Monoclonal antibody-mediated enhancement of dengue virus infection in vitro and in vivo and strategies for prevention (original) (raw)
Abstract
Infection with dengue virus (DENV) or any other flavivirus induces cross-reactive, but weakly neutralizing or nonneutralizing, antibodies that recognize epitopes involving the fusion peptide in the envelope glycoprotein. Humanized mAb IgG 1A5, derived from a chimpanzee, shares properties of cross-reactive antibodies. mAb IgG 1A5 up-regulated DENV infection by a mechanism of antibody-dependent enhancement (ADE) in a variety of Fc receptor-bearing cells in vitro. A 10- to 1,000-fold increase of viral yield in K562 cells, dependent on the DENV serotype, was observed over a range of subneutralizing concentrations of IgG 1A5. A significant increase of DENV-4 viremia titers (up to 100-fold) was also demonstrated in juvenile rhesus monkeys immunized with passively transferred dilutions of IgG 1A5. These results, together with earlier findings of ADE of DENV-2 infection by a polyclonal serum, establish the primate model for analysis of ADE. Considering the abundance of these cross-reactive antibodies, our observations confirm that significant viral amplification could occur during DENV infections in humans with prior infection or with maternally transferred immunity, possibly leading to severe dengue. Strategies to eliminate ADE were explored by altering the antibody Fc structures responsible for binding to Fc receptors. IgG 1A5 variants, containing amino acid substitutions from the Fc region of IgG2 or IgG4 antibodies, reduced but did not eliminate DENV-4-enhancing activity in K562 cells. Importantly, a 9-aa deletion at the N terminus of the CH2 domain in the Fc region abrogated the enhancing activity.
Keywords: antibody-dependent enhancement, nonhuman primate model, Fc mutations, cross-reactive mAb
The four dengue virus (DENV) serotypes (DENV-1 to DENV-4) are the most important arthropod-borne flaviviruses in terms of morbidity and geographic distribution. Up to 100 million DENV infections occur every year, mostly in tropical and subtropical areas where vector mosquitoes are abundant (1). Infection with any of the DENV serotypes may be asymptomatic or may lead to classic dengue fever or more severe dengue hemorrhagic fever (DHF) and dengue shock syndrome (DSS), which are increasingly common in the dengue endemic areas. Immunity to the same virus serotype (homotypic immunity) is life-long, whereas immunity to different serotypes (heterotypic immunity) lasts 2–3 months so that infection with a different serotype virus is possible (2). DHF/DSS often occurs in patients with second, heterotypic DENV infections or in infants with maternally transferred dengue immunity (3, 4). Severe dengue is a major cause of hospitalization, and fatality rates vary from <1% to 5% in children.
Antibody-dependent enhancement (ADE) has been proposed as an underlying pathogenic mechanism of DHF/DSS (3). ADE occurs because preexisting subneutralizing antibodies and the infecting DENV form complexes that bind to Fc receptor-bearing cells, leading to increased virus uptake and replication (4). ADE has been repeatedly demonstrated in vitro using dengue immune sera or monoclonal antibodies and cells of monocytic and recently, B lymphocytic lineages bearing Fc receptors (5–7). ADE of DENV-2 infection has also been demonstrated in monkeys infused with a human dengue immune serum (8).
Infection with DENV or any other flavivirus induces broadly cross-reactive but weak or nonneutralizing antibodies (9, 10). These antibodies remain detectable for a long period and rise rapidly during a subsequent heterotypic infection as a result of an anamnestic response. A major subset of these cross-reactive antibodies is directed to immuno-dominant epitopes involving determinants mapped to the flavivirus-conserved fusion peptide in the envelope glycoprotein (E) (11–13). The functional activities of these cross-reactive antibodies are not well characterized.
We have identified chimpanzee–human chimeric IgG1 mAbs capable of neutralizing or binding to one or more DENV serotypes (14, 15). Cross-reactive IgG 1A5 neutralizes DENV-1 and DENV-2 more efficiently than DENV-3 and DENV-4, and type-specific IgG 5H2 neutralizes DENV-4 at a high titer (14, 15). Analysis of antigenic variants has localized the IgG 1A5 binding site to the conserved fusion peptide in E (11). Thus, IgG 1A5 shares many characteristics with the cross-reactive antibodies detected in flavivirus infections.
We investigated the ability of IgG 1A5 to mediate enhancement of DENV replication in monocyte-derived cell lines and in juvenile rhesus monkeys after passive transfer. We also explored strategies to reduce ADE by mutational analysis of the key structures in the Fc of IgG 1A5. A 9-aa deletion at the N terminus of Fc was identified as responsible for complete abrogation of DENV ADE in vitro. These findings have implications for DENV pathogenesis as well as for antibody-mediated prevention of dengue.
Results
ADE of DENV Infection Mediated by IgG 1A5 in K562 Cells.
The multiplicity of infection (MOI) of each DENV for K562 cells was adjusted to produce a viral yield of ≈3 log10 focus-forming units (FFU)/ml 4 days after infection in the absence of added antibody. DENV-2 required an MOI of 0.05, whereas DENV-1 and DENV-4 required an MOI of 0.10 and DENV-3 required an MOI of 0.15 for such an infection. The viral yield from DENV infection in the presence of a DENV-negative human IgG1 was the same as for the control. To analyze the ADE of DENV infection in K562 cells, each DENV was preincubated with dilutions of IgG 1A5 (10−3 to 104 μg/ml) to form immune complexes before infecting K562 cells. Neutralization of DENV infection at high IgG 1A5 concentrations and a breakthrough at lower concentrations occurred. Further dilutions of IgG 1A5 led to an increase of viral yields, consistent with the ADE phenomenon (Fig. 1A). The maximum viral yield above baseline was ≈10-fold for DENV-1 and DENV-2, 54-fold for DENV-3, and 1,000-fold for DENV-4. The antibody concentration that mediated the maximum increase was ≈0.5 μg/ml for DENV-1 and DENV-2 and 5 μg/ml for DENV-3 and DENV-4, similar to the 50% plaque reduction neutralization test (PRNT50) titer against that DENV serotype (14).
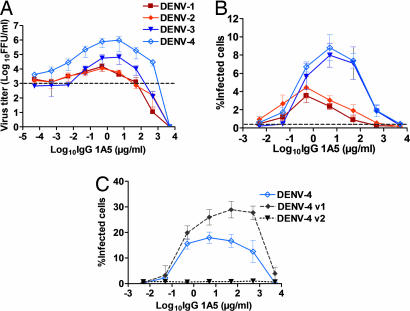
Fig. 1.
ADE of DENV replication in K562 cells mediated by various concentrations of IgG 1A5. (A) Increase of the viral yields (FFU/ml) of each DENV serotype. The baseline viral yield (dashed line) was ≈1,000 FFU/ml with a DENV sero-negative human IgG1 as control. (B) The percent of cells infected with DENV detected by flow cytometry. (C) The percent of cells infected with 1 MOI of DENV-4 or antigenic variant detected by flow cytometry. Variant DENV-4 v1 contains substitution Leu107Phe and variant DENV-4 v2 contains substitution Gly106Val in E.
The IgG 1A5-dependent enhancement of DENV infection was also analyzed by flow cytometry. Each DENV produced a ≈0.5% cell infection rate with DENV-negative human IgG1 2 days after incubation. In the presence of IgG 1A5, infected cells were increased up to 4.5% for DENV-1 and DENV-2 and up to 11.5% for DENV-3 and DENV-4 (Fig. 1B). The optimum antibody concentration for the enhancement of DENV infection was similar to that observed by focus assay.
The difference in ADE activities among the different DENV serotypes was probably due to sequence variations in the antibody-binding sites. This possibility was explored by ADE analysis using DENV-4 antigenic variants containing Gly106Val or Leu107Phe substitution in E, which reduced their antibody-binding affinity (11). Infection of K562 cells with IgG 1A5-low-binding DENV-4 Gly106Val [DENV-4 variant (v)2] was not enhanced by the antibody. In contrast, IgG 1A5 enhanced infection of IgG 1A5-moderate-binding DENV-4 Leu107Phe (DENV-4 v1) variant in K562 cells to 28.9 ± 3.2%, compared with parental DENV-4 (18.0 ± 2.2%) (Fig. 1C). The optimum IgG 1A5 concentration for infection was 50 μg/ml, similar to the PRNT50 titer of the variant.
IgG 1A5-Mediated Enhancement of DENV-4 Infection in Other Fc Receptor-Bearing Cells and in Rhesus Monkey Primary Monocytes.
We determined whether other Fc receptor-bearing cells would also support IgG 1A5-mediated enhancement of DENV-4 replication. At a MOI of 1 and in the absence of antibody, flow cytometry detected 5.3 ± 2.7% infection in U937 cells and 0.35 ± 0.03% in Raji-1 cells. A consistent increase of DENV-4 infection, up to 31.5 ± 2.3% in U937 cells and 45.2 ± 1.0% in Raji-1 cells, was detected when the virus was mixed with the antibody at various concentrations (Fig. 2A). IgG 1A5 failed to mediate enhancement of DENV-4 infection in Raji-1 (DC-SIGN) cells expressing DC-SIGN, which has been shown to facilitate DENV infection by a mechanism different from ADE (16) (Fig. 2B).
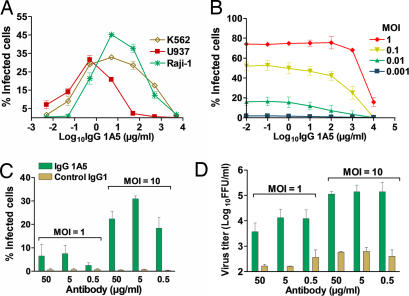
Fig. 2.
ADE of DENV-4 infection in other Fc receptor-bearing cells mediated by IgG 1A5. (A) ADE in U937 and Raji-1 cells infected with 1 MOI, detected by flow cytometry. (B) ADE in dendritic cell-specific intercellular adhesion molecule 3-grabbing nonintegrin (DC-SIGN)-expressing Raji-1 cells, detected by flow cytometry. (C) ADE in monkey primary monocytes, detected by flow cytometry. (D) Same as in C but detected by the viral yield.
IgG 1A5-mediated enhancement of DENV-4 infection in primary monocytes from juvenile rhesus monkeys was also analyzed. At a MOI of 1 or 10 and in the presence of dengue-negative human serum, <1% of the monocytes were infected with DENV-4. The number of infected cells detected by flow cytometry reached 31 ± 1.2%, when IgG 1A5 was added at 5 μg/ml (Fig. 2C). A 1,000-fold enhancement of DENV-4 replication was detected with 0.5, 5, and 50 μg/ml of IgG 1A5 when analyzed by focus assay (Fig. 2D).
Enhancement of DENV-4 Infection Mediated by IgG 1A5 in Juvenile Rhesus Monkeys.
The experiment included 18 monkeys in groups of three: five groups to receive IgG 1A5 antibody intravenously at various concentrations and the sixth group to receive PBS diluent as a control. The serum IgG 1A5 concentrations 24 h after infusion (before DENV-4 challenge) were confirmed by ELISA and by PRNT (supporting information (SI) Table 2). Fig. 3A shows the result of average DENV-4 viremia titers from days 2–10 for each group of monkeys. The viremia titers on these days were not significantly different between the monkey group that received 18 mg/kg of IgG 1A5 and the monkey group that received PBS. By comparison, a significant difference in the viremia titer in all monkey groups was observed for days 3–6 after challenge (P < 0.05; Kruskal–Wallis test). Based on the analysis of these four days, quantitative PCR detected a mean peak viremia titer of 0.76 log10 FFU/ml in the control group. The mean viremia titer increased from 0.58 to 2.76 log10 FFU/ml in the groups, as antibody concentration decreased from 18 to 0.22 mg/kg (Table 1). The viremia titer increased ≈15- and ≈8-fold in the monkey groups that received 6 and 2 mg/kg IgG 1A5, respectively, compared with that observed in the control group (P < 0.05; Mann–Whitney U test). The monkey groups administered 0.67 and 0.22 mg/kg IgG 1A5 had nearly ≈56- and ≈100-fold increases in viral titers, respectively, a highly significant increase compared with that observed in the control group (P < 0.001; Mann–Whitney U test).
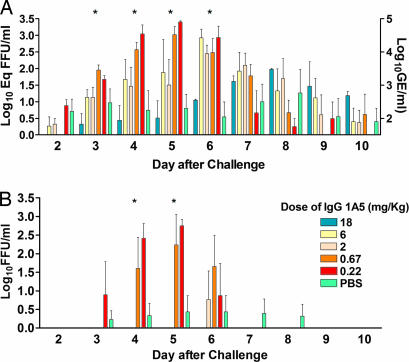
Fig. 3.
ADE of DENV-4 infection in juvenile rhesus monkeys passively administered with IgG 1A5. (A) Viremia titer in monkeys, detected by quantitative PCR. The results are expressed in genome equivalent (GE) and equivalent (Eq) FFU per milliliter. The viremia titers on days 3–6 (indicated by asterisks) for the monkey groups receiving 6, 2.0, 0.67, and 0.22 mg/kg IgG 1A5 were significantly different from that of the control group that received PBS. (B) Same as in A, except that the viremia titer was determined by a direct FFU assay. The variation bars indicate the titer differences (standard error) among monkeys in each group.
Table 1.
Peak viremia titers in serum of monkeys passively transferred with IgG 1A5 then infected with DENV-4
| Monkey group dose of IgG 1A5, mg/kg | Geometric mean peak viremia titer (log10FFU per milliliter ± SE) determined by | |
|---|---|---|
| Quantitative PCR* | Focus assay† | |
| 18 | 0.58 ± 0.16 | ≤0.60 |
| 6 | 1.92 ± 0.37‡ | ≤0.60 |
| 2 | 1.64 ± 0.28‡ | ≤0.60 |
| 0.67 | 2.51 ± 0.22§ | 1.92 ± 0.31‡ |
| 0.22 | 2.76 ± 0.38§ | 2.58 ± 0.16‡ |
| Control (PBS) | 0.76 ± 0.10 | 0.40 ± 0.05 |
The viremia titers of infected monkeys were also determined by FFU assay. Viremia was detected on days 3–8 after challenge in the control group but not in the monkey groups that received 18 and 6 mg/kg of IgG 1A5 (Fig. 3B). Compared with the mean viremia titer in the control group (0.40 log10 FFU/ml), a significant difference in the viremia titer was observed across the monkey groups that received lower IgG 1A5 concentrations on days 4 and 5 (P < 0.05; Kruskal–Wallis test). The mean viremia titer in the monkey groups that received 0.67 and 0.22 mg/kg of antibody increased ≈36- and ≈165-fold, respectively (P < 0.05; Mann–Whitney U test) (Table 1).
The time of peak viremia was delayed 2–3 days in the monkey group that received the highest dose of IgG 1A5 compared with the monkey groups that received lower doses of antibody or PBS. The high antibody concentration might have reduced DENV-4 replication and selected for escape variants in these monkeys. The latter possibility was ruled out by sequencing the E-specific DNA amplified from viremic samples on days 7, 8, and 9 after challenge, because no mutation was found in the sequence. DENV-4 infection in monkeys was also confirmed by sero-analysis 6 weeks after challenge. Semiquantitative analysis by radio-immunoprecipitation revealed that the levels of anti-NS1 antibody, an indirect measure of the extent of DENV replication, were significantly higher in the monkey groups that received antibody, except for the group that received 18 mg/kg, compared with that of the control group (P = 0.049) (data not shown). Thus, analysis of anti-NS1 antibodies also supported IgG 1A5-mediated enhancement of DENV-4 replication in the primates.
Mutations in the Fc Region of IgG 1A5 Reduce or Eliminate ADE of DENV-4 Infection.
We first sought to replace sequences in the Fc region of IgG 1A5 with the analogous sequences of IgG2 or IgG4 subclass, which have reduced Fcγ receptor-binding affinity (17). Three variants were constructed: (i) IgG 1A5 ΔA contained replacement amino acids at 327, 330, and 331 in the Fc of IgG4; (ii) IgG 1A5 ΔB contained replacement amino acids at 233–236 in the Fc of IgG2; and (iii) IgG 1A5 ΔC contained replacements of both variants ΔA and ΔB (Fig. 4A). Enhancement of DENV-4 infection in K562 cells mediated by each of these antibody variants was analyzed by flow cytometry. Compared with the enhancing activity of parental IgG 1A5 (43.3 ± 3.6% of cells infected), the enhancing activity of variant IgG 1A5 ΔA was 37.6 ± 3.5%, variant IgG 1A5 ΔB was 24.0 ± 1.8%, and variant IgG 1A5 ΔC was 18.8 ± 2.1% of cells infected. Thus, these Fc variants of IgG 1A5 diminished the DENV-4 enhancing activity of IgG 1A5 by up to 2.3-fold but did not eliminate it (Fig. 5A).
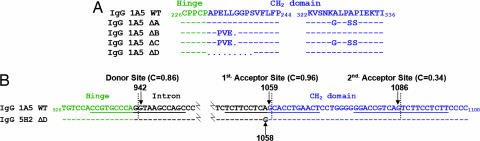
Fig. 4.
Sequence alterations and generation of a 9-aa deletion in the Fc region. (A) IgG 1A5 variants containing sequence alterations in the Fc that affect Fc receptor binding. The regions at positions 233–236 and at positions 327–331 are known to contribute to Fc receptor binding. The N terminus of CH2 is located at position 231 according to the numbering system used. The substitution sequences in ΔA, ΔB, and ΔC and the deletion sequence (represented by dots in ΔD) of the IgG 1A5 constructs are shown. (B) Altered splicing of mRNA to generate a 9-aa deletion in the Fc of IgG 5H2 ΔD. The illustration depicts a probable mechanism by which substitution of A1058G in IgG 5H2 ΔD renders the normal acceptor splice site at 1059 defective. Alternate splicing occurs at nucleotide position 1086 to generate the 9-aa deletion. C is the confidence value based on the sequence (underlined) for splicing to take place according to the NetGene 2 program (18).
Fig. 5.
ADE of DENV-4 infection at 1 MOI in K562 cells mediated by IgG 1A5 Fc variants. (A) IgG 1A5 variants containing sequence substitutions of subclass IgG2 or IgG4 in the Fc. (B) ADE activity of IgG 1A5 abrogated by the 9-aa deletion (ΔD) in the Fc region originally identified in IgG 5H2 ΔD. Dengue-negative human serum was used as control.
We also compared the enhancing activity of DENV cross-reactive IgG 1A5 with that of DENV-4-specific IgG 5H2. IgG 5H2 had no detectable enhancing activity of DENV-4 infection in K562 cells and other monocyte lines (data not shown). IgG 5H2 also did not appear to enhance DENV-4 replication in transfected CV-1 cells expressing Fcγ RI (CD64+) (Schlesinger and C.-J.L., unpublished observations). These observations prompted us to sequence mRNA from transformed CHO cells expressing IgG 5H2. Surprisingly, the coding sequence showed a deletion of 9 aa (positions 231–239) at the N terminus of the CH2 domain in the Fc region. Sequence analysis of the plasmid construct also revealed an A1058G substitution within the intron preceding the acceptor splice site (Fig. 4B). The substitution was not present in the original plasmid vector nor in other IgG expression plasmids derived from it. The fortuitously introduced mutation rendered the splice site defective and, instead, an alternative splice site was used to generate new mRNA of IgG 5H2 heavy chain with the 9-aa deletion (designated ΔD), as predicted according to the NetGene2 program (18).
To explore the mechanism of altered mRNA splicing, we introduced the A1058G mutation into the IgG 1A5-expressing plasmid. Analysis of mRNA from transfected cells confirmed the predicted 9-aa deletion in IgG 1A5 ΔD (Fig. 4A). The level of IgG 1A5 ΔD expression was low compared with that of IgG 1A5 (data not shown). To increase antibody production, another variant of IgG 1A5 ΔD was constructed by deleting the entire 27 nucleotides coding for amino acids 231–239 in the CH2 domain, maintaining the normal splice junction (Fig. 4B). IgG 1A5 ΔD did not mediate detectable enhancement of DENV-4 infection in K562 cells (Fig. 5B). Conversely, full-length IgG 5H2 was produced by restoring the wild-type sequence in the expression plasmid, and the product was shown to mediate enhancement of DENV-4 infection in K562 cells (Fig. 5B). Thus, the 9-aa deletion in the Fc CH2 region is responsible for abrogating ADE of DENV replication.
Discussion
We found that cross-reactive IgG 1A5 up-regulated DENV infection in monocyte-derived cells in vitro and that ADE activity varied widely among DENV serotypes, possibly reflecting amino acid variations in antibody binding site. This possibility was explored with DENV-4 antigenic variants of IgG 1A5 (11). A higher level of enhancement was detected in infection with DENV-4 v1 containing Leu107Phe substitution compared with the parental DENV-4. This mutation moderately reduced the IgG 1A5-binding affinity (≈10-fold), but there were sufficient immune complexes to facilitate infection of Fc receptor-bearing cells. The IgG 1A5-mediated enhancement was not observed with variant DENV-4 v2 containing Gly106Val substitution, which has a low binding affinity for the antibody (11). If the mutation in the flavivirus-conserved sequence proves to be a major determinant of an ADE epitope, such a DENV-4 variant can be explored to address vaccine safety related to ADE.
There is heterogeneity of Fc receptors on different human cell lines (19). ADE of DENV infection has been detected with K562 cells, which express only the Fcγ RII receptor and U937 cells which express Fcγ RI and Fcγ RII receptors (5). Fcγ RIIA has been shown to be more effective than Fcγ RI in mediating enhancement of immune complex infectivity (20). A comparable level of DENV-4 replication enhancement was detected among K562, U937, and Raji-1 cells. The ADE activity was not demonstrable in Raji-1 (DC-SIGN) cells expressing DC-SIGN, which is a DENV receptor found on dendritic cells (16). Thus, DENV infection of dendritic cells probably does not require an antibody for enhancement.
There have been attempts to demonstrate ADE of DENV infection in primates by sequential infection with different serotypes (21). Monkeys had significantly higher titers and longer duration of viremia in heterotypic infections with DENV-2 than in primary infections with the same virus. Contradictory results were also obtained, because lower viremia titers were consistently detected in heterotypic infections with DENV-1, -3, or -4 than in primary infections with the same virus. ADE of DENV-2 replication in monkeys was also studied by passive antibody transfer, in which monkeys infused with human dengue immune serum were found to develop viremia titers up to 50-fold higher than control monkeys (8). However, a similar study to demonstrate ADE with a monoclonal or polyclonal antibody in monkeys infected with other DENV serotypes has not been reported in the 28 years since that study.
The DENV infection-enhancing activity of IgG 1A5 in vitro was reproducibly demonstrated in juvenile monkeys. Compared with the earlier ADE study in monkeys infected with DENV-2 at a dose of 1,000 and 10,000 PFU after passive transfer with a dilution of human dengue immune serum (8), monkeys in the current study were passively transferred with a range of subneutralizing IgG 1A5 dilutions and infected with 10 FFU (100 monkey infectious dose50) of DENV-4. We detected infection enhancement of up to 100-fold in viremia titer, compared with the 50-fold increase in viremia titer described in the earlier study. It is significant that ADE was detected with a different DENV serotype and a considerable range of antibody concentrations. Further, the peak viremia titers were detected on days 5–6 in both studies. It is probably also significant that peak viremia was detected around the time when a patient's illness may progress to DHF.
In previous sequential DENV infections, only one in 118 monkeys appeared to have developed dengue illness that was possibly due to ADE (21). It was not surprising that monkeys in the current study, while experiencing ADE of DENV replication, did not become ill. Prospective studies in humans have suggested a correlation between higher viremia titers than attained by rhesus monkeys and increased risk of severe dengue in second, heterotypic DENV infections (22, 23). This conclusion, however, has not been completely supported in view of recent studies showing that the infection-enhancing activity detected with preillness sera in vitro did not correlate with increased viremia titers and disease severity in subsequent infection with DENV-2 or DENV-3 (22, 24). Differences in DENV serotype or even strain might be a factor in ADE and dengue severity (22, 23).
It is possible that dengue and its severe DHF/DSS may be a pathogenic course unique to humans. The rapid course in the development of DHF or DSS and its reversible nature, if properly managed, would suggest immunopathogenic elements involving cytokines and other vascular permeability mediators (25). In addition to increased viral replication attributed to ADE, interactions between the immune complex and Fc receptor might also trigger an array of effector cell functions, each with its distinct signaling pathway (26). Others have presented a hypothesis linking severe DHF/DSS and cytotoxic T lymphocytes involved in the clearance of DENV-infected monocytes (25). According to this model, activated effector cells lyse target monocytes to produce cytokines and other mediators, leading to increased vascular permeability and plasma leakage.
ADE has also been attributed to the increased virulence, known as early death, in mice passively administered certain monoclonal antibodies followed by infections with other flaviviruses, such as Japanese encephalitis virus (27) and yellow fever virus (28). Similarly, feline infectious peritonitis virus (FIPV), a coronavirus, causes often fatal infectious peritonitis in cats. ADE of FIPV infection has been shown to be Fc receptor-mediated by neutralizing monoclonal antibodies in vitro (29). Clinically significant HIV infection may also involve ADE through binding of its immune complex to Fc receptor or to complement component C1, which in turn reacts with C1q receptor on the cell surface (30). Increased uptake of immune complexes and virus infection in C1q-bearing cells, including monocytes/macrophages and epithelial cells, may also account for the rapid fatality of Ebola virus infection (31).
Significantly, we have identified a 9-aa deletion near one of the key structures in humanized antibody IgG 5H2 that completely abrogated the enhancing activity. The deletion did not alter the antibody neutralizing activity in vitro (data not shown). The deletion was generated as a result of altered mRNA splicing by a fortuitously introduced A1058G substitution in the antibody-expressing plasmid. The alternative splicing has been verified by plasmid construction and analysis of variant antibodies. This finding has important implications for the design and construction of antibodies for clinical applications. Alterations of the sequence in the Fc region affecting Fcγ receptor binding would be expected to affect other effector cell functions, such as antibody-dependent cellular cytotoxicity, and complement pathways, which play a role in viral clearance and which bridge innate and adaptive immune responses. Evidence suggests that antibodies reactive to the nonstructural protein NS1 of DENV and other flaviviruses can protect against infection through complement-dependent cytotoxicity (32). Contributions of the E-specific antibodies to host defense through the complement pathway are less clear. Recent genetic evidence indicates that a humanized monoclonal antibody against West Nile virus (WNV) and its Fc variants were protective against WNV infection in complement C1q- or Fcγ receptor-deficient mice (33). One interpretation is that the neutralizing activity of antibody plays a far more important role than the antibody-mediated effector functions.
Materials and Methods
Cultured Cells.
Simian Vero cells and mosquito C6/36 cells were grown in MEM. Human erythroleukaemic K562 cells were grown in Iscove's modified Dulbecco's medium, myelomonocytic U937, Raji-1 (a B cell line), and its derived Raji-1 (DC-SIGN) cells were grown in Advanced RPMI medium 1640, and 293 T cells were cultured in DMEM. All media were supplemented with 10% FBS, 0.05 mg/ml gentamycin, and 2.5 units/ml fungizone. Mammalian cells were propagated at 37°C, and C6/36 cells were propagated at 32°C. Media were purchased from Invitrogen (Carlsbad, CA), and cells were from American Type Culture Collection (Manassas, VA) except for cell lines Raji-1 and Raji-1 (DC-SIGN), which were supplied by D. Littman (New York University School of Medicine, New York, NY).
Primary Monocytes.
Mononuclear cells were separated from whole blood of rhesus monkeys by Ficoll/Hypaque gradient centrifugation, washed, and resuspended in PBS plus EDTA and 0.5% BSA. Monocytes were magnetically labeled with CD14 MicroBeads nonhuman primate (MACS) and retained in a magnetized column. After washing, CD14+ cells were eluted and resuspended in Advanced RPMI medium 1640 plus supplements at 105 cells per ml and then plated in a 24-well plate. After incubation for 2 h at 37°C, nonadherent cells were removed by washing with PBS, and the cell monolayers were infected with DENV. The CD14+ monocytes were 85–90% pure, as confirmed by immunostaining with FITC-conjugated anti-CD14 (Miltenyi Biotec, Auburn, CA).
DENV Stocks.
All four DENV serotypes were used in this study: DENV-1 (Hawaii prototype); DENV-2 (New Guinea B); DENV-3 (H87); and DENV-4 (H241 and 814669). Each virus stock was prepared from infected C6/36 cells grown in VP-SFM medium (Invitrogen). After removal of cell debris by centrifugation, the supernatant was stored at −80°C, after which the viral titer was determined.
Analysis of ADE In Vitro.
The MOI for each DENV was adjusted to produce a baseline level of ≈3 log10 FFU/ml in the supernatant of K562 cells 4 days after infection. For flow cytometry, cells were infected with DENV in the presence of various concentrations of test antibody or DENV sero-negative human IgG as a control essentially as described (34). Briefly, ≈4 × 105 cells were suspended in 100 μl of maintenance medium (Iscove's medium for K562 cells or Advanced RPMI medium 1640 for other cells, all supplemented with 2% FBS). Equal aliquots (50 μl) of serially diluted antibody or sero-negative IgG and the DENV inoculum were mixed. After 1 h incubation at 37°C under 5% CO2, the virus–antibody mixture was added to monocytes and incubated for an additional 1.5 h. The infected monocytes were rinsed with maintenance medium and centrifuged. Fresh maintenance medium was added, and the cells were transferred to a 24-well plate. After a 4-day incubation, the virus in the medium was titered by focus assay. For flow cytometry, the increase of DENV-infected cells was determined 1 or 2 days after infection.
Flow Cytometry.
DENV-infected cells were transferred to an Eppendorf (Westbury, NY) tube and centrifuged to remove the supernatant. Fixation, permeabilization, and intracellular fluorescence labeling were performed essentially as described (34). For labeling, cells were incubated with dengue complex-reactive monoclonal antibody MAB8705 (Chemicon, Temecula, CA) and then labeled with anti-mouse immunoglobulins/FITC (DakoCytomation, Glostrup, Denmark). Cells were resuspended in Dulbecco's PBS plus 0.2% BSA and subjected to flow cytometry analysis by using a Becton Dickinson (Mountain View, CA) FACScan instrument. Data were analyzed by using flowjo software (Tree Star, Ashland, OR).
ADE of DENV Infection in Rhesus Monkeys.
Five groups of three monkeys each were infused intravenously with IgG 1A5 at doses of 18, 6, 2, 0.67, and 0.22 mg/kg in PBS, and another group of three monkeys received PBS only. One day later, the concentration of IgG 1A5 in monkey sera was determined by ELISA (15). The PRNT was performed to determine the serum IgG 1A5 PRNT50 titer. All monkeys were challenged with 100 monkey infectious dose50 (equivalent to 10 FFU) of DENV-4 in 0.5 ml by the s.c. route. DENV-4 strain 814669 propagated in Vero cells was used. Serum samples from each monkey were collected daily for the next 10 days and again at 2, 4, 6, and 8 weeks for analysis of viremia and antibody.
Quantitative Analysis of DENV-4 Viremia and Sero-Response in Monkeys.
For assay of FFU, serial dilutions of serum samples in MEM plus 0.05% BSA were added to Vero cell monolayers in 24-well plates and incubated for 1 h at 37°C. A medium overlay containing 10% gum tragacanth (Sigma, St. Louis, MO) was added, and infected cells were incubated at 37°C for 3 days. The detection limit was 0.7 log10 FFU/ml. The DENV-4 titer in monkey sera was also determined by real-time, quantitative RT-PCR. DENV-4 M-specific primer pairs were 843CTCTTGGCAGGATTTATGGCTTA865 and 906CAAAGAAGACAGTTCGCTGGATT883. The probe was 867ATGATTGGGCAAACAG882 labeled with 6-carboxyfluorescein at the 5′ end and a minor groove binder plus nonfluorescent quencher at the 3′ end. Viral RNA was isolated from 100 μl of serum with the QIAmp Viral RNA Mini kit (Qiagen, Valencia, CA). RT-PCR was performed by using the TaqMan One-Step RT-PCR kit (Applied Biosystems, Foster City, CA) in an ABI PRISM 7900HT Sequence Detection System. DENV-4 strain 814669 was used to generate a standard curve with 10-fold dilutions of RNA isolated from a known amount of virus (6.3 log10 FFU/ml), covering a 5 log10 dynamic range (6.3 log10 to 1.3 log10 FFU/ml). The amount of infectious RNA transcripts per reaction corresponded to the known FFU per reaction and is expressed as equivalent FFU (Eq FFU). The detection limit was 0.8 log10 Eq FFU/ml. DENV-4 cDNA concentration curves were also generated, and the conversion factor was ≈0.034 Eq FFU per copy. Radio-immunoprecipitation was used to semiquantify the anti-NS1 antibodies present in monkey sera 2, 4, and 6 weeks after challenge as an independent measurement of DENV-4 infection as described (15).
Construction of IgG 1A5 Fc Variants.
Mutations in the Fc region of IgG 1A5 were generated in the pFab CMV expression vector by overlap extension PCR (15). Briefly, substitutions of C1348 → G, G1356 → T, and C1359 → T according to the numbering system of ref. 35 were introduced by using the Bsa I site at position 1334 near the C terminus of CH2 of IgG 1A5 to generate IgG 1A5 ΔA containing amino acid substitutions at 327, 330, and 331 according to the numbering system of ref. 17. Variant IgG 1A5 ΔB containing the substitution of amino acids 233–236 was created by replacing ACCGGTCGC for TGAACTCCTGGG1075 (to generate three amino acid substitutions and a deletion near the N terminus of CH2). These replacements generated an AgeI (ACCGGT) site for mutant construction. Variant IgG 1A5 ΔC was generated by combining ΔA and ΔB substitutions described above by replacement of the SacII-BsrGI fragment. To generate IgG 1A5 ΔD, containing the 9-aa deletion, two DraIII sites at positions 1053 and 1080 were first introduced to remove the intervening 27 nucleotides, and then the original splice site sequence was restored with a QuikChange Site-Directed Mutagenesis kit (Stratagene, La Jolla, CA).
Sequence Analysis of mRNA.
Total RNA was isolated from transfected 293 T cells or transformed CHO cells by using TRIzol Reagent (Invitrogen). First-strand cDNA was synthesized with the SuperScript II RT kit (Invitrogen) and the anti-sense primer 1806TTTACCCGGAGACAGGGAGAGG1785 at the 3′ end of the IgG CH3 domain. For sequencing, the DNA fragment covering the CH1, hinge, CH2, and CH3 domains of IgG was amplified using appropriate primers and Ampli-_Taq_DNA polymerase (Perkin-Elmer, Waltham, MA). Sequence assembly and analysis were performed by using Sequencher version 4.5 (Gene Codes Corporation, Ann Arbor, MI).
Expression and Purification of IgGs.
IgG 1A5 and IgG 5H2 ΔD were prepared from transformed CHO cells by a large-scale production method (14, 15) (Kemp Biotechnology, Gaithersburg, MD). Plasmids of parental or variant IgGs were also prepared by transient transfection of 293 T cells, and the products were affinity-purified on a protein A column (Kemp Biotechnology).
Supplementary Material
Supporting Table
Acknowledgments
We thank the Bioqual staff for help with animal procedures, Anjeanette Roberts for help in statistical analysis, and Ruhe Men for help with radio-immunoprecipitation. This work was supported by the Intramural Research Program of the National Institute of Allergy and Infectious Diseases, National Institutes of Health.
Abbreviations
DENV
dengue virus
ADE
antibody-dependent enhancement
E
envelope protein
DHF
dengue hemorrhagic fever
DSS
dengue shock syndrome
MOI
multiplicity of infection
FFU
focus forming units
v1, -2
variants 1 and 2
PRNT
plaque reduction neutralization test.
Footnotes
The authors declare no conflict of interest.
References
- 1.Monath TP. Proc Natl Acad Sci USA. 1994;91:2395–2400. doi: 10.1073/pnas.91.7.2395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sabin AB. Am J Trop Med Hyg. 1952;1:30–50. doi: 10.4269/ajtmh.1952.1.30. [DOI] [PubMed] [Google Scholar]
- 3.Halstead SB. Yale J Biol Med. 1970;42:350–362. [PMC free article] [PubMed] [Google Scholar]
- 4.Kliks SC, Nimmanitya S, Nisalak A, Burke DS. Am J Trop Med Hyg. 1988;38:411–419. doi: 10.4269/ajtmh.1988.38.411. [DOI] [PubMed] [Google Scholar]
- 5.Littaua R, Kurane I, Ennis FA. J Immunol. 1990;144:3183–3186. [PubMed] [Google Scholar]
- 6.Morens DM, Venkateshan CN, Halstead SB. J Gen Virol. 1987;68(Pt 1):91–8. doi: 10.1099/0022-1317-68-1-91. [DOI] [PubMed] [Google Scholar]
- 7.Lin YW, Wang KJ, Lei HY, Lin YS, Yeh TM, Liu HS, Liu CC, Chen SH. J Virol. 2002;76:12242–12249. doi: 10.1128/JVI.76.23.12242-12249.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Halstead SB. J Infect Dis. 1979;140:527–533. doi: 10.1093/infdis/140.4.527. [DOI] [PubMed] [Google Scholar]
- 9.Heinz FX. Adv Virus Res. 1986;31:103–168. doi: 10.1016/s0065-3527(08)60263-8. [DOI] [PubMed] [Google Scholar]
- 10.Roehrig JT, Bolin RA, Kelly RG. Virology. 1998;246:317–328. doi: 10.1006/viro.1998.9200. [DOI] [PubMed] [Google Scholar]
- 11.Goncalvez AP, Purcell RH, Lai CJ. J Virol. 2004;78:12919–12928. doi: 10.1128/JVI.78.23.12919-12928.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Oliphant T, Nybakken GE, Engle M, Xu Q, Nelson CA, Sukupolvi-Petty S, Marri A, Lachmi BE, Olshevsky U, Fremont DH, et al. J Virol. 2006;80:12149–12159. doi: 10.1128/JVI.01732-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stiasny K, Kiermayr S, Holzmann H, Heinz FX. J Virol. 2006;80:9557–9568. doi: 10.1128/JVI.00080-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Goncalvez AP, Men R, Wernly C, Purcell RH, Lai CJ. J Virol. 2004;78:12910–12918. doi: 10.1128/JVI.78.23.12910-12918.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Men R, Yamashiro T, Goncalvez AP, Wernly C, Schofield DJ, Emerson SU, Purcell RH, Lai CJ. J Virol. 2004;78:4665–4674. doi: 10.1128/JVI.78.9.4665-4674.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tassaneetrithep B, Burgess TH, Granelli-Piperno A, Trumpfheller C, Finke J, Sun W, Eller MA, Pattanapanyasat K, Sarasombath S, Birx DL, et al. J Exp Med. 2003;197:823–829. doi: 10.1084/jem.20021840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Armour KL, Clark MR, Hadley AG, Williamson LM. Eur J Immunol. 1999;29:2613–2624. doi: 10.1002/(SICI)1521-4141(199908)29:08<2613::AID-IMMU2613>3.0.CO;2-J. [DOI] [PubMed] [Google Scholar]
- 18.Brunak S, Engelbrecht J, Knudsen S. J Mol Biol. 1991;220:49–65. doi: 10.1016/0022-2836(91)90380-o. [DOI] [PubMed] [Google Scholar]
- 19.Hough DW, Narendran A, Hall ND. Immunol Lett. 1983;7:85–89. doi: 10.1016/0165-2478(83)90039-1. [DOI] [PubMed] [Google Scholar]
- 20.Rodrigo WW, Jin X, Blackley SD, Rose RC, Schlesinger JJ. J Virol. 2006;80:10128–10138. doi: 10.1128/JVI.00792-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Halstead SB, Shotwell H, Casals J. J Infect Dis. 1973;128:15–22. doi: 10.1093/infdis/128.1.15. [DOI] [PubMed] [Google Scholar]
- 22.Endy TP, Nisalak A, Chunsuttitwat S, Vaughn DW, Green S, Ennis FA, Rothman AL, Libraty DH. J Infect Dis. 2004;189:990–1000. doi: 10.1086/382280. [DOI] [PubMed] [Google Scholar]
- 23.Vaughn DW, Green S, Kalayanarooj S, Innis BL, Nimmannitya S, Suntayakorn S, Endy TP, Raengsakulrach B, Rothman AL, Ennis FA, Nisalak A. J Infect Dis. 2000;181:2–9. doi: 10.1086/315215. [DOI] [PubMed] [Google Scholar]
- 24.Laoprasopwattana K, Libraty DH, Endy TP, Nisalak A, Chunsuttiwat S, Vaughn DW, Reed G, Ennis FA, Rothman AL, Green S. J Infect Dis. 2005;192:510–519. doi: 10.1086/431520. [DOI] [PubMed] [Google Scholar]
- 25.Kurane I, Ennis FE. Semin Immunol. 1992;4:121–127. [PubMed] [Google Scholar]
- 26.Nimmerjahn F, Ravetch JV. Immunity. 2006;24:19–28. doi: 10.1016/j.immuni.2005.11.010. [DOI] [PubMed] [Google Scholar]
- 27.Kimura-Kuroda J, Yasui K. J Immunol. 1988;141:3606–3610. [PubMed] [Google Scholar]
- 28.Gould EA, Buckley A. J Gen Virol. 1989;70(Pt 6):1605–1608. doi: 10.1099/0022-1317-70-6-1605. [DOI] [PubMed] [Google Scholar]
- 29.Olsen CW, Corapi WV, Ngichabe CK, Baines0 JD, Scott FW. J Virol. 1992;66:956–965. doi: 10.1128/jvi.66.2.956-965.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fust G. Parasitology. 1997;115(Suppl):S127–S40. doi: 10.1017/s0031182097001819. [DOI] [PubMed] [Google Scholar]
- 31.Takada A, Feldmann H, Ksiazek TG, Kawaoka Y. J Virol. 2003;77:7539–7544. doi: 10.1128/JVI.77.13.7539-7544.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Falgout B, Bray M, Schlesinger JJ, Lai CJ. J Virol. 1990;64:4356–4363. doi: 10.1128/jvi.64.9.4356-4363.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Oliphant T, Engle M, Nybakken GE, Doane C, Johnson S, Huang L, Gorlatov S, Mehlhop E, Marri A, Chung KM, et al. Nat Med. 2005;11:522–530. doi: 10.1038/nm1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Guy B, Chanthavanich P, Gimenez S, Sirivichayakul C, Sabchareon A, Begue S, Yoksan S, Luxemburger C, Lang J. Vaccine. 2004;22:3563–3574. doi: 10.1016/j.vaccine.2004.03.042. [DOI] [PubMed] [Google Scholar]
- 35.Takahashi N, Ueda S, Obata M, Nikaido T, Nakai S, Honjo T. Cell. 1982;29:671–679. doi: 10.1016/0092-8674(82)90183-0. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting Table