Rapid Dissemination and Diversity of CTX-M Extended-Spectrum β-Lactamase Genes in Commensal Escherichia coli Isolates from Healthy Children from Low-Resource Settings in Latin America (original) (raw)
Abstract
A survey carried out in 2005 among members of a healthy population of children living in Bolivia and Peru revealed that fecal carriage of Escherichia coli strains resistant to expanded-spectrum cephalosporins was remarkably increased compared to that observed in the same settings in 2002 (1.7% in 2005 versus 0.1% in 2002). In this work, we demonstrated that this phenomenon was mainly related to the dissemination of CTX-M-type extended-spectrum β-lactamase (ESBL) determinants among commensal E. coli strains. Of 50 ESBL-producing isolates collected in the 2005 survey, 44 harbored a CTX-M-type and 6 an SHV-type (SHV-2 or SHV-12) ESBL. Compared to 2002 results, an increased diversity of CTX-M-type ESBLs was also observed: members of the CTX-M-1 group (CTX-M-15) emerged in Bolivia (where only CTX-M-2 was observed in 2002), while members of the CTX-M-9 group (CTX-M-14 and CTX-M-24) emerged in Peru (where only CTX-M-15 and CTX-M-2 were observed in 2002). A new CTX-M-2 variant named CTX-M-56 was also detected. Molecular characterization of the CTX-M-producing isolates and gene transfer experiments suggested that different mechanisms could be involved in the spreading of different CTX-M group determinants and revealed that additional resistance determinants for non-β-lactam antibiotics were preferentially carried by plasmids encoding certain CTX-M variants (CTX-M-15 and variants of the CTX-M-2 group). Three CTX-M-15-encoding conjugative plasmids from Peruvian isolates carried the new fluoroquinolone resistance gene aac(6_′)-Ib-cr_. To our best knowledge, this is the first report of the detection of aac(6_′)-Ib-cr_ in Latin America.
Plasmid-encoded extended-spectrum β-lactamases (ESBLs) impair the efficacy of expanded-spectrum cephalosporins and monobactams and are among the most important acquired resistance determinants emerging worldwide in members of the Enterobacteriaceae (7, 15, 21). ESBL-producing strains represent an emerging clinical threat not only for their rapid and widespread dissemination but also because they often exhibit a multidrug resistance phenotype, leaving only limited therapeutic options (7, 15, 21). In fact, a significant impact on morbidity, mortality, and health care-associated costs has been demonstrated previously for infections caused by ESBL producers (30).
The CTX-M-type β-lactamases are members of a lineage of ESBLs which exhibited dramatic dissemination in the past decade; in several clinical settings, these enzymes currently outnumber the classical TEM- and SHV-type ESBLs (5, 9, 21). Based on their amino-acidic sequence diversity, the vast number (more than 50) of CTX-M variants identified thus far have been classified into five major phylogenetic groups: CTX-M-1, CTX-M-2, CTX-M-8, CTX-M-9, and CTX-M-25 (http://www.lahey.org/studies/webt.stm) (5, 9). Strains producing CTX-M-type ESBLs have been reported as important causes of both nosocomial and community-acquired infections (5, 9). CTX-M determinants have been detected not only in clinical isolates but also in commensal bacteria from humans and animals and in isolates from products of the food chain and sewage, revealing a wide distribution and suggesting the presence of environmental reservoirs of these resistance determinants (8, 9). In fact, recent studies have addressed the importance of the influx into the hospitals of CTX-M-producing isolates from the community (3).
ANTRES is a collaborative research project dealing with antibiotic use and resistance in two countries of Latin America, Bolivia, and Peru (http://www.unifi.it/infdis/antres/default.htm). Within this project, a large-scale survey of fecal carriage of antibiotic-resistant Escherichia coli strains in preschool-age healthy children was carried out in 2002 (1) and was repeated in 2005. Comparative analysis of results from the two surveys revealed that, in this three-year period, a remarkable increase in the rates of resistance to expanded-spectrum cephalosporins had occurred (0.1% in 2002 versus 1.7% in 2005) (1; A. Bartoloni, L. Pallecchi, C. Fiorelli, T. Di Maggio, C. Fernandez, A. L. Villagran, A. Mantella, F. Bartalesi, M. Strohmeyer, A. Bechini, M. Gamboa, M. Rodriguez, C. Kristiansson, G. Kronvall, E. Gotuzzo, F. Paradisi, and G. M. Rossolini, unpublished data). In this report, we demonstrate that this phenomenon was mainly the consequence of the dissemination of CTX-M-type determinants among commensal E. coli strains.
(These results were presented in part at the 46th Interscience Conference on Antimicrobial Agents and Chemotherapy, San Francisco, CA, 2006.)
MATERIALS AND METHODS
Bacterial isolates.
The 54 E. coli isolates investigated in this study represented all the isolates showing reduced susceptibility to ceftriaxone (defined according to the Clinical and Laboratory Standards Institute [CLSI] modified breakpoint for screening of ESBL producers [12]) collected in the 2005 survey of the ANTRES project. The ANTRES project included two large surveys carried out in 2002 and 2005, respectively, of antibiotic resistance rates in commensal E. coli strains from healthy children (aged 6 to 72 months) living in four urban areas of Latin America (Camiri, Santa Cruz Department, and Villa Montes, Tarija Department, Bolivia, and Yurimaguas, Loreto Department, and Moyobamba, San Martin Department, Peru). The two surveys were conducted using the same study design and methodology and covered population samples of similar sizes (3,174 and 3,193 healthy children in the 2002 and 2005 surveys, respectively) (1; Bartoloni et al., unpublished data). The four CTX-M-producing E. coli isolates from the 2002 survey, which had been previously investigated (19), were included for comparative analysis.
In vitro susceptibility testing.
Antimicrobial susceptibility was determined by the disk diffusion test, according to the methods and interpretative criteria proposed by CLSI (12). Antibiotic disks were from Oxoid (Oxoid, Milan, Italy). E. coli ATCC 25922 was used for quality control purposes. The double-disk synergy test for confirmation of ESBL activity was carried out as described previously (16) by screening isolates for synergism between clavulanate (represented by a disk with amoxicillin-clavulanate) and cefotaxime, ceftazidime, and aztreonam.
Molecular analysis techniques.
Basic procedures for DNA extraction and analysis were performed as described by Sambrook and Russell (29). Nucleotide sequences were determined on both strands of PCR amplification products at the Macrogen sequencing facility (Macrogen Inc., Seoul, Korea). Analysis and comparisons of nucleotide sequence were carried out using programs available at the NCBI web interface (http://www.ncbi.nlm.nih.gov). The presence of CTX-M-related sequences was investigated by colony blot hybridization with a _bla_CTX-M probe, as described previously (19). Primers used in this work for PCR amplification of antibiotic resistance genes are reported in Table 1. PCR conditions were as described in the corresponding references or, for PCR amplification of bla_CTX-M alleles belonging to groups 1 and 9 and of bla_SHV genes, as follows: initial denaturation at 94°C for 5 min; denaturation at 94°C for 45 s, annealing at 50°C for 45 s, and elongation at 72°C for 5 min, repeated for 35 cycles; and final extension at 72°C for 10 min. Forward primers used for amplification of group 2 or for amplification of group 1 and 9 CTX-M genes targeted IS_CR1 and IS_Ecp1 elements, respectively. Phylogenetic grouping of the E. coli isolates was determined by the multiplex PCR-based method developed by Clermont et al., which allows identification of the four major phylogenetic groups (A, B1, B2, and D) (11). Randomly amplified polymorphic DNA (RAPD) genotyping was performed as previously described (17) using, separately, the decamer primers 1290 and 1254. RAPD patterns were considered to be different when the profiles differed by at least one band. Analysis of the RAPD patterns was performed with Diversity Database fingerprinting software, version 2 (Bio-Rad Laboratories, Hercules, CA).
TABLE 1.
Oligonucleotide primers used for PCR amplification of antibiotic resistance genes
| Target gene(s) | Oligonucleotide primer sequence (5′-3′)a | Reference or source | |
|---|---|---|---|
| Forward | Reverse | ||
| _bla_TEM-like | ATAAAATTCTTGAAGACGAA | ATATGAGTAAGCTTGGTCTGACAG | 19 |
| _bla_SHV-like | CCTCACTCAAGGATGTATTGTG | TTAGCGTTGCCAGTGYTCG | This study |
| _bla_CTX-M-like | ATGTGCAGYACCAGTAARGT | TGGGTRAARTARGTSACCAGA | 19 |
| _bla_CTX-M-1 group | ACTATCCGTACAAGGGAGT | CCGTTTCCGCTATTACAAAC | This study |
| _bla_CTX-M-2 group | GATCCATCACAGAGTCGTCTCT | GGCAGCTCATACAGGTAACTCT | 19 |
| _bla_CTX-M-9 group | ACTATCCGTACAAGGGAGT | CAGCCAGAAAGTTATGGAG | This study |
| qnrA | ATTTCTCACGCCAGGATTTG | GATCGGCAAAGGTTAGGTCA | 25 |
| qnrB | GATCGTGAAAGCCAGAAAGG | ACGATGCCTGGTAGTTGTCC | 25 |
| qnrS | ACGACATTCGTCAACTGCAA | TAAATTGGCACCCTGTAGGC | 25 |
| aac(_6_′)-Ib | TTGCGATGCTCTA TGAGTGGCTA | CTCGAATGCCTGGCGTGTTT | 20 |
Plasmid analysis.
Plasmid replicon typing was carried out by PCR as described by Carattoli et al. (10). Conjugal transfer of CTX-M determinants was assayed by mating experiments using Mueller-Hinton (MH) agar plates (Difco Laboratories, Detroit, MI) and E. coli J53 (pro met rifampin resistant and nalidixic acid resistant [NALr]) as the recipient and an initial donor/recipient ratio of 0.1. Mating plates were incubated at 30°C for 14 h. Transconjugants were selected on MH agar containing rifampin (400 μg/ml) and nalidixic acid (32 μg/ml) plus cefotaxime (2 μg/ml) (Sigma Chemical Co., St. Louis, MO). Transconjugants were always confirmed by testing for the recipient's genetic markers (pro met). Under the above-described conditions, the detection sensitivity of the mating assay was ≥5 × 10−8 transconjugants/recipient. Mobilization of nonconjugative _bla_CTX-M-harboring plasmids was carried out by electroporation using E. coli DH5α and MH agar containing cefotaxime (2 μg/ml) for selection of transformants. The presence of _bla_CTX-M genes in the transconjugants and transformants was always confirmed by PCR. Plasmid fingerprinting analysis after digestion with PstI was carried out with all transferable A/C-, I1-, and F-type plasmids carrying group 2, 9, and 1 CTX-M determinants, respectively.
Nucleotide sequence accession numbers.
The sequences of _bla_CTX-M-56 and the new variant allele of _bla_CTX-M-24 have been deposited in GenBank and assigned accession numbers EF374097 and EF374096, respectively.
RESULTS
Spread of ESBL-producing E. coli in the commensal microbiota of healthy children from Bolivia and Peru.
In the 2005 survey, the prevalence of children carrying isolates with reduced susceptibility to ceftriaxone was found to be remarkably increased compared to that observed three years earlier (1.7% versus 0.1%). The phenomenon was evident in each of the four surveyed areas, two in Bolivia (Camiri, 2.9% versus 0.1%; Villa Montes, 0.9% versus 0.1%) and two in Peru (Yurimaguas, 1.5% versus 0.1%; Moyobamba, 1.5% versus 0.1%) (1; Bartoloni et al., unpublished data).
Overall, 54 isolates showing reduced ceftriaxone susceptibility were collected in the 2005 survey, and 50 of them were confirmed as ESBL producers in a double-disk synergy test. The four isolates that did not exhibit ESBL production showed a resistance phenotype suggestive of production of an AmpC-type β-lactamase (resistance to cephamycins and to β-lactam-inhibitor combinations, susceptibility to cefepime) and were not further investigated in this work.
The 50 ESBL-producing isolates were tested for the presence of CTX-M-like determinants by colony-blot hybridization. Results showed that 44 isolates (88%) carried _bla_CTX-M-related sequences. Most (84%) of the CTX-M-producing isolates also carried a _bla_TEM-1b gene, while none of them carried _bla_SHV-related sequences. Prevalences of fecal carriers of CTX-M-positive E. coli strains were 2.4% in Camiri and 0.9% in Villa Montes, Bolivia, and 1.1% in Yurimaguas and 1.1% in Moyobamba, Peru. The six ESBL-producing _bla_CTX-M-negative isolates were shown to harbor SHV-type ESBL determinants, either _bla_SHV-2 (four isolates, two from Bolivia and two from Peru) or _bla_SHV-12 (two isolates from Peru). Two of these isolates (one SHV-2-producing isolate and one SHV-12-producing isolate, both from Peru) also carried a _bla_TEM-1b gene.
Characterization and distribution of the CTX-M determinants.
Sequencing of the CTX-M-encoding genes identified variants belonging to CTX-M-2 (41%), CTX-M-1 (32%), and CTX-M-9 (27%) groups. CTX-M-2 group determinants included _bla_CTX-M-2 and a new variant named _bla_CTX-M-56 (GenBank accession number EF374097) that differed from _bla_CTX-M-2 (2) by a single nucleotide mutation (G824A), resulting in a replacement of serine by asparagine at position 275. CTX-M-1 group determinants included only _bla_CTX-M-15. CTX-M-9 group determinants included _bla_CTX-M-14 and a new allele of _bla_CTX-M-24 (GenBank accession number EF374096), showing two synonymous transversions (C823A and C825A) compared to _bla_CTX-M-24 as described by Eckert et al. (13). This new _bla_CTX-M-24 allele differed from bla_CTX-M-14 (18) by a single transversion (C825A) that was responsible for the replacement of a serine by an arginine at position 275 and was likely derived from bla_CTX-M-14. As far as the 5′-flanking regions of CTX-M genes are concerned, all group 2 alleles were found to be associated with an IS_CR1 element, while all group 1 and 9 alleles were found to be associated with an IS_Ecp1 element.
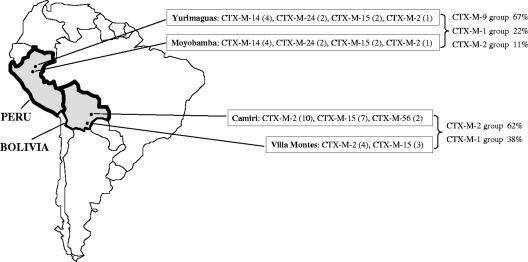
Concerning the geographic distribution, group 2 CTX-M determinants were the most prevalent in Bolivia (62%) and the least prevalent in Peru (11%), group 9 CTX-M determinants were the most prevalent in Peru (67%) and absent in Bolivia, while group 1 CTX-M determinants were the second most prevalent in both countries (38% in Bolivia and 22% in Peru). In Bolivia, the most prevalent CTX-M variant was _bla_CTX-M-2 (54%) followed by _bla_CTX-M-15 (38%) and _bla_CTX-M-56 (8%). In Peru, the most prevalent CTX-M variant was _bla_CTX-M-14 (45%) followed by _bla_CTX-M-24 (22%), _bla_CTX-M-15 (22%), and _bla_CTX-M-2 (11%) (Fig. 1).
FIG. 1.
Geographic distribution of CTX-M variants detected in fecal E. coli strains from healthy children in the 2005 survey of the ANTRES study. The number of isolates harboring each CTX-M variant is reported in brackets.
Antimicrobial susceptibility of isolates harboring _bla_CTX-M genes.
All the CTX-M-producing isolates showed a multidrug resistance phenotype: 86% showed coresistance to tetracycline, 77% to trimethoprim-sulfamethoxazole, 68% to gentamicin, 57% to nalidixic acid, and 54% to ciprofloxacin (Table 2). Higher coresistance rates were observed in CTX-M-15-producing isolates for quinolones (93%; resistance to both nalidixic acid and ciprofloxacin) and in CTX-M-2 group-producing isolates for gentamicin (100%) (Table 2).
TABLE 2.
Characteristics of the CTX-M-producing isolates and of the _bla_CTX-M-harboring plasmids
| Group | CTX-M type | RAPD type (no. of isolates) | Phylogenetic group | Origina | TEM typeb | Resistance to antibiotics other than β-lactamsc | Transfer in E. coli recipientsd | Resistance traits cotransferred with _bla_CTX-M genese | Plasmid replicon type(s) in recipients | Plasmid fingerprinting in recipientsf |
|---|---|---|---|---|---|---|---|---|---|---|
| CTX-M-2 | CTX-M-2 | 1 (1) | B1 | Y | TEM-1b* | GEN, SXT, NAL, CIP | Conj. | GEN | A/C | A |
| 2 (1) | D | M | GEN, TET, SXT, NAL, CIP | Conj. | TET | A/C | B | |||
| 3 (1) | A | C | GEN, TET, SXT | Conj. | GEN, SXT | Not identified | ND | |||
| 4 (1) | A | C | TEM-1b* | GEN, TET | Conj. | GEN, TET | A/C | C | ||
| 5 (1) | A | C | TEM-1b* | GEN, TET, SXT | Conj. | GEN | A/C | A | ||
| 6 (1) | A | C | GEN, TET, SXT | Conj. | GEN, TET, SXT | Not identified | ND | |||
| 7 (1) | B1 | C | TEM-1b | GEN, TET, SXT | Conj. | GEN, TET, SXT | FVII | ND | ||
| 8 (1) | B1 | C | TEM-1b* | GEN, TET, NAL, CIP | Conj. | GEN | A/C | D | ||
| 9 (1) | B1 | C | TEM-1b* | GEN, TET, SXT, NAL, CIP | Conj. | GEN | A/C | A | ||
| 10 (1) | D | C | TEM-1b* | GEN, TET, SXT | Conj. | GEN | A/C | E | ||
| 11 (1) | D | C | GEN, TET, SXT | Conj. | GEN, TET, SXT | Not identified | ND | |||
| 12 (1) | D | C | TEM-1b* | GEN, TET, SXT | Conj. | GEN, TET | A/C | F | ||
| 13 (1) | A | VM | GEN, TET, SXT | Conj. | GEN | I1 | ND | |||
| 14 (1) | A | VM | TEM-1b* | GEN, TET | Conj. | GEN | A/C | G | ||
| 15 (1) | B2 | VM | TEM-1b* | GEN, TET, SXT, NAL | Conj. | GEN | A/C | A | ||
| 16 (1) | D | VM | TEM-1b* | GEN, TET, SXT | Conj. | GEN, TET, SXT | A/C | H | ||
| CTX-M-56 | 17 (1) | A | C | TEM-1b* | GEN, TET, SXT | Conj. | GEN | A/C | G | |
| 18 (1) | A | C | TEM-1b* | GEN, TET, SXT | Conj. | GEN | A/C | G | ||
| CTX-M-9 | CTX-M-14 | 19 (1) | A | Y | TEM-1b | TET, SXT, NAL, CIP | No | |||
| 20 (3) | A | Y | TEM-1b | TET, SXT | Conj. | None | I1 | I | ||
| 21 (1) | A | M | TEM-1b | SXT, NAL, CIP | Transf. | None | I1 | L | ||
| 22 (1) | A | M | TEM-1b | GEN, TET, SXT, NAL, CIP | No | |||||
| 23 (1) | A | M | TEM-1b | GEN, TET, SXT, NAL, CIP | Transf. | None | I1 | L | ||
| 24 (1) | D | M | TEM-1b | SXT, NAL, CIP | Transf. | None | I1 | M | ||
| CTX-M-24 | 25 (2) | B1 | Y | TEM-1b* | SXT, NAL, CIP | Conj. | None | I1 | N | |
| 26 (2) | A | M | TEM-1b* | TET, SXT | Conj. | None | I1 | O | ||
| CTX-M-1 | CTX-M-15 | 27 (1) | B2 | Y | TEM-1b | GEN | No | |||
| 28 (1) | D | Y | TEM-1b* | GEN, TET, NAL, CIP | Conj. | TET, CIP | FIA, FIB, FII | P | ||
| 29 (2) | A | M | GEN, TET, SXT, NAL, CIP | Conj. | GEN, SXT, CIP | FIA, FIB, FII | Q | |||
| 30 (3 + 2) | A | C + VM | TEM-1b | GEN, TET, SXT, NAL, CIP | No | |||||
| 31 (4 + 1) | B1 | C + VM | TEM-1b | TET, NAL, CIP | Conj. | None | Not identified | ND |
Phylogenetic grouping and genotypes of the CTX-M-producing E. coli isolates.
CTX-M-producing isolates belonged to all phylogenetic groups (A, 55%; B1, 25%; D, 16%; and B2, 4%) (Table 2). No significant correlation was observed between the nature of the CTX-M determinant and the phylogenetic group.
RAPD genotyping identified 31 different types, of which 25 were unique and 6 included more than one isolate (Table 2). All the isolates harboring CTX-M-2 group determinants (_bla_CTX-M-2 and _bla_CTX-M-56) showed unique RAPD genotypes, while clonal expansion was observed for some isolates harboring CTX-M determinants of the other groups (Table 2). In particular, dissemination of CTX-M-15 in Bolivia (not observed in 2002) appeared to be the consequence of the spread of two clones (RAPD types 30 and 31) circulating in both Camiri and Villa Montes (Table 2). Clonal expansion of CTX-M-producing isolates was also observed in Peru for CTX-M-14-, CTX-M-15-, and CTX-M-24-producing isolates (RAPD types 20, 29, and 25 through 26, respectively), even though the spreading of each clone was limited to a single city (Table 2). None of the CTX-M-producing isolates collected in 2005 showed genomic similarity (based on RAPD analysis) to those collected from the same areas in the 2002 survey (data not shown).
Transferability of CTX-M determinants and typing of the _bla_CTX-M-harboring plasmids.
Conjugal transfer of CTX-M determinants was observed with 33 isolates (75%) representative of 24 different RAPD types (Table 2). All the CTX-M-2 group determinants were carried by conjugative plasmids, mainly of the A/C type (72%), which always carried other resistance genes (cotransfer of gentamicin resistance occurred in 94% of cases) (Table 2). Plasmid replicon typing of transconjugants obtained with the three CTX-M-2-producing isolates from the 2002 survey (19) identified in all cases plasmids of the A/C type, underlining the role of these mobile genetic elements in the dissemination of CTX-M-2 group determinants in the study areas. Conjugal transfer of CTX-M-1 and CTX-M-9 group determinants was observed less frequently (57% and 58%, respectively), and in some cases nonconjugative CTX-M-9 group determinants could be mobilized by electroporation (Table 2). Transfer of CTX-M-9 group determinants was related to I1-type plasmids and was never associated with cotransfer of other resistance traits. Transfer of CTX-M-1 group determinants was related to conjugative plasmids harboring none of the replicon types investigated (RAPD type 31 from Bolivia) or to F-type conjugative plasmids which also carried determinants responsible for fluoroquinolone resistance (RAPD types 28 and 29 from Peru) (Table 2).
Plasmid fingerprinting analysis was carried out with all transferable A/C-, I1-, and F-type plasmids carrying group 2, 9, and 1 CTX-M determinants, respectively. Different plasmid profiles were observed within plasmids carrying each replicon type (Table 2). However, in most cases, plasmids carrying CTX-M genes of the same group shared some bands of the same size, suggesting a common ancestry (data not shown). In particular, the plasmids carrying _bla_CTX-M-56 showed a profile identical to that of one of the plasmids carrying _bla_CTX-M-2, further supporting the hypothesis of a local evolution of the new CTX-M variant (Table 2 and data not shown). Moreover, the same profile (profile A) was observed with _bla_CTX-M-2-harboring plasmids from both Peru and Bolivia and was apparently identical to that observed with the A/C-type _bla_CTX-M-2-harboring plasmid detected in Peru during the 2002 survey (19), demonstrating the presence of an epidemic plasmid responsible for the dissemination of CTX-M-2 ESBL in these geographic areas (Table 2 and data not shown).
Characterization of the plasmid-mediated fluoroquinolone resistance determinants.
The three transconjugants showing decreased susceptibility to ciprofloxacin were investigated for the presence of known plasmid-mediated fluoroquinolone resistance genes (24). None of the qnr_-type determinants investigated (qnrA, qnrB, and qnrS) was detected. In contrast, all three transconjugants gave positive results in a PCR experiment using primers designed for amplification of aac(6_′)-Ib variants (20). Sequence analysis of the amplicons identified, in all cases, an aac(6_′)-Ib-cr_ variant (100% identity with aac(6_′)-Ib-cr_ of GenBank entry DQ303918) (26) that could account for the decreased susceptibility to ciprofloxacin expressed by the transconjugants. To our best knowledge, this is the first detection of aac(6_′)-Ib-cr_ in Latin America.
The F-type plasmids harboring bla_CTX-M-15 and aac(6_′)-Ib-cr showed identical patterns of F replicons (FIA, FIB, and FII) and similar plasmid profiles (Table 2 and data not shown). Sequence analysis of the FII-regulatory antisense RNA CopA, which is involved in the control of replication and in the incompatibility behavior of the FII plasmids (4), evidenced, in all cases, identical CopA sequences (100% identical to that of plasmid pRSB107 of GenBank entry AJ851089), further supporting the idea of a common origin of these three plasmids.
DISCUSSION
Results of this study provided an example of how ESBL determinants in general and CTX-M in particular are rapidly spreading among commensal E. coli strains in healthy subjects from low-resource settings. In the surveyed area, including urban settings in Bolivia and Peru, the prevalence of healthy children carrying ESBL-positive E. coli strains in their commensal microbiota underwent a dramatic (17-fold) increase over a 3-year time period that was mostly contributed by CTX-M-type determinants. This phenomenon is a matter of concern, since commensals can act as a reservoir of resistance genes (Reservoirs of Antibiotic Resistance Network [http://www.roarproject.org]; Alliance for Prudent Use of Antibiotics), while intestinal colonization by ESBL-producing isolates can be a source for influx of ESBL determinants into the hospital setting and represents a risk factor for subsequent infections caused by ESBL-producing strains in hospitalized patients (3). The reasons for this alarming evolution remain unclear. Although antibiotic consumption data are not available, it is reasonable to assume that carriage of commensal ESBL producers in preschool-age healthy children mostly reflected exposure to contamination in the family environment rather than an increased direct exposure to expanded-spectrum cephalosporins or other agents known to select ESBL producers (15, 21, 27, 28). To further clarify this point, it would be interesting to assess the extent of the phenomenon in the adult population from the same areas also.
Interestingly, the increased prevalence of ESBL-producing isolates was also associated with an increased diversity of circulating ESBL determinants, although the use of ceftriaxone as the only ESBL screening agent might have limited the detection of ESBLs with specific ceftazidimase activity. Compared to the baseline survey carried out in 2002 (19), members of the CTX-M-1 group (CTX-M-15) emerged in Bolivia also, while members of the CTX-M-9 group (CTX-M-14 and CTX-M-24) emerged in Peru. Moreover, SHV-type ESBLs emerged in both countries.
Molecular characterization of the CTX-M-producing isolates suggested different mechanisms of spreading for determinants belonging to different CTX-M groups. Concerning CTX-M-2 group determinants, which are widely disseminated in Latin America (5, 9, 22, 23) and have been present in the study areas since 2002 (19), their exclusive location on conjugative plasmids and the high genotypic diversity of bacterial hosts suggest that plasmid dissemination played a major role in their diffusion. This hypothesis is further supported by plasmid replicon typing and fingerprinting analysis results, which revealed that one or a few related A/C-type conjugative plasmids could be involved in their dissemination in these areas. In contrast, a role in clonal expansion, along with plasmid mobilization, was evidenced for dissemination of CTX-M determinants more recently introduced in the study areas (the CTX-M-1 group in Bolivia and the CTX-M-9 group in Peru).
Two new CTX-M alleles were identified in this study: a new CTX-M-2 group variant named _bla_CTX-M-56 (in Bolivia) and a new _bla_CTX-M-24 allele (in Peru). Interestingly, the two differed by a single nucleotide mutation from the most prevalent CTX-M-type gene detected in each country (CTX-M-2 in Bolivia and CTX-M-14 in Peru), suggesting a local evolution of these resistance determinants. This hypothesis was further supported by results of replicon typing and plasmid fingerprinting, which showed a common genetic context for these new _bla_CTX-M alleles and their likely precursors (A/C type plasmids for _bla_CTX-M-2 and _bla_CTX-M-56; I1-type plasmids for _bla_CTX-M-14 and _bla_CTX-M-24).
CTX-M-encoding plasmids are known to often carry additional determinants of resistance to non-β-lactam agents, including quinolones (9). In this study, we detected the presence of plasmid-mediated quinolone resistance determinants in three bla_CTX-M-15-harboring conjugative plasmids from Peruvian isolates. These plasmids carried the aac(6_′)-Ib-cr gene and showed identical patterns of replicon types (FIA, FIB, and FII) and similar plasmid profiles, suggesting a common origin. Moreover, sequence analysis of the FII replicons evidenced an IncFII plasmid backbone identical to that of pRSB107, which was recently also found in _bla_CTX-M-15-harboring plasmids from E. coli clinical isolates in the United Kingdom (14). These findings support the evidence of the dissemination of FII-type bla_CTX-M-15-harboring plasmids in different countries, a result that has recently also been observed for a different lineage of IncFII plasmids detected in CTX-M-15-producing E. coli strains from Canada and United Kingdom (6, 14). Furthermore, to our best knowledge this is the first detection of an aac(6_′)-Ib-cr gene in commensal bacteria from healthy humans and also the first report of the presence of this resistance determinant in Latin America.
Acknowledgments
This work was supported by the European Commission within the ANTRES project (Towards Controlling Antimicrobial Use and Resistance in Low-Income Countries: an intervention study in Latin America), INCO-DEV contract ICA4-CT-2001-10014.
We are grateful to Patrice Nordmann and Laurent Poirel (Université Paris-Sud, K.-Bicetre, France) for supplying controls for qnr genes. We wish to thank all the members of the ANTRES Study Group for their support in this study.
Footnotes
▿
Published ahead of print on 4 June 2007.
REFERENCES
- 1.Bartoloni, A., L. Pallecchi, M. Benedetti, C. Fernandez, Y. Vallejos, E. Guzman, A. L. Villagran, A. Mantella, C. Lucchetti, F. Bartalesi, M. Strohmeyer, A. Bechini, H. Gamboa, H. Rodriguez, T. Falkenberg, G. Kronvall, E. Gotuzzo, F. Paradisi, and G. M. Rossolini. 2006. Multidrug-resistant commensal Escherichia coli in children, Peru and Bolivia. Emerg. Infect. Dis. 12**:**907-913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bauernfeind, A., I. Stemplinger, R. Jungwirth, S. Ernst, and J. M. Casellas. 1996. Sequences of β-lactamase genes encoding CTX-M-1 (MEN-1) and CTX-M-2 and relationship of their amino acid sequences with those of other β-lactamases. Antimicrob. Agents Chemother. 40**:**509-513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ben-Ami, R., M. J. Schwaber, S. Navon-Venezia, D. Schwartz, M. Giladi, I. Chmelnitsky, A. Leavitt, and Y. Carmeli. 2006. Influx of extended-spectrum β-lactamase-producing Enterobacteriaceae into the hospital. Clin. Infect. Dis. 42**:**925-934. [DOI] [PubMed] [Google Scholar]
- 4.Blomberg, P., K. Nordstrom, and E. G. Wagner. 1992. Replication control of plasmid R1: RepA synthesis is regulated by CopA RNA through inhibition of leader peptide translation. EMBO J. 11**:**2675-2683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bonnet, R. 2004. Growing group of extended-spectrum β-lactamases: the CTX-M enzymes. Antimicrob. Agents Chemother. 48**:**1-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Boyd, D. A., S. Tyler, S. Christianson, A. McGeer, M. P. Muller, B. M. Willey, E. Bryce, M. Gardam, P. Nordmann, and M. R. Mulvey. 2004. Complete nucleotide sequence of a 92-kilobase plasmid harbouring the CTX-M-15 extended-spectrum β-lactamase involved in an outbreak in long-term-care facilities in Toronto, Canada. Antimicrob. Agents Chemother. 48**:**3758-3764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bradford, P. A. 2001. Extended-spectrum β-lactamases in the 21st century: characterization, epidemiology, and detection of this important resistance threat. Clin. Microbiol. Rev. 14**:**933-951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brinas, L., M. A. Moreno, M. Zarazaga, C. Porrero, Y. Saenz, M. Garcia, L. Dominguez, and C. Torres. 2003. Detection of CMY-2, CTX-M-14, and SHV-12 β-lactamases in Escherichia coli fecal-sample isolates from healthy chickens. Antimicrob. Agents Chemother. 47**:**2056-2058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Canton, R., and T. M. Coque. 2006. The CTX-M β-lactamase pandemic. Curr. Opin. Microbiol. 9**:**466-475. [DOI] [PubMed] [Google Scholar]
- 10.Carattoli, A., A. Bertini, L. Villa, V. Falbo, K. L. Hopkins, and E. J. Threlfall. 2005. Identification of plasmids by PCR-based replicon typing. J. Microbiol. Methods 63**:**219-228. [DOI] [PubMed] [Google Scholar]
- 11.Clermont, O., S. Bonacorsi, and E. Bingen. 2000. Rapid and simple determination of the Escherichia coli phylogenetic group. Appl. Environ. Microbiol. 66**:**4555-4558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Clinical and Laboratory Standards Institute. 2006. Performance standards for antimicrobial disk susceptibility tests; approved standard—ninth edition. Clinical Laboratory Standards Institute, Wayne, PA.
- 13.Eckert, C., V. Gautier, and G. Arlet. 2006. DNA sequence analysis of the genetic environment of various _bla_CTX-M genes. J. Antimicrob. Chemother. 57**:**14-23. [DOI] [PubMed] [Google Scholar]
- 14.Hopkins, K. L., E. Liebana, L. Villa, M. Batchelor, E. J. Threlfall, and A. Carattoli. 2006. Replicon typing of plasmids carrying CTX-M or CMY β-lactamases circulating among Salmonella and Escherichia coli isolates. Antimicrob. Agents Chemother. 50**:**3203-3206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jacoby, G. A., and L. S. Munoz-Price. 2005. The new β-lactamases. N. Engl. J. Med. 352**:**380-391. [DOI] [PubMed] [Google Scholar]
- 16.Luzzaro, F., M. Mezzatesta, C. Mugnaioli, M. Perilli, S. Stefani, G. Amicosante, G. M. Rossolini, and A. Toniolo. 2006. Trends in production of extended-spectrum β-lactamases among enterobacteria of medical interest: report of the second Italian nationwide survey. J. Clin. Microbiol. 44**:**1659-1664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pacheco, A. B., B. E. Guth, K. C. Soares, L. Nishimura, D. F. de Almeida, and L. C. Ferreira. 1997. Random amplification of polymorphic DNA reveals serotype-specific clonal clusters among enterotoxigenic Escherichia coli strains isolated from humans. J. Clin. Microbiol. 35**:**1521-1525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pai, H., E. H. Choi, H. J. Lee, J. Y. Hong, and G. A. Jacoby. 2001. Identification of CTX-M-14 extended-spectrum β-lactamase in clinical isolates of Shigella sonnei, Escherichia coli, and Klebsiella pneumoniae in Korea. J. Clin. Microbiol. 39**:**3747-3749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pallecchi, L., M. Malossi, A. Mantella, E. Gotuzzo, C. Trigoso, A. Bartoloni, F. Paradisi, G. Kronvall, and G. M. Rossolini. 2004. Detection of CTX-M-type β-lactamase genes in fecal Escherichia coli isolates from healthy children in Bolivia and Peru. Antimicrob. Agents Chemother. 48**:**4556-4561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Park, C. H., A. Robicsek, G. A. Jacoby, D. Sahm, and D. C. Hooper. 2006. Prevalence in the United States of aac(6_′)-Ib-cr_ encoding a ciprofloxacin-modifying enzyme. Antimicrob. Agents Chemother. 50**:**3953-3955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Paterson, D. L., and R. A. Bonomo. 2005. Extended-spectrum β-lactamases: a clinical update. Clin. Microbiol. Rev. 18**:**657-686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Quinteros, M., M. Radice, N. Gardella, M. M. Rodriguez, N. Costa, D. Korbenfeld, E. Couto, G. Gutkind, and the Microbiology Study Group. 2003. Extended-spectrum β-lactamases in Enterobacteriaceae in Buenos Aires, Argentina, public hospitals. Antimicrob. Agents Chemother. 47**:**2864-2867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Radice, M., P. Power, J. Di Conza, and G. Gutkind. 2002. Early dissemination of CTX-M-derived enzymes in South America. Antimicrob. Agents Chemother. 46**:**602-604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Robicsek, A., G. A. Jacoby, and D. C. Hooper. 2006. The worldwide emergence of plasmid-mediated quinolone resistance. Lancet Infect. Dis. 6**:**629-640. [DOI] [PubMed] [Google Scholar]
- 25.Robicsek, A., J. Strahilevitz, D. F. Sahm, G. A. Jacoby, and D. C. Hooper. 2006. qnr prevalence in ceftazidime-resistant Enterobacteriaceae isolates from the United States. Antimicrob. Agents Chemother. 50**:**2872-2874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Robicsek, A., J. Strahilevitz, G. A. Jacoby, M. Macielag, D. Abbanat, C. H. Park, K. Bush, and D. C. Hooper. 2006. Fluoroquinolone-modifying enzyme: a new adaptation of a common aminoglycoside acetyltransferase. Nat. Med. 12**:**83-88. [DOI] [PubMed] [Google Scholar]
- 27.Rodriguez-Bano, J., M. D. Navarro, L. Romero, M. A. Muniain, M. de Cueto, M. J. Rios, J. R. Hernandez, and A. Pascual. 2006. Bacteremia due to extended-spectrum β-lactamase-producing Escherichia coli in the CTX-M era: a new clinical challenge. Clin. Infect. Dis. 43**:**1407-1414. [DOI] [PubMed] [Google Scholar]
- 28.Rodriguez-Bano, J., M. D. Navarro, L. Romero, M. A. Muniain, E. J. Perea, R. Perez-Cano, J. R. Hernandez, and A. Pascual. 2006. Clinical and molecular epidemiology of extended-spectrum β-lactamase-producing Escherichia coli as a cause of nosocomial infection or colonization: implications for control. Clin. Infect. Dis. 42**:**37-45. [DOI] [PubMed] [Google Scholar]
- 29.Sambrook, J., and D. W. Russell. 2001. Molecular cloning: a laboratory manual, 3rd ed. Cold Spring Harbor Laboratory Press, Cold Spring Harbor, NY.
- 30.Schwaber, M. J., S. Navon-Venezia, K. S. Kaye, R. Ben-Ami, D. Schwartz, and Y. Carmeli. 2006. Clinical and economic impact of bacteremia with extended-spectrum-β-lactamase-producing Enterobacteriaceae. Antimicrob. Agents Chemother. 50**:**1257-1262. [DOI] [PMC free article] [PubMed] [Google Scholar]