Lack of In Vitro and In Vivo Recognition of Francisella tularensis Subspecies Lipopolysaccharide by Toll-Like Receptors (original) (raw)
Abstract
Francisella tularensis is an intracellular gram-negative bacterium that is highly infectious and potentially lethal. Several subspecies exist of varying pathogenicity. Infection by only a few organisms is sufficient to cause disease depending on the model system. Lipopolysaccharide (LPS) of gram-negative bacteria is generally recognized by Toll-like receptor 4 (TLR4)/MD-2 and induces a strong proinflammatory response. Examination of human clinical F. tularensis isolates revealed that human virulent type A and type B strains produced lipid A of similar structure to the nonhuman model pathogen of mice, Francisella novicida. F. novicida LPS or lipid A is neither stimulatory nor an antagonist for human and murine cells through TLR4 or TLR2. It does not appear to interact with TLR4 or MD-2, as it is not an antagonist to other stimulatory LPS. Consistent with these observations, aerosolization of F. novicida LPS or whole bacteria induced no inflammatory response in mice. These results suggest that poor innate recognition of F. tularensis allows the bacterium to evade early recognition by the host innate immune system to promote its pathogenesis for mammals.
Francisella tularensis is a highly infectious gram-negative bacterium, designated a class A select agent by the Centers for Disease Control and Prevention (12, 40). The genus Francisella consists of four organisms: F. tularensis subsp. tularensis (type A), F. tularensis subsp. holarctica (type B), F. tularensis subsp. mediasiatica, and Francisella novicida. F. tularensis subsp. tularensis (type A) is the most virulent and found in North America. F. tularensis subsp. holarctica (type B) is less virulent and is found in North America, Europe, and Asia. The live vaccine strain (LVS) is a type B isolate. LVS is nonpathogenic in humans (and is used as a vaccine) but causes severe disease in inbred mice (22, 42). F. tularensis subsp. mediasiatica has only been isolated from Central Asia and is also considered to be of low virulence (39). A fourth organism F. novicida, causes severe disease in inbred mice, similar to type A isolates in humans, but is not pathogenic for immunocompetent humans (12). F. novicida was not distinguishable from F. tularensis on the basis of DNA hybridization, and 16S ribosomal sequences of F. tularensis and F. novicida have a high degree of similarity (99.6%) (16, 24, 38). Recently, F. novicida has been shown to be more virulent in mice than LVS, requiring a smaller inoculum and having a shorter time to disease than LVS, although the basis for these differences is unknown (25).
Lipopolysaccharide (LPS) is the major component of the outer leaflet of the outer membrane of gram-negative bacteria. LPS has three structural regions: O-antigen, core, and lipid A. O-antigen and core consist of polysaccharide chains, whereas lipid A (the bioactive component of LPS) is primarily fatty acids and phosphate substituents bonded to a central glucosamine dimer (31, 41). LPS is also known as an endotoxin because the lipid A portion of LPS induces strong proinflammatory responses. LPS from enteric bacteria is the prototypical highly stimulatory lipid A recognized by Toll-like receptor 4 (TLR4) (1, 6, 27). In humans, TLR4 polymorphisms have been associated with hyporesponsiveness to inhaled endotoxin (2). When mice are exposed to aerosolized LPS, cytokines and chemokines are rapidly produced and large numbers of neutrophils are recruited into the airways by 4 h (34).
To date, the structure of the major lipid A component isolated from two F. tularensis subsp. holarctica (type B) strains, LVS and strain 1547-57, after growth at 37°C has been determined. A major lipid A for both type B strains was determined to be a tetra-acylated structure containing three 3-OH C18 fatty acids, one C16 fatty acid, and one phosphate group (30, 44). For strain 1547-57 only, an additional galactosamine residue was present on the 1-position phosphate (30).
In this report, we found that multiple clinical and environmental isolates of F. tularensis subspecies (F. tularensis subsp. tularensis [type A], F. tularensis subsp. holarctica [type B], and F. tularensis subsp. mediasiatica) shared the same lipid A structure as F. novicida. Therefore, we further analyzed the in vitro and in vivo activity of highly purified and well-characterized F. novicida LPS.
MATERIALS AND METHODS
Bacterial strains and growth conditions.
F. novicida strain U112, obtained from Francis Nano (University of Victoria, Victoria, Canada) was grown in tryptic soy broth (Gibco BRL, Grand Island, NY) supplemented with 0.1% cysteine (TSB-C) (Sigma-Aldrich, St. Louis, MO) at 37°C with aeration and harvested in stationary phase. F. tularensis subsp. tularensis (type A), F. tularensis subsp. holarctica (type B), and F. tularensis subsp. mediasiatica were from the University of Umeå, Umeå, Sweden. All strains are catalogued in the Francisella strain collection (Defense Research Agency, Umeå, Sweden). These strains were grown on chocolate II agar plates supplemented with hemoglobin and IsoVitaleX (Becton Dickinson Diagnostic Systems, San Jose, CA) at 37°C in a 5% CO2 incubator for 7 or 5 days, respectively, before harvesting. The Francisella subspecies isolates used are listed in Table 1.
TABLE 1.
Francisella tularensis subspecies isolates used in this study
| Sample no. | Source, collection date (yr), and collection locationa | Species | Subspecies type | Alternative name |
|---|---|---|---|---|
| 33 | Squirrel, Georgia | F. tularensis subsp. tularensis | A1 | SnMF |
| 41 | Tick, 1935, British Columbia, Canada | F. tularensis subsp. tularensis | A1 | Vavenby |
| 42 | Canada | F. tularensis subsp. tularensis | A1 | Utter |
| 46 | Human pleural fluid, 1940, Ohio | F. tularensis subsp. tularensis | A1 | Fox Downs |
| 54 | Hare, 1953, Nevada | F. tularensis subsp. tularensis | A2 | Nevada |
| 237 | Human ulcer, 1941, Ohio | F. tularensis subsp. tularensis | A1 | Schu4 |
| 604 | Foal, 1958, Montana | F. tularensis subsp. tularensis | A2 | BA 8859 |
| 35 | Beaver, 1976, Montana | F. tularensis subsp. holarctica | B423A | |
| 124 | Water, 1990, Ukraine | F. tularensis subsp. holarctica | 14588 | |
| 157 | Human blood, 1994, Sweden | _F. tularensis_subsp. holarctica | CCUG 33270 | |
| 200 | Human skin ulcer, 1998, Sweden | F. tularensis subsp. holarctica | ||
| 24-061 | Human blood, Sweden | F. tularensis subsp. holarctica | ||
| 24-071 | Human blood, Sweden | F. tularensis subsp. holarctica | ||
| 2-5512 | Human skin ulcer, 2003, Sweden | F. tularensis subsp. holarctica | ||
| 2-5738 | Human skin ulcer, 2003, Sweden | F. tularensis subsp. holarctica | ||
| 3-1840 | Human blood, Sweden | F. tularensis subsp. holarctica | ||
| 3-3867 | Human blood, Sweden | F. tularensis subsp. holarctica | ||
| 147 | Miday gerbil, 1965, Kazakhstan | F. tularensis subsp. mediasiatica | 543 | |
| 148 | Ticks, 1982, Central Asia (former USSR) | F. tularensis subsp. mediasiatica | 240 | |
| 149 | Hare, 1965, Central Asia | F. tularensis subsp. mediasiatica | 120 | |
| U112 | Human, 1950, Ogden Bay, Utah | F. novicida | ATCC 15482 |
LPS purification and lipid A isolation.
Large-scale F. novicida LPS preparations were extracted using a hot phenol-water extraction method (45). Subsequently, LPS was treated with RNase A, DNase I, and proteinase K to ensure purity from contaminating nucleic acids and proteins (14). Individual LPS samples were additionally extracted to remove contaminating phospholipids (15) and TLR2-contaminating proteins (21). The yield of LPS per mg dry cells was 0.91 mg LPS/10 mg dry cells. Small-scale LPS preparations were isolated using the rapid isolation method for mass spectrometry analysis as described previously (46). Lipid A was isolated after hydrolysis in 1% sodium dodecyl sulfate at pH 4.5 as described previously (7). Briefly, 500 μl of 1% sodium dodecyl sulfate in 10 mM Na acetate, pH 4.5, was added to a lyophilized sample. Samples were incubated at 100°C for 1 h, frozen, and lyophilized. The dried pellets were resuspended in 100 μl of water, and 1 ml of acidified ethanol (100 μl 4 N HCl in 20 ml 95% ethanol). Samples were centrifuged at 5,000 rpm for 5 min. The lipid A pellet was further washed (three times) in 1 ml of 95% ethanol. The entire series of washes was repeated twice. Samples were resuspended in 500 μl of water, frozen on dry ice, and lyophilized.
Fatty acid analysis.
LPS fatty acids were derivatized to fatty acid methyl esters and analyzed by gas chromatography as described previously (9, 37). Briefly, LPS fatty acids were derivatized to fatty methyl esters with 2 M methanolic HCl at 90°C for 18 h (Alltech, Lexington, KY) and identified and quantified by gas chromatography using an HP 5890 series II with a 7673 autoinjector. Pentadecanioc acid (10 μg; Sigma-Aldrich, St. Louis, MO) was added as an internal standard.
Mass spectrometry procedures.
Negative-ion matrix-assisted laser desorption ionization-time of flight (MALDI-TOF) mass spectrometry (MS) experiments were performed as described for the analysis of LPS or lipid A preparations with the following modifications (13, 18). Lyophilized lipid A was dissolved with 10 μl 5-chloro-2-mercaptobenzothiazole (Sigma-Aldrich, St. Louis, MO) MALDI matrix in chloroform-methanol, 1:1 (vol/vol), and then applied (1 μl) onto the sample plate. All MALDI-TOF experiments were performed using a Bruker Autoflex II MALDI-TOF mass spectrometer (Bruker Daltonics, Inc., Billerica, MA). Each spectrum was an average of 200 shots. ES tuning mix (Agilent, Palo Alto, CA) was used to calibrate the MALDI-TOF MS.
Additional endotoxins.
Escherichia coli O111:B4 and Salmonella minnesota Re595 LPS (Sigma-Aldrich, St. Louis, MO) were reconstituted to 5 mg/ml in 20 mM EDTA or H2O, clarified in an ultrasonic water bath (Cole-Parmer, Vernon Hills, IL), aliquoted, and stored at −80°C. Lipid IVA and Rhodobacter sphaeroides lipid A (RSLA) were from D. T. Golenbock (University of Massachusetts).
THP-1 cell stimulations.
THP-1 cells (200 μl at 2 × 105 cells/ml) were plated in RPMI 1640 medium containing 10% heat-inactivated fetal bovine serum (HyClone, Logan, UT), 2 mM l-glutamine, and 50 nM vitamin D3 (Sigma-Aldrich, St. Louis, MO) in 96-well plates (Corning Costar, Acton, MA) and incubated at 37°C in humid air with 5% CO2 (13). After 72 h, the medium was replaced with fresh medium containing sonically dispersed LPS ligands or no added stimulus. After 6 h or 24 h of incubation, supernatants were harvested and stored at −80°C until assayed. Interleukin-8 (IL-8) and tumor necrosis factor alpha (TNF-α) production by THP-1 cells was measured by enzyme-linked immunosorbent assay (ELISA) 22 h after stimulation per the manufacturer's instructions (Pierce-Endogen, Rockford, IL).
RAW 264.7 cell stimulation.
RAW 264.7 cells (200 μl at 2 × 105 cells/ml) were plated in RPMI containing 10% fetal calf serum (HyClone, Logan, UT) in flat-bottom 96-well plates 2 days before stimulation. On the day of stimulation, the medium was replaced with fresh medium containing various ligands in the presence of 5 μg/ml brefeldin A. Cells were stimulated for 3 h at 37°C in a CO2 incubator followed by staining for intracellular TNF-α as previously described (20). Fc receptors were blocked with 5% goat serum in 50 μl fluorescence-activated cell sorter (FACS) buffer (1% bovine serum albumin in phosphate-buffered saline plus 0.09% sodium azide) on ice for 10 min. Paraformaldehyde (150 μl at 2% [vol/vol] concentration) was then added to each well, and the cells were incubated at room temperature for 15 min. Cells were washed once in phosphate-buffered saline (PBS) and then stained and permeabilized with 0.1% saponin (in PBS with 1% fetal calf serum and 0.1% sodium azide) and 1:100 _R_-phycoerythrin-anti-TNF-α (PharMingen, San Diego, CA) for 30 min at room temperature. Cells were washed twice in PBS and analyzed on a FACScan (BD Biosciences, San Jose, CA) using CellQuest Pro software.
HEK-293 transfections.
HEK-293 cells (200 μl at 2 × 105 cells/ml) were plated in Dulbecco's modified Eagle's medium plus 10% fetal calf serum in flat-bottom 96-well plates the day before transfection (19). The next day, 5 μl of transfection reagent (1:1 mix of 0.25 M CaCl2 containing DNA and 2× BBS [50 mM BES, 280 mM NaCl, 1.5 mM Na2HPO4]) were added to each well. The following amounts of DNA were added per well: ELAM-Luc, 0.01 μg; _Renilla_-Luc, 0.0002 μg; murine CD14 (mCD14) or human CD14 (hCD14), 0.0025 μg; mMD-2 or hMD-2, 0.0025 μg; mTLR2 or hTLR2, 0.0025 μg (when alone) or 0.00125 μg (when cotransfected with TLR1 or TLR6); mTLR1, 0.0125 μg; mTLR6, 0.00125 μg; hTLR1, 0.00125 μg; hTLR6, 0.0125 μg; mTLR4, 0.00025 μg; hTLR4, 0.002 μg. All TLR constructs were hemagglutinin tagged, and the amount of TLR DNA used was normalized based on relative expression from anti-hemagglutinin Western blots. All transfections were normalized to 0.05 μg total DNA with the addition of empty vector. After 3 h, the medium was replaced with fresh medium. The cells were stimulated the next day for 4 h and then lysed with 50 μl passive lysis buffer (Promega, Madison, WI), and luciferase activity was measured in 10 μl of the lysate using the Dual Luciferase reporter assay system (Promega, Madison, WI).
Stimulation of mouse MH-S alveolar macrophages.
Low-passage MH-S cells in RPMI 1640 medium containing 10% heat-inactivated fetal calf serum, 10 mM HEPES, 2 mM l-glutamine, 100 U/ml penicillin, and 100 μg/ml streptomycin were seeded onto 24- or 48-well plates (Corning Costar, Acton, MA) that had been pretreated with 0.01% poly-l-lysine (Sigma-Aldrich, St. Louis, MO) and incubated at 37°C in humid air with 5% CO2. After 20 h, the medium was replaced with fresh medium containing sonically dispersed LPS ligands or no added stimulus. After 6 h or 24 h of incubation, supernatants were harvested and stored at −80°C until assayed.
Animals.
Male and female C57BL/6 mice, 6 to 8 weeks of age, were purchased from Jackson Laboratories (Bar Harbor, ME). Mice were housed in filtered cages under specific-pathogen-free conditions and permitted unlimited access to sterile food and water. All animal experiments were approved by the Institutional Animal Care and Use Committee of the University of Washington.
Animal exposure to aerosolized LPS and bacteria.
For each LPS exposure, an aliquot of F. novicida or E. coli LPS was thawed, sonically dispersed, and diluted in sterile, endotoxin-free PBS (Mediatech, Herndon, VA). For challenges with live bacteria, F. novicida was grown to stationary phase in TSB-C, washed twice, and resuspended in endotoxin-free PBS. Mice were exposed to aerosolized LPS or live bacteria in a 36-port nose-only chamber (In-Tox Products, Moriarty, NM). Aerosols were generated from UniHeart jet nebulizers (Westmed, Tucson, AZ) containing LPS suspended in 5 ml PBS at concentrations of 10, 100, or 1,000 μg/ml or live F. novicida suspended in 5 ml PBS at 108 (low dose) or 109 (high dose) CFU/ml (estimated by optical density and confirmed by quantitative culture). Control animals were exposed to aerosolized PBS. The nebulizers were driven at 40 lb/in2, and airflow through the chamber was maintained at 5 liter/min by negative pressure for the 10-min exposure period. Immediately after exposure to each concentration of live bacteria, 3 animals were killed with an overdose of intraperitoneal pentobarbital to determine bacterial deposition by quantitative culture of homogenized lung tissue. Four hours and 24 h after aerosol exposure, mice were killed with pentobarbital and exsanguinated by cardiac puncture before undergoing bronchoalveolar lavage (BAL), as described previously (36). Normal mice unexposed to aerosols also were lavaged for additional control specimens. BAL cells were pelleted by centrifugation and counted in a hemacytometer, and differentials were determined by examination of cytocentrifuge slides stained with Diff-Quik (Dade Behring, Dudingen, Switzerland). BAL fluid supernatants were stored at −80°C.
Measurement of cytokines.
Murine TNF-α, macrophage inflammatory protein-2 (MIP-2, CXCL2), keratinocyte-derived chemokine (KC, CXCL1), IL-10, and human IL-8 (CXCL8) were measured by sandwich ELISA, using antibody pairs and recombinant standards purchased from R&D Systems (Minneapolis, MN).
Data analysis.
Data are expressed as means ± standard errors. Statistical comparisons among groups for continuous variables measured at multiple time points were made by one-way analysis of variance with Tukey's post hoc test. A P value of ≤0.05 was considered significant.
RESULTS
Characterization of lipid A isolated from laboratory and clinical isolates of Francisella tularensis subspecies.
The structure of the lipid A component of LPS was determined from clinical and environmental isolates from F. tularensis subspecies. Lipid A was isolated from 7 F. tularensis subsp. tularensis (type A) isolates, 10 F. tularensis subsp. holarctica (type B) isolates, 3 F. tularensis subsp. mediasiatica isolates, and 1 F. novicida isolate grown at 37°C (Table 1) in TSB-C. Individual LPS preparations were hydrolyzed to lipid A using mild acid hydrolysis conditions and analyzed by MALDI-TOF MS (Fig. 1; representative examples for each F. tularensis subspecies are shown).
FIG. 1.
MALDI-TOF MS of lipid A of Francisella tularensis subspecies. Lipid A was isolated from clinical and environmental isolates of F. tularensis subspecies (Table 1) after growth at 37°C and analyzed by MALDI-TOF MS in the negative-reflection ion mode. Representative examples for each F. tularensis subspecies are shown. (A to C) F. tularensis subsp. Tularensis (type A); (D to F) F. tularensis subsp. holarctica (type B); (G and H) F. tularensis subsp. mediasiatica; (I) F. novicida.
MALDI-TOF analysis of lipid A isolated from all clinical and environmental isolates of F. tularensis subspecies grown at 37°C (Fig. 1; Table 1) contained two tetra-acylated molecular ion species, m/z 1,665 and m/z 1,637. Higher-order MS (IRC-FT-MS) structural analysis of only these molecular ion species for F. novicida lipid A showed that the species at m/z 1,665 represented a single lipid A structure that contained 2 3-OH C18, 1 3-OH C16, and 1 C18 acyl group, as previously described for two type B isolates (30, 44). However, the molecular ion species at m/z 1,637 represented a mixture of four different lipid A structures (three structures that contained 2 3-OH C18, 1 3-OH C16, and 1 C16 acyl groups at different locations on the lipid A backbone and one structure that contained 3 3-OH C18 and 1 C14 acyl group) (data not shown). In addition, lipid A structures (m/z 1,637 and 1,665) contained a phosphogalactosamine group located at the 1 position on the diglucosamine backbone as previously described (30). Finally, the two smaller molecular ion species at m/z 1,476 (from m/z 1,637) and 1,504 (from m/z 1,665) represent tetra-acylated lipid A structures corresponding to the loss of the 1 position phosphogalactosamine (m/z 161) and may represent precursors in the biosynthetic pathway of F. novicida lipid A or possibly artifacts of the samples preparation or MS analysis. As shown previously, the m/z 1,504 structure is similar to the lipid A structure isolated from F. tularensis subsp. holarctica strain LVS (44). Fatty acid quantitation by gas chromatography corroborated the interpretation of the MALDI-TOF spectra (data not shown).
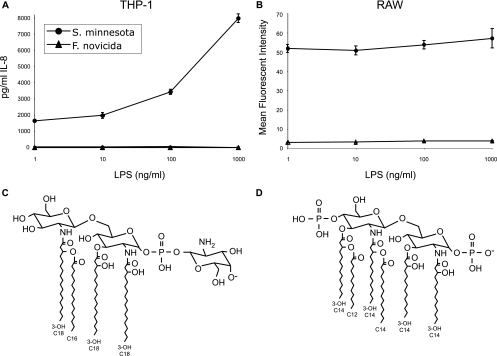
Neither human nor murine monocyte/macrophage cell lines respond to F. novicida LPS.
Since the structure of F. novicida lipid A was identical to that of all of the clinical and environmental isolates of F. tularensis subspecies (Fig. 1), we further characterized the biological activity of F. novicida LPS (Fig. 2C). The human monocytic THP-1 cell line and the murine macrophage RAW 264.7 cell line were each stimulated with increasing concentrations of F. novicida LPS (1 to 1,000 ng/ml). Salmonella minnesota Re595 LPS was used as a positive control (Fig. 2D). F. novicida LPS did not stimulate IL-8 production by THP-1 cells or TNF-α by RAW 264.7 cells at all concentrations tested (Fig. 2A and B). S. minnesota Re595 LPS, a prototypic highly acylated LPS, was a potent stimulator of both human and murine cells, resulting in production of high levels of IL-8 and TNF-α at all concentrations tested (Fig. 2A and B). These results demonstrate that human and murine cells that can respond to prototypical enteric LPS do not recognize tetra-acylated F. novicida LPS.
FIG. 2.
Lack of responsiveness to F. novicida LPS by monocytic cells. Human THP-1 cells (A) or murine RAW 264.7 cells (B) were stimulated with increasing amounts of F. novicida LPS or S. minnesota Re595 LPS. IL-8 secretion was measured in supernatants by ELISA 18 h after stimulation of THP-1 cells, and intracellular TNF-α production was measured by FACS in RAW cells 3 h after stimulation. Values are the means of results from triplicate wells ± standard deviations. One experiment representative of three similar experiments is shown. Chemical structures of the tetra-acylated lipid A from F. novicida (m/z 1,665) (C) and the hexa-acylated lipid A from S. minnesota Re595 (m/z 1797) (D) are shown.
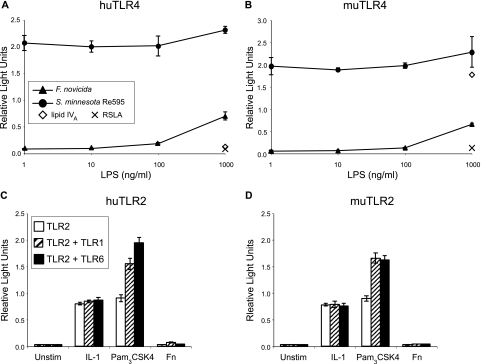
Neither human nor murine TLR4 or TLR2 recognize F. novicida LPS structures.
To test whether F. novicida LPS was recognized by TLR4 or TLR2, a human embryonic kidney cell line (HEK-293) that does not respond to LPS was transiently transfected with either mTLR4 or hTLR4, MD-2, and hCD14. Using ELAM-luciferase as a readout of NF-κB activity and β-actin-Renilla luciferase as a transfection control, cells transfected with hTLR4-MD-2 or mTLR4-MD-2 were found to respond only to the highest concentration (1,000 ng/ml) of F. novicida LPS (Fig. 3A and B). In contrast, S. minnesota Re595 LPS was a potent stimulator of both hTLR4 and mTLR4 even at 1 ng/ml (Fig. 3A and B). These responses required expression of all three components of the LPS receptor complex (CD14, MD-2, and TLR4), and similar responses were observed when mCD14 was substituted for hCD14 (data not shown). Identical responses were also observed when LPS preparations were repurified by phenol extraction to eliminate trace amounts of lipoprotein and when lipid A rather than LPS was used (data not shown). As controls, cells were also stimulated with 1,000 ng/ml of the disaccharide precursor of lipid A from enteric bacteria termed lipid IVA, a hTLR4 antagonist but mTLR4 agonist structure, and RSLA, an hTLR4 and mTLR4 antagonist structure (17). As expected, RSLA did not induce the reporter in either transfection, whereas lipid IVA did so only in mTLR4-MD-2-transfected cells (Fig. 3A and B).
FIG. 3.
Neither TLR4 nor TLR2 mediates recognition of F. novicida LPS. HEK-293 cells were transiently transfected with hTLR4-MD-2 (A), mTLR4-MD-2 (B), hTLR2 ± hTLR1 or TLR6 (C), or mTLR2 ± mTLR1 or TLR6 (D). All cells were also transfected with hCD14. Cells were stimulated for 4 h with indicated ligands, and ratios of the ELAM-luciferase reading to the β-actin-Renilla luciferase reading (relative light units) are plotted. IL-1β (10 ng/ml), Pam3CSK4 (1 μg/ml), or F. novicida LPS (1 μg/ml) was added to each well in experiments for which results are shown in panels C and D. Values are the means of results from triplicate wells ± standard deviations. One experiment representative of three similar experiments is shown. Unstim, unstimulated.
LPS from some bacterial species have been demonstrated to signal through TLR2 (reviewed in (23). Therefore, we also transfected HEK-293 cells with hTLR2 or mTLR2 either alone or in combination with TLR1 or TLR6. The cells were then stimulated with hIL-1 as a positive control (HEK-293 cells express IL-1 receptors), the TLR2 ligand Pam3CSK4, or F. novicida LPS (Fig. 3C and D). Although good induction of the reporter construct was observed for IL-1 and Pam3CSK4, the F. novicida LPS preparation did not demonstrate any activity in this assay.
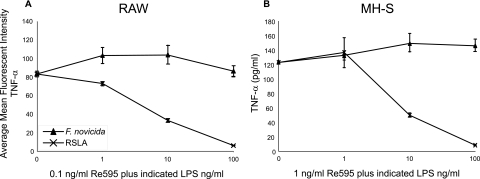
F. novicida LPS is not a TLR4 antagonist.
Since F. novicida LPS did not mediate activation through TLR4, we next determined whether it could act as an antagonist. RSLA, which does not signal via hTLR4 or mTLR4 (Fig. 3A and B) but rather inhibits responses to stimulatory LPS, was used as a positive control of antagonism (Fig. 4). RAW 264.7 or MH-S cells, mouse alveolar macrophages, were stimulated with a constant amount of stimulatory S. minnesota Re595 LPS in the presence of increasing amounts of RSLA or F. novicida LPS. While the response to S. minnesota Re595 LPS was completely inhibited in the presence of 100 ng/ml RSLA in both cell lines, this response was unaffected even in the presence of 100 ng/ml of F. novicida LPS. A similar lack of antagonism by F. novicida LPS was observed in HEK-293 cells transiently transfected with hTLR4 or mTLR4 (data not shown).
FIG. 4.
F. novicida LPS does not inhibit responsiveness to Re595 LPS. RAW cells (A) or MH-S cells (B) were stimulated with S. minnesota Re595 LPS (0.1 ng/ml [A] or 1 ng/ml [B]) alone or in the presence of R. sphaeroides lipid A (1, 10, or 100 ng/ml) or F. novicida LPS (1, 10, or 100 ng/ml). Intracellular TNF-α production after 3 h is shown in panel A, and TNF-α in supernatants after 6 h is shown in panel B. Data are means ± standard deviations (A) or means ± standard errors of the means (B) of results from triplicate wells. Data are representative of two independent experiments.
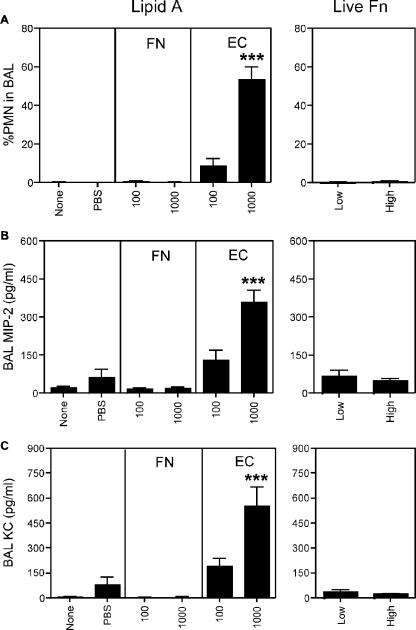
Aerosolized F. novicida LPS does not stimulate TLR4-mediated responses.
To determine whether F. novicida LPS was stimulatory in vivo, we exposed mice to aerosolized F. novicida or E. coli LPS and compared neutrophil (PMN) recruitment and chemokine production in BAL fluid (Fig. 5). E. coli LPS at concentrations of 100 or 1,000 μg/ml induced intrapulmonary secretion of the CXCR2 ligands MIP-2 and KC and stimulated an influx of neutrophils into the bronchoalveolar airspaces by 4 h after aerosol exposure. In contrast, F. novicida LPS did not induce chemokine production or neutrophil recruitment either 4 h after exposure (Fig. 5A to C) or 24 h after exposure (not shown).
FIG. 5.
Aerosolized F. novicida LPS or whole bacteria do not induce lung inflammation. Mice were exposed to aerosols containing F. novicida LPS or E. coli 0111:B4 LPS at concentrations of 100 or 1,000 μg/ml of LPS. Aerosols of live bacteria resulted in bacterial depositions of 52 ± 16 CFU (low, mean ± standard error of the mean) or 3,042 ± 1,048 CFU (high) in the lungs. After 4 h and 24 h, mice underwent bronchoalveolar lavage to enumerate cell counts (% PMN in panel A) and assay MIP-2 (B) and KC (C) by ELISA. Control animals were exposed to aerosolized PBS or were not exposed (none). Data are means ± standard errors of the means (n = 3 to 8 mice). ***, P < 0.001 compared to all other groups.
Aerosolized live F. novicida does not stimulate airway inflammation, consistent with lack of recognition of LPS.
To determine whether whole F. novicida was stimulatory in vivo, we exposed mice to two concentrations of aerosolized F. novicida and measured PMN recruitment and chemokine production in BAL (Fig. 5). As a control for airway immune responses, aerosolization of the gram-negative opportunistic pathogen Pseudomonas aeruginosa resulted in recruitment of large numbers of PMN (>105) and production of significant amounts of cytokines and chemokines by 4 h postinfection (34) (data not shown). In contrast, F. novicida did not induce chemokine, TNF, or IL-10 production or neutrophil recruitment 4 h postexposure (Fig. 5A to C and data not shown).
DISCUSSION
F. tularensis subsp. novicida LPS or lipid A is poorly stimulatory to mammalian cells compared to LPS or lipid A isolated from enteric bacteria. Several properties of F. tularensis subspecies lipid A are uncommon among gram-negative bacteria (27). First, the absence of a phosphate at the 4′ position of lipid A glucosamine backbone dimer likely contributes to the lack of stimulatory activity as demonstrated for monophosphoryl lipid A (3, 29, 43). Monophosphoryl lipid A is a chemically dephosphorylated Salmonella lipid A molecule that is of low endotoxic activity and has recently been used as a vaccine adjuvant (4, 29). Second, highly inflammatory lipid A from enteric bacteria is normally hexa-acylated, containing acyl side chains of 12 to 14 carbons in length, whereas F. tularensis lipid A is tetra-acylated, containing longer acyl side chains of 16 to 18 carbons in length (30, 44), indicating that the length and number of acyl side chains are critical for TLR4-mediated immune responses. Third, F. tularensis LPS or lipid A does not act as an antagonist for either human or mouse TLR4-mediated innate immune responses. As previously shown, the tetra-acylated intermediate in the biosynthetic pathway of lipid A, lipid IVA, and a major component of Yersinia pestis lipid A at 37°C, is an agonist for mouse TLR4 and an antagonist for human cell responses (28, 32, 33). In contrast, RSLA, which is a penta-acylated molecule, stimulates neither human nor mouse TLR4 but, interestingly, acts as an LPS antagonist for both. Therefore, F. novicida LPS does not appear to bind to TLR4 or other components of the LPS receptor complex because it did not antagonize nonsaturating amounts of stimulatory LPS. Recent results from Barker et al. using LPS isolated from F. tularensis subsp. holarctica strain LVS suggests that the lack of recognition of F. tularensis LPS occurs upstream of TLR4/MD-2/CD14 at the level of the LPS-sensing molecules that include LPS-binding protein or bactericidal/permeability-increasing protein (5). This is in contrast to Y. pestis LPS, which antagonizes human TLR4 but is well recognized by mouse TLR4, suggesting that the mouse is a poor model of human Y. pestis infection. Finally, the functional outcome of galactosamine modification of lipid A, previously described as a component of total lipid A preparations from the oral pathogen Selenomonas sputigena is unknown (26).
The results presented here suggest that Francisella lipid A and, thus, LPS are not recognized by TLRs. Using highly purified and well-characterized LPS isolated from F. novicida after growth at 37°C, we found that neither human nor murine monocytic cells responded to LPS. Since most LPS preparations stimulate cells through TLR4, though a small subset signal through TLR2, we also measured responsiveness in a HEK-293-based gain-of-function assay. Only very high, nonphysiologic concentrations of F. novicida LPS (1 μg/ml) induced the ELAM-luciferase reporter in cells transfected with TLR4, and neither LPS preparation mediated activation through TLR2, and this is similar to recently published results using F. tularensis subsp. holarctica strain LVS LPS in primary human (8) or murine (11) monocytes/macrophages using concentrations of LPS at greater than 5 μg/ml to elicit a minimal stimulatory response. In addition, Kieffer et al. demonstrated weak stimulatory activity of high concentrations (>1 μg/ml) of F. novicida LPS on bone-marrow-derived macrophages after 72 h of stimulation, although it is possible that this activity was due to contaminating lipoproteins, as the LPS preparation was not repurified (25). This group also found a protective effect of pretreating mice with LVS LPS followed by lethal challenge 2 to 3 days later with LVS (10). The mechanism of action is unclear, as this LPS, in comparison to E. coli LPS, was found to be inactive for proliferation or cytokine production by purified splenocytes, although B cells were required for this protective effect.
Taken together, these results demonstrate that F. novicida LPS is poorly stimulatory in vitro. Furthermore, inhalation of aerosolized F. novicida LPS failed to induce a pulmonary inflammatory response in mice, confirming its poorly stimulatory activity in vivo. When live F. novicida was aerosolized into mice, no inflammatory response was observed at 4 h, unlike the robust response seen in mice similarly infected with Pseudomonas aeruginosa (35; unpublished observations). No anti-inflammatory cytokines such as IL-10 were measured at 4 h following bacterial infection (data not shown). In addition, F. novicida is not flagellated and, hence, does not express ligands for TLR5, although it expresses lipoproteins that presumably can signal through TLR2. This indicates that the lack of recognition of F. novicida LPS, lipid A, and whole bacteria likely allows the bacterium to evade innate immune recognition, resulting in productive infection after exposure to only a few organisms. Due to the fact that the structure of F. novicida lipid A was identical to virulent human F. tularensis type A/type B clinical isolates, compared to strain LVS lipid A that lacks the 4′ galactosamine modification, it is likely that F. novicida infection in mice will in part mimic human disease, at least in terms of TLR-mediated stimulation. Therefore, it is plausible that the ability of francisellae to cause severe disease in humans is attributable to the ability of the Francisella LPS or lipid A to escape recognition by the host innate immune system. Furthermore, F. novicida infection of mice may provide a unique opportunity to study pathogenic bacteria with poor stimulation of TLR4 in a mouse model of infection.
Acknowledgments
We thank Duangjit Kanistanon for critical review of the manuscript.
Support was provided by grant U54 AI057141 from the NIH to S.I.M., D.R.G., C.B.W., S.J.S., and R.K.E.
Footnotes
▿
Published ahead of print on 18 September 2006.
REFERENCES
- 1.Alexander, C., and E. T. Rietschel. 2001. Bacterial lipopolysaccharides and innate immunity. J. Endotoxin Res. 7**:**167-202. [PubMed] [Google Scholar]
- 2.Arbour, N. C., E. Lorenz, B. C. Schutte, J. Zabner, J. N. Kline, M. Jones, K. Frees, J. L. Watt, and D. A. Schwartz. 2000. TLR4 mutations are associated with endotoxin hyporesponsiveness in humans. Nat. Genet. 25**:**187-191. [DOI] [PubMed] [Google Scholar]
- 3.Baldridge, J. R., and R. T. Crane. 1999. Monophosphoryl lipid A (MPL) formulations for the next generation of vaccines. Methods 19**:**103-107. [DOI] [PubMed] [Google Scholar]
- 4.Baldridge, J. R., P. McGowan, J. T. Evans, C. Cluff, S. Mossman, D. Johnson, and D. Persing. 2004. Taking a Toll on human disease: Toll-like receptor 4 agonists as vaccine adjuvants and monotherapeutic agents. Expert Opin. Biol. Ther. 4**:**1129-1138. [DOI] [PubMed] [Google Scholar]
- 5.Barker, J. H., J. Weiss, M. A. Apicella, and W. M. Nauseef. 2006. Basis for the failure of Francisella tularensis lipopolysaccharide to prime human polymorphonuclear leukocytes. Infect. Immun. 74**:**3277-3284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brandenburg, K., and A. Wiese. 2004. Endotoxins: relationships between structure, function, and activity. Curr. Top. Med. Chem. 4**:**1127-1146. [DOI] [PubMed] [Google Scholar]
- 7.Caroff, M., A. Tacken, and L. Szabo. 1988. Detergent-accelerated hydrolysis of bacterial endotoxins and determination of the anomeric configuration of the glycosyl phosphate present in the “isolated lipid A” fragment of the Bordetella pertussis endotoxin. Carbohydr. Res. 175**:**273-282. [DOI] [PubMed] [Google Scholar]
- 8.Cole, L. E., K. L. Elkins, S. M. Michalek, N. Qureshi, L. J. Eaton, P. Rallabhandi, N. Cuesta, and S. N. Vogel. 2006. Immunologic consequences of Francisella tularensis live vaccine strain infection: role of the innate immune response in infection and immunity. J. Immunol. 176**:**6888-6899. [DOI] [PubMed] [Google Scholar]
- 9.Darveau, R. P., M. D. Cunningham, C. L. Seachord, R. C. Page, and A. Aruffo. 1995. The ability of bacteria associated with chronic inflammatory disease to stimulate E-selectin expression and neutrophil adhesion. Prog. Clin. Biol Res. 392**:**69-78. [PubMed] [Google Scholar]
- 10.Dreisbach, V. C., S. Cowley, and K. L. Elkins. 2000. Purified lipopolysaccharide from Francisella tularensis live vaccine strain (LVS) induces protective immunity against LVS infection that requires B cells and gamma interferon. Infect. Immun. 68**:**1988-1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Duenas, A. I., M. Aceves, A. Orduna, R. Diaz, M. Sanchez Crespo, and C. Garcia-Rodriguez. 2006. Francisella tularensis LPS induces the production of cytokines in human monocytes and signals via Toll-like receptor 4 with much lower potency than E. coli LPS. Int. Immunol. 18**:**785-795. [DOI] [PubMed] [Google Scholar]
- 12.Ellis, J., P. C. Oyston, M. Green, and R. W. Titball. 2002. Tularemia. Clin. Microbiol. Rev. 15**:**631-646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ernst, R. K., T. Guina, and S. I. Miller. 1999. How intracellular bacteria survive: surface modifications that promote resistance to host innate immune responses. J. Infect. Dis. 179(Suppl. 2)**:**S326-S330. [DOI] [PubMed] [Google Scholar]
- 14.Fischer, W., H. U. Koch, and R. Haas. 1983. Improved preparation of lipoteichoic acids. Eur. J. Biochem. 133**:**523-530. [DOI] [PubMed] [Google Scholar]
- 15.Folch, J., M. Lees, and G. H. Sloane Stanley. 1957. A simple method for the isolation and purification of total lipides from animal tissues. J. Biol. Chem. 226**:**497-509. [PubMed] [Google Scholar]
- 16.Forsman, M., G. Sandstrom, and A. Sjostedt. 1994. Analysis of 16S ribosomal DNA sequences of Francisella strains and utilization for determination of the phylogeny of the genus and for identification of strains by PCR. Int. J. Syst. Bacteriol. 44**:**38-46. [DOI] [PubMed] [Google Scholar]
- 17.Golenbock, D. T., R. Y. Hampton, N. Qureshi, K. Takayama, and C. R. Raetz. 1991. Lipid A-like molecules that antagonize the effects of endotoxins on human monocytes. J. Biol. Chem. 266**:**19490-19498. [PubMed] [Google Scholar]
- 18.Guo, L., K. B. Lim, C. M. Poduje, M. Daniel, J. S. Gunn, M. Hackett, and S. I. Miller. 1998. Lipid A acylation and bacterial resistance against vertebrate antimicrobial peptides. Cell 95**:**189-198. [DOI] [PubMed] [Google Scholar]
- 19.Hajjar, A. M., R. K. Ernst, J. H. Tsai, C. B. Wilson, and S. I. Miller. 2002. Human Toll-like receptor 4 recognizes host-specific LPS modifications. Nat. Immunol. 3**:**354-359. [DOI] [PubMed] [Google Scholar]
- 20.Hajjar, A. M., D. S. O'Mahony, A. Ozinsky, D. M. Underhill, A. Aderem, S. J. Klebanoff, and C. B. Wilson. 2001. Cutting edge: functional interactions between toll-like receptor (TLR) 2 and TLR1 or TLR6 in response to phenol-soluble modulin. J. Immunol. 166**:**15-19. [DOI] [PubMed] [Google Scholar]
- 21.Hirschfeld, M., Y. Ma, J. H. Weis, S. N. Vogel, and J. J. Weis. 2000. Cutting edge: repurification of lipopolysaccharide eliminates signaling through both human and murine toll-like receptor 2. J. Immunol. 165**:**618-622. [DOI] [PubMed] [Google Scholar]
- 22.Isherwood, K. E., R. W. Titball, D. H. Davies, P. L. Felgner, and W. J. Morrow. 2005. Vaccination strategies for Francisella tularensis. Adv. Drug Deliv. Rev. 57**:**1403-1414. [DOI] [PubMed] [Google Scholar]
- 23.Ishii, K. J., C. Coban, and S. Akira. 2005. Manifold mechanisms of toll-like receptor-ligand recognition. J. Clin. Immunol. 25**:**511-521. [DOI] [PubMed] [Google Scholar]
- 24.Johansson, A., J. Farlow, P. Larsson, M. Dukerich, E. Chambers, M. Bystrom, J. Fox, M. Chu, M. Forsman, A. Sjostedt, and P. Keim. 2004. Worldwide genetic relationships among Francisella tularensis isolates determined by multiple-locus variable-number tandem repeat analysis. J. Bacteriol. 186**:**5808-5818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kieffer, T. L., S. Cowley, F. E. Nano, and K. L. Elkins. 2003. Francisella novicida LPS has greater immunobiological activity in mice than F. tularensis LPS, and contributes to F. novicida murine pathogenesis. Microbes Infect. 5**:**397-403. [DOI] [PubMed] [Google Scholar]
- 26.Kumada, H., K. Watanabe, A. Nakamu, Y. Haishima, S. Kondo, K. Hisatsune, and T. Umemoto. 1997. Chemical and biological properties of lipopolysaccharide from Selenomonas sputigena ATCC 33150. Oral Microbiol. Immunol. 12**:**162-167. [DOI] [PubMed] [Google Scholar]
- 27.Miller, S. I., R. K. Ernst, and M. W. Bader. 2005. LPS, TLR4 and infectious disease diversity. Nat. Rev. Microbiol. 3**:**36-46. [DOI] [PubMed] [Google Scholar]
- 28.Muroi, M., and K. Tanamoto. 2006. Structural regions of MD-2 that determine the agonist-antagonist activity of lipid IVa. J. Biol. Chem. 281**:**5484-5491. [DOI] [PubMed] [Google Scholar]
- 29.Persing, D. H., R. N. Coler, M. J. Lacy, D. A. Johnson, J. R. Baldridge, R. M. Hershberg, and S. G. Reed. 2002. Taking toll: lipid A mimetics as adjuvants and immunomodulators. Trends Microbiol. 10**:**S32-37. [DOI] [PubMed] [Google Scholar]
- 30.Phillips, N. J., B. Schilling, M. K. McLendon, M. A. Apicella, and B. W. Gibson. 2004. Novel modification of lipid A of Francisella tularensis. Infect. Immun. 72**:**5340-5348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Raetz, C. R., and C. Whitfield. 2002. Lipopolysaccharide endotoxins. Annu. Rev. Biochem. 71**:**635-700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rebeil, R., R. K. Ernst, B. B. Gowen, S. I. Miller, and B. J. Hinnebusch. 2004. Variation in lipid A structure in the pathogenic yersiniae. Mol. Microbiol. 52**:**1363-1373. [DOI] [PubMed] [Google Scholar]
- 33.Saitoh, S., S. Akashi, T. Yamada, N. Tanimura, M. Kobayashi, K. Konno, F. Matsumoto, K. Fukase, S. Kusumoto, Y. Nagai, Y. Kusumoto, A. Kosugi, and K. Miyake. 2004. Lipid A antagonist, lipid IVa, is distinct from lipid A in interaction with Toll-like receptor 4 (TLR4)-MD-2 and ligand-induced TLR4 oligomerization. Int. Immunol. 16**:**961-969. [DOI] [PubMed] [Google Scholar]
- 34.Skerrett, S. J., H. D. Liggitt, A. M. Hajjar, R. K. Ernst, S. I. Miller, and C. B. Wilson. 2004. Respiratory epithelial cells regulate lung inflammation in response to inhaled endotoxin. Am. J. Physiol. Lung Cell. Mol. Physiol. 287**:**L143-L152. [DOI] [PubMed] [Google Scholar]
- 35.Skerrett, S. J., H. D. Liggitt, A. M. Hajjar, and C. B. Wilson. 2004. Cutting edge: myeloid differentiation factor 88 is essential for pulmonary host defense against Pseudomonas aeruginosa but not Staphylococcus aureus. J. Immunol. 172**:**3377-3381. [DOI] [PubMed] [Google Scholar]
- 36.Skerrett, S. J., T. R. Martin, E. Y. Chi, J. J. Peschon, K. M. Mohler, and C. B. Wilson. 1999. Role of the type 1 TNF receptor in lung inflammation after inhalation of endotoxin or Pseudomonas aeruginosa. Am. J. Physiol. 276**:**L715-L727. [DOI] [PubMed] [Google Scholar]
- 37.Somerville, J. E. J., L. Cassiano, B. Bainbridge, M. D. Cunningham, and R. P. Darveau. 1996. A novel Escherichia coli lipid A mutant that produces an antiinflammatory lipopolysaccharide. J. Clin. Investig. 97**:**359-365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Svensson, K., P. Larsson, D. Johansson, M. Bystrom, M. Forsman, and A. Johansson. 2005. Evolution of subspecies of Francisella tularensis. J. Bacteriol. 187**:**3903-3908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Thomas, R., A. Johansson, B. Neeson, K. Isherwood, A. Sjostedt, J. Ellis, and R. W. Titball. 2003. Discrimination of human pathogenic subspecies of Francisella tularensis by using restriction fragment length polymorphism. J. Clin. Microbiol. 41**:**50-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Titball, R. W., A. Johansson, and M. Forsman. 2003. Will the enigma of Francisella tularensis virulence soon be solved? Trends Microbiol. 11**:**118-123. [DOI] [PubMed] [Google Scholar]
- 41.Trent, M. S. 2004. Biosynthesis, transport, and modification of lipid A. Biochem. Cell Biol. 82**:**71-86. [DOI] [PubMed] [Google Scholar]
- 42.Twine, S. M., H. Shen, J. F. Kelly, W. Chen, A. Sjostedt, and J. W. Conlan. 2006. Virulence comparison in mice of distinct isolates of type A Francisella tularensis. Microb. Pathog. 40**:**133-138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ulrich, J. T., and K. R. Myers. 1995. Monophosphoryl lipid A as an adjuvant. Past experiences and new directions. Pharm. Biotechnol. 6**:**495-524. [PubMed] [Google Scholar]
- 44.Vinogradov, E., M. B. Perry, and J. W. Conlan. 2002. Structural analysis of Francisella tularensis lipopolysaccharide. Eur. J. Biochem. 269**:**6112-6118. [DOI] [PubMed] [Google Scholar]
- 45.Westphal, O., and K. Jann. 1965. Bacterial lipopolysaccharides: extraction with phenol-water and further applications of the procedure. Methods Carbohydr. Chem. 5**:**83-91. [Google Scholar]
- 46.Yi, E. C., and M. Hackett. 2000. Rapid isolation method for lipopolysaccharide and lipid A from gram-negative bacteria. Analyst 125**:**651-656. [DOI] [PubMed] [Google Scholar]