T cell receptor for antigen induces linker for activation of T cell–dependent activation of a negative signaling complex involving Dok-2, SHIP-1, and Grb-2 (original) (raw)
Abstract
Adaptor proteins positively or negatively regulate the T cell receptor for antigen (TCR) signaling cascade. We report that after TCR stimulation, the inhibitory adaptor downstream of kinase (Dok)-2 and its homologue Dok-1 are involved in a multimolecular complex including the lipid phosphatase Src homology 2 domain–containing inositol polyphosphate 5′-phosphatase (SHIP)-1 and Grb-2 which interacts with the membrane signaling scaffold linker for activation of T cells (LAT). Knockdown of LAT and SHIP-1 expression indicated that SHIP-1 favored recruitment of Dok-2 to LAT. Knockdown of Dok-2 and Dok-1 revealed their negative control on Akt and, unexpectedly, on Zap-70 activation. Our findings support the view that Dok-1 and -2 are critical elements of a LAT-dependent negative feedback loop that attenuates early TCR signal. Dok-1 and -2 may therefore exert a critical role in shaping the immune response and as gatekeepers for T cell tolerance.
Improved knowledge of the molecular machine that directs TCR signaling provides insights to understand thymic selection, T cell response to antigen, peripheral tolerance, and homeostasis (1–4). The effectiveness and harmlessness of these processes must be ensured by control mechanisms during TCR signal initiation, maintenance, and extinction. Each of these phases is, therefore, likely to be the resultant of the contrasting action of signaling circuits, a stratagem to accurately drive toward physiological outcomes while avoiding damaging effects. Dysregulation of one or more of these phases, resulting in alteration in signal magnitude and/or duration, may promote immune deviation or break of tolerance (5, 6).
TCR signal is conveyed as a cascade of biochemical modifications controlling enzymatic activities, assembly, and localization of multimolecular complexes. Central to this cascade are adaptor proteins that connect signaling circuits by facilitating juxtaposition of effectors with their targets. Adaptors may contribute to promote and/or oppose TCR signaling (7–9). The membrane adaptor linker for activation of T cells (LAT) is prototypic of positive regulation (10), as TCR engagement induces Zap-70–mediated tyrosine phosphorylation of LAT which serves as an anchoring platform for complexes activating major intracellular signaling pathways. However, recent data have suggested that LAT may also be a source of negative regulation of antigen receptor signaling (11, 12). In addition, other adaptors such as downstream of kinase (Dok)-1, Dok-2, Gab-2, Grap, and LAX have been proposed to negatively regulate T cell activation (8, 13–16).
Dok adaptors constitute a family of six members. Dok-1 (17, 18) and Dok-2 (or Dok-R/FRIP) (19–21) are highly related in structure and are preferentially expressed, together with Dok-3, in hematopoietic cells (22). Whereas Dok-1 and Dok-2 are expressed in the T cell lineage (23, 24), B cells express Dok- 1 and Dok-3 (22). Mutant mice lacking Dok-1 exhibited increased proliferation of thymocytes (25) and B cells in vitro, the latter being caused by impaired FcγRIIB inhibitory function on B lymphocyte antigen receptor (BCR) signaling (26). Studies in Dok-1−/−/Dok-2−/− double deficient mice showed that these adaptors exert redundant (23, 24) yet not completely overlapping roles. Their absence intensified development and homeostasis of hematopoietic cell precursors and mature cells, especially within the myeloid cell lineage and in response to cytokines (23, 24). With age, these mice developed chronic myelogenous leukemia (CML)–like disease and lymphomas (23, 24). Interestingly, Dok-1−/−/Dok-2−/− mice had a noticeably increased number of lymphocytes, and enhanced T cell proliferation was found in mutant mice expressing low levels of Dok-2 in vitro (21). Conversely, mice overexpressing Dok-2 showed depressed T cell development (27). These data indicate that Dok-1 and Dok-2 are likely key regulators of homeostasis, activation, and proliferation in cells of hematopoietic origin.
Dok-1 and Dok-2 are typical docking proteins with an N-terminal module composed of tandem pleckstrin homology (PH)-PTB domains followed by a region rich in binding motifs to Src homology (SH)2 and SH3 domains (20, 28). The precise stage at which Dok-1 and Dok-2 intervene in receptor signaling and the underlying mechanism of their action are not yet fully understood. Moreover, Dok-2 function in T cell activation is essentially unknown. Upon tyrosine phosphorylation, Dok-1 and Dok-2 have been reported to bind Ras–GTPase-activating protein, an inhibitor of Ras (17–19). Consistently, Dok-1 has been implicated in FcγRIIB-mediated decrease of BCR-induced Ras–extracellular signal-regulated kinase (Erk)-1/2 activation (26, 29). Erk-1/2 activation was also found to be attenuated in CD2-stimulated Jurkat T cells overexpressing Dok-1 (13) and increased in Dok-1−/−/Dok-2−/− myeloid cells stimulated by cytokines (23, 24). However, other studies performed with mutations in the binding sites of Ras–GTPase-activating protein have questioned its role in Erk-1/2 down-regulation via Dok-1 and Dok-2 (30, 31). It has also been shown that Dok-1 and Dok-2 negatively control Akt/PKB activation (24, 30, 31).
We now report that in primary T cells, TCR stimulation results in early Dok-2 and Dok-1 tyrosine phosphorylation and their involvement in a multimolecular complex, which includes Src homology (SH)2 domain–containing inositol polyphosphate 5′-phosphatase (SHIP)-1, Grb-2, and LAT. We find that LAT and SHIP-1 are required for TCR-induced Dok-2 tyrosine phosphorylation and propose that SHIP-1 allows anchoring of Dok-2 to LAT. Moreover, we show that Dok-2 and Dok-1 together negatively control activation of Zap-70 and Akt kinases, indicating that these adaptors act as attenuators of TCR signal at its initiation phase.
RESULTS
TCR/CD3 ligation induces Dok-2 and Dok-1 tyrosine phosphorylation
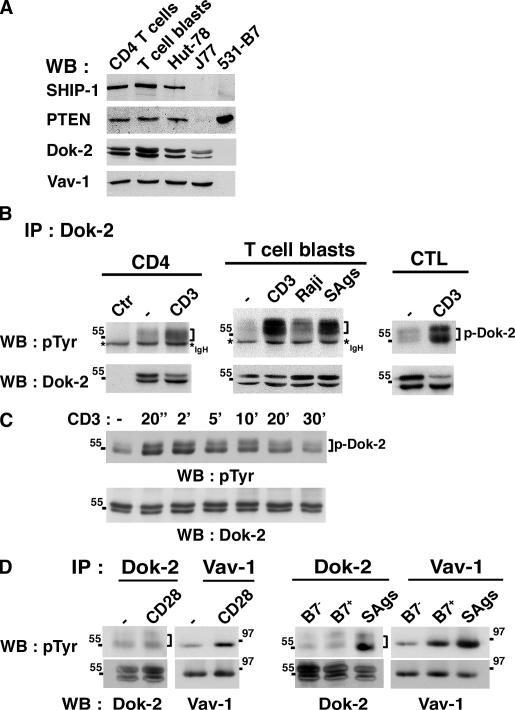
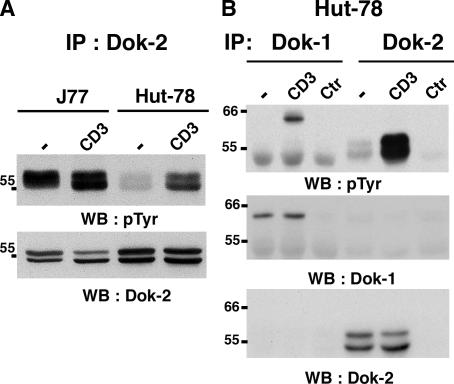
We investigated Dok-2 activation after CD3 and/or CD28 ligation. In normal T cells and transformed T cell lines, Dok-2 appeared as a doublet of ∼53–56 kD (Fig. 1 A). Dok-2 was found weakly tyrosine phosphorylated in unstimulated CD4 T cells, T cell blasts, a CD8 cytotoxic T cell clone (CTL) (Fig. 1 B), and Hut-78 cells (Fig. 2, A and B) but strongly phosphorylated in unstimulated J77 Jurkat cells (Fig. 2 A). TCR/CD3 stimulation led to substantial enhancement of Dok-2 phosphorylation in normal T cells (Fig. 1 B) and Hut-78 cells (Fig. 2, A and B) but little augmentation in J77 cells (Fig. 2 A). Phospho–Dok-2 migrated diffusely at and above 55 kD (Fig. 1 B, brackets), presumably because of the high content of phosphorylatable tyrosine motifs (19). Importantly, superantigen (SAg)-pulsed Raji cells (antigen-presenting cells not expressing Dok-2) induced a substantial increase in Dok-2 tyrosine phosphorylation in T cell blasts (Fig. 1 B, middle, lane 4), demonstrating that physiological TCR engagement induces activation of Dok-2. T cell contact with unpulsed Raji cells also induced weak Dok-2 phosphorylation (Fig. 1 B, middle, lane 3), possibly caused by engagement of a receptor distinct from TCR. Similar observations were made with unpulsed and SAg-pulsed autologous monocyte-derived dendritic cells (unpublished data). Dok-2 tyrosine phosphorylation was detected as early as 20 s after TCR stimulation, returning to background levels after 20–30 min (Fig. 1 C), a kinetics similar to that of Zap-70 activation and of other phosphoproteins (unpublished data).
Figure 1.
TCR-induced tyrosine phosphorylation of Dok-2 in primary T cells. (A) Expression of the indicated proteins in lysates of different cell types by immunoblot. (B) CD4+ and cytotoxic CD8+ T cells (CTL) were stimulated by CD3 cross-linking for 2 min at 37°C. T cell blasts were stimulated with Raji B cells (not expressing Dok-2) prepulsed or not with superantigens (SAgs) for 2 min. Dok-2 immunoprecipitates (IP) were analyzed by immunoblotting (WB) with anti-phosphotyrosine (pTyr) antibodies. Brackets indicate the doublet form of Dok-2 migrating above IgH chains (*) that are visible when serum 157–2 was used for immunoprecipitation. Ctr corresponds to protein A sepharose beads coated with anti–Dok-2 and without cell lysates. The bottom panels show reprobing with anti–Dok-2 mAbs. (C) Time course of CD3-mediated Dok-2 tyrosine phosphorylation in T cell blasts analyzed as in B. (D) T cells blasts were stimulated for 2 min with anti-CD28, 531 (B7−), 531-B7 (B7+) and SAgs-pulsed 531-B7 cells. Cell lysates were divided, immunoprecipitated with anti–Dok-2 (H192) and anti–Vav-1 (H191), and analyzed for tyrosine phosphorylation. Bottom panels show reprobing with mAbs. These assays were performed with at least 10 donors.
Figure 2.
TCR-mediated Dok-2 and Dok-1 tyrosine phosphorylation in transformed T cell lines. (A) Jurkat J77 and Hut-78 cells were stimulated with anti-CD3 for 2 min. Dok-2 was immunoprecipitated (H192) and analyzed for tyrosine phosphorylation. The bottom panel shows reprobing with anti–Dok-2 Abs. (B) Hut-78 cells were stimulated and analyzed as in A. Half of cell lysates was precipitated with anti–Dok-1 and anti–Dok-2 antibodies, respectively. Ctr, beads coated with antibodies. The two bottom panels show reprobing against the precipitated protein.
When T cells were stimulated with anti-CD28 antibody or B7-1–expressing cells (531-B7), Dok-2 tyrosine phosphorylation was only weakly induced above background level, whereas Vav-1, an effector of CD28 signaling, was more efficiently tyrosine phosphorylated (Fig. 1 D). In contrast, SAg-pulsed 531-B7 cells induced a substantial increment of Dok-2 tyrosine phosphorylation, confirming that TCR is the stronger inducer of this event (Fig. 1 D). Comprehensively, these data suggested that in normal T cells TCR engagement, rather than CD28, efficiently activated Dok-2. These data sharply contrasted with the behavior of Dok-1, the close Dok-2 homologue, which was reported to be inducibly phosphorylated in Jurkat cells by CD2 and CD28 but not by TCR triggering (13, 32, 33). One explanation for these opposite results may be the use of Jurkat cells, which also showed an unusually high basal phosphorylation of Dok-2 (Fig. 2 A). Jurkat cells lack expression of the lipid phosphatases, phosphatase and tensin homologue deleted in chromosome 10 (PTEN) and SHIP-1 (34), which causes dysregulated accumulation of phosphatidylinositol (PI) 3,4,5-trisphosphate and PI 3,4-bisphosphate and basal activation of certain PH domain–containing proteins (34, 35). Consistent with this idea, in Hut-78 cells, which express both PTEN and SHIP-1 at levels comparable with primary T cells (34) (Fig. 1 A), TCR/CD3 stimulation led to strong tyrosine phosphorylation of Dok-2 (Fig. 2 A). Interestingly, Dok-1 was also tyrosine phosphorylated in Hut-78 after TCR/CD3 stimulation (Fig. 2 B). Moreover, similarly to Dok-2, its phosphorylation was detected as early as 20 s after TCR triggering in primary T cells (Fig. S1, available at http://www.jem.org/cgi/content/full/jem.20060650/DC1). Overall, these observations suggest a rapid activation of both Dok-2 and Dok-1 adaptors concomitant with TCR signal development, and may explain opposite results because of the use of Jurkat cells versus normal T cells.
TCR-induced assembly of a multimolecular complex including Dok-2, SHIP-1, and Grb-2 to LAT
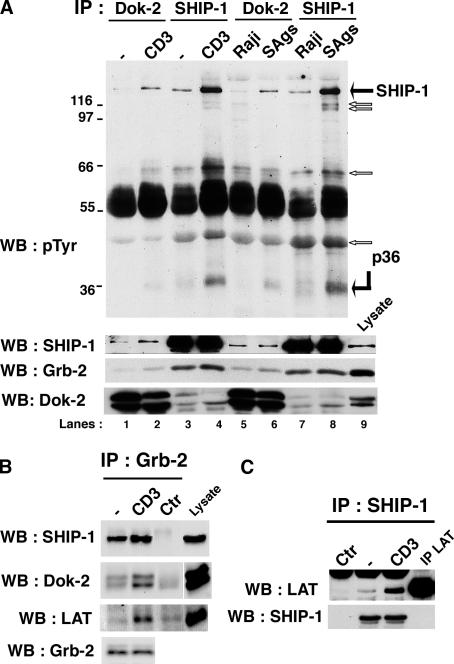
Because TCR ligation induced a very rapid phosphorylation of Dok-2, we investigated whether it physically engaged with TCR signaling effectors. T cell blasts were stimulated with anti-CD3 (Fig. 3 A, lanes 2 and 4) or Raji cells pulsed or not with SAgs (Fig. 3, last four lanes) and subjected to Dok-2 immunoprecipitation followed by antiphosphotyrosine immunoblot (Fig. 3 A, first panel). A major phosphoprotein of ∼145 kD coprecipitated with Dok-2 after TCR stimulation, comigrated with phosphorylated SHIP-1 (lanes 2 and 6 with 4 and 8) and was identified as SHIP-1 by immunoblotting (Fig. 3 A, second panel). Kinetic assays further confirmed its rapid and relatively prolonged coprecipitation with Dok-2 after TCR engagement (Fig. S2, right, available at http://www.jem.org/cgi/content/full/jem.20060650/DC1). This data is consistent with the reported Dok-2–SHIP-1 interaction upon SLAM stimulation (36). Similarly, tyrosine-phosphorylated SHIP-1 was detected in Dok-1 immunoprecipitates upon TCR stimulation (Fig. S3 A, available at http://www.jem.org/cgi/content/full/jem.20060650/DC1). A weak Dok-2–SHIP-1 association was seen in unstimulated cells and augmented after TCR stimulation (Fig. 3 A, anti–SHIP-1 immunoblot). Conversely, Dok-2 protein and its phosphorylated form were found in SHIP-1 immunoprecipitates (Fig. 3 A, fourth panel and Fig. S3 B). In accordance with the described interaction of SHIP-1 with one SH3 domain of Grb-2 (37), substantial amounts of Grb-2 were constitutively associated with SHIP-1 (Fig. 3 A, third panel, lanes 3, 4, 7, and 8) that slightly increased upon TCR stimulation. A much lower amount of Grb-2 was also observed constitutively in Dok-2 immunoprecipitates that weakly augmented after TCR triggering. This augmentation paralleled the increased binding of SHIP-1 with Dok-2 and suggested stabilization of Grb-2–SHIP-1–Dok-2. These findings were confirmed by probing Grb-2 immunoprecipitates with anti–SHIP-1 and anti–Dok-2 antibodies (Fig. 3 B). As demonstrated in previous studies (10), Grb-2 also bound to LAT upon TCR stimulation. Noteworthily, comparison of signal intensity of SHIP-1, Dok-2, and LAT coimmunoprecipitated with Grb-2 (Fig. 3 B, lanes 1 and 2) with their signals in the cell lysate (Fig. 3 B, lane 4) revealed the preferential association of SHIP-1 to Grb-2 with respect to Dok-2 and LAT, even after TCR stimulation.
Figure 3.
TCR-mediated assembly of a multimolecular complex including Dok-2 SHIP-1, Grb-2 with LAT. (A) T cell blasts were stimulated with anti-CD3 (lanes 2 and 4) and Raji cells pulsed or not with SAgs (lanes 5–8) for 2 min. Dok-2 and SHIP-1 immunoprecipitates were analyzed for tyrosine phosphorylation. Bottom panels show IP reprobing with the indicated antibodies. White arrows indicate unidentified phosphoproteins coprecipitating with SHIP-1 and more weakly with Dok-2. (B) Lysates from blasts stimulated with anti-CD3 or not were immunoprecipitated with anti–Grb-2 antibodies (lanes 2 and 1). Beads coated with anti–Grb-2 alone (Ctr, lane 3) were used as a negative control. The lysate of unstimulated cells (15 μg proteins, lane 4) was used to provide a measure of SHIP-1, Dok-2, and LAT expression. The nitrocellulose membrane was cut in three parts and probed with mAbs against SHIP-1, Dok-2, and LAT, respectively. (Bottom blot) Grb-2 expression in cell lysates that were immunoprecipitated. (C) SHIP-1 immunoprecipitates of anti-CD3–stimulated blasts were probed with anti-LAT mAbs. The bottom panel shows that equal amounts of SHIP-1 were precipitated. A, B, and C assays were reproduced with three donors.
Notably, pp36, pp47, and pp64 species were detected more strongly in SHIP-1 than Dok-2 immunoprecipitates, and an additional phosphoprotein of ∼116–118 kD was associated with SHIP-1 (Fig. 3 A, arrows). The broad appearance of the 36-kD molecular species was reminiscent of LAT. Indeed, immunoblotting of SHIP-1 immunoprecipitates with anti-LAT antibody confirmed that pp36 was LAT (Fig. 3 C). Moreover, tyrosine phosphorylation of SHIP-1 and coprecipitated LAT exhibited similar kinetic profiles, suggesting a causal link between these events (Fig. S2, left). Reciprocally, SHIP-1 and Dok-2 were observed in LAT immunoprecipitates upon TCR stimulation (unpublished data). Collectively, these data indicated that TCR triggering induced association of Dok-2–SHIP-1–Grb-2 to LAT, together with other phosphoproteins, suggesting that a bone fide negative signaling pathway is initiated coincidentally on the very same scaffold (i.e., LAT) that directs positive signal propagation.
TCR-mediated Dok-2 tyrosine phosphorylation depends on LAT and SHIP-1
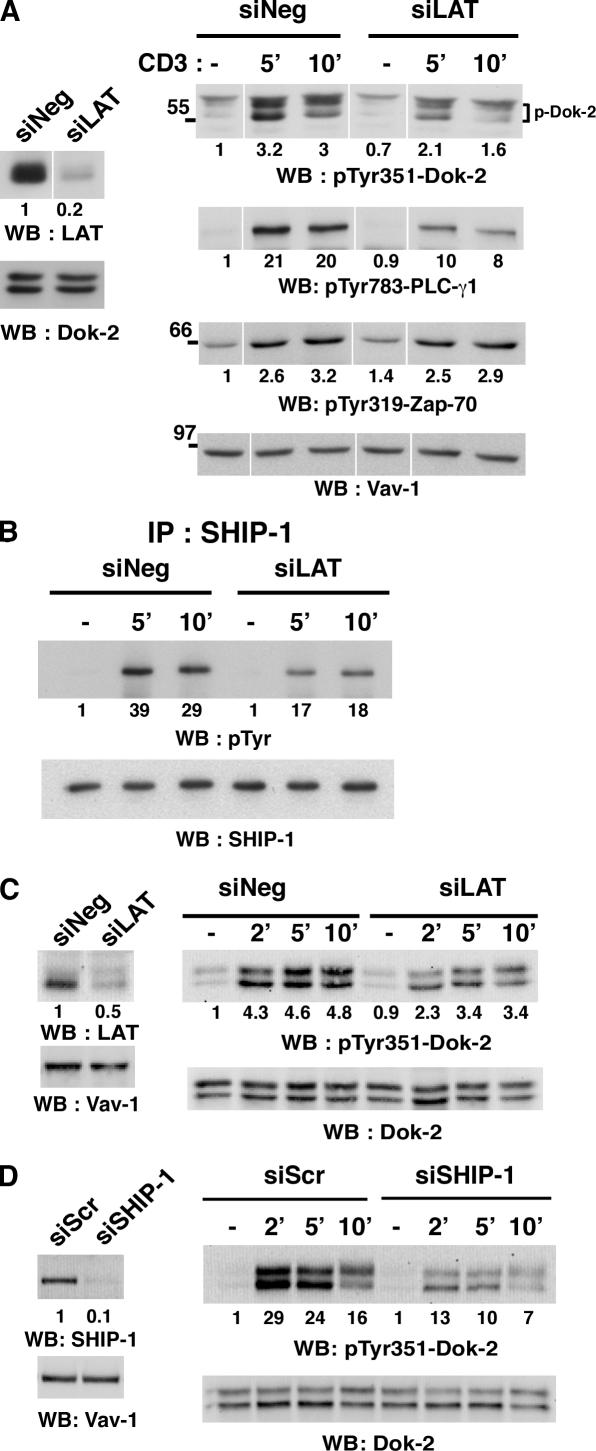
The association of Dok-2–SHIP-1–Grb-2 with LAT suggested that LAT may play a role in the activation of Dok-2 and SHIP-1. To answer this question, we inhibited LAT expression by small interfering (si)RNA and asked whether this modified SHIP-1 and Dok-2 phosphorylation. LAT expression was reduced in Hut-78 cells by 80–90% in comparison with cells transfected with irrelevant siRNA (siNeg or siScr), whereas expression of other proteins such as Dok-2, SHIP-1, PLC-γ1, Zap-70, and Vav-1 remained unaffected (Fig. 4, A and B and unpublished data). Upon TCR/CD3 stimulation, Hut-78 cells with reduced LAT expression exhibited impaired tyrosine phosphorylation of Dok-2 at 5 and 10 min (35–50% inhibition) as revealed with anti-pTyr351–Dok-2 antibody (Fig. 4 A). Consistent with previous findings in LAT-deficient Jurkat (38), activation of PLC-γ1, as estimated by anti-pTyr783–PLC-γ1 antibody, was also partially (50–60%) affected. Thus, when these data were compared with PLC-γ1 activation, the reduction of TCR-induced Dok-2 phosphorylation was substantial after LAT knockdown (80–90%). In contrast, TCR-induced Zap-70 activation, known to occur upstream of LAT (39), was not affected by LAT knockdown. Hut-78 cells with decreased LAT expression stimulated by CD3 also exhibited inhibition of SHIP-1 tyrosine phosphorylation (38–56% inhibition; Fig. 4 B). Importantly, impaired TCR- mediated phospho–Dok-2 was reproduced in primary T cells (30–47% reduction) in which LAT expression was inhibited by siRNA (50%) (Fig. 4 C) and with another siRNA against LAT in Hut-78 cells (unpublished data). The stronger association of LAT with SHIP-1 than with Dok-2 (Fig. 3, A and C) suggested that Dok-2 tyrosine phosphorylation may depend on SHIP-1. Consistent with this hypothesis, we found that reduced expression of SHIP-1 (90% by siRNA) substantially affected TCR-mediated tyrosine phosphorylation of Dok-2 (∼60%; Fig. 4 D) and of Dok-1 (∼40–50%; Fig. S4, available at http://www.jem.org/cgi/content/full/jem.20060650/DC1). Conversely, double knockdown of Dok-2 and Dok-1 expression did not impair TCR-induced tyrosine phosphorylation of SHIP-1 (unpublished data). Collectively, these data supported the idea that TCR stimulation induces association of the Dok-2–SHIP-1–Grb-2 complex with LAT followed by SHIP-1 and Dok-2 tyrosine phosphorylation.
Figure 4.
TCR-mediated Dok-2 tyrosine phosphorylation depends on LAT and SHIP-1 expression. (A) Hut-78 cells were transfected with control siNeg and siLAT RNA. 24 h later, cells were stimulated with soluble anti-CD3 for the indicated times. Cell lysates were analyzed by immunoblotting for LAT knockdown efficiency (left panels) and activation of Dok-2, PLC-γ1 and Zap-70 with phospho-specific antibodies (right panels). White lines indicate that intervening lanes have been spliced out. (B) Hut-78 cells were transfected and stimulated as in A. SHIP-1 immunoprecipitates were analyzed for tyrosine phosphorylation and reprobed with anti–SHIP-1 mAbs. LAT knockdown efficiency was 90% (not depicted). (C) Peripheral blood lymphocytes were electroporated by nucleofection with siNeg and siLAT (1.5 μM) and CD3-stimulated 48 h later. Cell lysates were analyzed for Dok-2 tyrosine phosphorylation and LAT knockdown efficiency as in A. Similar data were obtained with two other donors. (D) Hut-78 cells were transfected with control siScr and siSHIP-1. Cell lysates were analyzed for CD3-induced Dok-2 tyrosine phosphorylation and SHIP-1 knockdown efficiency as in A. The indicated values have been normalized to the protein loading in blots performed with anti–Vav-1, Dok-2 (A, C, and D) and SHIP-1 antibodies (B).
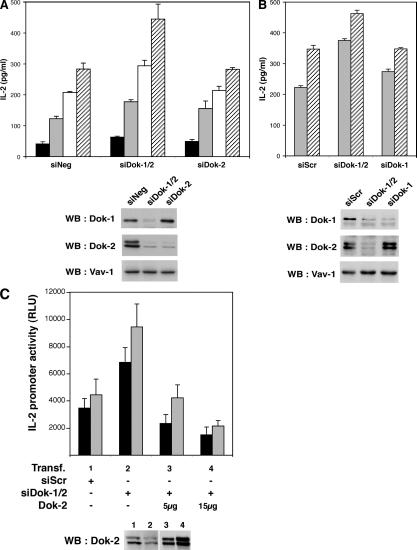
Knockdown of Dok-2 and Dok-1 enhances TCR-mediated IL-2 production and signaling
To assay the role of Dok-2 in TCR signaling, we measured TCR-mediated IL-2 secretion in Hut-78 cells knocked down for Dok-2 by siRNA. Inhibition of Dok-2 expression (∼90%; Fig. 5 A, middle blot) resulted in marginal or no increase in IL-2 secretion (Fig. 5 A, histograms). Similar to Dok-2, knockdown of Dok-1 alone (∼80%; Fig. 5 B, top blot) had minor or no impact on TCR-mediated IL-2 production (Fig. 5 B, histograms). In contrast, combined inhibition of Dok-2 and Dok-1 expression (∼90% and 80%, respectively) resulted in clear enhancement of TCR-induced IL-2 secretion in comparison with cells transfected with control siNeg or siScr RNA (Fig. 5, A and B). Collectively, these data indicated that Dok-1 and Dok-2 adaptors act together to negatively regulate TCR-mediated IL-2 gene activation. To examine the possibility of potential RNAi off-target effects, Dok-2 expression was restored in siDok-1/2–transfected cells, under the assumption that this would also substitute for Dok-1 function. To this aim, Hut-78 cells were cotransfected with a plasmid encoding human Dok-2 together with siDok-1/2 and IL-2 promoter–dependent luciferase reporter plasmid. Substantial levels of Dok-2 expression were detected in transfected cells (Fig. 5 C, blot panel). Complementation of siDok-1/2–transfected cells by Dok-2 cDNA alone was sufficient to repress TCR-mediated IL-2 gene expression and reverse the enhancement caused by siDok-1/2 (Fig. 5 C, histograms).
Figure 5.
Dok-2 and Dok-1 negatively control TCR-mediated IL-2 production. (A and B) Hut-78 cells were transfected with the indicated siRNA and, 24 h later, stimulated with immobilized anti-CD3 for 4 h. IL-2 secretion was determined by ELISA. Blots show inhibition of Dok-1 and Dok-2 expression by siDok-1 and siDok-2 (lanes 2) or a single siRNA (lanes 3). (C) Hut-78 cells were transfected as with siRNA. After 24 h, they were cotransfected with the same siRNA together with phIL-2–Luc and the indicated quantities of pCMV5–Dok-2 (Dok-2, μg) or empty vector (Dok-2, −) to adjust for equal amounts of total DNA. Luciferase activity was measured after 6h of stimulation with immobilized anti-CD3. The blot shows Dok-2 reexpressed upon cotransfection of siDok-1, si Dok-2, and pCMV5-Dok-2. In A, B, and C, IL-2 gene activation was normalized to PMA/A23187 stimulation. Histogram bars correspond to 0.48 (hatched), 0.12 (empty), 0.06 (gray), and 0.03 (black) μg/ml of anti-CD3.
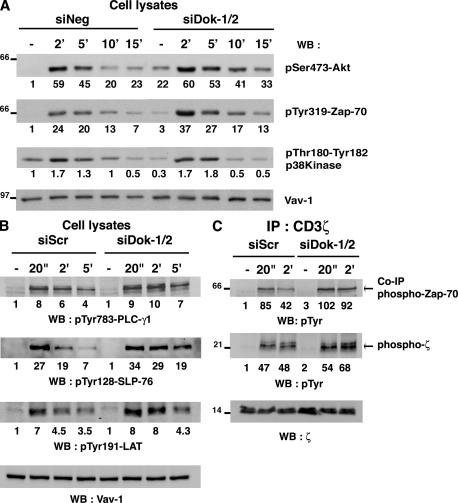
To begin understanding the molecular mechanism wherein the signaling cascade Dok-2 and Dok-1 influence TCR-mediated activation, we analyzed these adaptor effects on Akt/PKB and Erk-1/2. These kinases have been found to be more effectively activated upon cytokine stimulation of Dok-1−/−/Dok-2−/− myeloid cells (23, 24). We found that TCR-induced Erk-1/2 activation was poorly enhanced in Hut-78 doubly knocked down for Dok-2 and Dok-1 expression (unpublished data). However, double knockdown resulted in marked basal and prolonged TCR-mediated Akt activation as detected with an anti–pSer473-Akt antibody compared with siNeg-transfected Hut-78 cells (Fig. 6 A). These data are consistent with Dok1 and Dok-2 adaptors negatively controlling Akt activation (24) and extend this effect to the TCR signaling machinery.
Figure 6.
Knockdown of Dok-2 and Dok-1 results in enhanced TCR-mediated tyrosine phosphorylations and Akt kinase activation. Hut-78 cells were transfected with siDok-1 and siDok-2, control siRNAs, and stimulated with anti-CD3 for the indicated times. (A and B) Cell lysates were analyzed by immunoblotting with anti–phospho-specific antibodies. (C) CD3ζ was immunoprecipitated (8.73 antibodies) and analyzed for tyrosine phosphorylation and loading (448 antibodies). A, B, and C are representative of three experiments. Knockdown of Dok-2 and Dok-1 expression was ∼90% and 70–80%, respectively (not depicted). Numbers indicate increases in the phosphorylation level after normalization to protein loading in Vav-1 (A and B) and CD3ζ (C) blots.
Interestingly, by examining other TCR signal effectors in Hut-78 knocked down for Dok-2 and Dok-1, we consistently detected an increased activation of Zap-70 in stimulated cells as revealed by an anti-pTyr319–Zap-70 antibody (Fig. 6 A). This effect was particularly observed at early time points after TCR stimulation (and at 20 s; unpublished data). Enhanced Akt and Zap-70 activations were more pronounced in double than in single knockdown of Dok-2 and Dok-1 (unpublished data). Moreover, these effects appeared to be selective since p38 kinase activation was not enhanced and even decreased in unstimulated cells (Fig. 6 A). Alterations of the TCR-induced tyrosine phosphorylation profile were observed upon knockdown of Dok-2 and Dok-1. In particular, proteins of ∼36, 70, and 76 kD were more phosphorylated after TCR ligation (Fig. S5, http://www.jem.org/cgi/content/full/jem.20060650/DC1). In accordance with the enhancement of Zap-70 activation, LAT and SLP-76, as well as PLC-γ1, were found to be more phosphorylated (Y191, Y128 and Y783, respectively) (Fig. 6 B). Importantly, this was also the case for CD3ζ and its coprecipitated partner Zap-70 (Fig. 6 C). Overall, these data support the existence of a molecular mechanism that finely regulates TCR signal initiation by a negative feedback loop involving Dok-2 and Dok-1 recruitment, via SHIP-1, on LAT which reduces Zap-70 activation.
DISCUSSION
In this work we demonstrate that the adaptors Dok-2 and Dok-1 are key effectors of a TCR proximal negative feedback control mechanism. This notion stands on two novel sets of findings. First, TCR ligation induced rapid binding to LAT and tyrosine phosphorylation of Dok-2 and Dok-1 in complex with SHIP-1. The latter appeared to act as a carrier for these adaptors. Second, reduced expression of both Dok-2 and Dok-1 by siRNA resulted in increased amplitude and duration of TCR-induced Zap-70 activation and of other tyrosine-phosphorylated proteins and basal- and TCR-induced Akt activation with consequent augmentation of IL-2 gene expression. Individual knockdown of Dok-2 or Dok-1 had minimal or undetectable effects, suggesting that they exert redundant negative signaling functions, in agreement with previous data in cells of myeloid origin (23, 24). Comprehensively, our data demonstrate that LAT physically integrates, in apparent temporal coincidence, two opposing signals. A dominant signal promotes TCR-controlled activation (10), whereas the second, implicating Dok adaptors and probably other modulatory proteins (8), attenuates it. We propose that this type of mechanism may contribute to control the TCR activation threshold (“signal gatekeeper”) and/or to shape TCR signal form in intensity and duration (“signal tailoring”).
Triggering of BCR or FcɛRI was also reported to induce tyrosine phosphorylation of Dok adaptors and SHIP-1 (22, 29, 40). In light of our results, it will be of interest to determine whether antigen receptors use similar or distinct stratagems to recruit and activate Dok-dependent negative signals.
Previous studies in Jurkat cells showed that CD2 and CD28 receptors, but not TCR, induced potent tyrosine phosphorylation of Dok-1 and Dok-2, suggesting their participation in costimulatory signaling pathways (13, 32, 33; unpublished data). Our present results do not support this view in primary T cells because little or no tyrosine phosphorylation of Dok-2 was observed upon CD28 ligation. A possible explanation for this difference may be that in Jurkat cells, similar to Akt, activation of PH domain–containing Dok-1, 2 may be deregulated because of altered phosphatidylinositol metabolism, consequent to the absence of PTEN and SHIP-1 (34, 41).
In accordance with previous data (37), SHIP-1 was constitutively bound to Grb-2. We also found some basal SHIP-1–Dok-2 association that likely resulted from weak basal tyrosine phosphorylation of both proteins (Figs. 1, 3, and S2). However, TCR stimulation led to a marked increase in SHIP-1 and Dok-2 phosphorylations and their prolonged association. In support of phosphotyrosine-dependent interactions, Dok-2 and Dok-1 PTB domains were shown to bind to tyrosine-phosphorylated SHIP-1 (29, 36). We examined the reciprocal role of Dok-1, Dok-2 and SHIP-1 in their activation by knocking down their expression in Hut-78 cells. Knockdown of SHIP-1 revealed that it primarily controls TCR-induced tyrosine phosphorylation of Dok-2 and Dok-1. Conversely, a decrease in TCR-mediated SHIP-1 tyrosine phosphorylation was not observed in T cells knocked down for Dok-2 and Dok-1 (unpublished data). Moreover, knockdown of LAT resulted in a marked alteration of TCR-mediated SHIP-1, Dok-2, and Dok-1 tyrosine phosphorylation. Altogether, our data support the idea that in T cells, SHIP-1 mediates recruitment and activation of Dok-2 and Dok-1 to LAT. In accordance with a SHIP-1 “carrier” function, SHIP-1–deficient thymocytes do not exhibit Dok-2 tyrosine phosphorylation upon SLAM stimulation (36). A similar defect was observed for Dok-1 in SHIP-1–deficient B cells stimulated by BCR and FcγRIIB (29). How SHIP-1 is connected to LAT remains to be determined as we did not observe binding of the SHIP-1 SH2 domain to LAT in glutathione _S_-transferase pull-down assays (unpublished data). LAT contains several Grb-2 binding sites, and recent reports have indirectly suggested that LAT may be a source of negative signaling (11, 12). Thus, one scenario would involve recruitment to LAT of Grb-2/SHIP-1–Dok adaptors in direct competition with other positive signaling complexes containing Grb-2. It remains possible that other players may control Dok-2, Dok-1, and SHIP-1 recruitment/tyrosine phosphorylation because the latter was not completely abolished in LAT knocked down cells. A candidate may be, for instance, the inhibitory membrane adaptor LAX possessing several Grb-2 binding sites (42). This possibility may, however, be less likely because the inhibition of SHIP-1 and Dok-2 phosphorylation was comparable to that of PLCγ-1 in LAT knocked down T cells. Overall, our findings support the notion that LAT drives concomitantly negative and positive signals with potential consequences on T cell fate.
Our data also reveal a surprising negative control exerted by Dok-2 and Dok-1 on TCR-induced activation of Zap-70 and on substrates whose phosphorylation depend on Zap-70 (e.g., LAT, SLP-76, and PLC-γ1) (Fig. 6, A and B). Because TCR-induced tyrosine phosphorylation of Dok-2 and Dok-1 is very rapid (as early as 20 s), these data imply that these adaptors counteract TCR signal development at its initiation step. This finding can be related to a work proposing that Dok-2 binds to c-Src and attenuates its activity upon epidermal growth factor stimulation by recruiting Csk, the Src kinase family inhibitor kinase (31). Interestingly, Dok-1 was also recently demonstrated to control Csk localization at the plasma membrane and inhibit Src activation in a Csk-dependent manner upon platelet-derived growth factor stimulation (43). Similarly, in B cells, Dok-3 may dampen B cell activation through Csk association in addition to its binding to SHIP-1 (22, 44). Optimal activation of Zap-70 is tightly dependent on Lck binding and catalytic activity (45). Thus, the negative control of Dok-2 and Dok-1 on Zap-70 may be explained by their upstream control on Lck. In accordance with this proposition, we observed increased TCR-mediated tyrosine phosphorylation of CD3ζ upon knockdown of Dok-2 and Dok-1. However, the fact that knockdown of Dok-2 and Dok-1 did not dramatically affect these events suggests that these adaptors act as attenuators of TCR signal. This would also explain why we did not succeed in reproducibly detecting an increase in Zap-70 activation in siLAT-treated cells. In fact, LAT knockdown did not mimic the effect of Dok-2 and Dok-1 knockdown on Zap-70. Indeed, a 1.5– 2-fold increase in TCR-induced Zap-70 activation was detected, whereas Dok-2 and Dok-1 expressions were markedly decreased (90–80%). In contrast, LAT knockdown led to the clear reduced, but not abolished, Dok-2 and Dok-1 phosphorylation. The remaining phosphorylated Dok may still negatively control TCR-induced Zap-70 activation. Moreover, we observed a correlation between the levels of residual LAT expression and T cell activation. For instance, PLC-γ1 phosphorylation and IL-2 production were still noticeable (though strongly decreased) when residual LAT expression was around 10–15% or when the strength of TCR engagement was high (unpublished data).
A substantial enhancement of basal and prolonged TCR-induced activation of Akt was observed in Hut-78 cells knocked down for Dok-2 and Dok-1, in agreement with Akt activation increase in Dok-1−/−/Dok-2−/− mice (24). Our data of Dok-2 and Dok-1 knockdown in Hut-78 cells suggest that enhanced Akt activation may be a consequence of Zap-70 or, for the same matter, Src-PTK up-regulation. Indeed, although the precise mechanism of this regulation has yet to be determined, decreased Akt activation has been described upon overexpression of Dok-2 and epidermal growth factor receptor stimulation (31). What is then the role of SHIP-1 in this mechanism? One possibility is that SHIP-1 needs to be correctly localized in the TCR signalosome to exert, together with Dok-bound partners, its phosphatase activity on PI 3,4,5-trisphosphate, and contribute to this negative feedback loop. Indeed, SHIP−/− and Dok-2−/−/Dok-1−/− mice present close phenotypes characterized by enhanced Akt activation, survival, and expansion of myeloid cells (23, 24, 46). The negative control of SHIP-1 on Akt activation has also been demonstrated in T cells with an inducible expression system (41). However, because SHIP-1 appears to be mandatory for Dok-1 and Dok-2 recruitment (and phosphorylation), one appealing possibility is that SHIP-1 serves mostly as a carrier to facilitate the action of Dok proteins on signal attenuation. Since Akt plays an important role in T cell survival, IL-2 gene activation, and cell cycle progression (47, 48), Dok-2 and Dok-1 are therefore likely to play a role in these processes.
Several mechanisms that counteract signal onset and propagation have been proposed. These “negative” signals can emanate from membrane receptors (e.g., CD5, CTLA-4) or from phosphatases that constantly oppose activating phosphorylations on signaling components, or are activated as a consequence of receptor engagement (e.g., SHP-1, SHP-2). Our data show that Dok-2 and Dok-1 are involved in an early negative feedback mechanism acting through LAT. This molecular device may represent a mechanism to adapt toward homeostatic/tonic TCR signal intensity and/or attenuate incoming TCR signal. T cells indeed appear to require control mechanisms of their signaling machinery for maintaining a basal tonic signal and repress gene expression (49) while avoiding response to self-antigen and allowing survival and proliferative homeostasis (3, 4). Such a control implicating Dok-2 and Dok-1 is suggested by their slight basal tyrosine phosphorylation that we observed in primary T cells. Thus, Dok-1, 2 may play a gatekeeper function in setting the threshold of T cell activation and contributing to maintain peripheral T cell tolerance and homeostasis. Alternatively, but not exclusively, by shaping the intensity and duration of antigen-induced signals, Dok-2 and Dok-1 may influence naive T cell differentiation and effector functions.
MATERIALS AND METHODS
Cells and cultures.
Hut-78, Jurkat J77cl20 T cell, and Raji B cell lymphoma were cultured in RPMI 1640 containing 10% heat-inactivated FCS, 2 mM l-glutamine, penicillin, and streptomycin. L cells expressing DRB1*0101 (531) and B7-1 (531-B7) were cultured in complete DMEM with 50 μg/ml hygromycin B (33). Primary T cells were maintained overnight in complete RPMI supplemented with 1 mM sodium pyruvate and nonessential amino acids (GIBCO BRL). Blood samples from healthy donors were obtained from Etablissement Français du Sang (EFS), Paris, France in accordance with a convention signed between the Institut Pasteur and EFS. Human peripheral blood mononuclear cells (PBMCs) were isolated by Ficoll density gradient, and peripheral blood lymphocytes were obtained after PBMC adhesion (10 × 106/ml) in RPMI 2% FCS for 1 h at 37°C. Phytohemagglutinin/IL-2 T cell blasts were harvested at days 6–13 of culture established with PBMCs (3 × 106/ml) that were stimulated by phytohemagglutinin (2 μg/ml) for 2–3 d and then expanded with IL-2 (50 ng/ml; Chiron). Flow cytometric analysis showed that >97% cells were CD3+ and 95% CD28+ at days 6–8. Naive CD4 T cells were purified by negative selection (90–98%) and an AutoMACS apparatus (Miltenyi Biotec). The human CD8+ CTL clone specific of CMV has been previously described (50).
Antibodies.
Mouse mAbs were against CD3 (UCHT1; Serotec), CD28 (CD28.2; Immunotech), Vav-1 (Vav-30; a gift from J. Griffin, Dana Farber Cancer Institute, Boston, MA), Dok-2 (E10; Santa-Cruz Biotechnology, Inc.), LAT (2E9; Upstate), SHIP-1 (P1C1; Santa-Cruz Biotechnology, Inc.), PTEN (A2B1; Santa-Cruz Biotechnology, Inc.), a cocktail of antiphosphotyrosine mAbs including 4G10 (Upstate), PY20 (Transduction Lab.), and PY99 (Santa-Cruz Biotechnology, Inc.). Rabbit antibodies were against Dok-2 (H-192 [Santa-Cruz Biotechnology, Inc.] and serum 157–2[36]), Dok-1 (13602 [Abcam] and serum A.V.[22]), SHIP-1 165.1 3′ (22), CD3ζ chain (8.73 and 448 sera[51]), Grb2 (C23) and Vav-1 (H211) (Santa-Cruz Biotechnology, Inc.), phospho-Tyr351-Dok-2, Ser473-Akt, Tyr319Zap-70, Tyr783-PLC-γ1, and Thr180-Tyr182-p38 kinase (Cell Signaling). mAb against phosphorylated SLP-76 Y128 was from BD Biosciences. Goat anti–mouse IgG and IgG1 were from Southern Biotechnology Associates, Inc.
siRNA duplexes.
siRNA duplexes containing 19 nucleotides with 2 thymidine 3′ overhangs were purchased from Eurogentec, Qiagen, and Proligo-Sigma. The sequences were as follows: 5′-GAAUGCUGCACCCGCUACA-3′ for siDok-2, 5′-GGUCAUGUUCUCUUUCGAG-3′ for siDok-1, 5′-GCUAAGUGCUUUACGAACA-3′ for siSHIP-1, 5′-ACGCAUGUACACACUCGCG-3′ for a randomly Dok-2 scrambled sequence (siScr), and two negative control RNA duplexes (siNeg) from Qiagen and Ambion, respectively. SiRNA used for silencing LAT gene expression was from Santa-Cruz Biotechnology, Inc.
Cell transfections.
To achieve maximal RNAi, Hut-78 cells (12 × 106/0.4 ml) were electroporated two to three times at 24 h intervals with siRNAs (200–300 nM) at 260 V, 950 μF (Bio Rad Laboratories). Cells were harvested 24–48 h after the last electroporation. For IL-2 gene activation, Hut-78 cells were first transfected with siDok-1/2 or siScr (300 nM). After 24 h, these cells were cotransfected with the same siRNA together with pCMV5 encoding HA-tagged human Dok-2 (19) and IL-2 promoter luciferase reporter plasmid (phIL-2-Luc, 10 μg) at 230 V, 950 μF. The total amount of DNA was adjusted to 25 μg with empty vector. Luciferase activity was measured in triplicate 24 h after the second transfection using a microplate luminometer (LB96V, Berthold; PerkinElmer). Primary T cells (6 × 106) were transfected with siRNA (1–1.5 μM) by nucleofection (Amaxa) according to the supplier's instructions and incubated in p24-well plates in complete RPMI medium for 48 h.
Cell stimulation, immunoprecipitation, and immunoblots.
Primary T cells (6–10 × 106) were stimulated in RPMI (1.5 × 108/ml) at a ratio of 5:1 with APC (5 × 107/ml) previously pulsed for 1 h with a mixture of superantigens (Staphylococcal enterotoxin A, B, C3 at 0.2 μg/ml; Toxin Technology) at 37°C. Jurkat, Hut-78, and primary T cells (1.2 × 108/ml) were stimulated by cross-linking of CD3 (5 μg/ml) with anti-IgG1 antibodies (20 μg/ml) as previously described (33) or with soluble anti-CD3 (5 μg/ml). CD28 stimulation with antibodies was performed by cross-linking (10 μg/ml) and with 531 cells expressing B7.1 (33). Cells were lysed at 4°C for 10 min in buffer (20 mM Tris-HCl, pH 7.5, 150 mM NaCl, 1 mM MgCl2, 1 mM EGTA, 50 mM NaF, 10 mM Na4P2O7, 1 mM Na3VO4) containing 1% NP-40 and 1% _n_-dodecyl-β-d-maltoside (Sigma-Aldrich) and inhibitors of proteases. Lysates were cleared by centrifugation and equal amounts of protein, determined by Bradford assay (Bio Rad Laboratories), were immunoprecipitated for 2 h at 4°C with the indicated antibodies preadsorbed to protein A– or protein G–Sepharose (Amersham Biosciences). Immunoprecipitates and whole cell lysates (15 μg proteins) were separated by SDS-PAGE and transferred to nitrocellulose membrane. Immunoblots were analyzed by enhanced chemiluminescence (Western Lightning; PerkinElmer) or by near-infrared fluorescence using secondary goat anti–mouse or goat anti–rabbit IgG labeled with AlexaFluor 680 (Invitrogen) and IRDye 800 (Rockland Immunochemicals), respectively. Signals were acquired and quantified with a Kodak Image Station 440 cf or an Odyssey scanner and the Odyssey 1.2 software (Li-Cor Biosciences), or after scanning films in the linear range of exposure. Phosphoprotein signals and RNAi efficiency were normalized to the protein loading charge evaluated by immunoblot.
IL-2 production.
SiRNA-treated Hut-78 cells were stimulated in triplicate in p96-well round plates with immobilized anti-CD3 for 4 h at 37°C. Goat anti–mouse IgG (4 μg/ml) were coated in wells in PBS overnight at 4°C and washed twice. UCHT1 was added at different concentrations for 1 h at 37°C in PBS and washed twice. After saturation of wells in RPMI 10% FCS, T cells were added (5 × 105/ml). TCR-independent activation was induced with PMA (5 ng/ml) and A23187 (0.1 μg/ml). IL-2 production was measured from 4 h cell culture supernatants by ELISA (R&D Systems). A sample of siRNA-treated cells was kept to check for RNAi efficiency by immunoblot.
Online supplemental material.
In addition to Dok-2, Dok-1 was tyrosine phosphorylated (Fig. S1) and interacted with SHIP-1 (Fig. S3) after TCR stimulation of primary T cells. TCR-mediated Dok-1 tyrosine phosphorylation was dependent on SHIP-1 expression in Hut-78 cells (Fig. S4). Kinetics of TCR-induced SHIP-1–LAT and Dok-2–SHIP-1 complex formation are shown in Fig. S2. Fig. S5 shows TCR-induced tyrosine phosphorylation profile in Hut-78 cells knocked down for Dok-2 and Dok-1 expression in which enhanced phosphorylation of ∼36, 70, and 76 kD proteins was detected. Online supplemental material is available at http://www.jem.org/cgi/content/full/jem.20060650/DC1.
Supplemental Material
[Supplemental Material Index]
Acknowledgments
We thank P. Rohrlich and F. Lemonnier for reagents, V. Di Bartolo, B. Schurter, and S. Pellegrini for comments on the manuscript, and W. Houssin for secretarial assistance.
S. Dong is a Ph.D student financed by Ministere de l'Education Nationale, de la Rechereche et de la Technologie, and E. Foulon was a master's degree student. This work was supported by grants from the Institut Pasteur, the Association pour la Recherche sur le Cancer, and the Centre National pour la Recherche Scientifique.
The authors have no conflicting financial interests.
Abbreviations used: BCR, B lymphocyte antigen receptor; CML, chronic myelogenous leukemia; Dok, downstream of kinase; ERK, extracellular signal-regulated kinase; LAT, linker for activation of T cells; PH, pleckstrin homology; PI, phosphatidylinositol; PTEN, phosphatase and tensin homologue deleted in chromosome 10; SH, Src homology; SHIP, SH2 domain-containing inositol polyphosphate 5′-phosphatase; SAg, superantigen; si, small interfering.
S. Dong and B. Corre contributed equally to this work.
F. Michel's present address is Cytokine Signaling Unit, Institut Pasteur, Paris, 75015 France.
O. Acuto's present address is Sir William Dunn School of Pathology, Oxford OX1 3RE, UK.
References
- 1.Werlen, G., B. Hausmann, D. Naeher, and E. Palmer. 2003. Signaling life and death in the thymus: timing is everything. Science. 299:1859–1863. [DOI] [PubMed] [Google Scholar]
- 2.Leitenberg, D., and K. Bottomly. 1999. Regulation of naive T cell differentiation by varying the potency of TCR signal transduction. Semin. Immunol. 11:283–292. [DOI] [PubMed] [Google Scholar]
- 3.Seddon, B., and R. Zamoyska. 2003. Regulation of peripheral T-cell homeostasis by receptor signalling. Curr. Opin. Immunol. 15:321–324. [DOI] [PubMed] [Google Scholar]
- 4.Marquez, M.E., W. Ellmeier, V. Sanchez-Guajardo, A.A. Freitas, O. Acuto, and V. Di Bartolo. 2005. CD8 T cell sensory adaptation dependent on TCR avidity for self-antigens. J. Immunol. 175:7388–7397. [DOI] [PubMed] [Google Scholar]
- 5.Duan, L., A.L. Reddi, A. Ghosh, M. Dimri, and H. Band. 2004. The Cbl family and other ubiquitin ligases: destructive forces in control of antigen receptor signaling. Immunity. 21:7–17. [DOI] [PubMed] [Google Scholar]
- 6.Ohashi, P.S. 2002. T-cell signalling and autoimmunity: molecular mechanisms of disease. Nat. Rev. Immunol. 2:427–438. [DOI] [PubMed] [Google Scholar]
- 7.Jordan, M.S., A.L. Singer, and G.A. Koretzky. 2003. Adaptors as central mediators of signal transduction in immune cells. Nat. Immunol. 4:110–116. [DOI] [PubMed] [Google Scholar]
- 8.Yamasaki, S., and T. Saito. 2004. Inhibitory adaptors in lymphocytes. Semin. Immunol. 16:421–427. [DOI] [PubMed] [Google Scholar]
- 9.Horejsi, V., W. Zhang, and B. Schraven. 2004. Transmembrane adaptor proteins: organizers of immunoreceptor signalling. Nat. Rev. Immunol. 4:603–616. [DOI] [PubMed] [Google Scholar]
- 10.Samelson, L.E. 2002. Signal transduction mediated by the T cell antigen receptor: the role of adapter proteins. Annu. Rev. Immunol. 20:371–394. [DOI] [PubMed] [Google Scholar]
- 11.Yamasaki, S., K. Nishida, M. Sakuma, D. Berry, C.J. McGlade, T. Hirano, and T. Saito. 2003. Gads/Grb2-mediated association with LAT is critical for the inhibitory function of Gab2 in T cells. Mol. Cell. Biol. 23:2515–2529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Malbec, O., M. Malissen, I. Isnardi, R. Lesourne, A.M. Mura, W.H. Fridman, B. Malissen, and M. Daeron. 2004. Linker for activation of T cells integrates positive and negative signaling in mast cells. J. Immunol. 173:5086–5094. [DOI] [PubMed] [Google Scholar]
- 13.Nemorin, J.G., P. Laporte, G. Berube, and P. Duplay. 2001. p62dok negatively regulates CD2 signaling in Jurkat cells. J. Immunol. 166:4408–4415. [DOI] [PubMed] [Google Scholar]
- 14.Boulay, I., J.G. Nemorin, and P. Duplay. 2005. Phosphotyrosine binding-mediated oligomerization of downstream of tyrosine kinase (Dok)-1 and Dok-2 is involved in CD2-induced Dok phosphorylation. J. Immunol. 175:4483–4489. [DOI] [PubMed] [Google Scholar]
- 15.Shen, R., Y.B. Ouyang, C.K. Qu, A. Alonso, L. Sperzel, T. Mustelin, M.H. Kaplan, and G.S. Feng. 2002. Grap negatively regulates T-cell receptor-elicited lymphocyte proliferation and interleukin-2 induction. Mol. Cell. Biol. 22:3230–3236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhu, M., O. Granillo, R. Wen, K. Yang, X. Dai, D. Wang, and W. Zhang. 2005. Negative regulation of lymphocyte activation by the adaptor protein LAX. J. Immunol. 174:5612–5619. [DOI] [PubMed] [Google Scholar]
- 17.Carpino, N., D. Wisniewski, A. Strife, D. Marshak, R. Kobayashi, B. Stillman, and B. Clarkson. 1997. p62(dok): a constitutively tyrosine- phosphorylated, GAP-associated protein in chronic myelogenous leukemia progenitor cells. Cell. 88:197–204. [DOI] [PubMed] [Google Scholar]
- 18.Yamanashi, Y., and D. Baltimore. 1997. Identification of the Abl- and rasGAP-associated 62 kDa protein as a docking protein, Dok. Cell. 88:205–211. [DOI] [PubMed] [Google Scholar]
- 19.Di Cristofano, A., N. Carpino, N. Dunant, G. Friedland, R. Kobayashi, A. Strife, D. Wisniewski, B. Clarkson, P.P. Pandolfi, and M.D. Resh. 1998. Molecular cloning and characterization of p56dok-2 defines a new family of RasGAP-binding proteins. J. Biol. Chem. 273:4827–4830. [DOI] [PubMed] [Google Scholar]
- 20.Jones, N., and D.J. Dumont. 1998. The Tek/Tie2 receptor signals through a novel Dok-related docking protein, Dok-R. Oncogene. 17:1097–1108. [DOI] [PubMed] [Google Scholar]
- 21.Nelms, K., A.L. Snow, J. Hu-Li, and W.E. Paul. 1998. FRIP, a hematopoietic cell-specific rasGAP-interacting protein phosphorylated in response to cytokine stimulation. Immunity. 9:13–24. [DOI] [PubMed] [Google Scholar]
- 22.Lemay, S., D. Davidson, S. Latour, and A. Veillette. 2000. Dok-3, a novel adapter molecule involved in the negative regulation of immunoreceptor signaling. Mol. Cell. Biol. 20:2743–2754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Niki, M., A. Di Cristofano, M. Zhao, H. Honda, H. Hirai, L. Van Aelst, C. Cordon-Cardo, and P.P. Pandolfi. 2004. Role of Dok-1 and Dok-2 in leukemia suppression. J. Exp. Med. 200:1689–1695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yasuda, T., M. Shirakata, A. Iwama, A. Ishii, Y. Ebihara, M. Osawa, K. Honda, H. Shinohara, K. Sudo, K. Tsuji, et al. 2004. Role of Dok-1 and Dok-2 in myeloid homeostasis and suppression of leukemia. J. Exp. Med. 200:1681–1687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Di Cristofano, A., M. Niki, M. Zhao, F.G. Karnell, B. Clarkson, W.S. Pear, L. Van Aelst, and P.P. Pandolfi. 2001. p62(dok), a negative regulator of Ras and mitogen-activated protein kinase (MAPK) activity, opposes leukemogenesis by p210(bcr-abl). J. Exp. Med. 194:275–284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yamanashi, Y., T. Tamura, T. Kanamori, H. Yamane, H. Nariuchi, T. Yamamoto, and D. Baltimore. 2000. Role of the rasGAP-associated docking protein p62(dok) in negative regulation of B cell receptor-mediated signaling. Genes Dev. 14:11–16. [PMC free article] [PubMed] [Google Scholar]
- 27.Gugasyan, R., C. Quilici, I. ST, D. Grail, A.M. Verhagen, A. Roberts, T. Kitamura, A.R. Dunn, and P. Lock. 2002. Dok-related protein negatively regulates T cell development via its RasGTPase-activating protein and Nck docking sites. J. Cell Biol. 158:115–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cai, D., S. Dhe-Paganon, P.A. Melendez, J. Lee, and S.E. Shoelson. 2003. Two new substrates in insulin signaling, IRS5/DOK4 and IRS6/DOK5. J. Biol. Chem. 278:25323–25330. [DOI] [PubMed] [Google Scholar]
- 29.Tamir, I., J.C. Stolpa, C.D. Helgason, K. Nakamura, P. Bruhns, M. Daeron, and J.C. Cambier. 2000. The RasGAP-binding protein p62dok is a mediator of inhibitory FcgammaRIIB signals in B cells. Immunity. 12:347–358. [DOI] [PubMed] [Google Scholar]
- 30.Wick, M.J., L.Q. Dong, D. Hu, P. Langlais, and F. Liu. 2001. Insulin receptor-mediated p62dok tyrosine phosphorylation at residues 362 and 398 plays distinct roles for binding GTPase-activating protein and Nck and is essential for inhibiting insulin-stimulated activation of Ras and Akt. J. Biol. Chem. 276:42843–42850. [DOI] [PubMed] [Google Scholar]
- 31.Van Slyke, P., M.L. Coll, Z. Master, H. Kim, J. Filmus, and D.J. Dumont. 2005. Dok-R mediates attenuation of epidermal growth factor-dependent mitogen-activated protein kinase and Akt activation through processive recruitment of c-Src and Csk. Mol. Cell. Biol. 25:3831–3841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Martelli, M.P., J. Boomer, M. Bu, and B.E. Bierer. 2001. T cell regulation of p62(dok) (Dok1) association with Crk-L. J. Biol. Chem. 276:45654–45661. [DOI] [PubMed] [Google Scholar]
- 33.Michel, F., G. Attal-Bonnefoy, G. Mangino, S. Mise-Omata, and O. Acuto. 2001. CD28 as a molecular amplifier extending TCR ligation and signaling capabilities. Immunity. 15:935–945. [DOI] [PubMed] [Google Scholar]
- 34.Freeburn, R.W., K.L. Wright, S.J. Burgess, E. Astoul, D.A. Cantrell, and S.G. Ward. 2002. Evidence that SHIP-1 contributes to phosphatidylinositol 3,4,5-trisphosphate metabolism in T lymphocytes and can regulate novel phosphoinositide 3-kinase effectors. J. Immunol. 169:5441–5450. [DOI] [PubMed] [Google Scholar]
- 35.Seminario, M.C., P. Precht, S.C. Bunnell, S.E. Warren, C.M. Morris, D. Taub, and R.L. Wange. 2004. PTEN permits acute increases in D3-phosphoinositide levels following TCR stimulation but inhibits distal signaling events by reducing the basal activity of Akt. Eur. J. Immunol. 34:3165–3175. [DOI] [PubMed] [Google Scholar]
- 36.Latour, S., G. Gish, C.D. Helgason, R.K. Humphries, T. Pawson, and A. Veillette. 2001. Regulation of SLAM-mediated signal transduction by SAP, the X-linked lymphoproliferative gene product. Nat. Immunol. 2:681–690. [DOI] [PubMed] [Google Scholar]
- 37.Damen, J.E., L. Liu, P. Rosten, R.K. Humphries, A.B. Jefferson, P.W. Majerus, and G. Krystal. 1996. The 145-kDa protein induced to associate with Shc by multiple cytokines is an inositol tetraphosphate and phosphatidylinositol 3,4,5-triphosphate 5-phosphatase. Proc. Natl. Acad. Sci. USA. 93:1689–1693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Finco, T.S., T. Kadlecek, W. Zhang, L.E. Samelson, and A. Weiss. 1998. LAT is required for TCR-mediated activation of PLCgamma1 and the Ras pathway. Immunity. 9:617–626. [DOI] [PubMed] [Google Scholar]
- 39.Zhang, W., J. Sloan-Lancaster, J. Kitchen, R.P. Trible, and L.E. Samelson. 1998. LAT: the ZAP-70 tyrosine kinase substrate that links T cell receptor to cellular activation. Cell. 92:83–92. [DOI] [PubMed] [Google Scholar]
- 40.Abramson, J., G. Rozenblum, and I. Pecht. 2003. Dok protein family members are involved in signaling mediated by the type 1 Fcepsilon receptor. Eur. J. Immunol. 33:85–91. [DOI] [PubMed] [Google Scholar]
- 41.Horn, S., E. Endl, B. Fehse, M.M. Weck, G.W. Mayr, and M. Jucker. 2004. Restoration of SHIP activity in a human leukemia cell line downregulates constitutively activated phosphatidylinositol 3-kinase/Akt/GSK-3beta signaling and leads to an increased transit time through the G1 phase of the cell cycle. Leukemia. 18:1839–1849. [DOI] [PubMed] [Google Scholar]
- 42.Zhu, M., E. Janssen, K. Leung, and W. Zhang. 2002. Molecular cloning of a novel gene encoding a membrane-associated adaptor protein (LAX) in lymphocyte signaling. J. Biol. Chem. 277:46151–46158. [DOI] [PubMed] [Google Scholar]
- 43.Zhao, M., J.A. Janas, M. Niki, P.P. Pandolfi, and L. Van Aelst. 2006. Dok-1 independently attenuates ras/mitogen-activated protein kinase and Src/c-Myc pathways to inhibit platelet-derived growth factor-induced mitogenesis. Mol. Cell. Biol. 26:2479–2489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Robson, J.D., D. Davidson, and A. Veillette. 2004. Inhibition of the Jun N-terminal protein kinase pathway by SHIP-1, a lipid phosphatase that interacts with the adaptor molecule Dok-3. Mol. Cell. Biol. 24:2332–2343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Di Bartolo, V., D. Mege, V. Germain, M. Pelosi, E. Dufour, F. Michel, G. Magistrelli, A. Isacchi, and O. Acuto. 1999. Tyrosine 319, a newly identified phosphorylation site of ZAP-70, plays a critical role in T cell antigen receptor signaling. J. Biol. Chem. 274:6285–6294. [DOI] [PubMed] [Google Scholar]
- 46.Liu, Q., T. Sasaki, I. Kozieradzki, A. Wakeham, A. Itie, D.J. Dumont, and J.M. Penninger. 1999. SHIP is a negative regulator of growth factor receptor-mediated PKB/Akt activation and myeloid cell survival. Genes Dev. 13:786–791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kane, L.P., and A. Weiss. 2003. The PI-3 kinase/Akt pathway and T cell activation: pleiotropic pathways downstream of PIP3. Immunol. Rev. 192:7–20. [DOI] [PubMed] [Google Scholar]
- 48.Costello, P.S., M. Gallagher, and D.A. Cantrell. 2002. Sustained and dynamic inositol lipid metabolism inside and outside the immunological synapse. Nat. Immunol. 3:1082–1089. [DOI] [PubMed] [Google Scholar]
- 49.Roose, J.P., M. Diehn, M.G. Tomlinson, J. Lin, A.A. Alizadeh, D. Botstein, P.O. Brown, and A. Weiss. 2003. T cell receptor-independent basal signaling via Erk and Abl kinases suppresses RAG gene expression. PLoS Biol. 1:E53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hamel, Y., P. Rohrlich, V. Baron, D. Bonhomme, F. Rieux-Laucat, A. Necker, F. Lemonnier, L. Ferradini, A. Fischer, and M. Cavazzana-Calvo. 2003. Characterization of antigen-specific repertoire diversity following in vitro restimulation by a recombinant adenovirus expressing human cytomegalovirus pp65. Eur. J. Immunol. 33:760–768. [DOI] [PubMed] [Google Scholar]
- 51.Irles, C., A. Symons, F. Michel, T.R. Bakker, P.A. van der Merwe, and O. Acuto. 2003. CD45 ectodomain controls interaction with GEMs and Lck activity for optimal TCR signaling. Nat. Immunol. 4:189–197. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
[Supplemental Material Index]