Insulin regulates its own delivery to skeletal muscle by feed-forward actions on the vasculature (original) (raw)
Abstract
Insulin, at physiological concentrations, regulates the volume of microvasculature perfused within skeletal and cardiac muscle. It can also, by relaxing the larger resistance vessels, increase total muscle blood flow. Both of these effects require endothelial cell nitric oxide generation and smooth muscle cell relaxation, and each could increase delivery of insulin and nutrients to muscle. The capillary microvasculature possesses the greatest endothelial surface area of the body. Yet, whether insulin acts on the capillary endothelial cell is not known. Here, we review insulin's actions at each of three levels of the arterial vasculature as well as recent data suggesting that insulin can regulate a vesicular transport system within the endothelial cell. This latter action, if it occurs at the capillary level, could enhance insulin delivery to muscle interstitium and thereby complement insulin's actions on arteriolar endothelium to increase insulin delivery. We also review work that suggests that this action of insulin on vesicle transport depends on endothelial cell nitric oxide generation and that insulin's ability to regulate this vesicular transport system is impaired by inflammatory cytokines that provoke insulin resistance.
Keywords: caveolae, endothelium, microvasculature, insulin transport
several relatively recent reviews relate to insulin's vascular action. That by Muniyappa et al. (68) focuses particularly on pathways of insulin signaling in both endothelial and smooth muscle cells and how these molecular events explain insulin's vasodilatory action. A review by Clark (21) focuses on insulin as a regulator of nutritive vs. non-nutritive flow and the methodologies that have been developed and applied to skeletal muscle in order to address this role of insulin. We also recently summarized work relating to insulin's vascular action: in particular we focused on the temporal relationship between insulin delivery and insulin-mediated glucose disposal in skeletal muscle, arguing that insulin delivery to muscle is the rate limiting step for insulin action in that tissue (8). Readers are referred to those reviews for a comprehensive discussion of each topic. Here, we will focus first on insulin's vasodilatory effects as they relate to insulin's ability to regulate the delivery of both itself and nutrients to the tissue microvasculature where nutrient exchange occurs. We will then focus on transendothelial insulin movement, as this step appears to be rate limiting for insulin action in skeletal muscle. We will not deal with insulin's direct actions on vascular smooth muscle cells, as this has been well covered in a recent review (2). We will consider the relationship between insulin's effects on skeletal muscle microvascular perfusion and on transendothelial transport as potential regulatory steps in insulin action on skeletal muscle glucose metabolism. We would also emphasize that insulin affects a number of other substrates (e.g., amino acids, triglyceride/FFA) and insulin's delivery would presumably impact these variables as well. For each of these substrates the control systems regulating delivery and tissue uptake are likely to be quite complex. This is emphasized by work from the laboratories of Wasserman (110) and Kelley (11, 12, 116). Both laboratories have provided evidence for a distributed control of glucose's metabolism between tissue delivery, transit through the interstitium, plasma membrane glucose transport, and hexokinase activity. Typically, these measurements are made under conditions of either fasting or steady-state hyperinsulinemia and do not bear directly on the issue of the rate-limiting step for insulin's action. Thus, this role of the microvasculature in insulin delivery is separate from the complex control of glucose transport/metabolism and underscores the complexity of the integrated metabolic system.
Insulin's Vascular Actions: a Feed-Forward Pathway to Promote Insulin and Nutrient Delivery in Skeletal Muscle
Augmentation of blood flow to insulin target tissues.
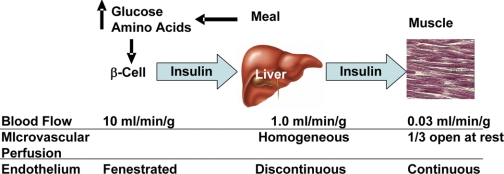
It is worth considering the differences in basal blood flow between different insulin-sensitive tissues. The liver and the myocardium each have a very substantial blood flow in the basal state (∼1 ml·min−1·g tissue−1). The islets of Langerhans have an even more luxuriant blood flow that is estimated to be about 5–12 mL/min/g of tissue (45). By contrast, skeletal muscle and adipose tissue basal blood flow averages only 0.03–0.04 ml·min−1·g tissue−1 (Fig. 1) (4). As a result, blood flow (or for insulin and some other solutes, plasma flow) can become an important factor limiting nutrient delivery and solute exchange to both muscle and adipose. We became aware of this more than a decade ago while conducting studies on the impact of raising plasma amino acid concentrations on the kinetics of skeletal muscle protein metabolism assessed using labeled amino acids (33). Based on the muscle clearance of labeled leucine and phenylalanine, it was quite clear that, due to the slow plasma flow, it required several hours for increases in plasma amino acid concentrations to equilibrate with the extracellular and intracellular water within skeletal muscle. Thus, for either labeled or unlabeled amino acids, measurements made at earlier times intrinsically are done at a nonsteady state.
Fig. 1.
Rate of blood flow and type of endothelium in several tissues involved in insulin secretion/action in the postprandial setting.
With exercise, muscle regulates its perfusion by increasing its blood flow up to 30- to 50-fold above basal. This allows both oxygen and nutrient delivery as well as the removal of metabolic products to match the needs of the tissue. In addition to increasing the total blood flow, exercise also recruits previously underperfused capillary beds (discussed below). We have observed that this capillary recruitment induced by muscle contraction is exquisitely sensitive to even very low workloads (44, 105). Indeed, in the rat hindlimb as well as in human forearm skeletal muscle, we have found that muscular contraction at workloads that do not appreciably affect total muscle blood flow expand the microvascular volume perfused within muscle two- to threefold. It appears that, when the need for nutrient and oxygen exchange has been only very modestly increased, the initial vascular response by skeletal muscle is to increase microvascular volume. Following this, an increase in total blood flow constitutes a second-stage response when metabolic demand is greater.
Such a staged vascular response may afford several advantages to muscle. First, solute exchange can be improved in the absence of changes in total blood flow or requirements for increases in cardiac output. In addition, by allowing more uniform flow distribution within the muscle, all muscle fibers would equally share the available nutrients presented. This may be the case with modest levels of exercise as well as in the postprandial state. There is a lack of agreement in the literature with regard to whether muscle total blood flow increases in the postprandial state. Some reports indicate a significant increase in skeletal muscle blood flow following meals (35, 43), whereas others fail to see such a response (37). We examined in both healthy and obese subjects the meal-related response of microvascular perfusion in addition to total blood flow (50). The obese subjects were significantly insulin resistant. While healthy subjects had an increase in both total muscle blood flow as well as microvascular perfusion following meal ingestion, this was not the case for the obese subjects.
Insulin relaxes resistance vessels and enhances total skeletal muscle flow.
Interest in insulin's vascular action was initially provoked by careful studies by Baron and colleagues (6, 55). They observed a strong correlation between leg blood flow, measured using a thermodilution method, and insulin-mediated glucose disposal. The thermodilution method allowed frequent measurement of blood flow without disturbing the flow, as occurs with plethysmographic methods. This may have enhanced their ability to detect changes in blood flow induced by insulin. In an impressive series of studies, they showed that leg blood flow responses to insulin closely paralleled leg insulin-mediated glucose disposal in control subjects. Most significantly, obesity (55) and type 1 (5) and type 2 diabetes (21, 56) appeared to proportionately diminish insulin-mediated blood flow and glucose disposal in the leg. They also observed that these leg blood flow responses to insulin were blocked by concomitant infusion of the nitric oxide (NO) synthase (NOS) inhibitor l-NMMA (97). In subsequent studies, they observed that raising plasma free fatty acid concentrations, which induced metabolic insulin resistance, also impaired insulin-mediated increases in leg blood flow (99).
As additional evidence accumulated indicating a link between a vascular action of insulin to enhance total limb blood flow and insulin's metabolic action, contrary findings were also reported. In particular, those reports raised the concern that increasing blood flow did not result in augmentation of insulin's metabolic action in healthy or insulin-resistant individuals (57, 69, 71) and that the time course for onset of insulin-induced increases in limb blood flow (particularly at physiological insulin concentrations) lagged behind insulin-induced increases in skeletal muscle glucose uptake (120). As a result, it was not possible to resolve whether total limb blood flow played a critical role in regulating delivery of either insulin or nutrients to skeletal muscle.
Insulin relaxes terminal arterioles in muscle to increase microvascular perfusion.
As the question of whether insulin action on limb blood flow was an important determinant of muscle glucose disposal became mired in controversy, our laboratory, in collaboration with Steve Rattigan and Michael Clark, took the approach of addressing whether insulin might be affecting skeletal muscle more by regulating microvascular perfusion and changing flow distribution rather than by altering total limb blood flow. Two considerations prompted this question. The first was the recognition that earlier studies had indicated that a significant fraction of skeletal muscle microvasculature was underperfused in the resting state and that muscle contraction “recruits” flow to these underperfused vessels (41, 42). We thought that insulin might, like contraction, call on a microvascular reserve. A second consideration, which followed from the first, was that increasing the volume of microvasculature perfused should, by increasing the endothelial surface available for insulin and nutrient exchange, directly enhance nutrient delivery to muscle even in the absence of changes in total blood flow. This could potentially serve as a more effective means of promoting solute delivery than increasing total blood flow, as the latter significantly augments delivery when the extraction ratio for solute is high (e.g., oxygen extraction by cardiac muscle) but has less impact when the extraction ratio is low (e.g., skeletal muscle insulin extraction is only ∼10%).
A limiting factor to investigating actions of insulin on the microvasculature was the lack of a validated method for measuring microvascular perfusion in vivo. This topic was extensively reviewed by Clark (21). We initially developed a biochemical method based on the single-pass extraction of 1-methylxanthine and its conversion to 1-methylurate as plasma coursed from the arterial to the venous circulation through skeletal muscle. We were encouraged by our first studies using the 1-methylxanthine method, which showed an effect of euglycemic hyperinsulinemia to “recruit” microvasculature within rat hindlimb skeletal muscle (82). Unfortunately, the volume of blood needed to measure 1-methylxanthine limited the number of samples that could be obtained for studies in rodents, and the clearance of 1-methylxanthine by human skeletal muscle is substantially lower than in the rodent, presumably because of a lower content of xanthine oxidase. As a result, this technique could not be easily adapted to clinical studies.
Subsequently, we adapted the contrast-enhanced ultrasound (CEU) method that had been extensively used in cardiac muscle (113) to measure microvascular blood volume within skeletal muscle. This technique offered the advantages of allowing repeated measurements over time and of being readily adaptable to clinical studies. CEU relies on the enhanced contrast afforded by intravenously infused lipid-coated microbubbles filled with perfluorocarbon gas. These microbubbles, which average 1–3 μm in diameter, course through the entire vasculature but are excluded from extravascular compartments. As such, the intensity of the contrast-enhanced signal provides an index of the volume of microvasculature perfused. Because these bubbles can be disrupted by a high-energy ultrasound pulse, it is possible to follow the time course for the refilling of a microvascular bed and from that to estimate both microvascular blood volume and the rate of flow of microbubbles into a vascular bed (113). In this fashion, multiple measurements can be made over time.
Using two independent techniques [laser Doppler flowmetry (20) and CEU (106)], we confirmed our initial findings of insulin's effect to recruit microvasculature in rats and then extended our studies to human skeletal muscle using the CEU method (25). As is the case for insulin's effect on resistance vessels and total blood flow, microvascular recruitment was dependent on insulin activation of endothelial (e)NOS (104). However, the effect on the microvasculature occurred much sooner than insulin's action to increase total blood flow (106) and was evident at lower insulin concentrations than required to increase total blood flow in the rat (122). Currently, we do not have a satisfactory explanation for the differences in time course and insulin sensitivity that we observed between terminal arterioles and resistance vessels, both of which are dependent on insulin signaling to enhance endothelial NO release (21). Interestingly, we observed that, despite high basal blood flow in the myocardium, raising the plasma insulin concentration effectively increased microvascular perfusion in cardiac as well as skeletal muscle (60, 61).
It is worth noting that these techniques [as well as others reviewed by Clark (21)] provide a measure of microvascular perfusion. They do not provide a direct visualization of the component vessels of the microvasculature. The microvasculature within skeletal muscle has been studied extensively using exteriorized thin muscle preparations (e.g., spinotrapezius and cremaster). However, these have not proved particularly useful for studying insulin's vascular action, and this may be secondary to changes in flow pattern that result from the surgical preparation and perfusion of the tissue (22). The technique of nail-fold video microscopy has allowed direct quantification in humans of the number of individual capillaries perfused in the presence and absence of insulin, albeit in skin and not muscle tissue (88). However, using this method, investigators have observed that the action of insulin on the skin microvasculature is also impacted negatively by insulin resistance as seen in metabolic syndrome (87) and obesity (26, 27). These direct observations of insulin-induced “capillary recruitment” in skin microvasculature is consistent with the conclusion that changes in microvascular volume quantified using CEU likely reflect a similar process within skeletal muscle rather than an increase in the functional diameter of previously opened capillaries.
Insulin increases the compliance of conduit arteries.
Until this point, we have focused the discussion on the action of insulin on resistance vessels and terminal arterioles, as there are extensive data demonstrating a significant physiological action of insulin on each of these. There is also a modest body of data to indicate that insulin has physiological actions on conduit arteries. This is of potential importance given the association between insulin resistance and accelerated atherosclerosis. Indeed, in a recent study, it was demonstrated that elimination of the insulin receptor specifically within the endothelium greatly accelerated the atherosclerotic process in apoE−/− mice (81). Insulin also exerts an acute effect to increase the compliance of conduit arteries; this effect was nicely shown using aplanation tonometry before and during a euglycemic hyperinsulinemic clamp (115). Raising plasma insulin has also been shown to increase the responsiveness of the femoral artery to methacholine-induced vasodilation (98). These latter actions of insulin have been demonstrated in healthy humans. We currently do not know whether the relationship between impaired endothelial insulin signaling in the vasculature and atherosclerosis seen in the apoE−/− mice translates to a similar risk in humans.
Insulin resistance is associated with dysfunction at all levels of the arterial vasculature.
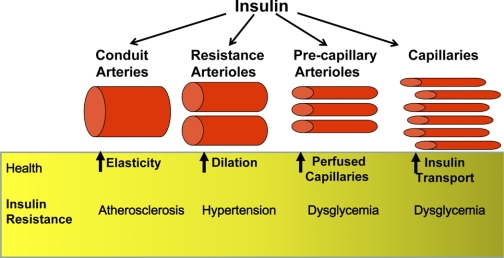
As noted above, Baron and colleagues observed that in multiple clinical circumstances metabolic insulin resistance was accompanied by vascular insulin resistance and that there appeared to be a significant correlation between these two entities. That work focused specifically on the relationship between metabolic insulin resistance and resistance to insulin's vasodilatory action on resistance arterioles. This suggestion that the impaired vascular responses to insulin might be contributing to the impaired metabolic response spurred considerable interest in further exploring insulin's vascular actions. We now understand (as reviewed above) that insulin exerts a physiological action at all levels of the arterial vascular tree. We also understand that insulin resistance is accompanied by dysfunction at each level (Fig. 2). At the level of conduit arteries, an extensive body of data indicates that metabolic insulin resistance, as seen in obesity, metabolic syndrome, and type 1 and type 2 diabetes, is accompanied by dysfunction that is manifested by increased vascular stiffness and/or impaired NO-mediated vasodilation (95, 102, 112, 114). In addition, the responsiveness of these vessels to insulin is impaired (114). Conduit vessel insulin resistance does not play any known pathogenetic role in metabolic insulin resistance; each is a distinct reflection of the general process of insulin resistance. Moreover, the demonstration of increased atherosclerosis within the conduit arteries of the apoE−/− mice that lack endothelial insulin receptor suggest a direct linkage between insulin resistance and accelerated atherosclerosis within the vasculature (81).
Fig. 2.
Insulin action at each level of the arterial tree and how this action is impacted adversely by insulin resistance with clinical consequences.
As the work from the Baron laboratory first clearly showed, metabolic insulin resistance is also accompanied by impaired insulin action on the resistance arterioles that regulate skeletal muscle blood flow (4, 7). The relationship between these two manifestations of insulin resistance remains somewhat controversial. It is important to note that these same resistance vessels have dysfunctional responses to intra-arterial methacholine (98, 100) or acetylcholine (38, 80, 111) infusion. Thus, metabolic insulin resistance is associated with a broader defect in vascular function beyond vascular insulin insensitivity. Indeed, impairment of insulin action on resistance vessels may underlie the increased prevalence of hypertension in states of insulin resistance.
Data from our laboratory suggest that insulin's action within skeletal muscles to relax terminal arterioles and expand the perfused vascular volume may be most closely linked to insulin-mediated glucose disposal by muscle. In healthy individuals, the time course (106) and concentration dependence (122) for insulin's action on the microvasculature are consistent with their playing a significant role in regulating insulin delivery and, hence, muscle glucose metabolism. Beyond that, this action of insulin is impaired in concert with impaired metabolic insulin sensitivity in a wide range of clinical (24, 50, 62) and experimental (23, 123) settings. As we will discuss later, this linkage between the metabolic and vascular actions of insulin likely relates to the role of the microvasculature within muscle to regulate insulin delivery.
Other hormones that influence limb blood flow or muscle microvascular flow.
The studies reviewed above describe in some depth the regulatory role that plasma insulin concentrations appear to exert on both total limb blood flow and microvascular perfusion, the latter presumably resulting from insulin acting on terminal arterioles. A number of other hormones (e.g., catecholamines and thyroxine) also influence limb blood flow, but their action on skeletal muscle microvascular perfusion has not been well studied. We observed a number of years ago that growth hormone (GH) infused locally into the brachial artery increases forearm blood flow dramatically (34). Raising GH concentrations to 35 ng/ml led to more than a doubling of forearm flow. In a subsequent study, IGF-I was observed to have a similar effect (32). The effects of GH, however, are likely independent of IGF-I generation, as the endothelial cell possesses GH receptors that, when stimulated, directly activate eNOS (59). Microvascular perfusion was not assessed in those studies, as the techniques for doing so had not yet been developed. In the rat hindlimb, we have observed that epinephrine, infused at a rate selected to raise total limb blood flow to a similar extent to that seen with insulin, did not mimic insulin's action to recruit microvasculature (82). Thus, it is possible to independently relax resistance vessels and increase total flow without impacting terminal arterioles and flow distribution. Conversely, we have observed that low-dose insulin infusions in both humans and rodents relax terminal arterioles and increase microvascular volume without increasing total limb blood flow (122). Low-intensity exercise appears to have a similar effect.
We have recently observed that infusion of angiotensin II, at a dose that does not raise arterial blood pressure substantially, increases muscle microvascular blood volume (17). Interestingly, nearly 20 years ago, Buchanan and colleagues had observed that, during hyperinsulinemia, angiotensin II infusion increased leg muscle glucose uptake in humans; they postulated that it might be acting to recruit microvasculature and thereby enhance glucose and insulin delivery to muscle (14). Equally interesting was the observation that blockade of the type 1 angiotensin receptor increased microvascular blood volume and muscle glucose uptake (measured by arterial venous difference across the rat hindlimb), whereas blockade of the type 2 angiotensin receptor decreased microvascular blood volume and muscle glucose extraction (17). This suggests that basal microvascular tone within skeletal muscle is significantly dependent on the balance between the activities of these two receptors.
How Does Insulin Exit the Vasculature?
Why should we care?.
We (8) have previously argued that the movement of insulin from the vascular to the interstitial compartment within skeletal muscle is rate limiting for insulin's metabolic action. Support for this argument is extensive and includes the early demonstration by Sherwin et al. (91) that the disappearance kinetics of intravenously injected insulin indicated a rapid equilibration of injected insulin within plasma and visceral tissue compartments but a slow equilibration within skeletal muscle. This early indication was further supported by the careful insulin clamp studies from Olefsky's laboratory demonstrating the slow onset of insulin's effect to enhance glucose disposal (half-time 44 min) in healthy young adults that is further delayed (half-time 75–95 min) in insulin-resistant obese and type 2 diabetic subjects (31, 64, 70, 73). Work from Bergman's laboratory subsequently demonstrated that, even at steady state during an insulin clamp, the muscle interstitial insulin concentration (as indexed by lymphatic insulin concentration) remains substantially lower than that of simultaneously sampled plasma (16, 117–119). This observation has been further confirmed in both human and experimental animal studies using microdialysis methods to directly sample interstitial fluid within muscle (36, 39, 40, 46, 93, 94). Finally, in a recent canine study it was observed that direct intramuscular injection of insulin resulted in a significantly more rapid onset of muscle glucose uptake compared with intravenous injection (19).
The finding that even after several hours of steady-state plasma hyperinsulinemia the interstitial insulin concentration remains at ∼50% of that in plasma suggests that a steady state is reached where insulin inflow to muscle interstitial fluid from plasma is matched by the disappearance of insulin through either lymphatic removal or its uptake and degradation, presumably within the muscle cell itself.
We have measured the rate of insulin transport into human forearm skeletal muscle both in the fasting state and during a euglycemic insulin clamp by combining arterial/venous sampling with measurements of forearm blood flow (28). These studies indicated that 10–15% of the insulin entering muscle with arterial plasma is removed in a single pass at fasting levels of insulin. Considering that the extracellular volume within skeletal muscle is ∼100 ml/kg (13) and resting skeletal muscle plasma flow is ∼18 ml·min−1·kg−1, it is readily appreciated that with a 10–15% extraction ratio it will require ∼50 min for the interstitial insulin concentration to reach 50% of arterial concentration. This assumes that none of the extracted insulin is degraded either during transit across the vessel wall or after reaching the muscle interstitium. Such a time agrees closely with the measured half-time for insulin's action on muscle glucose disposal noted above. At the present time, reliable measurements of insulin uptake/clearance by skeletal muscle in insulin-resistant humans and animals are not available. It would be anticipated that decreased microvascular perfusion, as we have observed in insulin-resistant humans and animals, could interfere with muscle insulin uptake.
During the studies above, we noted that when the insulin concentration was increased muscle insulin clearance declined. The latter suggests a saturable process for insulin transport. The question of whether insulin crossed the endothelium within muscle via a saturable process (presumably a process regulated by the endothelial cell) or via a nonsaturable diffusion-like process has been an area of some controversy. Below we will review information related to the general process of larger molecules crossing the endothelial barrier and how our understanding of this has evolved over the past two decades.
The endothelial architecture determines insulin's access to a tissue.
The fine structure of the vascular endothelium varies considerably within different vascular beds throughout the body (1). These structural differences impact the exchange of macromolecules between the plasma and tissue fluid. In the brain, for example, endothelial cells are joined by tight junctions, and there are very few caveolae (1). This may in part account for the very low rates of transport of large molecules into the brain and underlie the blood-brain barrier. At the opposite end of the spectrum, the liver has a discontinuous endothelium that includes gaps between endothelial cell membranes and a less well-developed basement membrane. This, combined with the high rate of blood flow to the liver (Fig. 1), may in part account for the rapid clearance of insulin by hepatic tissue (>50% single-pass extraction). This discontinuous endothelium allows for rapid exchange of both fluids and macromolecules between the two compartments. Skeletal muscle endothelium is somewhere in between those of brain and liver. It has a continuous endothelium with well-developed junctional structures. It also has abundant caveolae. Other tissues, for example the glomerular capillary bed of the kidney, have a fenestrated endothelium with discontinuities between endothelial cells bridged by a thin filamentous covering.
There are also differences in endothelial structure across a vascular bed within a given tissue. Thus, arterial and venous endothelial cells are more cuboidal than the very flattened endothelial cells of the capillary bed. Intercellular junctional structures are more developed on the arterial side of the circulation than are those of capillaries, and the venous endothelium has the least well-developed cell junctions. These structural differences impact the local movement of both macromolecules and cells across the endothelial barrier.
Transendothelial transit of macromolecules.
In the early 1950s, Pappenheimer described an empirically based model for the movement of molecules varying in size from single ions to macromolecules out of the vasculature (72). On the basis of measurements of diffusability of solutes of different sizes, he argued that a simple model postulating the presence of both small and large pores could satisfactorily account for most of the observed movement of molecules from the vasculature into the interstitial space. Anatomic sites assignable to these pores were not identified.
These estimates predate the elegant electron microscopic studies of Palade (74) and the Simonescus (92). Their work demonstrated the presence of junctional structures between endothelial cells in a number of tissues including skeletal muscle. They also noted that tissues like liver and gut had a less continuous endothelium with either fenestrations joining adjacent cells or with actual separation between endothelial cells having only a basement membrane separating the vascular and interstitial space. Palade was also among the first to describe caveolae. These 70- to 90-nm diameter flask-like vesicles are quite abundant in the vascular endothelium of a variety of tissues. Over several decades, investigators provided compelling electron microscopic evidence that caveolae or caveolae-like vesicles could mediate trans-cytosis of macromolecules labeled with electron-dense tracers. Importantly, capillary endothelium has been shown to have a higher density of caveolae than that of arteries, arterioles, veins, and venules (10).
The identification of caveolin-1 as a structural protein involved in the formation/stability of caveolae and the finding that transendothelial albumin transfer was impaired in the endothelium of caveolin-1 KO (KO) mice significantly advanced the argument that caveolae participate in transendothelial transport of macromolecules (85). Inasmuch as there is also anatomic evidence that caveolae can fuse and form multivesicular organelles, this fusion process might also lead to either transient or persistent “channels” that cross the very narrow cytosol of the vascular endothelium. Thus, it remains a viable consideration that transcellular channels could form something like the pore postulated by Pappenheimer.
Albumin as a prototype for the study of transendothelial transport.
The physiology as well as the cell and molecular biology of albumin transport across the vascular endothelium have been studied more intensively than that of any other macromolecule (63). As a 64-kDa protein with a Stoke's radius of ∼3.5 nm, it would, in the model of Pappenheimer, exit the vasculature through a large pore. However, when the movement of albumin was examined by electron microscopy, it was found that labeled albumin did not accumulate in the intercellular space, as might be expected had it crossed the endothelium by a paracellular pathway. Instead, labeled albumin was found within caveolae on the luminal side of the endothelium, within intracellular vesicles and seemingly being released from vesicles at the basolateral membrane. There was some accumulation of labeled albumin at the introitus to the intercellular space between endothelial cells, but the tracer did not appear to transit the junctional structure at the luminal side.
When similar studies were done in the vasculature of caveolin-1 KO mice, no vesicles akin to caveolae were identifiable in the endothelial cell, and the endothelial cell uptake of labeled albumin was greatly diminished (85). However, these KO mouse tissues develop leaky junctional structures in continuous endothelia. This also occurs when caveolin-1 is knocked down acutely using siRNA in vivo (66), indicating that caveolin-1 plays some regulatory role in maintaining junctional integrity (76). The leaky junctions seen in the caveolin-1 KO mice may be secondary to excess NO production (caveolin-1 is an endogenous inhibitor of eNOS), as treatment of the caveolin-1 KO mice with l-NAME reverses the microvascular hyperpermeability (86). There is other evidence that NO regulates the integrity of endothelial cell junctions as the vasculature of the eNOS KO mouse develops a paracellular leak of albumin, and this is also seen with acute infusions of the NOS inhibitor l-NAME (75).
Subsequent extensive and elegant work from the laboratories of Malik, Minshall, and Predescu and colleagues (53, 63, 77, 89) have substantially enhanced our understanding of the regulation of transendothelial albumin transport. First, it must be appreciated that this process appears to have several components. At low albumin concentrations, there is a specific high-affinity, relatively low-capacity receptor that binds albumin on the surface of the endothelial cell. This triggers a signaling process within the endothelial cell that involves an SRC-kinase that initiates the phosphorylation of caveolin-1 on a specific tyrosine residue (101) and leads to activation of a GTPase (dynamin 2) that is known to be involved in the scission of caveolae from the plasma membrane. In addition, a variety of proteins known to be involved in vesicle trafficking in other systems have been identified as associated with caveolae within the endothelial cell. This includes Snap 23, syntaxin-4, intersectin-s, and dynamin-2 (77, 79).
When the concentration of albumin on the luminal surface of the endothelial cell is low, this receptor-mediated transport process appears to be a major contributor to overall transendothelial transport. However, as the albumin concentration is raised into the range seen physiologically (∼0.4 mM), the bulk of albumin transport appears to occur via a fluid phase pinocytosis (48). This process also appears to involve caveolae.
Cellular vs. paracellular transendothelial transport in muscle: whither goes insulin?.
Early experimental support for a transcellular pathway of insulin movement across the endothelium was provided by the studies of King and Johnson (52). Using monolayers of vascular endothelial cells, they demonstrated that radioiodinated insulin movement across the endothelium could be blocked by unlabeled insulin as well as by an antibody against the insulin receptor. This suggested both that the process of insulin's movement across the endothelium was saturable and that the insulin receptor was involved in this process. Presumably, this involved a transcellular pathway. Some (84) but not all (65, 83) subsequent studies were able to duplicate these findings. Early evidence for a potential role of caveolae came from the finding that filipin, a sterol binding agent that disrupts caveolae but not clathrin-coated vesicles, inhibited transendothelial transport of both insulin and albumin but not the paracellular marker inulin (84). However, it is difficult to draw firm conclusions from these studies with endothelial monolayers, as endothelial cells in culture do not necessarily mimic the behavior of the endothelium in vivo. In particular, they do not appear to form as tight a cellular monolayer as exists within the vasculature.
Of concern were experiments performed in vivo in which insulin concentrations in the lymphatic fluid were sampled during a moderately or very-high-dose euglycemic insulin clamp (96). If insulin traversed the endothelium via a saturable receptor-mediated process, a decline in the ratio of interstitial to plasma insulin concentrations would be expected as plasma insulin concentration rose. If insulin passively leaked out of the vasculature, then the ratio should remain constant, as predicted by simple diffusion. Surprisingly, neither outcome was observed. Instead, the ratio of interstitial (lymphatic) to plasma insulin concentrations significantly increased at very high plasma insulin concentrations (96). This observation has not been satisfactorily explained. A potential explanation for this seemingly anomalous experimental observation is that at very high insulin concentrations transendothelial insulin transport was being mediated by both the IGF-I receptors. IGF-I receptors are present in greater abundance than the insulin receptors in the vascular endothelium (18). We subsequently showed (using insulin concentrations of 50 nM) that both IGF-I and antibody to the IGF-I receptor could block uptake and transendothelial movement of insulin across a monolayer composed of bovine aortic endothelial cells (107). This suggested that when insulin was present at sufficiently high concentrations the IGF-I receptor could mediate insulin transport.
Interestingly, another laboratory has measured the movement of 125I-labeled IGF-I across a monolayer composed of human umbilical vein endothelial cells (9). In that preparation, neither antibody to the IGF-I receptor nor unlabeled IGF-I interfered with movement of the labeled IGF-I across the monolayer. Furthermore, the rates of transport appeared similar for IGF-I and inulin (the latter was used as a marker for paracellular transport processes). Those investigators concluded that IGF-I passage across the endothelium occurred by passive diffusion through a paracellular pathway. This suggests that the type of endothelial cell used for these in vitro assays may influence the outcome. In particular, venous endothelia are generally known to be leakier than arterial endothelia.
Given that the rate of insulin entry into skeletal muscle interstitium appears to be the rate-limiting step for skeletal muscle insulin action, we thought it was important to reinvestigate whether insulin crossed the endothelium by a transcellular or a paracellular pathway. We have taken several approaches to evaluate this question and believe our studies have in the aggregate begun to define a complex pathway of insulin transendothelial transport.
First, we investigated in vivo whether insulin entered the endothelial cell (107). To accomplish this, we used a fluorescent-labeled insulin that maintains biological activity. This was infused intravenously in an overnight-fasted rat to reach concentrations sufficient to promote glucose disposal while maintaining euglycemia (insulin clamp). We then obtained serial biopsies of skeletal muscle that were rapidly fixed and examined by confocal microscopy. We found that within 10 min there was a striking localization of insulin in the endothelium. We could find no evidence for fluorescent-tagged insulin entering the muscle interstitium between endothelial cells via the intercellular junctions.
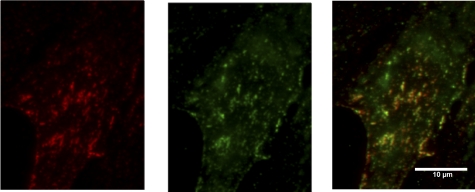
In that same study, using cultured bovine aortic endothelial cells (107), we addressed whether insulin, when taken up by the vascular endothelial cell, was associated with insulin receptors and whether it was discretely or diffusely localized within the endothelial cell. We took advantage of the ability of confocal microscopy to optically section through the endothelial cell, and using a fluorescent-tagged insulin allowed us to identify insulin within the endothelial cell as opposed to on the endothelial cell surface. Not only did we observe colocalization between insulin and the insulin receptor, but both colocalized with caveolin-1. Furthermore, coimmunoprecipitation experiments indicated physical juxtaposition of the insulin receptor and caveolin-1. As caveolae had already been implicated in the transcytosis of albumin and other proteins, we considered that these vesicular structures might also be important mediators of transendothelial insulin transport. More recently, we have used total internal reflectance fluorescence microscopy (TIRF-M) to address whether insulin receptor and caveolin-1 colocalize on the endothelial cell plasma membrane. Figure 3 illustrates this colocalization. The TIRF-M images are focused within 80 nM of the cell surface, providing better assessment of caveolin-insulin receptor interactions in that specific cell domain. We observed very extensive overlap between caveolin-1 and insulin receptor immunoreactivity (Upchurch, unpublished data). Interestingly, in 3T3-L1 cells, Foti et al. (30) have reported specific localization of the insulin receptor to the neck of caveolae by using electron microscopy with immunogold labeling.
Fig. 3.
Endothelial cell stained for cavelolin-1 (left), the insulin receptor (middle), and the overlay (right).
A note of caution with regard to these experiments using fluorescent-labeled insulin is that the sensitivity for measuring transport of the fluorescent tag requires the use of relatively high insulin concentrations (typically 10–100 nM). In addition, although the confocal microscopy of skeletal muscle biopsies clearly demonstrated intense cytoplasmic staining of insulin within the endothelial cell during its transendothelial transport, it was not possible to demonstrate colocalization of either insulin or insulin receptor with caveolae in these in vivo experiments. Whether the findings in the cultured endothelial cells translate directly to the in vivo circumstance is not yet resolved.
As the experiments above suggested that a cellular pathway involving the insulin receptor could be mediating insulin's transendothelial transport in muscle in vivo, we reexamined this in a series of in vivo experiments and in endothelial cell cultures. The in vivo experiments were performed both in rats and in humans. First, we took advantage of the observation made a number of years ago that the uptake of insulin by skeletal muscle could be measured in vivo in humans by using an arterial-venous sampling (49) . We found that, in postabsorptive humans, by using brachial artery and deep forearm vein sampling, the extraction ratio for insulin across the forearm ranged from 10 to 15% (28). After obtaining basal measurements of forearm insulin uptake, we raised plasma insulin concentrations using the euglycemic insulin clamp method. Although insulin uptake increased, it did not increase in proportion to the rise in arterial insulin concentration (as would be predicted for a diffusional process). Instead, the extraction ratio and clearance for insulin by forearm muscle declined. This was indicative of a saturable process within the physiological range of insulin concentrations.
A limitation to this type of study is that measurements were made at steady state after several hours of hyperinsulinemia. This rendered it difficult to address whether the decline in tissue uptake was secondary to a process occurring at the endothelium or a limitation to insulin uptake by the myocyte. However, as discussed above, even after several hours of hyperinsulinemia, the insulin concentration in the muscle interstitium did not approach plasma concentrations. This would suggest that transport by the endothelium is in fact the limiting process and responsible for the decline in insulin clearance as insulin concentration increases (28).
Subsequently, we addressed directly the uptake of 125I-insulin by rat hindlimb skeletal muscle after only 5 min of exposure to labeled insulin. We reasoned that the very initial stages of muscle 125I-insulin uptake would be dominated by the behavior of the endothelium. This initial uptake of labeled insulin was measured in the presence and absence of a high concentration of unlabeled insulin. The latter was given either as a bolus simultaneously with the 125I-insulin or as a 90-min high-dose euglycemic insulin clamp, with the 125I-insulin given during the last 5 min. In both circumstances, the unlabeled insulin significantly diminished the clearance of the labeled insulin. This finding is again consistent with a competitive process whereby unlabeled insulin decreases the uptake of the 125I-insulin and suggests involvement of the insulin receptor (Majumdar S, Genders A, and Barrett EJ., unpublished data).
We next examined transendothelial transport of 50 nM fluorescent-tagged insulin by using cultured bovine aortic endothelial cells grown on a Transwell device. We found that the transendothelial transport of fluorescent-tagged insulin was inhibited not only by unlabeled insulin but also by by IGF-I and by an antibody against the extracellular domain of the IGF-I receptor. We also confirmed that both filipin and β-methylcyclodextrin (which disrupt caveolae) inhibited endothelial cell insulin uptake (107).
Does insulin transport require insulin action?.
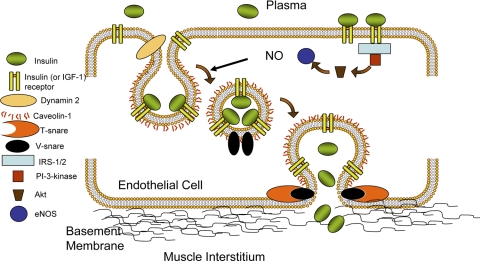
We were intrigued by the observation that when albumin was present at low concentrations its uptake was dependent on both its binding to a specific receptor (Gp60) (101) and its activation of a kinase cascade that ultimately resulted in the phosphorylation of Tyr14 on caveolin-1. This prompted us to address whether insulin uptake by the endothelial cell required not only insulin binding to its receptor but also activating insulin signaling processes within the endothelial cell. As noted earlier, a great deal of work has demonstrated that insulin acts on the endothelial cell and can promote the release of both the vasodilator NO and the vasoconstrictor endothelin-1 (15). The release of NO results from the phosphorylation of a specific serine (Ser1177) residue in eNOS that increases enzyme activity in a calcium-independent fashion (67). The phosphatidylinositol 3-kinase (PI 3-kinase)/protein kinase B (PKB or Akt) pathway appears to be responsible for this, with Akt being able to directly phosphorylate Ser1177 (121). Alternatively, the increase in endothelin-1 is secondary to a transcriptional regulation mediated via the extracellular signal-regulated kinases (ERK) pathway. It has been suggested that selective insulin resistance involving the PI 3-kinase/Akt pathway could tip the balance of insulin's vascular actions from a predominantly vasodilatory to a vasoconstrictor profile (47, 51).
We had previously found that culturing endothelial cells in serum-free media for 16 h enhanced our ability to detect insulin-mediated activation of Akt, eNOS, and ERK1/2 at physiological concentrations of insulin (58). Using cells cultured in this fashion, we examined the impact of inhibiting insulin action via the PI 3-kinase pathway (wortmannin), the ERK pathway (PD-98059), and the cSRC-kinase (PP1) as well as the effect of a general tyrosine kinase inhibitor (genistein) on the uptake of insulin by the endothelial cell. Each of these interfered with endothelial cell insulin uptake significantly. Conversely, inhibiting protein tyrosine phosphatase-1B enhanced endothelial cell insulin uptake (109). In aggregate, these findings suggested that insulin's action on the endothelial cell was required for insulin to be taken into the cell. Interestingly, while the NOS inhibitor l-NAME blocked endothelial uptake of insulin, providing sodium nitroprusside (NO donor) was able to at least partially overcome the inhibitory effect of wortmannin, PD-98059, and PP1 on insulin uptake. More recently, we have found that siRNA knockdown of caveolin-1 also substantially decreased uptake of insulin by the endothelial cell, further supporting a role for vesicle-mediating insulin transport (108).
A significant concern with regard to insulin playing a role in modulating its own delivery to skeletal muscle interstitium was raised by the demonstration that specific deletion of the insulin receptor from endothelial cells using Cre-recombinase driven by the Tie-2 promoter did not appear to affect body glucose metabolism under normal dietary conditions (103). Likewise, the global eNOS KO mouse is only mildly insulin resistant (90). In both cases, no measurements of vascular function were made in those studies (either microvascular recruitment or insulin transport), and the insulin dosage used for the insulin clamp procedure to assess insulin sensitivity was relatively high. This raised the question of whether activation of the IGF-I receptor by insulin might be compensating for the insulin receptor deficiency (107). A very recent study (54) reexamined this issue with an endothelial-specific IRS-2 KO mouse. Unlike the previous studies, in this mouse, vascular function and insulin delivery were carefully studied. This mouse was insulin resistant, failed to recruit microvasculature in response to an insulin challenge, and demonstrated impaired delivery of 125I-labeled insulin into skeletal muscle. This suggested that downstream insulin signaling within the endothelium was important for both normal glucose homeostasis and vascular responsiveness. This was further indicated by the observation that restoration of downstream insulin signaling to eNOS in the endothelium corrected the insulin resistance as well as microvascular function within the muscle. The lack of frank diabetes in this murine model is perhaps not surprising, as it is known that even muscle-specific knockout of the insulin receptor resulted in a phenotypic pattern consistent with the metabolic syndrome without even glucose intolerance.
Impact of insulin resistance on insulin transendothelial transport in cultured endothelial cells.
As noted earlier, the onset of insulin action during a euglycemic insulin clamp is delayed in insulin resistance states like obesity and type 2 diabetes. As the insulin action time course appears to be determined by insulin's transendothelial transport, the question arises whether insulin resistance interferes with the endothelial transport of insulin. We have observed that the cytokine TNF-α interferes with insulin signaling within the endothelial cell, and this is in part due to activation of p38 MAP kinase. We have also observed that both TNF-α and IL-6 are able to diminish the uptake of insulin by the endothelial cell. Both also interfere with NO generation and with insulin-induced caveolin-1 translocation to the plasma membrane in the endothelial cell (108). These observations suggest that these and perhaps other inflammatory cytokines may exert part of their action to provoke insulin resistance by acting directly on the endothelial cell.
The action of cytokines like TNF-α and IL-6 to provoke vascular insulin resistance may be particularly pertinent when they are produced locally in the region of the muscle microvasculature. Studies focusing on perivascular adipose tissue within muscle suggest that adipocyte-derived cytokines acting locally may influence the balance between NO and endothelin-1 production in favor of endothelin-1 (3, 29). This could impair microvascular perfusion and/or transendothelial insulin transport within the muscle tissue.
Current model for insulin transendothelial transport in continuous endothelia.
We close with a working model that we are using to test hypotheses regarding the cellular dynamics of insulin transendothelial transport (Fig. 4). Considerable in vivo and in vitro data indicate that insulin transits the endothelium in association with the insulin receptor. As noted above, this process requires not only receptor binding but activation of several protein kinase cascades downstream of insulin signaling. A significant fraction of the insulin receptor in endothelial cells appears to be associated with caveolae, and these vesicular structures are necessary for endothelial cell insulin uptake and transendothelial transport. This vesicle trafficking process may also be dependent on the cytoskeletal structure of the endothelial cell; in particular, microfilaments and/or microtubules may be involved in the transcellular movement of the insulin-containing vesicles. Dynamin-2 GTPase activity is required for separating caveolae from the plasma membrane, and we found that knockdown of dynamin-2 inhibits endothelial cell insulin uptake (H. Wang, unpublished observation).
Fig. 4.
Working model for transendothelial insulin transport.
We emphasize that Fig. 4 is simply a working model that affords the opportunity to test hypotheses related to the cellular mechanics of insulin transport. A great deal more work needs to be done to understand the regulation of this process in vivo. We have learned a good deal from cultured cell systems, and we are hopeful that they will continue to provide a faithful pathway to explore insulin's vascular regulation in clinically relevant settings. Clearly, in the future it will be important to develop methods that allow testing multiple aspects of this model in a more physiological setting and eventually in clinical studies. If the model proposed has validity, it has broad implications for understanding skeletal muscle insulin resistance. It would indicate that the endothelium becomes important as a potential therapeutic target for the development of pharmaceutical agents that improve insulin resistance. The fact that endothelial insulin resistance impacts skeletal muscle glucose metabolism underscores the contribution of the endothelium to metabolic insulin resistance. Insulin resistance in the vasculature may also be contributing to the multiple vasculopathies encountered in diabetes from the microvascular pathology seen in retinopathy, neuropathy, and nephropathy right up to the accelerated atherosclerosis in large and medium-size arteries.
GRANTS
This work was supported by American Diabetes Association grants 1-11-BS-06 (to E. J. Barrett),1-11-CR-30 and 9-09-NOVO-11 (to Z. Liu), and National Institutes of Health Grants R01 DK-057878 and R01 DK-073759 (to E. J. Barrett) and R01 HL-094722 (to Z. Liu).
DISCLOSURES
No conflicts of interest, financial or otherwise, are declared by the author(s).
REFERENCES
- 1.Aird WC. Phenotypic heterogeneity of the endothelium. II. Representative vascular beds. Circ Res 100: 174–190, 2007 [DOI] [PubMed] [Google Scholar]
- 2.Anfossi G, Russo I, Doronzo G, Trovati M. Contribution of insulin resistance to vascular dysfunction. Arch Physiol Biochem 115: 199–217, 2009 [DOI] [PubMed] [Google Scholar]
- 3.Bakker W, Sipkema P, Stehouwer CD, Serne EH, Smulders YM, van Hinsbergh VW, Eringa EC. Protein kinase C theta activation induces insulin-mediated constriction of muscle resistance arteries. Diabetes 57: 706–713, 2008 [DOI] [PubMed] [Google Scholar]
- 4.Baron A. Hemodynamic actions of insulin. Am J Physiol Endocrinol Metab 267: E187–E202, 1994 [DOI] [PubMed] [Google Scholar]
- 5.Baron AD, Laakso M, Brechtel G, Edelman SV. Mechanism of insulin resistance in insulin-dependent diabetes mellitus: a major role for reduced skeletal muscle blood flow. J Clin Endocrinol Metab 73: 637–643, 1991 [DOI] [PubMed] [Google Scholar]
- 6.Baron AD, Laakso M, Brechtel G, Hoit B, Watt C, Edelman SV. Reduced postprandial skeletal muscle blood flow contributes to glucose intolerance in human obesity. J Clin Endocrinol Metab 70: 1525–1533, 1990 [DOI] [PubMed] [Google Scholar]
- 7.Baron AD, Steinberg HO, Chaker H, Learning R, Johnson A, Brechtel G. Insulin-mediated skeletal muscle vasodilation contributes to both insulin sensitivity and responsiveness in lean humans. J Clin Invest 96: 786–792, 1995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Barrett EJ, Eggleston EM, Inyard AC, Wang H, Li G, Chai W, Liu Z. The vascular actions of insulin control its delivery to muscle and regulate the rate-limiting step in skeletal muscle insulin action. Diabetologia 52: 752–764, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bastian SE, Walton PE, Belford DA. Paracellular transport of insulin-like growth factor-I (IGF-I) across human umbilical vein endothelial cell monolayers. J Cell Physiol 170: 290–298, 1997 [DOI] [PubMed] [Google Scholar]
- 10.Bendayan M. Morphological and cytochemical aspects of capillary permeability. Microsc Res Tech 57: 327–349, 2002 [DOI] [PubMed] [Google Scholar]
- 11.Bertoldo A, Pencek RR, Azuma K, Price JC, Kelley C, Cobelli C, Kelley DE. Interactions between delivery, transport, and phosphorylation of glucose in governing uptake into human skeletal muscle. Diabetes 55: 3028–3037, 2006 [DOI] [PubMed] [Google Scholar]
- 12.Bertoldo A, Price J, Mathis C, Mason S, Holt D, Kelley C, Cobelli C, Kelley DE. Quantitative assessment of glucose transport in human skeletal muscle: dynamic positron emission tomography imaging of [O-methyl-11C]3-O-methyl-d-glucose. J Clin Endocrinol Metab 90: 1752–1759, 2005 [DOI] [PubMed] [Google Scholar]
- 13.Bonadonna RC, Saccomani MP, Delprato S, Bonora E, Defronzo RA, Cobelli C. Role of tissue-specific blood flow and tissue recruitment in insulin-mediated glucose uptake of human skeletal muscle. Circulation 98: 234–241, 1998 [DOI] [PubMed] [Google Scholar]
- 14.Buchanan TA, Thawani H, Kades W, Modrall JG, Weaver FA, Laurel C, Poppiti R, Xiang A, Hsueh W. Angiotensin II increases glucose utilization during acute hyperinsulinemia via a hemodynamic mechanism. J Clin Invest 92: 720–726, 1993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cardillo C, Nambi SS, Kilcoyne CM, Choucair WK, Katz A, Quon MJ, Panza JA. Insulin stimulates both endothelin and nitric oxide activity in the human forearm. Circulation 100: 820–825, 1999 [DOI] [PubMed] [Google Scholar]
- 16.Castillo C, Bogardus C, Bergman R, Thuillez P, Lillioja S. Interstitial insulin concentrations determine glucose uptake rates but not insulin resistance in lean and obese men. J Clin Invest 93: 10–16, 1994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chai W, Wang W, Liu J, Barrett EJ, Carey RM, Cao W, Liu Z. Angiotensin II type 1 and type 2 receptors regulate basal skeletal muscle microvascular volume and glucose use. Hypertension 55: 523–530, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chisalita SI, Arnqvist HJ. Insulin-like growth factor I receptors are more abundant than insulin receptors in human micro- and macrovascular endothelial cells. Am J Physiol Endocrinol Metab 286: E896–E901, 2004 [DOI] [PubMed] [Google Scholar]
- 19.Chiu JD, Richey JM, Harrison LN, Zuniga E, Kolka CM, Kirkman E, Ellmerer M, Bergman RN. Direct administration of insulin into skeletal muscle reveals that the transport of insulin across the capillary endothelium limits the time course of insulin to activate glucose disposal. Diabetes 57: 828–835, 2008 [DOI] [PubMed] [Google Scholar]
- 20.Clark ADH, Barrett EJ, Rattigan S, Wallis MG, Clark MG. Insulin stimulates laser Doppler signal by rat muscle in vivo consistent with nutritive flow recruitment. Clin Sci 100: 283–290, 2001 [PubMed] [Google Scholar]
- 21.Clark MG. Impaired microvascular perfusion: a consequence of vascular dysfunction and a potential cause of insulin resistance in muscle. Am J Physiol Endocrinol Metab 295: E732–E750, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Clark MG, Rattigan S, Barrett EJ, Vincent MA. Point:Counterpoint: There is/is not capillary recruitment in active skeletal muscle during exercise. J Appl Physiol 104: 889–891, 2008 [DOI] [PubMed] [Google Scholar]
- 23.Clerk LH, Vincent MA, Barrett EJ, Lankford MF, Lindner JR. Skeletal muscle capillary responses to insulin are abnormal in late-stage diabetes and are restored by angiogensin-converting enzyme inhibition. Am J Physiol Endocrinol Metab 293: E1804–E1809, 2007 [DOI] [PubMed] [Google Scholar]
- 24.Clerk LH, Vincent MA, Jahn LA, Liu Z, Lindner JR, Barrett EJ. Obesity blunts insulin-mediated microvascular recruitment in human forearm muscle. Diabetes 55: 1436–1442, 2006 [DOI] [PubMed] [Google Scholar]
- 25.Coggins MP, Lindner J, Rattigan S, Fasy E, Jahn L, Kaul S, Barrett EJ. Physiologic hyperinsulinemia enhances human skeletal muscle perfusion by capillary recruitment. Diabetes 50: 2682–2690, 2001 [DOI] [PubMed] [Google Scholar]
- 26.de Jongh RT, Ijzerman RG, Serne EH, Voordouw JJ, Yudkin JS, de Waal HA, Stehouwer CD, van Weissenbruch MM. Visceral and truncal subcutaneous adipose tissue are associated with impaired capillary recruitment in healthy individuals. J Clin Endocrinol Metab 91: 5100–5106, 2006 [DOI] [PubMed] [Google Scholar]
- 27.de Jongh RT, Serne EH, RGIJ, de Vries G, Stehouwer CD. Impaired microvascular function in obesity: implications for obesity-associated microangiopathy, hypertension, and insulin resistance. Circulation 109: 2529–2535, 2004 [DOI] [PubMed] [Google Scholar]
- 28.Eggleston EM, Jahn LA, Barrett EJ. Hyperinsulinemia rapidly increases human muscle microvascular perfusion but fails to increase muscle insulin clearance: evidence that a saturable process mediates muscle insulin uptake. Diabetes 56: 2958–2963, 2007 [DOI] [PubMed] [Google Scholar]
- 29.Eringa EC, Bakker W, Smulders YM, Serne EH, Yudkin JS, Stehouwer CD. Regulation of vascular function and insulin sensitivity by adipose tissue: focus on perivascular adipose tissue. Microcirculation 14: 389–402, 2007 [DOI] [PubMed] [Google Scholar]
- 30.Foti M, Porcheron G, Fournier M, Maeder C, Carpentier JL. The neck of caveolae is a distinct plasma membrane subdomain that concentrates insulin receptors in 3T3-L1 adipocytes. Proc Natl Acad Sci USA 104: 1242–1247, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Freidenberg GR, Suter S, Henry RR, Nolan J, Reichart D, Olefsky JM. Delayed onset of insulin activation of the insulin receptor kinase in vivo in human skeletal muscle. Diabetes 43: 118–126, 1994 [DOI] [PubMed] [Google Scholar]
- 32.Fryburg DA. Insulin-like growth factor I exerts growth hormone- and insulin-like actions on human muscle protein metabolism. Am J Physiol Endocrinol Metab 267: E331–E336, 1994 [DOI] [PubMed] [Google Scholar]
- 33.Fryburg DA, Jahn LA, Hill SA, Oliveras DM, Barrett EJ. Insulin and insulin-like growth factor-I enhance human skeletal muscle protein anabolism during hyperaminoacidemia by different mechanisms. J Clin Invest 96: 1722–1729, 1995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fryburg DA, Louard RJ, Gerow KE, Gelfand RA, Barrett EJ. Growth hormone stimulates skeletal muscle protein synthesis and blunts insulin's antiproteolytic action in humans. Diabetes 41: 424–429, 1992 [DOI] [PubMed] [Google Scholar]
- 35.Fugmann A, Sarabi M, Karlstrom B, Berne C, Lithell H, Lind L. Blood flow is an important determinant of forearm glucose uptake following a mixed meal. Acta Diabetol 40: 113–117, 2003 [DOI] [PubMed] [Google Scholar]
- 36.Gudbjornsdottir S, Sjostrand M, Strindberg L, Wahren J, Lonnroth P. Direct measurements of the permeability surface area for insulin and glucose in human skeletal muscle. J Clin Endocrinol Metab 88: 4559–4564, 2003 [DOI] [PubMed] [Google Scholar]
- 37.Hernandez Mijares A, Jensen MD. Contribution of blood flow to leg glucose uptake during a mixed meal. Diabetes 44: 1165–1169, 1995 [DOI] [PubMed] [Google Scholar]
- 38.Hogikyan RV, Galecki AT, Pitt B, Halter JB, Greene DA, Supiano MA. Specific impairment of endothelium-dependent vasodilation in subjects with type 2 diabetes independent of obesity. J Clin Endocrinol Metab 83: 1946–1952, 1998 [DOI] [PubMed] [Google Scholar]
- 39.Holmang A, Mimura K, Bjorntorp P, Lonnroth P. Interstitial muscle insulin and glucose levels in normal and insulin-resistant Zucker rats. Diabetes 46: 1799–1804, 1997 [DOI] [PubMed] [Google Scholar]
- 40.Holmang A, Niklasson M, Rippe B, Lonnroth P. Insulin insensitivity and delayed transcapillary delivery of insulin in oophorectomized rats treated with testosterone. Acta Physiol Scand 171: 427–438, 2001 [DOI] [PubMed] [Google Scholar]
- 41.Honig CR, Odoroff CL, Frierson JL. Active and passive capillary control in red muscle at rest and in exercise. Am J Physiol Heart Circ Physiol 243: H196–H206, 1982 [DOI] [PubMed] [Google Scholar]
- 42.Honig CR, Odoroff CL, Frierson JL. Capillary recruitment in exercise: rate, extent, uniformity, and relation to blood flow. Am J Physiol Heart Circ Physiol 238: H31–H42, 1980 [DOI] [PubMed] [Google Scholar]
- 43.Hoost U, Kelbaek H, Rasmusen H, Court-Payen M, Christensen NJ, Pedersen-Bjergaard U, Lorenzen T. Haemodynamic effects of eating: the role of meal composition. Clin Sci (Lond) 90: 269–276, 1996 [DOI] [PubMed] [Google Scholar]
- 44.Inyard AC, Clerk LH, Vincent MA, Barrett EJ. Contraction stimulates nitric oxide independent microvascular recruitment and increases muscle insulin uptake. Diabetes 56: 2194–2000, 2007 [DOI] [PubMed] [Google Scholar]
- 45.Iwase M, Tashiro K, Uchizono Y, Goto D, Yoshinari M. Pancreatic islet blood flow in conscious rats during hyperglycemia and hypoglycemia. Am J Physiol Regul Integr Comp Physiol 280: R1601–R1605, 2001 [DOI] [PubMed] [Google Scholar]
- 46.Jansson PA, Fowelin JP, von Schenck HP, Smith UP, Lonnroth PN. Measurement by microdialysis of the insulin concentration in subcutaneous interstitial fluid. Importance of the endothelial barrier for insulin. Diabetes 42: 1469–1473, 1993 [DOI] [PubMed] [Google Scholar]
- 47.Jiang ZY, Lin YW, Clemont A, Feener EP, Hein KD, Igarashi M, Yamauchi T, White MF, King GL. Characterization of selective resistance to insulin signaling in the vasculature of obese Zucker (fa/fa) rats. J Clin Invest 104: 447–457, 1999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.John TA, Vogel SM, Tiruppathi C, Malik AB, Minshall RD. Quantitative analysis of albumin uptake and transport in the rat microvessel endothelial monolayer. Am J Physiol Lung Cell Mol Physiol 284: L187–L196, 2003 [DOI] [PubMed] [Google Scholar]
- 49.Kalant N, Leibovici T, Rohan I, Ozaki S. Interrelationships of glucose and insulin uptake by muscle of normal and diabetic man. Evidence of a difference in metabolism of endogenous and exogenous insulin. Diabetologia 16: 365–372, 1979 [DOI] [PubMed] [Google Scholar]
- 50.Keske MA, Clerk LH, Price WJ, Jahn LA, Barrett EJ. Obesity blunts microvascular recruitment in human forearm muscle after a mixed meal. Diabetes Care 32: 1672–1677, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kim JA, Montagnani M, Koh KK, Quon MJ. Reciprocal relationships between insulin resistance and endothelial dysfunction: molecular and pathophysiological mechanisms. Circulation 113: 1888–1904, 2006 [DOI] [PubMed] [Google Scholar]
- 52.King GL, Johnson SM. Receptor-mediated transport of insulin across endothelial cells. Science 227: 1583–1586, 1985 [DOI] [PubMed] [Google Scholar]
- 53.Komarova YA, Mehta D, Malik AB. Dual regulation of endothelial junctional permeability. Sci STKE 2007: re8, 2007 [DOI] [PubMed] [Google Scholar]
- 54.Kubota T, Kubota N, Kumagai H, Yamaguchi S, Kozono H, Takahashi T, Inoue M, Itoh S, Takamoto I, Sasako T, Kumagai K, Kawai T, Hashimoto S, Kobayashi T, Sato M, Tokuyama K, Nishimura S, Tsunoda M, Ide T, Murakami K, Yamazaki T, Ezaki O, Kawamura K, Masuda H, Moroi M, Sugi K, Oike Y, Shimokawa H, Yanagihara N, Tsutsui M, Terauchi Y, Tobe K, Nagai R, Kamata K, Inoue K, Kodama T, Ueki K, Kadowaki T. Impaired insulin signaling in endothelial cells reduces insulin-induced glucose uptake by skeletal muscle. Cell Metab 13: 294–307 [DOI] [PubMed] [Google Scholar]
- 55.Laakso M, Edelman SV, Brechtel G, Baron AD. Decreased effect of insulin to stimulate skeletal muscle blood flow in obese man. J Clin Invest 85: 1844–1852, 1990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Laakso M, Edelman SV, Brechtel G, Baron AD. Impaired insulin-mediated skeletal muscle blood flow in patients with NIDDM. Diabetes 41: 1076–1083, 1992 [DOI] [PubMed] [Google Scholar]
- 57.Laine H, Yki-Jarvinen H, Kirvela O, Tolvanen T, Raitakari M, Solin O, Haaparanta M, Knuuti J, Nuutila P. Insulin resistance of glucose uptake in skeletal muscle cannot be ameliorated by enhancing endothelium-dependent blood flow in obesity. J Clin Invest 101: 1156–1162, 1998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Li G, Barrett EJ, Wang H, Chai W, Liu Z. Insulin at physiological concentrations selectively activates insulin but not insulin-like growth factor I (IGF-I) or insulin/IGF-I hybrid receptors in endothelial cells. Endocrinology 146: 4690–4696, 2005 [DOI] [PubMed] [Google Scholar]
- 59.Li G, Del Rincon JP, Jahn LA, Wu Y, Gaylinn B, Thorner MO, Liu Z. Growth hormone exerts acute vascular effects independent of systemic or muscle insulin-like growth factor I J Clin Endocrinol Metab 93: 1379–1385, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Liu J, Jahn LA, Fowler DE, Barrett EJ, Cao W, Liu Z. Free fatty acids induce insulin resistance in both cardiac and skeletal muscle microvasculature in humans. J Clin Endocrinol Metab 96: 438–446, [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Liu Z. Insulin at physiological concentrations increases microvascular perfusion in human myocardium. Am J Physiol Endocrinol Metab 293: E1250–E1255, 2007 [DOI] [PubMed] [Google Scholar]
- 62.Liu Z, Liu J, Jahn LA, Fowler DE, Barrett EJ. Infusing lipid raises plasma free fatty acids and induces insulin resistance in muscle microvasculature. J Clin Endocrinol Metab 94: 3543–3549, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Mehta D, Malik AB. Signaling mechanisms regulating endothelial permeability. Physiol Rev 86: 279–367, 2006 [DOI] [PubMed] [Google Scholar]
- 64.Miles PD, Levisetti M, Reichart D, Khoursheed M, Moossa AR, Olefsky JM. Kinetics of insulin action in vivo. Identification of rate-limiting steps. Diabetes 44: 947–953, 1995 [DOI] [PubMed] [Google Scholar]
- 65.Milton SG, Knutson VP. Comparison of the function of the tight junctions of endothelial cells and epithelial cells in regulating the movement of electrolytes and macromolecules across the cell monolayer. J Cell Physiol 144: 498–504, 1990 [DOI] [PubMed] [Google Scholar]
- 66.Miyawaki-Shimizu K, Predescu D, Shimizu J, Broman M, Predescu S, Malik AB. siRNA-induced caveolin-1 knockdown in mice increases lung vascular permeability via the junctional pathway. Am J Physiol Lung Cell Mol Physiol 290: L405–L413, 2006 [DOI] [PubMed] [Google Scholar]
- 67.Montagnani M, Chen H, Barr VA, Quon MJ. Insulin-stimulated activation of eNOS is independent of Ca2+ but requires phosphorylation by Akt at Ser (1179). J Biol Chem 276: 30392–30398, 2001 [DOI] [PubMed] [Google Scholar]
- 68.Muniyappa R, Montagnani M, Koh KK, Quon MJ. Cardiovascular actions of insulin. Endocr Rev 28: 463–491, 2007 [DOI] [PubMed] [Google Scholar]
- 69.Natali A, Quinones Galvan A, Pecori N, Sanna G, Toschi E, Ferrannini E. Vasodilation with sodium nitroprusside does not improve insulin action in essential hypertension. Hypertension 31: 632–636, 1998 [DOI] [PubMed] [Google Scholar]
- 70.Nolan JJ, Ludvik B, Baloga J, Reichart D, Olefsky JM. Mechanisms of the kinetic defect in insulin action in obesity and NIDDM. Diabetes 46: 994–1000, 1997 [DOI] [PubMed] [Google Scholar]
- 71.Nuutila P, Raitakari M, Laine H, Kirvela O, Takala T, Utrlainen T, Makimattila S, Pitkanen O, Routsalainen U, Lida H, Knuuti J, Yki-Jarvinen H. Role of blood flow in regulating insulin-stimulated glucose uptake in humans: studies using bradykinin, [15O]water, and [18F]fluoro-deoxy-glucose and positron emission tomagraphy. J Clin Invest 97: 1741–1747, 1996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Pappenheimer J. Passage of molecules trhough capillary walls. Physiol Rev 33: 387–423, 1953 [DOI] [PubMed] [Google Scholar]
- 73.Prager R, Wallace P, Olefsky JM. In vivo kinetics of insulin action on peripheral glucose disposal and hepatic glucose output in normal and obese subjects. J Clin Invest 78: 472–481, 1986 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Predescu D, Palade GE. Plasmalemmal vesicles represent the large pore system of continuous microvascular endothelium. Am J Physiol Heart Circ Physiol 265: H725–H733, 1993 [DOI] [PubMed] [Google Scholar]
- 75.Predescu D, Predescu S, Shimizu J, Miyawaki-Shimizu K, Malik AB. Constitutive eNOS-derived nitric oxide is a determinant of endothelial junctional integrity. Am J Physiol Lung Cell Mol Physiol 289: L371–L381, 2005 [DOI] [PubMed] [Google Scholar]
- 76.Predescu D, Vogel SM, Malik AB. Functional and morphological studies of protein transcytosis in continuous endothelia. Am J Physiol Lung Cell Mol Physiol 287: L895–L901, 2004 [DOI] [PubMed] [Google Scholar]
- 77.Predescu SA, Predescu DN, Malik AB. Molecular determinants of endothelial transcytosis and their role in endothelial permeability. Am J Physiol Lung Cell Mol Physiol 293: L823–L842, 2007 [DOI] [PubMed] [Google Scholar]
- 79.Predescu SA, Predescu DN, Shimizu K, Klein IK, Malik AB. Cholesterol-dependent syntaxin-4 and SNAP-23 clustering regulates caveolar fusion with the endothelial plasma membrane. J Biol Chem 280: 37130–37138, 2005 [DOI] [PubMed] [Google Scholar]
- 80.Preik M, Kelm M, Rosen P, Tschope D, Strauer BE. Additive effect of coexistent type 2 diabetes and arterial hypertension on endothelial dysfunction in resistance arteries of human forearm vasculature. Angiology 51: 545–554, 2000 [DOI] [PubMed] [Google Scholar]
- 81.Rask-Madsen C, Li Q, Freund B, Feather D, Abramov R, Wu IH, Chen K, Yamamoto-Hiraoka J, Goldenbogen J, Sotiropoulos KB, Clermont A, Geraldes P, Dall'Osso C, Wagers AJ, Huang PL, Rekhter M, Scalia R, Kahn CR, King GL. Loss of insulin signaling in vascular endothelial cells accelerates atherosclerosis in apolipoprotein E null mice. Cell Metab 11: 379–389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Rattigan S, Clark MG, Barrett EJ. Hemodynamic actions of insulin in rat skeletal muscle: Evidence for capillary recruitment. Diabetes 46: 1381–1388, 1997 [DOI] [PubMed] [Google Scholar]
- 83.Salvetti F, Cecchetti P, Janigro D, Lucacchini A, Benzi L, Martini C. Insulin permeability across an in vitro dynamic model of endothelium. Pharm Res 19: 445–450, 2002 [DOI] [PubMed] [Google Scholar]
- 84.Schnitzer JE, Oh P, Pinney E, Allard J. Filipin-sensitive caveolae-mediated transport in endothelium: reduced transcytosis, scavenger endocytosis, and capillary permeability of select macromolecules. J Cell Biol 127: 1217–1232, 1994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Schubert W, Frank PG, Razani B, Park DS, Chow CW, Lisanti MP. Caveolae-deficient endothelial cells show defects in the uptake and transport of albumin in vivo. J Biol Chem 276: 48619–48622, 2001 [DOI] [PubMed] [Google Scholar]
- 86.Schubert W, Frank PG, Woodman SE, Hyogo H, Cohen DE, Chow CW, Lisanti MP. Microvascular hyperpermeability in caveolin-1 (-/-) knock-out mice. Treatment with a specific nitric-oxide synthase inhibitor, l-NAME, restores normal microvascular permeability in Cav-1 null mice. J Biol Chem 277: 40091–40098, 2002 [DOI] [PubMed] [Google Scholar]
- 87.Serne EH, de Jongh RT, Eringa EC, Ijzerman RG, Stehouwer CD. Microvascular dysfunction: a potential pathophysiological role in the metabolic syndrome. Hypertension 50: 204–211, 2007 [DOI] [PubMed] [Google Scholar]
- 88.Serne EH, Ijzerman RG, Gans RO, Nijveldt R, De Vries G, Evertz R, Donker AJ, Stehouwer CD. Direct evidence for insulin-induced capillary recruitment in skin of healthy subjects during physiological hyperinsulinemia. Diabetes 51: 1515–1522, 2002 [DOI] [PubMed] [Google Scholar]
- 89.Shajahan AN, Timblin BK, Sandoval R, Tiruppathi C, Malik AB, Minshall RD. Role of Src-induced dynamin-2 phosphorylation in caveolae-mediated endocytosis in endothelial cells. J Biol Chem 279: 20392–20400, 2004 [DOI] [PubMed] [Google Scholar]
- 90.Shankar RR, Wu Y, Shen HQ, Zhu JS, Baron AD. Mice with gene disruption of both endothelial and neuronal nitric oxide synthase exhibit insulin resistance. Diabetes 49: 684–687, 2000 [DOI] [PubMed] [Google Scholar]
- 91.Sherwin RS, Kramer KJ, Tobin JD, Insel PA, Liljenquist JE, Berman M, Andres R. A model of the kinetics of insulin in man. J Clin Invest 53: 1481–1492, 1974 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Simionescu M, Simionescu N. Endothelial transport of macromolecules: transcytosis and endocytosis. A look from cell biology. Cell Biol Rev 25: 1–78, 1991 [PubMed] [Google Scholar]
- 93.Sjöstrand M, Holmäng A, Lönnroth P. Measurement of interstitial insulin in human muscle. Am J Physiol Endocrinol Metab 276: E151–E154, 1999 [DOI] [PubMed] [Google Scholar]
- 94.Sjöstrand M, Holmäng A, Strindberg L, Lönnroth P. Estimations of muscle interstitial insulin, glucose, and lactate in type 2 diabetic subjects. Am J Physiol Endocrinol Metab 279: E1097–E1103, 2000 [DOI] [PubMed] [Google Scholar]
- 95.Stehouwer CD, Henry RM, Ferreira I. Arterial stiffness in diabetes and the metabolic syndrome: a pathway to cardiovascular disease. Diabetologia 51: 527–539, 2008 [DOI] [PubMed] [Google Scholar]
- 96.Steil GM, Ader M, Moore DM, Rebrin K, Bergman RN. Transendothelial insulin transport is not saturable in vivo. No evidence for a receptor-mediated process. J Clin Invest 97: 1497–1503, 1996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Steinberg HO, Brechtel G, Johnson A, Fineberg F, Baron AD. Insulin-mediated skeletal muscle vasodilation is nitric oxide dependent: a novel action of insulin to increase nitric oxide release. J Clin Invest 94: 1172–1179, 1994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Steinberg HO, Chaker H, Leaming R, Johnson A, Brechtel G, Baron AD. Obesity/insulin resistance is associated with endothelial dysfunction. Implications for the syndrome of insulin resistance. J Clin Invest 97: 2601–2610, 1996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Steinberg HO, Paradisi G, Hook G, Crowder K, Cronin J, Baron AD. Free fatty acid elevation impairs insulin-mediated vasodilation and nitric oxide production. Diabetes 49: 1231–1238, 2000 [DOI] [PubMed] [Google Scholar]
- 100.Steinberg HO, Tarshoby M, Monestel R, Hook G, Cronin J, Johnson A, Bayazeed B, Baron AD. Elevated circulating free fatty acid levels impair endothelium-dependent vasodilation. J Clin Invest 100: 1230–1239, 1997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Tiruppathi C, Song W, Bergenfeldt M, Sass P, Malik AB. Gp60 activation mediates albumin transcytosis in endothelial cells by tyrosine kinase-dependent pathway. J Biol Chem 272: 25968–25975, 1997 [DOI] [PubMed] [Google Scholar]
- 102.Vehkavaara S, Seppala-Lindroos A, Westerbacka J, Groop PH, Yki-Jarvinen H. In vivo endothelial dysfunction characterizes patients with impaired fasting glucose. Diabetes Care 22: 2055–2060, 1999 [DOI] [PubMed] [Google Scholar]
- 103.Vicent D, Ilany J, Kondo T, Naruse K, Fisher SJ, Kisanuki YY, Bursell S, Yanagisawa M, King GL, Kahn CR. The role of endothelial insulin signaling in the regulation of vascular tone and insulin resistance. J Clin Invest 111: 1373–1380, 2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Vincent MA, Barrett EJ, Lindner JR, Clark MG, Rattigan S. Inhibiting NOS blocks microvascular recruitment and blunts muscle glucose uptake in response to insulin. Am J Physiol Endocrinol Metab 285: E123–E129, 2003 [DOI] [PubMed] [Google Scholar]
- 105.Vincent MA, Clerk LH, Lindner JR, Price WJ, Jahn LA, Leong-Poi H, Barrett EJ. Mixed meal and light exercise each recruit muscle capillaries in healthy humans. Am J Physiol Endocrinol Metab 290: E1191–E1197, 2006 [DOI] [PubMed] [Google Scholar]
- 106.Vincent MA, Dawson D, Clark AD, Lindner JR, Rattigan S, Clark MG, Barrett EJ. Skeletal muscle microvascular recruitment by physiological hyperinsulinemia precedes increases in total blood flow. Diabetes 51: 42–48, 2002 [DOI] [PubMed] [Google Scholar]
- 107.Wang H, Liu Z, Li G, Barrett EJ. The vascular endothelial cell mediates insulin transport into skeletal muscle. Am J Physiol Endocrinol Metab 291: E323–E332, 2006 [DOI] [PubMed] [Google Scholar]
- 108.Wang H, Wang AX, Barrett EJ. Caveolin-1 is required for vascular endothelial insulin uptake. Am J Physiol Endocrinol Metab 300: E134–E144, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Wang H, Wang AX, Liu Z, Barrett EJ. Insulin signaling stimulates insulin transport by bovine aortic endothelial cells. Diabetes 57: 540–547, 2008 [DOI] [PubMed] [Google Scholar]
- 110.Wasserman DH, Kang L, Ayala JE, Fueger PT, Lee-Young RS. The physiological regulation of glucose flux into muscle in vivo. J Exp Biol 214: 254–262, [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Watts GF, O'Brien SF, Silvester W, Millar JA. Impaired endothelium-dependent and independent dilatation of forearm resistance arteries in men with diet-treated non-insulin-dependent diabetes: role of dyslipidaemia. Clin Sci 91: 567–573, 1996 [DOI] [PubMed] [Google Scholar]
- 112.Webb DR, Khunti K, Silverman R, Gray LJ, Srinivasan B, Lacy PS, Williams B, Davies MJ. Impact of metabolic indices on central artery stiffness: independent association of insulin resistance and glucose with aortic pulse wave velocity. Diabetologia 53: 1190–1198, [DOI] [PubMed] [Google Scholar]
- 113.Wei K, Jayaweera AR, Firoozan S, Linka A, Skyba DM, Kaul S. Quantification of myocardial blood flow with ultrasound-induced destruction of microbubbles administered as a constant venous infusion. Circulation 97: 473–483, 1998 [DOI] [PubMed] [Google Scholar]
- 114.Westerbacka J, Vehkavaara S, Bergholm R, Wilkinson I, Cockcroft J, Yki-Jarvinen H. Marked resistance of the ability of insulin to decrease arterial stiffness characterizes human obesity. Diabetes 48: 821–827, 1999 [DOI] [PubMed] [Google Scholar]
- 115.Westerbacka J, Wilkinson I, Cockcroft J, Utriainen T, Vehkavaara S, Yki-Jarvinen H. Diminished wave reflection in the aorta A novel physiological action of insulin on large blood vessels. Hypertension 33: 1118–1122, 1999 [DOI] [PubMed] [Google Scholar]
- 116.Williams KV, Bertoldo A, Mattioni B, Price JC, Cobelli C, Kelley DE. Glucose transport and phosphorylation in skeletal muscle in obesity: insight from a muscle-specific positron emission tomography model. J Clin Endocrinol Metab 88: 1271–1279, 2003 [DOI] [PubMed] [Google Scholar]
- 117.Yang YJ, Hope I, Ader M, Poulin RA, Bergman RN. Dose-response relationship between lymph insulin and glucose uptake reveals enhanced insulin sensitivity of peripheral tissues. Diabetes 41: 241–253, 1992 [DOI] [PubMed] [Google Scholar]
- 118.Yang YJ, Hope ID, Ader M, Bergman RN. Importance of transcapillary insulin transport to dynamics of insulin action after intravenous glucose [published erratum appears in Am J Physiol 1997 Aug;173 (2 Pt 1):section E following table of contents]. Am J Physiol Endocrinol Metab 266: E17–E25, 1994 [DOI] [PubMed] [Google Scholar]
- 119.Yang YJ, Hope ID, Ader M, Bergman RN. Insulin transport across capillaries is rate limiting for insulin action in dogs. J Clin Invest 84: 1620–1628, 1989 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Yki-Jarvinen H, Utriainen T. Insulin-induced vasodilatation: physiology or pharmacology? Diabetologia 41: 369–379, 1998 [DOI] [PubMed] [Google Scholar]
- 121.Zeng G, Quon MJ. Insulin-stimulated production of nitric oxide is inhibited by wortmannin. Direct measurement in vascular endothelial cells. J Clin Invest 98: 894–898, 1996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Zhang L, Vincent MA, Richards SM, Clerk LH, Rattigan S, Clark MG, Barrett EJ. Insulin sensitivity of muscle capillary recruitment in vivo. Diabetes 53: 447–453, 2004 [DOI] [PubMed] [Google Scholar]
- 123.Zhang L, Wheatley CM, Richards SM, Barrett EJ, Clark MG, Rattigan S. TNF-α acutely inhibits vascular effects of physiological but not high insulin or contraction. Am J Physiol Endocrinol Metab 285: E654–E660, 2003 [DOI] [PubMed] [Google Scholar]