Brown-Vialetto-Van Laere Syndrome, a Ponto-Bulbar Palsy with Deafness, Is Caused by Mutations in C20orf54 (original) (raw)
Abstract
Brown-Vialetto-Van Laere syndrome is a rare neurological disorder with a variable age at onset and clinical course. The key features are progressive ponto-bulbar palsy and bilateral sensorineural deafness. A complex neurological phenotype with a mixed picture of upper and lower motor neuron involvement reminiscent of amyotrophic lateral sclerosis evolves with disease progression. We identified a candidate gene, C20orf54, by studying a consanguineous family with multiple affected individuals and subsequently demonstrated that mutations in this gene were the cause of disease in other, unrelated families.
Main Text
Brown-Vialetto-Van Laere syndrome (BVVLS [MIM 211530]) was first reported by Brown in 18941 as familial amyotrophic lateral sclerosis (ALS [MIM 105400]) with onset in infancy. Following the reports by Vialetto, in 1936,2 and Van Laere, in 1966,3 the name BVVLS was adopted. The observation of recurrences in siblings in some families suggested that the condition was probably autosomal recessive. However, the variable age at onset and clinical course raised the possibility that it may be etiologically heterogeneous and that some cases may be caused by a new dominant mutation.4
BVVLS is a rare disorder characterised by progressive ponto-bulbar palsy and bilateral sensorineural hearing loss. The disease presents with VII, IX, X, XI, and XII cranial nerve palsies, which develop over a relatively short period of time in a previously healthy individual. Sensorineural hearing loss may precede the neurological signs.1–5 The course is invariably progressive, but the rate of decline is variable within and between families. With disease evolution, long tract signs, lower motor neuron signs, cerebellar ataxia, and lower cranial nerve (III-VI) palsies develop, giving rise to a complex picture resembling amyotrophic lateral sclerosis.5,6,7,8 Diaphragmatic weakness and respiratory compromise are some of the most distressing features, leading to recurrent chest infections and respiratory failure, which are often the cause of patients' demise.5,6
Fifty-eight cases have been documented in the literature. Sathasivam provided a comprehensive review of the published reports, showing a female to male prevalence of 3:1, with an apparently more severe clinical course in males.5 The age at onset ranged from infancy to early in the third decade, with the majority presenting in the second decade. Hearing loss preceded the onset of neurological signs in most cases. The neurological picture, severity, and disease duration were variable.5
The early-onset cases tend to have a much more rapid course, lasting between 6 and 18 mo,6 but survival is prolonged with active management (personal observation). The early motor milestones are usually normal. On detailed questioning, a history of increased susceptibility to chest infections can be elicited in some cases (personal observation), and occasionally, the disease onset may follow an episode of viral infection.7 The age at onset and clinical presentation may vary within the same family.6 Also, childhood- and adult-onset disease have been observed in the same sibship (personal observation).
Appropriate informed consent was obtained from the patients and guardians of the participants in this study, in compliance with the UK National Research Ethics Service regulation on research in human subjects. The clinical details of the patients included in this report are presented in Table 1.
Table 1.
Clinical Features of Patients with BVVLS
| Case | Origin | Consanguinity | Pre-Morbid Status | Age at Onset | Sex | Initial Presentation | Deafness, Age at Diagnosis | Respiratory Compromise, Age | Associated Features | Disease Duration |
|---|---|---|---|---|---|---|---|---|---|---|
| Family 1 | ||||||||||
| Case 1 | Arabic | Yes | Recurrent chest infections since age 4 mo | 13 mo | M | Sub-acute encephalopathy | 13 mo | 17 mo | Hypotonia, cerebellar signs, brisk reflexes in the lower limbs, persistent ankle clonus, stridor, EMG: bulbar palsy, anterior horn involvement; phrenic nerve denervation, auditory neuropathy | Alive by age 2 yr; required respiratory support |
| Case 2 | Arabic | Yes | Not known | 6 mo | M | Hypotonia, bulbar palsy | Not known | 6 mo | Hypotonia, bulbar palsy, respiratory difficulties | Died, age 13 mo |
| Family 2 | ||||||||||
| Case 3 | European ancestry | No | Normal | 16 mo | F | Progressive bulbar palsy | 16 mo | Ventilated, over last few mo | Anterior horn neuropathy; Intact cognitive development | Died, age < 3yr |
| Family 3 | ||||||||||
| Case 4 | European/Asian | No | Normal | 9 mo | M | Breathing problems | Yes | 2 yr | Multiple cranial nerve involvement | Died, age 2 yr |
| Family 4 | ||||||||||
| Case 5 | Pakistani | Yes | Normal | 12 yr | F | VII nerve palsy, deafness | 12 yr | Stridor on exercise, age 28 yr | Progressive muscle weakness | Alive, age 36 yr |
| Case 6 | Pakistani | Yes | Normal | 12 yr | F | Deafness, Tongue wasting and fasciculations | 12 yr, cochlear implant, age 15 yr | Stridor on exercise, age 21 yr | Poor balance, proximal muscle group weakness | Alive, age 29 yr |
| Family 5 | ||||||||||
| Case 7 | Pakistani | Yes | Normal | 5 yr | F | Tongue fasciculations, facial palsy, | 7 yr, aided | 13 yr | Progressive muscle weakness and wasting, external ophthalmoplegia | Died, age 14 yr |
| Family 6 | ||||||||||
| Case 8 | European | No | Normal | 3 mo | F | Breathing difficulties, weakness | Yes | 3 mo | General weakness, flaccid | Died, age 11 mo |
| Family 7 | ||||||||||
| Case 9 | European | No | Normal | Second decade | M | Multiple peripheral neuropathy | Yes | No | Progressive weakness, muscle wasting and truncal ataxia | Alive, age 57 yr |
Initial work was undertaken on family 1. The proband (case 1) came from a multiply consanguineous family with several similarly affected children, who died in infancy, strongly suggesting involvement of an autosomal-recessive gene. We were able to identify a stored muscle biopsy sample from a deceased cousin (case 2), which enabled us to undertake this study. The pedigree could not be included for reasons of confidentiality.
Case 4 was born with complex congenital heart disease. He developed the condition at the age of 9 mo and died 18 mo later. He had a similarly affected sister whose DNA was not available for testing.
Cases 5 and 6 are two siblings of a consanguineous Pakistani couple, who presented in early childhood on the background of previously normal motor and cognitive development. Careful exploration of the previous medical history, however, raised the possibility of mild early respiratory difficulties upon exercise. They both have had a slow progressive course and are alive in their late twenties and thirties, respectively.
Case 7 is one of four siblings of a consanguineous Pakistani family, who were reported by Dipti et al. in 2005.6
Patient 9 developed the condition in his early twenties. He is now in his fifties and is still able to walk a short distance with a stick. He has significant muscle wasting, truncal ataxia, and progressive sensorineural deafness, but he does not have respiratory compromise. There is a similarly affected brother who has not been available for testing at this stage. Two sisters died in childhood and had a clinical picture consistent with BVVLS.
DNA from the proband and the affected relative was used for autozygosity mapping with the use of the Illumina Human CNV370 array. Only one region of shared homozygosity longer than 1 Mb was identified: a 2.25 Mb region on chromosome 20p13, containing 44 genes (172128–2459030).
Several genes from the candidate region were sequenced by Sanger dideoxy sequencing. We elected to first analyze NRSN2 (MIM 610666), TCF15 (MIM 601010), SNPH (MIM 604942), SD_CBP2_, and NSFL1C because of their high expression in the brain, followed by sequencing of the remaining exons within the target region. A homozygous 2 bp frameshift mutation was identified in exon 5 of C20orf54 (Table 2). The mutation was also homozygous in the affected cousin and was heterozygous in the proband's parents and healthy sibling. The mutation was predicted to cause a frameshift resulting in a mutant protein built of 504 amino acids, 35 residues longer than the wild-type protein (Figure S1, available online). A second change was also found in these two patients (c.1048T>A [p.L350M]). The change is not a known SNP but is unlikely to be pathogenic, because it is predicted to be tolerated by SIFT9 and L350 is not highly conserved, even among mammalian orthologs.
Table 2.
Mutations Found in Patients with BVVLS
| Case | Ethnic Origin | Consanguinity | Number of Affect Cases | Nucleotide Change | Amino Acid Change | Location |
|---|---|---|---|---|---|---|
| 1, 2 | Arabic | Y | 2 | c.1048T>Ac.1325_1326 delTG | p.L350Mp.L442RfsX35 | Exon 3Exon 5 |
| 3 | European ancestry | N | 1 | c.211G>T | p.E71X | Exon 2 |
| 4 | European/Asian | N | 1 | c.639C>G | p.Y213X | Exon 3 |
| 5, 6 | Pakistani | Y | 2 | c.394C>T | p.R132W | Exon 2 |
| 7 | Pakistani | Y | 1 | c.670T>C | p.F224L | Exon 3 |
| 8 | European | N | 1 | c.1371C>G | p.F457L | Exon 5 |
| 9 | European | N | 1 | c.106G>A, c.1237T>C | p.E36K, p.V413A | Exon 2, Exon 5 |
DNA from an additional seven patients (cases 3–9, Table 1) was sequenced for the entire C20orf54. Homozygous nonsense mutations were found in cases 3 and 4 (Table 2), whereas both siblings from family 4 (cases 5 and 6) and cases 7 and 8 harbored homozygous missense mutations (Table 2). Conservation of the residues involved in missense mutations across a range of species is shown in Figure 1. Evidently, these three residues are highly conserved (although R132 can also be Q). Residue R132 is predicted to occur in an intracellular loop, F224 is predicted to be part of transmembrane helix 6, and F457 is predicted to occur in the extracellular tail. All three are predicted to be deleterious by SIFT.
Figure 1.
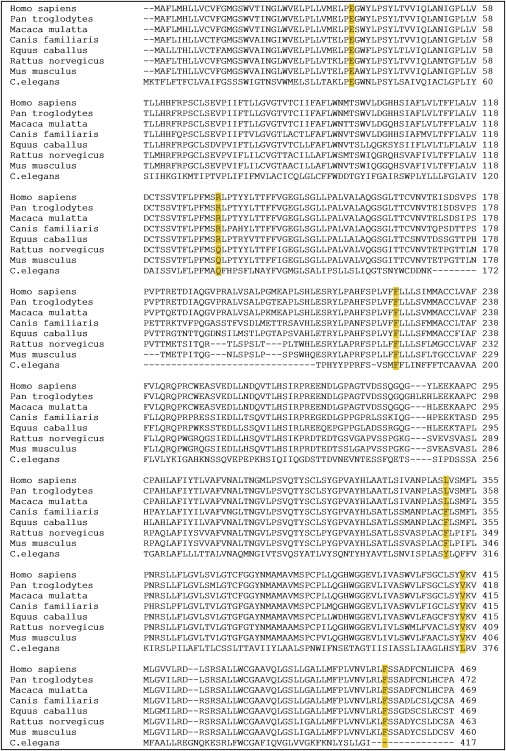
Multiple Alignment of C20orf54 Protein Sequence
The C20orf54 protein sequence with the six missense mutations (p.E36K, p.R132W, p.F224L, p.L350M, p.V413A, and p.F457L) is shown in eight orthologs. The mutations p.E36K and p.V413A are found in case 9 (Table 1), who is a compound heterozygote. The alignment was performed with ClustalW2, and the GenBank accession numbers are NP_212134.3, XP_001152229.1, XP_001112427.1, XP_542938.2, XP_001916183.1, NP_001032275.1, NP_081448.2, and NP_001033515.
Case 9 was found to carry two heterozygous missense mutations (Table 2). p.E36K is predicted to be deleterious by SIFT, whereas the other, p.V413A, is predicted to be tolerated. This would be in keeping with the somewhat milder phenotype in this patient.
With the exception of case 9 (compound heterozygote), all patients reported here were homozygous for their respective mutations. Cases 1, 2, 3, 5, 6, and 7 were also homozygous for all 18 polymorphisms covered by the sequenced regions, suggesting a common origin for each mutation (as expected for the consanguineous families 1, 4, and 5). However, cases 4 and 8 were heterozygous for one or more SNPs, indicating that the same mutation has occurred on more than one background (Table S1).
None of the mutations identified in our cohort was found in 210 control chromosomes, demonstrating that they are uncommon in the general population (allele frequency below 1%, 80% power10).
C20orf54 is a 5 exon gene located in 20p13 within our candidate region. It comprises 11 predicted transmembrane helices and is therefore likely to be a transmembrane protein. C20orf54 is highly conserved in evolutionary terms, sharing 59% identity with chicken and zebrafish and 36% with C. elegans (homologene).
Evidence of a possible function for this protein has recently come from a study by Yamamoto et al., who speculate that the rat ortholog (rRFT2) is a transporter of riboflavin in the small intestine.11 The human ortholog, C20orf54, shares 83% similarity with rRFT2; hence, they suggest renaming the gene RFT2.
Riboflavin deficiency has a clinical picture very different from that of BVVLS; therefore, the postulated function of the protein is unlikely to play a substantive role in disease mechanism. Riboflavin is essential for synthesis of Flavin Adenine Dinucleotide (FAD) and Flavin Mononucleotide (FMN). Both operate as cofactors for a number of biological processes involved in energy metabolism. Flavoproteins have been implicated as having signal transduction roles in apoptosis12 and DNA repair.13 Flavins contribute to oxidative stress through their ability to produce superoxide, as well as in the reduction of hydroperoxides by forming parts of multi-redox-center enzymes, such as the succinate and NADH dehydrogenases, xanthine oxidase/dehydrogenase, cytochrome P450 systems, and nitric oxide synthase.14 It is plausible that the protein has a maintenance function in the nervous system and that the disease is precipitated by exhaustion of a pathway tightly regulated by this protein.
The clinical similarity between BVVLS syndrome and ALS has long been recognized, suggesting that the two conditions may be part of the same spectrum. On the basis of the limited evidence that C20orf54 product is involved in the synthesis of molecules with pivotal role in cell energy metabolism, it is tempting to speculate that these conditions share a common pathway. It is conceivable that some cases of early-onset ALS, especially of the familial type, may be due to mutations in C20orf54, and it is worthwhile exploring this hypothesis by testing an appropriate cohort of patients. A locus on 20p13 designated as ALS7 (MIM 608037), which was identified by studying a large dominant family with multiple affected individuals,15 overlaps with C20orf54. However, the absence of any symptomatic carriers in our cohort makes it less likely that heterozygous mutations in this gene are associated with dominant ALS.
In conclusion, we have identified a gene that is highly conserved across the evolutionary time scale. The function of this gene in the nervous system is as yet unknown. We have demonstrated that recessive mutations give rise to BVVLS. The methodology used here to locate the causative gene confirms the power of autozygosity mapping together with targeted sequencing in identifying genes in rare recessive disorders for which consanguineous families are available.
Acknowledgments
The authors acknowledge the use of BRC Core Facilities provided by the financial support from the Department of Health via the National Institute for Health Research (NIHR) comprehensive Biomedical Research Centre award to Guy's & St Thomas' NHS Foundation Trust in partnership with King's College London and King's College Hospital NHS Foundation Trust. We also thank Evelina Charity for funding this research. The authors are extremely grateful to patients and families for the use of genetic samples and clinical information. The authors would like to thank Lucy Feng, Dubowitz Neuromuscular Centre, London, and Gladys Kramer and Alicia Chan, Medical Genetics, Edmonton, Canada, for providing specimens. They would also like to thank all of the clinicians for contributing samples not included in the current manuscript.
Supplemental Data
Document S1. Two Figures and One Table
Web Resources
The URLs for data presented herein are as follows:
- ClustalW2, http://www.ebi.ac.uk/Tools/clustalw2/index.html
- Homologene, http://www.ncbi.nlm.nih.gov/sites/entrez
- Online Mendelian Inheritance in Man (OMIM), http://www.ncbi.nlm.nih.gov/Omim/
- SIFT, http://sift.jcvi.org/
- TMHMM-2.0, http://www.cbs.dtu.dk/services/TMHMM-2.0/
- Translate, http://www.expasy.ch/tools/DNA.html
Accession Numbers
The GenBank accession numbers for the C20orf54 orthologous sequences reported in this paper are NP_212134.3, XP_001152229.1, XP_001112427.1, XP_542938.2, XP_001916183.1, NP_001032275.1, NP_081448.2, and NP_001033515.1.
References
- 1.Brown C.H. Infantile amyotrophic lateral sclerosis of the familial type. J. Nerv. Ment. Dis. 1894;19:707–716. [Google Scholar]
- 2.Vialetto E. Contributo all forma ereditaria della paralisi bulbare progressive. Riv. Sper. Fren. 1936;40:1–24. [Google Scholar]
- 3.Van Laere J. [Familial progressive chronic bulbo-pontine paralysis with deafness. A case of Klippel-Trenaunay syndrome in siblings of the same family. Diagnostic and genetic problems] Rev. Neurol. (Paris) 1966;115:289–295. [PubMed] [Google Scholar]
- 4.Hawkins S.A., Nevin N.C., Harding A.E. Pontobulbar palsy and neurosensory deafness (Brown-Vialetto-Van Laere syndrome) with possible autosomal dominant inheritance. J. Med. Genet. 1990;27:176–179. doi: 10.1136/jmg.27.3.176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sathasivam S. Brown-Vialetto-Van Laere syndrome. Orphanet J. Rare Dis. 2008;17:3–9. doi: 10.1186/1750-1172-3-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dipti S., Childs A., Livingston J.H., Aggarwal A.K., Miller M., Williams C., Crow Y. Brown-Vialetto Van Laere syndrome; variability in age at onset and disease progression highlighting the phenotypic overlap with Fazio-Londe disease. Brain Dev. 2005;6:443–446. doi: 10.1016/j.braindev.2004.10.003. [DOI] [PubMed] [Google Scholar]
- 7.Gallai V., Hockaday J.M., Hughes J.T., Lane D.J., Oppenheimer D.R., Rushworth G. Ponto-bulbar palsy with deafness (Brown-Vialetto-Van Laere syndrome) J. Neurol. Sci. 1981;50:259–275. doi: 10.1016/0022-510x(81)90172-6. [DOI] [PubMed] [Google Scholar]
- 8.Mégarbané A., Desguerres I., Rizkallah E., Delague V., Nabbout R., Barois A., Urtizberea A. Brown-Vialetto-Van Laere syndrome in a large inbred Lebanese family: confirmation of autosomal recessive inheritance? Am. J. Med. Genet. 2000;92:117–121. doi: 10.1002/(sici)1096-8628(20000515)92:2<117::aid-ajmg7>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- 9.Kumar P., Henikoff S., Ng P.C. Predicting the effects of coding non-synonymous variants on protein function using the SIFT algorithm. Nat. Protoc. 2009;4:1073–1081. doi: 10.1038/nprot.2009.86. [DOI] [PubMed] [Google Scholar]
- 10.Collins J.S., Schwartz C.E. Detecting polymorphisms and mutations in candidate genes. Am. J. Hum. Genet. 2002;71:1251–1252. doi: 10.1086/344344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yamamoto S., Inoue K., Ohta K.Y., Fukatsu R., Maeda J.Y., Yoshida Y., Yuasa H. Identification and functional characterization of rat riboflavin transporter 2. J. Biochem. 2009;145:437–443. doi: 10.1093/jb/mvn181. [DOI] [PubMed] [Google Scholar]
- 12.Susin S.A., Lorenzo H.K., Zamzami N., Marzo I., Snow B.E., Brothers G.M., Mangion J., Jacotot E., Costantini P., Loeffler M. Molecular characterization of mitochondrial apoptosis-inducing factor. Nature. 1999;397:441–446. doi: 10.1038/17135. [DOI] [PubMed] [Google Scholar]
- 13.Jorns M.S., Wang B., Jordan S.P. DNA repair catalyzed by Escherichia coli DNA photolyase containing only reduced flavin: elimination of the enzyme's second chromophore by reduction with sodium borohydride. Biochemistry. 1987;26:6810–6816. doi: 10.1021/bi00395a034. [DOI] [PubMed] [Google Scholar]
- 14.Massey V. The chemical and biological versatility of riboflavin. Biochem. Soc. Trans. 2000;28:283–296. [PubMed] [Google Scholar]
- 15.Sapp P.C., Hosler B.A., McKenna-Yasek D., Chin W., Gann A., Genise H., Gorenstein J., Huang M., Sailer W., Scheffler M. Identification of two novel loci for dominantly inherited familial amyotrophic lateral sclerosis. Am. J. Hum. Genet. 2003;73:397–403. doi: 10.1086/377158. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Document S1. Two Figures and One Table