PKCλ in liver mediates insulin-induced SREBP-1c expression and determines both hepatic lipid content and overall insulin sensitivity (original) (raw)
Abstract
PKCλ is implicated as a downstream effector of PI3K in insulin action. We show here that mice that lack PKCλ specifically in the liver (L-λKO mice), produced with the use of the Cre-loxP system, exhibit increased insulin sensitivity as well as a decreased triglyceride content and reduced expression of the sterol regulatory element–binding protein-1c (SREBP-1c) gene in the liver. Induction of the hepatic expression of Srebp1c and of its target genes involved in fatty acid/triglyceride synthesis by fasting and refeeding or by hepatic expression of an active form of PI3K was inhibited in L-λKO mice compared with that in control animals. Expression of Srebp1c induced by insulin or by active PI3K in primary cultured rat hepatocytes was inhibited by a dominant-negative form of PKCλ and was mimicked by overexpression of WT PKCλ. Restoration of PKCλ expression in the liver of L-λKO mice with the use of adenovirus-mediated gene transfer corrected the metabolic abnormalities of these animals. Hepatic PKCλ is thus a determinant of hepatic lipid content and whole-body insulin sensitivity.
Introduction
The liver is essential for both carbohydrate and lipid homeostasis. Individuals with type 2 diabetes often exhibit impairment of insulin action in the liver (1), and liver-specific inhibition of insulin signaling in mice results in glucose intolerance and dyslipidemia (2), indicating the physiological importance of hepatic insulin action in energy homeostasis. Among the signaling molecules activated by insulin, PI3K plays a key role in the metabolic actions of this hormone (3, 4). Prevention of the insulin-induced activation of PI3K in the liver of mice thus results in glucose intolerance and dyslipidemia (5). However, the signaling molecules that function downstream of PI3K to mediate the metabolic actions of insulin in living animals have remained unclear.
Two atypical PKC (aPKC) isozymes, PKCλ and PKCζ (6), have been identified in mammals. We have previously shown that PKCλ acts downstream of PI3K in PDGF or insulin signaling in cultured cells (7, 8). Furthermore, evidence suggests that 3′-phosphoinositide–dependent kinase-1 (PDK-1), thought to be a key mediator of PI3K signaling, contributes to the activation of AGC protein kinases (which include Akt, p70 S6 kinase, p90rsk, and aPKC) by phosphorylating these enzymes on residues located in their activation loops (9, 10). On the basis of these various observations, we hypothesized that PKCλ participates in insulin action in vivo. To verify this hypothesis, using homologous recombination, we generated mice that harbor a PKCλ gene containing loxP sites. Disruption of the corresponding aPKC genes in Caenorhabditis elegans and Drosophila melanogaster resulted in embryonic death (11, 12). As expected, PKCλ-deficient mice generated from the floxed PKCλ transgenic animals also died during embryonic development (K. Akimoto et al., unpublished observations).
Given that the liver is one of the most important target organs of insulin, we next generated mice in which the floxed PKCλ gene was specifically deleted in the liver as a result of Cre recombinase expression in this organ. Characterization of these animals has now revealed that PKCλ mediates the regulatory effect of insulin on hepatic triglyceride content by contributing to the expression of the gene for sterol regulatory element–binding protein-1c (SREBP-1c), and that the lack of PKCλ in the liver results in increased insulin sensitivity.
Methods
Animals.
Mice harboring a floxed PKCλ gene in which exon 5 was flanked by loxP sequences (PKCλlox/+ mice) were generated by homologous recombination (K. Akimoto et al., unpublished observations). Mice that express Cre recombinase under the control of the albumin gene promoter (Alb-Cre mice) (13) were provided by D. LeRoith (Diabetes Branch, National Institute of Diabetes and Digestive and Kidney Diseases, NIH, Bethesda, Maryland, USA). We used only male mice for the present studies. For the fasting-refeeding experiments, mice in the fasted group were deprived of food for 24 hours; mice in the refed group were deprived of food for 24 hours and then allowed access to food for 12 hours before analysis. The liver X receptor agonist T0901317 (kindly provided by K. Murakami, Kyorin Pharmaceutical Co.,Tokyo, Japan) was administered daily by oral gavage at a dose of 10 mg/kg body mass for 4 days. For oral glucose intake experiments, mice deprived of food for 16 hours were loaded orally with glucose (2 g/kg body mass). For in vivo adenovirus-mediated gene transfer experiments, mice were injected with the indicated adenovirus vector (1 × 108 PFU) via the tail vein 72 hours before experiments.
Analysis of metabolic parameters.
Blood glucose and plasma insulin concentrations were determined as described (5). For glucose tolerance and insulin tolerance tests, mice deprived of food for 16 hours were injected intraperitoneally with glucose (2 g/kg body mass); mice in the randomly fed state were injected intraperitoneally with human regular insulin (0.75 U/kg). Serum leptin and adiponectin concentrations were measured with a mouse leptin ELISA kit (Morinaga Institute of Biological Science, Yokohama, Japan) and a mouse/rat adiponectin ELISA kit (Otsuka Pharmaceutical Co. Ltd., Tokyo, Japan), respectively. Serum cholesterol, triglyceride, and FFA concentrations were determined with a cholesterol C-II kit, a triglyceride G kit, and a NEFA C kit, respectively (Wako Pure Chemical Industries Ltd., Osaka, Japan). For assay of the cholesterol and triglyceride contents of liver or hind limb skeletal muscle, lipids were extracted from the tissue as described (14) and the concentrations of the analytes in the extract were determined with a cholesterol C-II kit or a triglyceride G kit.
Northern blot, immunoblot, kinase activity, real-time quantitative RT-PCR analyses, and primary culture of hepatocytes.
Total RNA (∼15 μg) was subjected to Northern blot analysis essentially as described (15); autoradiograms were visualized and signal intensity was quantitated with a BAS2000 image analyzer (Fujifilm Co., Tokyo, Japan). The probes for the genes encoding PPAR-α, acyl-CoA oxidase-1, and uncoupling protein-2 mRNA’s (mouse full-length cDNAs) were synthesized by PCR; the other probes were as described (5, 16, 17). Primary cultures of rat hepatocytes were prepared and subjected to adenovirus infection as described (15).
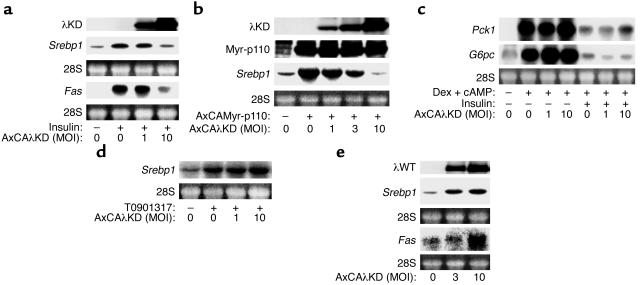
For assay of the expression of the genes encoding SREBP-1 and fatty acid synthase, cells infected or not with adenoviruses were incubated for 6 hours and 20 hours, respectively, with 100 nM insulin or with 10 μM T0901317; for assay of the expression of the genes encoding phosphoenolpyruvate carboxykinase-1 (PKC-1) and glucose-6-phosphatase catalytic subunit (G6PC), cells were incubated for 6 hours with 500 nM dexamethasone and 0.1 mM pCPT-cAMP in the absence or presence of 100 nM insulin. Adenovirus vectors encoding a dominant-negative mutant of PKCλ (AxCAλKD), WT PKCλ (AxCAλWT) (8), or a Myc epitope–tagged active form of PI3K (the 110-kDa catalytic subunit fused with a myristoylation signal sequence at its NH2-terminus; AxCAMyr-p110) (15, 18) were described previously, and that encoding β-gal (AxCALacZ) was kindly provided by I. Saito (University of Tokyo, Tokyo, Japan). The antibodies specific for mouse SREBP-1c were as described (14).
For assay of the abundance of PKCλ and PKCζ, total tissue homogenates were subjected to immunoprecipitation with antibodies to PKCλ (αλ190) or to PKCζ (αζ170) (8), and the resulting precipitates were subjected to immunoblot analysis with antibodies to PKCλ/ι (Transduction Laboratories, Lexington, Kentucky, USA) or to PKCζ (Life Technologies Inc., Rockville, Maryland, USA), respectively. Antibodies that recognize both PKCλ and PKCζ (C-20, a rabbit polyclonal antibody, and C-20-G, a goat polyclonal antibody) were obtained from Santa Cruz Biotechnology (Santa Cruz, California, USA). For immunodepletion of aPKC, liver homogenates were subjected to three sequential immunoprecipitations for 120 minutes with αλ190 or with αζ170. The supernatants of the immunoprecipitations were then subjected to immunoprecipitation with C-20-G and the precipitates were subjected to immunoblot analysis with C-20. The kinase activity of aPKC was assayed in the immunoprecipitates with αλ190 or with αζ170 as described previously (8). For real-time quantitative reverse transcription and PCR analysis, cDNA synthesized from total RNA was evaluated in a sequence detector (model 7900; Applied Biosystems, Foster City, California, USA) with specific primers and SYBR Green PCR Master Mix (Applied Biosystems). The relative abundance of mRNA’s was calculated with 36B4 mRNA as the invariant control. The primers used were as follows: mouse Srebp1a, 5′-GGAACAGACACTGGCCGAGA-3′ (sense) and 5′-GCATAGGGGGCGTCA-3′ (antisense); mouse Srebp1c, 5′-ATCGGCGCGGAAGCTGTCGGGGTAGCGTC-3′ (sense) and 5′-ACTGTCTTGGTTGTTGATGAGCTGGAGCAT-3′ (antisense). The primers for mouse 36B4 were as described previously (5).
Results
Generation of mice with liver-specific deficiency of PKCλ.
We bred PKCλlox/+ mice with Alb-Cre mice (13). We then bred the PKCλlox/+, Alb-Cre offspring of this cross with PKCλlox/+ mice. The offspring of this breeding were born in a Mendelian ratio (PKCλ+/+, n = 12, or 9.9%; PKCλ+/+, Alb-Cre, n = 14, or 11.6%; PKCλlox/+, n = 29, or 24.0%; PKCλlox/+, Alb-Cre, n = 33, or 27.3%; PKCλlox/lox, n = 15, or 12.4%; PKCλlox/lox, Alb-Cre, n = 18, or 14.9%).
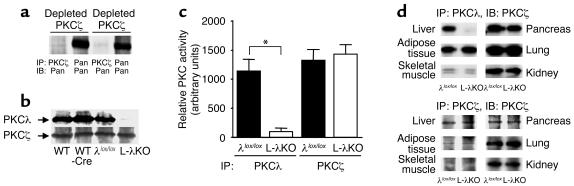
Two closely related isoforms comprise aPKC: PKCλ and PKCζ (6). We first investigated the amounts of PKCλ and PKCζ in liver homogenates of PKCλ+/+ (WT) mice. After three sequential immunoprecipitations with antibodies to PKCλ or to PKCζ, the corresponding isoforms of aPKC were almost completely depleted from the homogenates (Figure 1a). aPKC protein, detected by antibodies that recognize both PKCλ and PKCζ, was present both in the PKCλ -depleted and the PKCζ-depleted homogenates, suggesting that liver contains both PKCλ and PKCζ. The relative abundance of each isoform was comparable. The amount of PKCλ in the liver of PKCλlox/lox, Alb-Cre (L-λKO) mice was markedly reduced compared with that in the liver of WT, PKCλ+/+, Alb-Cre (WT-Cre), and PKCλlox/lox (λlox/lox) animals (Figure 1b). In contrast, the hepatic abundance of PKCζ was similar among all four genotypes of mice.
Figure 1.
The abundance and kinase activity of PKCλ and PKCζ in mice with liver-specific PKCλ deficiency. (a) Total homogenates prepared from the liver of 20-week-old PKCλ+/+ mice were subjected to three sequential immunoprecipitations with antibodies to PKCλ (depleted PKCλ) or to PKCζ (deplete PKCζ). The resultant supernatants were subjected to immunoprecipitation with antibodies to PKCλ, to PKCζ, or with antibodies that recognize both PKCλ and PKCζ (Pan), and the precipitates were subjected to immunoblot analysis with antibodies that recognize both PKCλ and PKCζ (Pan). (b) Total homogenates prepared from the liver of 18-week-old PKCλ+/+ (WT); PKCλ+/+, Alb-Cre (WT-Cre); PKCλlox/lox (λlox/lox); or PKCλlox/lox, Alb-Cre (L-λKO) mice were subjected to immunoprecipitation with antibodies to PKCλ or to PKCζ, and the resulting precipitates were subjected to immunoblot analysis with corresponding antibodies. (c) Total homogenates prepared from the liver of λlox/lox or L-λKO mice were subjected to immunoprecipitation (IP) with antibodies to PKCλ or to PKCζ, and the resulting precipitates were assayed for kinase activity. (d) Extracts of the indicated tissues prepared from λlox/lox or L-λKO mice were subjected to immunoprecipitation with antibodies to PKCλ or to PKCζ, and the resulting precipitates were subjected to immunoblot analysis (IB) with corresponding antibodies. Data in a, b, and d are representative of at least three mice of each genotype; those in c are mean ± SEM of values from six mice. *P < 0.01 for the indicated comparison (ANOVA).
Given the similarity in the hepatic expression level of PKCλ in WT, WT-Cre, and λlox/lox mice, which indicates that neither the insertion of the loxP sequences in the PKCλ gene nor the expression of Cre recombinase alone affected the abundance of PKCλ, we performed subsequent experiments with L-λKO and λlox/lox mice. The kinase activity of PKCλ, but not that of PKCζ, was greatly reduced in the liver of L-λKO mice compared with that in the liver of λlox/lox mice (Figure 1c). The abundance of PKCλ in other tissues, including skeletal muscle, adipose tissue, the pancreas, the lung, and the kidney, did not differ between L-λKO and λlox/lox mice (Figure 1d). The abundance of PKCζ in the two genotypes of mice was similar in all tissues we examined. The gross appearance and histology of the liver, including the arrangement of hepatocytes in plates and the structure of hepatic lobules, appeared normal in L-λKO mice (data not shown). The serum levels of aspartate aminotransferase, alanine aminotransferase, alkaline phosphatase, lactate dehydrogenase, and albumin also did not differ significantly between L-λKO and λlox/lox mice (data not shown). These results indicate that the lack of PKCλ did not affect the development or general function of the liver.
Metabolic characteristics of L-λKO mice.
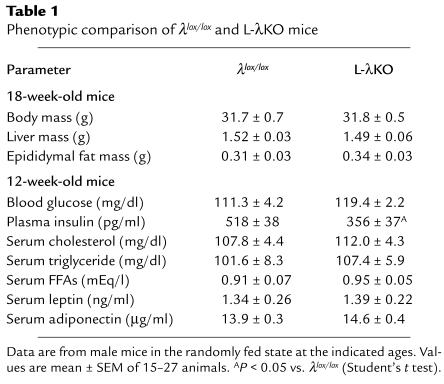
The body mass, mass of the liver, and mass of epididymal fat tissue of L-λKO mice were similar to those of λlox/lox mice (Table 1). The serum concentrations of triglyceride, cholesterol, FFAs, leptin, and adiponectin in the randomly fed state also did not differ between mice of the two genotypes. Although the blood glucose concentration in the randomly fed state was similar in the two types of mice, the plasma concentration of insulin in L-λKO mice was significantly lower than that in λlox/lox mice. Blood glucose concentrations during a glucose tolerance test were similar in both L-λKO and λlox/lox mice (Figure 2a). Again, however, the increase in plasma insulin concentration induced by glucose intake was smaller in L-λKO mice than in λlox/lox animals (Figure 2b). Moreover, the glucose-lowering effect of exogenously administered insulin was exaggerated in L-λKO mice (Figure 2c). These observations indicated that the insulin sensitivity of L-λKO mice was increased.
Table 1.
Phenotypic comparison of λlox/lox and L-λKO mice
Figure 2.
Glucose and insulin tolerance, insulin signaling, and hepatic gene expression in mice with liver-specific deficiency of PKCλ. (a–c) Blood glucose (a) and plasma insulin (b) concentrations during a glucose-tolerance test in L-λKO and λlox/lox mice at 14 weeks of age, and blood glucose concentration during an insulin tolerance test at 12 weeks of age (c). Data are mean ± SEM of values from nine to 20 mice. *P < 0.05 vs. the corresponding value for λlox/lox mice (Student’s t test). (d) Tyrosine phosphorylation of IRS-1 and IRS-2 and serine phosphorylation of Akt in the liver of λlox/lox or L-λKO mice induced by a bolus injection of insulin. Liver homogenates prepared 2 minutes after administration of insulin (5 U/kg of body mass) or saline were subjected to immunoprecipitation with antibodies to IRS-1 or to IRS-2, and the resulting precipitates were subjected to immunoblot analysis with antibodies to phosphotyrosine (PY). Alternatively, liver homogenates were subjected directly to immunoblot analysis with antibodies specific for phosphorylated Akt (p-Akt). Data are representative of six mice of each genotype. (e–g) Total RNA extracted from the liver of λlox/lox or L-λKO mice (18 weeks of age) in the randomly fed state (n = 8) (e) or after fasting with or without refeeding (n = 4–7) (f and g) was either separately combined and subjected to Northern blot analysis (e and f) or subjected individually to RT-PCR analysis (g) for the indicated mRNA’s. Ethidium bromide staining of 28S rRNA is also shown for Northern analysis. *P < 0.01 (ANOVA). (h) The nuclear fraction of liver homogenates prepared from λlox/lox or L-λKO mice after fasting with or without refeeding was subjected to immunoblot analysis with antibodies to SREBP-1c. Data shown are from two mice and are representative of four to six animals. (i and j) Mice (λlox/lox or L-λKO) 16–18 weeks of age (n = 10–16) were injected with AxCAMyr-p110 or AxCALacZ and were subsequently deprived of food for 16 hours. The abundance of Myr-p110 in liver homogenates was then examined by immunoblot analysis with antibodies to Myc (i, upper panel), blood glucose concentration was determined (i, lower panel), and the amounts of Srebp1 and Fas mRNA’s among separately combined total RNA extracted from the liver were evaluated by Northern analysis (j). *P < 0.05, **P < 0.01 (ANOVA). (k) Total RNA extracted from the liver of λlox/lox or L-λKO mice treated with either T0901317 or vehicle was separately combined and subjected to Northern blot analysis for Srebp1 and Fas mRNA’s. Data are shown for two mice and are representative of four animals.
Altered hepatic gene expression in L-λKO mice.
Early events of hepatic insulin signaling, including phosphorylation of insulin receptor substrate-1 (IRS-1), IRS-2, and Akt, did not differ between L-λKO and λlox/lox mice after bolus injection of insulin (Figure 2d). We have previously shown that PKCλ contributes to PI3K-dependent gene expression induced by growth factors (7). We therefore examined L-λKO mice for the hepatic expression of genes that are regulated by insulin. The abundance of mRNA’s for glucokinase (GCK), PKC-1, and G6PC in the liver of randomly fed animals was similar in L-λKO and λlox/lox mice (Figure 2e). However, the amount of transcripts encoding SREBP-1, a transcription factor that regulates the expression of genes important in triglyceride synthesis (19, 20), as well as the amount of those encoding fatty acid synthase, the gene for which is regulated by SREBP-1 (19, 20), were reduced by approximately 50% in the liver of L-λKO mice.
The expression of Srebp1 and its target genes in the liver is induced when mice are refed after starvation (21, 22), a treatment that also results in an increase in the circulating insulin concentration. The increases in the hepatic expression of Srebp1, Fas, and the gene for stearoyl-CoA desaturase-1 (SCD-1; another target of SREBP-1) (19) induced by refeeding were inhibited by about 50%, 35%, and 25%, respectively, in L-λKO mice (Figure 2f). Of the two splice variants of Srebp1 mRNA (19), only the abundance of Srebp1c mRNA, not that of Srebp1a mRNA, is increased in the liver in response to insulin or refeeding (22). The induction of Srebp1c expression in the liver in response to refeeding was inhibited by about 50% in L-λKO mice (Figure 2g). Moreover, immunoblot analysis with antibodies specific for SREBP-1c (14) revealed that the increase in the amount of this protein in a nuclear fraction of the liver induced by refeeding was markedly reduced in L-λKO mice (Figure 2h).
We and other investigators have shown that the effect of insulin on the expression of Srebp1 is mediated by a PI3K-dependent pathway (15, 23). We therefore next took advantage of the fact that systemic infusion of adenoviral vectors results in liver-specific expression of exogenous genes (5). Infusion of AxCAMyr-p110, but not of AxCALacZ, resulted in the expression of the Myr-p110 protein in the liver of both L-λKO and λlox/lox mice (Figure 2i); expression of Myr-p110 was not detected in skeletal muscle or adipose tissue (data not shown). Infusion of AxCAMyr-p110, but not of AxCALacZ, also resulted in a reduction in the blood glucose concentration of both L-λKO and λlox/lox mice in the fasted state, suggesting that activation of hepatic PI3K signaling lowers blood glucose concentration. However, the glucose-lowering effect of AxCAMyr-p110 was greater in L-λKO mice than in the control animals, consistent with our observation that the glucose-lowering effect of exogenously administered insulin was exaggerated in L-λKO mice.
Although the hepatic expression of Srebp1 and Fas was induced by the infusion of AxCAMyr-p110 in both L-λKO and λlox/lox mice (Figure 2j), the extent of this effect was greatly reduced in the former animals, indicating that PKCλ functions as a downstream effector of PI3K in the induction of Srebp1c expression in the liver. Activation of the liver X receptor also increases the expression of Srebp1c in the liver (16, 24). The hepatic expression of Srebp1 and Fas induced by gavage with T0901317, a liver X receptor agonist (24), was similar in L-λKO and λlox/lox mice (Figure 2k), suggesting that the lack of PKCλ does not affect the general machinery responsible for the induction of Srebp1c but rather results in a specific disruption in PI3K-dependent signaling that leads to increased expression of this gene.
Hepatic lipid content and expression of genes important in β-oxidation in L-λKO mice.
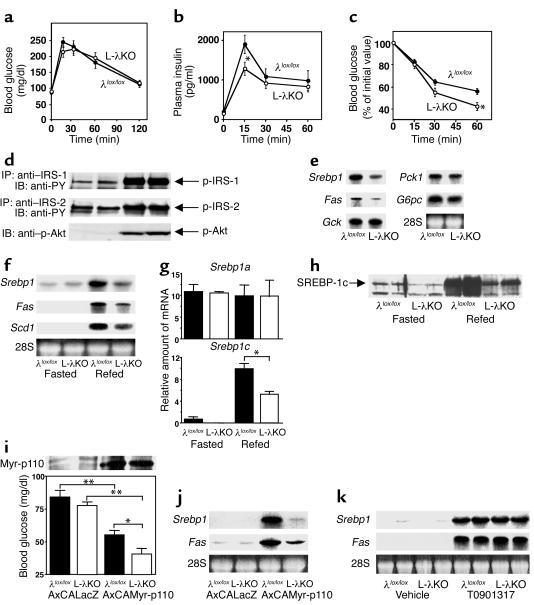
The triglyceride content of the liver was reduced (Figure 3a), whereas the hepatic cholesterol content (Figure 3b) and the triglyceride content of skeletal muscle (Figure 3c) were unchanged in L-λKO mice in the randomly fed state compared with the corresponding values for λlox/lox mice. The synthesis and breakdown (β-oxidation) of triglyceride are the two major determinants of hepatic triglyceride content. The expression of genes that contribute to the oxidation of triglyceride in the liver, including those encoding PPAR-α, acyl-CoA oxidase-1, and uncoupling protein-2, did not differ between L-λKO and λlox/lox mice in the randomly fed state (Figure 3d), suggesting that the reduced hepatic triglyceride content of L-λKO mice is attributable to the reduced expression of Srebp1c.
Figure 3.
Hepatic lipid and glycogen content and the expression of genes involved in β-oxidation and gluconeogenesis in mice with liver-specific PKCλ deficiency. (a–c) Triglyceride (a) and cholesterol (b) content of the liver and triglyceride content of hind limb muscle (c) of L-λKO and λlox/lox mice in the randomly fed state at 18 weeks of age. Data are expressed as mg analyte/g wet tissue and are the mean ± SEM from seven mice. *P < 0.05 (Student’s t test). (d) Total RNA extracted from the liver of λlox/lox or L-λKO mice (n = 8) at 18 weeks of age and in the randomly fed state was separately combined and subjected to Northern blot analysis for mRNA’s encoding PPAR-α, acyl-CoA oxidase-1 (ACOX-1), and uncoupling protein-2 (UCP-2). (e) Hepatic glycogen content of λlox/lox or L-λKO mice at 20 weeks of age before (Pre) and 2 hours after (Post) oral glucose intake. Data are mean ± SEM from four to six mice. (f) Total RNA extracted from the liver of λlox/lox or L-λKO mice (18 weeks of age) after fasting with or without refeeding (n = 4–7) was separately combined and subjected to Northern blot analysis with probes specific for Pck1 or G6pc mRNA’s.
Hepatic accumulation of glycogen and the induction of Pck1 and G6pc by starvation/refeeding in L-λKO mice.
The hepatic glycogen content in the randomly fed state (data not shown) and the increase in hepatic glycogen content in response to oral glucose intake (Figure 3e) were similar in L-λKO and λlox/lox mice. The expression of Pck1 and G6pc in the liver is inhibited by refeeding after food deprivation. The effect of refeeding on the hepatic expression of these genes was slightly exaggerated in L-λKO mice compared with that apparent in λlox/lox animals (Figure 3f). These results thus suggested that PKCλ signaling is not required for either the hepatic accumulation of glycogen or for inhibition of the expression of gluconeogenesis genes in the liver. The slight enhancement of refeeding-induced suppression of Pck1 and G6pc expression apparent in L-λKO mice may be related to the increased insulin sensitivity of these animals.
Effects of dominant-negative and WT PKCλ on insulin-induced expression of Srebp1 in cultured hepatocytes.
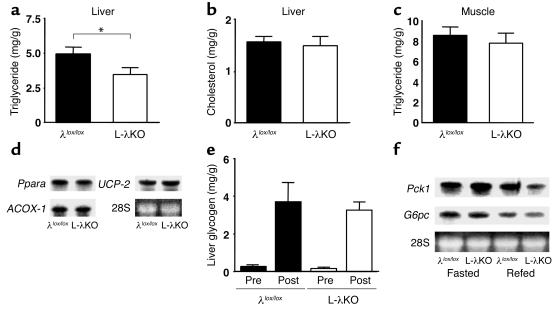
To confirm a causal relation between PKCλ deficiency and the altered hepatic expression of Srebp1 in L-λKO mice, we examined the effect of PKCλ signaling on the abundance of Srebp1 mRNA in primary cultures of rat hepatocytes. Incubation of the cells with insulin induced an increase in the amounts of Srebp1 and Fas mRNA’s (Figure 4a), and this effect was inhibited by adenovirus-mediated expression of λKD, which acts in a dominant-negative manner (7, 8). Expression of λKD also inhibited the increase in the amount of Srebp1 mRNA induced by Myr-p110 (Figure 4b). In contrast, λKD did not affect either the insulin-induced inhibition of Pck1 and G6pc expression (Figure 4c) or the expression of Srebp1 induced by T0901317 (Figure 4d), indicating that PKCλ signaling specifically contributes to insulin-induced expression of Srebp1. Moreover, expression of recombinant WT PKCλ increased the abundance of Srebp1 and Fas mRNA’s in the absence of insulin (Figure 4e), indicating that PKCλ signaling is sufficient for the induction of these genes.
Figure 4.
Effects of dominant-negative and WT PKCλ on the expression of Srebp1, Fas, Pck1, and G6pc in primary cultured rat hepatocytes. (a, c, and d) Cells that had been infected (or not) with an adenoviral vector for a dominant-negative form of PKCλ (AxCAλKD) at the indicated MOI (in PFU/cell) were incubated in the absence or presence of insulin, dexamethasone (Dex), or T0901317, plus pCPT-cAMP (these two agents were used to induce the expression of Pck1 and G6pc), as indicated. Total cell lysates were then subjected to immunoblot analysis with antibodies to PKCλ, and total RNA extracted from the cells was subjected to Northern blot analysis with probes specific for Srebp1, Fas, Pck1, or G6pc mRNA’s. (b) Cells that had been infected (or not) with an adenovirus encoding a constitutively active form of PI3K (AxCAMyr-p110) at an MOI of three plaque-forming units/cell were then infected with AxCAλKD at the indicated MOI. Total cell lysates were subjected to immunoblot analysis with antibodies to PKCλ or to Myc (for the detection of Myr-p110), and total RNA extracted from the cells was subjected to Northern blot analysis with a probe specific for Srebp1 mRNA. (e) Cells were infected (or not) with an adenovirus encoding WT PKCλ (AxCAλWT) at the indicated MOI, after which cell lysates were subjected to immunoblot analysis with antibodies to PKCλ and total RNA extracted from the cells was subjected to Northern blot analysis with probes specific for Srebp1 or Fas mRNAs. All data are representative of at least three independent experiments.
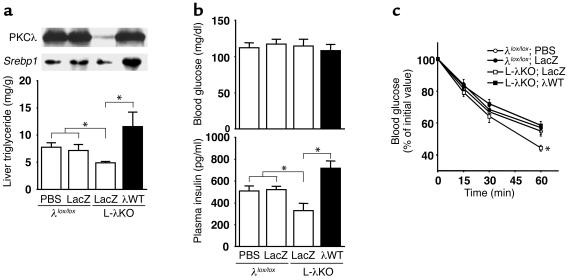
Restoration of PKCλ expression reverses the decrease in hepatic lipid content and the increase in insulin sensitivity in L-λKO mice. To verify that the altered insulin sensitivity and hepatic triglyceride content of L-λKO mice are attributable to the lack of PKCλ in the liver, we restored the hepatic expression of this enzyme in L-λKO animals. Infusion of AxCAλWT into L-λKO mice resulted in the expression of PKCλ in the liver at a level similar to that apparent in λlox/lox mice (Figure 5a). The restoration of PKCλ expression in the liver increased both the abundance of Srebp1 mRNA and the triglyceride content in this organ of L-λKO mice. Blood glucose concentration was similar in L-λKO mice infused with AxCAλWT or with AxCALacZ and in λlox/lox mice infused with AxCALacZ or with PBS. The plasma insulin concentration of L-λKO mice was increased by infusion of AxCAλWT, but not of AxCALacZ, to an extent similar to that apparent in λlox/lox mice infused with AxCALacZ or with PBS (Figure 5b). Moreover, the enhancement of the glucose-lowering effect of exogenously administered insulin apparent in L-λKO mice was also reversed by restoration of PKCλ expression in the liver (Figure 5c). These results thus indicate that the changes in the expression of Srebp1 and in triglyceride content in the liver as well as in whole-body insulin sensitivity apparent in L-λKO mice are directly attributable to the lack of PKCλ in the liver.
Figure 5.
Effects of adenovirus-mediated restoration of PKCλ expression in the liver of mice with liver-specific PKCλ deficiency on hepatic lipid content, expression of Srebp1 in the liver, and insulin sensitivity. (a) Twenty-week-old λlox/lox or L-λKO mice (n = 7–9) were injected with PBS or with adenoviruses encoding either β-gal (LacZ) or WT PKCλ (λWT), as indicated. Total liver homogenates were subsequently subjected to immunoprecipitation and immunoblot analysis with antibodies to PKCλ (upper panel; data are representative of three experiments). Total RNA extracted from the liver was separately combined and subjected to Northern blot analysis with a probe specific for Srebp1 mRNA (middle panel), and hepatic triglyceride content was determined (lower panel; data are shown as mean ± SEM). *P < 0.05 (ANOVA). (b and c) Twelve-week-old λlox/lox or L-λKO mice were injected with PBS or with adenoviruses encoding either β-gal or WT PKCλ, after which blood glucose and plasma insulin concentrations were determined in the randomly fed state (b) or an insulin tolerance test was performed (c). Data represent mean ± SEM from six to ten mice. *P < 0.05 for the indicated comparisons (b) or for the comparison of L-λKO mice injected with the adenovirus encoding β-gal vs. all other conditions.
Discussion
On the basis of observations with cultured cells (7, 8), we hypothesized that PKCλ participates in insulin action in vivo as a downstream effector of PI3K. Our present results now demonstrate such a function for PKCλ, at least in the liver. Several of the metabolic effects of insulin in the liver are exerted through the regulation of gene expression. We have previously shown that the regulation by insulin of the expression of Gck, Srebp1c, G6pc, and Pck1 in mouse liver is mediated by PI3K (5). Of these four genes, each of which participates in the metabolic actions of insulin, we have now revealed that the expression of Srebp1c, a key regulator of fatty acid and triglyceride synthesis (19, 20), is regulated by PKCλ acting downstream of PI3K. At present, a signaling pathway that links PKCλ and the expression of Srebp1c remains unclear. Cycloheximide, an inhibitor of general protein synthesis, has been shown to prevent insulin-induced expression of Srebp1c in cultured hepatocytes (25), suggesting that de novo protein synthesis is required for this action of insulin. PKCλ thus may contribute to induce expression of such a protein involved in the transcriptional activation of Srebp1c.
The hepatic expression of Srebp1c induced by refeeding or by an active PI3K was markedly, but not completely, prevented in L-λKO mice, suggesting that the induction of Srebp1c is not solely dependent on PKCλ signaling. Given that the liver expresses both PKCλ and PKCζ, PKCζ may be responsible for the residual signaling of Srebp1c. A membrane-targeted form of Akt that exhibits higher kinase activity than does WT Akt increases the abundance of Srebp1c mRNA when it is expressed in primary cultured hepatoyctes (23), suggesting that Akt, a downstream effector of PI3K, may also contribute to the induction of Srebp1c. However, we have previously shown that the inhibition of endogenous Akt activity with the use of a dominant-negative mutant of the kinase did not prevent, but rather augmented, insulin-induced expression of Srebp1c (15). Moreover, in ob/ob mice and a mouse model with lipodystrophic diabetes, the abundance of Srebp1c mRNA is increased, whereas insulin-induced phosphorylation of Akt is markedly reduced in the liver of these animals (26). Mice lacking Akt2, a major isoform of Akt in the liver, have been established (27). The physiological importance of Akt in the induction of Srebp1c in vivo may be revealed by characterization of the mutant mice.
Atypical PKC isozymes are evolutionarily conserved proteins required for the formation of apical-basal polarity in cells (28), which is important for the structural organization and function of organs. However, the structures of hepatic lobules and hepatocyte plates and the serum parameters of general liver function appeared normal in L-λKO mice. This observation may be attributable to the fact that disruption of the PKCλ gene was accomplished by Cre recombinase expressed under the control of the promoter of the albumin gene, which is a marker gene of fully differentiated hepatocytes. A role for PKCλ in the development of cellular polarity in the liver might be revealed by characterization of hepatectomy-induced liver regeneration in L-λKO mice, given that the liver regenerates predominantly through the replication of mature hepatocytes under this experimental condition (29).
An unexpected finding of the present study was that L-λKO mice exhibit increased insulin sensitivity. The tissue-specific disruption of a gene important for insulin signaling thus paradoxically resulted in an increase in whole-body insulin sensitivity. A similar phenomenon has been observed with mice lacking the insulin receptor specifically in adipose tissue (30). Restoration of the hepatic expression of PKCλ reversed this metabolic phenotype of L-λKO mice, indicating that the lack of PKCλ in the liver is indeed responsible for the increased insulin sensitivity of these animals. The precise mechanism that underlies this phenomenon remains unclear. Evidence suggests that the alteration of fatty acids/triglyceride metabolism in insulin’s target tissues is an important determinant of insulin sensitivity. The increase in circulating FFAs leads to insulin resistance and the accumulation of triglyceride in skeletal muscle (31), and triglyceride content in the liver or in skeletal muscle negatively correlates with insulin sensitivity in humans (32, 33). Leptin and adiponectin, the two major fat-derived hormones, increase insulin sensitivity and concomitantly reduce hepatic triglyceride content (probably by promoting fatty acid oxidation) in an animal model of insulin resistance or in humans with lipodystrophic diabetes (34–36). Moreover, overexpression of lipoprotein lipase in liver or skeletal muscle resulted in an increase in fatty acid metabolites and consequently in the accumulation of triglyceride in the respective tissue, as well as insulin resistance (37). The decrease in the hepatic expression of the lipogenic genes and the subsequent alterations in fatty acid metabolism in L-λKO mice may thus be related to the increased insulin sensitivity of these animals.
TNF-α secreted from adipose tissue is implicated in the development of obesity-induced insulin resistance (38). Atypical PKC is activated by cytokines, including TNF-α and IL-1 (39, 40), and directly phosphorylates and activates I-κB kinase-β (IKKβ) (41). Administration of salicylic acid derivatives that inhibit IKKβ (42) was shown to increase insulin sensitivity both in rodent models of diabetes and in human subjects (43, 44). Moreover, heterozygous disruption of the IKKβ gene ameliorated the insulin resistance of obese model mice (44). It is therefore possible that the hepatic deficiency of PKCλ in L-λKO mice results in inhibition of a TNF-α/PKCλ/IKKβ signaling pathway and a consequent increase in whole-body insulin sensitivity.
Transgenic mice that overexpress lipoprotein lipase in skeletal muscle or the liver exhibit an impairment of the insulin-induced increase in PI3K activity associated with IRS-1 or IRS-2, respectively (37). Moreover, administration of salicylic acid derivatives enhanced insulin-induced tyrosine phosphorylation of the insulin receptor in genetically obese animals (44). However, we did not detect changes in the insulin-induced phosphorylation of IRS proteins or of Akt in the liver of L-λKO mice. Although we cannot exclude the possibility that a small increase in the extent of insulin signaling went undetected under our experimental conditions, it is possible that the enhancement of insulin action apparent in L-λKO mice occurs at a step other than IRS or Akt phosphorylation. Evidence suggests that PKCζ participates in a negative feedback pathway of insulin signaling leading to the phosphorylation of IRS proteins in cultured cells (45). Given that the insulin-induced phosphorylation of IRS proteins was not significantly increased in the liver of L-λKO mice, PKCλ appears not to participate in such a negative feedback pathway in mouse liver.
In summary, we have shown that, among the various metabolic actions of insulin, PKCλ specifically contributes to induction of the expression of Srebp1c and of its target genes important in triglyceride synthesis in the liver. Animal models of insulin resistance or obesity often manifest increases both in lipid content and in the expression of Srebp1c in the liver (26, 46). Reagents that block PKCλ signaling specifically in the liver might thus prove effective for reducing hepatic Srebp1c expression and consequently hepatic triglyceride content, as well as for ameliorating insulin resistance.
Acknowledgments
We thank D. LeRoith, T. Noguchi, H. Nakajima, N. Iritani, D.K. Granner, and K. Murakami for Alb-Cre mice, probes for Gck, G6pc, Fas, and Pck1, and for T0901317, respectively. This work was supported by a grant from the Ministry of Education, Culture, Sports, Science, and Technology of Japan (to M. Kasuga and W. Ogawa), a grant-in-aid for the Research for the Future Program from the Japan Society for the Promotion of Science (to M. Kasuga), and a grant from Cooperative Link of Unique Science and Technology for Economy Revitalization (CLUSTER) (to M. Kasuga).
Footnotes
Conflict of interest: The authors have declared that no conflict of interets exists.
Nonstandard abbreviations used: atypical PKC (aPKC); sterol regulatory element–binding protein-1c (SREBP-1c); glucose-6-phosphatase catalytic subunit (G6PC); insulin receptor substrate (IRS); glucokinase (GCK); I-κB kinase-β (IKKβ).
References
- 1.DeFronzo RA. Pathogenesis of type 2 diabetes: metabolic and molecular implications for identifying diabetic genes. Diabetes Rev. 1997;5:177–269. [Google Scholar]
- 2.Michael MD, et al. Loss of insulin signaling in hepatocytes leads to severe insulin resistance and progressive hepatic dysfunction. Mol. Cell. 2000;6:87–97. [PubMed] [Google Scholar]
- 3.Ogawa W, Matozaki T, Kasuga M. Role of binding proteins to IRS-1 in insulin signalling. Mol. Cell. Biochem. 1998;182:13–22. [PubMed] [Google Scholar]
- 4.Shepherd PR, Withers DJ, Siddle K. Phosphoinositide 3-kinase: the key switch mechanism in insulin signalling. Biochem. J. 1998;333:471–490. doi: 10.1042/bj3330471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Miyake K, et al. Hyperinsulinemia, glucose intolerance, and dyslipidemia induced by acute inhibition of phosphoinositide 3-kinase signaling in the liver. J. Clin. Invest. 2002;110:1483–1491. doi:10.1172/JCI200215880. doi: 10.1172/JCI15880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Suzuki A, Akimoto K, Ohno S. Protein kinase C λ/ι (PKC λ/ι): a PKC isoform essential for the development of multicellular organisms. J. Biochem. (Tokyo). 2003;133:9–16. doi: 10.1093/jb/mvg018. [DOI] [PubMed] [Google Scholar]
- 7.Akimoto K, et al. EGF or PDGF receptors activate atypical PKCλ through phosphatidylinositol 3-kinase. EMBO J. 1996;15:788–798. [PMC free article] [PubMed] [Google Scholar]
- 8.Kotani K, et al. Requirement of atypical protein kinase Cλ for insulin stimulation of glucose uptake but not for Akt activation in 3T3-L1 adipocytes. Mol. Cell. Biol. 1998;18:6971–6982. doi: 10.1128/mcb.18.12.6971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Williams MR, et al. The role of 3-phosphoinositide-dependent protein kinase 1 in activating AGC kinases defined in embryonic stem cells. Curr. Biol. 2000;10:439–448. doi: 10.1016/s0960-9822(00)00441-3. [DOI] [PubMed] [Google Scholar]
- 10.Le Good JA, et al. Protein kinase C isotypes controlled by phosphoinositide 3-kinase through the protein kinase PDK1. Science. 1998;281:2042–2045. doi: 10.1126/science.281.5385.2042. [DOI] [PubMed] [Google Scholar]
- 11.Tabuse Y. Atypical protein kinase C cooperates with PAR-3 to establish embryonic polarity in Caenorhabditis elegans. Development. 1998;125:3607–3614. doi: 10.1242/dev.125.18.3607. [DOI] [PubMed] [Google Scholar]
- 12.Wodarz A, Ramrath A, Grimm A, Knust E. Drosophila atypical protein kinase C associates with Bazooka and controls polarity of epithelia and neuroblasts. J. Cell Biol. 2000;150:1361–1374. doi: 10.1083/jcb.150.6.1361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yakar S, et al. Normal growth and development in the absence of hepatic insulin-like growth factor I. Proc. Natl. Acad. Sci. U. S. A. 1999;96:7324–7329. doi: 10.1073/pnas.96.13.7324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yahagi N, et al. A crucial role of sterol regulatory element-binding protein-1 in the regulation of lipogenic gene expression by polyunsaturated fatty acids. J. Biol. Chem. 1999;274:35840–35844. doi: 10.1074/jbc.274.50.35840. [DOI] [PubMed] [Google Scholar]
- 15.Matsumoto M, et al. Role of the insulin receptor substrate 1 and phosphatidylinositol 3-kinase signaling pathway in insulin-induced expression of sterol regulatory element binding protein 1c and glucokinase genes in rat hepatocytes. Diabetes. 2002;51:1672–1680. doi: 10.2337/diabetes.51.6.1672. [DOI] [PubMed] [Google Scholar]
- 16.Repa JJ, et al. Regulation of mouse sterol regulatory element-binding protein-1c gene (SREBP-1c) by oxysterol receptors, LXRα and LXRβ. Genes Dev. 2000;14:2819–2830. doi: 10.1101/gad.844900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Katsurada A, et al. Effects of nutrients and hormones on transcriptional and post-transcriptional regulation of fatty acid synthase in rat liver. Eur. J. Biochem. 1990;190:427–433. doi: 10.1111/j.1432-1033.1990.tb15592.x. [DOI] [PubMed] [Google Scholar]
- 18.Kitamura T, et al. Insulin-induced phosphorylation and activation of cyclic nucleotide phosphodiesterase 3B by the serine-threonine kinase Akt. Mol. Cell. Biol. 1999;19:6286–6296. doi: 10.1128/mcb.19.9.6286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Horton JD, Goldstein JL, Brown MS. SREBPs: activators of the complete program of cholesterol and fatty acid synthesis in the liver. J. Clin. Invest. 2002;109:1125–1131. doi:10.1172/JCI200215593. doi: 10.1172/JCI15593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shimano H, et al. Sterol regulatory element-binding protein-1 as a key transcription factor for nutritional induction of lipogenic enzyme genes. J. Biol. Chem. 1999;274:35832–35839. doi: 10.1074/jbc.274.50.35832. [DOI] [PubMed] [Google Scholar]
- 21.Horton JD, Bashmakov Y, Shimomura I, Shimano H. Regulation of sterol regulatory element binding proteins in livers of fasted and refed mice. Proc. Natl. Acad. Sci. U. S. A. 1998;95:5987–5992. doi: 10.1073/pnas.95.11.5987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shimomura I, et al. Insulin selectively increases SREBP-1c mRNA in the livers of rats with streptozotocin-induced diabetes. Proc. Natl. Acad. Sci. U. S. A. 1999;96:13656–13661. doi: 10.1073/pnas.96.24.13656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fleischmann M, Iynedjian PB. Regulation of sterol regulatory-element binding protein 1 gene expression in liver: role of insulin and protein kinase B/cAkt. Biochem. J. 2000;349:13–17. doi: 10.1042/0264-6021:3490013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schultz JR, et al. Role of LXRs in control of lipogenesis. Genes Dev. 2000;14:2831–2838. doi: 10.1101/gad.850400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Foretz M, et al. ADD1/SREBP-1c is required in the activation of hepatic lipogenic gene expression by glucose. Mol. Cell. Biol. 1999;19:3760–3768. doi: 10.1128/mcb.19.5.3760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shimomura I, et al. Decreased IRS-2 and increased SREBP-1c lead to mixed insulin resistance and sensitivity in livers of lipodystrophic and ob/ob mice. Mol. Cell. 2000;6:77–86. [PubMed] [Google Scholar]
- 27.Cho H, et al. Insulin resistance and a diabetes mellitus-like syndrome in mice lacking the protein kinase Akt2 (PKB β) Science. 2001;292:1728–1731. doi: 10.1126/science.292.5522.1728. [DOI] [PubMed] [Google Scholar]
- 28.Ohno S. Intercellular junctions and cellular polarity: the PAR-aPKC complex, a conserved core cassette playing fundamental roles in cell polarity. Curr. Opin. Cell Biol. 2001;13:641–648. doi: 10.1016/s0955-0674(00)00264-7. [DOI] [PubMed] [Google Scholar]
- 29.Fausto N, Campbell JS. The role of hepatocytes and oval cells in liver regeneration and repopulation. Mech. Dev. 2003;120:117–130. doi: 10.1016/s0925-4773(02)00338-6. [DOI] [PubMed] [Google Scholar]
- 30.Bluher M, et al. Adipose tissue selective insulin receptor knockout protects against obesity and obesity-related glucose intolerance. Dev. Cell. 2002;3:325–338. doi: 10.1016/s1534-5807(02)00199-5. [DOI] [PubMed] [Google Scholar]
- 31.Bachmann OP, et al. Effects of intravenous and dietary lipid challenge on intramyocellular lipid content and the relation with insulin sensitivity in humans. Diabetes. 2001;50:2579–2584. doi: 10.2337/diabetes.50.11.2579. [DOI] [PubMed] [Google Scholar]
- 32.Ryysy L, et al. Hepatic fat content and insulin action on free fatty acids and glucose metabolism rather than insulin absorption are associated with insulin requirements during insulin therapy in type 2 diabetic patients. Diabetes. 2000;49:749–758. doi: 10.2337/diabetes.49.5.749. [DOI] [PubMed] [Google Scholar]
- 33.Krssak M, et al. Intramyocellular lipid concentrations are correlated with insulin sensitivity in humans: a 1H NMR spectroscopy study. Diabetologia. 1999;42:113–116. doi: 10.1007/s001250051123. [DOI] [PubMed] [Google Scholar]
- 34.Kakuma T, et al. Leptin, troglitazone, and the expression of sterol regulatory element binding proteins in liver and pancreatic islets. Proc. Natl. Acad. Sci. U. S. A. 2000;97:8536–8541. doi: 10.1073/pnas.97.15.8536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yamauchi T, et al. The fat-derived hormone adiponectin reverses insulin resistance associated with both lipoatrophy and obesity. Nat. Med. 2001;7:941–946. doi: 10.1038/90984. [DOI] [PubMed] [Google Scholar]
- 36.Petersen KF, et al. Leptin reverses insulin resistance and hepatic steatosis in patients with severe lipodystrophy. J. Clin. Invest. 2002;109:1345–1350. doi:10.1172/JCI200215001. doi: 10.1172/JCI15001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kim JK, et al. Tissue-specific overexpression of lipoprotein lipase causes tissue-specific insulin resistance. Proc. Natl. Acad. Sci. U. S. A. 2001;98:7522–7527. doi: 10.1073/pnas.121164498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Uysal KT, Wiesbrock SM, Mario MW, Hotamisligil GS. Protection from obesity-induced insulin resistance in mice lacking TNF-α function. Nature. 1997;389:610–614. doi: 10.1038/39335. [DOI] [PubMed] [Google Scholar]
- 39.Muller G, et al. PKCζ is a molecular switch in signal transduction of TNF-α, bifunctionally regulated by ceramide and arachidonic acid. EMBO J. 1995;14:1961–1969. doi: 10.1002/j.1460-2075.1995.tb07188.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Limatola C, Barabino C, Nista A, Santoni A. Interleukin 1-β-induced protein kinase C-ζ activation is mimicked by exogenous phospholipase D. Biochem. J. 1997;321:497–501. doi: 10.1042/bj3210497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lallena MJ, Diaz-Meco MT, Bren G, Paya CV, Moscat J. Activation of IκB kinase β by protein kinase C isoforms. Mol. Cell. Biol. 1999;19:2180–2188. doi: 10.1128/mcb.19.3.2180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Yin MJ, Yamamoto Y, Gaynor RB. The anti-inflammatory agents aspirin and salicylate inhibit the activity of IκB kinase-β. Nature. 1998;396:77–80. doi: 10.1038/23948. [DOI] [PubMed] [Google Scholar]
- 43.Hundal RS, et al. Mechanism by which high-dose aspirin improves glucose metabolism in type 2 diabetes. J. Clin. Invest. 2002;109:1321–1326. doi:10.1172/JCI200214955. doi: 10.1172/JCI14955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Yuan M, et al. Reversal of obesity- and diet-induced insulin resistance with salicylates or targeted disruption of Ikkβ. Science. 2001;293:1673–1677. doi: 10.1126/science.1061620. [DOI] [PubMed] [Google Scholar]
- 45.Liu YF, et al. Insulin stimulates PKCζ-mediated phosphorylation of insulin receptor substrate-1 (IRS-1). A self-attenuated mechanism to negatively regulate the function of IRS proteins. J. Biol. Chem. 2001;276:14459–14465. doi: 10.1074/jbc.M007281200. [DOI] [PubMed] [Google Scholar]
- 46.Tobe K, et al. Increased expression of the sterol regulatory element-binding protein-1 gene in insulin receptor substrate-2(–/–) mouse liver. J. Biol. Chem. 2001;276:38337–38340. doi: 10.1074/jbc.C100160200. [DOI] [PubMed] [Google Scholar]