Buffer management to solve bed-blocking in the Netherlands 2000–2010. Cooperation from an integrated care chain perspective as a key success factor for managing patient flows (original) (raw)
Abstract
Introduction
Bed-blocking problems in hospitals reflect how difficult and complex it is to move patients smoothly through the chain of care. In the Netherlands, during the first decade of the 21st century, some hospitals attempted to tackle this problem by using an Intermediate Care Department (ICD) as a buffer for bed-blockers. However, research has shown that ICDs do not sufficiently solve the bed-blocking problem and that bed-blocking is often caused by a lack of buffer management.
Tool
Buffer management (BM) is a tool that endeavors to balance patient flow in the hospital to nursing home chain of care.
Results
Additional research has indicated that the absence of BM is not the result of providers’ thinking that BM is unnecessary, unethical or impossible because of unpredictable patient flows. Instead, BM is hampered by a lack of cooperation between care providers.
Conclusion
Although stakeholders recognize that cooperation is imperative, they often fail to take the actions necessary to realize cooperation. Our assumption is that this lack of willingness and ability to cooperate is the result of several impeding conditions as well as stakeholders’ perceptions of these conditions and the persistence of their current routines, principles and beliefs (RPBs).
Discussion
We recommend simultaneously working on improving the conditions and changing stakeholders’ perceptions and RPBs.
Keywords: buffer management, bed-blocking, integrated care, care chain, cooperation, patient flow, theory of constraints
Introduction
Continuous care delivery demands that health care providers lead patients smoothly through a chain of care that includes a number of professionals, departments and organizations, each of which are necessary for the provision of quality care at the right time and in the right place for each and every patient [1–5]. Experience has taught us that this process is complex. Indeed, in countries like Sweden, England, the Netherlands and Austria, hospitals struggle with a bed-blocking problem. A bed-blocker is a patient who has completed treatment in one part of the care chain (e.g. a hospital) and is waiting for admittance to the next part of the chain (e.g. a nursing home or home care). Bed-blocking has consequences at various levels. At the micro level, it increases waiting time for new patients. At the macro level, it impacts health care costs as an occupied bed in a hospital is more expensive than an occupied bed in a nursing home or, alternatively, an occupied bed at home.
Hospitals have attempted to tackle the bed-blocking problem by setting up departments or areas that handle bed-blockers. In Austria, these are called After Care Areas [6]. In the Netherlands, where in 2006 6.1% of all hospital days were bed-blocking days, Intermediate Care Departments (ICD) have been established [7–10]. An ICD is a nursing department—usually situated in the hospital building—that functions as a buffer when the hospital is over its capacity. It essentially controls the amount of patients admitted to the hospital. Earlier in the millennium, approximately 40% of Dutch hospitals had an ICD. Initially, the establishment of ICDs appeared to be a promising and effective solution to bed-blocking. In fact, between 1999 and 2002, the total number of bed blocking days in hospitals with an ICD decreased by 30% while hospitals without an ICD saw a decrease of only 15% [8]. However, with the establishment of ICDs, another problem arose, namely queues for admission to the ICDs. This occurred in more than half of all ICD hospitals (56%). Although the average waiting time and the size of the queue had decreased between 2003 and 2006 from 11 to 8 days and from 8 to 7 patients, respectively, the queue remained [7, 9]. In essence, the solution (i.e. ICDs) generated the same problem it was meant to solve (i.e. waiting times and bed-blocking). Clearly, ICDs have failed to solve the bed-blocking problem. Previously, we explained that this was likely caused by a lack of buffer management (BM), a tool that endeavors to balance patient flow in the hospital to nursing home chain of care. We hypothesized that BM was not applied by health care professionals and management because of a number of negative beliefs regarding BM. We further concluded that BM is indeed the most promising way for increasing the effectiveness of buffering [8]. However, we must question whether our assumption that providers and managers hold negative beliefs about BM is correct. We are also interested in what can be done to make BM more feasible in health care settings.
With this in mind, this paper seeks to firstly explain the theory of BM and then discuss the tenability of our previous assumptions given the results of (explorative) research recently conducted.
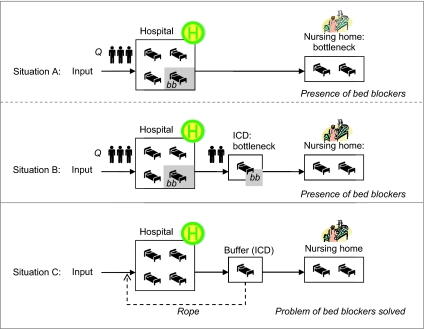
The theory of buffer management
BM builds upon the theory of constraints ‘drum-buffer-rope’ [11–17]. It aims to maximize the throughput in the chain by firstly identifying impeding factors or constraints and then taking measures to manage them properly. Constraints can be identified by analyzing the sub-processes of the (patient) flow in the chain. The most impeding factor is called the system’s bottleneck. Because all sub-processes are linked to one other, the bottleneck determines the flow of the entire process and thus requires immediate and appropriate attention. In identifying the bottleneck, the entire chain should be taken into account. When the bottleneck is found, the ‘drum-buffer-rope’ method is used to balance the patient flow in the whole chain. In the Dutch hospital to nursing home or home care chain of care, the patient flow into the nursing home is the bottleneck [7, 9]. The ‘drum-buffer-rope’ method prescribes determining how many patients should be admitted to the hospital as well as the throughput from the hospital to the nursing home via the ICD using a so-called rope. When the buffer overflows, the rope, which is an information stream, closes the hospital doors for potential (elective) buffer patients, which are mainly patients with mobility problems, rehabilitation needs or cardiovascular problems [7, 9]. This procedure is illustrated in Figure 1, which displays three situations: the chain with no buffer (situation A), the chain with a buffer but without BM (situation B) and the chain with a buffer and BM (situation C).
Figure 1.
No buffer (situation A), a buffer without buffer management (situation B) and a buffer with buffer management (situation C); bb, bed blocker; Q, queue.
Correct execution of BM requires that the following prerequisites for successful BM be taken into account [13, 18]:
- In order to balance the flow, the entire process including its sub-processes must be considered.
- Total flow can only be effectively increased by increasing the flow in the bottleneck.
- In order to prevent queues, the buffer needs free space to absorb fluctuations which are most frequently caused by non-elective patients. A maximum occupancy of 70% is considered acceptable.
- The use of a rope to adjust the input rate at the beginning of the process is necessary to prevent overflow in the sub-processes.
In practice, the buffer is often used incorrectly. The abovementioned prerequisites for effective BM are infrequently considered and the rope is rarely used. Another misconception is that if the sub-processes are optimized, the flow of the entire process will increase. This is not the case. In fact, this leads to an unbalanced flow because the flow is determined by the bottleneck. With respect to bed-blocking, what will happen is the following: because patient flow in nursing homes is lower than patient flow in hospitals and because fluctuations at the entrance cannot be absorbed, in the absence of BM, the ICD will overflow. As mentioned earlier, a queue will form. This will result in bed blockers in the hospital (bb) who are waiting to be transferred to the ICD. Subsequently, a queue for hospital admittance will form (Q) [7]. This is illustrated as situation B in Figure 1.
Although this appears to be pretty straightforward, the problem of bed-blocking nonetheless remains. It is thus important to better understand why care providers involved fail to fulfill the abovementioned prerequisites. One possible explanation is that management and professionals in hospitals and/or nursing homes hold one or more negative beliefs about BM. We have previously provided objections to these beliefs [8]. The beliefs and our objections are:
- Buffer management is unnecessary.
The argument is that BM is unnecessary when discharge management is a sufficient and more manageable alternative [cf. 19–24]. However, discharge management does not balance patient flow nor does it establish a figurative tap to prevent additional patients per time unit from entering the chain when upstream capacity is limited. Although discharge management, when used effectively, is a helpful coordination tool, research has indicated that discharge management has many problems with respect to, among other things, communication and information exchange [25]. - Patient arrivals are unpredictable.
The argument is that fluctuations in patient flow with respect to the frequency and intensity of patient arrivals cannot be predicted. We disagree. Patient flow is predictable when elective and non-elective admissions are distinguished from one another [cf. 26–28]. Additionally, although it might not be possible to predict the exact number of emergent arrivals per day, the size of emergent demand generally appears to be quite stable and predictable over time. As such, we contend that the required size of the departments and buffer can be defined. - Buffer management is unethical.
The argument is that putting a figurative tap on patient flows is ethically unacceptable as it implies the refusal of some patients [cf. 29]. We ask whether it is safe and ethically acceptable to treat (elective) patients without knowing if they can be nursed and cared for afterwards [cf. 30]. Apparently, it is impossible to provide accessible high quality care that is tailored to the needs of the patient [31]. We contend that we must be aware of this dilemma and subsequently take conscious clinical and political decisions. - Care organizations are unwilling to cooperate.
Cooperation between care providers using a chain perspective is necessary in order to maintain the delicate balance in the chain. Previous research has indicated that care organizations are often unwilling to cooperate [5, 32] thus supporting this argument against BM. However, we contend that the current trend in many European countries actually demonstrates an increased awareness of the importance of cooperation among most care providers [5, 33, 34].
Investigating the tenability of the objections: methods and results
Van Hartingsveldt [7] conducted three small case studies to further explore care providers’ beliefs about BM (regarding both the sub-processes and the chain as a whole) and to investigate whether or not providers held the four negative beliefs about BM as we assumed. The case studies were derived from qualitative data gathered in a larger mixed methods research project, using questionnaires and interviews with top-managers that addressed the availability of ICDs in all Dutch hospitals and their functioning in terms of patient flows, waiting times, manpower, task division and responsibilities. The data gathered in 2006 were compared with data from a similar study conducted in 2003 [9] in order to determine if things had changed over the years. The ICDs selected for the case studies differed with respect to their quantitative outcomes. One case study was conducted with an ICD that had an average outcome, another with an ICD that had a lower than average outcome and yet another with an ICD that had a higher than average outcome. In each case study, an in-depth interview was conducted with ICD executives using a structured interview protocol. The managers of the selected ICDs were interviewed and asked to mention two additional interview candidates, one that is responsible for referring patients to the ICD and one that is responsible for admitting patients to nursing homes. Consequently, in each case study, three people with different work positions were interviewed. In total, nine interviews were conducted. The interviews were tape-recorded and transcribed verbatim. Hermeneutic and narrative approaches were applied in the analyses. Based on the assumption that respondents’ answers derive meaning from the whole and the whole derives meaning from the parts, the interviews were read and reread in an effort to develop a comprehensive understanding of the data [7].
The interview data showed the following:
- All respondents considered the hospital, the ICD and the nursing home to be separate links in the care chain. In their view, the organizations are independent. Meetings that aimed to enable optimal patient flow and that included representatives of the three organizations failed to discuss whether equal numbers of patients were being admitted and discharged from the ICD.
- Because ICDs are financed according to how many beds are occupied, it is not surprising that ICD respondents emphasized striving for a 100% occupancy rate in order to gain sufficient funding. This was also illustrated by the following citations: “We celebrated the moment that our department was fully occupied”; “Currently we have an occupancy rate of 70%. I am therefore searching for patients to stay in the ICD so that I can reach my production target.”
- All ICD and nursing home respondents said that they did not have any information regarding planned patient referrals from nursing departments and ICDs, respectively. This was confirmed by respondents from nursing departments referring to ICDs and respondents from ICDs referring to nursing homes.
- One nursing home respondent said that she did not benefit from investing energy into the facilitation of patient flow from the ICD to the nursing home as “the number of patients being admitted to nursing homes is already high enough to fill all the nursing home beds”.
- All respondents shared objections to the contention that BM is unnecessary. They were aware that management is necessary. However, they emphasized that the current financial structures inhibit the application of BM. More specifically, they indicated that insurers do not reimburse empty beds.
- All respondents did not agree with the contention that patient flows are unpredictable and that this serves as an inhibitor to BM. They, in fact, claimed that health care providers always have to deal with unpredictability.
- None of the respondents felt that BM is unethical. They indicated that patient refusal is simply part of daily practice in health care. According to one ICD respondent: “Also here at the ICD, we are sometimes fully occupied. Even the hospital and the emergency department are sometimes full. Then you have to refuse patients. That’s just how it is in practice.”
- All respondents indicated that cooperation is necessary in order to enable optimal patient flow and in order to reduce the number of bed-blockers.
At first sight, the interview data suggest that our previous assumption that health care providers and management hold negative beliefs about BM is incorrect. For, they broadly supported the necessity and feasibility of BM [cf. 5–7]. In practice, however, they do not apply the BM solution and they do not cooperate as is needed for BM application. For, although respondents said that cooperation is most valuable and necessary [cf. 8], they acted in ways that were inconsistent with this claim. They failed to share information with one another; they failed to provide feedback about patient flows to one another; and they sought to meet the interests of their own department or organization (e.g. acquiring maximum funding) before considering the interests of the total chain and its patient flow [cf. 1–4]. They quite simply failed to cooperate in ways that are imperative to the success of BM. Such a paradox between words and actions has previously been referred to as skilled incompetence by Argyris [35].
In order to shed light on why, when it comes to cooperation, respondents’ actions did not coincide with their words, we will further explore the inhibiting and promoting conditions for cooperation below.
Exploring cooperation
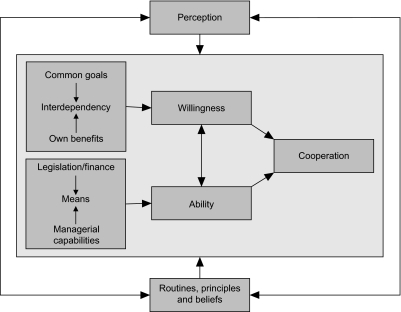
In seeking to understand cooperation between organizations, organizational units or professionals in health care, we have opted to borrow from organizational theories and literature on integrated care. Organizational theories claim that organizational operations, like cooperation, communication, governance and knowledge transfer, are, in the end, determined by actions. Actions are, in turn, dependent on the willingness and ability of those involved [36–39].
Many conditions contribute to willingness and ability to act.
Willingness
One of the basic conditions for willingness to cooperate is the presence of interdependency between the organizations involved [39–41]. In health care, interdependency among providers is rapidly increasing as pressure to coordinate services and deliver integrated care is increasing [2, 4, 42, 43]. A second basic condition for willingness to cooperate is the presence of at least one common goal [5, 39, 44]. In health care, common goals are often construed in one’s mind but not manifested in one’s actions. A third basic condition is that the cooperation contributes to the department or organization’s own goals [44–47]. With the resource dependency theory [41] in mind, we assume that interdependency increases when the number and weight of common goals and the benefits of cooperation for the organization’s involved increases. We also assume that greater willingness generates more opportunities to act.
Ability
In order to act, one must also have means. Means include money, personnel, time, equipment and accommodation. In health care, means are always scarce. To make matters worse, cooperation always requires transaction costs in order to generate revenues later [48]. This combination of scarce resources and transaction costs for cooperation does not promote providers’ abilities to cooperate. Furthermore, limited ability is likely to reduce willingness. In most health care systems, the availability of means is dependent on legal and financial structures and regulations [3, 34, 49]. Many legal frameworks are ambiguous when it comes to promoting cooperation in health care. Most countries have some laws and regulations fostering cooperation and others that hinder cooperation [5, 33, 49]. The availability of means is also dependent on managerial capabilities [38, 50], especially political and negotiating skills but also certain leadership characteristics, such as transformational leadership (vision, ability to motivate and convince) and intrinsic personal leadership features, such as charisma, charm and attractiveness [38, 50–53]. Our previous research on integrated care revealed that managerial capabilities, especially leadership features and behavior, were strongly related to success or failure of integrated care networks [44, 46, 47].
Perceptions, routines, principles and beliefs
Cooperation is not simply determined by promoting and inhibiting conditions. In the real world, the willingness and ability to act in cooperative ways is also dependent on the answers to two questions. The first is, ‘How do those involved perceive the abovementioned conditions?’ [cf. 37, 39, 41]. According to the Thomas Theorem—“If men perceive things as real, they are real in their consequences” [54]—the perception of the situation affects the actions taken. We must therefore explore whether those involved are really aware of their interdependency. Do they perceive common goals? Do they think cooperation will benefit their own goals? Do they see possibilities to acquire additional means? The second question concerns the extent they are able to change the routines, principles and beliefs (RPBs) employed in their daily work in order to achieve successful cooperation. We must ask if they are able to shift their focus from their own organization or department to the chain as a whole. Are they able to find solutions for financial problems and develop trust in their partners instead of harboring distrust and prejudice? Are they able to replace their belief in their own power with a belief in shared power? We assume that both aspects are also mutually dependent. It is likely that the ability to change RPBs is in part dependent on perceptions while RPBs also impact perceptions. As such, perceptions and RPBs enforce and reinforce one another. This is a vicious cycle and experience has taught us that breaking vicious cycles is often a laborious endeavor.
Figure 2 provides an overview of the conditions necessary for cooperation.
Figure 2.
Conditions for cooperation.
Discussion and conclusion
With respect to the ICD case, we must question whether the Dutch hospitals and nursing homes are aware of their interdependency on a daily basis. It is quite likely that hospital staff members (doctors, interns, administrative personnel) are unaware of their dependency on nursing home capacities when admitting potential buffer patients. At the same time, nursing home staff members probably do not realize that their hampered patient flow causes waiting lists for hospitals. Furthermore, we must question whether the hospitals and nursing homes are truly aware of a common goal. Most hospitals and nursing homes do formulate common goals to improve patient flow in a formal agreement [7, 9] but are they really making decisions on the basis of these goals in their daily work? It is likely that some parties in some parts of the chain do not even feel that improvement of the patient flow is necessary. This seems to be the case in nursing homes where the patient flow into the nursing home is sufficient to fill the available beds. Nursing homes are thus likely to believe that a buffer is unnecessary. We must also question whether hospitals and nursing homes are really aware of BM and how it can contribute to the attainment of an organization or department’s own goals. Instead, they most often consider BM to be a threat to their own goals. They may believe that BM threatens their autonomy and the acquisition of sufficient funding. At the same time, they fail to tackle the impeding factors that make BM a threat. For instance, with respect to funding, they often do not realize that it may be worthwhile fighting the prevailing system for the provision of funding. It may also be worthwhile to seek other resources or work more efficiently in order to enlarge their ability to cooperate. As such, it appears that the advantages of the ICD buffer and BM; namely improved patient flow and increased nursing home capacity due to additional beds in hospitals, is not perceived, or is at the very least, not perceived as important enough to change the RPBs of those involved.
Our conclusion is that, in health care practice, three of the four negative beliefs regarding BM can be refuted. The argument concerning cooperation, however, remains. Although the providers involved in the case studies perceived a need for cooperation, they were not able or willing to translate this into action. Their own (professional, organizational and managerial) interests took precedence. In addition, a shortage of means caused by inappropriate incentives from financiers hampered concrete efforts to improve cooperation. In fact, the financial structure may very well be used as an argument against cooperation. We must realize that the current behavior is difficult to change as it is part of a vicious cycle of RPBs and perceptions, both of which are not in favor of cooperation. More importantly, a major reason for not favoring cooperation has institutional roots [cf. 55], more specifically, the health care system’s financial structures, rules and regulations as well as its professional values (i.e. professional autonomy). In essence, providers’ skilled incompetence with respect to cooperation is in part an ‘institutionalized skilled incompetence’ that is very difficult to tackle.
In order to make BM not only theoretically feasible, but also practically applicable, the vicious cycle of perceptions and RPBs should be broken. Essentially, it boils down to a shift of focus from parts (i.e. each individual organization) to the whole (i.e. the flow between participating organizations). Only then theoretical acceptance of BM will be followed by consistent BM actions. For this to be achieved, we recommend the promotion of providers’ willingness and ability to take actions which foster cooperation (i.e. the heart of our cooperation model—Figure 2). Two (change) strategies could be followed simultaneously: first, a negotiating strategy, to create win-win-situations, and second, a learning strategy, on how to adopt cooperation in the daily routines, anchored in people’ principles and beliefs [cf. 56]. Within each strategy several interventions at the system’s macro, meso or micro level are possible.
Examples of interventions related to the negotiating strategy are:
- Convincing politicians and other powerful stakeholders to change the system such that incentives for cooperation are present. Once practiced, cooperation can save costs. As this is a macro-level intervention, it is an important job for top managers, but also for occupational organizations.
- Making care providers and professionals aware of the chain perspective. Convincing them that adopting this perspective is needed to solve their bed-blocking problems and, by doing that, improve quality and save costs. More concrete: an ICD manager could stress the chain perspective and its advantages on the meso and micro levels, in discussions with medical professionals, hospital governors and nursing home managers.
- Negotiating with care insurers or health authorities in order to enlarge financial means for cooperation. It is important to stress cost savings on the macro level, related to successful cooperation. This should be part of the annual negotiations on budgets.
- Striving for funding based on cooperation between organizations (i.e. flow funding) instead of funding the participating organizations individually (as is the case now).
- Appointing a chain manager or director that can oversee the entire care process and consider the prerequisites for BM in this process. Appointment of a chain manager should be a common action on meso/micro level, i.e. the (top) managers of the organizations involved in the chain, with commitment of professionals. The chain director should be provided with the right competences, like transformational leadership [53] and have appropriate negotiating skills as this can promote change in providers’ RPBs.
- Drafting and signing agreements that ensure provider compliance with the BM prerequisites, including obligations and potentially even sanctions. The chain manager (at meso level) could prepare this in cooperation with the organizational managers and professionals involved.
- Examples of interventions related to the learning strategy are:
- Learning to find and use other (local) sources at macro and meso levels to finance a care process that allows for the regulation of hospital intakes based on ICD bed occupancy. This learning can be stimulated in brainstorm sessions of professionals and providers involved (meso and micro level). Top managers and other motivated managers could start up this process.
- Motivating and teaching professionals and providers involved to develop common goals and to come to common adherence based on those common goals. Higher management and the chain manager could take initiatives in this direction by first mobilizing professionals who understand the chain perspective and are motivated to convince their colleagues of the advantages of cooperation. So, meso and micro levels should be involved.
- Setting up a virtual network organization to manage cooperation and learn how to make use of the virtual organization (meso level). ICT is a helpful tool to execute cooperative actions, but it takes time to become familiar with using it. Use of ICT experts can be helpful, but more important is that ICT becomes part of providers’ daily routines.
Table 1 gives an overview of the two strategies, and the related interventions on macro, meso and micro level of the health and social system.
Table 1.
A framework of a multi-level strategy (including examples of interventions) to promote cooperation in order to allow for BM
| Strategies | Interventions | ||
|---|---|---|---|
| Macro level | Meso level | Micro level | |
| Negotiating strategy | Convincing politicians to provide incentives for cooperation | Promoting chain perspective | Promoting chain perspective |
| Budget negotiations with care insurers or health authorities | Appointment chain manager | Appointment chain manager | |
| Drafting and signing agreements | |||
| Learning strategy | Finding and using additional financial sources | Finding and using additional financial sources | Finding and using additional financial sources |
| Developing common goals and adherence | Developing common goals and adherence | ||
| Setting up and using virtual network | Using virtual network |
The interventions described above are not complete, but mere examples. It depends of the individual situation what interventions to choose and when to apply them. In addition, we realize that the chain manager’s task is not a simple one. Breaking down the non-cooperation needs time, authority and special capacities. Very important is that the chain manager is or makes him/herself accepted by those involved. If not, it will be difficult to realize the conditions for cooperation, as mentioned in Figure 2. So, the interventions require investments, and the return on investment in terms of quality and savings should be analyzed in advance.
Our conclusion is that, in health care, the failure to cooperate is a serious inhibitor of BM. Continuous persistent and purposeful efforts to improve cooperation between care providers are therefore imperative, as people often relapse into old routines, principles and beliefs.
Acknowledgments
The authors thank Ron Handels, master’s student at Maastricht University, for his helpful suggestions and his contribution to the visualization of the theory of buffer management (Figure 1).
Contributor Information
Ingrid Mur-Veeman, Department of HOPE, Maastricht University, School for Public Health and Primary Care (CAPHRI), Faculty of Health, Medicine and Life Sciences, P.O. Box 616, 6200 MD Maastricht, Netherlands.
Mark Govers, Department of HOPE, Maastricht University, School for Public Health and Primary Care (CAPHRI), Faculty of Health, Medicine and Life Sciences, P.O. Box 616, 6200 MD Maastricht, Netherlands.
Reviewers
Maren Sogstad, Associate Professor, PhD, Centre for Care Research, Gjøvik University College, Post Box 191, 2802 Gjøvik, Norway
Birthe Dinesen, PhD, Associate Professor, Department of Health Science and Technology, Aalborg University, Fredrik BajersVej 7 D1, DK-9220 Aalborg, Denmark
Jason CH Yap, MBBS, MMed (Public Health), FAMS, MBA(IS), Chief (Health Information & Innovation), Agency for Integrated Care, Singapore
References
- 1.Ackerman III. The movement to vertically integrated regional health systems. Health Care Management Review. 1992;17(3):81–8. [PubMed] [Google Scholar]
- 2.Ahgren B. Chain of care development in Sweden: results of a national study. International Journal of Integrated Care. [serial online] 2003 Oct 7;3. [Cited 2011 8 June]. Available from: http://www.ijic.org. URN:NBN:NL:UI:10-1-100330. [PMC free article] [PubMed] [Google Scholar]
- 3.Hardy B, Mur-Veeman I, Steenbergen M, Wistow G. Inter-agency services in England and The Netherlands. A comparative study of integrated care development and delivery. Health Policy. 1999;48:87–105. doi: 10.1016/s0168-8510(99)00037-8. [DOI] [PubMed] [Google Scholar]
- 4.Minkman MMN, Schouten LMT, Huijsman R, van Splinteren PT. Integrated care for patients with a stroke in the Netherlands: results and experiences from a national breakthrough collaborative improvement project. International Journal of Integrated Care [serial online] 2005 Mar 23;5 doi: 10.5334/ijic.118. [Cited 2011 8 June]. Available from: http://www.ijic.org. URN:NBN:NL:UI:10-1-100360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Raak A van, Mur-Veeman I, Hardy B, Steenbergen M, Paulus A, editors. Integrated care in Europe. Description and comparison of integrated care in six EU countries. Maarssen: Reed Business Information; 2003. [Google Scholar]
- 6.Kaltenbrunner I. Master’s thesis. Maastricht: Maastricht University; 2009. Development and implementation of an orthopaedic (after care) remobilisation area. [Google Scholar]
- 7.Hartingsveldt C van. Master’s thesis. Maastricht: Maastricht University; 2006. One for all, and all for one? [Google Scholar]
- 8.Mur-Veeman I, Govers M. The benefits of ‘buffer management’ in health care. British Journal of Health Care Management. 2006;12(11):340–54. [Google Scholar]
- 9.Verhoef K. Transmurale afdelingen. Een inventariserend onderzoek naar verpleeghuisafdelingen in Nederlandse ziekenhuizen. [Intermediate care departments. An inventory of nursing home departments in Dutch hospitals]. Maastricht University: Maastricht; 2003. Master’s thesis. [in Dutch] [Google Scholar]
- 10.Verhoef K, Borghans I. Transmurale afdelingen. Een tijdelijke oplossing. [Intermediate care departments. A temporary solution]. Zorgvisie. 2005:39. [in Dutch] [Google Scholar]
- 11.Goldratt ME. The Haystack Syndrome: shifting data out of the data ocean. New York: Cronton-on-Hudson; 1990. [Google Scholar]
- 12.Goldratt ME, Cox J. The goal. 2nd revised edition. New York: Cronton-on-Hudson; 1992. [Google Scholar]
- 13.Goldratt ME, Fox R. The race. New York: Cronton-on-Hudson; 1986. [Google Scholar]
- 14.Atwater JB, Chakravorty SS. A study of the utilization of capacity constrainted resources in drum-buffer-rope systems. Production and Operations Management. 2002;11(2):259–73. [Google Scholar]
- 15.Gupta M, Ko HJ, Min H. TOC-based performance measures and five focusing steps in job shop manufacturing environment. International Journal of Production Research. 2002;40(4):907–30. [Google Scholar]
- 16.Plenert G, Best TD. MRP, JIT, and OPT: what is best? Productions and Inventory Management Journal. 1986;27(2):22–8. [Google Scholar]
- 17.Schragenheim E, Ronen B. Drum-buffer-rope shop floor control. Productions and Inventory Management Journal. 1990;31(3):18–22. [Google Scholar]
- 18.Umble M, Umble EJ. Utilizing buffer management to improve performance in a health care environment. European Journal of Operational Research. 2006;174:1060–75. [Google Scholar]
- 19.Bowles KH, Foust JB, Naylor MD. Hospital discharge referral decision making: a multidisciplinary perspective. Applied Nursing Research. 2004;16(3):134–43. doi: 10.1016/s0897-1897(03)00048-x. [DOI] [PubMed] [Google Scholar]
- 20.Collier EJ, Harrington C. Discharge planning, nursing home placement, and the Internet. Nursing Outlook. 2005;53(2):95–103. doi: 10.1016/j.outlook.2004.02.002. [DOI] [PubMed] [Google Scholar]
- 21.Foust J. Discharge planning as part of daily nursing practice. Applied Nursing Research. 2007;20(2):72–7. doi: 10.1016/j.apnr.2006.01.005. [DOI] [PubMed] [Google Scholar]
- 22.Taylor Reed Jr PA, Veith FJ, Gargiulo NJ, Timaran CH, Ohkit T, Lipsitz EC, et al. System to decrease length of stay for vascular surgery. Journal of Vascular Surgery. 2004;39(2):395–9. doi: 10.1016/j.jvs.2003.09.015. [DOI] [PubMed] [Google Scholar]
- 23.Watts R. Nurses’ perceptions of discharge planning. Nursing and Health Sciences. 2004;7(3):175–83. doi: 10.1111/j.1442-2018.2005.00229.x. [DOI] [PubMed] [Google Scholar]
- 24.Watts R, Gardner H. Factors that enhance or impede critical care nurses’ discharge planning practices. Intensive and Critical Care Nursing. 2005;21(5):302–13. doi: 10.1016/j.iccn.2005.01.005. [DOI] [PubMed] [Google Scholar]
- 25.Hegney D, MacCartny A, Beth de la Rue M, Fahey P, Gounan D, MacDonald KM, et al. Discharge planning from the acute sector for people over the age of 65. Journal of the Royal College of Nursing. 2002;9(3):15–21. doi: 10.1016/s1322-7696(08)60420-5. [DOI] [PubMed] [Google Scholar]
- 26.Amelsvoort PJLM. The design of work and organisation: the modern sociotechnical systems approach: an overview of the Dutch sociotechnical systems approach. Netherlands: Vlijmen; 2000. [Google Scholar]
- 27.Eijnatten FM van. The paradigm that changed the work place. Social science for social action: toward organizational renewal. Van Gorcum: Assen; 1993. [Google Scholar]
- 28.Sitter LU de, Dankbaar B, Hertog JH den. Designing simple organizations and complex jobs. Maastricht: MERIT; 1994. [Google Scholar]
- 29.Butler J. The ethics of health care rationing. Principles and practices. New York: Cassel; 1999. [Google Scholar]
- 30.Karlberg HI, Brinkmo BM. The unethical focus on access: a study of medical ethics and the waiting time guarantee. Scandinavian Journal of Public Health. 2009;37(2):117–21. doi: 10.1177/1403494808101359. [DOI] [PubMed] [Google Scholar]
- 31.Weale A. Rationing health care. Editorial. British Medical Journal. 1998;316:40. doi: 10.1136/bmj.316.7129.410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kümpers SNS. A neo-institutional comparative study. PhD thesis. Enschede: PrintPartners Ipskamp; 2005. Steering integrated care in England and the Netherlands: the case of dementia care. [Google Scholar]
- 33.Leichsenring K, Alaszewski AM. Providing integrated health and social care for older persons. A European overview of issues at stake. Aldershot: Ashgate Publishing Ltd; 2004. [Google Scholar]
- 34.Nies H, Berman PC, Integrating services for older people . A resource book for managers. Almere: PlantijnCasparie; 2004. [Google Scholar]
- 35.Argyris C. Skilled incompetence. Harvard Business Review. 1986;64(5):74–9. [Google Scholar]
- 36.Kerr S, Slocum JR. Controlling the performances of people in organizations. In: Nystrom PC, Starbuck WH, editors. Handbook of organizational design. New York: Oxford University Press; 1981. [Google Scholar]
- 37.Kümpers S, Mur I, Hardy B, Maarse H, Raak A van. The importance of knowledge transfer between specialist and generic services in improving dementia care. The International Journal of Health Planning and Management. 2006;21(2):51–67. doi: 10.1002/hpm.837. [DOI] [PubMed] [Google Scholar]
- 38.Mintzberg H. Power in and around organizations. NJ: Prentice Hall Inc: Englewood Cliffs; 1983. [Google Scholar]
- 39.Rijk A de, Raak A van, Made J van der. A new theoretical model for cooperation in public health settings: the RDIC model. Qualitative Health Research. 2007;17(8):1103–16. doi: 10.1177/1049732307308236. [DOI] [PubMed] [Google Scholar]
- 40.Pfeffer J, Nowak P. Joint ventures and interorganizational interdependence. Science Quarterly. 1976;2:398–418. [Google Scholar]
- 41.Pfeffer J, Salancik GR The external control of organizations . . A resource dependence perspective. New York: Harper and Row; 1978. [Google Scholar]
- 42.Kodner DL, Kyriacou C. Fully integrated care for the frail elderly: two American models. International Journal of Integrated Care [serial online] 2000 doi: 10.5334/ijic.11. Nov 1;0. [cited 2011 8 June]. Available from: http://www.ijic.org. URN:NBN:NL:UI:10-1-100253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kodner DL, Spreeuwenberg C. Integrated care: meaning, logic, applications, and implications—a discussion paper. International Journal of Integrated Care [serial online] 2002 doi: 10.5334/ijic.67. Nov 14;5. [cited 2011 8 June]. Available from: http://www.ijic.org. URN:NBN:NL:UI:10-1-100309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Leurs M. A collaborative approach to tailored whole-school health promotion—the schoolBeat study. PhD thesis. Maastricht University. Enschede: PrintPartners Ipskamp; 2008. [Google Scholar]
- 45.Bohlmeijer E, Ruland E, Raak A van, Mur-Veeman I, editors. Procesmanagement in public health. Ontwerp, Analyse & Verandering. [Process management in public health. Design, analysis & change]. Utrecht: Trimbos Instituut; 2005. [in Dutch] [Google Scholar]
- 46.Leurs MTW, Mur-Veeman IM, Sar R van de, Schaalma HP, Vries N de. Diagnosis of sustainable collaboration in health promotion—a case study. BMC Public Health. 2008;8:382. doi: 10.1186/1471-2458-8-382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Raak A van, Jongerius-de Gier G, Massop J, Mur-Veeman I. Brug tussen gisteren en morgen. Zorgvernieuwing als veranderingsstrategie voor een betere zorg in de toekomst. Evaluatie Programma Zorgvernieuwingsprojecten Thuiszorg van WVC. Eindrapportage. [Evaluation of twelve integrated care projects in The Netherlands. Final report]. Maastricht: Datawyse Universitaire Pers; 1993. [in Dutch] [Google Scholar]
- 48.Raak A van, Paulus A, Merode F van, Mur-Veeman I. Integrated care management: applying control theory to networks. Journal of Management in Medicine. 1999;13(6):390–404. doi: 10.1108/02689239910299795. [DOI] [PubMed] [Google Scholar]
- 49.Mur-Veeman I, Raak A van, Paulus A. Comparing integrated care policy in Europe: does policy matter? Health Policy. 2008;85:172–83. doi: 10.1016/j.healthpol.2007.07.008. [DOI] [PubMed] [Google Scholar]
- 50.Daft RL, Noe RA. Organizational behaviour. Orlando: Harcourt College Publishers; 2001. [Google Scholar]
- 51.Bass BM. Two decades of research and development in transformational leadership. European Journal of Work and Organizational Psychology. 1999;8(1):9–32. [Google Scholar]
- 52.Bass BM, Avolio BJ. Improving organizational effectiveness through transformational leadership. Thousand Oaks, CA: Sage Publications; 1998. [Google Scholar]
- 53.Bass BM, Riggio RE. Transformational leadership. Mahwah, New Jersey, London: Lawrence Erlbaum Associates Publishers; 2006. [Google Scholar]
- 54.Thomas WI, Thomas DS. The child in America: behavior problems and programs. New York: Knopf; 1928. [Google Scholar]
- 55.DiMaggio PJ, Powell WW. The iron case revisited: institutional isomorphism and collective rationality in organizational fields. American Sociological Review. 1986;48:147–60. [Google Scholar]
- 56.Caluwé L de, Vermaak H. Learning to change. Thousand Oaks, CA: Sage Publications; 2003. [Google Scholar]