et al.9 demonstrated excessive use of broad-spectrum antibiotics for predominantly viral illnesses. Educational interventions conducted in single Health Maintenance Organization (HMO) settings and a small number of practices have demonstrated improved antibiotic prescribing.10–12
Given the broader concerns for antimicrobial resistance, the Centers for Disease Control and Prevention (CDC) launched a national campaign, in 1995, to reduce antimicrobial resistance through promotion of more appropriate antibiotic use.13 Information from the CDC and other advisory groups explicitly states that antibiotic treatment of adults with nonspecific upper respiratory tract infections, acute bronchitis, or cough, regardless of duration, does not enhance illness resolution and is not recommended.14–18 One of the objectives of this national campaign was to reduce inappropriate antibiotic use.
The impact of these national efforts to improve antibiotic prescribing has not been fully evaluated in all populations. We conducted a comprehensive analysis of antibiotic prescribing for adults in office-, hospital-based practices, and emergency departments (ED) from 1995 to 2002 to determine whether antibiotic prescribing for inappropriate indications has decreased and whether there were changes in the use of broad-spectrum antibiotics. In addition, as trends in visit rates may influence the population burden of antibiotics, we measured visits and visit-associated antibiotic prescriptions per 1,000 U.S. adults.
METHODS
Data Sources
Information on the utilization of medical services provided by office-based practices is collected in the National Ambulatory Medical Care Survey (NAMCS). Data include patient visits to nonfederally employed medical care providers within private, nonhospital-based clinics, and HMOs. National Ambulatory Medical Care Survey uses a multistage probability sample design to obtain primary sampling units, practices within these sampling units, and patient visits within provider practices. Visits are randomly selected to provide representative visits throughout the year. The data are weighted to estimate the annual number of visits. Visits from Internal Medicine, Family Practice, General Practice, Occupational Health/Preventative Medicine, Geriatrics, Emergency Medicine, or Adolescent Medicine are included in this analysis. During the 8 study years, 190 to 400 providers and 4,100 to 8,868 patient visits were sampled annually, with participation rates averaging 68.2%.
The information on utilization of ambulatory services in hospital emergency and outpatient departments is collected in the National Hospital Ambulatory Medical Care Survey (NHAMCS). Findings are based on a national sample of visits to noninstitutional nonfederal short-stay hospitals. The NHAMCS uses a 4-stage probability sample design involving the selection of primary sampling units in geographically defined areas, hospitals within primary sampling units, ED or outpatient practices within hospitals, and patient visits within ED or outpatient clinics. Hospital staff complete patient record forms for a systematic random sample of patient visits during a randomly assigned 4-week period. Sample data are weighted to determine the number of annual visits. The number of outpatient settings surveyed annually ranged from 360 to 396 for the ED and 174 to 190 for the hospital-based clinics. The total number of visits per year sampled ranged from 15,195 to 26,883 in the ED and 10,157 to 12,016 in the hospital clinics. Participation rates ranged from 80.4% to 91.2%.
The NAMCS and NHAMCS visit forms are completed by each provider and ask for all diagnoses made by the provider. Centers for Disease Control and Prevention staff subsequently assigns the International Classification of Diseases (ICD) codes to all diagnoses. Data are coded and keyed by the Constella group Inc., with data quality control checks by the National Center for Health Statistics. National Ambulatory Medical Care Survey and NHAMCS are conducted by the CDC and the National Center for Health Statistics (NCHS), Division of Health Care Statistics, and National Health Care Survey. Public access data files and detailed documentation about these surveys are available at NAMCS on ftp.cdc.gov19 or NHAMCS on ftp.cdc.gov.20
Population trends for visits rates and antibiotics rates were determined by using U.S. census data for adults 18 years and older. The Population Estimates Program publishes total population estimates each year including demographic components (births, deaths, and migration) as well as estimates by age, sex, race, and Hispanic origin. Public access data are available at http://www.census.gov/popest/estimates.php.21
Classification of Outpatient Visits
All outpatient visit records for adults aged 18 years and older between 1995 and 2002 were included. The unweighted number of encounters in all the study years was 284,008. Each outpatient encounter had up to 3-coded diagnoses, using ICD 9th revision (ICD9).22 All outpatient visits were classified into 1 of 4 mutually exclusive groups. The primary population of interest included patients seen for ARI for which antibiotics are rarely indicated (unweighted number of visits 13,048) and included acute bronchitis [ICD9-CM codes 466.0, 466.1, 490], cough [786.2], upper respiratory infection [460.0, 487.1, 465.9], and laryngitis [464.0].
Patients with ARIs in which antibiotics are often appropriate (_N_=17,415 unweighted visits) included otitis media [382.9, 381.4], sinusitis [461.0, 461.9, 473.9, 473.0] pharyngitis and tonsillitis [462.0, 034.0, 034.1], and pneumonia [481, 482, 485, 486]. Patients with nonrespiratory infections in which antibiotics are often appropriate (_N_=13,706 unweighted visits) included urinary tract infection [595.0, 595.9, 599.0, 599.7, 590.0, 590.1, 590.8], orchitis/cervicitis [614.9, 616.0, 616.10, 604.90], sexually transmitted diseases [098.0, 099.0, 099.40, 099.41, 131.00, 131.9], prostatitis [601.0, 601.9], and cellulitis [680.X, 681.X, 682.X]. Visits with multiple diagnoses were classified in the following priority: (1) ARIs—antibiotics often indicated, (2) Nonrespiratory infections—antibiotics often indicated, and (3) ARIs—antibiotics rarely indicated. Patients with none of these diagnoses were grouped into a fourth category: all other visits (239,839 unweighted visits). We excluded patients with any diagnosis of chronic obstructive pulmonary disease (COPD) or HIV infection, as antibiotics may be indicated for a wider group of respiratory diagnoses for patients with these conditions.23–25
Antibiotics
We identified antibiotic prescriptions using both trade and generic names. We classified penicillin, amoxicillin, ampicillin, erythromycin, tetracycline, doxycycline, sulfonamides, and trimethoprim as narrow spectrum-agents, and amoxicillin-clavulanic acid, cephalosporins, other macrolides, and fluoroquinolones as broad-spectrum antibiotics. This classification strategy is consistent with those used in previous investigations,9 and included 92% to 96% of oral antimicrobials prescribed in the outpatient settings.
Statistical Analysis
Both NAMCS and NHAMCS files were combined in a single dataset, accounting for the sampling design as recommended by the NCHS. In order to improve the precision of the estimates, individual years were combined in pairs and 4 time periods were defined. All estimates had <30% relative standard error and were based on 30 or more cases in the sample data, which is considered reliable by the standards of the National Center for Health Statistics.
Antibiotic Prescribing for ARI
We estimated the proportion of all outpatient visits and diagnosis-specific outpatient visits that were associated with an antibiotic prescription, and the proportion of antibiotics that were broad spectrum. We used a multiple logistic regression analysis to evaluate time trends in the proportion of visits associated with an antibiotic prescription, using odds ratios (ORs) and 95% confidence intervals (CIs). We determined a priori other covariates in the model based on clinical significance. These included patient age (18 to 64, 65 to 74, >75 years old), sex, race (white, black, other), practice location (urban or rural), location of care (office-based practice, hospital-based practice, ED), region of country (North, South, East, West), practitioner type (physician, resident physician or nonphysician provider), and insurance type (insured, Medicare, Medicaid, self-pay, other). We chose clinically relevant interaction terms to develop our model, which included interactions between the time period and provider type and between time period and location of care. These were not statistically significant and were not included in the final model. To account for the survey's multistage sampling design, weights were incorporated into the logistic regression model.26 The statistical analyses were conducted using Stata version 8, (Stata Corporation, College Station, Tex).
Population Level Analysis
To determine average annual rates of outpatient visits per 1,000 persons, we defined the total number of visits and visits that resulted in an antibiotic prescription, divided by the civilian U.S. population aged 18 years and older, derived from U.S. Census Bureau, for each year 1995 to 2002.21 Rates were generated accounting for both the sampling design and the combination of 2 years.
This study was approved by the Institutional Review Board of Vanderbilt University. The funding agency played no role in the design, conduct, analysis, interpretation, preparation, review, or approval of the data, and manuscript.
RESULTS
Antibiotic Prescribing by Diagnosis
Overall, the proportion of visits in which an antibiotic was prescribed decreased from 17.9% to 15.3% during the study period (Table 1), with antibiotic prescribing for patients with ARIs where antibiotics are rarely indicated falling from 59.9% to 49.1%. Over the same time period, approximately 70% of patients with ARIs where antibiotics are appropriate received an antibiotic prescription. Between 58% and 65% of patients with nonrespiratory diagnoses requiring antibiotics received an antibiotic prescription, but only 6.3% to 6.8% of patients with all other diagnoses received an antibiotic prescription.
Table 1.
Percentage of Antibiotics Prescribed for Each Diagnostic Category over Time (Top) and Proportion of Antibiotics Prescribing by Location of Care for Respiratory Diagnoses Where Antibiotics Are Rarely Indicated (Bottom)
| Percent (%) | ||||
|---|---|---|---|---|
| 1995 to 1996 | 1997 to 1998 | 1999 to 2000 | 2001 to 2002 | |
| Proportion of outpatient visits in which antibiotics were prescribed by visit category | ||||
| Total | 17.9 | 16.3 | 15.6 | 15.3 |
| Acute respiratory infections—antibiotics rarely indicated | 59.9 | 54.8 | 43.1 | 49.1 |
| Respiratory infections—antibiotics often indicated | 71.4 | 71.4 | 70.0 | 72.4 |
| Nonrespiratory infections—antibiotics often indicated | 65.6 | 58.3 | 62.8 | 62.4 |
| All other diagnoses | 6.9 | 6.3 | 6.5 | 6.5 |
| Proportion of antibiotics prescribed for acute respiratory infections—antibiotics rarely indicated by location of care | ||||
| Emergency department | 57.8 | 50.5 | 45.7 | 50.7 |
| Office practice | 60.9 | 55.4 | 42.8 | 48.9 |
| Hospital practice | 49.4 | 55.1 | 42.2 | 48.9 |
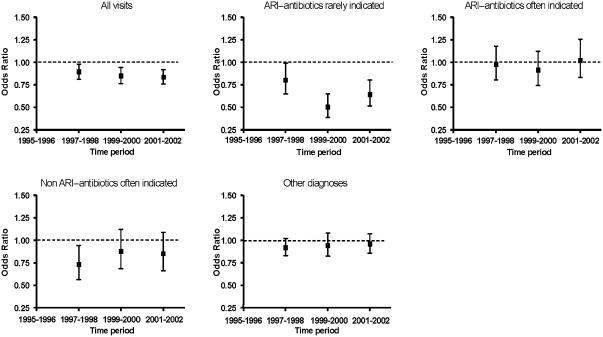
After adjusting for potential confounders, a consistent decline in the proportion of all visits in which an antibiotic was prescribed was observed over the study period. Compared with 1995 to 1996, the proportion of visits associated with an antibiotic prescription was lower in 1997 to 1998 (adjusted OR 0.89; 95% CI 0.81 to 0.98), 1999 to 2000 (adjusted OR 0.85; 95% CI 0.76 to 0.94), and 2001 to 2002 (adjusted OR 0.84; 95% CI 0.76 to 0.92). When each diagnostic category was examined for a reduction in antibiotic use, a significant decline in antibiotic prescribing was observed only for ARIs where antibiotics are rarely indicated. There was no consistent decrease in antibiotic prescribing associated with the other diagnostic categories (Fig. 1).
Figure 1.
Antibiotic prescription (as odds ratio) during study periods, by diagnosis. Outpatients aged 18 and older, U.S. 1995 to 2002.(Model adjusted for patient age, sex, race, rural location, practitioner type, region of country, location of care, and patient insurance. The time period 1995 to 1996 is the reference).
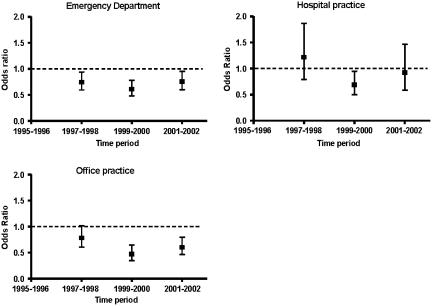
Antibiotic Prescribing by Location of Care
We examined antibiotic prescribing for ARIs in which antibiotics are rarely indicated in all 3 outpatient settings. Antibiotic prescribing from 1995–1996 to 2001–2002 decreased from 57.8% to 50.6% in the ED and from 60.9% to 48.9% in office-based clinics, whereas, there was little change in prescribing associated with hospital-based clinics (Table 1). Antibiotic prescribing in the ED decreased in 1997 to 1998 and remained below 1995 to 1996 levels (adjusted OR 0.76, 95% CI 0.60 to 0.95 for 2001 to 2002 compared with 1995 to 1996). The decline in antibiotic prescribing in office-based practices was statistically significant in 1999 to 2000 (adjusted OR 0.47, 95% CI 0.34 to 0.65) and 2001 to 2002 (adjusted OR 0.60, 95% CI 0.46 to 0.79), compared with 1995 to 1996 (Fig. 2).
Figure 2.
Antibiotic prescription (as odds ratio) during the study period by location of care for acute respiratory infection—antibiotics rarely indicated. Outpatients aged 18 and older in the U.S. 1995 to 2002. (Model adjusted for patient age, sex, race, rural location, practitioner type, region of country, and patient insurance. The time period 1995 to 1996 is the reference.)
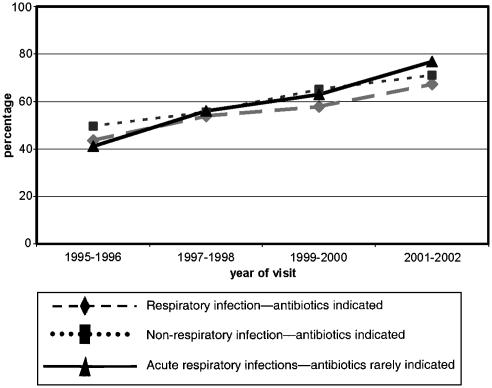
Antibiotics Prescribed for Each Diagnostic Category
The percentage of broad-spectrum antibiotics prescribed for each diagnostic category increased over time (Fig. 3). The largest net increase, 35.7%, was for ARIs where antibiotics were rarely indicated. In this category, broad-spectrum antibiotic prescribing increased from 41.0% of all antibiotics prescribed in 1995 to 1996 to 76.8% of all antibiotics prescribed in 2001 to 2002. For ARIs where antibiotics are often indicated, broad-spectrum antibiotic prescribing increased 23.8% from 43.5% of prescriptions to 67.3% of prescriptions. In the nonrespiratory infections category where antibiotics are often indicated, broad-spectrum use increased 21.5% from 49.6% to 71.1%.
Figure 3.
Trends in Broad-Spectrum antibiotic prescribing in United States for each diagnostic category.
Population-Level Analysis
There was a 17.3% relative increase in outpatient visits between 1995 to 1996 and 2001 to 2002. Over the study period, the absolute number of antibiotics prescribed during outpatient visits fluctuated, with a decrease between 1995 to 1996 and 1999 to 2000, from 302.4 to 294.1 prescriptions, with a subsequent increase in 2001 to 2002 to 304.1 prescriptions per 1,000 adults (Table 2). With increasing numbers of visits and decreasing numbers of prescriptions per visit, the overall number of antibiotics prescribed during outpatient visits for the U.S. adult population changed little over the study period.
Table 2.
Total Visit Rate, and Antibiotic Rates for All Diagnoses Followed by Visit Rate and Antibiotic Rates for Each Diagnostic Category per 1.000 U.S. Adults ≥18 y Old, 1995–2002
| Rates per 1,000 Adults | All Outpatient Visits | ||||
|---|---|---|---|---|---|
| 1995 to 1996 | 1997 to 1998 | 1999 to 2000 | 2001 to 2002 | Percent change1995–1996 to 2001–2002 | |
| Total visits | 1692.7 | 1889.0 | 1880.2 | 1985.7 | +17.3 |
| Antibiotics prescribed | 302.4 | 307.7 | 294.1 | 304.1 | +0.6 |
| Acute respiratory infections—antibiotics rarely indicated | |||||
| Visits | 110.1 | 123.0 | 119.3 | 108.0 | −2.0 |
| Antibiotics prescribed | 65.9 | 67.4 | 51.4 | 53.0 | −19.6 |
| Respiratory diagnoses—antibiotics often indicated | |||||
| Visits | 127.8 | 135.0 | 133.7 | 129.0 | +0.9 |
| Antibiotics prescribed | 91.3 | 96.4 | 93.6 | 93.5 | +2.4 |
| Nonrespiratory diagnoses—antibiotics often indicated | |||||
| Visits | 77.3 | 78.4 | 76.0 | 77.7 | +0.5 |
| Antibiotics prescribed | 50.7 | 45.7 | 47.8 | 48.5 | −4.1 |
| All other diagnoses | |||||
| Visits | 1377.5 | 1552.7 | 1551.2 | 1671.1 | +21.3 |
| Antibiotics prescribed | 94.5 | 98.2 | 101.3 | 109.0 | +15.3 |
DISCUSSION
This study demonstrates that between 1995 and 2002, there was a significant decline in the proportion of outpatient visits that resulted in antibiotics prescribed for U.S. adults. Moreover, our analyses show that this decline was because of a decrease in the proportion of antibiotic prescriptions written for ARIs where antibiotics are rarely indicated. However, despite the observed decline in antibiotic prescribing per health care visit, the use of broad-spectrum antibiotics increased in each diagnostic category, with the largest increase in the category of ARIs where antibiotics are rarely indicated. Financial returns on broad-spectrum antibiotics far exceed the return on narrow-spectrum antibiotics for pharmaceutical companies.27 Directed marketing to both providers and patients may have contributed to the increase in prescribing of more costly and broader-spectrum antimicrobials.27,28
The decrease in antimicrobial prescribing is consistent with the results reported by McCaig et al.29 in adults and similar to our findings and others in children.30,31 This study offers additional evidence that the decrease in antimicrobial prescribing between 1995 and 2002 was because of a decrease in prescribing for ARIs where antibiotics are rarely indicated, suggesting that national educational efforts about appropriate antibiotic prescribing have had a positive effect. While visits rates for this category decreased modestly, there was a relatively large decrease in antibiotic prescriptions associated with these visits. There was no evidence for a shift in coding during the study period to ARIs or other infections where antibiotics are often indicated, because visits for these diagnoses did not change significantly. The finding of reduced antibiotic prescribing for inappropriate indications is encouraging given that antibiotic resistance and health care expenditures are reduced when practitioners limit inappropriate antibiotic prescribing.32 Antibiotic prescribing associated with all other visit categories either decreased or remained stable over the study period. However, because overall visits increased substantially, there was virtually no change in the overall numbers of antibiotics prescribed during medical care visits.
Our study has several limitations. The NAMCS and NHAMCS data are collected through a survey of practitioners' records, and the appropriateness of an antimicrobial prescription cannot always be assessed because of the inability to link to a specific diagnosis. Practitioners were given the “benefit of the doubt” and appropriate antibiotic use was assigned if one of the diagnoses in which antibiotics were appropriate were listed. Another limitation of the study was the exclusion of persons with COPD and AIDS as well as those cared for at federal hospitals from the numerator, but not from the denominator. This will consistently underestimate the rates of antibiotics prescribed, but should have minor effects on trends seen over time.
Given the large number of visits and the inclusion of a representative sample of outpatient clinics and ED settings in the United States, our findings that antibiotic prescribing has declined for adults with ARIs in which antibiotics are rarely indicated are positive. However, many opportunities for improving antibiotic prescribing remain. If there were no further antibiotics prescribed for respiratory diagnoses where antibiotics are rarely indicated, there would be 53 fewer antimicrobial prescriptions per 1,000 adults in the United States. Antibiotic prescribing, however, would still be substantial. In fact, 6% of visits in which there is no diagnostic indication of infection resulted in an antibiotic prescription; in order to have a population-level impact on the absolute number of antibiotics prescribed, further studies are needed to explain the reasons why antibiotics are prescribed during these types of visits.
To maximize appropriate antibiotic utilization, new approaches may be needed. For example, new and improved viral and bacterial vaccines could reduce respiratory infections and subsequent antibiotic use.30,31,33–37 Another approach is to identify situations where treatment with “watchful waiting” is appropriate, such as otitis media with effusion.38 Educational efforts and evidence-based practice guidelines directed at both providers and patients should clearly delineate situations in which antibiotic are appropriate and when narrow-spectrum antibiotics are the best choice. Finally, we need to question whether educational efforts alone are sufficient to address the important problem of antibiotic overuse.
Acknowledgments
This material is based upon work supported by the Veterans Affairs Clinical Research Center of Excellence (CRCoE)(C. L. R., M. R. G.).
Public Health Service award K12 RR017697 for the Vanderbilt Mentored Clinical Research Scholar Program (N. B. H.).
Vanderbilt Center for Education and Research Vanderbilt Center for Education and Research on Therapeutics, Vanderbilt University School of Medicine (M. R. G.).
Geriatric Research Education and Clinical Center, Veterans Affairs, Tennessee Valley Healthcare System, Nashville, Tenn (C. L. R., M. R. G., R. S. D.)
General Clinical Research Center, Vanderbilt University School of Medicine, Nashville, Tenn (K. M. E.).
References
- 1.Arroll B, Kenealy T. Antibiotics for the common cold. Cochrane Database Syst Rev. 2002:CD000247. doi: 10.1002/14651858.CD000247. [DOI] [PubMed] [Google Scholar]
- 2.Thomas MG, Arroll B. “Just say no”—reducing the use of antibiotics for colds, bronchitis and sinusitis. N Z Med J. 2000;113:287–9. [PubMed] [Google Scholar]
- 3.McGowan JE., Jr Economic impact of antimicrobial resistance. Emer Infect Dis. 2001;7:286–92. doi: 10.3201/eid0702.010228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bertino JS. Cost burden of viral respiratory infections: issues for formulary decision makers. Am J Med. 2002;112(suppl 6A):42S–9S. doi: 10.1016/s0002-9343(01)01063-4. [DOI] [PubMed] [Google Scholar]
- 5.McCaig LF, Hughes JM. Trends in antimicrobial drug prescribing among office-based physicians in the United States. JAMA. 1995;273:214–9. [PubMed] [Google Scholar]
- 6.Gonzales R, Steiner JF, Sande MA. Antibiotic prescribing for adults with colds, upper respiratory tract infections, and bronchitis by ambulatory care physicians. JAMA. 1997;278:901–4. [PubMed] [Google Scholar]
- 7.Steinman MA, Landefeld CS, Gonzales R. Predictors of broad-spectrum antibiotic prescribing for acute respiratory tract infections in adult primary care. JAMA. 2003;289:719–25. doi: 10.1001/jama.289.6.719. [DOI] [PubMed] [Google Scholar]
- 8.Steinman MA, Gonzales R, Linder JA, Landefeld CS. Changing use of antibiotics in community-based outpatient practice, 1991–1999. Ann Intern Med. 2003;138:525–33. doi: 10.7326/0003-4819-138-7-200304010-00008. [DOI] [PubMed] [Google Scholar]
- 9.Mainous AG, III, Hueston WJ, Davis MP, Pearson WS. Trends in antimicrobial prescribing for bronchitis and upper respiratory infections among adults and children. Am J Public Health. 2003;93:1910–4. doi: 10.2105/ajph.93.11.1910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Finkelstein JA, Davis RL, Dowell SF, et al. Reducing antibiotic use in children: a randomized trial in 12 practices. Pediatrics. 2001;108:1–7. doi: 10.1542/peds.108.1.1. [DOI] [PubMed] [Google Scholar]
- 11.Gonzales R, Steiner JF, Lum A, Barrett PH., Jr Decreasing antibiotic use in ambulatory practice: impact of a multidimensional intervention on the treatment of uncomplicated acute bronchitis in adults. JAMA. 1999;281:1512–9. doi: 10.1001/jama.281.16.1512. [DOI] [PubMed] [Google Scholar]
- 12.Perz JF, Craig AS, Coffey CS, et al. Changes in antibiotic prescribing for children after a community-wide campaign. JAMA. 2002;287:3103–9. doi: 10.1001/jama.287.23.3103. [DOI] [PubMed] [Google Scholar]
- Get smart know when antibiotics work. Centers for Disease Control and Prevention; Available at: http://www.cdc.gov/drugresistance/community/ Accessed February 15, 2005.
- 14.Snow V, Mottur-Pilson C, Gonzales R. Principles of appropriate antibiotic use for treatment of nonspecific upper respiratory tract infections in adults. Ann Intern Med. 2001;134:487–9. doi: 10.7326/0003-4819-134-6-200103200-00014. [DOI] [PubMed] [Google Scholar]
- 15.Snow V, Mottur-Pilson C, Gonzales R. Principles of appropriate antibiotic use for treatment of acute bronchitis in adults. Ann Intern Med. 2001;134:518–20. doi: 10.7326/0003-4819-134-6-200103200-00020. [DOI] [PubMed] [Google Scholar]
- 16.Gonzales R, Bartlett JG, Besser RE, et al. Principles of appropriate antibiotic use for treatment of uncomplicated acute bronchitis: background. Ann Intern Med. 2001;134:521–9. doi: 10.7326/0003-4819-134-6-200103200-00021. [DOI] [PubMed] [Google Scholar]
- 17.Gonzales R, Bartlett JG, Besser RE, et al. Principles of appropriate antibiotic use for treatment of acute respiratory tract infections in adults: background, specific aims, and methods. Ann Intern Med. 2001;134:479–86. doi: 10.7326/0003-4819-134-6-200103200-00013. [DOI] [PubMed] [Google Scholar]
- 18.Gonzales R, Bartlett JG, Besser RE, Hickner JM, Hoffman JR, Sande MA. Principles of appropriate antibiotic use for treatment of nonspecific upper respiratory tract infections in adults: background. Ann Intern Med. 2001;134:490–4. doi: 10.7326/0003-4819-134-6-200103200-00015. [DOI] [PubMed] [Google Scholar]
- 19.NAMCS. Available at: http://www.cdc.gov/nchs/about/major/ahcd/namcsdes.htm Accessed February 15, 2005.
- 20.NHAMCS. Available at: http://www.cdc.gov/nchs/about/major/ahcd/nhamcsds.htm Accessed February 15, 2005.
- 21.US Population Estimates. Available at: http://www.census.gov/population/www/estimates/uspop.html Accessed February 15, 2005.
- 22.International Classification of Diseases, Ninth Revision, Clinical Modification. Washington, DC: Public Health Service, US Department of Health and Human Services; 1988. [Google Scholar]
- 23.Snow V, Lascher S, Mottur-Pilson C. The evidence base for management of acute exacerbations of COPD: clinical practice guideline, part 1. Chest. 2001;119:1185–9. doi: 10.1378/chest.119.4.1185. [DOI] [PubMed] [Google Scholar]
- 24.Peng CC, Aspinall SL, Good CB, Atwood CW, Jr, Chang CC. Equal effectiveness of older traditional antibiotics and newer broad-spectrum antibiotics in treating patients with acute exacerbations of chronic bronchitis. South Med J. 2003;96:986–91. doi: 10.1097/01.SMJ.0000054536.50460.F1. [DOI] [PubMed] [Google Scholar]
- 25.Adams SG, Melo J, Luther M, Anzueto A. Antibiotics are associated with lower relapse rates in outpatients with acute exacerbations of COPD. Chest. 2000;117:1345–52. doi: 10.1378/chest.117.5.1345. [DOI] [PubMed] [Google Scholar]
- 26.Eltinge JL, Sribney WM. Estimates of linear combinations and hypothesis tests for survey data. Stata Tech Bull. 1996;31:31–42. 246–59. [Google Scholar]
- 27.Reed SD, Laxminarayan R, Black DJ, Sullivan SD. Economic issues and antibiotic resistance in the community. Ann Pharmacother. 2002;36:148–54. doi: 10.1345/aph.1A121. [DOI] [PubMed] [Google Scholar]
- 28.Vogel RJ, Ramachandran S, Zachry WM. A 3-stage model for assessing the probable economic effects of direct-to-consumer advertising of pharmaceuticals. Clin Ther. 2003;25:309–29. doi: 10.1016/s0149-2918(03)90043-9. [DOI] [PubMed] [Google Scholar]
- 29.McCaig LF, Besser RE, Hughes JM. Antimicrobial drug prescription in ambulatory care settings, United States, 1992–2000. Emerg Infect Dis. 2003;9:432–7. doi: 10.3201/eid0904.020268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Halasa NB, Griffin MR, Zhu Y, Edwards KM. Decreased number of antibiotic prescriptions in office-based settings from 1993 to 1999 in children less than five years of age. Pediatr Infect Dis J. 2002;21:1023–8. doi: 10.1097/00006454-200211000-00009. [DOI] [PubMed] [Google Scholar]
- 31.Finkelstein JA, Stille C, Nordin J, et al. Reduction in antibiotic use among US children, 1996–2000. Pediatrics. 2003;112(3 Part 1):620–7. doi: 10.1542/peds.112.3.620. [DOI] [PubMed] [Google Scholar]
- 32.Molstad S, Cars O. Major change in the use of antibiotics following a national programme: Swedish Strategic Programme for the Rational Use of Antimicrobial Agents and Surveillance of Resistance (STRAMA) Scand J Infect Dis. 1999;31:191–5. doi: 10.1080/003655499750006263. [DOI] [PubMed] [Google Scholar]
- 33.O'Brien KL, Santosham M. Potential impact of conjugate pneumococcal vaccines on pediatric pneumococcal diseases. Am J Epidemiol. 2004;159:634–44. doi: 10.1093/aje/kwh082. [DOI] [PubMed] [Google Scholar]
- 34.Amsden GW. Pneumococcal resistance in perspective: how well are we combating it? Pediatr Infect Dis J. 2004;23(2 suppl):S125–8. doi: 10.1097/01.inf.0000112526.55182.e0. [DOI] [PubMed] [Google Scholar]
- 35.Jenson HB, Baltimore RS. Impact of pneumococcal and influenza vaccines on otitis media. Curr Opin Pediatr. 2004;16:58–60. doi: 10.1097/00008480-200402000-00011. [DOI] [PubMed] [Google Scholar]
- 36.Talbot TR, Poehling KA, Hartert TV, et al. Reduction in high rates of antibiotic-nonsusceptible invasive pneumococcal disease in tennessee after introduction of the pneumococcal conjugate vaccine. Clin Infect Dis. 2004;39:641–8. doi: 10.1086/422653. [DOI] [PubMed] [Google Scholar]
- 37.Talbot TR, Poehling KA, Hartert TV, et al. Elimination of racial differences in invasive pneumococcal disease in young children after introduction of the conjugate pneumococcal vaccine. Pediatr Infect Dis J. 2004;23:726–31. doi: 10.1097/01.inf.0000133046.60555.de. [DOI] [PubMed] [Google Scholar]
- 38.Subcommittee on Otitis Media with Effusion. Clinical practice guideline from American Academy of Otolaryngology—Head and Neck Surgery and American Academy of Pediatics Subcommittee on Otitis Media with Effusion. Pediatrics. 2004;113:1412–29. [Google Scholar]