Physical activity and low back pain: a systematic review of recent literature (original) (raw)
Abstract
The objective of the study is to systematically evaluate the available evidence on the association between physical activity (i.e. occupational load and non-occupational physical activities) and low back pain (LBP). A systematic approach was used to explore the literature between 1999 and 2009. Studies were selected for inclusion following a comprehensive search of Medline, Embase and CINAHL. The methodological quality of each study was assessed. Studies were considered to be of ‘high quality’ if they met the cut-off criterion of 60% of the maximum available quality score. Thirty-six cohort or case–control studies were retrieved. Heavy workload and the accumulation of loads or frequency of lifts were moderate to strong risk factors for LBP. Strong associations were found for flexed, rotated and the awkward positions of the lumbar spine. Inconsistent results were found for leisure time physical activities, sports and physical exercise. Studies focusing on daily habitual physical activities (e.g. domestic activities and commuting) in association with LBP are lacking. In conclusion, the occurrence of LBP is related to the nature and intensity of the physical activities undertaken. However, physical activities can be subdivided into separate types and intensities and the ultimate physical load is the sum of all these activities. This makes it difficult to designate one particular activity as the cause of LBP.
Keywords: Back pain, Case–control, Cohort, Aetiology, Human activities, Longitudinal study, Review, Risk
Introduction
Low back pain (LBP) continues to be one of the most common and challenging problems in primary care. A large variation in community prevalence rates is observed, but methodological differences amongst studies and lack of methodological rigour have made it difficult to draw conclusions [1]. Substantial costs are associated with LBP including lost productivity and income from work, the expense of medical, rehabilitation and surgical interventions and the costs of disabling pain and limited daily function. The economic cost of back pain to society in the Netherlands has been estimated to be 1.7% of the gross national product [2] and 0.9% (€337 million) of the total cost of health care [3].
Within the domain of low back pain, the dose–response gradients of physical activity are important research issues in controlling risks for low back pain. Studies focusing on the relation between back pain and physical activity (such as occupational, recreational and sports-related activities) have produced results that are compatible with a U-shaped model, addressing the detrimental effect of both sedentary behaviour and strenuous levels of physical activity [4–6]. Biomechanical loading seems to be the most important occupational factor predicting both recurrent low back pain and sick leave attributed to back disorders [7]. Exposure to manual materials handling activities is considered to be an important risk factor, consistently associated with work-related back disorders [8, 9]. People in such jobs are significantly more often on sick leave because of back pain [10].
Several reviews assessed aspects of physical load as possible risk factors for LBP [11–14]. A common problem is the accurate assessment of physical activity with regard to its intensity and frequency [11]. In 1999, Hoogendoorn et al. [15] systematically reviewed aspects of physical load during work and leisure time as risk factors for back pain. Heavy physical work, manual handling and bending and twisting were found to be risk factors for back pain. No evidence was found for standing or walking, sitting, sports and total leisure time physical activity. However, exposure to physical load is not limited to one specific back threatening activity, but encompasses a compilation of activities, such as flexion, rotation, lifting, carrying and pulling. The results from a cross-sectional investigation of the prevalence of risk factors for chronic diseases in a randomly selected sample of the Dutch population showed that the reduction in physical load can theoretically reduce the burden of low back pain by 13–18% [16].
This paper examines the evidence of physical activity, i.e. occupational load as well as non-occupational activities (leisure time activities, sports and physical exercise) as risk factors for back pain, considering type and intensity of activity and time spent on these activities. A systematic approach was used to explore the literature published during the period November 1999–2009.
Materials and methods
Selection
The available literature was identified using a computerised search of bibliographical databases, including PubMed, CINAHL and Embase during the period November 1999–2009. The following medical subject headings were used: back pain, low back pain, physical activity, human activity, motor activity, locomotion, activities of daily living, life style, sports, occupation, occupational incident, occupational diseases, workload, risk, attributable risk, precipitating factors, epidemiologic factors, cohort analysis, cohorts studies, longitudinal studies, prospective studies, follow-up studies, case–control studies and retrospective studies. To optimise the retrieval of clinically relevant qualitative studies, a methodological filter aimed upon aetiology was used within the sensitive search strategy [17].
The search was focused on samples/populations of adults (≥18) and manuscripts published in the English, German, French and Dutch languages. The abstracts of all citations were retrieved and examined. The computerised search was done by the first reviewer (HH) supported by librarian expertise from the University of Applied Sciences Utrecht. All identified citations were screened to identify relevant studies, first by title, secondly by abstract and thirdly by full text screening.
Studies were eligible if they met all of the following criteria:
- the design of the study had to be longitudinal (prospective or retrospective) with at least 3 months follow-up;
- the study had to concern a community-based population or working population, free of back pain (no work absence and/or medical consult) during the 3 months before baseline assessment;
- back pain complaints had to be characterised by signs and symptoms of non-specific back pain, self-reported or measured otherwise;
- the exposure was restricted to physical activities in daily living, occupational workload, activities in leisure time and sports;
- the outcome measure was low back pain, including such consequences of back pain as disability or restriction in participation or work absenteeism.
The references of all selected articles were screened for additional, potentially eligible citations.
Data extraction and analysis
We extracted the design of the study, population characteristics, number of participants (at baseline and follow-up), characteristics of the exposure and risk estimates including the adjustment for confounding variables.
Methodological quality assessment
The selected studies were scored by two reviewers (HH, MvR) independently, using a predefined set of criteria for the appraisal of cohort studies and case–control studies [18]. Non-applicable criteria, such as blinding procedures for exposure were deleted, resulting in seven items for the cohort analysis and five items for the case–control studies. The criteria concerned the description of the study population, the preclusion of selection bias, the description and measurement of exposure and outcome variable(s), the length of the follow-up assessment, a non-selective loss-to-follow-up analysis and the inclusion of confounding variables in the statistical analysis. Preceding the final screening, reviewers pilot tested the methodological quality assessment of two similar articles that were not included in this review.
All disagreements between the reviewers were subsequently discussed during a consensus meeting. If disagreements were not resolved during this meeting, a third reviewer (GA) was consulted for final judgment. Each study was assigned a total score, which was the sum of all positive ratings according to the methodological criteria. The reviewers considered studies to be of high quality if the methodological quality score was more than 60% of the maximum score. The findings of the studies were considered to be inconsistent if <75% of the available studies reported the same conclusion. This qualitative analysis was used to qualify the level of scientific evidence of explored exposures of physical activities as risk factors for back pain. This procedure led to the qualification of five levels of scientific evidence: (1) strong evidence provided by generally consistent findings in multiple high quality studies; (2) moderate evidence provided by one high quality study or by generally consistent findings in multiple low quality studies; (3) limited evidence in case of one low quality study; (4) conflicting evidence in case of inconsistent findings and (5) no evidence [19].
Analysis
Exposures were grouped into occupational physical load, i.e. manual handling and posture, and non-occupational physical activities, i.e. leisure time activities, sports and physical exercise. Risk estimates were retrieved from the original article together with the variables that were adjusted for the statistical analysis. Findings were expressed as relative risks (RRs), odds ratios (ORs), prevalence rate ratios (PRs) or hazard rate ratios (HRs) and their 95% confidence intervals. If provided, findings were retrieved from multivariate analyses.
The strength of evidence for causality of a risk factor can be evaluated by summarising the available evidence about the consistency of the association across studies and the strength of the association. An association (e.g. RR, OR) of ≥2.0 or ≤0.5 was considered to be indicative of a strong association, as previously described in the study by van der Windt et al. [20]. Non-significant associations were excluded from further analyses.
The interobserver agreement (e.g. Kappa) of the quality assessment was calculated by the Kappa statistic, considering values between 0.61 and 0.80 as substantial and values beyond 0.80 as almost perfect [21].
Results
Selection of studies
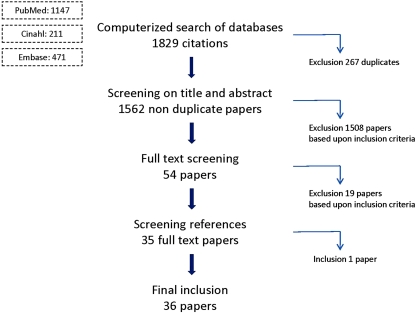
After the screening on titles and abstracts, 54 studies were considered eligible for full text screening. After this full text screening, 19 studies were excluded based on discordance with the inclusion criteria (Fig. 1). Two studies described the occupation without a precise description of the associated physical load exertions. Another two studies did not satisfy the topic of this review whilst three studies analysed the dose–response pattern between exposure to occupational whole body vibrations and LBP. We did not consider whole body vibration to be an expression of physical behaviour (which was the focus of our research) and therefore excluded it from this review. One study focused primarily on psychosocial factors and a total of 11 studies included persons with back pain <3 months before baseline or back pain at baseline. Finally, 36 publications fulfilled all selection criteria, including 30 cohort studies and six case–control studies.
Fig. 1.
Flow diagram of papers included and excluded by two reviewers during the selection procedure
Study characteristics
Twenty-five cohort studies [22–46] and five case–control studies [47–51] explored the exposure within a working population. One study [52] explored non-occupational physical activity whilst five studies [53–57] explored both occupational as well as non-occupational physical activities.
The statistical analysis of these studies was done in samples with sizes varying between n = 174 [45] and n = 3,615 [28] for cohort studies and n = 137 [5o] and n = 240 [48] for case–control studies. With respect to the population-based studies, the analysis was done on sample sizes varying between n = 237 [53] and n = 25,271 [30] for cohort studies and n = 333 [49] and n = 791 [51] for the case–control studies.
The shortest follow-up period was 3 months [25] and the longest 28 years [24]. The percentage loss to follow-up varied between 11 [53] and 43% [31] in studies with a follow-up of ≤1 year [25, 28, 29, 31, 37, 38, 42, 46, 52, 53, 55, 56], between 10 [54] and 60% [31] in studies with a follow-up >1 and ≤3 years [22, 23, 25, 28, 31, 34, 35, 39, 41, 49, 54, 55] and between 12 [45] and 28% [30, 44] in studies with a follow-up of more than 3 years. In studies with a follow-up of more than 15 years [24, 33, 43, 47] percentages loss to follow-up varied between 38 [47] and 84% [24].
Low back pain was defined in 22 studies [24–29, 31, 32, 34, 40, 42, 44, 47, 56, 57] by describing pain and/or pain drawing. Ten studies [25–27, 32, 34, 36, 37, 39, 42, 56] used the standardised Nordic Questionnaire (or an adaptation thereof) [58]. The occurrence of new episodes of LBP was measured by the use of questionnaires [22, 24, 25, 27, 28, 31–34, 36, 38, 39, 42, 49, 53–56], interviews [24, 41, 49] or reports by care providers [50–52, 57]. Sick leave was derived from questionnaires [25, 26, 28, 29, 33, 37, 38, 43, 45, 47], company registers [23, 26, 35, 40] and social insurance administrations [30, 40, 48].
Exposures varied between performances of manual handling (i.e. lifting, carrying, pushing and strenuous arm movements), posture (i.e. standing, awkward positions such as flexed-twisted-rotated), magnitudes of work and non-work-related physical loadings (light, moderate, heavy), sports and physical exercise. The measurement of the outcome (dependent) variable varied between the occurrence of new episodes of LBP [22–24, 27, 31, 32, 34, 36, 39, 41, 44, 46, 50, 52, 54, 57], sick leave due to LBP [23, 26, 29, 30, 35, 40, 43, 48] or a combination of both [25, 28, 33, 36, 38, 42, 44–46, 49, 51, 53, 55]. Twenty-eight studies applied (self-administered) questionnaires in the screening of exposures [22–24, 26–33, 36, 37, 39, 40, 42–45, 47–49, 52–57]. In 28% of the studies, authors gave information on the validation and/or reproducibility of the questionnaires [22, 28, 31, 32, 46, 47, 49, 53, 57]. Four studies used an interview [24, 41, 50, 51] and four studies [25, 34, 35, 38] used an observational method.
Associations have been most widely expressed by odds ratios or relative risks. Based on their design, three case–control studies [48, 51, 57] interpreted the odds ratio as an estimate of the incidence rate ratio [59, 60].
Methodological quality
Tables 1 and 2 include all studies in hierarchical and alphabetic order according to their methodological quality. Initially, both reviewers did not agree in 21 (9%) of the 240 cases and a criterion had to be applied, resulting in a substantial initial agreement (Kappa value 0.76; SE 0.58; p = 0.000). Most disagreement was due to differences in the interpretation of the exclusion of selection bias and selective loss-to-follow-up. All disagreements were resolved during one consensus meeting. The sum of all positive ratings ranged from 4 to 7 (maximum score) for the cohort studies. All case–control studies received the maximum score of 5. Based on the cut-off criteria for quality of 60% of the maximum score, 35 studies were considered to be high quality studies. One study [55] did not fulfil the 60% criterion.
Table 1.
Methodological quality assessment of cohort studies
| References | 1 | 2 | 3 | 4 | 5 | 6 | 7 | + | φ |
|---|---|---|---|---|---|---|---|---|---|
| Friedrich et al. [29] | + | + | + | + | + | + | + | 7 | |
| Jacob [53] | + | + | + | + | + | + | + | 7 | |
| Krause et al. [40] | + | + | + | + | + | + | + | 7 | |
| Miranda et al. [42] | + | + | + | + | + | + | + | 7 | |
| Muller et al. [43] | + | + | + | + | + | + | + | 7 | |
| Tubach et al. [44] | + | + | + | + | + | + | + | 7 | |
| Videman et al. [45] | + | + | + | + | + | + | + | 7 | |
| Yip [46] | + | + | + | + | + | + | + | 7 | |
| Andersen et al. [22] | + | – | + | + | + | + | + | 6 | |
| Bergstrom et al. [23] | + | – | + | + | + | + | + | 6 | |
| Bildt et al. [24] | + | – | + | + | + | + | + | 6 | |
| Burdorf et al. [25] | + | – | + | + | + | + | + | 6 | |
| Croft et al. [52] | + | + | + | + | + | – | + | 6 | |
| Elders et al. [27] | + | – | + | + | + | + | + | 6 | |
| Harkness et al. [31] | + | – | + | + | + | + | + | 6 | |
| Hartvigsen et al. [32] | + | + | + | + | + | + | + | 6 | |
| Hoogendoorn et al. [34] | + | + | + | + | + | – | + | 6 | |
| Hoozemans et al. [36] | + | – | + | + | + | + | + | 6 | |
| Latza et al. [41] | + | – | + | + | + | + | + | 6 | |
| Van Nieuwenhuyse et al. [56] | + | + | + | + | + | – | + | 6 | |
| IJzelenberg et al. [37] | + | – | + | + | + | + | + | 6 | |
| Elders et al. [26] | + | – | + | + | + | – | + | 5 | |
| Eriksen et al. [28] | + | – | + | + | + | – | + | 5 | |
| Hagen et al. [30] | + | + | φ | + | + | – | + | 5 | 1 |
| Hellsing et al. [33] | + | – | – | + | + | + | + | 5 | |
| Hoogendoorn et al. [35] | + | – | + | + | + | – | + | 5 | |
| Jansen et al. [38] | + | – | + | + | + | – | + | 5 | |
| Juul-Kristensen et al. [39] | + | – | + | + | + | – | + | 5 | |
| Kopec et al. [54] | + | – | + | + | + | – | + | 5 | |
| Nolting et al. [55] | + | φ | φ | + | + | φ | + | 4 | 3 |
Table 2.
Methodological quality assessment of case–referent studies
| References | 1 | 2 | 3 | 4 | 5 | + |
|---|---|---|---|---|---|---|
| Bildt Thorbjornsson et al. [47] | + | + | + | + | + | 5 |
| Engkvist [48] | + | + | + | + | + | 5 |
| Josephson et al. [49] | + | + | + | + | + | 5 |
| Kerr [50] | + | + | + | + | + | 5 |
| Mortimer et al. [51] | + | + | + | + | + | 5 |
| Vingard et al. [57] | + | + | + | + | + | 5 |
Data extraction and analysis
A summary of the included studies and the reproduction of their main findings are presented in Table 3.
Table 3.
Summary of the main characteristics, data extraction and analysis of studies on physical activity and low back pain
| References | Design | FU | Population | Outcome | Exposure | Exposure measurement | Univariate analysis | Multivariate analysis |
|---|---|---|---|---|---|---|---|---|
| Andersen et al. [22] | Pro | 24 months | General working population industrial companies and service sectorBaseline : n = 4,006FU: n = 3,276 | Severe LBP by questionnaire | Physical factors at work (i.e. manual handling, posture, repetitive movement, lifting, pulling, pushing) | Self-administered questionnaires | Cox proportional hazards analysis (HR 95% CI) adjusted 1,2,5Repetitive work: 0–9 min/h: 1.0; 45–60 min/h: 1.7 (1.2–2.6); lifting: never: 1.0; ≥100 kg/h: 1.9 (1.3–2.8); pushing: 1–354 kg/h: 1.9 (1.3–2.8); ≥355 kg/h: 1.7 (1.1–2.5); standing >30 min/h: no 1.0; yes 2.1 (1.3–3.3); squatting >5 min/h: no 1.0, yes 1.5 (1.0–2.1). | Adjusted 1,2,5.Lifting: never: 1.0; ≥100 kg/h: 1.5 (1.0–2.3); standing: no: 1.0; >30 min/h: 1.9 (1.2–3.0) |
| Bergstrom et al. [23] | Pro | 18 months and 3 years | AHA studyWork and Health in the Processing and Engineering IndustriesBaseline: n = 2,187FU I: n = 1,587FU II: n = 1,595 | Sick leave attributed to neck or back pain bycompanies registers | Physical factors at work (i.e. heavy lifting); physical activities in leisure time except exercise | Self-administered questionnaires | Logistic regression analysis (OR 95% CI) adjusted 1,2Variables with a p ≤ 0.10 were analysed by stepwise multiple logistic regressionsData not presented | Adjusted 1,2,5.18 months by variable set: heavy lifting: almost never: 1.0; >10 times/day: 2.03 (1.20–3.43)3 years by variable set: physical activities in leisure time: no activity: 1.0; <30 min/day: 0.44 (0.22–0.88); 1 h/day: 0.39 (0.20– 0.76). Final multivariate model: none of the variables concerning physical work environment (i.e. heavy lifting, vibration tools) were significantly related to sick leave attributed to neck or back pain |
| Bildt et al. [24] | Retro | 24 and 28 years | Population-based REBUS study (Sweden 1969)Baseline: n = 2,579FU I: n = 484FU II: n = 420 | LBP requiring medical consultation and treatment by interview and self-administered questionnaires | Physical work conditions (i.e. sedentary work, work with hands below knee level, bent and twisted body postures, lifting) | Self-administered questionnaire | Logistic regression analysis (OR 95% CI)Bivariate (LBP vs. healthy subjects) adjusted 1.Men (ILBP): sedentary work: 0.3 (0.1–0.5); lifting 5–15 kg: 4.0 (2.4–6.7)Men (CLBP): work with hands below knee level: 4.5 (2.2–9.0); lifting 5–15 kg: 3.7 (1.9–7.4). | Adjusted 1Men (ILBP): lifting 5–15 kg: 4.1 (2.1–8.1); men (CLBP): work with hands below knee level 4.7 (1.9–12.1) |
| Bildt Thorbjornsson et al. [47] | Case-Ref. | 24 years in 5-year periods | Population-based REBUS study (Sweden)Baseline: n = 783FU: n = 484 | LBP requiring medical consultation and treatment or sick leave by questionnaire | Occupational risk factors (i.e. bent or twisted body postures, lifting/carrying loads); non-occupational factors (i.e. physical exercise) | Self-administered questionnaire | Logistic regression analysis(OR 95% CI) adjusted 1Men: high perceived load outside work: 1.6 (1.0–2.7). | Adjusted 1.5 years before onset: women: heavy physical work 1.9 (1.1–3.6); men: high perceived load outside work 1.9 (1.1–3.3). 1 year before onset: women: heavy physical work 2.2 (1.2–4.0); sedentary work 1.7 (1.0–3.1); men: high perceived load outside work 1.7 (1.0–2.9). |
| Burdorf et al. [25] | Pro | 1–2 years | Workers from nursing homes (≥10 h week)Baseline: n = 796FU I: n = 523FU II: n = 341 | LBP and sickness absence due to LBP by (Nordic) questionnaire | Physical load (i.e. trunk flexion, lifting or carrying loads) | Observations | Logistic regression analysis (95% CI) adjusted 1,41 year. FU: sickness absence: physical load low 1.0; intermediate: 2.0 (1.04–3.85); high: 2.95 (1.52–5.71) | |
| Croft et al. [52] | Pro | 12 months | South Manchester Back Pain StudyBaseline: n = 2,715FU: n = 1,649 | New episodes of LBP by consultations primary care physician | Self-rated level of non-occupational (specific) PA | Self-administered questionnaires | Cox regression analysis (RR 95% CI) adjusted 1,5No clear or strong patterns of risk associated with specific markers of PA, besides men (regular ‘do-it-yourself’ activity: 1.8 (1.2–2.6) and women (regular sports: 1.3 (1.0–1.6) | |
| Elders et al. [26] | Pro | 1–2–3 years | Workers of a scaffolding companyBaseline: n = 288FU I: n = 209FU II: n = 182FU III: n = 144 | Absence ratio because of LBP by absence report to the health service of the company | Physical workload (i.e. lifting, carrying heavy loads, awkward positions, strenuous arm movements) | Self-administered questionnaire | Log-linear regression analysis (PR 95% CI)Sickness absence ≤14 days: high manual handling of materials: 2.26 (1.34–3.83); high awkward back posture: 1.78 (1.11–2.87); high strenuous arm movements: 3.43 (1.81–6.49). Sickness absence >14 days: high manual handling of materials: 1.88 (1.06–3.43) | Adjusted 1Sickness absence <14 days: high strenuous arm movements: 2.98 (1.57–5.66)Sickness absence >2 weeks: no significant outcome |
| Elders et al. [27] | Pro | 1–2–3 years | Workers of a scaffolding companyBaseline: n = 288FU I: n = 209FU II: n = 163FU III: n = 127 | Cumulative incidence and cumulative recurrence of LBP by questionnaire | Physical workload (i.e. lifting, carrying heavy loads, awkward positions, strenuous arm movements) | Self-administered questionnaire | Generalised estimating equations (OR 95% CI)Cumulative recurrence: high manual handling: 2.14 (1.17–3.89). | Adjusted 1,4,5Cumulative recurrence: high manual handling of materials: 2.02 (1.12–3.66). |
| Engkvist [48] | Case-Ref. | Nursing personnel Stockholm County hospitalsCases: n = 240Referents: n = 614 | Work-related over exertion back injury by social insurance office | Work-related and non-work-related exposure (i.e. patient transfers, physical exertion at work) | Postal questionnaires, perceived exertion scale | Logistic regression analysis (RR 95% CI) adjusted 3,4,5Patient transfer (≥1/shift): 2.7 (1.6–4.5) | ||
| Eriksen et al. [28] | Pro | 3 and 15 months | Norwegian nurses’ aidesBaseline: n = 7,478FU I: n = 3,808FU II: n = 3,615 | Extent of LBP and absence of work by questionnaire | Physical factors at work (i.e. patients positioning, lifting or supporting, lifting, carrying or pushing heavy objects); physical leisure time activities | Questionnaires (Likert scale 5 points) | Logistic regression analysis (OR-95% CI)Data not presented | Adjusted 1,2,4,5Intense LBP during 3 months: positioning patients in bed per average shift: 0: 1.0; 5–9: 1.63 (1.14–2.31); special tasks of caring nature in leisure time: no: 1.0; rather much or very much: 1.58 (1.03–2.42)Sick leave >8 weeks prior to 15 months: lifting, carrying and pushing heavy objects at work per average shift: 0: 1.0; 1–4: 0.99 (0.59–1.64); 5–9: 2.21 (1.17–4.16) |
| Friedrich et al. [29] | Retro | 12 months | Sewage workersBaseline: n = 370FU: n = 255 | Work disability due to LBP by Low Back Outcome Scale questionnaire | Physical workload (i.e. combined stooping and lifting, lifting loads) | Self-administered questionnaire | Logistic regression analysis (OR-95% CI)Data not presented | (Stepwise) adjusted 1,2,4,5Workload disability scores: 0.94 (0.92–0.95) |
| Hagen et al. [30] | Pro | 7 years | Occupationally active men and womenBaseline: n = 31.263FU :: n = 25.271 | Disability retirement because of LBP by files National Insurance Administration | Occupational risk factors (i.e. physically demanding work); lifestyle factors (i.e. physical exercise) | Self-administered questionnaires | Logistic regression analysis (OR 95% CI) adjusted 1,2,3,5Physically demanding work: almost never: 1.0; fairly infrequently: 1.6 (1.1–2.4); fairly often: 3.5 (2.4–5.2); nearly always: 5.7 (3.7–8.8)Physical exercise index: lowest percentile (91–100%): 1.9 (1.4–2.4). Combined regression model: physically demanding work nearly always: 4.1 (2.7–6.4). | |
| Harkness et al. [31] | Pro | 12 and 24 months | Newly employed workers from 12 diverse occupational groupsBaseline: n = 1,081FU I: n = 625FU II: n = 430 | New onset of LBP by questionnaire | Work-related manual handling activities and postures | Self-administered questionnaire | Generalised estimating equations (OR 95% CI) adjusted 1,2,5Manual handling activities: lift or carry with two hands: never: 1.0; >24 lb 1.8(1.1–2.9); lifting at or above shoulder level: never: 1.0; >23 lb 2.1 (1.2–3.8); pulling: >56 lb 2.1 (1.2–3.4)Postural factors: never: 1.0; kneeling: ≥15 min 1.8 (1.1–3.3); squatting: ≥15 min 1.8 (1.1–3.1); bending: <15 min 1.6 (1.1–2.3); working with hands above shoulders: <15 min 1.6 (1.1–2.4) | Adjusted 1,2,5Work-related mechanical factors not significant. |
| Hartvigsen et al. [32] | Pro | 5 years | Population-based Danish cohortBaseline: n = 1,397FU: n = 1,163 | LBP by Standardised Nordic Questionnaire | Physical workload (sedentary, light, heavy) | Self-administered questionnaires | Logistic regression analysis (OR-95% CI)LBP short and long: sedentary: 1.0; light: 1.09–1.86; heavy: 1.80 (1.31–2.48). LBP long: heavy physical workload 2.35 (1.58–3.49). | Adjusted 1,2,5LBP short and long: sedentary: 1.0; light physical workload: 1.33 (1.01–1.75); heavy physical workload: 1.68 (1.22–2.33). LBP long: heavy physical workload: 2.26 (1.50–3.40). |
| Hellsing et al. [33] | Pro | 20 years | 18 years old men enlisted for military serviceBaseline: n = 6,626FU: n = 3,287 | LBP within the work environment, sick –listing, absence from work and effect on everyday life by follow-up postal questionnaire | Physical strain at work (i.e. mostly sitting, changing, not physically heavy, medium heavy, physically heavy work) | Self-administered questionnaires | Logistic regression analysis (OR 95% CI)LBP: mostly sitting: 1.0; physically medium heavy: 1.82 (1.54–2.17); physically heavy work: 2.25 (1.57–3.24). | Adjusted 3,4,5LBP: mostly sitting: 1.0; physical medium heavy 1.48 (1.22–1.79); physical heavy 1.61 (1.08–2.39). Sick-listing or absence from work 5 years before FU: mostly sitting: 1.0; changing not physically heavy: 1.49 (1.16–1.93); medium heavy: 2.18 (1.74–2.74); heavy :2.31 (1.48–3.59). Effect on everyday life work 5 years before FU: mostly sitting: 1.0; medium heavy: 1.62 (1.30–2.04); heavy: 3.16 (2.05–4.85). |
| Hoogendoorn et al. [34] | Pro | 3 years | Blue and white collar workersBaseline: n = 1,192FU: n = 861 | Occurrence of LBP by an adaptation of the Nordic Questionnaire | Physical load at work place(i.e. flexion, rotation of the trunk and lifting) | Video recording and measurements at workplace | Cox regression (RR 95% CI)Percentage of the working time flexion: ≤5% ≥30o: 1.0; >5% ≥60o: 1.47 (1.01–2.14). Number of lifts per 8 h working: never: 1.0; >15 times ≥25 kg: 1.61 (1.11–2.34). | Adjusted 1,2,4,5Number of lifts per 8 h working: never: 1.0; >15 times ≥25 kg: 1.62 (1.04–2.53). |
| Hoogendoorn et al. [35] | Pro | 3 years | Blue and white collar workersBaseline: n = 1,738FU: n = 988 | Sickness absence due to LBP by company records | Physical workload exposure | Video recording and measurements at workplace | Poisson regression models (RR 95% CI)Percentage of the working time with trunk flexed ≥30o: ≤5%: 1.0; 10–15%: 2.83 (1.81–4.32); 15–20%: 4.02 (2.40–6.45); >20%: 3.01 (1.80–4.84). Percentage of the working time with trunk flexed: ≤5% ≥30o:1.0; 5–10% ≥30o: 1.75 (1.12–2.67); >10% ≥30o and ≤5% ≥60o: 2.91 (1.97–4.25); >5% ≥60o: 3.65 (2.31–5.62). Percentage of the working time with trunk rotated ≥30o: ≤5%: 1.0; 5–10%: 2.90 (2.11–3.97). Number of lifts/8 h working day: never: 1.0; never ≥10 kg/working day: 2.31 (1.35–3.92); never ≥25 kg/working day: 2.76 (1.78–4.39); 1–15 ≥ 25 kg/working day: 3.60 (2.18–5.99); >15 ≥ 25 kg/working day: 3.81 (2.14–6.68). | Adjusted 1,2,3,4,5Short absences (3–7 days) Number of lifts/8 h working day never: 1.0; never ≥10 kg: 2.68 (1.13–6.46)Long absences(>7 days). Percentage of the working time with trunk flexed ≥30o flexion ≤5%: 1.0; 10–15%: 3.21(1.91–5.34); 15–20%: 3.66 (1.86–6.91); >20: 2.93 (1.55–5.33). Percentage of working time with trunk flexed ≤5 ≥30o: 1.0; >10 ≥ 30o and ≤ 5 ≥ 60o: 3.08 (1.90–4.96); >5 ≥60o: 3.49 (2.03–5.89)Percentage of working time with trunk rotated ≥ 30o ≤5: 1.0; 5–10: 2.30 (1.51–3.47); >10: 2.54 (1.30–4.71)Number of lifts/8 h working day: never: 1.0; never ≥10 kg: 3.19 (1.72–6.01); never ≥25 kg: 2.99 (1.68–5.54); 1–5 ≥ 25 kg: 2.78 (1.40– 5.58); >5 ≥25 kg: 3.26 (1.52–6.98). |
| Hoozemans et al. [36] | Pro | 1 year | Employees of companies known with pushing and pulling activitiesBaseline: n = 629FU: n = 459 | Prevalence of LBP by the Standardised Nordic Questionnaire | Exposure to pushing and pulling | Dutch Musculoskeletal Questionnaire; observation at work | Cox’s proportional hazard regression analysis (PR 95% CI)Data not presented. | Adjusted 1,2Prevalence rate ratios of self-reported exposure, observed frequency and observed duration did not significantly increase between the reference group and the medium and high exposed groups. |
| IJzelenberg et al. [37] | Pro | 6 months | Industrial workersBaseline: n = 505FU: n = 407 | Occurrence LBP, sick leave and health care as a result of LBP by Standardised Nordic Questionnaire and medical questionnaires | Physical workload exposure (i.e. manual material handling, awkward back postures) | 4-point questionnaire | Logistic regression analysis (OR 95% CI)Data not presented. | Adjusted 1,2,3,4,5No significant associations between work-related physical loads and LBP. |
| Jacob [53] | Pro | 1 year | Community-based random sampleBaseline: n = 237FU: n = 212 | LBP by interview and questionnaire | Occupational—leisure time and sports activities | Baecke Physical Activity Questionnaire | Logistic regression analysis (OR 95% CI)Data not significant. | |
| Jansen et al. [38] | Pro | 1 year | Workers in nursing homes working >10 h/weekBaseline: n = 769FU: n = 523 | Incident LBP by Nordic Questionnaire; LBP with disability by Von Korff disability score | Physical workload exposure (i.e. trunk flexion, lifting and carrying loads) | Observational multimoment method | Hierarchical log linear models (RR 95% CI) adjusted 1,4,5Trunk flexion over 45o 30 min/week: 1.0; 45 min/week: 1.31 (1.03–1.65); 1 h/week:1.71 (1.08–2.72); 90 min/week: 2.82 (1.16–6.86); 105 min/week: 3.18 (1.13–9.00). | |
| Josephson et al. [49] | Case—Ref. | Population-based sampleCases: n = 333Referents: n = 733 | Seeking care due to LBP by interview and questionnaire | Physical workload (i.e. energetic work load-time-weighted MET, manual lifting working in forward-bent, positions with hands below knee, work in same positions) | Self-administered questionnaire | Logistic regression analysis (OR 95% CI) adjusted 1Working in forward bent positions 4.3 (1.6–12); high energetic work load 2.1 (1.1–4.2). | Adjusted 1,3Working in forward bent positions: 60 min/day 8.7 (2.1–46); high energetic work load 2.3 (1.0–5.3). | |
| Juul-Kristensen et al. [39] | Pro | Mean FU: 21 months (range 17–23) | Office workers (different types of computer work)Baseline: n = 3,475FU: n = 2,576 | Frequency and intensity of self-reported LBP by modified version of the Nordic questionnaire | Physical workload – ergonomic parameters (i.e. chair adjustment, time standing up at desk, rest pause) | Self-administered questionnaire | Logistic regression analysis (OR 95% CI) adjusted 1,2Tendency for proportion of working time related to the intensity of LBP (p = 0.092). | |
| Kerr [50] | Case— Ref. | Employees automobile productionCases : n = 97Referents: n = 124 | New episode of LBP by report to a onsite occupational nursing station | Physical workload at work (i.e. peak shear forces, hand force, compressive forces) | Interview-assisted questionnaire and worksite assessment | (Stepwise)Logistic regression analysis (OR 95% CI) adjusted 1, 3, 4, 5Higher peak lumbar shear: 1.7 (1.02–2.86). Higher cumulative lumbar disc compression: 2.0 (1.22–3.59)Higher peak hand force: 1.9 (1.21–3.10). | ||
| Kopec et al. [54] | Pro | 2 years | Canadian National Population Health Survey (NPHS) ≥ 18 yearsBaseline: n = 11.063FU: n = 10.007 | Incidence rate of LBP by questionnaires | Specific physical activity and work-related variables | Self-administered questionnaire | Logistic regression (OR 95% CI)Insignificant effects (p > 0.25) were dropped out for further considerationData not presented. | (Stepwise) adjusted 1Men: usual daily activity walking or standing 1.59 (1.11–2.28); lifting light loads 1.61 (1.03–2.51); heavy work 1.84 (1.14–2.99); gardening/yard work <3 h/months: 0.62 (0.40–0.94); ≥3 h/months 0.55 (0.38–0.80). |
| Krause et al. [40] | Pro | 7.5 years | Transit vehicle operatorsBaseline: n = 1,974FU: n = 1,233 | First incidence of a compensated LB injury by company employment record and/or workers compensation insurer’s database | Physical workload (i.e. type and duration of exposure) | Occupational questionnaire and baseline health survey | Cox proportional hazard regression analysis (HR 95% CI) adjusted 1,2Total driving h/week: 20–30: 1.0; 31–50: 1.53 (1.00–2.33); >50: 2.05 (1.24–3.37). | Adjusted 1,2,4Total driving h/week 20–30: 1.0; >50: 2.17: (1.28–3.68). |
| Latza et al. [41] | Pro | 3 years | Workers construction industryBaseline: n = 285FU: n = 230 | Prevalence of self-reported LBP by interview | Work tasks (i.e. bricklayers) | Interview | Cox’s regression analysis (PR 95% CI)Sawing wood h/shift: 0: 1.0; >0–1.0: 2.0 (1.0–4.3). | Adjusted 1,5.Sawing wood h/shift: 0: 1.0; >0–1.0: 2.4 (1.1–5.2). |
| Miranda et al. [42] | Pro | 1 year | Employees Finnish forest industryBaseline: n = 2,256FU: n = 1,676 | 1 year incidence of a new episode of LBP by Nordic questionnaire | Work-related physical exposure (i.e. lifting, awkward positions, twisting, physical exercise) | Self-administered questionnaire | Log-binominal regression (RR 95% CI) adjusted 1,2.By variable: <40 years: heavy lifting 1.5 (1.1–2.1); 40–49 years: awkward positions: 1.6 (1.2–2.3); ≥50 years: physical exercise ≥2–3: times/week 1.0; 0 to <1 time/week 1.5 (1.0–2.4). By number of physical exposures: <40 years: 0: 1.0; 3: 2.5 (1.5–4.2); 40–49 years: 0: 1.0; 1: 1.7 (1.2–2.6); 3: 2.3(1.3–4.1). | Adjusted 1,2.By variable: <40 years: heavy lifting 1.4 (1.0–2.1); 40–49 years: awkward positions 1.6 (1.1–2.3). By number of physical exposures: <40 years: 0: 1.0; 3: 2.4 (1.4–4.2); 40–49 years: 0: 1.0; 1: 1.6 (1.1–2.4); 3: 2.1 (1.2–3.9). |
| Mortimer et al. [51] | Case—Ref. | Population –based cohortCases: n = 791Referents: n = 1,610 | Seeking care for LBP by reports care givers | Physical loads during occupational work; sports activities (i.e. low and high intensity in combination with duration) | Interview | Mantel–Haenszel method (RR 95% CI) adjusted 1Outcome not significant. | Logistic regression analysis (RR 95% CI) adjusted 1, 3, 4, 5Women: no sports activities1.0; 1–2 h/week high intensity: 1.6 (1.1–2.4). | |
| Muller et al. [43] | Retro | 15 years | Inhabitants of a municipality in Denmark30–40–50-year-oldBaseline: n = 928FU: n = 467 | Self-reported sick-listing caused by LBP by questionnaire | Working conditions (i.e. physical load such as sedentary work, walking, carrying, heavy physical work, no work) | Self-administered questionnaire | Logistic regression analysis (OR 95% CI)Data not presented. | Adjusted for 1,2Outcome not significant. |
| Nolting et al. [55] | Pro. and retro | <12 monthsand>12 months | Employees chemical industry<12 months: _n_ = 435>12 months: n = 216 | LBP by questionnaire | Physical workload; sports activities; gardening | Self-administered questionnaire | Logistic regression analysis (OR 95% CI) adjusted 1Physical workload: ≤ median 1.0; >median 3.28 (2.09–5.17). | (Stepwise) adjusted 1Retro: Physical workload x perceived work demands: 3.71 (1.90–7.23). Pro: 4.34 (1.43–13.15). |
| Tubach [44] | Pro | 4 years | GAZEL cohort; employees French national electricity and gas companyBaseline: n = 3,123FU: n = 2,236 | LBP and sick leave due to LBP by self-administered questionnaire | Physical work load (i.e. carry loads, driving, bending or twisting) | Self-administered questionnaire | Logistic regression analysis (RR 95% CI)LBP without sick leave:carry loads >10 kg: never: 1.0; every day: 1.3 (1.0–1.8); driving: never: 1.0; every day: 1.3 (1.0–1.7); bending forward or backward: never or seldom: 1.0; occasionally: 1.7 (1.3–2.1); often: 1.7 (1.3–2.2); every day repetitively: 1.9 (1.4–2.6). twisting: never or seldom: 1.0; occasionally: 1.3 (1.0–1.6); often: 1.7 (1.3–2.3); every day, repetitively: 1.8 (1.3–2.4)LBP with sick leave:carry loads >10 kg: never: 1.0; >once/week: 1.9 (1.0–3.7); every day: 4.1 (2.2.–7.5). driving: never: 1.0; every day: 2.8 (1.6–4.9). bending forward or backward: never or seldom: 1.0; occasionally: 3.4 (1.6–7.3); often: 4.7 (2.2–10.1); every day repetitively: 8.2 (3.7–17.9). twisting: never or seldom: 1.0; often: 2.9 (1.5–5.5); every day, repetitively: 3.7 (1.8–7.5). | Logistic regression analysis (polytomous/OR 95% CI) adjusted 1,3,4LBP without sick leave: bending forward or backward: never or seldom: 1.0; occasionally: 1.6 (1.1–2.3); twisting: never or seldom: 1.0; often: 1.5 (1.0–2.2). LBP with sick leave:bending backward; never or seldom: 1.0; occasionally: 4.8 (1.8–13); often: 4.7 (1.6–14). |
| Van Nieuwenhuyse et al. [56] | Pro | 1 year | Employees of four healthcare institutes(Belgian Cohort Back Study)Baseline: n = 851FU: n = 585 | LBP by modified version of the Nordic Questionnaire | Physical workload (i.e. exposure awkward positions, manual materials handling such as lifting, carrying, pushing, pulling loads, static postures); physical load during LT (i.e. sporting activities, construction and embellishment work, motor vehicle driving) | Self-administered questionnaire | Cox regression analysis (RR 95% CI)Working with trunk in bent and twisted position: no 1.0; >2 h/day 2.35 (1.28–4.31). Ability to change posture regularly: yes: 1.0; no: 2.51 (1.50–4.17). | Adjusted 1,2,4,5Working with trunk in bent and twisted position: no: 1.0; >2 h/day: 2.21 (1.20–4.07)Ability to change posture regularly yes: 1.0; no: 2.11 (1.26–3.54). |
| Videman et al. [45] | Pro | 1 and 5 years | Nursing studentsBaseline: n = 255FU I: n = 197FU II: n = 174 | LBP by questionnaire anddisability by the Oswestry Low Back Pain Disability Questionnaire | Physical workload (i.e. twisted and bent work positions) | Self-administered questionnaires | Logistic regression analysis (OR 95% CI)Other LBP: twisted-bent work position: no: 1.0; yes 5.5 (1.9–15.7). Disability score: twisted-bent work position: no: 1.0; yes 7.0 (3.0–16.3). | Adjusted 3,4,5Other LBP: twisted-bent work position: no: 1.0; yes 6.2 (1.7–23.2). Disability score: twisted-bent work position: no: 1.0; yes 7.5 (2.9–19.6). |
| Vingard et al. [57] | Case—Ref. | Population –based cohortCases: n = 695Referents: n = 1,423 | Seeking care for LBP by reports care givers | Current and past work-related factors (i.e. specific work tasks, energy expenditure time-weighted average, manual materials, work postures); leisure time; sports | Self-administered questionnaires and interviews | Logistic regression analysis (RR 95% CI) adjusted 1,5Men: heavy lifting: >15 kg many times/day: 1.5 (1.1–2.1); time-weighted MET: ≥3.0: 1.4 (1.0–2.0). Women: time-weighted MET ≥3.5: 2.5 (1.4–4.6); ≥3.0: 1.9 (1.2–2.8). | Adjusted 1,4,5Men: forward bending ≥60 min/day: 1.8 (1.1–3.1); heavy lifting: 1.4 (1.0–2.0). Women: vehicle driving ≥240 min/day: 2.8 (1.0–8.5); time-weighted MET ≥ 3.0: 2.0 (1.2–3.2). | |
| Yip [46] | Pro | 12 months | Nurses Hong Kong districtBaseline: n = 244FU: n = 144 | New episode LBP by interview | Physical work activities (i.e. material handling, lifting and carrying); leisure time (i.e. sedentary, underactive, active) | Baseline interview | Logistic regression analysis(RR 95% CI)Data not presented. | (Stepwise) adjusted 1Bent to lift an item from floor level: lowest tertile: 1.0; highest tertile: 2.76 (1.06–7.22). |
Associations between physical activity and LBP are presented by categories of exposure: occupational physical loading and non-occupational physical activities, i.e. leisure time activities, sports and physical exercise. Adjustments were made for age, gender, life style factors (e.g. smoking, alcohol, leisure time activities), psychological related work and environmental factors (e.g. job demands, superior support, control workplace), individual and health-related factors (e.g. education, body mass index, self-rated health, general health, fitness, fatigue) and the duration of the exposure.
Occupational physical loading
A total of 35 studies on exposure to occupational physical loading and the occurrence of LBP complaints were reviewed. Exposures were described in self-reported magnitudes of physical workload and loads specifically related to manual handling such as lifting, carrying and pushing, posture and specific occupational tasks related to back exertion. The dose–response relationship between physical load and LBP was explored by dimensions of physical exertion (sedentary, light, medium and heavy load), by energy expenditure as an overall proxy for the energetic work load, by multiples of the resting metabolic rate (MET) and by peak lumbar shear forces by biomechanically modelling spinal loading estimates. Work-related posture involved duration and degree of awkward positions, such as working in forward-bent positions, twisted-bent positions and the ability to change posture regularly.
Heavy workload or physically demanding work
Eleven studies [25, 30, 32, 33, 42, 46, 49, 50, 54, 55, 57] exploring the intensities of physical workload reported a significant association of heavy workload or physically demanding work with LBP. Work-related risk factors were not just associated with the occurrence of LBP. A significant trend was observed for the level of physical load and sick leave due to LBP. One study [47] described the association of both heavy physical load and sedentary work with LBP amongst both genders, although both exposures had a slightly stronger association with LBP in women than in men. Four studies exploring different levels of physical workload [25, 30, 33, 57] reported increasing risk estimates for LBP, related to the accumulation of workload. The study by Vingård et al. [57] described the gender-specific risk of physical load measured as time-weighted average MET ≥ 3 in women. One study [50] performed separate loading analyses for each job component using a biomechanical model generating spinal loading estimates. Peak lumbar shear forces proved to be a robust risk factor, as did cumulative lumbar disc compression. The magnitude of the risk estimates of physical load ranged between 1.61 (1.08–2.39) [33] and 4.1 (2.7–6.4) [30]. According to these results, there is strong evidence that heavy workload is a moderate to strong risk factor for LBP.
Loads specifically related to manual handling
Separate from the magnitude of occupational physical loading, 10 cohort studies [22–24, 26–28, 34, 35, 42, 54] and one case–control study [57] explored the dose–response relationship between loads specifically related to manual handling, in particular lifting and carrying. Eight studies specifically focused on a working population [22, 23, 26, 28, 34, 35, 42] and three studies were population-based [24, 54, 57]. Lifting and carrying were explored in 10 studies [22–24, 27, 28, 34, 35, 42, 54, 56] whilst one study [26] focused on the association between strenuous arm movements in scaffolding and back pain. All studies reported positive associations with cumulative risk estimates associated with the accumulation of loads or frequency of lifts varying from 1.4 (1.0–2.1) [42] to 3.26 (1.52–6.98) [35]. The population-based studies by Bildt et al. [24] and Vingård et al. [57] reported significant risk estimates amongst men. According to the results, there is strong evidence that the accumulation of loads or frequency of lifts is moderately-to-strongly associated with LBP.
Posture of the lumbar spine
The dose–response relationship between posture of the lumbar spine and LBP is primarily explored by trunk flexion, twisted positions or awkward positions, expressed by duration, extent and percentage of working time. Ten studies, of which seven were based on a working population [35, 38, 42, 44–46, 56] and three population-based studies [24, 49, 56] reported statistically significant effects for flexed and/or rotated postures, positively associated with the duration and extent of the posture. Risk estimates varied between 1.8 (1.1 and 3.1) [57] and 8.7 (2.1 and 46) [49] for the mainly flexed positions, between 1.5 (1.0–2.2) [44] and 2.54 (1.30–4.71) [35] for trunk rotation and between 1.6 (1.1–2.3) [42] and 7.5 (2.9–19.6) [45] for the twisted-bent positions. A twofold increased risk was observed in case of the inability to change posture regularly [56]. According to these results, there is strong evidence that positioning of the lumbar spine in a flexed and/or rotated position is moderately to strongly associated with LBP.
Walking and standing
Only one study [22] explored the association between walking or standing in a general working population and found a moderate association between prolonged standing (>30 min) and LBP.
Specific occupational loads
Several studies analysed the association between LBP and the exposure to specific occupational tasks. The studies by Elders et al. [26, 27] explored the absence ratio and cumulative incidence and recurrence of LBP in workers in a scaffolding company and found high manual handling of materials, i.e. strenuous arm movements to be strongly associated with LBP (2.98: 1.57–5.66). Six studies [25, 28, 38, 45, 46, 48] explored the occupational physical loading of workers in nursing, related to twisted and bent work positions, the positioning of patients in bed and the transfer of patients per average shift. Associations with LBP complaints varied between moderate values (1.6: 1.14–2.3) [28] and strong values (6.2: 1.7–23.2) [45]. The exposure to vehicle driving was explored in both a working population [40] and a population-based cohort [57]. A higher amount of total driving hours was strongly associated with LBP in transit vehicle operators (2.17: 1.28–3.68) [40] and in women (2.8: 1.0–8.5) [57]. According to these results, there is strong evidence that the performance of occupational tasks, such as manual handling of materials, physical exertion in nursing and the exposure to vehicle driving are moderately to strongly associated with LBP.
Non-occupational physical activity
Levels of physical activity and physical exertion of the spine were explored in leisure time activities [23, 46, 52, 54] and sports and physical exercise [30, 51, 52]. Specific types of exposure of physical activities in leisure time, such as regular home improvement activities [52] and high perceived load during leisure time (e.g. engaging in vigorous exercise) [47], were moderately associated with an increased risk for LBP. Risk estimates ranged between 1.8 (1.2–2.6) [52] and 1.9 (1.1–3.3) [47]. Sports and physical exercise were explored in three studies. Both regular and high intensity sports [51, 52] by women and physical exercises in the upper percentile (91–100%) [30] were moderately associated with LBP. The magnitude of the risk estimates ranged from 1.3 (1.0–1.6) to 1.9 (1.4–2.4). According to these results, there is strong evidence that intense physical exertion during leisure time is moderately associated with LBP.
In contrast to these positive associations, everyday physical activities in leisure time except exercise (e.g. cleaning) [23] and the performance of gardening/yard work [54] were found to be strongly (0.39: 0.20–0.76) to moderately (0.55: 0.38–0.80) associated with decreased risks for LBP.
Discussion
In this review, we explored the most recent literature (1999–2009) on the association between occupational physical loading, non-occupational physical activities, i.e. leisure time activities, sports and physical exercise and low back pain. Thirty-six studies met the inclusion criteria. We found strong evidence that heavy workload and the accumulation of loads or frequency of lifts result in a moderate to strong risk for LBP. Furthermore, a strong association was found for flexed, rotated and awkward positions. Inconsistent results were found for leisure time physical activities, sports and physical exercise. Results endorse the main conclusions of the review by Hoogendoorn et al. [15]. The outcome of studies published after 1999 did not change the view on the existing evidence.
Although a systematic approach was used with regard to physical activity, i.e. occupational load as well as non-occupational activities, the majority of the retrieved studies focused on occupational workload. Only six studies [23, 28, 30, 47, 51, 52] explored the association between physical leisure time, i.e. physical exercises and LBP. No studies focused on the association between daily habitual physical activities (e.g. domestic work or commuting) and LBP, which is a significant deficiency within the domain of studying dose–response gradients of physical activity. We do not assume that the results were biased in a particular direction because of erroneous exclusion. One of the problems that may hamper the search of epidemiologic evidence is the phenomenon that studies not showing positive results are less likely to be published. Cross-sectional studies were excluded because the design of the study had to be longitudinal. The main argument for the exclusion of this type of study is that the entity of baseline and follow-up measurement—the only unarguable and therefore necessary criterion for causality—is not met in cross-sectional studies, in which exposure and outcome are assessed simultaneously.
Thirty-five studies were considered to be high quality studies. Quality assessment of studies included in systematic reviews is important and at the same time considered as a resource of scientifically controversial dispute [61]. Some authors have suggested that quality scores can be misleading because there is no objective way of quality assessment and different methods are likely to produce different scores that may lead to different results if these scores are used in the analysis [62]. In addition, it is difficult to determine how to weight each item in an overall quality score. However, other authors have suggested that using sum scores is helpful in a systematic review to make a distinction between studies with a low and a high risk of bias, and found empirical evidence supporting this [63]. We used quality scores in order to gain an insight into the risk of bias within the results but it should be a serious consideration to abandon the use of firm cut-off points.
Two issues in the review coincide. First, the operationalisation of low back pain, and secondly, the validity of the exposure measurement. Low back complaints are of a complex and multidimensional nature with time playing a critical role. However, different definitions of back pain may result in different estimates of prevalence and incidence and no single definition has been generally accepted in back pain research. The development of standardised definitions of back pain could provide standards that improve future comparisons of LBP prevalence figures by person, place and time characteristics and offer opportunities for statistical summaries [64]. Within the studies of this review, operationalisation of LBP and methods used to determine risk estimates varied widely. Back pain has been operationalised by self-reports, sick leave, registration by company records, social insurance administrations, reports of medical consultation and treatment. In most studies, self-administered questionnaires were used. A disadvantage of self-reporting is the influence of subjective determinants. For instance, people who are exposed are more likely to report back pain than people who are the non-exposed [65]. In 10 studies [25–27, 32, 34, 36, 37, 39, 42, 56] information on symptoms was collected with the standardised Nordic questionnaire (or adaptation thereof) for the analysis of musculoskeletal symptoms and this questionnaire has been considered an international standard [58, 66]. Owing to the recurrent nature of low back pain, it is far from easy to determine whether a given episode of low back pain is independent from a previous episode or not. Therefore, dispute remains about the length of follow-up because the follow-up needs to be long enough to record sufficient new cases of back pain. However, it would be of much more interest to assess whether people without pre-existing low back pain are as likely as those having had low back pain to show occurrence (or reoccurrence) of low back pain within a certain time frame. The exposure to type and intensity of physical activities has been measured by various instruments. Ten studies used a validated questionnaire in physical activity assessment [22, 28, 31, 32, 36, 37, 47, 49, 53, 57] while four studies used video recording and measurements at the workplace [25, 34, 35, 38] and two studies used an interview [50, 51]. This variety in measurement techniques raises questions on the comparability of outcomes. An estimation of physical demands by self-reports has been criticised as being inaccurate, especially for the more complex load-bearing activities carried out by employees [67]. Otherwise, it has been shown that workload and occupational physical activity can be reliably assessed by questionnaires and that questionnaires can classify groups with heterogeneous occupational tasks [68–76].
We searched for evidence on type and intensity of physical activity such as mechanical risk factors for LBP and found associations with a variety of physical loads. Although the load of whole body vibrations is considered to be associated with LBP [71–73], we excluded this variable because we considered this exertion as an external mechanical force and not as a result of physical activity behaviour, which was the focus of our research. It is generally agreed that the aetiology of back pain is multifactorial [74] and that physical load only partially explains the prevalence of back pain [75]. There is robust evidence that psychological factors are related to future episodes of back pain and its related disability [76–78]. Three studies [29, 31, 53] demonstrated in a multidisciplinary approach that not mechanical factors alone but a combination of socio-demographic, work-related and psychosocial factors was important in predicting new onsets of LBP. These results emphasise that the back pain disabling process is complex and significantly influenced by mechanical and environmental as well as individual factors.
We retrieved six studies examining the effects of physical leisure time activities such as sports, daily activity walking, gardening and perceived load outside work. We found physical exercises in the upper percentile (91–100%) [30] associated with LBP. For women, the same finding was found for sports on a regular basis [52] and high intensity training [51]. In general, engaging in sport activities is not associated with back problems [6, 79] although specific sport activities may be detrimental to the spine [80]. After all, participating in regular sporting activities is considered an indicator of a healthy lifestyle. Other such indicators include; less smoking, participating in sporting activities on a regular basis and being more active during leisure time. This phenomenon is comparable to the so-called healthy worker effect, defined as a self-selection process that allows relatively healthy people to continue their participation in certain activities or jobs. An important aspect in all the studies on physical activity during leisure time and sports was that the operationalisation of physical activity in the studies differed and was, in general, not very specific. The positive association of physical exercises and sports with LBP might be interpreted as a result of the accumulation of the total of exercise and sports, as part of a continuum of activity levels with different consequences for LBP [6]. This accumulation might be especially true in healthy subjects. However, this phenomenon is an unavoidable source of bias that may intrude on studies focused on type and levels of physical activity.
Conclusion
According to the literature reviewed in this paper, there is strong evidence that heavy physical workload and the exposure to awkward positions are risk factors for back pain. Moderate to strong risk estimates exist for manual materials handling, defined as the sum of ‘lift and carry burden’ and ‘push or pull’, bending and twisting. These results correspond with the results in the review by Hoogendoorn et al. [15]. Inconsistent findings were found for leisure time physical activities, sports and physical exercise. With regard to the association between physical load and low back pain, studies are mainly focused on occupational physical activity. Large studies focusing on daily habitual physical activities in association with LBP are lacking. It is important to take both the complex aetiology and multi-dimensional structure of risk factors into account. It can be assumed that there is no bivariate, but multivariate association, so physical activity is one but not the only factor.
Perspectives
To establish the relative contribution of each risk factor and the role of potential confounding variables, studies should evaluate not only the multi-dimensional structure of risk factors, but also exposures in the past and during leisure time. One should be cautious when interpreting the risks of separate types and intensities of activity, because the ultimate physical load is the sum of all these activities. This makes it difficult to designate one particular activity as the cause of LBP.
References
- 1.Loney PL, Stratford PW. The prevalence of low back pain in adults: a methodological review of literature. Phys Ther. 1999;79(4):384–396. [PubMed] [Google Scholar]
- 2.Tulder MW, Koes BW, Bouter LM. A cost-of-illness study of back pain in the Netherlands. Pain. 1995;62:233–240. doi: 10.1016/0304-3959(94)00272-G. [DOI] [PubMed] [Google Scholar]
- 3.Picavet HSJ (2004) Een multimedia campagne gericht op de preventie van lage rugpijn: de potentiële gezondheidswinst. [Multiple media campaign aimed upon the prevention of low back pain: potential health profits]. RIVM rapport 260401001. Bilthoven, The Netherlands. National Institute of Public Health and Environment; available at http://rivm.openrepository.com/rivm/bitstream/10029/8838/1/260401001.pdf. Accessed 10 January 2010
- 4.Tulder MW, Koes BW, Bouter LM. Low back Pain in Primary Care: effectiveness of diagnostic and therapeutic interventions. Amsterdam: Institute for Research in Extramural Medicine, Faculty of Medicine, Vrije Universiteit; 1996. [Google Scholar]
- 5.Abenhaim L, Rossignol M, Valat JP, Nordin M, Avouac B, Blotman F, Charlot J, Dreiser RL, Legrand E, Rozenberg S, Vautravers P. The role of activity in the therapeutic management of back pain. Report of the International Paris Task Force on Back Pain. Spine. 2000;25(4 Suppl):1S–33S. doi: 10.1097/00007632-200002151-00001. [DOI] [PubMed] [Google Scholar]
- 6.Heneweer H, Vanhees L, Picavet HSJ. Physical activity and low back pain: a U-shaped relation? Pain. 2009;143:21–25. doi: 10.1016/j.pain.2008.12.033. [DOI] [PubMed] [Google Scholar]
- 7.Wickström GJ, Pentti J. Occupational factors affecting sick leave attributed to low-back pain. Scand J Work Environ Health. 1998;24(2):145–152. doi: 10.5271/sjweh.292. [DOI] [PubMed] [Google Scholar]
- 8.Skovron ML. Epidemiology of low back pain. Baillieres Clin Rheumatol. 1992;6(3):559–573. doi: 10.1016/S0950-3579(05)80127-X. [DOI] [PubMed] [Google Scholar]
- 9.Burdorf A, Sorock G. Positive and negative evidence on risk factors for back disorders. Scand J Work Environ Health. 1997;23:243–256. doi: 10.5271/sjweh.217. [DOI] [PubMed] [Google Scholar]
- 10.Anonymous. Bandolier J (1995;19–1). Evidence based health care. Back pain. http://www.medicine.ox.ac.uk/bandolier/band19/b19-1.html. Accessed 10 January 2010
- 11.Plowman SA. Physical activity, physical fitness, and low back pain. Exerc Sport Sci Rev. 1992;20:221–242. doi: 10.1249/00003677-199200200-00008. [DOI] [PubMed] [Google Scholar]
- 12.Lagerström M, Hansson T, Hagberg M. Work-related low-back problems in nursing. Scand J Work Environ Health. 1998;24(6):449–464. doi: 10.5271/sjweh.369. [DOI] [PubMed] [Google Scholar]
- 13.Gerr F, Mani L. Work-related low back pain. Prim Care. 2000;27(4):865–876. doi: 10.1016/s0095-4543(05)70181-0. [DOI] [PubMed] [Google Scholar]
- 14.Vuori IM. Dose-response of physical activity and low back pain, osteoarthritis and osteoporosis. Med Sci Sports Exerc. 2001;33(6 Suppl):S551–S586. doi: 10.1097/00005768-200106001-00026. [DOI] [PubMed] [Google Scholar]
- 15.Hoogendoorn WE, Poppel MNM, Bongers PM, Koes BW, Bouter LM. Physical load during work and leisure time as risk factors for back pain. Scand J Work Environ Health. 1999;25(5):387–403. doi: 10.5271/sjweh.451. [DOI] [PubMed] [Google Scholar]
- 16.Picavet HSJ, Schouten JSAG. Physical load in daily life and low back problems in the general population, the Morgen study. Prev Med. 2000;31:506–512. doi: 10.1006/pmed.2000.0737. [DOI] [PubMed] [Google Scholar]
- 17.Haynes RB, McKibbon KA, Wilczynski NL, Walter SD, Were R. Optimal search strategies for retrieving scientifically strong studies of treatment from Medline: analytical survey. Br Med J. 2005;330(7501):1179. doi: 10.1136/bmj.38446.498542.8F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dutch Cochrane Centre (2010) Evidence-based Richtlijn Ontwikkeling [Evidence-Based Guideline Development]. Formulier III: Het beoordelen van cohortonderzoek [Form III:To assess cohort studies]. Formulier IV: Het beoordelen van patient-controleonderzoek [Form IV: To assess patient-control studies]. http://www.Cochrane.nl. Accessed 10 March 2010
- 19.Tulder M, Furlan A, Bombardier C, Bouter L. Updates method guidelines for systematic reviews in the Cochrane Collaboration Back Review Group. Spine. 2003;28(12):1290–1299. doi: 10.1097/01.BRS.0000065484.95996.AF. [DOI] [PubMed] [Google Scholar]
- 20.Windt DAWM, Thomas E, Pope DP, Winter AF, Macfarlane GJ, Bouter LM. Occupational risk factors for shoulder pain: a systematic review. Occup Environ Med. 2000;57:433–442. doi: 10.1136/oem.57.7.433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Landis RJ, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–174. doi: 10.2307/2529310. [DOI] [PubMed] [Google Scholar]
- 22.Andersen JH, Haahr JP, Frost P. Risk factors for more severe regional musculoskeletal symptoms: a two-year prospective study of a general working population. Arthritis Rheum. 2007;56(4):1355–1364. doi: 10.1002/art.22513. [DOI] [PubMed] [Google Scholar]
- 23.Bergstrom G, Bodin L, Bertilsson H, Jensen IB. Risk factors for new episodes of sick leave due to neck or back pain in a working population. A prospective study with an 18-month and a three-year follow-up. Occup Environ Med. 2007;64(4):279–287. doi: 10.1136/oem.2006.026583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bildt C, Alfredsson L, Michélsen H, Punnett L, Vingård E, Torgén M, Öhman A, Kilbom A. Occupational and nonoccupational risk indicators for incident and chronic low back pain in a sample of the Swedish general population during a 4-year period: an influence of depression? Int J Behav Med. 2000;7(4):372–392. doi: 10.1207/S15327558IJBM0704_07. [DOI] [Google Scholar]
- 25.Burdorf A, Jansen JP. Predicting the long term course of low back pain and its consequences for sickness absence and associated work disability. Occup Environ Med. 2006;63(8):522–529. doi: 10.1136/oem.2005.019745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Elders LAM, Heinrich J, Burdorf A. Risk factors for sickness absence because of low back pain among scaffolders: a 3-year follow-up study. Spine. 2003;28(12):1340–1346. doi: 10.1097/01.BRS.0000065481.43111.7B. [DOI] [PubMed] [Google Scholar]
- 27.Elders LAM, Burdorf A. Prevalence, incidence, and recurrence of low back pain in scaffolders during a 3-year follow-up study. Spine. 2004;29(6):E101–E106. doi: 10.1097/01.BRS.0000115125.60331.72. [DOI] [PubMed] [Google Scholar]
- 28.Eriksen W, Bruusgaard D, Knardahl S. Work factors as predictors of intense or disabling low back pain; a prospective study of nurses’ aides. Occup Environ Med. 2004;61(5):398–404. doi: 10.1136/oem.2003.008482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Friedrich M, Cermak T, Heiller L. Spinal troubles in sewage workers: epidemiological data and work disability due to low back pain. Int Arch Occup Environ Health. 2000;73(4):245–254. doi: 10.1007/s004200050424. [DOI] [PubMed] [Google Scholar]
- 30.Hagen KB, Tambs K, Bjerkedal T. A prospective cohort study of risk factors for disability retirement because of back pain in the general working population. Spine. 2002;27(16):1790–1796. doi: 10.1097/00007632-200208150-00019. [DOI] [PubMed] [Google Scholar]
- 31.Harkness EF, Macfarlane GJ, Nahit ES, Silman AJ, McBeth J. Risk factors for new-onset low back pain amongst cohorts of newly employed workers. Rheumatology (Oxford) 2003;42(8):959–968. doi: 10.1093/rheumatology/keg265. [DOI] [PubMed] [Google Scholar]
- 32.Hartvigsen J, Bakketeig LS, Leboeuf-Yde C, Engberg M, Lauritzen T. The association between physical workload and low back pain clouded by the “healthy worker” effect. Population-based cross-sectional and 5-year prospective questionnaire study. Spine. 2001;26(167):1788–1793. doi: 10.1097/00007632-200108150-00011. [DOI] [PubMed] [Google Scholar]
- 33.Hellsing A, Bryngelsson I. Predictors of musculoskeletal pain in men: a twenty-year follow-up from examination at enlistment. Spine. 2000;25(23):3080–3086. doi: 10.1097/00007632-200012010-00016. [DOI] [PubMed] [Google Scholar]
- 34.Hoogendoorn WE, Bongers PM, Vet HC, Douwes M, Koes BW, Miedema MC, Ariëns GA, Bouter LM. Flexion and rotation of the trunk and lifting at work are risk factors for low back pain: results of a prospective cohort study. Spine. 2000;25(23):3087–3092. doi: 10.1097/00007632-200012010-00018. [DOI] [PubMed] [Google Scholar]
- 35.Hoogendoorn WE, Bongers PM, Vet HCW, Ariëns GAM, Mechelen W, Bouter LM. High physical work load and low job satisfaction increase the risk of sickness absence due to low back pain: results of a prospective cohort study. Occup Environ Med. 2002;59(5):323–328. doi: 10.1136/oem.59.5.323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hoozemans MJ, Beek AJ, Fring-Dresen MH, Woude LH, Dijk FJ. Low-back and shoulder complaints among workers with pushing and pulling tasks. Scand J Work Environ Health. 2002;28(5):293–303. doi: 10.5271/sjweh.678. [DOI] [PubMed] [Google Scholar]
- 37.IJzelenberg W, Burdorf A. Risk factors for musculoskeletal symptoms and ensuing health care use and sick leave. Spine. 2005;30(13):1550–1556. doi: 10.1097/01.brs.0000167533.83154.28. [DOI] [PubMed] [Google Scholar]
- 38.Jansen JP, Morgenstern H, Burdorf A. Dose-response relations between occupational exposures to physical and psychosocial factors and the risk of low back pain. Occup Environ Med. 2004;61(12):972–979. doi: 10.1136/oem.2003.012245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Juul-Kristensen B, Sogaard K, Stroyer J, Jensen C. Computer users’ risk factors for developing shoulder, elbow and back symptoms. Scand J Work Environ Health. 2004;30(5):390–398. doi: 10.5271/sjweh.827. [DOI] [PubMed] [Google Scholar]
- 40.Krause N, Rugulies R, Ragland DR, Syme SL. Physical workload, ergonomic problems, and incidence of low back injury: a 7.5-year prospective study of San Francisco transit operators. Am J Ind Med. 2004;46(6):570–585. doi: 10.1002/ajim.20094. [DOI] [PubMed] [Google Scholar]
- 41.Latza U, Karmaus W, Sturmer T, Steiner M, Neth A, Rehder U. Cohort study of occupational risk factors of low back pain in construction workers. Occup Environ Med. 2000;57(1):28–34. doi: 10.1136/oem.57.1.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Miranda H, Viikari-Juntura E, Punnett L, Riihimaki H. Occupational loading, health behavior and sleep disturbance as predictors of low-back pain. Scand J Work Environ Health. 2008;34(6):411–419. doi: 10.5271/sjweh.1290. [DOI] [PubMed] [Google Scholar]
- 43.Muller CF, Monrad T, Biering-Sorensen F, Darre E, Deis A, Kryger P. The influence of previous low back trouble, general health, and working conditions on future sick-listing because of low back trouble. A 15-year follow-up study of risk indicators for self-reported sick-listing caused by low back trouble. Spine. 1999;24(15):1562–1570. doi: 10.1097/00007632-199908010-00010. [DOI] [PubMed] [Google Scholar]
- 44.Tubach F. Risk factors for sick leave due to low back pain: a prospective study. JOEM. 2002;44(5):451–458. doi: 10.1097/00043764-200205000-00013. [DOI] [PubMed] [Google Scholar]
- 45.Videman T, Ojajarvi A, Riihimäki H, Troup JDG. Low back pain among nurses: a follow-up beginning at entry to the nursing school. Spine. 2005;30(20):2334–2341. doi: 10.1097/01.brs.0000182107.14355.ca. [DOI] [PubMed] [Google Scholar]
- 46.Yip VY. New low back pain in nurses: work activities, work stress and sedentary lifestyle. J Adv Nurs. 2004;46(4):430–440. doi: 10.1111/j.1365-2648.2004.03009.x. [DOI] [PubMed] [Google Scholar]
- 47.Bildt Thorbjornsson CB, Alfredsson L, Fredriksson K, Michelsen H, Punnett L, Vingård E, Torgén M, Kilbom A. Physical and psychosocial factors related to low back pain during a 24-year period. A nested case–control analysis. Spine. 2000;25(3):369–374. doi: 10.1097/00007632-200002010-00019. [DOI] [PubMed] [Google Scholar]
- 48.Engkvist IL, Hjelm EW, Hagberg M, Menckel WE, Ekenvall L. Risk indicators for reported over-exertion back injuries among female nursing personnel. Epidemiology. 2000;11(5):519–522. doi: 10.1097/00001648-200009000-00006. [DOI] [PubMed] [Google Scholar]
- 49.Josephson M, Vingård E, MUSIC-Norrtälje Study Group Workplace factors and care seeking for low-back pain among female nursing personnel. Scand J Work Environ Health. 1998;24(6):465–472. doi: 10.5271/sjweh.370. [DOI] [PubMed] [Google Scholar]
- 50.Kerr MS. Biomechanical and psychosocial risk factors for low back pain at work. Am J Pubic Health. 2001;91(7):1069–1075. doi: 10.2105/AJPH.91.7.1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Mortimer M, Wiktorin C, Pernol G, Svensson H, Vingård E. Sports activities, body weight and smoking in relation to low-back pain: a population-based case–referent study. Scand J Med Sci Sports. 2001;11(3):178–184. doi: 10.1046/j.1524-4725.2001.110308.x. [DOI] [PubMed] [Google Scholar]
- 52.Croft PR, Papageorgiou AC, Thomas E, Macfarlane GJ, Silman AJ. Short-term physical risk factors for new episodes of low back pain. Prospective evidence from the South Manchester Back Pain Study. Spine. 1999;24(15):1556–1561. doi: 10.1097/00007632-199908010-00009. [DOI] [PubMed] [Google Scholar]
- 53.Jacob T. Low back pain incident episodes: a community-based study. Spine J. 2006;6(3):306–310. doi: 10.1016/j.spinee.2005.06.011. [DOI] [PubMed] [Google Scholar]
- 54.Kopec JA, Sayre EC, Esdaile JM. Predictors of back pain in a general population cohort. Spine. 2003;29(1):70–77. doi: 10.1097/01.BRS.0000103942.81227.7F. [DOI] [PubMed] [Google Scholar]
- 55.Nolting HD, Grabbe Y, Pluto RP, Zober A. Multivariate analysis of the risk factors associated with the development of back problems in persons employed in the chemical industry. Arbeitsmed Sozialmed Umweltmed. 2005;40(12):630–638. [Google Scholar]
- 56.Nieuwenhuyse A, Somville PR, Crombez G, Burdorf A, Verbeke G, Johannik K, Bergh O, Masschelein R, Mairiaux P, Moens GF, BelCoBack Study Group The role of physical workload and pain related fear in the development of low back pain in young workers: evidence from the BelCoBack Study; results after one year of follow up. Occup Environ Med. 2006;63(1):45–52. doi: 10.1136/oem.2004.015693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Vingård E, Alfredsson L, Hagberg M, et al. To what extent do current and past physical and psychosocial occupational factors explain care-seeking for low back pain in a working population? Results from the Musculoskeletal Intervention Center-Norrtälje Study. Spine. 2000;25(4):493–500. doi: 10.1097/00007632-200002150-00017. [DOI] [PubMed] [Google Scholar]
- 58.Kuorinka I, Jonsson B, Kilbom A, Vinterberg H, Biering-Sørensen F. Standardised Nordic questionnaire for the analysis of musculoskeletal symptoms. Appl Ergon. 1987;18(3):233–237. doi: 10.1016/0003-6870(87)90010-X. [DOI] [PubMed] [Google Scholar]
- 59.Miettinen OS. Estimability and estimation in case–referent studies. Am J Epidemiol. 1976;103:226–235. doi: 10.1093/oxfordjournals.aje.a112220. [DOI] [PubMed] [Google Scholar]
- 60.Schmidt CO, Kohlmann T. When to use the odds ratio or the relative risk? Int J Public Health. 2008;53:165–167. doi: 10.1007/s00038-008-7068-3. [DOI] [PubMed] [Google Scholar]
- 61.Greenland S. Quality scores are useless and potentially misleading. Am J Epidemiol. 1994;140:300–302. [Google Scholar]
- 62.Whiting P, Harbord R, Kleijnen J. No role for quality scores in systematic reviews of diagnostic accuracy studies. BMC Med Res Methodol. 2005;5:19. doi: 10.1186/1471-2288-5-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Tulder MW, Suttorp M, Morton S, Bouter LM, Shekelle P. Empirical evidence of an association between internal validity and effect size in randomized controlled trials of low-back pain. Spine. 2009;34(16):1685–1692. doi: 10.1097/BRS.0b013e3181ab6a78. [DOI] [PubMed] [Google Scholar]
- 64.Dionne CE, Dunn KM, Croft PR, Nachemson AL, Buchbinder R, Walker BF, Wyatt M, Cassidy JD, Rossignol M, Leboeuf-Yde C, Hartvigsen J, Leino-Arjas P, Latza U, Reis S, Gil Del Real MT, Kovacs FM, Oberg B, Cedraschi C, Bouter LM, Koes BW, Picavet HS, Tulder MW, Burton K, Foster NE, Macfarlane GJ, Thomas E, Underwood M, Waddell G, Shekelle P, Volinn E, Korff M. A consensus approach towards the standardization of back pain definitions for use in prevalence studies. Spine. 2008;33(1):95–103. doi: 10.1097/BRS.0b013e31815e7f94. [DOI] [PubMed] [Google Scholar]
- 65.Kuiper JI, Burdorf A, Verbeek JHAM, Frings-Dresen MHW, Beek AJ, Viikari-Juntura ERA. Epidemiologic evidence on manual materials handling as a risk factor for back disorders: a systematic review. Int J Ind Ergon. 1999;24:389–404. doi: 10.1016/S0169-8141(99)00006-2. [DOI] [Google Scholar]
- 66.Palmer K, Smith G, Kellingray S, Cooper C. Repeatability and validity of an upper limb and neck discomfort questionnaire: the utility of the standardized Nordic Questionnaire. Occup Med (Lond) 1999;49(3):171–175. doi: 10.1093/occmed/49.3.171. [DOI] [PubMed] [Google Scholar]
- 67.Burdorf A. Reducing random measurement error in assessing postural load on the back in epidemiological surveys. Scand J Work Environ Health. 1995;21:15–23. doi: 10.5271/sjweh.3. [DOI] [PubMed] [Google Scholar]
- 68.Ainsworth BE, Richardson MT, Jacobs DRJ, Leon AS, Sternfeld B. Accuracy of recall of occupational physical activity by questionnaire. J Clin Epidemiol. 1999;52:219–227. doi: 10.1016/S0895-4356(98)00158-9. [DOI] [PubMed] [Google Scholar]
- 69.Riihimäki H. Hands up or back to work: future challenges in epidemiologic research on musculoskeletal diseases. Scand J Work Environ Health. 1995;21:401–403. doi: 10.5271/sjweh.54. [DOI] [PubMed] [Google Scholar]
- 70.Torgen M, Winkel J, Alfredsson L, Kihlbom A. Evaluation of questionnaire-based information on previous physical work loads: Stockholm MUSIC 1 Study Group. Musculoskeletal Intervention Center. Scand J Work Environ Health. 1999;25:246–254. doi: 10.5271/sjweh.431. [DOI] [PubMed] [Google Scholar]
- 71.Kumar A, Varghese M, Mohan D, Mahajar P, Gulati P, Kale S. Effect of whole-body vibration in the low back. Spine. 1999;24(23):2506–2515. doi: 10.1097/00007632-199912010-00013. [DOI] [PubMed] [Google Scholar]
- 72.Bovenzi M. Metrics of whole-body vibration and exposure–response relationships for low back pain in professional drivers: a prospective study. Int Arch Occup Environ Health. 2009;82:893–917. doi: 10.1007/s00420-008-0376-3. [DOI] [PubMed] [Google Scholar]
- 73.Tiemessen IJH, Hulshof CJT, Frings-Dresen MHW. Low back pain in drivers exposed to whole body vibration: analysis of a dose response pattern. Occup Environ Med. 2008;65:667–675. doi: 10.1136/oem.2007.035147. [DOI] [PubMed] [Google Scholar]
- 74.Borkan J, Tulder MW, Reis S, Schoene ML, Croft P, Hermoni D. Advances in the field of low back pain in primary care. Spine. 2002;27:E128–E132. doi: 10.1097/00007632-200203010-00019. [DOI] [PubMed] [Google Scholar]
- 75.Walsh K, Varnes N, Osmond C, Styles R, Coggon D. Occupational causes of low-back pain. Scand Work Environ Health. 1989;15:54–59. doi: 10.5271/sjweh.1891. [DOI] [PubMed] [Google Scholar]
- 76.Bongers PM, Winter CR, Kompier MA, Hildebrandt VH. Psychosocial factors at work and musculoskeletal disease. Scand J Work Environ Health. 1993;19:297–312. doi: 10.5271/sjweh.1470. [DOI] [PubMed] [Google Scholar]
- 77.Hoogendoorn WE, Poppel MN, Bongers PM, Koes BW, Bouter LM. Systematic review of psychosocial factors at work and private life as risk factors for back pain. Spine. 2000;25:2114–2125. doi: 10.1097/00007632-200008150-00017. [DOI] [PubMed] [Google Scholar]
- 78.Linton SJ. Occupational psychological factors increase the risk for back pain: a systematic review. J Occup Rehabil. 2001;11:53–66. doi: 10.1023/A:1016656225318. [DOI] [PubMed] [Google Scholar]
- 79.Mogensen AM, Gausel AM, Wedderkopp N, Kjaer P, Leboeuf-Yde C. Is active participation in specific sport activities linked with back pain. Scand J Med Sci Sports. 2007;17(6):680–686. doi: 10.1111/j.1600-0838.2006.00608.x. [DOI] [PubMed] [Google Scholar]
- 80.Iwamoto J, Abe H, Tsukimura Y, Wakano K. Relationship between radiographic abnormalities of lumbar spine and incidence of low back pain in high school rugby players: a prospective study. Scand J Med Sci Sports. 2005;15(3):163–168. doi: 10.1111/j.1600-0838.2004.00414.x. [DOI] [PubMed] [Google Scholar]