A randomized clinical trial of home-based exercise combined with a slight caloric restriction on obesity prevention among women (original) (raw)
. Author manuscript; available in PMC: 2011 Sep 1.
Abstract
Objective
The study investigated the effectiveness of home-based exercise combined with a slight caloric restriction on weight change during 12 months in non obese women.
Methods
A randomized clinical trial with a factorial design was conducted from 2003 to 2005. Two hundred three middle-aged women (Rio de Janeiro/Brazil), 25–45 years, were randomly assigned to one of two groups: control (CG) and home-based exercise (HB). The HB group received a booklet on aerobic exercise that could be practiced at home (3 times/week - 40 min/session), in low-moderate intensity, during 12 months. Both groups received dietary counseling aimed at a slight energy restriction of 100–300 calories per day.
Results
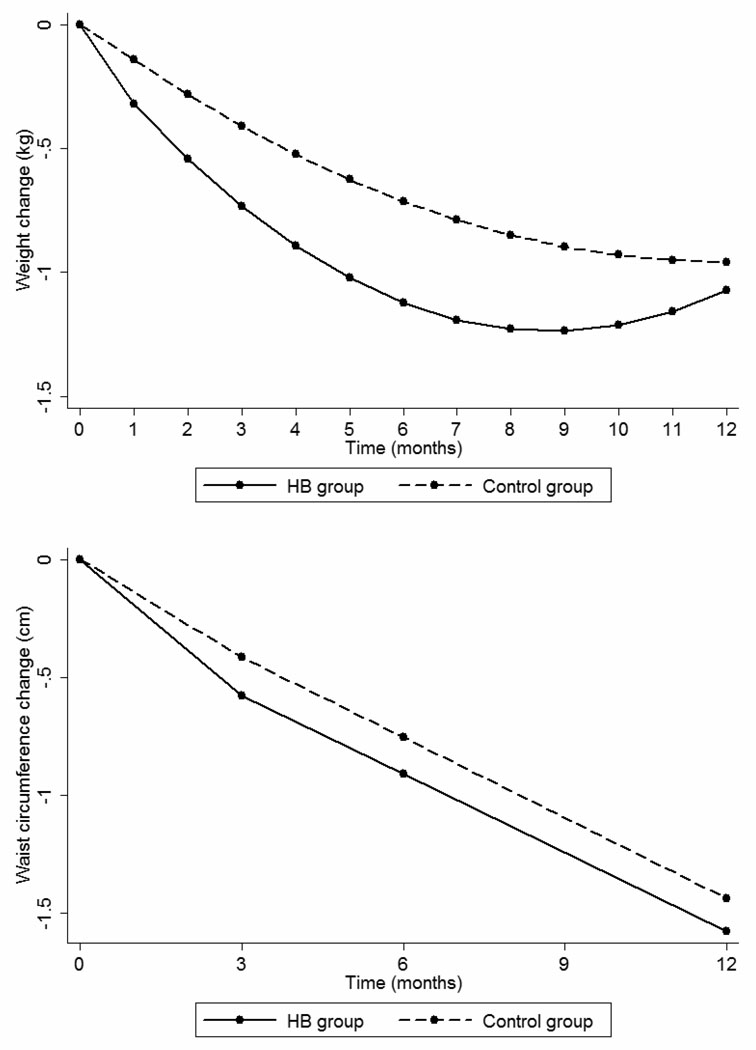
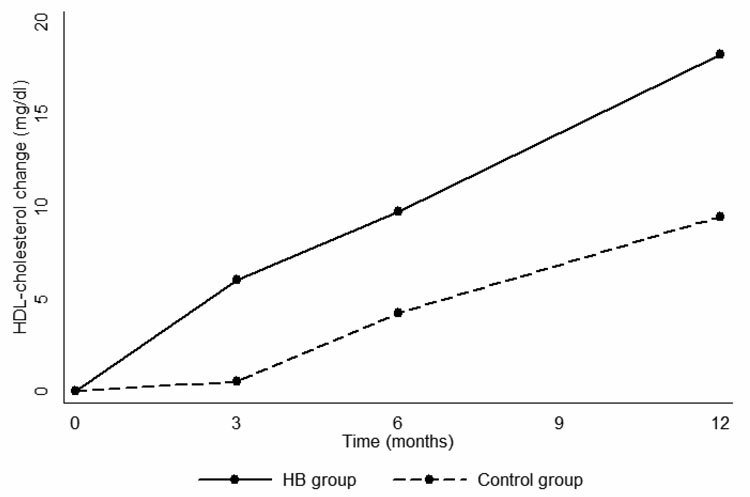
The HB experienced a greater weight loss in the first 6 months (−1.4 vs. −0.8 kg; p=0.04), but after 12 months there was no differences between groups (−1.1 vs. −1.0; p=0.20). Of the serum biochemical markers, HDL-cholesterol showed major change, with an increase at month 12 of 18.3 mg/dl in the HB compared to 9.5 in the CG (p<0.01).
Conclusion
Home-based exercise promoted greater weight reduction during the first six months after which no further benefits are observed. Continuous favorable changes in HDL-cholesterol after 1 year suggest that home-based exercise promote health benefits.
Introduction
Although small-changes approach has been suggested to be an effective way to curb the obesity epidemic, (Hill, 2009) others have questioned this approach (Swinburn, et al., 2009). Dietary restriction combined with physical activity (PA) may represent an effective strategy to promote weight loss and reduce fat mass (Jakicic and Otto, 2005; Mediano, et al., 2007). In a review article, Hansen et al. (2007) reinforced the role of PA on weight control, although many studies reported that the inclusion of PA in addition to a restriction in energy intake did not appear to facilitate weight loss (Christ, et al., 2004; Miller, et al., 1997). Despite these controversies, PA is considered to be a key part of the therapy for obesity, both for its effects on weight loss, and for the improvements it promotes in metabolic parameters such as insulin sensitivity and lipid profile (Bensimhon, et al., 2006; Votruba, et al., 2000).
Few studies have investigated the role of small amounts of exercise in preventing obesity (Kraus et al., 2001; Slentz et al., 2005). Since weight loss is difficult to maintain, weight gain prevention or prevention of obesity may be a useful strategy. In a 4-yr observational research in the Health Professionals Follow-up Study on predictors of weight change, Coakley et al. (1998) found that a decrease in 1.5 hours per week in physical activity predicted a gain of 0.6 kg, whereas an increase in activity over 1.5 hours per week predicted a weight loss of 0.9 kg. More recently, Williams et al. (2007) evaluated weight control practices and the resulting 2-yr weight changes among middle-aged women and found that only the combination of diet and exercise prevented mean weight gain. The mean weight gain of the cohort in that study was of 1.19 kg over the 2-yr period.
An important aspect of PA on prevention and treatment of obesity is the low adherence to formal programs, limiting the efficacy of these strategies (Rhodes et al., 2009). Many individual are unable to engage in a formal program due to difficulty with transportation, or not having adequate financial resources justifying the counseling of home-based exercise, but few studies compared this approach to traditional ones. Perri et al. (1997) compared the effectiveness of center- versus home-based exercise in a sample of sedentary, middle-aged obese women undergoing behavior weight loss treatment and found a better adherence to exercise in a home-based group after 12 months of follow-up. Krousel-Wood et al. (2008) found a BMI reduction in persons with diabetes, submitted to three months of home-based exercise intervention, with high adherence rates, about 80%. Therefore, home-based exercises could be an option that would improve PA adherence.
The purpose of this study was to investigate the effectiveness of home-based exercise combined with a slight caloric restriction on maintenance of small weight change in non obese women. Secondary outcomes were changes in waist circumference and biochemical markers. We hypothesized that addition of home-based exercise to a slight caloric restriction could facilitate weight loss.
Materials and methods
This randomized clinical study was primarily aimed at small weight loss comparing a low with a high glycemic index diet. Results did not indicate a difference between the low and high glycemic index diets on weight change. The full description and results of dietary intervention have been published elsewhere (Sichieri, et al., 2007). The trial had a factorial design, with half of the dietary intervention receiving also orientation for home-based exercise during 12 months, and the other half only dietary intervention. The study was conducted from October 2003 to March 2005.
In brief, 644women were screened and 230 were ineligible based on the following criteria: aged between 25 and 45 years with a body mass index (BMI) of 23–29.9 kg/m2, not pregnant, not breastfeeding, had at least one child and did not anticipate a pregnancy in the next year. Women with physician-diagnosed thyroid disease or diabetes or who were menopausal were not eligible to participate. Recruitment was conducted in two primary health care centers of the Rio de Janeiro State University, in Brazil. Randomization regarding a home-based exercise program and the progress of women during the study are shown in figure 1. All participants received information about the goals of the study, which aimed at a small weight loss during the follow-up. The study was approved by the Institutional Review Boards of Harvard School of Public Health and of Rio de Janeiro State University. A sample calculation made before the beginning of the study was based on a BMI difference of 1.2 kg/m2, with a standard deviation of 2.5 kg/m2, assuming 90% of power and a 5% significance level. The needed total sample size was 148 (Pocock, 1993). Allowing for non-compliance in both groups (Sato, 2000), the estimated sample size was 172, and with further accommodation for 20% of loss to follow-up, the total sample size was estimated to be 206.
Figure 1.
Progress of participants through the trial (Rio de Janeiro/Brazil, 2003–2005).
LGI - Low glycemic index; HGI - High glycemic index
Study design
Both groups received dietary counseling based on a slight energy restriction (100–300 kcal per day), with 26–28% of energy as fat (Sichieri, et al., 2007). Women were randomly assigned in a non blinded fashion to diet and to home-based exercise using sequentially numbered opaque sealed envelopes. The randomization list was computer-generated with blocking in advance and dieticians responsible for placing participants on study had no participation in the process of randomization. The intervention group received a booklet on physical exercise that could be practiced at home at least three times per week during 40 minutes per session (available at www.nebin.org). The exercise sessions were divided in three parts: 1) A warm-up routine consisting of gentle body movement and stretching exercises (5 minutes); 2) An aerobic cycle performed in a circuit with continuous movements involving large arm and leg muscles, as well as exercises using a ball, ropes, stair climbing, and standing up from a chair (balls and ropes were given to the participants) (30 minutes); and 3) a cool-down period, in which the same initial stretching exercises were performed (5 minutes). The participants were encouraged to engage in low to moderate exercise intensity with low impact, at least three times a week during 12 months. In the first week, women were advised to perform only a 20-minute session, increasing gradually (10 minutes/session/week) up to 40 minutes per session. Each session comprised activities with balls, ropes, stairs and chair. Additionally, all women were advised that they could reduce the exercising intensity if they felt any discomfort (e.g., if they were experiencing breathlessness or muscle aches). Compliance to the exercise program was assessed once a month during the nutritional counseling sessions. In the week prior to the counseling sessions, participants were asked to mark the days in which they exercised in a card printed with the days of the week, and then to bring the card with them to the appointment in order for us to ascertain whether they had performed the recommended exercises at three non-consecutive days.
Measurements
Weight was measured monthly, while circumferences, body composition, and fasting blood samples were collected at baseline and after 3, 6, and 12 months of follow-up. All measurements were performed in the morning, and blood was collected after the subjects had fasted for 10h. Height was measured to the nearest 0.5cm with a wall-mounted stadiometer, and body weight was measured by using the same calibrated digital scale for all participants. Circumference measures were taken at the largest girth of the hip and smallest girth of the waist. Body composition was assessed by means of a tetrapolar bioelectrical impedance analysis (BIA) using a RJL-101 and the software originally included in the analyzer. Electrodes were placed on the wrist and ankle, as specified by the manufacturer.
Plasma lipids and glucose were measured using GoldAnalisa kits with an intra-assay CV varying from 0.9% to 1.2%, and an inter-assay CV from 1.9% to 2.7%. The LDL and VLDL cholesterol concentrations were calculated according to the Friedewald equation (Friedewald, et al., 1972) based on the triacylglycerol measures. Serum insulin concentration was determined by radioimmunoassay using an ImmuChem™ 125/RIA kit with an intra-assay CV varying from 4.2% to 8.2%, and an inter-assay CV from 6.4% to 8.8%. Relative insulin resistance [Homeostasis model assessment of insulin resistance (HOMA-IR)] was estimated according to the formula [(glucose in mmol/L × insulin µU/ml)/22.5].
Data analysis
Baseline characteristics of the two groups were compared by using either the Student’s t-test or the chi-square test. We examined the temporal changes between groups for weight, circumferences, body composition, and blood lipids by performed repeated random regression (RRR) analysis using PROC MIXED in SAS (version 9.1; SAS Institute Inc, Cary, NC). The RRR is an intention-to-treat analysis because it includes all observations of each one of the subjects regardless of loss to follow-up or compliance. Analysis of weight and waist included BMI at baseline as a covariate, while for blood lipids, the baseline measures were included. Because of the nonlinear weight change observed, the model incorporated a quadratic term (time × time) variable. The term of interest was treatment × time interaction, which estimates the rate of changes in the outcomes. Residual plots of all models were examined and their distribution did not show major deviations from regression assumptions.
Changes between the groups for glucose, insulin and HOMA-IR, which were taken twice, were determined by Student’s t-test. Statistical significance was set at p<0.05 for all analyses.
Results
Baseline characteristics of the women randomly assigned to the two groups are shown in table 1. Most of the baseline characteristics showed no difference between the groups, but age showed a small difference and BMI and HDL cholesterol showed statistically significant difference (p<0.05). Losses to follow-up during the 1-yr period were 45% for CG and 42% for the HB group (figure 1). No differences between completers and drop-outs were found for any baseline characteristics (p>0.20). The number of women followed up at specific visits, as well as means changes from baseline for anthropometric variables, are show in table 2. The HB group had a greater weight loss in the first 6 months (−1.4 vs. −0.8 kg; p=0.04), but after 12 months of follow-up the weight change was not significantly different between groups (−1.1 vs. −1.0; p=0.20). The same pattern was found for BMI in the first 6 months, without significant differences thereafter. The HB group showed a reduction in waist circumference at the third month (−1.4 compared with −0.6 cm; p=0.05), and there were no significant differences between groups for waist-to-hip ratio and body composition at any time during the follow-up (table 2).
Table 1.
Baseline characteristics of participants (Rio de Janeiro/Brazil, 2003–2005).
| Variable | Control(n=101) | Intervention(n=102) | _p_-valuea |
|---|---|---|---|
| Age (years) | 38.1 (5.5) | 36.6 (5.4) | 0.06 |
| Body weight (kg) | 67.6 (7.5) | 68.6 (6.6) | 0.31 |
| Height (m) | 1.61 (0.06) | 1.60 (0.06) | 0.62 |
| Waist circumference (cm) | 81.1 (5.5) | 81.6 (5.2) | 0.50 |
| Hip circumference (cm) | 104.2 (6.0) | 104.1 (5.4) | 0.87 |
| Body mass index (kg/m2) | 26.2 (1.95) | 26.8 (1.8) | 0.03 |
| Waist-to-hip ratio | 0.78 (0.05) | 0.79 (0.06) | 0.44 |
| Total cholesterol (mg/dl) | 191.7 (35.3) | 191.3 (36.6) | 0.93 |
| HDL cholesterol (mg/dl) | 45.4 (17.5) | 40.9 (13.1) | 0.04 |
| LDL cholesterol (mg/dl) | 128.7 (34.1) | 132.2 (35.8) | 0.47 |
| VLDL cholesterol (mg/dl) | 17.7 (7.4) | 18.1 (10.5) | 0.72 |
| Triacylglycerol (mg/dl) | 88.3 (37.1) | 89.7 (52.0) | 0.83 |
| Glucose (mg/dl) | 84.6 (11.7) | 87.5 (17.2) | 0.17 |
| Insulin (µU/ml) | 11.3 (3.8) | 12.1 (4.8) | 0.24 |
| HOMA -IR | 2.37 (0.92) | 2.59 (1.11) | 0.15 |
| Race (%) | |||
| White | 57.4 | 46.9 | 0.23 |
| Mulato | 28.7 | 31.2 | |
| Black | 13.9 | 21.9 | |
| Schooling (%) | |||
| < 8 years | 28.0 | 22.3 | 0.64 |
| 8 – 12 years | 46.0 | 47.9 | |
| ≥ 12 years | 26.0 | 29.8 |
Table 2.
Crude means (standard deviation) and changes from baseline (Δ) for anthropometric characteristics and fat mass (%) during the follow-up by physical activity groups (Rio de Janeiro/Brazil, 2003–2005).
| 3 months(Control=56 Intervention=60) | 6 months(Control=48 Intervention=56) | 12 months(Control=55 Intervention=59) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean(sd) | Δa | pa | Mean(sd) | Δa | pa | Mean(sd) | Δa | pa | |
| Body Weight (kg) | |||||||||
| Control | 67.2 (8.7) | −0.5 | 66.6 (7.5) | −0.8 | 65.7 (7.1) | −1.0 | |||
| Intervention | 67.3 (5.9) | −0.9 | 0.08 | 67.6 (7.6) | −1.4 | 0.04 | 68.0 (6.6) | −1.1 | 0.20 |
| Body Mass Index (kg/m2) | |||||||||
| Control | 26.0 (2.1) | −0.2 | 25.9 (2.0) | −0.3 | 25.6 (2.0) | −0.4 | |||
| Intervention | 26.3 (2.1) | −0.4 | 0.06 | 26.2 (2.0) | −0.6 | 0.03 | 26.1 (2.1) | −0.4 | 0.21 |
| Waist Circumference (cm) | |||||||||
| Control | 81.1 (6.2) | −0.6 | 80.0 (5.4) | −1.0 | 78.7 (5.2) | −1.3 | |||
| Intervention | 80.7 (5.2) | −1.4 | 0.05 | 82.2 (5.4) | −1.1 | 0.94 | 80.7 (5.8) | −1.2 | 0.55 |
| Waist – to – hip ratio | |||||||||
| Control | 0.79 (0.05) | 0.001 | 0.78 (0.05) | 0.002 | 0.77(0.04) | 0.0004 | |||
| Intervention | 0.79 (0.05) | −0.005 | 0.09 | 0.80 (0.06) | −0.002 | 0.55 | 0.78(0.06) | −0.005 | 0.70 |
| Fat mass (%) | |||||||||
| Control | 31.3 (4.6) | − 0.4 | 29.9 (5.33) | − 1.9 | 29.9 (5.00) | − 2.9 | |||
| Intervention | 31.4 (5.1) | − 0.5 | 0.71 | 31.8 (4.83) | − 0.8 | 0.09 | 31.5 (5.74) | − 1.7 | 0.17 |
Of the serum biochemical markers analyzed (cholesterol, triglycerides, glucose, HOMA-IR), HDL-cholesterol showed major change during follow-up, with an increase of 18.3 mg/dl in the HB compared to 9.5 in the CG (p<0.01). Except for a reduction in LDL-cholesterol at month 6 in the HB (−15.6 vs. −4.0 mg/dl; p<0.01) in comparison to the CG, none of the other serum markers showed significant differences between groups (tables 3 and 4; p>0.20). The main changes during the 12 months of follow-up are shown in figure 2.
Table 3.
Crude means (standard deviation) and changes from baseline (Δ) for lipid profile during 3, 6 and 12 months of follow-up by physical activity groups (Rio de Janeiro/Brazil, 2003–2005).
| 3 months(Control=62 Intervention=68) | 6 months(Control=55 Intervention=63) | 12 months(Control=43 Intervention=36) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean(sd) | Δa | pa | Mean(sd) | Δa | pa | Mean(sd) | Δa | pa | |
| Total Cholesterol (mg/dl) | |||||||||
| Control | 193.7 (43.2) | 1.2 | 193.8 (34.7) | −2.0 | 188.2 (38.6) | −5.4 | |||
| Intervention | 195.2 (34.1) | 1.3 | 0.90 | 177.9 (36.3) | −4.8 | 0.24 | 199.5 (34.5) | 0.3 | 0.11 |
| HDL−cholesterol (mg/dl) | |||||||||
| Control | 45.7 (12.5) | −1.8 | 49.1 (10.2) | 3.4 | 54.7 (14.0) | 9.5 | |||
| Intervention | 46.1 (9.3) | 6.5 | 0.001 | 53.5 (13.9) | 12.5 | 0.0006 | 55.3 (15.4) | 18.3 | 0.01 |
| LDL−cholesterol (mg/dl) | |||||||||
| Control | 130.9 (42.2) | 3.3 | 128.6 (34.4) | −4.0 | 113.4 (36.2) | −15.9 | |||
| Intervention | 130.6 (33.5) | −4.2 | 0.08 | 110.6 (35.2) | −15.6 | 0.005 | 123.8 (34.7) | −18.5 | 0.79 |
| VLDL−cholesterol (mg/dl) | |||||||||
| Control | 17.0 (8.6) | −0.2 | 16.2 (7.1) | −1.1 | 20.1 (15.9) | 1.4 | |||
| Intervention | 18.5 (10.5) | −1.0 | 0.65 | 16.0 (8.0) | −0.4 | 0.59 | 20.6 (10.4) | 1.4 | 0.99 |
| Triacylglycerol (mg/dl) | |||||||||
| Control | 84.8 (43.0) | −1.4 | 78.5 (33.0) | −7.6 | 100.7 (79.3) | 6.1 | |||
| Intervention | 87.3 (50. 8) | −9.1 | 0.17 | 78.1 (39.3) | −4.3 | 0.45 | 99.9 (53.3) | 5.5 | 0.99 |
Table 4.
Serum fasting glucose, insulin and homeostasis model assessment of insulin resistance (HOMA-IR) by physical activity groups (Rio de Janeiro/Brazil, 2003–2005).
| Baseline | 3 months | Change from baseline | |||||
|---|---|---|---|---|---|---|---|
| Control(n=99) | Intervention(n=101) | Control(n=68) | Intervention(n=67) | Control(n=67) | Intervention(n=66) | pa | |
| Glucose (mg/dl) | 84.6 (11.7) | 87.5 (17.2) | 83.8 (9.7) | 84.4 (14.7) | −0.6 (14.7) | −5.5 (17.7) | 0.09 |
| Insulin (µU/ml) | 11.3 (3.8) | 12.1 (4.8) | 11.6 (3.5) | 12.2 (4.5) | −0.1 (4.6) | 0.4 (3.5) | 0.54 |
| HOMA-IR | 2.37 (0.92) | 2.59 (1.11) | 2.40 (0.89) | 2.53(1.08) | −0.04(1.21) | −0.05(0.88) | 0.93 |
Figure 2.
Estimated changes in weight, waist circumference and HDL-cholesterol based on repeated measurement analysis (Rio de Janeiro/Brazil, 2003–2005).
HB group – home-based exercise group
The compliances to the exercise protocol among those in follow-up were: 78.2%, 79.5% and 86.1% for months 3, 6 and 12, respectively, and the HB exercise arm had almost the same percentage of loss to follow-up compared to the non-exercise group.
Weight change at 12 months according to the number of sessions accomplished per week had an average of 0.4 kg (±1.8), 0.5 kg (±2.0), and 1.9 (±3.2) kg for women who exercised once, twice, and at least three times a week, respectively. The changes according to the number of sessions accomplished per week were not statistically significant and most women completed at least three sessions per week.
Discussion
The major finding of the present study was that a small volume of home-based exercise in addition to a slight caloric restriction promoted a higher reduction in body weight during the first six months in comparison with a caloric restriction only. However, this change was not sustainable during one year of follow up. In addition, the exercise program did correlate with a substantial increase in serum HDL cholesterol levels, even at 12 months, indicating continued compliance and resulting in important health benefits. Also, weight loss was greater among those with higher compliance.
The role of exercise on body weight maintenance is considered important (Foster, 2006; Jequier, 2002), but there is no recommendation based on well designed randomized controlled trial. Redman et al. (2007) compared the effects of a 25% energy deficit by diet alone or diet plus exercise in 35 overweight subjects during 6 months. The authors found no additional effects of physical exercise on body weight, fat mass, and fat-free mass in comparison with diet alone, and concluded that exercise plays a role equivalent to caloric restriction in terms of energy balance.
On the other hand, in a randomized controlled trial, McTierman et al.(2007) studied the effects of 300 minutes (high volume) of moderately vigorous exercise without dietary intervention on prevention of weight gain during 12 months of follow up. Women lost 1.4+1.8 kg compared to an increase of 0.7+0.9 kg in controls and men lost 1.8 +1.9 kg compared to an increase of 0.1+0.1 in controls. It is important to highlight that our study had a small caloric restriction in both groups allowing examining the effects of a smaller amount of exercise that could be recommended in clinical practice.
A meta-analysis by Curioni and Lourenço (2005) compared six randomized clinical trials (n = 265) with follow-up ranging from 10 to 52 weeks, and found a 20% greater weight loss in diet-plus-exercise groups, as well as a 20% greater sustained weight loss after 1 yr, when compared with the diet-only groups. Another recent meta-analysis (Shaw, et al., 2006) found a small yet significant decrease of 1kg in body weight in the diet-plus-exercise group when compared to the diet-only group. In addition, Bond Brill et al. (2002) studied the effects of walking in combination with a low-fat diet on weight loss and other health-related variables in 88 overweight women and, in accordance with our finding, a relatively small amount of exercise (30 min/d) during eight months of follow-up reversed the weight gain experienced in the control group.
The effects of different amounts of exercise training on body weight was evaluated by Slentz et al. (2004) in 120 overweight dyslipidemic subjects during eight months, with no changes in diet. They found that a modest amount of exercise (30 min/d) during the follow-up was positively associated with weight maintenance and improved the adherence to exercise programs. Poor adherence to a given exercise protocol may be one of the main reasons why randomized controlled trials often fail to find an association between physical activity and weight loss, especially in obese individuals. The prescribed amount of exercise may have paramount importance on exercise adherence, with more demanding exercise programs associated with poorer adherence (Fogelholm and Kukkonen-Harjula, 2000). The compliance to the exercise protocol in the present study was high at all times, and the HB exercise arm had almost the same percentage of loss to follow-up compared to the non-exercise group.
As reported in many other studies, maintenance of the weight loss after 6 months is difficult to sustain, and a substantial proportion of the patients will eventually revert to their original body weight (Jeffery, et al., 2000; Wing and Hill, 2001). Although the results regarding the role of PA on prevention of weight regain are still considered controversial, its application has become a part of the strategies for weight maintenance following weight loss programs (Haskell, et al., 2007; Saris, et al., 2003; Wu, et al., 2009), and officially endorsed by the American College of Sports Medicine (Donnelly, et al., 2009). This institution states the need for a greater amount of physical activity, reaching 250 to 300 min per week of moderate-intensity PA, in order to help prevent weight regain. Our study suggest that a small volume of PA, about 120 min per week, may be a good start for increasing in PA and it also suggest that after 6 months this volume should be increased to maintain long-term weight losses.
We did not find any major differences between the groups for measures of central obesity, except at the third month, when the HB group showed a greater reduction in waist circumference. Mourier et al. (1997) studied 24 overweight and obese subjects and showed that, although the exercise group showed major reduction of abdominal fat as evaluated by magnetic resonance, no differences were found for waist circumference and waist-to-hip ratio in comparison with non-exercisers. Thus, more accurate methods to determine small changes in abdominal fat would be necessary. In addition, no differences between the groups were found for fat-mass percentage during the follow-up and bio-impedance is not also a golden measure of fatness (Dehghan and Merchant, 2008; Pateyjohns et al., 2006).
Numerous studies have documented that PA has favorable effects on metabolic parameters such as lipid profile and insulin sensitivity (Kraus, et al., 2002; Tuomilehto, et al., 2001; Warburton, et al., 2006). For the metabolic parameters analyzed in our study, the most striking difference between the groups was for HDL-cholesterol, with a two-fold elevation for the HB in comparison with controls after 1 year of follow-up. These results have been extensively described (Donnelly, et al., 2000; Durstine, et al., 2001; Leon and Sanchez, 2001) among obese and hypercholesterolemic subjects, and our findings confirmed this association for middle-aged non-obese and non-hypercholesterolemic women, an important finding since high HDL cholesterol is one of the few protective factors for cardiovascular disease (Alwaili, 2010; Singh et al., 2007).
Although many studies have shown beneficial effects of PA on insulin sensitivity, (Holloszy, 2005; Matthaei, et al., 2000; Tuomilehto, et al., 2001) others which evaluated the combined effects of PA and diet in comparison with diet-only showed no differences in the results (Larson-Meyer, et al., 2006; Weinstock, et al., 1998). Our results suggest no significant additional effects of PA on insulin sensitivity evaluated by HOMA-IR. However, most women evaluated in the present study were not insulin resistant at baseline, according to the Brazilian criteria for insulin resistance (Geloneze, et al., 2006), which may explain the lack of a difference between the groups.
Limitations of the present studies include: 1) We have not used a golden standard measure of PA but self reported diary shows good correlation with other methods such as accelerometers and double labeled water (Besson, et al., 2010; Meriwether, et al., 2006). In addition, we did not assess PA in control group during the intervention, but a lack of major changes for metabolic parameters in this group, mainly for HDL cholesterol, may confirm no changes in PA status; 2) adiposity was measured by BIA, which is a measurement with many limitations (Dehghan and Merchant, 2008); 3) subjects were only females and not obese, therefore we may not extrapolate the results to obese and males individuals. These measurements error appears to be non differential and would change findings towards the null hypothesis.
In conclusion, a home-based exercise program was feasible and promoted greater weight reduction in the first 6 months, after which no further weight reduction was observed. Favorable changes in HDL-cholesterol after 1 year suggest that home-based exercise is a good strategy to initiate and increase physical activity and promote health benefits. Whether modifying training modalities after 6 months would increase these clinical benefits could be an important topic for future research.
Supplementary Material
01
Acknowledgments
Research relating to this study was funded by grant R03 TW005773-03 from National Institutes of Health - NIH and Grant 500404/2003-8 from Brazilian National Research Council – CNPq
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest statement
The authors declare that there are no conflicts of interest.
References
- Alwaili K, Awan Z, Alshahrani A, Genest J. High-density lipoproteins and cardiovascular disease: 2010 update. Expert Rev Cardiovasc Ther. 2010;8:413–423. doi: 10.1586/erc.10.4. [DOI] [PubMed] [Google Scholar]
- Bensimhon DR, Kraus WE, Donahue MP. Obesity and physical activity: a review. Am Heart J. 2006;151:598–603. doi: 10.1016/j.ahj.2005.03.005. [DOI] [PubMed] [Google Scholar]
- Besson H, Brage S, Jakes RW, Ekelund U, Wareham NJ. Estimating physical activity energy expenditure, sedentary time, and physical activity intensity by self-report in adults. Am J Clin Nutr. 2010;91:106–114. doi: 10.3945/ajcn.2009.28432. [DOI] [PubMed] [Google Scholar]
- Bond Brill J, Perry AC, Parker L, Robinson A, Burnett K. Dose-response effect of walking exercise on weight loss. How much is enough? Int J Obes Relat Metab Disord. 2002;26:1484–1493. doi: 10.1038/sj.ijo.0802133. [DOI] [PubMed] [Google Scholar]
- Christ M, Iannello C, Iannello PG, Grimm W. Effects of a weight reduction program with and without aerobic exercise in the metabolic syndrome. Int J Cardiol. 2004;97:115–122. doi: 10.1016/j.ijcard.2004.01.034. [DOI] [PubMed] [Google Scholar]
- Coakley EH, Rimm EB, Colditz G, Kawachi I, Willett W. Predictors of weight change in men: results from the Health Professionals Follow-up Study. Int J Obes Relat Metab Disord. 1998;22:89–96. doi: 10.1038/sj.ijo.0800549. [DOI] [PubMed] [Google Scholar]
- Curioni CC, Lourenco PM. Long-term weight loss after diet and exercise: a systematic review. Int J Obes (Lond) 2005;29:1168–1174. doi: 10.1038/sj.ijo.0803015. [DOI] [PubMed] [Google Scholar]
- Dehghan M, Merchant AT. Is bioeletrical impedance accurate for use in large epidemiological studies? Nutr J. 2008;7:26. doi: 10.1186/1475-2891-7-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donnelly JE, Blair SN, Jakicic JM, Manore MM, Rankin JW, Smith BK. American College of Sports Medicine Position Stand. Appropriate physical activity intervention strategies for weight loss and prevention of weight regain for adults. Med Sci Sports Exerc. 2009;41:459–471. doi: 10.1249/MSS.0b013e3181949333. [DOI] [PubMed] [Google Scholar]
- Donnelly JE, Jacobsen DJ, Heelan KS, Seip R, Smith S. The effects of 18 months of intermittent vs. continuous exercise on aerobic capacity, body weight and composition, and metabolic fitness in previously sedentary, moderately obese females. Int J Obes Relat Metab Disord. 2000;24:566–572. doi: 10.1038/sj.ijo.0801198. [DOI] [PubMed] [Google Scholar]
- Durstine JL, Grandjean PW, Davis PG, Ferguson MA, Alderson NL, DuBose KD. Blood lipid and lipoprotein adaptations to exercise: a quantitative analysis. Sports Med. 2001;31:1033–1062. doi: 10.2165/00007256-200131150-00002. [DOI] [PubMed] [Google Scholar]
- Fogelholm M, Kukkonen-Harjula K. Does physical activity prevent weight gain--a systematic review. Obes Rev. 2000;1:95–111. doi: 10.1046/j.1467-789x.2000.00016.x. [DOI] [PubMed] [Google Scholar]
- Foster GD. Clinical implications for the treatment of obesity. Obesity (Silver Spring) 2006;14 Suppl 4:182S–185S. doi: 10.1038/oby.2006.303. [DOI] [PubMed] [Google Scholar]
- Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18:499–502. [PubMed] [Google Scholar]
- Geloneze B, Repetto EM, Geloneze SR, Tambascia MA, Ermetice MN. The threshold value for insulin resistance (HOMA-IR) in an admixtured population IR in the Brazilian Metabolic Syndrome Study. Diabetes Res Clin Pract. 2006;72:219–220. doi: 10.1016/j.diabres.2005.10.017. [DOI] [PubMed] [Google Scholar]
- Hansen D, Dendale P, Berger J, van Loon LJ, Meeusen R. The effects of exercise training on fat-mass loss in obese patients during energy intake restriction. Sports Med. 2007;37:31–46. doi: 10.2165/00007256-200737010-00003. [DOI] [PubMed] [Google Scholar]
- Haskell WL, Lee IM, Pate RR, Powell KE, Blair SN, Franklin BA, Macera CA, Heath GW, Thompson PD, Bauman A. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Circulation. 2007;116:1081–1093. doi: 10.1161/CIRCULATIONAHA.107.185649. [DOI] [PubMed] [Google Scholar]
- Hill JO. Can a small-changes approach help address the obesity epidemic? A report of the Joint Task Force of the American Society for Nutrition, Institute of Food Technologists, and International Food Information Council. Am J Clin Nutr. 2009;89:477–484. doi: 10.3945/ajcn.2008.26566. [DOI] [PubMed] [Google Scholar]
- Holloszy JO. Exercise-induced increase in muscle insulin sensitivity. J Appl Physiol. 2005;99:338–343. doi: 10.1152/japplphysiol.00123.2005. [DOI] [PubMed] [Google Scholar]
- Jakicic JM, Otto AD. Physical activity considerations for the treatment and prevention of obesity. Am J Clin Nutr. 2005;82:226S–229S. doi: 10.1093/ajcn/82.1.226S. [DOI] [PubMed] [Google Scholar]
- Jeffery RW, Drewnowski A, Epstein LH, Stunkard AJ, Wilson GT, Wing RR, Hill DR. Long-term maintenance of weight loss: current status. Health Psychol. 2000;19:5–16. doi: 10.1037/0278-6133.19.suppl1.5. [DOI] [PubMed] [Google Scholar]
- Jequier E. Pathways to obesity. Int J Obes Relat Metab Disord. 2002;26 Suppl 2:S12–S17. doi: 10.1038/sj.ijo.0802123. [DOI] [PubMed] [Google Scholar]
- Kraus WE, Houmard JA, Duscha BD, Knetzger KJ, Wharton MB, McCartney JS, Bales CW, Henes S, Samsa GP, Otvos JD, Kulkarni KR, Slentz CA. Effects of the amount and intensity of exercise on plasma lipoproteins. N Engl J Med. 2002;347:1483–1492. doi: 10.1056/NEJMoa020194. [DOI] [PubMed] [Google Scholar]
- Kraus WE, Torgan CE, Duscha BD, Norris J, Brown SA, Cobb FR, Bales CW, Annex BH, Samsa GP, Houmard JA, Slentz CA. Studies of a terget reduction intervention through defined exercise (STRRIDE) Med Sci Sports Exec. 2001;33:1774–1784. doi: 10.1097/00005768-200110000-00025. [DOI] [PubMed] [Google Scholar]
- Krousel-Wood MA, Berger L, Jiang X, Blonde L, Myers L, Webber L. Does home-based exercise improve body mass index in patients with type 2 diabetes? Results of feasibility trial. Diabetes Res Clin Pract. 2008;79:230–236. doi: 10.1016/j.diabres.2007.08.028. [DOI] [PubMed] [Google Scholar]
- Larson-Meyer DE, Heilbronn LK, Redman LM, Newcomer BR, Frisard MI, Anton S, Smith SR, Alfonso A, Ravussin E. Effect of calorie restriction with or without exercise on insulin sensitivity, beta-cell function, fat cell size, and ectopic lipid in overweight subjects. Diabetes Care. 2006;29:1337–1344. doi: 10.2337/dc05-2565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leon AS, Sanchez OA. Response of blood lipids to exercise training alone or combined with dietary intervention. Med Sci Sports Exerc. 2001;33:S502–S515. doi: 10.1097/00005768-200106001-00021. discussion S528-509. [DOI] [PubMed] [Google Scholar]
- Matthaei S, Stumvoll M, Kellerer M, Haring HU. Pathophysiology and pharmacological treatment of insulin resistance. Endocr Rev. 2000;21:585–618. doi: 10.1210/edrv.21.6.0413. [DOI] [PubMed] [Google Scholar]
- McTiernan A, Sorensen B, Irwin ML, Morgan A, Yasui Y, Rudolph RE, Surawicz C, Lampe JW, Lampe PD, Ayub K, Potter JD. Exercise effect on weight and body fat in men and women. Obesity (Silver Spring) 2007;15:1496–1512. doi: 10.1038/oby.2007.178. [DOI] [PubMed] [Google Scholar]
- Mediano MF, Barbosa JS, Sichieri R, Pereira RA. Effects of exercise on insulin sensitivity in obese women submitted to a weight loss program: a clinical trial. Arq Bras Endocrinol Metabol. 2007;51:993–999. doi: 10.1590/s0004-27302007000600015. [DOI] [PubMed] [Google Scholar]
- Meriwether RA, McMahon PM, Islam N, Steinmann WC. Physical activity assessment: validation of a clinical assessment tool. Am J Prev Med. 2006;31:484–491. doi: 10.1016/j.amepre.2006.08.021. [DOI] [PubMed] [Google Scholar]
- Miller WC, Koceja DM, Hamilton EJ. A meta-analysis of the past 25 years of weight loss research using diet, exercise or diet plus exercise intervention. Int J Obes Relat Metab Disord. 1997;21:941–947. doi: 10.1038/sj.ijo.0800499. [DOI] [PubMed] [Google Scholar]
- Mourier A, Gautier JF, De Kerviler E, Bigard AX, Villette JM, Garnier JP, Duvallet A, Guezennec CY, Cathelineau G. Mobilization of visceral adipose tissue related to the improvement in insulin sensitivity in response to physical training in NIDDM. Effects of branched-chain amino acid supplements. Diabetes Care. 1997;20:385–391. doi: 10.2337/diacare.20.3.385. [DOI] [PubMed] [Google Scholar]
- Pateyjohns IR, Brinkworth GD, Buckley JD, Noakes M, Clifton PM. Comparison of three bioeletrical impedance methods with DXA in overweight and obese men. Obesity. 2006;14:2064–2070. doi: 10.1038/oby.2006.241. [DOI] [PubMed] [Google Scholar]
- Perri MG, Martin AD, Leermakers EA, Sears SF, Notelovitz M. Effects of group- versus home-based exercise in the treatment of obesity. J Consult Clin Psychol. 1997;65:278–285. doi: 10.1037//0022-006x.65.2.278. [DOI] [PubMed] [Google Scholar]
- Pocock SJ. Clinical Trials: A practical approach. Brisbane: John Wiley & Sons; 1993. [Google Scholar]
- Redman LM, Heilbronn LK, Martin CK, Alfonso A, Smith SR, Ravussin E. Effect of calorie restriction with or without exercise on body composition and fat distribution. J Clin Endocrinol Metab. 2007;92:865–872. doi: 10.1210/jc.2006-2184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhodes RE, Warburton DER, Murray H. Characteristics of physical activity guidelines and their effect on adherence. A review of randomized trials. Sports Med. 2009;39:355–375. doi: 10.2165/00007256-200939050-00003. [DOI] [PubMed] [Google Scholar]
- Saris WH, Blair SN, van Baak MA, Eaton SB, Davies PS, Di Pietro L, Fogelholm M, Rissanen A, Schoeller D, Swinburn B, Tremblay A, Westerterp KR, Wyatt H. How much physical activity is enough to prevent unhealthy weight gain? Outcome of the IASO 1st Stock Conference and consensus statement. Obes Rev. 2003;4:101–114. doi: 10.1046/j.1467-789x.2003.00101.x. [DOI] [PubMed] [Google Scholar]
- Sato T. Sample size calculations with compliance information. Stat Med. 2000;19:2689–2697. doi: 10.1002/1097-0258(20001015)19:19<2689::aid-sim555>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- Shaw K, Gennat H, O'Rourke P, Del Mar C. Exercise for overweight or obesity. Cochrane Database Syst Rev. 2006 doi: 10.1002/14651858.CD003817.pub3. CD003817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sichieri R, Moura AS, Genelhu V, Hu F, Willett WC. An 18-mo randomized trial of a low-glycemic-index diet and weight change in Brazilian women. Am J Clin Nutr. 2007;86:707–713. doi: 10.1093/ajcn/86.3.707. [DOI] [PubMed] [Google Scholar]
- Singh IM, Shishehbor MH, Ansell BJ. High-Density Lipoprotein as a Therapeutic Target. J Am Med Assoc. 2007;298:786–798. doi: 10.1001/jama.298.7.786. [DOI] [PubMed] [Google Scholar]
- Slentz CA, Aiken LB, Bales CW, Johnson JL, Tanner CJ, Duscha BD, Kraus WE. Inactivity, exercise, and visceral fat. STRRIDE: a randomized, controlled study of exercise intensity and amount. J Appl Physiol. 2005;99:1613–1618. doi: 10.1152/japplphysiol.00124.2005. [DOI] [PubMed] [Google Scholar]
- Slentz CA, Duscha BD, Johnson JL, Ketchum K, Aiken LB, Samsa GP, Houmard JA, Bales CW, Kraus WE. Effects of the amount of exercise on body weight, body composition, and measures of central obesity: STRRIDE--a randomized controlled study. Arch Intern Med. 2004;164:31–39. doi: 10.1001/archinte.164.1.31. [DOI] [PubMed] [Google Scholar]
- Swinburn BA, Sacks G, Lo SK, Westerterp KR, Rush EC, Rosenbaum M, Luke A, Schoeller DA, DeLany JP, Butte NF, Ravussin E. Estimating the changes in energy flux that characterize the rise in obesity prevalence. Am J Clin Nutr. 2009;89:1723–1728. doi: 10.3945/ajcn.2008.27061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tuomilehto J, Lindstrom J, Eriksson JG, Valle TT, Hamalainen H, Ilanne-Parikka P, Keinanen-Kiukaanniemi S, Laakso M, Louheranta A, Rastas M, Salminen V, Uusitupa M. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med. 2001;344:1343–1350. doi: 10.1056/NEJM200105033441801. [DOI] [PubMed] [Google Scholar]
- Votruba SB, Horvitz MA, Schoeller DA. The role of exercise in the treatment of obesity. Nutrition. 2000;16:179–188. doi: 10.1016/s0899-9007(99)00264-6. [DOI] [PubMed] [Google Scholar]
- Warburton DE, Nicol CW, Bredin SS. Health benefits of physical activity: the evidence. CMAJ. 2006;174:801–809. doi: 10.1503/cmaj.051351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinstock RS, Dai H, Wadden TA. Diet and exercise in the treatment of obesity: effects of 3 interventions on insulin resistance. Arch Intern Med. 1998;158:2477–2483. doi: 10.1001/archinte.158.22.2477. [DOI] [PubMed] [Google Scholar]
- Williams L, Germov J, Young A. Preventing weight gain: a population cohort study of the nature and effectiveness of mid-age women's weight control practices. Int J Obes (Lond) 2007;31:978–986. doi: 10.1038/sj.ijo.0803550. [DOI] [PubMed] [Google Scholar]
- Wing RR, Hill JO. Successful weight loss maintenance. Annu Rev Nutr. 2001;21:323–341. doi: 10.1146/annurev.nutr.21.1.323. [DOI] [PubMed] [Google Scholar]
- Wu T, Gao X, Chen M, van Dam RM. Long-term effectiveness of diet-plus-exercise interventions vs. diet-only interventions for weight loss: a meta-analysis. Obes Rev. 2009;10:313–323. doi: 10.1111/j.1467-789X.2008.00547.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
01