The joint effects of apolipoprotein B, apolipoprotein A1, LDL cholesterol, and HDL cholesterol on risk: 3510 cases of acute myocardial infarction and 9805 controls (original) (raw)
Abstract
Aims
Plasma levels of apolipoprotein B (apoB), the main surface protein on LDL particles, and LDL-C, the amount of cholesterol in those particles, are closely correlated and, considered separately, are positive risk factors. Plasma levels of apolipoprotein A1, the main surface protein on HDL particles, and HDL-C, the amount of cholesterol in those particles, are also closely correlated with each other and, considered separately, are negative risk factors. The interdependence of these four risk factors is unclear.
Methods and results
Case–control study among 3510 acute myocardial infarction patients (without prior vascular disease, diabetes, or statin use) in UK hospitals and 9805 controls. Relative risks (age, sex, smoking, and obesity-adjusted) were more strongly related to apoB than to LDL-C and, given apoB, more strongly negatively related to apoA1 than to HDL-C. The ratio apoB/apoA1 was uncorrelated with time since symptom onset in cases, was reproducible in samples collected a few years apart in controls (correlation 0.81), and encapsulated almost all the predictive power of these four measurements. Its effect was continuous, substantial throughout the UK normal range [relative risk, top vs. bottom decile of this ratio, 7.3 (95% CI 5.8–9.2)] and varied little with age. The ratio apoB/apoA1 was substantially more informative about risk (_χ_12 = 550) than were commonly used measures such as LDL-C/HDL-C, total/HDL cholesterol, non-HDL cholesterol, and total cholesterol (_χ_12 = 407, 334, 204, and 105, respectively). Given apoB and apoA1, the relationship with risk of LDL-C was reversed, and this reversal was strengthened by appropriate allowance for random measurement errors in two correlated variables. Given usual apoB, lower LDL-C (consistent with smaller LDL particles) was associated with higher risk (P < 0.0001). During the first 8 h after symptom onset HDL-C increased by about 10%, precluding reliable assessment of the joint relationship of apoA1 and pre-onset HDL-C with risk in such retrospective case–control studies.
Conclusion
Apolipoprotein ratios are more informative about risk than lipid fractions are. This suggests that, among lipoprotein particles of a particular type (LDL or HDL), some smaller and larger subtypes differ in their effects on risk. Direct measurements of even more specific subtypes of lipoprotein particles may be even more informative about risk.
Keywords: Myocardial infarction, Lipoproteins, Lipids, Cholesterol, Risk factors
Introduction
Some low-density lipoprotein (LDL) particles can damage coronary arteries, and some high-density lipoprotein (HDL) particles can help limit the damage. Hence, plasma levels of LDL cholesterol (LDL-C) and HDL cholesterol (HDL-C)—the total amounts of cholesterol being carried in LDL and in HDL particles—are, respectively, positive and negative risk factors for coronary heart disease, as are plasma levels of apolipoproteins B (apoB) and A1 (apoA1), which are, respectively, the main surface proteins on LDL and on HDL particles. Consideration of all four factors could improve risk prediction and understanding.
Plasma LDL and HDL particles have different origins and functions. Big, triglyceride-laden precursors of LDL particles enter the circulation as very-low-density lipoprotein particles and deliver their contents to peripheral tissues, rapidly shrinking into intermediate-density lipoprotein particles which, unless cleared, shrink to LDL particles. Each LDL precursor particle has exactly one molecule of apoB on its surface, which remains there during shrinkage to an LDL particle.1 Generally, more than 90% of plasma apoB is on LDL particles (the remainder being on their precursors) and most plasma cholesterol is in LDL particles. Larger LDL particles carry about 2500 molecules of cholesterol, but smaller, denser LDL particles might carry only about 2000.2 Some studies have suggested that small, dense LDL particles may be particularly hazardous,3 although other studies have not.4,5
The precursors of HDL particles are initially small (containing no cholesterol) and then repeatedly gain cholesterol and lose some cholesterol, but even the largest HDL particles are much smaller and denser than any LDL particles. The HDL particles each have a few (e.g. two or three) molecules of apoA1 on their surface and account for nearly all plasma apoA1.6 They vary considerably in size, cholesterol content, and probably in biological activity. Collectively, HDL particles (and their precursors) can reverse-transport excess cholesterol from peripheral tissues, such as artery walls. Small HDL particles, which are more numerous, typically carry only two molecules of apoA1 and a few dozen cholesterol molecules, while large ones might carry three molecules of apoA1 and over 100 cholesterol molecules. Such HDL particles can transfer some of their load of cholesterol to the triglyceride-rich precursors of LDL particles, and high triglyceride levels are associated with low HDL-C levels. The independent relevance of HDL-C (or of particular types of HDL particle) to risk is, therefore, best assessed by analyses that are adjusted for any effects on risk of LDL particles or their precursors.
As the ratios of cholesterol to apolipoprotein within LDL and within HDL particles can vary, the positive associations of apoB and of LDL-C with risk may differ, as may the negative associations of apoA1 and of HDL-C with risk. It has been reported that apoB and apoA1 are even stronger correlates of risk than LDL-C and HDL-C are,7,8 but no study with a large number of cases with disease has involved direct measurement of all four factors.
The present study, with direct measurements of LDL-C, HDL-C, apoB, and apoA1, investigates risk associations in 3510 cases of non-fatal acute myocardial infarction (MI) and 9805 controls, all without any previous history of vascular disease or diabetes (and hence little use of lipid-altering drugs).
Methods
Design, setting, and participants
The study design is described elsewhere, and in Supplementary material online, Appendix.9–15 Potential cases were acute MI survivors aged 30–79 in 1989–90 in the UK who had given blood on entry to hospital (mean 6 h from pain onset). Controls were first degree relatives of potential cases or spouses of such relatives. Whole blood spent a mean of 1.8 days in the post before being separated in Oxford (Supplementary material online, Tables A1–A3). This report is of the 3510 cases and 9805 controls with valid assay results for apoB, apoA1, LDL-C, HDL-C, and total cholesterol, and with no prior vascular disease or diabetes (Table 1; Supplementary material online, Tables A4–A5). The apoB, apoA1, LDL-C, and total cholesterol levels were not associated with hours from onset of pain in cases; HDL-C increased with hours from pain onset, however (Supplementary material online, Figure A1), and this was corrected for.
Table 1.
Lipid-related factors in cases and controls: means and coefficients of variation of measured values, calculated after adjustment for age, sex, smoking, and body mass index
| Characteristic | Cases (3510) | Controls (9805) | ||
|---|---|---|---|---|
| Mean | CV, % | Mean | CV, % | |
| Lipid-related measurements | ||||
| LDL-C (mmol/L) | 3.636 | 25 | 3.362 | 23 |
| ApoB (g/L) | 1.166 | 21 | 1.064 | 20 |
| HDL-C (mmol/L) | 1.122 | 22 | 1.242 | 23 |
| ApoA1 (g/L) | 1.375 | 15 | 1.449 | 15 |
| Total cholesterol (mmol/L) | 5.864 | 19 | 5.596 | 17 |
| Ratios of measurements | ||||
| LDL-C/apoB | 3.118 | 13 | 3.162 | 13 |
| HDL-C/apoA1 | 0.814 | 16 | 0.853 | 16 |
| LDL-C/HDL-C | 3.411 | 32 | 2.881 | 30 |
| Total cholesterol/HDL-C | 5.512 | 30 | 4.786 | 26 |
| ApoB/apoA1 | 0.863 | 23 | 0.749 | 22 |
Statistical methods
For details see Supplementary material online, Appendix.
Relative risks and floating absolute risks
Relative risks of MI (RRs; case vs. control odds ratios) were estimated by logistic regression using SAS16,17 adjusted for age, sex, current smoking, and body mass index (BMI). Plots of risk use groupings based on decile boundaries (among cases) of similarly adjusted analyte values. Relative risks are presented as ‘floating absolute risks’18 with 95% confidence intervals (CIs), and _P_-values are two-sided.
Measured values and usual values
Logistic regression yields b, the log of the relative risk associated with a unit difference in the measured value of a lipid-related factor. Because of random measurement error (which includes any within-person fluctuation), this regression coefficient tends to underestimate the real importance of a unit difference in the ‘usual’ (i.e. medium-term average) level of that factor.19 This ‘regression dilution’ bias is corrected for by dividing b by r, the self-correlation between measurements of that factor in blood samples taken 2–3 years apart from 1042 controls. Likewise, when the measured values of a lipid-related factor are divided into several groups, the mean usual value in each group is taken to differ from that in the central group by r times the corresponding difference in the measured values. (Simultaneous correction for measurement error in two positively correlated factors is described in the Results.)
Relative risk per two standard deviation difference in the usual value
To facilitate direct comparison of the strengths of different associations, for each factor relative risks are presented for a 2SD difference of that factor, where SD is defined as the standard deviation of the usual value in cases (given age, sex, smoking and BMI). Plots of risk (Figure 1) have been scaled so that the same physical distance horizontally represents 2SD for each factor. (Note that the difference between the mean values in the top and bottom thirds of a normal distribution is 2.2 standard deviations.)
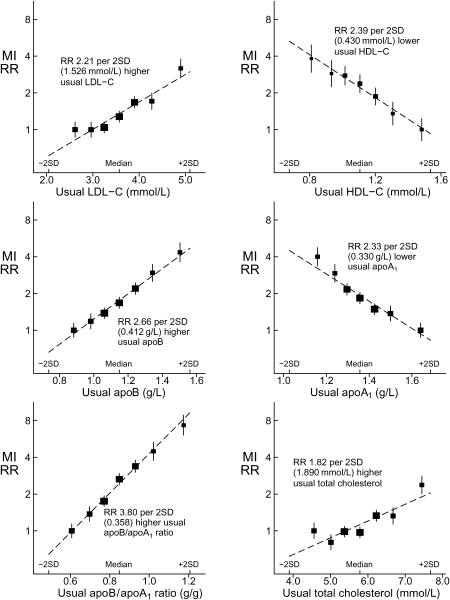
Figure 1.
Relative risk of myocardial infarction at different usual levels of LDL-C, HDL-C, apoB, apoA1, their ratio (apoB/apoA1) and total cholesterol based on 3510 cases vs. 9805 controls, all without prior vascular disease. Relative risks and 95% CIs, adjusted for age, sex, smoking, and body mass index, are plotted against the mean usual value (i.e. the medium-term average value after allowance for measurement error). The seven groups are based on deciles or, for the middle three groups, quintiles of the values among cases. Horizontal scales are defined similarly in all graphs, with the marked points 2SD above and below the median (in the middle group) at the same positions. MI, myocardial infarction; RR, relative risk; SD, standard deviation of usual value in cases.
Magnitude of improvement in risk prediction
Twice the increase in the log-likelihood on the addition of extra terms gives a _χ_2 statistic, with degrees of freedom equal to the number of extra terms added. This provides not only a significance test for the improvement in fit from including the added terms but also, more importantly, a quantitative measure of the extent to which the added terms improve risk prediction. (The _χ_2 improvement on jointly fitting several independent risk factors is approximately the sum of the _χ_2 improvements on fitting each separately.)
Robustness
Further analyses, and sensitivity analyses of the robustness of the main findings, are in Supplementary material online, Tables A6–A9.
Results
Relationship of risk to usual values of single factors
Table 1 gives the means in cases and controls of the five directly measured biochemistries and selected ratios of them. Figure 1 shows MI risk vs. usual values for six lipid-related factors, with fitted lines from Table 2. The association was strongly positive for LDL-C and apoB, strongly negative for HDL-C and apoA1, and even more strongly positive for the ratio apoB/apoA1. The relative risk comparing the top vs. bottom decile of this ratio was 7.33 (95% CI 5.81–9.24, allowing for the floated variances in both groups). Total cholesterol was more weakly related to risk.
Table 2.
Relative risks associated with differences of 2SD in the usual values of various lipid-related factors
| Lipid-related factor | _r_a | Meana | 2SDb | RR associated with a difference of 2SD in usual valueb | |
|---|---|---|---|---|---|
| RR (95% CI) | _χ_2 | ||||
| LDL-related factors | |||||
| LDL-C (mmol/L) | 0.730 | 3.64 | 1.526 | 2.21 (1.96–2.48) | 175.2 |
| ApoB (g/L) | 0.733 | 1.17 | 0.412 | 2.66 (2.37–2.99) | 279.7 |
| HDL-related factors | |||||
| HDL-C (mmol/L) | 0.768 | 1.12 | 0.430 | 2.39 (2.03–2.81) | 290.6 |
| ApoA1 (g/L) | 0.680 | 1.38 | 0.330 | 2.33 (2.07–2.62) | 212.9 |
| HDL-related factors, adjusted for apoB | |||||
| HDL-C (mmol/L) | 2.06 (1.76–2.44) | 187.7 | |||
| ApoA1 (g/L) | 2.71 (2.40–3.06) | 278.5 | |||
| Total and non-HDL cholesterol | |||||
| Total cholesterol (mmol/L) | 0.757 | 5.86 | 1.890 | 1.82 (1.62–2.04) | 104.9 |
| Non-HDL cholesterol (mmol/L) | 0.771 | 4.74 | 1.756 | 2.10 (1.89–2.33) | 204.3 |
| Ratios | |||||
| LDL-C/apoB | 0.327 | 3.12 | 0.466 | 0.78 (0.66–0.92) | 8.7 |
| HDL-C/apoA1 | 0.531 | 0.81 | 0.194 | 1.94 (1.52–2.47) | 106.9 |
| Total/HDL cholesterol | 0.717 | 5.51 | 2.766 | 3.10 (2.63–3.64) | 334.5 |
| LDL-C/HDL-C | 0.741 | 3.41 | 1.834 | 3.26 (2.82–3.78) | 406.8 |
| ApoB/apoA1 | 0.812 | 0.86 | 0.358 | 3.80 (3.38–4.27) | 549.6 |
Table 2 gives relative risks per 2SD difference for several common measures. The ratio apoB/apoA1 was a substantially stronger risk factor than the ratio LDL-C/HDL-C (_χ_12 = 549.6 and 406.8, respectively) or any other measure. If total and HDL cholesterol were the only measurements used, then for risk prediction the ratio total/HDL cholesterol was much better than non-HDL cholesterol (_χ_12 = 334.5 and 204.3, respectively).
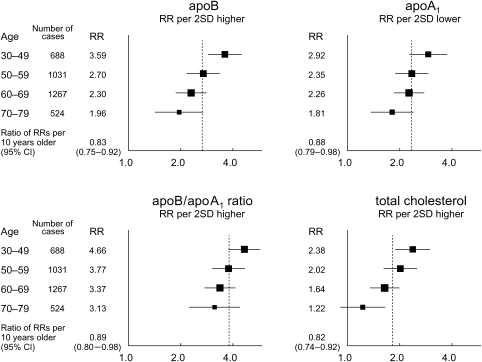
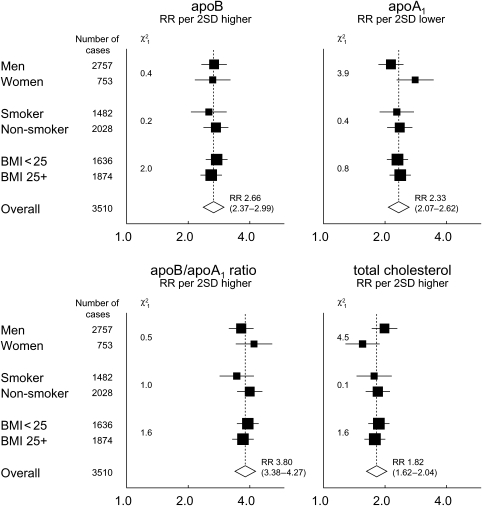
Figure 2 shows the effects of age on the relative risks. For apoB, apoA1, and particularly, apoB/apoA1, any attenuation appeared to be small in proportion to the effect in middle age. So, even at ages 70–79, a 2SD higher apoB/apoA1 ratio was associated with a highly significant (P < 0.00001) relative risk of 3.13. For total cholesterol, however, there appeared to be substantial attenuation with age (as in some other studies20–23). Relative risks within other subgroups (Figure 3) showed no clear heterogeneity of effect with respect to sex, smoking, or BMI.
Figure 2.
Effect of age on relative risk per 2SD difference in the usual levels of apolipoproteins and total cholesterol. Relative risks and 95% confidence intervals (for 3510 cases and 9805 controls) are adjusted for sex, smoking, and body mass index. RR, relative risk; SD, standard deviation of usual value in cases.
Figure 3.
Effects of sex, smoking, and body mass index on relative risk per 2SD difference in the usual levels of apolipoproteins and total cholesterol. Relative risks, with 95% confidence intervals and _χ_2 tests for heterogeneity, for 3510 cases and 9805 controls. Analyses of each factor are adjusted for age and the two other factors. RR, relative risk; SD, standard deviation of usual value in cases; BMI, body mass index.
Correlations between measurements of different factors
Correlations between measurements some time apart (Table 3, right), which avoid artefactual same-sample effects, showed that apoB and LDL-C were not just two equivalent ways of assaying LDL particles, nor were apoA1 and HDL-C two equivalent ways of assaying HDL particles. For, there was a highly significantly negative correlation between apoB and HDL-C (c = −0.20, SE 0.02), but not between LDL-C and apoA1 (c = 0.00, SE 0.02). Moreover, the ratios LDL-C/apoB and HDL-C/apoA1 were positively correlated with each other (c = 0.17, SE 0.02), showing that both were informative. These correlations have been independently replicated24 (Supplementary material online, Table A6).
Table 3.
Correlation coefficients (c) between measurements of different lipid-related factors
| Same sample (9805) | Different sample (2 × 1042) | |
|---|---|---|
| Within LDL particles | ||
| ApoB vs. LDL-C | 0.85 | 0.68 |
| Within HDL particles | ||
| ApoA1 vs. HDL-C | 0.70 | 0.64 |
| Between LDL and HDL particles | ||
| ApoB vs. apoA1 | 0.09 | −0.06 |
| ApoB vs. HDL-C | −0.22 | −0.20 |
| ApoB vs. HDL-C/apoA1 | −0.39 | −0.25 |
| LDL-C vs. apoA1 | 0.06 | 0.00 |
| LDL-C vs. HDL-C | −0.06 | −0.08 |
| LDL-C vs. HDL-C/apoA1 | −0.13 | −0.13 |
| LDL-C/apoB vs. apoA1 | −0.04 | 0.11 |
| LDL-C/apoB vs. HDL-C | 0.24 | 0.18 |
| LDL-C/apoB vs. HDL-C/apoA1 | 0.39 | 0.17 |
The negative correlation between apoB and HDL-C corresponds to the correlations of triglycerides with high apoB and low HDL-C (and, particularly, with a low ratio of HDL-C to apoA1; Supplementary material online, Table A7).
Joint relationship of risk to measured values of more than one factor
Table 4 (and Supplementary material online, Table A8) gives the improvements in fit when one or several extra terms were added into the logistic regression. The _χ_2 for adding apoB alone (279.7) was virtually as great as that for adding both LDL-related factors, apoB and LDL-C (281.3: Table 4). Indeed, given the measured value of apoB, that of LDL-C was slightly negatively related to risk. The _χ_2 for adding LDL-C alone was, in contrast, only 175.2, giving a _χ_2 of 106.1 (281.3–175.2; P < 0.00001) for the addition of apoB given LDL-C.
Table 4.
Comparison of predictive strengths for myocardial infarction relative risk of adding different combinations of lipid-related terms
| Added lipid-related terms | Degrees of freedom (df) | Improvement in fit (_χ_2)a | Direction of association of respective terms |
|---|---|---|---|
| LDL related | |||
| LDL-C | 1 | 175.2 | + |
| ApoB | 1 | 279.7 | + |
| ApoB, LDL-C | 2 | 281.3 | +, − |
| HDL related | |||
| HDL-C | 1 | 290.6 | − |
| ApoA1 | 1 | 212.9 | − |
| ApoA1, HDL-C | 2 | 312.6 | −, − |
| HDL related, with apoB already in the model | |||
| HDL-C | 1 | 187.7 | − |
| ApoA1 | 1 | 278.5 | − |
| ApoA1, HDL-C | 2 | 287.2 | −, − |
Taken singly, without any information about LDL particles, HDL-C was somewhat more informative than the other HDL-related factor, apoA1 (_χ_2 = 290.6 and 212.9, respectively: Table 4). However, part of the negative predictive power of HDL-C came from its negative association with apoB (Table 3). Given apoB, the gain from adding HDL-C was reduced and that from adding apoA1 was increased, so apoA1 became more informative than HDL-C (_χ_2 = 278.5 and 187.7, respectively, Table 4). In the joint relationship of risk to the measurements of apoB, apoA1, and HDL-C the regression coefficient for HDL-C remained slightly negative.
The two strongest risk factors were apoB and, given apoB, apoA1. Moreover, their joint effect was much stronger than that of either alone [_χ_2 = 558.2 for their joint fit: Supplementary material online, Table A8 (279.7+278.5 in Table 4)]. Measurements of LDL-C and HDL-C were weaker predictors (_χ_2 = 462.9 for their joint fit: Supplementary material online, Table A8). ApoB was positively and apoA1 negatively associated with risk, and the ratio apoB/apoA1 encapsulated almost all the risk prediction from these two measurements, or from all four measurements (Supplementary material online, Table A8). When all four measurements were fitted, the improvement in predictive power over just apoB and apoA1 was conventionally significant, but slight (_χ_2 = 567.0–558.2=8.8 on 2 df; P = 0.02: Supplementary material online, Table A8).
Joint relationship of risk to usual values
The joint relationship of risk with two strongly correlated factors, such as apoB and LDL-C, cannot be as easily corrected for measurement error25 as single-factor relationships can be. If, however, both analytes are expressed comparably, in units of 2SD, then their sum is approximately uncorrelated with the difference between them. When risk is related jointly to this sum and difference, the appropriate correction factors for the two terms should therefore be approximately independent of each other. As the sum (apoB +LDL-C) is more reproducible in measurements taken a few years apart than is the difference (apoB−LDL-C), correction for the effects of measurement error has less effect on the regression coefficient for the sum than on that for the difference.
Numerical detail of joint relationship (Supplementary material online, Panel A1):
The log relative risk (with both analytes in units of 2SD) was:
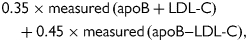
which depends strongly on measured apoB but not on measured LDL-C. After correction for measurement error, however, this formula became:
which rearranges to:
This indicates that, given the usual value of apoB, the usual value of LDL-C was strongly negatively correlated with risk (regression coefficient –1.05, SE 0.26, P < 0.0001).
Sensitivity analyses
Although apoA1, apoB, and LDL-C among cases were approximately independent of hours from onset of symptoms, HDL-C increased by about 1% per hour (Supplementary material online, Figure A1). Despite correcting for this (Supplementary material online, Appendix), the exact pre-infarction value was somewhat uncertain. Although reasonable uncertainties in how to extrapolate HDL-C back to pre-infarction levels have little effect on the results for HDL-C alone (or for HDL-C given apoB), they could appreciably affect results for HDL-C given apoA1, so no analyses of this are presented (beyond those in Table 4).
In some age/sex groups, cases substantially outnumbered controls, or vice-versa. This has been allowed for by adjustment of all analyses for age and sex, but similar results were obtained by random selection of a subset balanced by sex and single year of age. This and the other sensitivity analyses are in Supplementary material online, Table A9.
Discussion
As expected, when each of the four main risk factors was considered separately, usual levels of apoB and LDL-C were both strongly positively associated with risk, while usual levels of apoA1 and HDL-C were both strongly negatively associated with risk. A key additional finding is that, given the usual apoB, usual LDL-C was negatively associated with risk.
Causal relevance of low-density lipoprotein particles
Plasma apoB reflects precisely the total number of LDL-related particles (LDL particles or their triglyceride-rich precursors). As LDL particles greatly outnumber their precursors, plasma apoB is closely correlated with the number of LDL particles per unit volume. Genetic defects that decrease clearance of LDL particles cause familial hypercholesterolaemia and very high risk, showing that LDL particles can actually cause coronary artery disease. Likewise, statin treatment increases clearance of LDL particles and, in randomized trials, causes a substantial reduction in apoB, in LDL-C, and in risk.26 Hence, the strong association of apoB with MI risk must to some considerable extent reflect the causal relationship between LDL particles and disease. Our finding that, for a given usual apoB, lower LDL-C was associated with a higher risk of MI supports previous suggestions27 that, on average, LDL particles with low cholesterol content per particle (small, dense LDL particles) are particularly hazardous. Reliable assessment of the risks caused by particular types of LDL particle requires, however, more direct measurement of the numbers of particles of different types and subtypes, allowing their inter-relationships to be explored.
Causal relevance of high-density lipoprotein particles
Plasma apoB is not strongly related to apoA1, but it is strongly inversely related to HDL-C. (This is partly because triglyceride-rich LDL precursors can remove cholesterol from the larger HDL particles, reducing HDL-C levels but not HDL particle numbers.) To the extent that adjustment for apoB can allow for the effects of the LDL-related particles on risk and on the HDL system, the independent relevance of the HDL system is best assessed by its relationship with risk given apoB. This was stronger for low apoA1 than for low HDL-C. These associations of risk with low levels of HDL-related factors presumably reflect a real protective effect of some type(s) of HDL particle, since the HDL system is, among other things, responsible for reverse cholesterol transport. The difference between apoA1 and HDL-C in the strengths of their independent associations with risk (given apoB) suggests that some types of HDL particle may be more protective than others. Unfortunately, however, uncertainty in the extrapolation of post-infarction HDL-C (and triglyceride) values in cases back to their pre-infarction values precluded further pursuit of this. Nonetheless, the strong correlation of apoA1 with low risk provides evidence of a real protective effect of at least some type(s) of small HDL particle.
Causal relevance of triglyceride-rich precursors
Triglyceride-rich precursors of LDL particles are important determinants of the plasma levels of particular types of LDL particle and (as they can remove cholesterol from some HDL particles) of particular types of HDL particle. Our statistical analyses sought to elucidate the effects of LDL and HDL particles on disease, so it was not appropriate to adjust for triglyceride levels, even if these do correlate with some aspects of the HDL and LDL system of particles. (Moreover, triglyceride levels change after the onset of MI, distorting case–control comparisons of them.)
Risk prediction from a single blood sample
Given the usual values of apoB and apoA1, the usual values of LDL-C and HDL-C appeared to be informatively related to risk. Given the measured values of apoB and apoA1, however, the measured values of LDL-C and HDL-C were only weakly related to risk, and for risk prediction from a single set of measurements on a single blood sample what matters is the relevance of the measured values.
In this study, the ratio apoB/apoA1 encapsulated almost all the information from measurements of these two lipoproteins and of both cholesterol fractions (Table 2, Supplementary material online, Table A8). It was substantially more informative than the ratio LDL-C/HDL-C, more than twice as informative as either LDL-C or non-HDL cholesterol (the main biochemical treatment criteria in various current guidelines28,29) and about five times as informative as total cholesterol.
Routine measurement of apoB, apoA1, and their ratio apoB/apoA1 is widely practicable, and the present results indicate that there is about seven-fold variation in the relative risk of MI between the top and bottom deciles of the measured values of this ratio in UK heart disease patients (Figure 1). Moreover, the apoB/apoA1 ratio is informative even in old age (70–79) and is highly reproducible, with a self-correlation coefficient of 0.81 in the present study between measurements on samples taken a few years apart (Table 2). Although the present study was restricted to the UK, the large INTERHEART case–control study30 demonstrated the global importance of a single measurement of this ratio, and reported it to be better than any cholesterol-based ratios. (We note, however, that time from onset of symptoms in cases was not corrected for in their HDL-C analyses.)
If total and HDL cholesterol are the only measurements available, then our study suggests that risk prediction would be better based on their ratio than on their difference, non-HDL cholesterol, which was substantially less predictive of risk. This was also found in a meta-analysis of prospective studies.21 In those studies (none with posted blood samples), a 1.33 lower usual value of total/HDL cholesterol was associated with relative risks of 0.56 and 0.60, respectively, for ischaemic heart disease mortality at ages 40–59 and 60–69 years. In the present study of non-fatal MI (at a median age of 60 years), the corresponding relative risk was 0.58, in close agreement.
Case–control designs have inherent limitations, but our analyses are unaffected by any uncertainties of calibration and have incorporated appropriate adjustments for the main potential biases, and for the regression dilution bias. In addition, a range of sensitivity analyses (Supplementary material online, Table A9) have confirmed that alternative adjustments make little difference. Furthermore, the ratio apoB/apoA1 should be little affected by methodological problems. The conclusion that single measurements of apoB and apoA1 are more predictive than single measurements of LDL-C and HDL-C is consistent with a recent review,7 and is what would be expected if, given the usual apoB and apoA1, the usual LDL-C is negatively related to risk.
Potential value of further measures
A technique that directly counts particular subtypes of lipoprotein particles may well be much more informative about risk than just apoB and apoA1 (which effectively ignore differences between subtypes of LDL and of HDL particles). Nuclear magnetic resonance or gradient gel electrophoresis could help provide this, based on differences in particle size or structure,4 although there may be complex inter-relationships between the errors with which different subtypes are measured. Such approaches may help identify more relevant targets for intervention than simply lowering LDL cholesterol or raising HDL cholesterol.
Conclusion
The strongly positive association of the ratio apoB/apoA1 with the relative risk of MI in this study, which remains steep even at the lowest end of the normal range in the UK, should be qualitatively generalizable to other populations without prior vascular disease or medication. In patients with prior disease, or taking statins or other drugs that affect apolipoprotein values and/or recurrence risks, however, the apparent associations may well be distorted, and the widespread use of lipid-altering drugs means that studies nowadays might not be as directly informative. The other main qualitative conclusions should also be generalizable: different types of LDL particle differ, perhaps substantially, in their adverse effects; the evidence of a protective effect is definite for at least some subtypes of HDL particles; the total numbers of LDL particles (or, perhaps better, of small LDL particles) and of HDL particles (or, perhaps better, of particular subtypes of HDL particles) may well be more informative about risk than the total amounts of cholesterol being carried by those particles; measurements of apoB and apoA1 are more informative about risk than measurements of LDL-C and HDL-C; and, at given levels of apoB and apoA1, HDL-C should not be considered to be an independent protective factor. More detailed information about the numbers of particular subtypes of LDL particle and of HDL particle, especially in large prospective studies, could well be even more informative both for risk prediction and, more importantly, for understanding the mechanisms that underlie that risk.
Supplementary material
Supplementary material is available at European Heart Journal online.
[Supplementary Data]
Funding
Direct support from the UK Medical Research Council (MRC), British Heart Foundation (BHF), and Cancer Research UK to the Clinical Trial Service Unit and Epidemiological Studies Unit (CTSU) in the Nuffield Department of Clinical Medicine, University of Oxford, by a grant from the UK Department of Health Tobacco Products Research Trust, and by a grant from the Wolfson Foundation to the CTSU laboratories. Funding to pay the Open Access publication charges for this article was provided by the UK Medical Research Council.
Conflict of interest: S.P., R.P., and R.C. declare that no authors have any relevant conflict of interest. The CTSU has a policy of staff not accepting fees, but is involved in clinical trials of cholesterol modification therapy with funding from the MRC, BHF, and/or various companies (Merck, AstraZeneca, Schering, Pfizer, Solvay) as research grants to (and administered by) Oxford University. P.S. has received honoraria for participating in meetings.
Acknowledgements
The chief acknowledgement is to patients and relatives, and medical and nursing staff from the UK hospitals in the ISIS-3 study.9 Jill Barton and Kathy Jayne co-ordinated the case–control study. Sample storage, retrieval, and assay was co-ordinated by S.C., Karen Kourellias, Martin Radley, and L.Y. (and involved help from many people).
References
- 1.Fielding PE, Fielding CJ. Dynamics of lipoprotein transport in the human circulatory system. In: Vance DE, Vance JE, editors. Biochemistry of Lipids, Lipoproteins and Membranes. 4th ed. Amsterdam: Elsevier; 2002. pp. 527–552. [Google Scholar]
- 2.Chapman MJ, Laplaud PM, Luc G, Forgez P, Bruckert E, Goulinet S, Lagrange D. Further resolution of the low density lipoprotein spectrum in normal human plasma: physicochemical characteristics of discrete subspecies separated by density gradient ultracentrifugation. J Lipid Res. 1988;29:442–458. [PubMed] [Google Scholar]
- 3.Sacks FM, Campos H. Clinical review 163: Cardiovascular endocrinology: Low-density lipoprotein size and cardiovascular disease: a reappraisal. J Clin Endocrinol Metab. 2003;88:4525–4532. doi: 10.1210/jc.2003-030636. [DOI] [PubMed] [Google Scholar]
- 4.Carmena R, Duriez P, Fruchart JC. Atherogenic lipoprotein particles in atherosclerosis. Circulation. 2004;109:1112–1117. doi: 10.1161/01.CIR.0000131511.50734.44. [DOI] [PubMed] [Google Scholar]
- 5.Lada AT, Rudel LL. Associations of low density lipoprotein particle composition with atherogenicity. Curr Opin Lipidol. 2004;15:19–24. doi: 10.1097/00041433-200402000-00005. [DOI] [PubMed] [Google Scholar]
- 6.Barter PJ. Hugh Sinclair lecture: the regulation and remodelling of HDL by plasma factors. Atheroscler Suppl. 2002;3:39–47. doi: 10.1016/s1567-5688(02)00041-7. [DOI] [PubMed] [Google Scholar]
- 7.Walldius G, Jungner I. The apoB/apoA-I ratio: a strong, new risk factor for cardiovascular disease and a target for lipid-lowering therapy–a review of the evidence. J Intern Med. 2006;259:493–519. doi: 10.1111/j.1365-2796.2006.01643.x. [DOI] [PubMed] [Google Scholar]
- 8.Barter PJ, Ballantyne CM, Carmena R, Castro Cabezas M, Chapman MJ, Couture P, de Graaf J, Durrington PN, Faergeman O, Frohlich J, Furberg CD, Gagne C, Haffner SM, Humphries SE, Jungner I, Krauss RM, Kwiterovich P, Marcovina S, Packard CJ, Pearson TA, Reddy KS, Rosenson R, Sarrafzadegan N, Sniderman AD, Stalenhoef AF, Stein E, Talmud PJ, Tonkin AM, Walldius G, Williams KM. ApoB versus cholesterol in estimating cardiovascular risk and in guiding therapy: report of the thirty-person/ten-country panel. J Intern Med. 2006;259:247–258. doi: 10.1111/j.1365-2796.2006.01616.x. [DOI] [PubMed] [Google Scholar]
- 9.Parish S, Collins R, Peto R, Youngman L, Barton J, Jayne K, Clarke R, Appleby P, Lyon V, Cederholm-Williams S, Marshall J, Sleight P for the International Studies of Infarct Survival (ISIS) Collaborators. Cigarette smoking, tar yields, and non-fatal myocardial infarction: 14,000 cases and 32,000 controls in the United Kingdom. BMJ. 1995;311:471–477. doi: 10.1136/bmj.311.7003.471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.ISIS-3 (Third International Study of Infarct Survival) Collaborative Group. ISIS-3: a randomised comparison of streptokinase vs tissue plasminogen activator vs anistreplase and of aspirin plus heparin vs aspirin alone among 41,299 cases of suspected acute myocardial infarction. Lancet. 1992;339:753–770. [PubMed] [Google Scholar]
- 11.Clark S, Youngman LD, Palmer A, Parish S, Peto R, Collins R. Stability of plasma analytes after delayed separation of whole blood: implications for epidemiological studies. Int J Epidemiol. 2003;32:125–130. doi: 10.1093/ije/dyg023. [DOI] [PubMed] [Google Scholar]
- 12.Marcovina SM, Albers JJ, Henderson LO, Hannon WH. International Federation of Clinical Chemistry standardization project for measurements of apolipoproteins A-I and B. III. Comparability of apolipoprotein A-I values by use of international reference material. Clin Chem. 1993;39:773–781. [PubMed] [Google Scholar]
- 13.Marcovina SM, Albers JJ, Kennedy H, Mei JV, Henderson LO, Hannon WH. International Federation of Clinical Chemistry standardization project for measurements of apolipoproteins A-I and B. IV. Comparability of apolipoprotein B values by use of International Reference Material. Clin Chem. 1994;40:586–592. [PubMed] [Google Scholar]
- 14.Bachorik PS, Lovejoy KL, Carroll MD, Johnson CL. Apolipoprotein B and AI distributions in the United States, 1988–1991: results of the National Health and Nutrition Examination Survey III (NHANES III) Clin Chem. 1997;43:2364–2378. [PubMed] [Google Scholar]
- 15.Carroll MD, Lacher DA, Sorlie PD, Cleeman JI, Gordon DJ, Wolz M, Grundy SM, Johnson CL. Trends in serum lipids and lipoproteins of adults, 1960–2002. JAMA. 2005;294:1773–1781. doi: 10.1001/jama.294.14.1773. [DOI] [PubMed] [Google Scholar]
- 16.SAS version 8.2. SAS, Cary, NC, USA: [Google Scholar]
- 17.Pearce N. What does the odds ratio estimate in a case-control study? Int J Epidemiol. 1993;22:1189–1192. doi: 10.1093/ije/22.6.1189. [DOI] [PubMed] [Google Scholar]
- 18.Plummer M. Improved estimates of floating absolute risk. Stat Med. 2004;23:93–104. doi: 10.1002/sim.1485. [DOI] [PubMed] [Google Scholar]
- 19.Clarke R, Shipley M, Lewington S, Youngman L, Collins R, Marmot M, Peto R. Underestimation of risk associations due to regression dilution in long-term follow-up of prospective studies. Am J Epidemiol. 1999;150:341–353. doi: 10.1093/oxfordjournals.aje.a010013. [DOI] [PubMed] [Google Scholar]
- 20.Law MR, Wald NJ, Thompson SG. By how much and how quickly does reduction in serum cholesterol concentration lower risk of ischaemic heart disease? BMJ. 1994;308:367–372. doi: 10.1136/bmj.308.6925.367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Prospective Studies Collaboration. Blood cholesterol and vascular mortality by age, sex, and blood pressure: a meta-analysis of individual data from 61 prospective studies with 55 000 vascular deaths. Lancet. 2007;370:1829–1839. doi: 10.1016/S0140-6736(07)61778-4. [DOI] [PubMed] [Google Scholar]
- 22.Clarke R, Emberson JR, Parish S, Palmer A, Shipley M, Linksted P, Sherliker P, Clark S, Armitage J, Fletcher A, Collins R. Cholesterol fractions and apolipoproteins as risk factors for heart disease mortality in older men. Arch Intern Med. 2007;167:1373–1378. doi: 10.1001/archinte.167.13.1373. [DOI] [PubMed] [Google Scholar]
- 23.Prospective Studies Collaboration. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903–1913. doi: 10.1016/s0140-6736(02)11911-8. [DOI] [PubMed] [Google Scholar]
- 24.Heart Protection Study Collaborative Group. MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20,536 high-risk individuals: a randomised placebo-controlled trial. Lancet. 2002;360:7–22. [Google Scholar]
- 25.Rosner B, Spiegelman D, Willett WC. Correction of logistic regression relative risk estimates and confidence intervals for random within-person measurement error. Am J Epidemiol. 1992;136:1400–1413. doi: 10.1093/oxfordjournals.aje.a116453. [DOI] [PubMed] [Google Scholar]
- 26.Cholesterol Treatment Trialists’ (CTT) Collaborators. Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet. 2005;366:1267–1278. doi: 10.1016/S0140-6736(05)67394-1. [DOI] [PubMed] [Google Scholar]
- 27.Austin MA, Rodriguez BL, McKnight B, McNeely MJ, Edwards KL, Curb JD, Sharp DS. Low-density lipoprotein particle size, triglycerides, and high-density lipoprotein cholesterol as risk factors for coronary heart disease in older Japanese-American men. Am J Cardiol. 2000;86:412–416. doi: 10.1016/s0002-9149(00)00956-5. [DOI] [PubMed] [Google Scholar]
- 28.JBS 2. Joint British Societies’ guidelines on prevention of cardiovascular disease in clinical practice. Heart. 2005;91(Suppl. 5):v1–v52. doi: 10.1136/hrt.2005.079988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Grundy SM, Cleeman JI, Merz CN, Brewer HB, Jr, Clark LT, Hunninghake DB, Pasternak RC, Smith SC, Jr, Stone NJ. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III Guidelines. J Am Coll Cardiol. 2004;44:720–732. doi: 10.1016/j.jacc.2004.07.001. [DOI] [PubMed] [Google Scholar]
- 30.McQueen MJ, Hawken S, Wang X, Ounpuu S, Sniderman A, Probstfield J, Steyn K, Sanderson JE, Hasani M, Volkova E, Kazmi K, Yusuf S. Lipids, lipoproteins, and apolipoproteins as risk markers of myocardial infarction in 52 countries (the INTERHEART study): a case-control study. Lancet. 2008;372:224–233. doi: 10.1016/S0140-6736(08)61076-4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
[Supplementary Data]