Orthostatic hypotension: framework of the syndrome (original) (raw)
Abstract
According to the 1996 consensus definition, orthostatic hypotension (OH) is diagnosed when a fall in systolic blood pressure of at least 20 mm Hg and/or diastolic blood pressure of at least 10 mm Hg within 3 min of standing is recorded. The elements of orthostatic blood pressure drop that are relevant to the definition of OH include magnitude of the drop, time to reach the blood pressure difference defined as OH, and reproducibility of the orthostatic blood pressure drop. In each of these elements, there exist issues that argue for modification of the presently accepted criteria of OH. Additional questions need to be addressed. Should one standard orthostatic test be applied to different patient populations or should tests be tailored to the patients' clinical circumstances? Are different OH thresholds relevant to various clinical settings, aetiologies of OH and comorbidity? Which test has the best predictive power of morbidity and mortality?
Orthostatic hypotension (OH) has been formally defined by expert consensus as a fall in systolic blood pressure (SBP) of at least 20 mm Hg and/or diastolic blood pressure (DBP) of at least 10 mm Hg within 3 min of standing.1 When a normal individual stands, 10–15% of the blood is pooled in the legs, thereby secondarily reducing venous return, cardiac output and arterial pressure. This fall in blood pressure activates baroreceptors with a subsequent reflex increase in sympathetic outflow and parasympathetic inhibition, leading in turn to peripheral vasoconstriction and increased heart rate and contractility. There may be a slight fall in SBP, a slight rise in DBP and a mild increase in heart rate accompanying this chain of events.2 Orthostatic hypotension is an excessive fall in blood pressure occurring early on postural challenge when orthostatic stress overwhelms autonomic defences.3 Numerous factors may influence blood pressure homeostasis and impact on the occurrence of OH: autonomic nervous system function, intravascular volume, duration of erect posture, time of day, postprandial state and ambient temperature.4,5
Dizziness and syncope are the classical symptoms of postural stress and their connection to OH is readily established. The relationship of other symptoms to OH may not be obvious, unless one is aware of the wider spectrum of orthostatic disturbances. Thus, weakness, fatigue, visual blurring, vertigo, suboccipital and paracervical pain, chest pain on upright posture, headaches, palpitations, low back pain or dyspnoea may occur on standing and disappear when lying flat.6,7,8,9
The diagnostic consensus criteria defining OH1 are necessarily arbitrary. There are questions open as to the magnitude of hypotension and rapidity of its development in the definition of OH. Patients may feel dizzy, weak or even faint upon standing while orthostatic blood pressure decrement is insufficient to meet the criteria for OH.10,11,12,13 And yet, if a patient has posturally induced symptoms and a decrease in BP but does not fit the strict definition for OH, it has been suggested that one may still consider OH as a possible diagnosis.14 Therefore, in limiting one's self to the consensus criteria for the definition of OH1 one may lose useful clinical information.
Importance of diagnosing orthostatic hypotension
The burden of OH on public health is substantial, with a prevalence of 7% in the elderly, even when excluding patients with known risk factors to this condition.15 It increases to 13% and 55% in high risk groups.16,17,18,19,20 The prevalence of OH among patients presenting with syncope in the emergency room was 24% in one study20 and 64% among elderly patients hospitalised for acute conditions.21
In the clinical setting, the diagnosis of OH has a threefold significance: OH may underlie symptoms of cerebral hypoperfusion as well as the above enumerated systemic symptoms; OH may be a risk factor for falls; it may be a marker of frailness and predictor of mortality.
Epidemiological studies have shown that individuals with OH have a propensity for falls.22 A prospective study of 844 elderly long‐term nursing home residents were evaluated during a mean of 1.2 years.22 Among those with a fall in the previous 6 months, those with OH had an increased risk for recurrence (adjusted relative risk (RR) 2.1). Those who had OH demonstrated on two or more measurements had the greatest risk (RR 2.6). The association between OH and recurrent falls was independent of other measured demographic or clinical risk factors for falls. In disagreement with the latter are results of a meta‐analysis, showing that OH was not an independent risk factor of falls in elderly community‐dwelling persons.23 OH is predictive of ischaemic stroke. In 11 707 persons from the Atherosclerosis Risk in Communities cohort who were free of stroke and overt heart disease at baseline, the association between OH and incident ischaemic stroke over 7.9 years of follow‐up was assessed. OH was independently predictive of ischaemic stroke, even after adjustment for numerous other stroke risk factors (hazard ratio 2.0).24 Also, OH was found to be a clinical correlate of pathological white matter findings on cranial magnetic resonance imaging in elderly people (p<0.01).25
Search strategy and selection criteria
We searched PubMed using the key words “orthostatic hypotension” and “postural hypotension” with the relevant topics—“epidemiology”, “diagnosis”, “tilt test”, “symptoms”, “syncope”, “falls”, “morbidity” and “mortality”. Fields were restricted to publications in English. We also searched the citations from obtained papers. References were chosen based on the best evidence from clinical or laboratory studies. Review articles of orthostatic hypotension published in the past 10 years were also examined to ensure minimum overlap with this review article. Recent articles that provided comprehensive overviews were included where appropriate instead of multiple references of original work.
OH is an independent predictor of all‐cause mortality.14 In a prospective study of a cohort of 3522 elderly Japanese American men, OH, as measured in the supine position and after 3 min of standing, was assessed in relation to subsequent 4 year all‐cause mortality. The overall prevalence of OH was 6.9% and it increased with age. Four year age‐adjusted mortality rates in those with and without OH were 56.6 and 38.6 per 1000 person‐years, respectively. With the use of Cox proportional hazards models, after adjustment for age, smoking, diabetes mellitus, body mass index, physical activity, seated SBP, antihypertensive medications, haematocrit, alcohol intake, and prevalent stroke, coronary heart disease and cancer, OH was a significant independent predictor of 4 year all‐cause mortality (RR 1.64). There was a significant linear correlation between change in SBP from supine position to standing and 4 year mortality rates (p = 0.001), suggesting a “dose–response” relationship.
Another study evaluated the risks of non‐vascular and vascular deaths, according to different definitions of OH, among 792 home‐dwelling persons aged 70 years or older.16 The hazard ratio for vascular death associated with diastolic OH 3 min after standing up, adjusted for other significant factors associated with vascular death, was 2.04. The corresponding hazard ratio for systolic OH was 1.69. In another work the risk for vascular death associated with OH was especially high among diabetic patients26; the hazard ratio of vascular death associated with diastolic OH was 3.69 and 2.7 with systolic OH.
Methodology
The diagnosis of OH depends on blood pressure measurement technique, positioning of the patient and timing of measurements.27
Blood pressure measurement techniques
The mercury column sphygmomanometer is preferred by us and by others14,28 for routine clinical testing because of its reliability and simplicity. This is the standard method to which other non‐invasive devices of blood pressure measurement are validated.29 Automatic arm‐cuff devices, as they are programmed to repeat and confirm measurements when discrepant values are recorded, may be at a disadvantage in following the rapidly dropping blood pressure during OH. Auscultatory measurements of blood pressure should be done by a physician skilled in the technique recommended by the American Heart Association.30 To avoid an erroneous measurement, the cuffed arm should be positioned so that the brachial artery is held at the level of the heart.31 Potential confounding factors in detection of OH include: inadequate cuff inflation in those with an auscultatory gap; rapid cuff deflation in those with a slow or irregular pulse rate leading to underestimation of the SBP32; and repeated measurements at intervals more frequently than 15 s causing venous stasis of the arm.31,32
Beat‐to‐beat non‐invasive blood pressure measurement with the Finapres monitor is widely used in research and tilt laboratories.33,34 The Finapres blood pressure monitor uses the method of Penaz to record the arterial waveform indirectly. Studies on its accuracy have suggested little systematic bias versus intra‐arterial pressure but substantial variability. Inconsistency between studies, as relating to magnitude, direction and variance of bias, has been described in validation studies versus direct intra‐arterial blood pressure. However, in combined data from 20 published studies,34 the average (SD) Finapres systolic bias was 2.2 (12.4) mm Hg and the Finapres diastolic bias was −0.3 (7.9) mm Hg. Another beat‐to‐beat non‐invasive blood pressure measurement device has been developed to monitor radial artery pressure and its waveform based on arterial tonometry. Arterial tonometry provides near continuous and non‐invasive arterial blood pressure monitoring and may be an alternative to direct intra‐arterial measurement. It has been evaluated in adult and paediatric patients. Excellent agreement between arterial tonometric and intra‐arterial blood pressure was documented.35,36
Heart rate monitoring
Heart rate recording is integral to testing for OH and is indispensable to the differentiation between certain clinical syndromes. At the bedside, the heart rate is acquired intermittently together with blood pressure measurement when using standard automatic blood pressure measurement devices. The method routinely used by us, along with intermitted blood pressure measurements by mercury column sphygmomanometry, is continuous electrocardiographic heart rate monitoring. The option generally favoured is by beat‐to‐beat tracking of blood pressure and heart rate via Finapres. In a normal subject, the heart rate will increase by 5–12 beats/min when arising from recumbence.8 Failure of the heart rate to rise concurrent with a fall in blood pressure upon arising is indicative of sympathetic autonomic insufficiency37—that is, neurogenic OH is typically associated with a blunted heart rate response on standing or passive tilt. There are exceptions to this rule: healthy older individuals may display a similarly blunted heart rate response due to downregulation of baroreceptors related to aging38; when the heart rate may be slowed by medication; or there may be a paradoxical increase in heart rate in patients with autonomic failure, presumably due to parasympathetic withdrawal.39 On the other hand, an exaggerated increase in heart rate in the erect position may be indicative of a contracted intravascular volume.40
Orthostatic stress tests
The ideal orthostatic test should be suitable for assessment of a variety of clinical conditions, should correspond to real life situations, be simple to perform, its instruments should be generally available, and should require minimal patient cooperation. Of the tests in common use, usually in assessment of dizziness and syncope, the lying‐to‐standing orthostatic test appears the closest fit, while the head‐up tilt test (HUTT) is farthest from representation of the real‐life situation. Few studies have compared results of different orthostatic tests directly.41 It has been suggested that the orthostatic fall in SBP may be greater on HUTT than on standing,42 but data on this issue are scarce. Many more studies of this nature are required for any definitive conclusions.
Three orthostatic challenges are widely applied in practice: the lying‐to‐standing test, lying‐to‐sitting test, and the head‐up tilt tests. Lower body negative pressure tests are mainly used in research settings.43 The sitting‐to‐standing test has inferior sensitivity in detecting OH as compared to the other orthostatic tests, and as many as two thirds of the cases may go undetected.44
The lying‐to‐standing orthostatic test
A frequently utilised protocol is the short, bedside orthostatic test: the patient's blood pressure is measured after 5–10 min of rest in the supine position; the patient arises and the measurements are then repeated while he stands motionless for 3–5 min with the cuffed arm supported at heart level. On standing, the patient is asked to report dizziness, faintness or light‐headedness, with the examiner recording its transience/persistence. The procedure is aborted for safety reasons if blood pressure drops precipitously or presyncope ensues. Patients with severe autonomic failure have an immediate drop in blood pressure on standing and OH is easily diagnosed with this simple method.4,27,45 However, there are individuals in whom onset of hypotension on standing may be delayed and these cases may be missed by the short bedside orthostatic test.43,46
The lying‐to‐sitting orthostatic test
The methodology of the lying‐to‐sitting orthostatic test is not standardised.47,48,49,50,51 One frequently used protocol involves a single blood pressure measurement after prolonged recumbence followed by blood pressure measurements after 1, 3 and 5 min of sitting.49 The others differ in the number and timing of blood pressure measurements. Other technical details are similar to those of the above described supine‐to‐standing test.
The head‐up tilt test
A more accurate evaluation of the haemodynamic response to postural challenge may be obtained with HUTT. This method utilises a controlled passive postural stress to challenge the cardiovascular response as measured in blood pressure and heart rate changes. HUTT comprises two phases: (1) supine pre‐tilt phase; and (2) the passive head‐up tilt. Various protocols are used in performing this test. According to recommendations of the European Society of Cardiology, the supine pre‐tilt phase should last at least 5 min, when no venous cannulation is performed, and at least 20 min when venous blood sampling is part of the study; the tilt angle recommended is 60°–70°; the duration of passive tilt should be a minimum of 20 min and maximum of 45 min.45,51 Repeated measurements are taken at 30 s intervals when self‐reported dizziness or faintness occur; the test is discontinued in the event of loss of consciousness. The blood pressure can be measured conveniently with a mercury column sphygmomanometer at pre‐established intervals and the heart rate recorded on an electrocardiographic monitor. Continuous blood pressure and heart rate monitoring with finger plethysmography is preferable to discontinuous measurement.52
Clear guidelines for the supine resting time necessary to achieve stable blood pressure levels are scant. A span of 5 min of supine rest ensured reliable and reproducible baseline blood pressure values by Finapres in healthy elderly subjects in one study; however, at least 12 min of rest were necessary to obtain full haemodynamic stability in elderly patients with diminished cardiac compliance.53 In other studies, the recommended time of supine rest before measuring supine blood pressure and starting a postural challenge varied from 5 min,26 5–10 min,45 15 min or more,14,53 or at “first morning standing up”.54
There is uncertainty as to the minimum duration of postural stress needed to detect OH. In a recent study, 88% of patients developed OH by 1 min of tilt, with an additional 11% developing OH by 2 min and the remaining 1% developing OH by 3 min.55 Another study (Naschitz et al, personal communication, 2007) extracted data from 400 charts of consecutive patients evaluated for syncope or non‐specific dizziness by HUTT. “Classical” OH was defined as reduction of SBP of ⩾20 mm Hg and/or diastolic blood pressure of ⩾10 mm Hg within 3 min of HUTT. A similar decrease in SBP occurring during the 4th or 5th min of HUTT, not associated with a decrease in heart rate by >10%, was referred to as “late” OH. In this study, 17.2% of patients developed OH by 1 min of tilt, another 9.5% by 2 min, and 4.7% more by 3 min. “Late” OH was diagnosed in an additional 7.2% of patients. Patients with “classical” and “late” OH had comparable clinical characteristics: systolic OH, diastolic OH and mixed systolic–diastolic OH occurred with similar frequency in “classical” and “late” OH; the “classical” and “late” OH were associated with identical heart rate changes on tilt, differing from vasovagal reactions; on continuation of tilt, after OH, blood pressure behaviour was similar in both groups. Thus, by all parameters examined, OH in the first 3 min and that occurring at the 4th and 5th min were comparable, different from the earlier described “delayed orthostatic intolerance”.46 Results of this study indicate that extending postural stress to 5 min may reveal a significant number of additional cases of OH.
Streeten et al first drew attention to “delayed” OH, that occurred 13–30 min of standing.46 In a recent study,56 “delayed” OH occurred as frequently as classical OH: out of 108 having OH, 46% developed in the first 3 min of tilt, 3% between 3–5 min, 12% between 5–10 min, and 39% after 10 min of tilt.
Patterns of OH, describing the time course of the SBP during the initial 5 min of tilt, have been recently described55; stable OH; transient systolic OH with either early or late partial recovery of blood pressure; and progressive systolic OH with continuous reduction in blood pressure. Patients with progressive OH had significantly higher score on the adrenergic subscale of the Composite Autonomic Symptom Score and are assumed to have more severe adrenergic impairment. The progressive systolic OH pattern predicts increased risk of developing syncope on continuing postural challenge.53 A recent study confirmed the correlation of progressive systolic OH with early tilt termination due to syncope.57 Five minutes of orthostatic challenge also permit assessment of OH patterns, thereby providing additional information beyond the classical 3 min test.
Validity of orthostatic hypotension testing
Two important aspects relating to the validity of OH testing are accuracy and reproducibility of the measurements. Accuracy refers to the agreement between a measured value and its “true” value (or values that are as close to the true values as possible—that is, the gold standard). Reproducibility of the measurements is calculated by comparing several measurements taken in the same subject. Ideally, measurements utilised in OH testing should be both accurate and reproducible.
Reproducibility of cardiovascular responses on orthostatic challenge has been inconsistent. While some studies have observed gross reproducibility of OH,43,58 others, on detailed examination, have shown uneven results on repeated challenges.59,60,61,62,63,64,65,66,67 In one study utilising HUTT, asymptomatic orthostatic falls in SBP were reproducible 1 week after initial testing.47 In another study in healthy volunteers, medium‐term (1 week) and long‐term (1 year) baroreflex responses proved to be reliable (r = 0.54–0.87).58
Variability of postural responses is well documented, with diurnal, day‐to‐day and seasonal patterns (see box 1). To evaluate the stability of OH during the day, orthostatic tests were performed three times during the day on 502 acute geriatric ward inpatients (mean age 81.6 years). Sixty‐eight per cent of patients manifested OH on one of the measurements, but only 35% on two or all three of the measurements. OH was most prevalent and severe in the morning, when subjects first arose.65 Several studies have shown that OH is underestimated when orthostatic testing is performed in the afternoon.65,67 In addition, the influence of meals on diurnal variation of OH has been observed.68 Postprandial hypotension, almost immediately apparent after a meal, can be found after any meal during the day. Blood pressure usually reaches a nadir within 30–60 min postprandially. The nutrient composition of meals seems to affect the magnitude of the decrease in postprandial blood pressure.69,70 Carbohydrates and, more specifically, glucose have been found to play a significant role.70 In addition, sitting during the postprandial period was associated with a more severe decline in blood pressure.67,68
Box 1 Variability of orthostatic hypotension
- Diurnal variability
- -
At first arising—more frequent - -
Postprandial enhancement
- -
- Day‐to‐day variability
- Seasonal variability
Observations have suggested the existence of day‐to‐day variability in blood pressure reactivity to postural stress.59,60,61,62,63,64,65 In one representative study performed in a morning outpatient clinic, 40 elderly persons presenting with postural symptoms of dizziness, falls or syncope were recruited. All patients had a symptomatic drop in orthostatic SBP of >20 mm Hg documented in the clinic. Blood pressure and heart rate measurements were then repeated on standing, as well as with head‐up tilt, on two further morning clinic visits. A total of 67.5% patients had a drop in SBP of >20 mm Hg on both subsequent visits; in the remainder, the initial response was not reproduced. In those of the study with abnormal autonomic function tests, OH was reproducible in 79%, while those with normal autonomic function tests had OH reproduced in 57%.61 Seasonal variations in OH have also been noted. OH was more prevalent in summer than in winter in one study of elderly patients (38% vs 27%; p = 0.02). After adjusting for confounders, the risk of experiencing OH in summer was 64% higher than in winter.66
All findings of OH “variability” may be considered only if the measurement methodology used is accurate and precise. Indeed, some problems in studies on reproducibility of OH may be due to poor technique and lack of adherence to guidelines in daily practice.71 To diagnose OH, many physicians rely on blood pressure measurements performed by nurses. One study evaluated nurses' skills of supine and standing blood pressure determination with important deviations in technique from published guidelines found: time between supine and standing blood pressure measurement varied from 1–30 min; in 28% the arm position was not at heart level during standing blood pressure measurements; in 46% the cuff was placed incorrectly.71 Large differences in measurement technique and timing of standing blood pressure may influence the detection of OH and thus confound the reported prevalence of OH.71
The accuracy of postural tests has not been studied well. There is no widely accepted gold standard measurement to which various postural tests can be compared.72,73 A central issue relates to the routine use of brachial blood pressure measurements. It has been appreciated that there may be significant differences between central and peripheral blood pressure. It would appear that orthostatic symptoms are better reflected by central blood pressure as measured non‐invasively in the carotids. When carotid and brachial blood pressure were measured simultaneously using cuff‐oscillometric and tonometric methods the orthostatic decline in blood pressure was more prominent in the carotid artery. Thus, in one study, while nine subjects were diagnosed with OH via the brachial blood pressure, 21 subjects were diagnosed by carotid blood pressure (p<0.001), results indicating that evaluation of OH by brachial blood pressure may underestimate OH.74
Symptomatic versus asymptomatic orthostatic hypotension
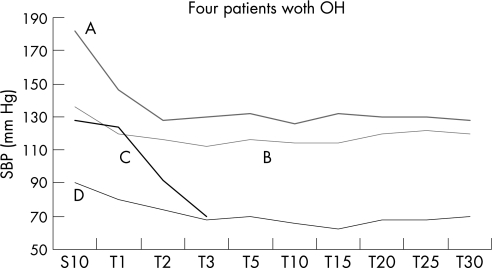
The occurrence of orthostatic symptoms, largely representative of inadequate central nervous system perfusion with a fall in blood pressure, depends not only on the magnitude of the blood pressure decline upon assuming upright posture (fig 1), but also on a number of other factors. Cerebrovascular autoregulation acts as a safeguard to protect the brain against excessive oscillations of blood pressure. In the average individual under normal physiologic conditions, changes in mean arterial blood pressure between 60 and 160 mm Hg produce little or no change in cerebral blood flow.75 Thus, cerebral arterioles dilate as mean arterial blood pressure decreases and constrict as mean arterial blood pressure increases. Beyond these limits of autoregulation, cerebral blood flow is directly proportional to mean arterial blood pressure and is “pressure‐passive”. A sudden decrease in cerebral blood flow occurs at the lower limit of autoregulation.
Figure 1 Inconsistent correlation between onset of dizziness and onset of orthostatic hypotension (OH) on head‐up tilt test, as illustrated in four cases. In patients A and B, OH was asymptomatic throughout the test. In case C, dizziness was reported simultaneously with a blood pressure drop diagnostic of OH. In case D, the patient was dizzy before tilt and subsequent OH had no additional effect on the patient's symptoms. SBP, systolic blood pressure.
The limits of cerebral autoregulation, and hence susceptibility to orthostatic symptoms, can be affected by a number of conditions. For example, in chronically hypertensive adults, the autoregulatory curve is shifted to the right. Therefore, while in otherwise normal individuals orthostatic symptoms may appear with a drop in the mean blood pressure below 60 mm Hg, in hypertensives a less drastic drop in blood pressure will be accompanied by symptoms. In more acute conditions (for example, ischaemic stroke, subarachnoid haemorrhage, intracerebral haemorrhage and post‐ictally), cerebral blood flow may become temporarily pressure passive, thus augmenting effects of OH on cerebral blood flow.76 In addition, hypercapnia (Paco2 >60 mm Hg)77 as well as hypocapnia (Paco2 <25 mm Hg) may consistently impair cerebral autoregulation78,79 and distort the correlation between symptoms and OH.
Not only do orthostatic symptoms not necessarily correlate with absolute blood pressure levels, but also the correlation with the magnitude of the blood pressure drop on orthostasis is not constant. It has been proposed that symptoms induced during a decrease in blood pressure, not fully meeting the strict definition for OH, should still be considered expressions of possible OH.14,80,81 Recently, the Joint National Committee on prevention, detection, evaluation and treatment of high blood pressure (the JNC 7 report) stated that a 10 mm Hg SBP drop should be regarded as clinically relevant when it is associated with symptoms.81
Orthostatic symptoms may correlate with the nadir blood pressure on orthostasis, with the magnitude of blood pressure drop, and also with the rate of blood pressure change. Thus, in a study of 400 patients who had HUTT for evaluation of non‐specific dizziness, the feeling of dizziness on tilt occurred uniformly only in patients in whom OH criteria were met within 3 min, while only 25% of patients having a more gradual decrease in blood pressure complained of dizziness.82
Symptoms occurring with the onset of OH are routinely diagnosed as “orthostatic”. It should be noted, however, that similar symptoms may be induced by postural change, but without a drop in blood pressure, and be caused by a panic attack, occult hyperventilation, cerebrovascular disease or postural tachycardia syndrome.78,79,83
The relationship between symptoms occurring during an orthostatic test, essentially representative of a laboratory phenomenon, and symptoms occurring in the patients' natural ambience is not always clear. In one study, the finding of OH on HUTT and its connection to dizziness, which was the patients' presenting complaint, was not straightforward.82 In another study there was also no statistically significant association between orthostatic symptoms and detection of OH.84
Thus, on the one hand, orthostatic symptoms may occur in the absence of measurable OH and, on the other hand, detected OH may be asymptomatic.
Are present orthostatic hypotension diagnostic criteria adequate?
The elements of orthostatic blood pressure drop that are relevant to the definition of OH include magnitude, time to reaching the blood pressure difference defined as OH, and reproducibility of orthostatic blood pressure drop.
Magnitude of orthostatic blood pressure decrease
It is unknown whether the above described lower OH threshold represents a general phenomenon or reflects varying susceptibilities of patient subsets to decreases in blood pressure in different clinical settings, aetiologies of OH and presence of comorbidity.77,80 For example, in chronic hypertension, acute traumatic brain injury, ischaemic cerebrovascular disease, subarachnoid haemorrhage, post‐ictal state or hypercapnia, where cerebral autoregulation is impaired, a relatively smaller decrease in blood pressure on standing may result in a clinically important decrease in cerebral blood flow.85,86 Possibly, the magnitude of decrease in blood pressure required for diagnosing OH in the above conditions should be lower than presently recommended. In addition, a lower OH cut‐off at 3 min of orthostatism may be warranted in patients exhibiting the “progressive systolic OH pattern” described by Gehrking et al.55 This subset is associated with an increased risk of syncope later on continued postural challenge.58
Furthermore, different OH cut‐offs may be relevant in utilising the postural test as a diagnostic test in patients with presyncope or utilising the orthostatic test as a screening tool in evaluating the risk of falls, cardiovascular events and mortality. In the Honolulu Heart Program,14 there was a significant dose–response relationship between orthostatic change in blood pressure and mortality. The authors suggest that a better definition of OH in this cohort, in terms of its relation to subsequent mortality, would refer to a decrease in SBP of >10 mm Hg or a decrease in diastolic blood pressure of >5 mm Hg.14 The JNC 7 report recommend use of a 10 mm Hg blood pressure drop in blood pressure when associated with symptoms as clinically relevant.81
Time threshold for orthostatic hypotension
As shown above, the optimal time duration of orthostatic challenge for the diagnosis of OH is probably longer than the 3 min set in the consensus definition.1 A 5 min test may permit the identification of systolic OH patterns, which, in turn, correlate with the severity of autonomic failure and predict the risk of syncope on continuing postural challenge.55 A 5 min test may also reveal a significant number of additional cases of OH (Naschitz et al, personal communication).
Repetitions of orthostatic tests required
A single orthostatic test demonstrating the presence of OH is sufficient for diagnosis. As OH is poorly reproducible, it has been shown that several measurements may be required, on several occasions, to detect OH.42,43,59,60,61,62,63,64,65,80,87 To improve sensitivity, readings should be timed for that time of the day when symptoms are reported to occur.22 In addition, assessing reproducibility of OH over several weeks may be helpful in differentiating acute OH (main causes: intercurrent illness, medications, transient hypovolaemia) from chronic OH (main cause: autonomic failure, baroreceptor desensitisation, hypoadrenalism).
Key references
- Brignole M, Alboni P, Benditt D, et al. Task Force Report. Guidelines on management (diagnosis and treatment) of syncope. Eur Heart J 2001;22:1256–306.
- Carlson JE. Assessment of orthostatic blood pressure. Measurement technique and clinical applications. South Med J 1999;92:167–73.
- Puisieux F, Boumbar Y, Bulckaen H, et al. Intraindividual variability in orthostatic blood pressure changes among older adults: the influence of meals. J Am Geriatr Soc 1999;47:1332–6.
- Masaki KH, Schatz IJ, Burchfiel CM, et al. Orthostatic hypotension predicts mortality in elderly men: the Honolulu Heart Program. Circulation 1998;98:2290–5.
- Chobanian AV, Bakris GL, Black HR, et al. National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure; National High Blood Pressure Education Program Coordinating Committee. The Seventh Report of the Joint National Committee on prevention, detection, evaluation and treatment of high blood pressure the JNC 7 report. JAMA 2003;289:2573–5.
A call for revision of the OH criteria has been recently expressed.14,80,81,84,87 The evidence cited above suggests there may be room for changes in the criteria with respect to the magnitude of OH drop, the time threshold for OH, and number of measurements required in order to establish the diagnosis of OH. Further questions may need to be addressed by the criteria. Should one standard orthostatic test be applied to different patient populations or should tests be tailored to the patients' clinical circumstances? Are different OH thresholds relevant to various clinical settings, aetiologies of OH and comorbidity? Which test has the best predictive power of morbidity and mortality? There is at present no adequate response to the posed questions.
Standardising the assessment of OH is an intermediary goal, which could permit us to identify more accurately OH‐related thresholds for falls, stroke and cardiovascular mortality. To this end, comparative studies of the variety of postural tests and instruments should be carried out. Multicentre studies are needed to compare prospectively the prognostic impact of OH as diagnosed according to present consensus criteria versus OH diagnosed by utilising a 10 mm Hg or 15 mm Hg SBP drop, a 5 mm Hg DBP drop and extending the duration of the postural challenge to 5 min. It is recognised that in reducing the blood pressure drop threshold and extending the duration of the test many more individuals may then be diagnosed with OH, with an unclear impact on medical care. On the other hand, a requirement for reproducibility of OH, which should be incorporated into the prospective studies, may again limit the number of those thus diagnosed.
Multiple choice questions (true (T)/false (F); answers after the references)
1. The following symptoms may be expressions of orthostatic hypotension:
- Dizziness
- Fatigue
- Nocturia
- Chest pain in upright posture
2. The following illustrate the relationship between orthostatic hypotension and orthostatic symptoms:
- Orthostatic symptoms may occur in the absence of orthostatic hypotension
- Orthostatic hypotension may occur in the absence of orthostatic symptoms
- Population based studies showed no significant dose–response relationship between orthostatic change in blood pressure and mortality
- A 10 mm Hg drop in systolic blood pressure when associated with symptoms is clinically relevant
3. The occurrence of orthostatic hypotension is affected by:
- Time of the day
- Season
- Postprandial state
- Febrile illness
4. In assessing orthostatic hypotension:
- The golden standard is the head‐up tilt test
- Beat‐to‐beat blood pressure monitoring is essential for the diagnosis of orthostatic hypotension
- Reproducibility of orthostatic hypotension has been definitely established
- Monitoring heart during orthostatic tests is non‐contributory
5. The burden of orthostatic hypotension on public health is reflected by the following:
- According to different studies, the prevalence of orthostatic hypotension was 7% in elderly subjects and 55% in high risk groups
- The prevalence of orthostatic hypotension among patients presenting with syncope in the emergency room was 24%
- Orthostatic hypotension is independently predictive of ischaemic stroke
- Orthostatic hypotension is independently predictive of cardiovascular mortality
Abbreviations
DBP - diastolic blood pressure
HUTT - head‐up tilt test
OH - orthostatic hypotension
RR - relative risk
SBP - systolic blood pressure
ANSWERS
- (A) T (B) T (C) T (D) T
- (A) T (B) T (C) F (D) T
- (A) T (B) T (C) T (D) T
- (A) F (B) F (C) F (D) F
- (A) T (B) T (C) T (D) T
Footnotes
Competing interests: None.
References
- 1.Kaufmann H. Consensus statement on the definition of orthostatic hypotension, pure autonomic failure and multiple system atrophy. Clin Auton Res 19966125–126. [DOI] [PubMed] [Google Scholar]
- 2.Streeten D H. Orthostatic intolerance. A historical introduction to the pathophysiological mechanisms. Am J Med Sci 199931778–87. [DOI] [PubMed] [Google Scholar]
- 3.Low P A. Laboratory evaluation of autonomic function. In: Low PA, ed. Clinical autonomic disorders: evaluation and management Philadelphia: Lippincott‐Raven, 1997179–208.
- 4.Low P A. Neurogenic orthostatic hypotension. In: Johnson RT, Griffin JW, eds. Current therapy in neurologic disease. St Louis: Mosby‐Year Book, Inc, 199321–26.
- 5.Smit A A J, Halliwill J R, Low P A.et al Pathophysiological basis of orthostatic hypotension in autonomic failure. J Physiol 19995191–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Viramo P, Luukinen H, Koski K.et al Orthostatic hypotension and cognitive decline in older people. J Am Geriatr Soc 199947600–604. [DOI] [PubMed] [Google Scholar]
- 7.Craig G M. Clinical presentation of orthostatic hypotension in the elderly. Postgrad Med 199570638–642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Streeten D H. Variations in the clinical manifestations of orthostatic hypotension. Mayo Clin Proc 199570713–714. [DOI] [PubMed] [Google Scholar]
- 9.Gibbons C H, Freeman R. Orthostatic dyspnea: a neglected symptom of orthostatic hypotension. Clin Auton Res 20051540–44. [DOI] [PubMed] [Google Scholar]
- 10.Lipsitz L A. Orthostatic hypotension in the elderly. N Engl J Med 1989321952–957. [DOI] [PubMed] [Google Scholar]
- 11.Mader S L. Aging and postural hypotension. An update. J Am Geriatr Soc 198937129–137. [DOI] [PubMed] [Google Scholar]
- 12.American Autonomic Society, American Academy of Neurology Consensus statement on the definition of orthostatic hypotension, pure autonomic failure, and multiple system atrophy. The Consensus Committee of the American Autonomic Society and the American Academy of Neurology. Neurology 1996461470. [DOI] [PubMed] [Google Scholar]
- 13.Mathias C J. Orthostatic hypotension: causes, mechanisms, and influencing factors. Neurology 199545S6–S11. [PubMed] [Google Scholar]
- 14.Masaki K H, Schatz I J, Burchfiel C M.et al Orthostatic hypotension predicts mortality in elderly men: the Honolulu Heart Program. Circulation 1998982290–2295. [DOI] [PubMed] [Google Scholar]
- 15.Hale W A, Chambliss M L. Should primary care patients be screened for orthostatic hypotension? J Fam Pract 199948547–552. [PubMed] [Google Scholar]
- 16.Luukinen H, Koski K, Laippala P.et al Prognosis of diastolic and systolic orthostatic hypotension in older persons. Arch Intern Med 1999159273–280. [DOI] [PubMed] [Google Scholar]
- 17.Mader S L, Josephson K R, Rubenstein L Z. Low prevalence of postural hypotension among community‐dwelling elderly. JAMA 19872581511–1514. [PubMed] [Google Scholar]
- 18.Poon I O, Braun U. High prevalence of orthostatic hypotension and its correlation with potentially causative medications among elderly veterans. J Clin Pharm Ther 200530173–178. [DOI] [PubMed] [Google Scholar]
- 19.Rutan G H, Hermanson B, Bild D E.et al Orthostatic hypotension in older adults: the cardiovascular health study. Hypertension 199219508–519. [DOI] [PubMed] [Google Scholar]
- 20.Sarasin F P, Louis‐Simonet M, Carballo D.et al Prevalence of orthostatic hypotension among patients presenting with syncope in the ED. Am J Emerg Med 200220497–501. [DOI] [PubMed] [Google Scholar]
- 21.Gorelik O, Fishlev G, Litvinov V.et al First morning standing up may be risky in acutely ill older inpatients. Blood Press 200514139–143. [DOI] [PubMed] [Google Scholar]
- 22.Ooi W L, Hossain M, Lipsitz L A. The association between orthostatic hypotension and recurrent falls in nursing home residents. Am J Med 2000108106–111. [DOI] [PubMed] [Google Scholar]
- 23.Ganz D A, Bao Y, Shekelle P G.et al Will my patient fall? JAMA 200729777–86. [DOI] [PubMed] [Google Scholar]
- 24.Eigenbrodt M L, Rose K M, Couper D J.et al Orthostatic hypotension as a risk factor for stroke: the atherosclerosis risk in communities (ARIC) study, 1987–1996. Stroke 2000312307–2313. [DOI] [PubMed] [Google Scholar]
- 25.Longstreth W T, Jr, Manolio T A, Arnold A, for the Cardiovascular Health Study Collaborative Research Group. et al Clinical correlates of white matter findings on cranial magnetic resonance imaging of 3301 elderly people. Stroke 1996271274–1282. [DOI] [PubMed] [Google Scholar]
- 26.Luukinen H, Airaksinen K E. Orthostatic hypotension predicts vascular death in older diabetic patients. Diabetes Res Clin Pract 200567163–166. [DOI] [PubMed] [Google Scholar]
- 27.Carlson J E. Assessment of orthostatic blood pressure. Measurement technique and clinical applications. South Med J 199992167–173. [DOI] [PubMed] [Google Scholar]
- 28.Grimm C M, Grimm C E. Blood pressure measurement. In: Izzo JL, Black HE, eds. Hypertension primer, 3rd ed. Lippincott Williams & Wilkins 2003321–324.
- 29.O'Brien E, Petrie J, Littler W A.et al British hypertension protocol: evaluation of automated and semi‐automated blood pressure measuring devices with special reference to ambulatory systems. J Hypertens 19908607–619. [DOI] [PubMed] [Google Scholar]
- 30.Anon Training and certification of blood pressure observers. Hypertension 19835610–614. [DOI] [PubMed] [Google Scholar]
- 31.Bates B, Bickley L S, Hoekelman R A. eds. A guide to physical examination and history taking, 6th ed. Philadelphia: JB Lippincott Co, 1995276–279.
- 32.Baker R H, Ende J. Confounders of auscultatory blood pressure measurement. J Gen Intern Med 199510223–231. [DOI] [PubMed] [Google Scholar]
- 33.Parati G, Casadei R, Groppelli A.et al Comparison of finger and intra‐arterial blood pressure monitoring at rest and during laboratory testing. Hypertension 198913(6 Pt 1)647–655. [DOI] [PubMed] [Google Scholar]
- 34.Silke B, McAuley D. Accuracy and precision of blood pressure determination with the Finapres: an overview using re‐sampling statistics. J Hum Hypertens 199812403–409. [DOI] [PubMed] [Google Scholar]
- 35.Cua C L, Thomas K, Zurakowski D.et al A comparison of the Vasotrac with invasive arterial blood pressure monitoring in children after pediatric cardiac surgery. Anesth Analg 20051001289–1294. [DOI] [PubMed] [Google Scholar]
- 36.O'Rourke M F, Seward J B. Central arterial pressure and arterial pressure pulse: new views entering the second century after Korotkov. Mayo Clin Proc 2006811057–1068. [DOI] [PubMed] [Google Scholar]
- 37.Low P A, Opfer‐Gehrking T L, McPhee B P. Prospective evaluation of clinical characteristics of orthostatic hypotension. Mayo Clin Proc 199570617–622. [DOI] [PubMed] [Google Scholar]
- 38.Abrass I B. The biology and physiology of aging. West Med J 1990153641–645. [PMC free article] [PubMed] [Google Scholar]
- 39.Schutzman J, Jaeger F, Maloney J.et al Head‐up tilt and hemodynamic changes during orthostatic hypotension in patients with supine hypertension. J Am Coll Cardiol 199424454–461. [DOI] [PubMed] [Google Scholar]
- 40.Weinberg A D, Minaker K L. Dehydration: evaluation and management in older adults. JAMA 19952741552–1556. [DOI] [PubMed] [Google Scholar]
- 41.Winker R, Prager W, Haider A.et al Schellong test in orthostatic hypotension: a comparison with tilt table testing. Wien Klin Wochenschrift 200511736–41. [DOI] [PubMed] [Google Scholar]
- 42.Horrocks P M, FitzGerald M G, Wright A D.et al The time course and diurnal variation of postural hypotension in diabetic autonomic neuropathy. Diabet Med 19874307–310. [DOI] [PubMed] [Google Scholar]
- 43.Patel A, Maloney A, Damato A N. On the frequency and reproducibility of orthostatic blood pressure changes in healthy community‐dwelling elderly during 60‐degree head‐up tilt. Am Heart J 1993126184–188. [DOI] [PubMed] [Google Scholar]
- 44.Mader S, Hornick T, Winger J. Effect of initial recumbent or sitting positions on postural blood pressure measurements [abstract]. Gerontologist 198727206A [Google Scholar]
- 45.Biaggioni I, Robertson R M. Hypertension in orthostatic hypotension and autonomic dysfunction. Cardiology Clinics 200220291–301. [DOI] [PubMed] [Google Scholar]
- 46.Streeten D H, Anderson G H., Jr Delayed orthostatic intolerance. Arch Intern Med 19921521066–1072. [PubMed] [Google Scholar]
- 47.Aronow W S, Lee N H, Sales F F.et al Prevalence of postural hypotension in elderly patients in a longterm health care facility. Am J Cardiol 198862336. [DOI] [PubMed] [Google Scholar]
- 48.Kennedy G T, Crawford M H. Optimal position and timing of blood pressure and heart rate measurements to detect orthostatic changes in patients with ischemic heart disease. J Cardiac Rehabil 19844219–223. [Google Scholar]
- 49.Kuchel G A, Avorn J, Reed M J.et al Cardiovascular responses to phlebotomy and sitting in middle aged and elderly subjects. Arch Intern Med 1992152366–370. [PubMed] [Google Scholar]
- 50.Cohen N, Gorelik O, Fishlev G.et al Seated postural hypotension is common among older inpatients. Clin Auton Res 200313447–449. [DOI] [PubMed] [Google Scholar]
- 51.Brignole M. Alboni P, Benditt D, et al. Task Force Report. Guidelines on management (diagnosis and treatment) of syncope. Eur Heart J 2001221256–1306. [DOI] [PubMed] [Google Scholar]
- 52.Wieling W, Karemaker J M, Mathias J. Measurement of heart rate and blood pressure to evaluate disturbances in neurocardiovascular control. In: ed. Autonomic failure. A textbook of clinical disorders of the autonomic nervous system, 4th ed. Oxford: Oxford University Press, 1999198–210.
- 53.Mehagnoul‐Schipper D J, van Kraaij D J, Jansen R W. Achieving haemodynamic baseline values with Finapres in elderly subjects during supine rest. Clin Physiol 200020466–473. [DOI] [PubMed] [Google Scholar]
- 54.Gorelik O, Fishlev G, Litvinov V.et al First morning standing up may be risky in acutely ill older inpatients. Blood Press 200514139–143. [DOI] [PubMed] [Google Scholar]
- 55.Gehrking J A, Hines S M, Benrud‐Larson L M.et al What is the minimum duration of headup tilt necessary to detect orthostatic hypotension? Clin Auton Res 20051571–75. [DOI] [PubMed] [Google Scholar]
- 56.Gibbons C H, Freeman R. Delayed orthostatic hypotension: a frequent cause of orthostatic intolerance. Neurology 20066728–32. [DOI] [PubMed] [Google Scholar]
- 57.Naschitz J E, Mussafia‐Priselac R, Kovalev Y.et al Predicting outcomes on head‐up tilt based on orthostatic hypotension patterns. J Hypertens 2006241033–1039. [DOI] [PubMed] [Google Scholar]
- 58.Herpin D, Ragot S. Mid‐ and long‐term reproducibility of noninvasive measurements of spontaneous arterial baroreflex sensitivity in healthy volunteers. Am J Hypertens 199710790–797. [DOI] [PubMed] [Google Scholar]
- 59.Giaconi S, Palombo C, Genovesi‐Ebert A.et al Medium‐term reproducibility of stress tests in borderline arterial hypertension. J Clin Hypertens 19873654–660. [PubMed] [Google Scholar]
- 60.Jost W H, Rapp C, Konig J.et al Are heart rate responses reproducible in the tilt‐table test? Clin Invest 199472996–999. [DOI] [PubMed] [Google Scholar]
- 61.Ward C, Kenny R A. Reproducibility of orthostatic hypotension in symptomatic elderly. Am J Med 1996100418–422. [DOI] [PubMed] [Google Scholar]
- 62.Vanhanen H, Thijs L, Birkenhager W.et al Prevalence and persistency of orthostatic blood pressure fall in older patients with isolated systolic hypertension. Syst‐Eur Investigators. J Hum Hypertens 199610607–612. [PubMed] [Google Scholar]
- 63.Jansen R W, Kelly‐Gagnon M M, Lipsitz L A. Intraindividual reproducibility of postprandial and orthostatic blood pressure changes in older nursing‐home patients: relationship with chronic use of cardiovascular medications. J Am Geriatr Soc 199644383–389. [DOI] [PubMed] [Google Scholar]
- 64.Weiss A, Grossman E, Beloosesky Y.et al Orthostatic hypotension: is it a consistent finding? Arch Intern Med 20021622369–2374. [DOI] [PubMed] [Google Scholar]
- 65.Ooi W L, Barrett S, Hossain M.et al Patterns of orthostatic blood pressure change and their clinical correlates in a frail, elderly population. JAMA 19972771299–1304. [PubMed] [Google Scholar]
- 66.Weiss A, Beloosesky Y, Grinblat J.et al Seasonal changes in orthostatic hypotension among elderly admitted patients. Aging Clin Exp Res 20061820–24. [DOI] [PubMed] [Google Scholar]
- 67.Vaitkevicius P V, Esserwein D M, Maynard A K.et al Frequency and importance of postprandial blood pressure reduction in elderly nursing‐home patients. Ann Intern Med 1991115865–870. [DOI] [PubMed] [Google Scholar]
- 68.Maurer M S, Karmally W, Rivadeneira H.et al Upright posture and postprandial hypotension in elderly persons. Ann Intern Med 2000133533–536. [DOI] [PubMed] [Google Scholar]
- 69.Potter J F, Heseltine D, Hartley G.et al Effects of meal composition on the postprandial blood pressure, catecholamine and insulin changes in elderly subjects. Clin Sci 198977265–272. [DOI] [PubMed] [Google Scholar]
- 70.Mader S L. Effects of meals and time of day on postural blood pressure responses in young and elderly subjects. Arch Intern Med 19891492757–2760. [PubMed] [Google Scholar]
- 71.Vloet L C, Smits R, Frederiks C M.et al Evaluation of skills and knowledge on orthostatic blood pressure measurements in elderly patients. Age Ageing 200231211–216. [DOI] [PubMed] [Google Scholar]
- 72.Caine S E, Alsop K, Mac Mahon M. Overlooking orthostatic hypotension with routine blood‐pressure equipment. Lancet 1998352458. [DOI] [PubMed] [Google Scholar]
- 73.Boddaert J, Magula D, Belmin J. Diagnosis of orthostatic hypotension. Lancet 19983521705–1706. [DOI] [PubMed] [Google Scholar]
- 74.Tabara Y, Nakura J, Kondo I.et al Orthostatic systolic hypotension and the reflection pressure wave. Hypertens Res 200528537–543. [DOI] [PubMed] [Google Scholar]
- 75.Paulson O B, Strandgaard S, Edvinsson L. Cerebral autoregulation. Cerebrovasc Brain Metab Rev 19902161–192. [PubMed] [Google Scholar]
- 76.Roman R R. Autoregulation of cerebral blood flow. In: Izzo JL, Black HR, eds. Hypertension primer, 3d ed. American Heart Association 2003114–117.
- 77.Edwards M R, Devitt D L, Hughson R L. Two‐breath CO2 test detects altered dynamic cerebrovascular autoregulation and CO2 responsiveness with changes in arterial PCO2. Am J Physiol Regul Integr Comp Physiol 2004287R627–R632. [DOI] [PubMed] [Google Scholar]
- 78.Robertson D. Orthostatic tachycardia and orthostatic intolerance. Am J Med Sci 199931775–77. [DOI] [PubMed] [Google Scholar]
- 79.Naschitz J E, Gaitini L, Mazov I.et al The capnography‐tilt test for the diagnosis of hyperventilation syncope. Q J M 199790139–145. [DOI] [PubMed] [Google Scholar]
- 80.Weiss A, Chagnac A, Beloosesky Y.et al Orthostatic hypotension in the elderly: are the diagnostic criteria adequate? J Human Hypertens 200418301–305. [DOI] [PubMed] [Google Scholar]
- 81.Chobanian A V, Bakris G L, Black H R.et al National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure; National High Blood Pressure Education Program Coordinating Committee. The Seventh Report of the Joint National Committee on prevention, detection, evaluation and treatment of high blood pressure the JNC 7 report. JAMA 20032892573–2575. [DOI] [PubMed] [Google Scholar]
- 82.Naschitz J E, Mussafia‐Priselac R, Kovalev Y.et al Nonspecific dizziness: frequency of supine hypertension associated with hypotensive reactions on head‐up tilt. J Hum Hypertens 200520157–162. [DOI] [PubMed] [Google Scholar]
- 83.Sorond F A, Khavari R, Serrador J M.et al Regional cerebral autoregulation during orthostatic stress: age‐related differences. J Gerontol A Biol Sci Med Sci 2005601484–1487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Chambers J C. Should we screen hospice inpatients for orthostatic hypotension? Palliat Med 200519314–318. [DOI] [PubMed] [Google Scholar]
- 85.Ginsberg M D. Cerebral circulation: its regulation, pharmacology, and pathophysiology. In: Asbury AK, McKhaann GM, Mcdonald WI, eds. Diseases of the nervous system. Clinical neurobiology Philadelphia: Saunders, 1992989–1001.
- 86.Vavila M S, Lee L A, Lam A M. Cerebral blood flow and vascular physiology. Anesthesiol Clin N Am 200220247–264. [DOI] [PubMed] [Google Scholar]
- 87.Puisieux F, Boumbar Y, Bulckaen H.et al Intraindividual variability in orthostatic blood pressure changes among older adults: the influence of meals. J Am Geriatr Soc 1999471332–1336. [DOI] [PubMed] [Google Scholar]