Lymphocytes are detrimental during the early innate immune response against Listeria monocytogenes (original) (raw)
Abstract
Mice deficient in lymphocytes are more resistant than normal mice to Listeria monocytogenes infection during the early innate immune response. This paradox remains unresolved: lymphocytes are required for sterilizing immunity, but their presence during the early stage of the infection is not an asset and may even be detrimental. We found that lymphocyte-deficient mice, which showed limited apoptosis in infected organs, were resistant during the first four days of infection but became susceptible when engrafted with lymphocytes. Engraftment with lymphocytes from type I interferon receptor–deficient (IFN-αβR−/−) mice, which had reduced apoptosis, did not confer increased susceptibility to infection, even when the phagocytes were IFN-αβR+/+. The attenuation of innate immunity was due, in part, to the production of the antiinflammatory cytokine interleukin 10 by phagocytic cells after the apoptotic phase of the infection. Thus, immunodeficient mice were more resistant relative to normal mice because the latter went through a stage of lymphocyte apoptosis that was detrimental to the innate immune response. This is an example of a bacterial pathogen creating a cascade of events that leads to a permissive infective niche early during infection.
Mice genetically deficient in lymphocytes (SCID, RAG−/−, and nude) and splenectomized mice are all more resistant to early Listeria monocytogenes infection (1–4). These finding are surprising because T lymphocytes are required for sterilizing immunity against listeriosis, and in their absence, strains such as nude and SCID become chronic carriers after infection (1, 4, 5).
Within the first 2–12 h of infection, L. monocytogenes is initially trapped in the marginal zone of the spleen (6–8). At 24 h of infection, the bacteria are taken to the T cell zones of the spleen by a Mac3+ cell and are no longer found in abundance in the marginal zone or the red pulp (8). Entry of Listeria into the white pulp leads to apoptosis of the splenic lymphocytes (9, 10), a process that we have proposed is catalyzed by the bacterial toxin listeriolysin O (11) and enhanced by the presence of type I IFN in the infected mouse (12, 13). Cell death induced by L. monocytogenes in the hematopoietic system may not be confined to the lymphocyte, as infected macrophages (14, 15) and dendritic cells (16) also die by necrosis or apoptosis. Apoptosis induced by L. monocytogenes can also be found in nonhematopoetic cells, such as the hepatocytes of the liver (17) and neurons of the hippocampus and cerebellum (18).
Several reports have suggested a correlation between lymphocyte apoptosis and increased susceptibility to L. monocytogenes infection. Type I IFN receptor–deficient (IFN-αβR−/−) mice were more resistant to infection (12, 13, 19) and displayed decreased lymphocyte apoptosis in the infected spleen (12, 13). It was proposed that the absence of lymphocyte apoptosis (12, 13), or survival of a subset of monocytes (19), during infection of IFN-αβR−/− mice could be related to the increased resistance to infection. Additionally, TRAIL-deficient mice were also more resistant to infection with L. monocytogenes and displayed decreased apoptosis of splenic cells (20).
We have proposed that lymphocyte apoptosis during listeriosis could be detrimental to the early innate immune response by triggering a cascade of events that inhibit the effector reactions (11, 12). Others have related death of cells to impaired inflammation. For example, culture experiments indicated that direct contact of apoptotic cells with macrophages enhanced Trypanosoma cruzi growth due to sensing of the apoptotic body by the infected macrophage (21). Apoptotic cells were shown to impair inflammatory responses by macrophages by promoting secretion of cytokines that antagonize inflammation, such as IL-10, prostaglandin E2, tumor growth factor β, and platelet-activating factor (22–25).
The main approach used here was to reconstitute immunodeficient mice with lymphocytes and then compare the early growth of L. monocytogenes. Immunodeficient mice engrafted with lymphocytes were more susceptible to early infection. However, mice engrafted with lymphocytes that were resistant to apoptosis harbored lower colony counts throughout infection. IL-10 produced by dendritic cells and macrophages was a key mediator of the increased susceptibility to listeriosis downstream of apoptosis. Our data suggests that L. monocytogenes has exploited host–cell death pathways to create an infective niche early during infection.
RESULTS
SCID mice are more resistant than wild-type mice
Normal and lymphocyte-deficient mice (either CB.17 SCID [SCID] or RAG2-deficient mice [RAG−/−] on the C57BL/6J or 129/SvEv strains) harbored equivalent numbers of L. monocytogenes in their spleens and livers at 6 h after infection. We used a high infectious dose in the experiment with SCID mice (depicted in Fig. 1 A) to reliably detect the numbers of bacteria in the spleens and livers. In contrast, at the fourth day of infection, normal mice had 103–104 more L. monocytogenes in their spleens and livers than SCID mice infected at the same dose (Fig. 1 B; reference 4). Our results were valid over a wide range of infectious doses (Fig. 1 C). Similar results were observed in RAG−/− mice on both the C57BL/6J and the 129/SvEv backgrounds, indicating that the increase in resistance was not peculiar to the SCID mutation or the genetic background (see below). By days 8–12, the normal mice cleared the infection, whereas the immunodeficient strains maintained a burden of L. monocytogenes in the livers and spleens (not depicted and references 1, and 3–5).
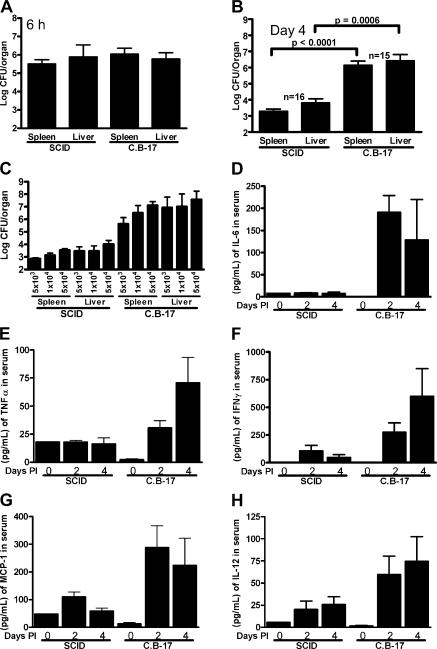
Figure 1.
SCID mice are more resistant to L. monocytogenes growth than wild-type C.B-17 mice. (A) Mice were infected with 107 CFU and colony counts were determined after 6 h. (B) Mice were infected with 5 × 104 CFU and colony counts were determined at day 4 after infection. (C) SCID and C.B-17 mice were infected with the indicated doses, and spleen and liver colony counts were determined at day 4 of infection. All bars represent the mean ± SEM for 5–16 mice per group. (D) IL-6, (E) TNF-α, (F) IFN-γ, (G) MCP-1, and (H) IL-12 were determined for C.B-17 and SCID mice infected with 5 × 104 CFU at the indicated times after infection.
A constitutively activated innate immune system, or more rapid activation or expansion of it after infection, could explain the increased resistance of immunodeficient mice. Macrophages taken from normal and SCID mice controlled in vitro infection with L. monocytogenes equivalently, indicating that the cells were not activated before infection (26). Furthermore, the level of MHC class II molecules on peritoneal macrophages, an indication of their state of activation, was comparable between wild-type and SCID mice before infection (10% I-Ad high cells) and throughout the first 4 d of infection (75% positive cells; not depicted and references 4 and 27). In addition, SCID mice produced significantly lower levels of IL-6, TNF-α, IFN-γ, monocyte chemoattractant protein 1 (MCP-1), and IL-12 than the normal mice throughout the course of infection (Fig. 1, D–H). Therefore, there was not an enhanced cytokine response in the SCID mice early during infection that could account for their increased resistance.
Lastly, the differences in L. monocytogenes growth between immunodeficient and normal mice could not be explained by the presence of serum immunoglobulin in the latter (28). After infection, SCID mice that received 500 μl of normal serum had colony counts comparable to mock-treated mice (a mean of 2.5 × 103 and 5 × 103 CFU in the spleens and 3.2 × 104 and 1.6 × 105 CFU in the livers for untreated and serum-treated mice, respectively, at day 4 after infection). Thus, the increased resistance of immunocompromised strains of mice was not explained by constitutively activated macrophages, a more robust cytokine response early during infection, or natural antibody.
Listeriosis in lymphocyte-reconstituted RAG−/− mice
Another way to explain the differences in L. monocytogenes growth at the early stage of the infection is to posit that the normal mice exhibit an immunologically unfavorable environment that is absent in the immunodeficient counterpart. Thus, our attention turned to events that involve lymphocytes early in the infection, and in this context, death of lymphocytes is a striking event in the initial stage of listeriosis (9, 10, 12, 13). To evaluate if dying lymphocytes were responsible for an increased susceptibility to L. monocytogenes infection, lethally irradiated RAG−/− mice were engrafted with two types of bone marrow cells: 129/SvEv bone marrow, which duplicated the normal situation, or bone marrow from IFN-αβR−/− mice. We have shown that lymphocyte apoptosis triggered by the L. monocytogenes protein listeriolysin O is enhanced if the cells are activated with antigen or treated with IFN-αA (11, 12). Thus, bone marrow from IFN-αβR−/− mice was chosen because these mice were resistant to the induction of apoptosis triggered by L. monocytogenes infection and harbored lower colony counts throughout the course of infection (12, 13, 19). Indeed, the examination of the IFN-αβR−/− mice already suggested but did not prove that lymphocyte death could affect the infection. Others have indicated that Listeria infection also led to death of phagocytes (19).
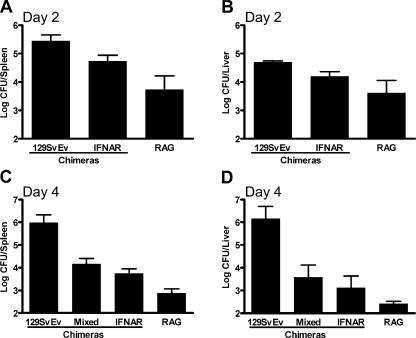
Before infection, engrafted mice had normal levels of T and B lymphocytes in the circulation and showed restored splenic morphology. At the second day of infection, there was a slightly higher bacterial burden in the mice that received lymphocytes (Fig. 2, A and B). By the fourth day of infection, the difference between the chimeric mice was profound. Mice engrafted with bone marrow cells from normal mice (129/SvEv in the figures) had 102–103 more bacteria in their spleens and livers compared with RAG−/− mice or mice that received IFN-αβR−/− bone marrow cells (Fig. 2, C and D). Therefore, engraftment of IFN-αβR+/+ lymphocytes was sufficient to restore the increased susceptibility to infection in RAG−/− mice.
Figure 2.
Engraftment of lymphocytes into RAG2−/− mice increases susceptibility to listeriosis. Lethally irradiated RAG2−/− recipients were engrafted with the indicated bone marrow donors (chimeras) for 70–80 d. All mice were infected with 2.5 × 104 L. monocytogenes. Colony counts were determined at (A and B) days 2 and (C and D) 4 after infection. For all graphs: 129SvEv, 129/SvEv→RAG2−/−; IFNAR, IFN-αβR−/−→RAG2−/−; mixed, a five to one RAG2−/− to IFN-αβR−/− mix→RAG2−/−; RAG, untransplanted RAG2−/− mice. All bars represent the mean ± SEM for four to nine mice per group.
L. monocytogenes infection can lead to death of both dendritic cells and macrophages. For the macrophages, type I IFN, which is produced in response to L. monocytogenes infection both in vivo and in vitro (15, 29, 30), has been shown to be a determinant of the death response. In the normal infected mice, apoptotic death occurs in both lymphocytes and phagocytes. Estimating the presence of apoptotic or dead phagocytes among the extensive lymphocyte apoptosis has been difficult. Ultrastructural studies of the infected foci have indicated the presence of dead macrophages containing L. monocytogenes as well as infected cells compatible with dendritic cells with apoptotic nuclei (unpublished data).
To distinguish if the apoptosis of one or both could affect the outcome of the infection, mixed chimeras were developed. Because the expression of IFN-αβR on macrophages has been associated with increased susceptibility to _L. monocytogenes_–induced cell death (15, 19), lethally irradiated RAG−/− mice were engrafted with a combination of RAG−/− and IFN-αβR−/− bone marrow (at a 5:1 ratio, referred to as “mixed chimeras”). This engraftment protocol resulted in a mixture of IFN-αβR−/− and IFN-αβR+/+ macrophages and IFN-αβR−/− lymphocytes. The myeloid compartment in these mice was mostly IFN-αβR+/+, whereas the lymphocytes were IFN-αβR−/− (80–95% IFN-αβR+/+/CD11b+ cells and >95% IFN-αβR−/−/CD3+ cells in the blood as determined by immunocytometry before infection).
Thus, these mice contained innate cells like macrophages and dendritic cells potentially sensitive to L. monocytogenes apoptosis but contained lymphocytes resistant to apoptosis. Infected mixed chimeras were also resistant to infection with L. monocytogenes, harboring 102 fewer bacteria in their spleens and livers than wild-type engrafted RAG−/− mice (Fig. 2, C and D). Importantly, there was no significant difference in the colony counts in the mixed chimera compared with the IFN-αβR−/− chimera, suggesting that sensitivity to infection caused by type I IFNs is dependent on lymphocytes (P = 0.2677 for spleen, P = 0.5303 for liver). Therefore, increased susceptibility to L. monocytogenes infection was caused by apoptosis promoted by type I IFN signaling on lymphocytes (Fig. 2, C and D).
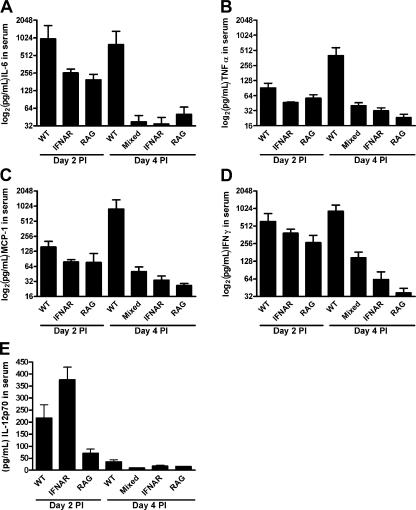
There are two additional points to note. First, the cytokine responses in the chimeras were similar to those found in SCID mice. Mice reconstituted with bone marrow from normal mice had higher cytokine responses throughout infection, whereas IFN-αβR−/− and mixed chimeras and untransplanted RAG−/− mice had relatively low levels (Fig. 3, A–E). Second, histological examination revealed that IFN-αβR−/− mice and chimeras that received IFN-αβR−/− cells showed considerably less apoptotic lymphocytes in infective foci (Fig. 4, A–F; references 12 and 13). In contrast, the spleens of uninfected SCID mice or SCID mice after infection contained a few apoptotic splenocytes throughout the atrophic white pulp and the red pulp (Fig. 4 D).
Figure 3.
Increased inflammatory cytokine responses in 129/SvEv engrafted RAG2−/− mice. Mice were transplanted and infected i.p. with 2.5 × 104 L. monocytogenes. Serum levels of (A) IL-6, (B) TNF-α, (C) MCP-1, (D) IFN-γ, and (E) IL-12p70 were determined at days 2 and 4 after infection as indicated on the graphs. For all graphs: 129/SvEv, 129→RAG2−/−; IFNAR, IFN-αβR−/−→RAG2−/−; mixed, a five to one RAG2−/− to IFN-αβR−/−→RAG2−/−; RAG, untransplanted RAG2−/− mice. All bars indicate the mean ± SEM for 4–10 mice per group.
Figure 4.
Histological analysis of bone marrow chimeras infected with L. monocytogenes. Mice were chimerized as described in the legend to Fig. 2. Spleens from mice infected with 2.5 × 104 CFU of L. monocytogenes EGD strain were stained as described previously by (A, C, and E) H&E or (B, D, and F) TUNEL. Results are shown for (A and B) 129/SvEv→RAG2−/− chimeras, (C and D) IFN-αβR−/−→RAG2−/− chimeras, or untransplanted RAG2−/− mice. Of note is the dramatic lymphocyte apoptosis found only in 129/SvEV chimeras but not IFN-αβR−/− chimeras. Bar, 50 μM.
Type I IFN in the SCID mouse
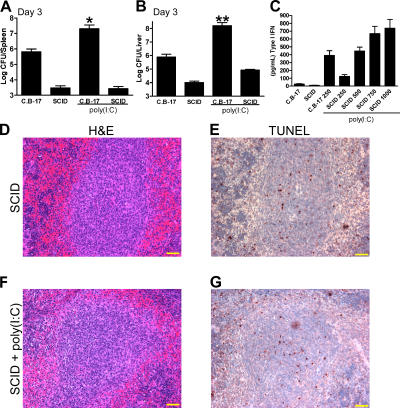
It has been reported that type I IFN is produced during infection of the mouse (30) and of macrophages in culture (15, 29) with virulent L. monocytogenes. The relationship between the lymphocyte apoptotic response brought about by type I IFNs and the resistance of immunodeficient strains of mice was further evaluated using poly(I:C). Poly(I:C) treatment induces type I IFN production and enhanced L. monocytogenes infection in normal mice (13). The enhancement of L. monocytogenes growth driven by poly(I:C) treatment is dependent on the expression of IFN-αβR, as mice deficient in the receptor show no difference in the handling of the infection when compared with the wild-type mice. Indeed, normal mice injected with 250 μg poly(I:C) had a 20- and 100-fold increase in colony counts in their spleens and livers after 3 d of infection (Fig. 5, A and B). Fig. 5 C shows that SCID mice required an injection of 500 μg poly(I:C) to have the same level of circulating type I IFN as C.B-17 mice treated with 250 μg poly(I:C). SCID mice that received 500 μg poly(I:C) showed bacterial burdens not significantly higher than the untreated SCID mice in the spleen and only marginally higher in the liver. Cytokine levels were comparable to our previous observations, as poly(I:C) treatment enhanced the inflammatory cytokine production in normal but not in SCID mice (not depicted). By histology, there was limited apoptosis in either SCID mice or SCID mice treated with poly(I:C) after infection (Fig. 5, E–G). However, normal mice treated with poly(I:C) had extensive lymphocyte apoptosis (not depicted and reference 13). The results with poly(I:C)-treated mice further bolster the claim that the cellular target of type I IFN sensitization during listeriosis was the lymphocyte, and without lymphocytes, as shown with the response of the SCID mice, there was no untoward effect of type I IFN induction.
Figure 5.
Effect of poly(I:C) on listeriosis in SCID mice. (A and B) C.B-17 or SCID mice were left untreated or were treated with 250 (C.B-17) or 500 μg (SCID) poly(I:C) i.v. and then infected with 5 × 104 L. monocytogenes strain EGD i.p. (A) Spleen and (B) liver colony counts were determined at day 3 after infection. (C) SCID and C.B-17 mice were injected with the indicated doses of poly(I:C) i.v. for 6 h, and type I IFN levels were measured in the serum. Bars represent the mean ± SEM for 8–14 mice per group. (D and E) SCID and (F and G) SCID mice treated with 500 μg poly(I:C) were infected for 3 d with 5 × 104 L. monocytogenes EGD strain, and spleen sections were stained by (D and F) H&E or (E and G) by TUNEL. Yellow bars, 50 μm. *, P = 0.0002; **, P < 0.0001 by Mann-Whitney U test.
IL-10 slows L. monocytogenes control
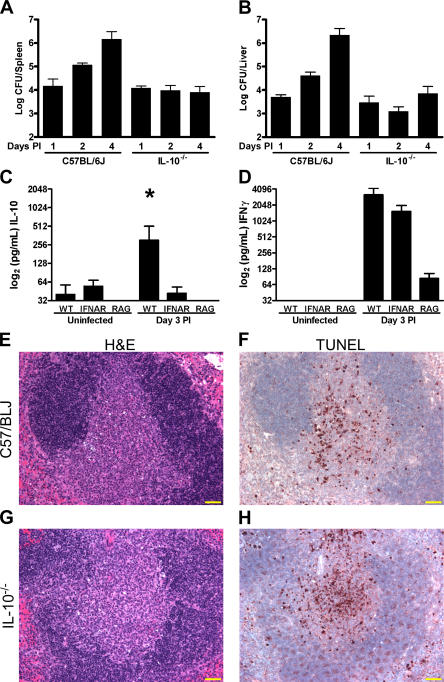
To explore the mechanisms underlying the effects, we considered whether the extensive lymphocyte apoptosis induced by L. monocytogenes infection could induce antiinflammatory proteins in the infective foci. These would be absent in the SCID or RAG−/− mice devoid of lymphocytes. IL-10 inhibits L. monocytogenes resistance and is known to be produced by macrophages (22, 31). Therefore, IL-10–deficient mice infected with L. monocytogenes were examined for the presence of apoptotic lymphocytes and their resistance to infection. In agreement with previous reports (32), mice lacking IL-10 (IL-10−/−) were more resistant to L. monocytogenes infection, with 102–103 fewer colony counts in their spleens and livers relative to normal controls at day 4 after infection (Fig. 6, A–C). Histological examination of IL-10−/− mice revealed that the infective foci in the periarteriolar lymphoid sheath of the white pulp contained extensive lymphocyte apoptosis (Fig. 6, E–H) essentially similar to normal mice. For one representative experiment, 37% (19/51, n = 5) of the white pulp profiles of normal mice contained apoptotic profiles versus 29% (17/59, n = 4) in IL-10−/− mice. Apoptotic lesions ranged from mild (affecting <50% of the white pulp) to extensive (affecting >75% of the white pulp) for both groups of mice. Therefore, IL-10−/− mice displayed increased resistance to infection in the presence of apoptotic cells, indicating that IL-10 could be an effector of susceptibility to listeriosis downstream of dying cells.
Figure 6.
Increased resistance to listeriosis in IL-10−/− mice. (A and B) C57BL/6J and IL-10−/− mice were infected with 105 L. monocytogenes and colony counts were determined for the (A) spleen and (B) liver at the indicated days. Levels of (C) IL-10 and (D) IFN-γ were determined for cell-free spleen homogenates of uninfected or infected 129/SvEv, IFN-αβR−/−, or RAG2−/− mice as indicated on the graph. All bars represent the mean ± SEM for at least 4–10 mice per group. *, P = 0.0104, Mann-Whitney U test. Serial sections were made from the spleens of (E and G) C57/BL6J or (F and H) IL-10−/− mice and stained by (E and F) H&E or (G and H) TUNEL. Yellow bars, 50 μm.
If induction of IL-10 is related to the death of lymphocytes, we would expect to find lower levels of IL-10 in RAG−/− and IFN-αβR−/− mice. This was indeed the case as levels of IL-10 extracted from the spleens of infected mice were significantly higher in normal mice than in IFN-αβR−/− and RAG−/− mice at the third day of infection (Fig. 6 C). Levels of IL-6, IFN-γ, IL-12, MCP-1, and TNF-α from the spleens were similar to those found in circulation. Only the data on IFN-γ is presented in Fig. 6 D showing high levels in the normal and IFN-αβR−/− mice compared with the RAG−/− mice. IL-10 can be produced by lymphocytes, dying macrophages, or macrophages that have ingested apoptotic bodies (22, 33), but the source during L. monocytogenes infection is unknown. We determined that the spleens of _L. monocytogenes_–infected mice contained innate cells that generated IL-10: 0.012% of the CD11b+ and 0.091% of the CD11c+ cells isolated from infected wild-type mice were positive by IL-10 ELISPOT (two independent experiments, n = 4). The CD19+ and the CD19−/CD11b−/CD11c− populations of cells isolated from infected wild-type mice contained no detectable IL-10–producing cells. No IL-10–producing cells were found in the spleen cells taken from uninfected mice or the infected RAG−/− or IFN-αβR−/− mice.
DISCUSSION
These results establish that the increased susceptibility to listeriosis of normal versus immunodeficient mice is because of the presence of lymphocytes and specifically of lymphocytes that die during the first 2 d of infection. Constitutive or enhanced activation of the innate immune system of immunodeficient mice could not account for the increased resistance. Moreover, the mixed chimera experiments indicated that IFN-αβR+/+ macrophages were not responsible for a negative effect in the presence of apoptosis-resistant lymphocytes from IFN-αβR−/− mice. Therefore, these findings link two previous observations: the increased resistance to infection in immunodeficient strains of mice (2–4) with the increased resistance to infection in IFN-αβR−/− mice (12, 13, 19). It supports the conclusion that the lymphocytes are detrimental to early host responses against this bacterial infection because of their sensitivity to apoptosis, a situation in which type I IFN and the L. monocytogenes protein listeriolysin O play a role (11–13). Collectively, the evidence indicates that there is a participation of IL-10 on L. monocytogenes control after the apoptotic lesion. Lack of IL-10 did not impair the apoptosis of lymphocytes but resulted in increased resistance. In this instance, lymphocyte apoptosis did not correlate with higher susceptibility. In addition, IL-10 was produced by phagocytes after lymphocyte apoptosis. We propose that IL-10 production was driven, in part, by the dying lymphocytes and that the antiinflammatory signaling of IL-10, and possibly other cytokines, enhanced early innate susceptibility to L. monocytogenes infection (21, 25). In summary, normal mice have a limited but susceptible period to infection triggered by a cascade of events in which lymphocyte apoptosis is prominent.
We envision the following scenario: the immediate infection by phagocytes releases cytokines, including type I IFNs (15, 29), while L. monocytogenes releases listeriolysin O, a protein that causes apoptosis of lymphocytes “primed” by type I IFNs (11, 12). Uptake of the dead cells leads to the release of IL-10 and other antiinflammatory molecules that results in an environment that hinders the early control of the infection. L. monocytogenes will grow exponentially in the milieu of dead cells and antiinflammatory cytokines that fosters its growth. Eventually this negative stage is superseded as phagocytes are able to control the growth of L. monocytogenes and the adaptive immune system is brought into operation (4, 34).
Our findings have important implications for our understanding of infection with intracellular bacterial pathogens as well as many important human pathogens. In the case of Yersinia enterocolitica, Mycobacterium bovis BCG, and Toxoplasma gondii, apoptosis can be associated with decreased host resistance and increased pathogen spread (35–37). Although apoptosis of infected cells is important in containing infections and promoting activation of the adaptive immune response (38), selective inhibition of lymphocyte death should be investigated as a potential therapeutic strategy against intracellular microbial infections (39). Although our focus has been to emphasize the deleterious effect of lymphocyte apoptosis on L. monocytogenes handling, it is possible that apoptosis at the same time has a positive effect, enhancing antigen presentation and adaptive immunity to infection (10, 38, 40).
MATERIALS AND METHODS
Mice and Listeria infection.
All mice were infected i.p. with varying doses of L. monocytogenes EGD strain in pyrogen-free saline. The doses used in each experiment are given in the figure legends. The 129/SvEv and IFN-αβR−/− mice were obtained from our own department (provided by H.W. Virgin). The 129/SvEv RAG2−/− mice were obtained from Taconic. The C57BL/6J and IL-10−/− deficient mice on a C57BL/6J background were obtained from The Jackson Laboratory. The C.B-17 and C.B-17 SCID (SCID) strains have been in continuous breeding in our colony since our initial report on macrophage activation in the SCID mouse (4). All mice were bred and maintained under specific pathogen-free conditions at the Washington University School of Medicine and were handled in accordance to the guidelines set forth by the Division of Comparative Medicine of Washington University. Colony counts were determined by titration on brain heart infusion agar (BHI) plates using conventional techniques. For all graphs, data were plotted using Prism software (Graphpad, Inc.). A Mann-Whitney unpaired test with two-tailed p-values and 95% confidence intervals was used for all statistical analyses.
For all bone marrow engraftment protocols, donor cells were isolated from mice treated with 5-fluorouracil (Sigma-Aldrich) for 3–5 d before mice were killed. Recipient mice received a single lethal 9.50-Gy dose using a cesium source and were engrafted with 105 to 5 × 105 bone marrow cells i.v. Transplanted mice were given water supplemented with antibiotic (trimethoprim-sulfamethoxazole) ad libitum for 2 wk and were allowed to engraft for a minimum of 70 d before infection with L. monocytogenes. Mice were phenotyped by peripheral blood cell analysis by immunocytometry with antibodies against CD3, CD11b, and CD19 (BD Biosciences), and anti–IFN-αβR (R.D. Schreiber, Washington University, Saint Louis, MO). For poly(I:C) experiments, mice were injected i.v. with 250–1,000 μg poly(I:C) (Sigma-Aldrich) dissolved in pyrogen-free saline immediately before i.p. infection with L. monocytogenes.
Histology.
All histological analysis was performed on paraffin-embedded formalin-fixed tissue sections and stained by hematoxylin and eosin (H&E). TUNEL assays were performed using standard protocols.
Cytokines.
Levels of IL-6, IL-12, MCP-1, IFN-γ, IL-10, and TNF-α were determined by Cytometric Bead Array (BD Biosciences) analysis as described previously (12). Type I IFNs in the sera of mice 6 h after i.v. injection with 250–1,000 μg poly(I:C) were determined using the Mouse IFN-α ELISA kit (PBL Biomedical Laboratories). For IL-10 determination, spleens of infected mice were disrupted in 1 ml of ice-cold phosphate-buffered saline using a homogenizer. Cells were lysed by freezing at −80°C, and cell-free supernatants were collected after centrifugation for 10 min at 10,000 g. IL-10 levels in spleen extract were determined using the OptEIA IL-10 ELISA kit (BD Biosciences). IL-10 ELISPOT was performed using the Mouse IL-10 ELISPOT Pair (BD Biosciences) on cells fractionated using magnetic bead separation (Miltenyi Biotec). Both cell separation and IL-10 ELISPOT were performed using the manufacturer's protocols.
Acknowledgments
We would like to thank Kathy Frederick for her animal husbandry and help with experiments involving mice. We would like to acknowledge Dr. Brian T. Edelson and Dr. Anish Suri for many helpful discussions and experimental advice, and Scott B. Lovitch for helpful discussions and a critical reading of the manuscript. We thank Drs. Robert D. Schreiber, Herbert W. Virgin IV, and Wayne M. Yokoyama for a critical reading of the manuscript. Dr. Kathy C. Sheehan and Dr. Robert D. Schreiber provided the anti–IFN-αβR antibody, and Dr. Herbert W. Virgin IV provided the IFN-αβR−/− mice.
This work was supported by a grant (no. 1RO1AI062832) from the National Institutes of Health to E.R. Unanue. J.A. Carrero is a trainee on a Training Program in Immunology and Immunogenetics grant (no. 5T32AI007163).
The authors have no conflicting financial interests.
Abbreviations used: H&E, hematoxylin and eosin; IFN-αβR−/−, type I IFN receptor–deficient; MCP-1, monocyte chemoattractant protein 1.
References
- 1.Emmerling, P., H. Finger, and J. Bockemuhl. 1975. Listeria monocytogenes infection in nude mice. Infect. Immun. 12:437–439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Skamene, E., and W. Chayasirisobhon. 1977. Enhanced resistance to Listeria monocytogenes in splenectomized mice. Immunology. 33:851–858. [PMC free article] [PubMed] [Google Scholar]
- 3.Newborg, M.F., and R.J. North. 1980. On the mechanism of T cell-independent anti-Listeria resistance in nude mice. J. Immunol. 124:571–576. [PubMed] [Google Scholar]
- 4.Bancroft, G.J., M.J. Bosma, G.C. Bosma, and E.R. Unanue. 1986. Regulation of macrophage Ia expression in mice with severe combined immunodeficiency: induction of Ia expression by a T cell-independent mechanism. J. Immunol. 137:4–9. [PubMed] [Google Scholar]
- 5.Bhardwaj, V., O. Kanagawa, P.E. Swanson, and E.R. Unanue. 1998. Chronic Listeria infection in SCID mice: requirements for the carrier state and the dual role of T cells in transferring protection or suppression. J. Immunol. 160:376–384. [PubMed] [Google Scholar]
- 6.Conlan, J.W. 1996. Early pathogenesis of Listeria monocytogenes infection in the mouse spleen. J. Med. Microbiol. 44:295–302. [DOI] [PubMed] [Google Scholar]
- 7.Aichele, P., J. Zinke, L. Grode, R.A. Schwendener, S.H. Kaufmann, and P. Seiler. 2003. Macrophages of the splenic marginal zone are essential for trapping of blood-borne particulate antigen but dispensable for induction of specific T cell responses. J. Immunol. 171:1148–1155. [DOI] [PubMed] [Google Scholar]
- 8.Muraille, E., R. Giannino, P. Guirnalda, I. Leiner, S. Jung, E.G. Pamer, and G. Lauvau. 2005. Distinct in vivo dendritic cell activation by live versus killed Listeria monocytogenes. Eur. J. Immunol. 35:1463–1471. [DOI] [PubMed] [Google Scholar]
- 9.Merrick, J.C., B.T. Edelson, V. Bhardwaj, P.E. Swanson, and E.R. Unanue. 1997. Lymphocyte apoptosis during early phase of Listeria infection in mice. Am. J. Pathol. 151:785–792. [PMC free article] [PubMed] [Google Scholar]
- 10.Jiang, J., L.L. Lau, and H. Shen. 2003. Selective depletion of nonspecific T cells during the early stage of immune responses to infection. J. Immunol. 171:4352–4358. [DOI] [PubMed] [Google Scholar]
- 11.Carrero, J.A., B. Calderon, and E.R. Unanue. 2004. Listeriolysin O from Listeria monocytogenes is a lymphocyte apoptogenic molecule. J. Immunol. 172:4866–4874. [DOI] [PubMed] [Google Scholar]
- 12.Carrero, J.A., B. Calderon, and E.R. Unanue. 2004. Type I interferon sensitizes lymphocytes to apoptosis and reduces resistance to Listeria infection. J. Exp. Med. 200:535–540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.O'Connell, R.M., S.K. Saha, S.A. Vaidya, K.W. Bruhn, G.A. Miranda, B. Zarnegar, A.K. Perry, B.O. Nguyen, T.F. Lane, T. Taniguchi, et al. 2004. Type I interferon production enhances susceptibility to Listeria monocytogenes infection. J. Exp. Med. 200:437–445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Barsig, J., and S.H. Kaufmann. 1997. The mechanism of cell death in _Listeria monocytogenes_-infected murine macrophages is distinct from apoptosis. Infect. Immun. 65:4075–4081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stockinger, S., T. Materna, D. Stoiber, L. Bayr, R. Steinborn, T. Kolbe, H. Unger, T. Chakraborty, D.E. Levy, M. Muller, and T. Decker. 2002. Production of type I IFN sensitizes macrophages to cell death induced by Listeria monocytogenes. J. Immunol. 169:6522–6529. [DOI] [PubMed] [Google Scholar]
- 16.Guzman, C.A., E. Domann, M. Rohde, D. Bruder, A. Darji, S. Weiss, J. Wehland, T. Chakraborty, and K.N. Timmis. 1996. Apoptosis of mouse dendritic cells is triggered by listeriolysin, the major virulence determinant of Listeria monocytogenes. Mol. Microbiol. 20:119–126. [DOI] [PubMed] [Google Scholar]
- 17.Rogers, H.W., M.P. Callery, B. Deck, and E.R. Unanue. 1996. Listeria monocytogenes induces apoptosis of infected hepatocytes. J. Immunol. 156:679–684. [PubMed] [Google Scholar]
- 18.Schluter, D., E. Domann, C. Buck, T. Hain, H. Hof, T. Chakraborty, and M. Deckert-Schluter. 1998. Phosphatidylcholine-specific phospholipase C from Listeria monocytogenes is an important virulence factor in murine cerebral listeriosis. Infect. Immun. 66:5930–5938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Auerbuch, V., D.G. Brockstedt, N. Meyer-Morse, M. O'Riordan, and D.A. Portnoy. 2004. Mice lacking the type I interferon receptor are resistant to Listeria monocytogenes. J. Exp. Med. 200:527–533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zheng, S.J., J. Jiang, H. Shen, and Y.H. Chen. 2004. Reduced apoptosis and ameliorated listeriosis in TRAIL-null mice. J. Immunol. 173:5652–5658. [DOI] [PubMed] [Google Scholar]
- 21.Freire-de-Lima, C.G., D.O. Nascimento, M.B. Soares, P.T. Bozza, H.C. Castro-Faria-Neto, F.G. de Mello, G.A. DosReis, and M.F. Lopes. 2000. Uptake of apoptotic cells drives the growth of a pathogenic trypanosome in macrophages. Nature. 403:199–203. [DOI] [PubMed] [Google Scholar]
- 22.Voll, R.E., M. Herrmann, E.A. Roth, C. Stach, J.R. Kalden, and I. Girkontaite. 1997. Immunosuppressive effects of apoptotic cells. Nature. 390:350–351. [DOI] [PubMed] [Google Scholar]
- 23.Fadok, V.A., D.L. Bratton, A. Konowal, P.W. Freed, J.Y. Westcott, and P.M. Henson. 1998. Macrophages that have ingested apoptotic cells in vitro inhibit proinflammatory cytokine production through autocrine/paracrine mechanisms involving TGF-beta, PGE2, and PAF. J. Clin. Invest. 101:890–898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Savill, J., and V. Fadok. 2000. Corpse clearance defines the meaning of cell death. Nature. 407:784–788. [DOI] [PubMed] [Google Scholar]
- 25.Savill, J., I. Dransfield, C. Gregory, and C. Haslett. 2002. A blast from the past: clearance of apoptotic cells regulates immune responses. Nat. Rev. Immunol. 2:965–975. [DOI] [PubMed] [Google Scholar]
- 26.Edelson, B.T., and E.R. Unanue. 2001. Intracellular antibody neutralizes Listeria growth. Immunity. 14:503–512. [DOI] [PubMed] [Google Scholar]
- 27.Rogers, H.W., K.C. Sheehan, L.M. Brunt, S.K. Dower, E.R. Unanue, and R.D. Schreiber. 1992. Interleukin 1 participates in the development of anti-Listeria responses in normal and SCID mice. Proc. Natl. Acad. Sci. USA. 89:1011–1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ochsenbein, A.F., T. Fehr, C. Lutz, M. Suter, F. Brombacher, H. Hengartner, and R.M. Zinkernagel. 1999. Control of early viral and bacterial distribution and disease by natural antibodies. Science. 286:2156–2159. [DOI] [PubMed] [Google Scholar]
- 29.O'Riordan, M., C.H. Yi, R. Gonzales, K.D. Lee, and D.A. Portnoy. 2002. Innate recognition of bacteria by a macrophage cytosolic surveillance pathway. Proc. Natl. Acad. Sci. USA. 99:13861–13866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Serbina, N.V., T.P. Salazar-Mather, C.A. Biron, W.A. Kuziel, and E.G.P. Am. 2003. TNF/iNOS-producing dendritic cells mediate innate immune defense against bacterial infection. Immunity. 19:59–70. [DOI] [PubMed] [Google Scholar]
- 31.Tripp, C.S., S.F. Wolf, and E.R. Unanue. 1993. Interleukin 12 and tumor necrosis factor alpha are costimulators of interferon gamma production by natural killer cells in severe combined immunodeficiency mice with listeriosis, and interleukin 10 is a physiologic antagonist. Proc. Natl. Acad. Sci. USA. 90:3725–3729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dai, W.J., G. Kohler, and F. Brombacher. 1997. Both innate and acquired immunity to Listeria monocytogenes infection are increased in IL-10-deficient mice. J. Immunol. 158:2259–2267. [PubMed] [Google Scholar]
- 33.Byrne, A., and D.J. Reen. 2002. Lipopolysaccharide induces rapid production of IL-10 by monocytes in the presence of apoptotic neutrophils. J. Immunol. 168:1968–1977. [DOI] [PubMed] [Google Scholar]
- 34.Unanue, E.R. 1997. Studies in listeriosis show the strong symbiosis between the innate cellular system and the T-cell response. Immunol. Rev. 158:11–25. [DOI] [PubMed] [Google Scholar]
- 35.Monack, D.M., J. Mecsas, D. Bouley, and S. Falkow. 1998. Yersinia-induced apoptosis in vivo aids in the establishment of a systemic infection of mice. J. Exp. Med. 188:2127–2137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kremer, L., J. Estaquier, I. Wolowczuk, F. Biet, J.C. Ameisen, and C. Locht. 2000. Ineffective cellular immune response associated with T-cell apoptosis in susceptible Mycobacterium bovis BCG-infected mice. Infect. Immun. 68:4264–4273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Luder, C.G., and U. Gross. 2005. Apoptosis and its modulation during infection with Toxoplasma gondii: molecular mechanisms and role in pathogenesis. Curr. Top. Microbiol. Immunol. 289:219–237. [DOI] [PubMed] [Google Scholar]
- 38.Winau, F., G. Hegasy, S.H. Kaufmann, and U.E. Schaible. 2005. No life without death—apoptosis as prerequisite for T cell activation. Apoptosis. 10:707–715. [DOI] [PubMed] [Google Scholar]
- 39.Hotchkiss, R.S., K.C. Chang, P.E. Swanson, K.W. Tinsley, J.J. Hui, P. Klender, S. Xanthoudakis, S. Roy, C. Black, E. Grimm, et al. 2000. Caspase inhibitors improve survival in sepsis: a critical role of the lymphocyte. Nat. Immunol. 1:496–501. [DOI] [PubMed] [Google Scholar]
- 40.Grode, L., P. Seiler, S. Baumann, J. Hess, V. Brinkmann, A. Nasser Eddine, P. Mann, C. Goosmann, S. Bandermann, D. Smith, et al. 2005. Increased vaccine efficacy against tuberculosis of recombinant Mycobacterium bovis bacille Calmette-Guerin mutants that secrete listeriolysin. J. Clin. Invest. 115:2472–2479. [DOI] [PMC free article] [PubMed] [Google Scholar]