Quantitative Impact of Thymic Clonal Deletion on the T Cell Repertoire (original) (raw)
Abstract
Interactions between major histocompatibility complex (MHC) molecules expressed on stromal cells and antigen-specific receptors on T cells shape the repertoire of mature T lymphocytes emerging from the thymus. Some thymocytes with appropriate receptors are stimulated to undergo differentiation to the fully mature state (positive selection), whereas others with strongly autoreactive receptors are triggered to undergo programmed cell death before completing this differentiation process (negative selection). The quantitative impact of negative selection on the potentially available repertoire is currently unknown. To address this issue, we have constructed radiation bone marrow chimeras in which MHC molecules are present on radioresistant thymic epithelial cells (to allow positive selection) but absent from radiosensitive hematopoietic elements responsible for negative selection. In such chimeras, the number of mature thymocytes was increased by twofold as compared with appropriate control chimeras. This increase in steady-state numbers of mature thymocytes was not related to proliferation, increased retention, or recirculation and was accompanied by a similar two- to threefold increase in the de novo rate of generation of mature cells. Taken together, our data indicate that half to two-thirds of the thymocytes able to undergo positive selection die before full maturation due to negative selection.
Tlymphocytes express a heterodimeric αβ TCR that recognizes peptides bound to cell surface molecules encoded by the MHC. Whereas TCRs expressed on mature CD4+ T helper cells respond to peptides associated with MHC class II, CD8+ cytotoxic cells express MHC class I–restricted TCRs (1). For effective maturation in the thymus, precursor T cells need to undergo a suitable interaction between their clonotypic TCR and MHC–peptide ligands expressed on thymic cortical epithelium (2, 3), though minor exceptions to this rule have been reported (4–7).
To avoid potentially pathogenic responses to self-peptide–MHC complexes, precursor T lymphocytes are monitored for strong autoreactivity during intrathymic development and after emergence in the periphery (8, 9). Many self-reactive T cells are physically deleted by induction of programmed cell death. While some clonal deletion can occur in response to MHC–peptide ligands expressed on thymic epithelium (10–17), the main cell type involved in this process is known to be of hematopoietic origin (2). In normal mice expressing endogenous mouse mammary tumor virus (MMTV)1–encoded superantigens that interact with TCRs containing particular Vβ elements, or in transgenic mice with predominant expression of both a single TCR and its cognate ligand, deletion of developing thymocytes can markedly decrease the total number of T cells undergoing full maturation (18–20). Moreover, in transgenic mice expressing MHC molecules associated with either a single or highly predominant peptide, a strong reactivity of mature T cells to normal syngeneic MHC is observed, indicating that many of these T cells under normal circumstances would have been tolerized during development (21–24). It has recently been shown that thymocytes and peripheral T cells from mice expressing MHC class II molecules only on thymic cortical epithelium react to the same MHC presented by professional APCs (25), confirming that thymic medullary epithelial cells and hematopoietic elements normally induce T cell tolerance. However, it remains unclear whether active deletion of thymocytes potentially capable of effective positive selection in the presence of the usual diverse array of peptide–MHC complexes displayed on thymic stromal cells involves a small or large proportion of this population. This is a critical issue for a full understanding of the events involved in intrathymic T cell development, construction of a useful repertoire, and characterization of the ligands involved in these processes (3). In this study, we analyze the quantitative impact of thymic clonal deletion mediated by cells of hematopoietic origin using bone marrow chimeras with different combinations of MHC deficiencies.
Materials and Methods
Mice.
Wild-type mice were C57BL/6 (H-2b haplotype) (see Fig. 1; Jackson Laboratories, Bar Harbor, ME; other experiments, Harlan Netherlands, Zeist, The Netherlands). Mice deficient in MHC class I expression (MHC I°) because of a targeted disruption of the β2-microglobulin gene (26) were obtained from Dr. B. Koller and Genpharm (Mountain View, CA). Mice of H-2b haplotype (I-Eα−) with an introduced null mutation in the I-Aβ b gene (27), and therefore deficient in MHC class II expression (MHC II°), were obtained from Dr. L. Glimcher and Genpharm and used in the experiment shown in Fig. 1. In all other experiments, mice deficient in MHC class II expression due to an induced disruption of the I-Aα b gene (28) in C57BL/6 stem cells (I-Eα−) were used (provided by Dr. H. Bluethmann, Basel, Switzerland). MHC I° and MHC II° animals were interbred in our facilities to obtain MHC I°II° mice. The β2-microglobulin–deficient mice, as well as the I-Aβ b mutants, were crossed at least six generations to C57BL/6 mice, after which intercrossing yielded mice homozygous for the disrupted alleles.
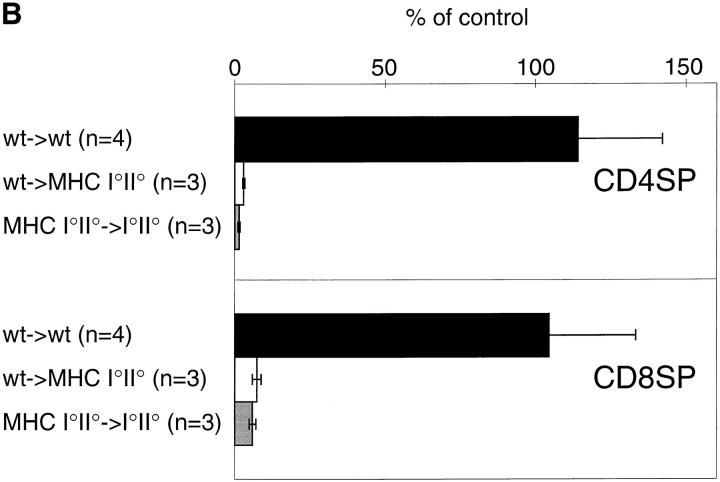
Figure 1.
Positive selection depends on expression of MHC molecules on radioresistant thymic epithelial cells. (A) Thymi from wild-type→ wild-type, MHC I°II°→ I°II°, and wild-type→ I°II° chimeras were analyzed by flow cytometry 6 wk after grafting. Thymocytes were stained with anti-CD8, anti-TCR, and anti-CD4 antibodies and analyzed on a FACScan® using LYSYS II software. Contour plots are 75% logarithmic and TCR histograms are from total thymus and from electronically gated cells using the gates indicated in the figure. (B) Percentages of CD4SP (CD4+CD8− TCRhigh) and CD8SP cells (CD4−CD8+TCRhigh) in thymi from the indicated chimeras were determined and depicted as percentage of an age- and sex-matched nonchimeric control mouse ± SD.
Chimeras.
Chimeras were prepared essentially as described previously (29). In brief, hosts were lethally irradiated (1,000 rads) with a Cs137 source and injected the next day i.v. with 10–20 × 106 bone marrow cells depleted of T cells by complement killing using anti-Thy1 antibody JIJ (30) and anti-Ly1 antibody C3P0 (31) in the experiment shown in Fig. 1 and anti-Thy1 antibody AT83 (32) in other experiments.
Three-color Flow Cytometry.
Single-cell suspensions of thymocytes were incubated on ice with saturating concentrations of the following antibodies: Fig. 1, anti-CD8–FITC, anti-TCR–PE (PharMingen, San Diego, CA), and anti-CD4–Red613 (GIBCO BRL, Gaithersburg, MD); Figs. 2 and 4, anti-TCR–FITC (H57-597), anti-CD4–PE (_Boehringer_-Mannheim, Mannheim, Federal Republic of Germany), and anti-CD8–Red613 (GIBCO BRL, Gaithersburg, MD). The samples were analyzed on a FACScan® using LYSYS II software (Becton Dickinson, Mountain View, CA).
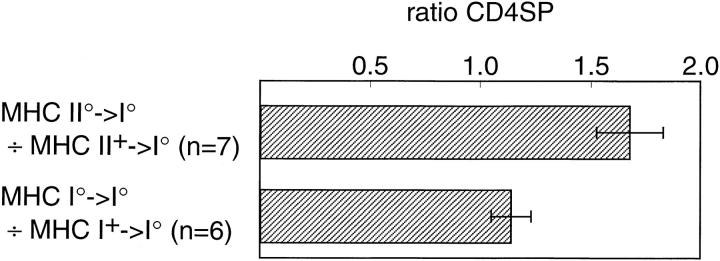
Figure 2.
Increased CD4SP (CD4+CD8−TCRhigh) thymocytes in chimeras lacking MHC class II expression on hematopoietic elements. Groups of sex- and age-matched chimeras were analyzed on the same day 6–8 wk after engraftment. Flow cytometry was performed using antiTCR, anti-CD4, and anti-CD8 antibodies. In each experiment, the ratio of CD4SP cells in the indicated groups was calculated. Error bars indicate SD. The increased ratio of CD4SP cells in MHC II°→ MHC I° versus MHC II+→ MHC I° chimeras is statistically significant as assessed by the Student's t test (P <0.0001), whereas the ratio of CD4SP thymocytes in MHC I°→ MHC I° versus MHC I+→ MHC I° chimeras is not significantly increased (P = 0.02).
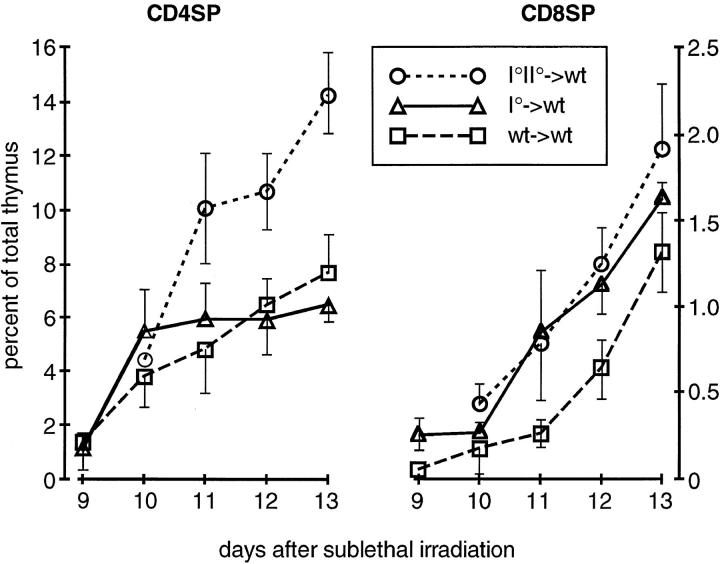
Figure 4.
Accelerated kinetics of generation of CD4SP and CD8SP thymocytes in wild-type hosts lacking MHC class II or I, respectively, on hematopoietic elements. 6-wk-old wt→ wt (n = 3, day 9; n = 6, days 10– 13), MHC I°II°→ wt (n = 3 each day), and MHC I°→ wt (n = 3) chimeras were sublethally irradiated (720 rads) and analyzed on day 9–13 as in Fig. 2. Data represent average percentage of CD4+CD8−TCRhigh and CD4−CD8+TCRhigh thymocytes ± SD.
Four-Color Flow Cytometry.
Single-cell suspensions of thymocytes were incubated on ice with saturating concentrations of the following antibodies: FITC-labeled anti-CD44 (Pgp-1) mAb IM7.8.1 (33), FITC-labeled anti-heat soluble antigen (HSA) mAb M1/69 (34) or FITC-labeled anti-CD69 mAb H1-2F3 (35), combined with anti-TCR–PE (PharMingen, San Diego, CA), antiCD8–Red613 (GIBCO BRL, Gaithersburg, MD), and anti-CD4– bio mAb GK1.5 (36) followed by streptavidin–APC. Four-color flow cytometry was performed on a FACStar Plus® using LYSYS II software (Becton Dickinson, Mountain View, CA).
Kinetics of Generation of Mature Thymocytes.
Chimeras were sublethally irradiated (720 rads, Cs137 source) 6 wk after engraftment and thymocytes analyzed 9–13 d later by flow cytometry. CD4 single-positive (CD4SP) cells are CD4+CD8−TCRhigh and CD8SP cells are CD4−CD8+TCRhigh.
Results and Discussion
To determine the quantitative impact of thymic clonal deletion on the T cell repertoire, we have examined thymocyte development in radiation bone marrow chimeras of H-2b haplotype in which MMTV superantigen–mediated deletion is not a significant factor (18, 19). Chimeras in which the donor bone marrow was from wild-type (wt) mice and the lethally irradiated host animals were deficient in both MHC class I and II expression (wt→ MHC I°II° chimeras) (37, 38) lacked significant numbers of mature CD4+8− or CD4−8+TCRhigh thymocytes (CD4SP and CD8SP, respectively; Fig. 1 A). A quantitative assessment reveals the development of less than 3% of wt levels of CD4SP cells and less than 8% of CD8SPs in such chimeras (Fig. 1 B). These results confirm previous data showing that efficient positive selection depends on expression of MHC molecules on radioresistant thymic epithelial cells (2, 3) and indicate that in the system used here the previously reported low level of T cell differentiation induced by hematopoietic elements (4–7) plays a negligible role.
Experiments were then conducted to examine the development of mature thymocytes in the absence of the major characterized source of negative selection signals (2). To this end, chimeric mice were produced in which MHC class II was expressed on the radioresistant thymic epithelium to support positive selection of CD4SP cells, but not on the negatively selecting radiosensitive hematopoietic elements (MHC II°→ MHC I° chimeras). A significant (1.7 ± 0.2-fold) increase in the steady-state percentage of mature CD4SP thymocytes was observed in these chimeras as compared with control (MHC II+→ MHC I°) chimeras (Fig. 2). As expected, lack of MHC class I on hematopoietic elements (MHC I°→ MHC I° chimeras) did not result in significantly increased CD4SP percentages (1.1 ± 0.1-fold) as compared with appropriate control (MHC I+→ MHC I°) chimeras (Fig. 2). Because thymi from the chimeras had similar total cell numbers (data not shown), these results reflect increases in the absolute number of CD4SP cells. Thus, in the absence of MHC class II expression on hematopoietic elements, a 1.7-fold increase in mature CD4SP cells occurs, suggesting that approximately half of the positively selectable thymocytes with receptors specific for selfMHC class II undergo negative selection on the same MHC molecule.
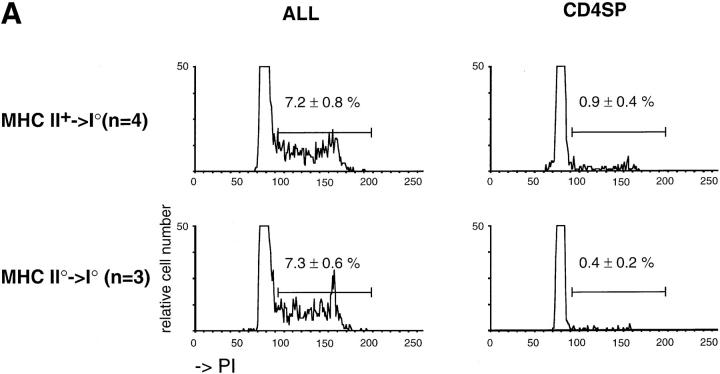
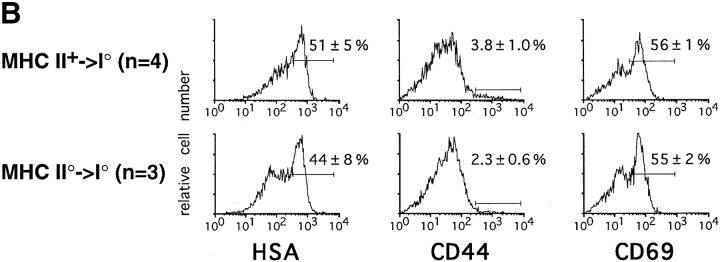
Several explanations other than the lack of negative selection could account for the increased number of CD4SP cells in MHC II°→ MHC I° chimeras. However, proliferation of mature CD4SP does not account for the increase as cell cycle analysis reveals no augmentation in the number of CD4SP cells in S+G2/M phase (Fig. 3 A). A change in their maturation/export rate could result in an increased retention of CD4SP cells in the thymus. CD69 is a molecule transiently expressed during thymocyte development: in vivo, it is first expressed on CD4+CD8+ cells that have undergone MHC-mediated activation and is downmodulated only when the thymocytes have already reached the SP stage (39–41, 29). The normal ratio of mature thymocytes from the chimeras expressing high versus low levels of CD69 therefore is an indication of normal thymic maturation (Fig. 3 B). Expression of HSA on CD4SP thymocytes is also downmodulated during their final maturation (42, 43). Again, the normal ratio of HSAhigh versus HSAlow CD4SP cells in the chimeras indicates normal maturation. Taken together, the data on the expression of CD69 and HSA suggest normal thymocyte development and render the possibility of prolonged retention of CD4SP cells in the thymus unlikely. Another possibility would be the recirculation into the thymus of mature peripheral T cells (44–46). Peripheral T lymphocytes do not express significant levels of HSA (42, 43) and the lack of an increased percentage of HSA− CD4SP thymocytes (Fig. 3 B) thus is inconsistent with a recirculation model. Reentry into the adult thymus of peripheral T cells is known to be restricted to activated cells (44–46). These cells may be expected to express high levels of the memory/activation marker CD44 (47). No evidence for an increase in CD44high CD4SP thymocytes was found in the chimeras (Fig. 3 B). Collectively, these data strongly suggest that the increased number of CD4SP cells in chimeras lacking MHC class II on hematopoietic elements is not due to proliferation, to increased retention of thymocytes in the thymus, or to recirculation of peripheral T lymphocytes.
Figure 3.
Increase in CD4SP thymocytes in MHC II°→ MHC I° chimeras is not due to (A) proliferation or (B) recirculation of peripheral T lymphocytes. (A) Cell cycle analysis (PI incorporation) was performed on ethanol-fixed total thymocytes and electronically sorted CD4+CD8− TCRhigh cells (purity ⩾95%). Representative results are shown. The statistics represent mean percentage cells in S+G2/M phase ± SD from the indicated number of experiments. (B) Four-color flow cytometry was performed using anti-CD4, anti-CD8, and anti-TCR antibodies combined with anti-CD44, anti-HSA, or anti-CD69. The CD44, HSA, and CD69 histograms are of electronically gated CD4+CD8−TCRhigh cells. Representative results are shown. The statistics represent mean percentage ± SD from the indicated number of experiments.
Analysis of cell number in the steady-state thymus measures the accumulation rather than the rate of de novo generation of thymocytes. Because the latter parameter more directly addresses the issue of whether additional cells are surviving the selection/differentiation process in the absence of hematopoietic MHC-mediated negative selection, we analyzed the kinetics of development of mature thymocytes in MHC-deficient chimeric mice. Most thymocytes are highly radiosensitive and die upon sublethal irradiation, whereas a small radioresistant CD4−CD8− precursor population will repopulate the thymus upon such treatment. In this model system, CD4+CD8+ immature thymocytes appear around day 6 after irradiation and 3–4 d later mature SP cells can be observed (41, 48–52). Using this post-irradiation repopulation model, we studied the kinetics of generation of mature thymocytes in bone marrow chimeras (Fig. 4). In particular, 6 wk after grafting, MHC I°II°→ wt, MHC I°→ wt, and control wt→ wt chimeras were sublethally irradiated (720 rads) and their thymi analyzed 9–13 d later. A significant, approximately twofold greater, generation of CD4SP thymocytes was observed in the absence of MHC class II expression on bone marrow–derived cells, whereas in the absence of MHC class I, CD4SP cells developed at the same rate as in control chimeras (Fig. 4). CD8SP thymocytes were also generated more efficiently in the absence of their negatively selecting ligand (MHC class I) on hematopoietic elements (Fig. 4). Thus, in MHC I°→ wt and MHC I°II°→ wt chimeras a two- to threefold increase in generation of CD8SP thymocytes was observed. During the reconstitution no differences in the number of total thymocytes were seen between the different types of chimeras (data not shown), again indicating that absolute increases in SP cells were occurring in these circumstances. These data confirm that the increase in the number of CD4SP cells seen in the steady-state thymus of mice lacking MHC class II on hematopoietic cells is due to the lack of negative selection rather than to alterations in proliferation, homeostasis, or recirculation of these cells. Moreover, they reveal a similarly large impact of negative selection on the development of CD8SP thymocytes.
Collectively, our results indicate that a remarkably large fraction (half to two-thirds) of thymocytes recognizing ligands able to mediate their positive selection do not reach maturity due to overriding negative selection in the presence of physiological ligands expressed on hematopoietic cells. These data, combined with those on the kinetics of thymocyte development (53, 54), imply that ∼90% of developing thymocytes die of neglect and 5% die due to deletion, whereas the remaining 5% survive to populate the periphery. In considering this calculation, one caveat is that the proportion of negatively selected thymocytes could theoretically be larger if some cells are normally deleted despite being unable to be positively selected. However, we observe no increase in the absolute number of CD4+CD8+ thymocytes in deletion-deficient chimeras (data not shown), which is inconsistent with the existence of any appreciable number of such cells. Therefore, when considering the entire thymocyte precursor pool, effective signaling for positive selection places a much greater constraint on the repertoire than negative selection. This conclusion is also consistent with a study by Surh and Sprent (55), which showed that the extent of intrathymic death caused by negative selection is less than that due to neglect, although no quantitative estimate of the extent of deletion could be inferred from these data. However, if one considers only those thymocytes whose interaction with self-peptide–MHC ligands can initiate the positive selection process necessary for contribution to the functional repertoire, the data presented here clearly show that many of these cells never complete maturation, but are eliminated by recognition of the same class of MHC as that responsible for initiating their differentiation.
Two very recent studies bear on the issue of the frequency of positively selected thymocytes that subsequently undergo negative selection. Using transgenic mice expressing a single peptide–MHC class II complex, Ignatowicz et al. (22) found that 65% of T cell hybridomas established from positively selected CD4+ cells reacted with wild-type MHC class II molecules presented by APCs. These data were interpreted to mean that 65% of positively selected thymocytes in these transgenic mice would normally have undergone negative selection. However, in another transgenic model in which MHC class II was expressed only on thymic cortical epithelium, Laufer et al. (25) estimated the frequency of positively selected CD4+ cells reactive with MHC class II on APCs to be only 5% by limiting dilution analysis. The apparent discrepancy in the frequency estimates of thymocytes that are potentially subject to negative selection in these two studies could result from differences in the transgenic models and/or assay systems used. Whatever the explanation, it should be emphasized that neither study directly addresses the extent of thymic clonal deletion, because the fate of the MHC-reactive cells in these transgenic systems in vivo could have been either deletion or induction of anergy.
Based on the requirement for epithelial MHC recognition in positive selection, the negative selection events mediated by hematopoietic MHC molecules here appear to occur after initiation of this process. This raises the question of what is different about recognition by partially mature T cells of MHC ligands on bone marrow–derived cells as compared with the recognition of possibly the identical peptide–MHC complex on epithelial cells by immature precursors, such that the former leads to cell death and the latter to promotion of differentiation. Two of the most obvious possibilities are the increased surface expression of TCR by partially mature cells (56, 57, 41), which could change the quantity or even quality of signals received by the cell, and the expression of costimulatory ligands such as CD80/ CD86 on the hematopoietic cells. In some models, the latter has been shown to contribute to thymocyte death when combined with TCR signals (58, 59). Whatever the explanation, these data focus attention on the issue of whether peptides unique to epithelial cells make a predominant contribution to repertoire development. Whereas no epitheliumspecific peptides could be eluted from class II MHC molecules (60), the existence of such tissue-specific ligands has been demonstrated by transplant experiments (10).
Finally, central (thymic) and peripheral tolerization by means other than deletion have been described (61, 62). In this respect, it will be of considerable interest to determine whether mature T cells from our chimeras that have escaped negative selection will respond when confronted with professional APCs expressing the MHC ligands encountered during positive selection.
Acknowledgments
We thank E. O'Connell, C. Eigsty, A.-L. Peitrequin, and P. Zaech for expert technical help and Drs. H. Bluethmann, L. Glimcher, and B. Koller for providing MHC mutant mice.
Footnotes
1 Abbreviations used in this paper: CD4SP, CD4+CD8−TCRhigh; CD8SP, CD4−CD8+TCRhigh; HSA, heat stable antigen; MHC I°/II°, MHC class I/II deficient; MMTV, mouse mammary tumor virus; wt, wild-type.
References
- 1.Swain SL. T cell subsets and the recognition of MHC class. Immunol Rev. 1983;74:129–142. doi: 10.1111/j.1600-065x.1983.tb01087.x. [DOI] [PubMed] [Google Scholar]
- 2.Anderson G, Moore NC, Owen JJT, Jenkinson EJ. Cellular interactions in thymocyte development. Annu Rev Immunol. 1996;14:73–99. doi: 10.1146/annurev.immunol.14.1.73. [DOI] [PubMed] [Google Scholar]
- 3.Jameson SC, Hogquist KA, Bevan MJ. Positive selection of thymocytes. Annu Rev Immunol. 1995;13:93–126. doi: 10.1146/annurev.iy.13.040195.000521. [DOI] [PubMed] [Google Scholar]
- 4.Bendelac A, Killeen N, Littman DR, Schwartz RH. A subset of CD4+thymocytes selected by MHC class I molecules. Science (Wash DC) 1994;263:1774–1778. doi: 10.1126/science.7907820. [DOI] [PubMed] [Google Scholar]
- 5.Bix M, Coles M, Raulet D. Positive selection of Vβ8+ CD4−8−thymocytes by class I molecules expressed by hematopoietic cells. J Exp Med. 1993;178:901–908. doi: 10.1084/jem.178.3.901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bix M, Raulet D. Inefficient positive selection of T cells directed by haematopoietic cells. Nature (Lond) 1992;359:330–333. doi: 10.1038/359330a0. [DOI] [PubMed] [Google Scholar]
- 7.Markowitz JS, Auchincloss HJ, Grusby MJ, Glimcher LH. Class II–positive hematopoietic cells cannot mediate positive selection of CD4+T lymphocytes in class II–deficient mice. Proc Natl Acad Sci USA. 1993;90:2779–2783. doi: 10.1073/pnas.90.7.2779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nossal GJ. Negative selection of lymphocytes. Cell. 1994;76:229–239. doi: 10.1016/0092-8674(94)90331-x. [DOI] [PubMed] [Google Scholar]
- 9.Schwartz RH. Acquisition of immunologic self-tolerance. Cell. 1989;57:1073–1081. doi: 10.1016/0092-8674(89)90044-5. [DOI] [PubMed] [Google Scholar]
- 10.Bonomo A, Matzinger P. Thymus epithelium induces tissue-specific tolerance. J Exp Med. 1993;177:1153–1164. doi: 10.1084/jem.177.4.1153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Burkly LC, Degermann S, Longley J, Hagman J, Brinster RL, Lo D, Flavell RA. Clonal deletion of V beta 5+T cells by transgenic I-E restricted to thymic medullary epithelium. J Immunol. 1993;151:3954–3960. [PubMed] [Google Scholar]
- 12.Carlow DA, Teh SJ, Teh HS. Altered thymocyte development resulting from expressing a deleting ligand on selecting thymic epithelium. J Immunol. 1992;148:2988–2995. [PubMed] [Google Scholar]
- 13.Degermann S, Surh CD, Glimcher LH, Sprent J, Lo D. B7 expression on thymic medullary epithelium correlates with epithelium-mediated deletion of V beta 5+thymocytes. J Immunol. 1994;152:3254–3263. [PubMed] [Google Scholar]
- 14.Gao EK, Lo D, Sprent J. Strong T cell tolerance in parent→ F1 bone marrow chimeras prepared with supralethal irradiation. Evidence for clonal deletion and anergy. J Exp Med. 1990;171:1101–1121. doi: 10.1084/jem.171.4.1101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pircher H, Brduscha K, Steinhoff U, Kasai M, Mizuochi T, Zinkernagel RM, Hengartner H, Kyewski B, Muller KP. Tolerance induction by clonal deletion of CD4+8+thymocytes in vitro does not require dedicated antigen-presenting cells. Eur J Immunol. 1993;23:669–674. doi: 10.1002/eji.1830230315. [DOI] [PubMed] [Google Scholar]
- 16.Robey E, Fowlkes BJ. Selective events in T cell development. Annu Rev Immunol. 1994;12:675–705. doi: 10.1146/annurev.iy.12.040194.003331. [DOI] [PubMed] [Google Scholar]
- 17.Speiser DE, Pircher H, Ohashi PS, Kyburz D, Hengartner H, Zinkernagel RM. Clonal deletion induced by either radioresistant thymic host cells or lymphohemopoietic donor cells at different stages of class I–restricted T cell ontogeny. J Exp Med. 1992;175:1277–1283. doi: 10.1084/jem.175.5.1277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.MacDonald HR, Glasebrook AL, Schneider R, Lees RK, Pircher H, Pedrazzini T, Kanagawa O, Nicolas JF, Howe RC, Zinkernagel RM, Hengartner H. T-cell reactivity and tolerance to Mls a-encoded antigens. Immunol Rev. 1989;107:89–108. doi: 10.1111/j.1600-065x.1989.tb00004.x. [DOI] [PubMed] [Google Scholar]
- 19.Simpson E, Dyson PJ, Knight AM, Robinson PJ, Elliott JI, Altmann DM. T-cell receptor repertoire selection by mouse mammary tumor viruses and MHC molecules. Immunol Rev. 1993;131:93–115. doi: 10.1111/j.1600-065x.1993.tb01532.x. [DOI] [PubMed] [Google Scholar]
- 20.von Boehmer H. Developmental biology of T cells in T cell-receptor transgenic mice. Annu Rev Immunol. 1990;8:531–556. doi: 10.1146/annurev.iy.08.040190.002531. [DOI] [PubMed] [Google Scholar]
- 21.Fung-Leung W-P, Surh CD, Liljedahl M, Pang J, Leturcq D, Peterson PA, Webb SR, Karlsson L. Antigen presentation and T cell development in H2-M-deficient mice. Science (Wash DC) 1996;271:1278–1281. doi: 10.1126/science.271.5253.1278. [DOI] [PubMed] [Google Scholar]
- 22.Ignatowicz L, Kappler J, Marrack P. The repertoire of T cells shaped by a single MHC/peptide ligand. Cell. 1996;84:521–529. doi: 10.1016/s0092-8674(00)81028-4. [DOI] [PubMed] [Google Scholar]
- 23.Martin WD, Hicks GG, Mendiratta SK, Leva HI, Ruley HE, Van Kaer L. H2-M mutant mice are defective in the peptide loading of class II molecules, antigen presentation, and T cell repertoire selection. Cell. 1996;84:543–550. doi: 10.1016/s0092-8674(00)81030-2. [DOI] [PubMed] [Google Scholar]
- 24.Miyazaki T, Wolf P, Tourne S, Waltzinger C, Dierich A, Barois N, Ploegh H, Benoist C, Mathis D. Mice lacking H2-M complexes, enigmatic elements of the MHC class II peptide-loading pathway. Cell. 1996;84:531–541. doi: 10.1016/s0092-8674(00)81029-6. [DOI] [PubMed] [Google Scholar]
- 25.Laufer TM, DeKoning J, Markowitz JS, Lo D, Glimcher LH. Unopposed positive selection and autoreactivity in mice expressing class II MHC only on thymic cortex. Nature (Lond) 1996;383:81–85. doi: 10.1038/383081a0. [DOI] [PubMed] [Google Scholar]
- 26.Koller BH, Marrack P, Kappler JW, Smithies O. Normal development of mice deficient in β2M, MHC class I proteins, and CD8+T cells. Science (Wash DC) 1990;248:1227–1230. doi: 10.1126/science.2112266. [DOI] [PubMed] [Google Scholar]
- 27.Grusby MJ, Johnson RS, Papaioannou VE, Glimcher LH. Depletion of CD4+T cells in major histocompatibility complex class II–deficient mice. Science (Wash DC) 1991;253:1417–1420. doi: 10.1126/science.1910207. [DOI] [PubMed] [Google Scholar]
- 28.Koentgen F, Suess G, Stewart C, Steinmetz M, Bluethmann H. Targeted disruption of the MHC class II Aα gene in C57BL/6 mice. Int Immunol. 1993;5:957–964. doi: 10.1093/intimm/5.8.957. [DOI] [PubMed] [Google Scholar]
- 29.van Meerwijk JPM, O'Connell EM, Germain RN. Evidence for lineage commitment and initiation of positive selection by thymocytes with intermediate surface phenotypes. J Immunol. 1995;154:6314–6324. [PubMed] [Google Scholar]
- 30.Bruce J, Symington FW, McKearn TJ, Sprent J. A monoclonal antibody discriminating between subsets of T and B cells. J Immunol. 1981;127:2496–2501. [PubMed] [Google Scholar]
- 31.Mark C, Figueroa F, Nagy ZA, Klein J. Cytotoxic monoclonal antibody specific for the Lyt-1.2 antigen. Immunogenetics. 1982;16:95–97. doi: 10.1007/BF00364447. [DOI] [PubMed] [Google Scholar]
- 32.Dialynas DP, Loken MR, Glasebrook AL, Fitch FW. Lyt-2−/Lyt-3−variants of a cloned cytolytic T cell line lack an antigen receptor functional in cytolysis. J Exp Med. 1981;153:595–604. doi: 10.1084/jem.153.3.595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lesley J, Trowbridge IS. Genetic characterization of a polymorphic murine cell-surface glycoprotein. Immunogenetics. 1982;15:313–320. doi: 10.1007/BF00364339. [DOI] [PubMed] [Google Scholar]
- 34.Springer T, Galfre G, Secher DS, Milstein C. Monoclonal xenogeneic antibodies to murine cell surface antigens: identification of novel leukocyte differentiation antigens. Eur J Immunol. 1978;8:539–551. doi: 10.1002/eji.1830080802. [DOI] [PubMed] [Google Scholar]
- 35.Yokoyama WM, Koning F, Kehn PJ, Pereira GM, Stingl G, Coligan JE, Shevach EM. Characterization of a cell surface–expressed disulfide-linked dimer involved in murine T cell activation. J Immunol. 1988;141:369–376. [PubMed] [Google Scholar]
- 36.Dialynas DP, Quan ZS, Wall KA, Pierres A, Quintans J, Loken MR, Pierres M, Fitch FW. Characterization of the murine T cell surface molecule, designated L3T4, identified by monoclonal antibody GK1.5: similarity of L3T4 to the human Leu-3/T4 molecule. J Immunol. 1983;131:2445–2451. [PubMed] [Google Scholar]
- 37.Grusby MJ, Glimcher LH. Immune responses in MHC class II–deficient mice. Annu Rev Immunol. 1995;13:417–435. doi: 10.1146/annurev.iy.13.040195.002221. [DOI] [PubMed] [Google Scholar]
- 38.Raulet DH. MHC class I–deficient mice. Adv Immunol. 1994;55:381–421. doi: 10.1016/s0065-2776(08)60514-3. [DOI] [PubMed] [Google Scholar]
- 39.Bendelac A, Matzinger P, Seder RA, Paul WE, Schwartz RH. Activation events during thymic selection. J Exp Med. 1992;175:731–742. doi: 10.1084/jem.175.3.731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Swat W, Dessing M, von Boehmer H, Kisielow P. CD69 expression during selection and maturation of CD4+8+thymocytes. Eur J Immunol. 1993;23:739–746. doi: 10.1002/eji.1830230326. [DOI] [PubMed] [Google Scholar]
- 41.van Meerwijk JPM, Germain RN. Development of mature CD8+ thymocytes: selection rather than instruction? . Science (Wash DC) 1993;261:911–915. doi: 10.1126/science.8102208. [DOI] [PubMed] [Google Scholar]
- 42.Nikolic-Zugic J, Bevan MJ. Functional and phenotypic delineation of two subsets of CD4 single positive cells in the thymus. Int Immunol. 1990;2:135–141. doi: 10.1093/intimm/2.2.135. [DOI] [PubMed] [Google Scholar]
- 43.Ramsdell F, Jenkins M, Dinh Q, Fowlkes BJ. The majority of CD4+8−thymocytes are functionally immature. J Immunol. 1991;147:1779–1785. [PubMed] [Google Scholar]
- 44.Agus DB, Surh CD, Sprent J. Re-entry of T cells to the adult thymus is restricted to activated T cells. J Exp Med. 1991;173:1039–1046. doi: 10.1084/jem.173.5.1039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Fukushi N, Arase H, Wang B, Ogasawara K, Gotohda T, Good RA, Onoe K. Thymus: a direct target tissue in graft-versus-host reaction after allogeneic bone marrow transplantation that results in abrogation of induction of self-tolerance. Proc Natl Acad Sci USA. 1990;87:6301–6305. doi: 10.1073/pnas.87.16.6301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Surh CD, Sprent J, Webb SR. Exclusion of circulating T cells from the thymus does not apply in the neonatal period. J Exp Med. 1993;177:379–385. doi: 10.1084/jem.177.2.379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Budd RC, Cerottini JC, Horvath C, Bron C, Pedrazzini T, Howe RC, MacDonald HR. Distinction of virgin and memory T lymphocytes. Stable acquisition of the Pgp-1 glycoprotein concomitant with antigenic stimulation. J Immunol. 1987;138:3120–3129. [PubMed] [Google Scholar]
- 48.Ayukawa K, Tomooka S, Asano T, Taniguchi K, Yoshikai Y, Nomoto K. ‘Radioresistant' CD4−CD8− intrathymic T cell precursors differentiate into mature CD4+ CD8− and CD4−CD8+ T cells. Development of ‘radioresistant' CD4−CD8−intrathymic T cell precursors. Thymus. 1990;15:65–78. [PubMed] [Google Scholar]
- 49.Huiskamp R, van Ewijk W. Repopulation of the mouse thymus after sublethal fission neutron irradiation. I. Sequential appearance of thymocyte subpopulations. J Immunol. 1985;134:2161–2169. [PubMed] [Google Scholar]
- 50.Kadish JL, Basch RS. Thymic regeneration after lethal irradiation: evidence for an intrathymic radioresistant T cell precursor. J Immunol. 1975;114:452–458. [PubMed] [Google Scholar]
- 51.Tomooka S, Matsuzaki G, Kishihara K, Tanaka K, Yoshikai Y, Taniguchi K, Himeno K, Nomoto K. Sequential appearance of thymocyte subpopulations and T cell antigen receptor gene messages in the mouse thymus after sublethal irradiation. J Immunol. 1987;139:3986–3990. [PubMed] [Google Scholar]
- 52.Zúñiga-Pflücker JC, Kruisbeek AM. Intrathymic radioresistant stem cells follow an IL-2/IL-2R pathway during thymic regeneration after sublethal irradiation. J Immunol. 1990;144:3736–3740. [PubMed] [Google Scholar]
- 53.Egerton M, Scollay R, Shortman K. Kinetics of mature T-cell development in the thymus. Proc Natl Acad Sci USA. 1990;87:2579–2582. doi: 10.1073/pnas.87.7.2579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Huesmann M, Scott B, Kisielow P, von Boehmer H. Kinetics and efficacy of positive selection in the thymus of normal and T cell receptor transgenic mice. Cell. 1991;66:533–540. doi: 10.1016/0092-8674(81)90016-7. [DOI] [PubMed] [Google Scholar]
- 55.Surh CD, Sprent J. T-cell apoptosis detected in situ during positive and negative selection in the thymus. Nature (Lond) 1994;372:100–103. doi: 10.1038/372100a0. [DOI] [PubMed] [Google Scholar]
- 56.Chan SH, Cosgrove D, Waltzinger C, Benoist C, Mathis D. Another view of the selective model of thymocyte selection. Cell. 1993;73:225–236. doi: 10.1016/0092-8674(93)90225-f. [DOI] [PubMed] [Google Scholar]
- 57.Guidos CJ, Danska JS, Fathman CG, Weissman IL. T cell receptor–mediated negative selection of autoreactive T lymphocyte precursors occurs after commitment to the CD4 or CD8 lineages. J Exp Med. 1990;172:835–845. doi: 10.1084/jem.172.3.835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kishimoto H, Cai Z, Brunmark A, Jackson MR, Peterson PA, Sprent J. Differing roles for B7 and intercellular adhesion molecule-1 in negative selection of thymocytes. J Exp Med. 1996;184:531–537. doi: 10.1084/jem.184.2.531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Punt JA, Osborne BA, Takahama Y, Sharrow SO, Singer A. Negative selection of CD4+CD8+thymocytes by T cell receptor–induced apoptosis requires a costimulatory signal that can be provided by CD28. J Exp Med. 1994;179:709–713. doi: 10.1084/jem.179.2.709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Marrack P, Ignatowicz L, Kappler JW, Boymel J, Freed JH. Comparison of peptides bound to spleen and thymus class II. J Exp Med. 1993;178:2173–2183. doi: 10.1084/jem.178.6.2173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ramsdell F, Fowlkes BJ. Clonal deletion and clonal anergy: The role of the thymus in inducing self tolerance. Science (Wash DC) 1990;248:1342–1348. doi: 10.1126/science.1972593. [DOI] [PubMed] [Google Scholar]
- 62.Sprent J, Kosaka H, Gao E-K, Surh CD, Webb SR. Intrathymic and extrathymic tolerance in bone marrow chimeras. Immunol Rev. 1993;133:151–176. doi: 10.1111/j.1600-065x.1993.tb01515.x. [DOI] [PubMed] [Google Scholar]