Neurobiology of obsessive-compulsive disorder: insights into neural circuitry dysfunction through mouse genetics (original) (raw)
. Author manuscript; available in PMC: 2012 Dec 1.
Published in final edited form as: Curr Opin Neurobiol. 2011 May 24;21(6):842–848. doi: 10.1016/j.conb.2011.04.010
Abstract
The precise causal factors for obsessive-compulsive disorder (OCD) are not known, however, decades of research have honed in on the cortico-striatal-thalamo-cortical (CSTC) circuitry in the brain as a critical pathway involved in obsessions and the intimately linked compulsive-repetitive behaviors. Recent progress in human and mouse genetics have led to the identification of novel candidate susceptibility genes, which in turn have facilitated a more focused approach to unraveling the nature of circuitry dysfunction in OCD. The ability to perform invasive techniques in genetic animal models of OCD will be crucial for rapid advances in this field, and as such we review the most recent developments and highlight the importance of searching out common circuitry defects underlying compulsive-repetitive behaviors.
Keywords: OCD, glutamate, glutamatergic, basal ganglia, CSTC, fronto-subcortical, synapse, neurotransmission, genetics, Sapap3, Tourette syndrome, trichotillomania, TTM, neuropsychiatric disorder, N-acetylcysteine, NAC, Slc1a1, EAAC1, Hoxb8, Slitrk5, Slitrk1, Shank3, MeCP2, corticostriatal, cortico-striatal, obsessive-compulsive spectrum disorder, OCD circuit
Introduction
Despite the fact that the causes of OCD remain elusive, in recent years this disorder, once considered relatively obscure, has experienced a reemergence in the public consciousness. This is underscored by the creation of not one, but two separate reality/documentary-style television shows dedicated to this topic within the past two years (“OCD Project” which aired on VH1 and “Obsessed” which aired on A&E). Perhaps this is the result of a growing acceptance that OCD is not obscure, but rather, ranks among the most prevalent neuropsychiatric disorders such as major depression, schizophrenia, and bipolar disorder.
It is estimated that the lifetime prevalence of OCD is 1–3% in the general population [1,2], suggesting that within each of our social networks we may find family members, friends, or colleagues that live with this often debilitating condition. While there are several treatment options currently available [3,4], the stark reality is that there remains a significant percentage of OCD sufferers that are either non-responsive or only partially responsive to the available treatment paradigms. Furthermore, last-resort invasive procedures such as deep brain stimulation or surgical procedures have had mixed success in alleviating severe symptoms [5], and thus these options remain an empirical art that is far from being mastered. This highlights the importance of continued research into the precise causes of OCD and continued exploration of novel targets that have promise to one day bring relief to all in need.
Theoretical framework for circuitry dysfunction in OCD
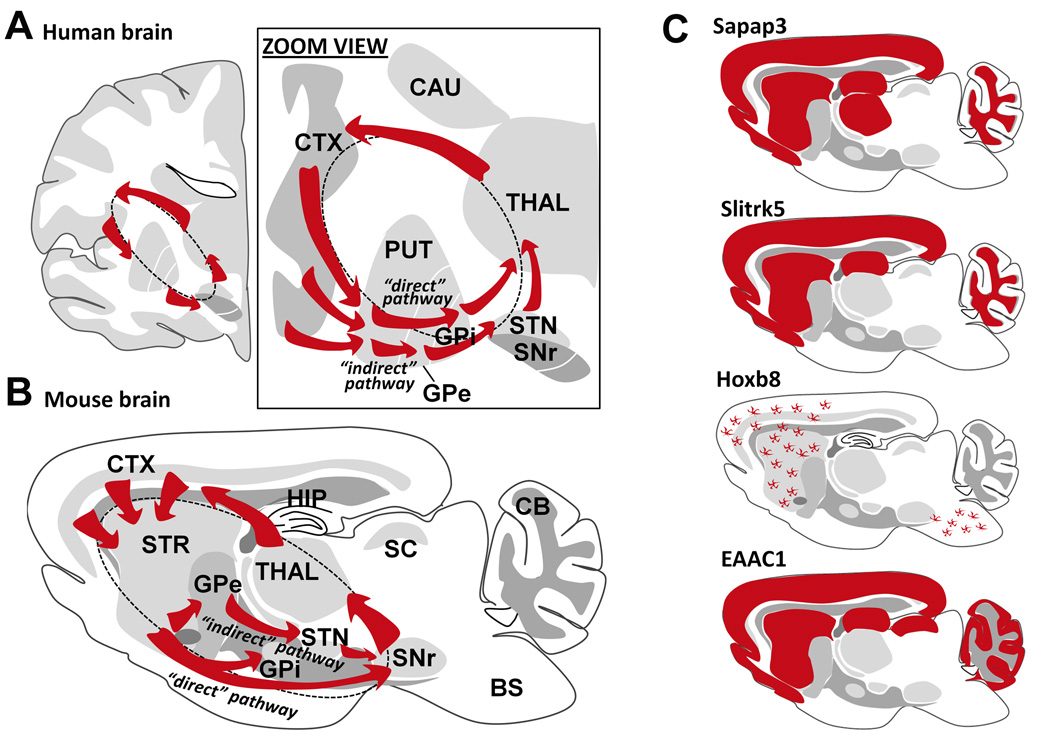
Diverse functional brain imaging technologies have allowed researchers to delve deep into the brains of OCD patients to seek out aberrations in neural circuits that control behavior. Over the past 25 years these noninvasive imaging approaches have consistently identified abnormal patterns of activity in a particular circuit, the CSTC loop [6] (Figure 1), and these studies have been highly influential in synthesizing the modern views on the neurobiology of OCD. Perhaps equally important over this span were emerging views on basal ganglia circuitry function, such as the description of numerous parallel and partially closed loops through the CSTC pathway proposed to sub-serve discrete motor or cognitive functions [7]. This model has been revised to incorporate the proposed opposing functions of the “direct” versus “indirect” projection pathways of the basal ganglia as well as compartmentalization of function with respect to neurochemically defined striosome and matrix [8–11]. One prominent hypothesis, which integrates the human OCD imaging findings with these earlier models on basal ganglia circuitry function, posits that hyperactivity of the orbitofrontal-subcortical loops caused by a disruption in the balance of activity through these opposing basal ganglia pathways (specifically, excessive direct pathway activation) underlies the manifestation of OCD symptoms [6].
Figure 1. Central role of the CSTC circuitry in obsessive-compulsive disorder in humans and compulsive-repetitive behaviors in mice.
A. Diagram of a human brain section (coronal) illustrating a simplified CSTC loop. Right panel, zoom view of the CSTC loop illustrating the intermingled but functionally distinct “direct” and “indirect” projection pathways of the basal ganglia that are thought to exert opposing control over selection of motor behaviors. B. Diagram of a mouse brain section (sagittal) illustrating the equivalent CSTC loop in the corresponding rodent brain structures. Abbreviations: CTX, cortex; STR, striatum; CAU, caudate; PUT, putamen; HIP, hippocampus; THAL, thalamus; STN, sub-thalamic nucleus; SNr, substantia nigra pars reticulata; GPe, globus pallidus externa; GPi, globus pallidus interna; SC, superior colliculus; BS, brain stem; CB cerebellum. C. Highly simplified diagram of candidate OCD gene expression patterns throughout the mouse brain demonstrating extensive overlap of expression in brain regions composing the CSTC circuitry. NOTES: The Sapap3 expression pattern is based on in situ data as reported in [17]. The Slitrk5 expression pattern is based on LacZ activity as reported in [25]. The Hoxb8 expression pattern was inferred from [28], and importantly this pattern is intended merely to reflect the regions of highest concentration of Hoxb8-expressing microglia rather than all Hoxb8-expressing microglia in the brain. The EAAC1 expression pattern is based on anti-EAAC1 antibody staining in brain slices as reported in [35].
While surely this represents an oversimplification of the neural circuitry that gates obsessions and compulsive behavior, it provides a useful theoretical framework for devising testable hypotheses on the mechanisms of circuitry dysfunction in OCD. Surprisingly, despite the accumulating evidence for the involvement of the CSTC circuit dysfunction and the proposed role of basal ganglia circuitry imbalance, there has been a marked absence of direct experimental evidence in the past two decades to support or refute this idea. The most likely explanations include ethical issues that preclude the majority of invasive procedures in human patients and the lack of well-established alternative animal models for exploring such detailed mechanistic insights. In this light, we concisely review the most recent progress specifically toward development of novel genetic animal models of OCD and explore intersections with recent human genetics studies on OCD. Comprehensive reviews on the various other animal models relevant to OCD-like behaviors have been covered elsewhere [12–16].
Recent insights from genetic mouse models
Sapap3 null mice
SAP90/PSD95-associated protein 3 (SAPAP3) belongs to a family of four homologous genes encoding SAPAP proteins that are widely yet differentially expressed in the nervous system [17]. SAPAP3 is localized to the postsynaptic density (PSD) at excitatory synapses and is the only family member strongly expressed in the striatum. Genetic deletion of Sapap3 in mice caused behavioral abnormalities consisting of increased anxiety and compulsive self-grooming to the point of facial hair loss and skin lesions [18]. Sapap3 null mice were also found to have defects in glutamatergic transmission at cortico-striatal synapses, and both synaptic and behavioral defects were rescued by virus-mediated reintroduction of SAPAP3 specifically into the striatum [18], thus confirming the critical role of cortico-striatal circuitry function to the expression of compulsive grooming behavior. Repeated administration of fluoxetine (which is known to be effective in treating human OCD) successfully alleviated compulsive grooming and anxiety.
These findings on Sapap3 null mice prompted two recent genetic studies of Sapap3 and OCD. Züchner et al. [19] performed Sapap3 gene re-sequencing analysis in OCD and trichotillomania (TTM) case samples. This study identified seven rare non-synonymous heterozygous Sapap3 variants. The combined load of these rare Sapap3 mutations was significantly higher in OCD/TTM cases compared to controls. These findings await further validation, including analysis of the functional relevance of these rare mutations. Additionally, a relatively large family-based gene association study of Sapap3 in OCD and grooming disorders has also been conducted [20]. The evidence suggests that multiple variations in the Sapap3 gene are associated with grooming disorders. No direct association between Sapap3 variants and OCD was reported, although it is noteworthy that grooming disorders without OCD were uncommon in this study. With this in mind the authors suggest the possibility that Sapap3 variants may be involved in a subtype of OCD involving pathological grooming behaviors.
Slitrk5 null mice
Slit and Trk-like proteins (Slitrks) represent a relatively newly discovered family of structurally related transmembrane proteins that are predominantly expressed in the CNS and regulate neurite outgrowth and neuronal survival. Although not consistently replicated, prior work supports a link between Slitrk1 and Tourette syndrome [21] as well as TTM [22], and Slitrk1 was shown to be highly expressed in significant portions of the CSTC circuitry [23]. However, Slitr1 null mice display only limited behavioral abnormalities such as moderately elevated anxiety [24]. In contrast, more recently described mice in which the Slitrk5 coding region was replaced with the LacZ reporter gene (a null/reporter allele) exhibit compulsive self-grooming and increased anxiety [25]. The LacZ expression allowed unequivocal determination of the predominantly neuronal expression pattern throughout cortex and striatum. Slitrk5 was found to localize to the PSD and mutant mice further displayed significant alterations in striatal ionotropic glutamate receptor subunit expression in PSD enriched fractions and functional disruption of cortico-striatal glutamatergic transmission. The compulsive grooming was corrected by chronic fluoxetine treatment. These findings bear striking similarity to those reported for the Sapap3 null mice, and in both models virtually all homozygous mutants develop overgrooming-induced facial lesions at 3–6 months of age, with less severe defects including delayed appearance of lesions in heterozygous mice [18,25]. In addition, the Slitrk5 mice had reduced striatal volume and dendritic complexity of striatal medium spiny neurons, and elevated neuronal activity (indicated by elevated FosB expression) specifically in orbito-frontal cortex, providing further evidence to strengthen the relevance of this model to OCD in humans. The collective findings on Slitrk1 and Slitrk5 may point to a common pathway to neuropsychiatric disorders through disruption of Slitrk gene function in the CNS [26].
Hoxb8 null mice
The investigations focused on Hoxb8 mutant mice over the past decade have provided unexpected discoveries and striking insights concerning the causes of compulsive grooming in mice. In 2002, the Capecchi lab reported that Hoxb8lox mutant mice exhibited compulsive grooming and fur loss with 100% penetrance [27]. The mutant mice engaged in excessive self-grooming as well as excessive grooming of wildtype cage-mates, and this phenotype was identical on two different genetic backgrounds, thus providing strong evidence for a specific role of Hoxb8 in normal grooming behavior. This was unexpected given that Hoxb8 is a member of a large family of transcription factors best known for their important roles in establishing body patterning during embryonic development. However, Hoxb8 expression is detected in adult brain, including regions comprising the CSTC circuitry. It was not until 2010 that we learned the expression of Hoxb8 which is evident in brain did not in fact originate from brain, but rather, came from bone marrow-derived microglia that migrate into the brain in the postnatal period [28]. Cell-type specific disruption of Hoxb8 restricted to this microglia progenitor population fully recapitulated the grooming defects. Remarkably, bone marrow transplantation from Hoxb8 mutants into wildtype mice led to increased grooming and fur loss in a subset of mice, while bone marrow transplantation from wildtype mice into Hoxb8 mutants completely rescued the pathological grooming in a subset of mice. Further studies are needed to clarify exactly how Hoxb8 deficient microglia impact neural circuitry involved in grooming behavior, although it is already recognized that microglia have diverse roles in regulating brain function [29]. The evidence on Hoxb8 in mice reminds us that although OCD is believed to be a disorder caused by dysfunctional neurons within CSTC circuits, the underlying causal insults need not be exclusively neuronal or even waged by cells that originate in the brain at all. This finding adds food for thought in the ongoing debate concerning a subtype of childhood-onset OCD that is thought to be precipitated by autoimmune dysfunction following streptococcal infections [30].
Slc1a1/EAAC1 null mice
The neuronal excitatory amino acid transporter EAAC1 has a dual role in regulating neuronal function through limiting glutamate diffusion in extrasynaptic regions [31], and mediating neuronal cysteine transport, an essential rate-limiting step in the production of the endogenous antioxidant glutathione [32]. EAAC1 null mice exhibit a range of neuronal defects largely due to increased vulnerability to oxidative stress in multiple brain regions [32,33]. Given that the strongest and most well-replicated findings of genetic linkage in OCD center on Slc1a1 [34], the gene that encodes EAAC1, it is of great interest whether EAAC1 null mice exhibit OCD-like behaviors. It has been reported that EAAC1 null mice beyond one year of age exhibit increased aggression and excessive self-grooming, and approximately 30% of these mice develop fur loss [32] (Dr. Raymond Swanson, personal communication). This is intriguing given the neuronal perisynaptic localization and strong expression in the CSTC circuitry [35]. In addition, EAAC1 functionally interacts with NMDA receptor subunits [36], which is interesting given that a GRIN2B variant was previously reported to be associated with OCD [37], and since NMDAR subunit expression in the PSD fraction is significantly altered in Sapap3 null mice [18]. One rare variant in Slc1a1 has been identified in a single OCD family to date [38]. EAAC1 homozygous loss-of-function mutations are exceedingly rare in humans and cause the renal condition dicarboxylic aminoaciduria. It is provocative that one such patient self-reported lifelong obsessive-compulsive behaviors but declined formal psychological evaluation [39].
The elevated widespread oxidative stress observed in EAAC1 null mice was alleviated by treatment with N-acetyl-cysteine (NAC), a cell-permeable amino acid that can normalize neuronal glutathione levels [32,33]. It is of great interest that NAC is currently being explored in clinical trials for the treatment of OCD on the basis of putative anti-glutamatergic properties relating to transporter activity [4], and recent studies indicate an improvement in symptom severity with NAC treatment in SSRI-refractory OCD and TTM patients [40,41]. It would seem the importance of EAAC1-dependent glutathione synthesis may be under-appreciated in this context. In light of the weak evidence to support EAAC1 null mice as a bona fide model for OCD-like behaviors but strong evidence of genetic linkage for Slc1a1 in OCD, EAAC1 functional deficits may confer broad susceptibility when coincident with other rare mutations in a variety of genes important for CSTC circuitry function.
In search of a common neural circuitry defect
Despite the varying degrees to which each genetic mouse model recapitulates core aspects of the human condition of OCD, some notable commonalities have emerged. First, no single model is sufficient to recapitulate the entirety of the human condition of OCD. This is especially true given that the presence and content of obsessional thinking that is intimately tied to compulsive behavior is perhaps impossible to assess in a mouse [12]. Thus, it is important to focus on robust and easily quantifiable behaviors—in this case compulsive grooming—for which we can pinpoint and probe the underlying neural circuitry defects. Second, with respect to the genes that are disrupted in the genetic mouse models described herein, there is a striking degree of overlap in the endogenous expression patterns throughout the brain, and the regions of overlap are the same regions strongly implicated in human OCD (Figure 1). Third, mounting functional evidence from these recently developed genetic mouse models also demonstrates convergence on CSTC circuitry in OCD-like behaviors, including evidence for cortico-striatal synaptic dysfunction and orbito-frontal hyperactivity, which are highly consistent with earlier functional imaging data from human OCD cases. Sustained intensified effort on this front will be necessary to fill in crucial gaps in our understanding of the origins of common circuitry defects in OCD, such as elucidating how glial and immune system dysfunction might perturb neuronal function in the CSTC circuitry.
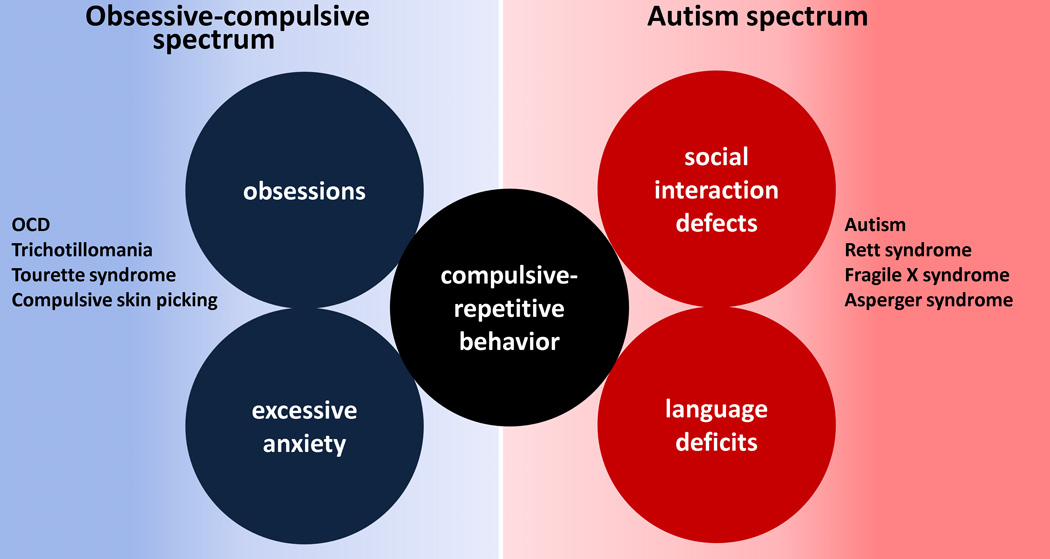
The core feature of compulsive-repetitive behavior is not unique to OCD. In fact, this feature is central to an extensive group of broader neuropsychiatric disorders. Some such disorders (TTM, Tourette syndrome, and compulsive skin picking) fall into the obsessive-compulsive spectrum of disorders, while others (Autism, Asperger syndrome, Fragile X syndrome, and Rett syndrome) fall into a category called autism-spectrum disorders (ASDs) (Figure 2). Importantly, it is estimated that as many as 30–40% of autistic patients are also diagnosed with OCD [42], and there are high rates of co-morbidity with OCD in other ASDs. The recent development of novel genetic mouse models of autism and ASD-like behaviors that specifically exhibit robust compulsive-repetitive behaviors [43,44] will no doubt help researchers to search out common circuitry defects and improve our understanding of these presently perplexing human conditions.
Figure 2. Compulsive-repetitive behavior is a core feature that is shared between obsessive-compulsive spectrum disorders and autism spectrum disorders.
Specific features of obsessive-compulsive spectrum disorders include obsession and excessive anxiety; whereas specific features of autism spectrum disorders include social interaction defects and language deficits.
Conclusions and future perspectives
Searching out common circuitry defects in genetic animal models of OCD and various other disorders with overlap in the domain of compulsive-repetitive behaviors represents one of the most promising directions for future research in this field. In this respect it is important to urge inclusive (yet with tempered skepticism) as opposed to dismissive views concerning novel animal models. No animal model will adequately capture all aspects of a complex human disorder, yet significant aspects of specific core features can reasonably be investigated in a salient neurobiological context. Furthermore, genetic animal models represent an exceptionally attractive platform for carrying out detailed investigations on the functional impacts of novel candidate gene mutations identified from genetic studies of human OCD. Given the polygenic and heterogeneous nature of OCD and related disorders, we should welcome the availability of diverse genetic animal models and actively explore interactions across multiple mutations that may converge on a common pathway of brain function. This strategy should hasten progress in the search for genes that may be causal and genes that may confer susceptibility to the expression of compulsive-repetitive behaviors. Elucidation of common circuitry mechanisms will greatly facilitate the development of more effective treatments for these debilitating disorders.
Research Highlights.
- OCD is a prevalent neuropsychiatric disorder
- Cortico-striatal-thalamo-cortical circuits are central to OCD core features
- Several recently described genetic mouse models exhibit OCD-like behaviors
- Genetic mouse models may help researchers identify common circuitry defects in OCD
- Common circuitry defects may also help to explain key aspects of autism spectrum disorders
Acknowledgements
We are grateful to Dr. Tanya Daigle for constructive comments on the manuscript. G.F. is supported by grants from the National Institutes of Health (NIMH R01MH081201), The Hartwell Foundation, Simons Foundation Autism Research Initiative (SFARI), Stanley Center for Psychiatric Research, and the SPARC program from Broad Institute of MIT and Harvard. J.T.T. would like to acknowledge support from NARSAD: The Brain and Behavior Research Fund (Young Investigator Award) and the NIMH (Ruth L. Kirschstein National Research Service Award F32MH084460).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest
None declared
References and recommended reading
Papers of particular interest, published within the annual period of review, have been highlighted as:
• of special interest
•• of outstanding interest
- 1.Weissman MM, Bland RC, Canino GJ, Greenwald S, Hwu HG, Lee CK, Newman SC, Oakley-Browne MA, Rubio-Stipec M, Wickramaratne PJ, et al. The cross national epidemiology of obsessive compulsive disorder. The Cross National Collaborative Group. J Clin Psychiatry. 1994;55 Suppl:5–10. [PubMed] [Google Scholar]
- 2.Karno M, Golding JM, Sorenson SB, Burnam MA. The epidemiology of obsessive-compulsive disorder in five US communities. Arch Gen Psychiatry. 1988;45:1094–1099. doi: 10.1001/archpsyc.1988.01800360042006. [DOI] [PubMed] [Google Scholar]
- 3.Jenike MA. Clinical practice. Obsessive-compulsive disorder. N Engl J Med. 2004;350:259–265. doi: 10.1056/NEJMcp031002. [DOI] [PubMed] [Google Scholar]
- 4.Pittenger C, Krystal JH, Coric V. Glutamate-modulating drugs as novel pharmacotherapeutic agents in the treatment of obsessive-compulsive disorder. NeuroRx. 2006;3:69–81. doi: 10.1016/j.nurx.2005.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Haynes WI, Mallet L. High-frequency stimulation of deep brain structures in obsessive-compulsive disorder: the search for a valid circuit. Eur J Neurosci. 2010;32:1118–1127. doi: 10.1111/j.1460-9568.2010.07418.x. [DOI] [PubMed] [Google Scholar]
- 6.Saxena S, Rauch SL. Functional neuroimaging and the neuroanatomy of obsessive-compulsive disorder. Psychiatr Clin North Am. 2000;23:563–586. doi: 10.1016/s0193-953x(05)70181-7. •• This review discusses the critical findings from diverse functional imaging studies in OCD patients. These findings implicate aberrant activity in the CSTC circuitry as critically involved in the manifestation of OCD symptoms. A model is described whereby hyperactivity in frontal-subcortical circuitry, namely excessive tone in the direct pathway of the basal ganglia, leads to pathway imbalance and expression of obsessions and compulsive behaviors.
- 7.Alexander GE, DeLong MR, Strick PL. Parallel organization of functionally segregated circuits linking basal ganglia and cortex. Annu Rev Neurosci. 1986;9:357–381. doi: 10.1146/annurev.ne.09.030186.002041. • This classical review describes in considerable detail both anatomic and functional aspects of the proposed parallel, "partially closed" CSTC loops in the brain. Multiple parallel loops are hypothesized to exist, each to sub-serve discrete behavioral functions.
- 8.Albin RL, Young AB, Penney JB. The functional anatomy of basal ganglia disorders. Trends Neurosci. 1989;12:366–375. doi: 10.1016/0166-2236(89)90074-x. • This study synthesizes the existing data on basal ganglia structure and function, incorporating the proposed opposing functions of the direct and indirect projection pathways of the basal ganglia, to discuss pathophysiology of various movement disorders.
- 9.DeLong MR. Primate models of movement disorders of basal ganglia origin. Trends Neurosci. 1990;13:281–285. doi: 10.1016/0166-2236(90)90110-v. [DOI] [PubMed] [Google Scholar]
- 10.Canales JJ, Graybiel AM. A measure of striatal function predicts motor stereotypy. Nat Neurosci. 2000;3:377–383. doi: 10.1038/73949. • This study describes how functional imbalances of neuronal activation between the neurochemically defined striosome and matrix compartments of the striatum can lead to stereotypic behaviors in rats.
- 11.Gerfen CR. The neostriatal mosaic: multiple levels of compartmental organization in the basal ganglia. Annu Rev Neurosci. 1992;15:285–320. doi: 10.1146/annurev.ne.15.030192.001441. [DOI] [PubMed] [Google Scholar]
- 12.Wang L, Simpson HB, Dulawa SC. Assessing the validity of current mouse genetic models of obsessive-compulsive disorder. Behav Pharmacol. 2009;20:119–133. doi: 10.1097/FBP.0b013e32832a80ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Korff S, Harvey BH. Animal models of obsessive-compulsive disorder: rationale to understanding psychobiology and pharmacology. Psychiatr Clin North Am. 2006;29:371–390. doi: 10.1016/j.psc.2006.02.007. [DOI] [PubMed] [Google Scholar]
- 14.Ting JT, Feng G. Glutamatergic Synaptic Dysfunction and Obsessive-Compulsive Disorder. Curr Chem Genomics. 2008;2:62–75. doi: 10.2174/1875397300802010062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Joel D. Current animal models of obsessive compulsive disorder: a critical review. Prog Neuropsychopharmacol Biol Psychiatry. 2006;30:374–388. doi: 10.1016/j.pnpbp.2005.11.006. [DOI] [PubMed] [Google Scholar]
- 16.Boulougouris V, Chamberlain SR, Robbins TW. Cross-species models of OCD spectrum disorders. Psychiatry Res. 2009;170:15–21. doi: 10.1016/j.psychres.2008.07.016. [DOI] [PubMed] [Google Scholar]
- 17.Welch JM, Wang D, Feng G. Differential mRNA expression and protein localization of the SAP90/PSD-95-associated proteins (SAPAPs) in the nervous system of the mouse. J Comp Neurol. 2004;472:24–39. doi: 10.1002/cne.20060. [DOI] [PubMed] [Google Scholar]
- 18.Welch JM, Lu J, Rodriguiz RM, Trotta NC, Peca J, Ding JD, Feliciano C, Chen M, Adams JP, Luo J, et al. Cortico-striatal synaptic defects and OCD-like behaviours in Sapap3-mutant mice. Nature. 2007;448:894–900. doi: 10.1038/nature06104. •• This mouse model of OCD-like behaviors was the first genetic mouse model to show predictive validity for OCD. The mutant mice display compulsive grooming, anxiety, and cortico-striatal synaptic defects that were all alleviated by repeated fluoxetine treatment.
- 19.Zuchner S, Wendland JR, Ashley-Koch AE, Collins AL, Tran-Viet KN, Quinn K, Timpano KC, Cuccaro ML, Pericak-Vance MA, Steffens DC, et al. Multiple rare SAPAP3 missense variants in trichotillomania and OCD. Mol Psychiatry. 2009;14:6–9. doi: 10.1038/mp.2008.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bienvenu OJ, Wang Y, Shugart YY, Welch JM, Grados MA, Fyer AJ, Rauch SL, McCracken JT, Rasmussen SA, Murphy DL, et al. Sapap3 and pathological grooming in humans: Results from the OCD collaborative genetics study. Am J Med Genet B Neuropsychiatr Genet. 2009;150B:710–720. doi: 10.1002/ajmg.b.30897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Abelson JF, Kwan KY, O'Roak BJ, Baek DY, Stillman AA, Morgan TM, Mathews CA, Pauls DL, Rasin MR, Gunel M, et al. Sequence variants in SLITRK1 are associated with Tourette's syndrome. Science. 2005;310:317–320. doi: 10.1126/science.1116502. [DOI] [PubMed] [Google Scholar]
- 22.Zuchner S, Cuccaro ML, Tran-Viet KN, Cope H, Krishnan RR, Pericak-Vance MA, Wright HH, Ashley-Koch A. SLITRK1 mutations in trichotillomania. Mol Psychiatry. 2006;11:887–889. doi: 10.1038/sj.mp.4001898. [DOI] [PubMed] [Google Scholar]
- 23.Stillman AA, Krsnik Z, Sun J, Rasin MR, State MW, Sestan N, Louvi A. Developmentally regulated and evolutionarily conserved expression of SLITRK1 in brain circuits implicated in Tourette syndrome. J Comp Neurol. 2009;513:21–37. doi: 10.1002/cne.21919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Katayama K, Yamada K, Ornthanalai VG, Inoue T, Ota M, Murphy NP, Aruga J. Slitrk1-deficient mice display elevated anxiety-like behavior and noradrenergic abnormalities. Mol Psychiatry. 2010;15:177–184. doi: 10.1038/mp.2008.97. [DOI] [PubMed] [Google Scholar]
- 25.Shmelkov SV, Hormigo A, Jing D, Proenca CC, Bath KG, Milde T, Shmelkov E, Kushner JS, Baljevic M, Dincheva I, et al. Slitrk5 deficiency impairs corticostriatal circuitry and leads to obsessive-compulsive-like behaviors in mice. Nat Med. 2010;16:598–602. doi: 10.1038/nm.2125. 591p following 602. •• This study describes a mouse model for OCD-like behaviors that bears a striking similarity to the Sapap3 null phenotype. In addition, these mice have hyperactivity specifically in the orbito-frontal cortex, which has been repeatedly demonstrated in human functional imaging studies on OCD.
- 26.Proenca CC, Gao KP, Shmelkov SV, Rafii S, Lee FS. Slitrks as emerging candidate genes involved in neuropsychiatric disorders. Trends Neurosci. 2011 doi: 10.1016/j.tins.2011.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Greer JM, Capecchi MR. Hoxb8 is required for normal grooming behavior in mice. Neuron. 2002;33:23–34. doi: 10.1016/s0896-6273(01)00564-5. • The initial description of the Hoxb8lox mutant mice described compulsive self-grooming and excessive grooming of wildtype cagemates, thus demonstrating the role of Hoxb8 in regulating normal grooming behaviors. A second mutant line Hoxb8NEO was also created but not explored in detail due to skeletal defects that were attributed to disruption of the Hox gene cluster surrounding the Hoxb8 locus by the presence of the NEO cassette.
- 28.Chen SK, Tvrdik P, Peden E, Cho S, Wu S, Spangrude G, Capecchi MR. Hematopoietic origin of pathological grooming in Hoxb8 mutant mice. Cell. 2010;141:775–785. doi: 10.1016/j.cell.2010.03.055. •• This follow up study from Capecchi and colleagues provides evidence that Hoxb8 expression in the brain originates from a hematopoeitic cell lineage in bone marrow that gives rise to nearly half of all microglia. _Hoxb8_-expressing microglia migrate into the brain in the postnatal period and are concentrated in regions overlapping the CSTC circuitry. In a miraculous series of experiments involving bone marrow transplantation it is shown that _Hoxb8_-deficient microglia have a causal role in compulsive grooming behaviors.
- 29.Schlegelmilch T, Henke K, Peri F. Microglia in the developing brain: from immunity to behaviour. Curr Opin Neurobiol. 2010 doi: 10.1016/j.conb.2010.08.004. [DOI] [PubMed] [Google Scholar]
- 30.Martino D, Defazio G, Giovannoni G. The PANDAS subgroup of tic disorders and childhood-onset obsessive-compulsive disorder. J Psychosom Res. 2009;67:547–557. doi: 10.1016/j.jpsychores.2009.07.004. [DOI] [PubMed] [Google Scholar]
- 31.Scimemi A, Tian H, Diamond JS. Neuronal transporters regulate glutamate clearance, NMDA receptor activation, and synaptic plasticity in the hippocampus. J Neurosci. 2009;29:14581–14595. doi: 10.1523/JNEUROSCI.4845-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Aoyama K, Suh SW, Hamby AM, Liu J, Chan WY, Chen Y, Swanson RA. Neuronal glutathione deficiency and age-dependent neurodegeneration in the EAAC1 deficient mouse. Nat Neurosci. 2006;9:119–126. doi: 10.1038/nn1609. •• Previous work mainly focused on the putative role of EAAC1 in regulating synaptic glutamate levels. This study provided critical evidence that EAAC1 is a neuronal transporter for the amino acid cysteine, and that cysteine transport is the rate limiting step in neuronal glutathione synthesis. EAAC1 null mice exhibit neuronal glutathione depletion and dramatically enhanced susceptibility to oxidative damage, and this vulnerability could be mitigated by treatment with N-acetyl cysteine, a cell-permeable glutathione precursor.
- 33.Berman AE, Chan WY, Brennan AM, Reyes RC, Adler BL, Suh SW, Kauppinen TM, Edling Y, Swanson RA. N-acetylcysteine prevents loss of dopaminergic neurons in the EAAC1(−/−) mouse. Ann Neurol. 2010 doi: 10.1002/ana.22162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Grados MA. The genetics of obsessive-compulsive disorder and Tourette syndrome: an epidemiological and pathway-based approach for gene discovery. J Am Acad Child Adolesc Psychiatry. 2010;49:810–819. doi: 10.1016/j.jaac.2010.04.009. 819 e811–812. • This review on the genetics of OCD and Tourette syndrome provides a concise overview of the human genetic studies on the candidate gene Slc1a1 in OCD (refer to Table 1 in this review). The strongest and most well-replicated findings of genetic linkage in OCD center on Slc1a1.
- 35.Rothstein JD, Martin L, Levey AI, Dykes-Hoberg M, Jin L, Wu D, Nash N, Kuncl RW. Localization of neuronal and glial glutamate transporters. Neuron. 1994;13:713–725. doi: 10.1016/0896-6273(94)90038-8. [DOI] [PubMed] [Google Scholar]
- 36.Waxman EA, Baconguis I, Lynch DR, Robinson MB. N-methyl-D-aspartate receptor-dependent regulation of the glutamate transporter excitatory amino acid carrier 1. J Biol Chem. 2007;282:17594–17607. doi: 10.1074/jbc.M702278200. [DOI] [PubMed] [Google Scholar]
- 37.Arnold PD, Rosenberg DR, Mundo E, Tharmalingam S, Kennedy JL, Richter MA. Association of a glutamate (NMDA) subunit receptor gene (GRIN2B) with obsessive-compulsive disorder: a preliminary study. Psychopharmacology (Berl) 2004;174:530–538. doi: 10.1007/s00213-004-1847-1. [DOI] [PubMed] [Google Scholar]
- 38.Wang Y, Adamczyk A, Shugart YY, Samuels JF, Grados MA, Greenberg BD, Knowles JA, McCracken JT, Rauch SL, Murphy DL, et al. A screen of SLC1A1 for OCD-related alleles. Am J Med Genet B Neuropsychiatr Genet. 2009;153B:675–679. doi: 10.1002/ajmg.b.31001. [DOI] [PubMed] [Google Scholar]
- 39.Bailey CG, Ryan RM, Thoeng AD, Ng C, King K, Vanslambrouck JM, Auray-Blais C, Vandenberg RJ, Broer S, Rasko JE. Loss-of-function mutations in the glutamate transporter SLC1A1 cause human dicarboxylic aminoaciduria. J Clin Invest. 2011;121:446–453. doi: 10.1172/JCI44474. • This study examines the only known human cases of Slc1a1/EAAC1 complete loss-of-function, which leads to the condition dicarboxylic aminoacidurea. Two independent homozygous mutations are identified in separate family pedigrees, and intriguingly, one patient self-reported life-long behavioral features consistent with OCD but declined further psychiatric evaluation.
- 40.Lafleur DL, Pittenger C, Kelmendi B, Gardner T, Wasylink S, Malison RT, Sanacora G, Krystal JH, Coric V. N-acetylcysteine augmentation in serotonin reuptake inhibitor refractory obsessive-compulsive disorder. Psychopharmacology (Berl) 2006;184:254–256. doi: 10.1007/s00213-005-0246-6. [DOI] [PubMed] [Google Scholar]
- 41.Grant JE, Odlaug BL, Kim SW. N-acetylcysteine, a glutamate modulator, in the treatment of trichotillomania: a double-blind, placebo-controlled study. Arch Gen Psychiatry. 2009;66:756–763. doi: 10.1001/archgenpsychiatry.2009.60. [DOI] [PubMed] [Google Scholar]
- 42.Leyfer OT, Folstein SE, Bacalman S, Davis NO, Dinh E, Morgan J, Tager-Flusberg H, Lainhart JE. Comorbid psychiatric disorders in children with autism: interview development and rates of disorders. J Autism Dev Disord. 2006;36:849–861. doi: 10.1007/s10803-006-0123-0. • This study describes the co-morbidity rates of several disorders in children with autism. Of particular interest, the study found that 37% of autistic children included in the study exhibited clinical OCD.
- 43.Peca J, Feliciano C, Ting JT, Wang W, Wells MF, Venkatraman TN, Lascola CD, Fu Z, Feng G. Shank3 mutant mice display autistic-like behaviours and striatal dysfunction. Nature. doi: 10.1038/nature09965. (In Press) • This study describes a novel mouse model of autism-like behaviors resulting from disruption of the Shank3 gene. The Shank3B mutants described in this study have a near complete deletion of all putative Shank3 isoforms, and as a result these mice exhibit striatal postsynaptic dysfunction and compulsive self-grooming leading to back and neck lesions.
- 44.Chao HT, Chen H, Samaco RC, Xue M, Chahrour M, Yoo J, Neul JL, Gong S, Lu HC, Heintz N, et al. Dysfunction in GABA signalling mediates autism-like stereotypies and Rett syndrome phenotypes. Nature. 2010;468:263–269. doi: 10.1038/nature09582. • This study describes autism-like stereotypies resulting from deletion of Mecp2 from GABAergic neurons. In particular, Viaat-Mecp2−/y mice exhibited excessive self-grooming leading to fur loss and skin lesions. These mice also displayed a significant increase in the number of sequential nose-pokes in a hole-board assay for compulsive-repetitive behavior.