Pteropid Bats are Confirmed as the Reservoir Hosts of Henipaviruses: A Comprehensive Experimental Study of Virus Transmission (original) (raw)
Abstract
Bats of the genus Pteropus have been identified as the reservoir hosts for the henipaviruses Hendra virus (HeV) and Nipah virus (NiV). The aim of these studies was to assess likely mechanisms for henipaviruses transmission from bats. In a series of experiments, Pteropus bats from Malaysia and Australia were inoculated with NiV and HeV, respectively, by natural routes of infection. Despite an intensive sampling strategy, no NiV was recovered from the Malaysian bats and HeV was reisolated from only one Australian bat; no disease was seen. These experiments suggest that opportunities for henipavirus transmission may be limited; therefore, the probability of a spillover event is low. For spillover to occur, a range of conditions and events must coincide. An alternate assessment framework is required if we are to fully understand how this reservoir host maintains and transmits not only these but all viruses with which it has been associated.
Introduction
Hendra virus (HeV) and Nipah virus (NiV) are zoonotic viruses responsible for outbreaks of respiratory and neurological disease in livestock and humans. Both belong to the genus Henipavirus, subfamily Paramyxovirinae family Paramyxoviridae, and order Mononegavirales.
Originally isolated from humans and domestic animals, pteropid bats have been identified as the reservoir for both viruses. HeV antibody was first identified in the serum of Pteropus sp. bats in 1996 followed by the isolation from a grey-headed flying fox, Pteropus poliocephalus and a black flying-fox Pteropus alecto.1,2 Subsequently, both Pteropus spp. occurring in Malaysia were found seropositive for NiV neutralizing antibodies, and the virus has been isolated from Pteropus hypomelanus and Pteropus vampyrus.3–5
HeV was initially isolated from the uterine fluid of a P. poliocephalus female that had miscarried and from fetal tissues.2 NiV has been isolated from pools of voided urine of P. hypomelanus collected by Chua and others4 from under roosting bat colonies, from urine of Pteropus lylei in Cambodia, using similar techniques, and from the urine of a wild-caught P. vampyrus in peninsular Malaysia.5,6
In this study, we attempted to identify the routes of transmission between bats and their spillover hosts by using geographically appropriate henipaviruses and hosts. Specifically, we aim to determine routes of virus excretion in bats and whether their gender or pregnancy status influenced the amount and route of excreted virus. This work outlines the experimental studies and the detailed findings.
Materials and Methods
Animals.
Twenty wild-caught adult Pteropus alecto bats from Queensland, Australia (12 pregnant females [Bats 1–12], five non-pregnant females [Bats 13–17], and three males [Bats 18–20]) and eight wild-caught adult P. vampyrus bats from Malaysia (four non-pregnant females [Bats 21–24] and four males [Bats 25–28]) were used in these experiments. Pteropus alecto was chosen because its distribution overlaps the locations where HeV outbreaks have occurred and it is the most abundant species of flying fox in Australia. Pteropus vampyrus was chosen because its distribution overlaps the putative location of the NiV spillover in Malaysia, which led to the 1998–9 outbreak.
Australian bats were kept in captivity in Queensland (3 weeks) before shipment to the Commonwealth Scientific and Industrial Research Organization (CSIRO) Australian Animal Health Laboratory (AAHL). The Malaysian bats were kept at Taiping Zoo (3 months) before export to Australia. All animals were seronegative to henipavirus infection on the basis of virus neutralization tests (VNTs) at the time of capture and for the period before the experiment. Animal husbandry methods and experimental design were endorsed by the CSIRO AAHL's Animal Ethics Committee (protocol no. 1023). For the duration of the study, bats were housed in a single room at Biosafety level 4 (BSL-4). Room temperature was maintained at 22°C with 15 air changes/hour. Humidity varied between 40% and 60%. Bats were housed individually in squeeze bottom cages (750 mm wide by 570 mm deep and 600 mm high). They were fed a variety of fresh fruit and provided with water ad lib. Bat weights were recorded before the start and periodically throughout the study.
Before experimentation, animals were immobilized with a mixture of ketamine HCl (5 mg/kg) (Ketamil; Ilium, Glendenning, Australia) and medetomidine (50 μg/kg) (Domitor; Novartis, Pendle Hill, Australia) by intramuscular injection. For reversal, atipamezole (Antisedan; Novartis) was given intramuscularly at 50% of the dose used for medetomidine. At termination of the study, bats were immobilized as above, with euthanasia by cardiac exsanguination. Serology, virus isolation, and the initial stages of RNA extraction were also carried out at BSL-4; staff wore fully encapsulated suits with breathing apparatus.
Viral inoculum.
HeV used to infect Australian bats was originally isolated from P. poliocephalus.2 P. alecto bats were infected with Vero cells (passage #6) cell culture supernatant (1.5 × 107 TCID50/mL). Because of the unavailability of a bat isolate for NiV, the virus used to infect the Malaysian bats was originally isolated from the central nervous system of persons with fatal NiV encephalitis during the 1999 outbreak in Malaysia. A stock of low passage virus was grown in Vero cells and used to infect P. vampyrus individuals. The cell culture supernatant had a titer of 5 × 105 TCID50/mL.
Experimental infections.
The study was conducted in three parts: Part 1, 12 pregnant P. alecto; Part 2, 8 P. alecto; and Part 3, 8 P. vampyrus. The P. alecto were exposed oronasally as described previously with 50 × 103 TCID50 HeV. The P. vampyrus were exposed by dripping 1 mL of inoculum (50 × 103 TCID50 NiV) into the nostrils and throat and then rechallenged on Day 28 with the same virus inoculum by the same route. Clinical signs were assessed daily. In Part 1 and 2, animals were sampled, and rectal temperatures recorded every second day for 19 days. In Part 3, animals were sampled every second day for 21 days, and every second day from Days 30 to 42. Blood, urine, throat, and rectal swabs were collected at each sampling. Urine was collected by gentle manual compression of the bladder. Blood was collected from either the marginal wing vein or the uropatagial vein using a 25 gauge needle and 3 ml syringe. Swabs were placed immediately into 1 mL of viral transport medium (phosphate buffered saline [PBS] containing 100 U Penicillin, 100 μg/mL Streptomycin, and 500 μg/mL Fungizone). All specimens were stored at −80°C. Blood for serology was collected from Australian bats on either Day 10 or 11 and at postmortem, and from Malaysian bats on Days 14, 21, 28, 35, 42, and at postmortem.
The Australian bats were euthanaized on Day 20, 21, or 22 and a wide range of tissues were collected for analysis. The Malaysian bats were rechallenged on Day 28, and the experiment terminated on Day 49, 50, or 51 when a wide range of tissues were collected at postmortem.
Samples were analyzed for the presence of henipavirus genome by TaqMan analysis. Virus isolation was only attempted on samples that were positive by TaqMan analysis. Seroconversion was assessed by virus neutralization. Tissues were also preserved in formalin and prepared for immunohistochemical staining and histopathological analysis.
Serology.
A VNT was used, with either 100 TCID50 NiV or 100 TCID50 HeV and Vero cells as previously described.7 Serum neutralizing titers were recorded as the reciprocal of the serum dilution. Positive and negative controls and a back-titration of the virus were included in each test. Serum samples with a titer of 1/10 and above were assessed to be positive. Serology was carried out at BSL-4. At the time of these experiments other assays including Bioplex assays were not available.
HeV and NiV genome Taqman polymerase chain reaction assays.
Samples collected during the study and tissues collected aseptically at postmortem were assayed for the detection of henipavirus genome by TaqMan assay as previously described.7,8
Primers and TaqMan probe to detect HeV genome and NiV genome were designed from the N gene sequence of HeV (Genbank accession no. AF017149) and NiV (Genbank accession no. AF212302), respectively, using specified criteria in the Primer Express Software version 1.5 (Applied Biosystems, Foster City, CA). The specific HeV oligonucleotide primers were: Hendra-N1433F 5′-atc tca gat cca gat tag ctg caa-3′ and Hendra-N1572R 5′-atc att ttg ggc agg ttt gg-3′. The fluorogenic 5′ nuclease (TaqMan) probe was Hendra 1642comp 5′-[6-carboxy-fluorescein (FAM)]-cct ggt cat ctt tcc ttc ct-3′-[MGBNFQ]. The specific NiV oligonucleotide primers were: Nipah-N1198F 5′-tcagcaggaaggcaagagagtaa-3′ and Nipah-N1297R 5′-ccccttcatcgatatcttgatca-3′. The fluorogenic 5′ nuclease (TaqMan) probe was Nipah 1247comp 5′-[6-carboxy-fluorescein (FAM)]-tgctggcaccagacttgccctc-3′-[6-carboxy-tetramethyl rhodamine (TAMRA)].
Assays were performed using a two-step protocol consisting of an initial reverse transcription (RT) reaction followed by complementary DNA (cDNA) amplification. The appropriate virus inoculum was used as the positive control in the TaqMan assays. All TaqMan reagents were purchased from Applied Biosystems except primers, which were manufactured by Geneworks (Hindmarsh, Australia). RNA was reverse transcribed using the TaqMan Gold RT-polymerase chain reaction (PCR) kit (Applied Biosystems). RNA (3.5 μL) diluted to 500 μg/3.5 μL (tissue samples) or undiluted (swabs, urine, and blood) was added to 6.5 μL of a reaction mix containing 1× TaqMan RT buffer, 5.5 mM magnesium chloride, 2 mM deoxyNTP mixture, 2.5 μM random hexamers, 0.4 U/μL RNase inhibitor, and 1.25 U/μL MultiScribe reverse transcriptase. The samples were reversed transcribed in a Px2 thermal cycler (Hybaid; Thermo Scientific, Wilmington, MA) at 22°C for 15 min, 48°C for 30 min, and 95°C for 5 min. The cDNA (5 μL) was added to 20 μL of PCR reaction mix in each well of a MicroAmp (Applied Biosystems) optical reaction plate containing 12.5 μL of Taqman Universal PCR mastermix, 3.75 μL distilled water, 1.25 μL each of 18 μM forward and reverse primers, and 1.25 μL of 5 μM labeled probe.
The samples were tested in duplicate and amplified in a GeneAmp 7700 Sequence Detection System (Applied Biosystems) using the following program: 50°C for 2 min, 1 cycle; 95°C for 10 min, 1 cycle; 50 cycles at 95°C for 15 s, 60°C for 60 s. Primer and probe optimization experiments were done as recommended in the AB7700 Sequence Detection System protocol. A dilution series was made of each primer and probe set to determine the optimum concentrations (data not shown). Samples were positive if the cycle threshold (CT) value was < 45 cycles. If a sample tested positive it was then retested in triplicate along with a random selection of negative samples that were also tested in triplicate. The average retested CT value was recorded. Where only one or two wells in the triplicate testing registered a CT value < 45, an indeterminate result was recorded.
Virus isolation.
Samples that tested positive or indeterminate for henipavirus genome by TaqMan assay were then processed for virus isolation in Vero cells. A 10% w/v homogenate of tissue samples was prepared, blood was diluted 1 in 10 with PBS, and the fluids from swabs and urine were tested neat, as previously described.9
Histopathologic and immunohistochemical methods.
Submandibular lymph node, submandibular salivary gland, adrenal gland, tonsil, lung, kidney, bladder, spleen, heart, forebrain, hindbrain, liver, pancreas, mesenteric lymph node, ileum, genital and gonadal tissues (placenta, ovary, uterus, vagina, testis, penis), and bone marrow (hyoid and laryngeal bones) were collected. From Part 1, fetal tissues were collected from the pregnant bats, and these typically included intestine, kidney, lung, liver, brain, pancreas, adrenal, heart, and spleen. Tissues were fixed in 10% neutral buffered formalin, processed through to paraffin. A rabbit polyclonal anti-Nipah virus antibody was used as the primary antibody for tissues collected from the Malaysian bats and a rabbit polyclonal anti-Hendra virus antibody was used as the primary antibody for tissues collected from the Australian bats. Immunohistochemistry protocols were as described previously.10
Results
Animals.
The 12 pregnant P. alecto bats were captured in south-east Queensland in July 2003. The remaining P. alecto bats were captured from the same site in January 2004, with this timing overlapping the end of the birthing season for this species. The P. vampyrus bats were captured in Peninsular Malaysia in late 2005. The weights for all bats (P. alecto and P. vampryus), ranged from 540 g to 1,000 g.
Clinical observations.
All bats remained clinically well throughout the study period. No febrile responses were recorded in either Part 1 or 2 of the experiment after virus inoculation. Because of the absence of a febrile response, rectal temperatures were not recorded in Part 3. All animals maintained their initial bodyweight or exhibited a slight gain in weight and ate copious amounts of fruit.
Detection of henipavirus genome.
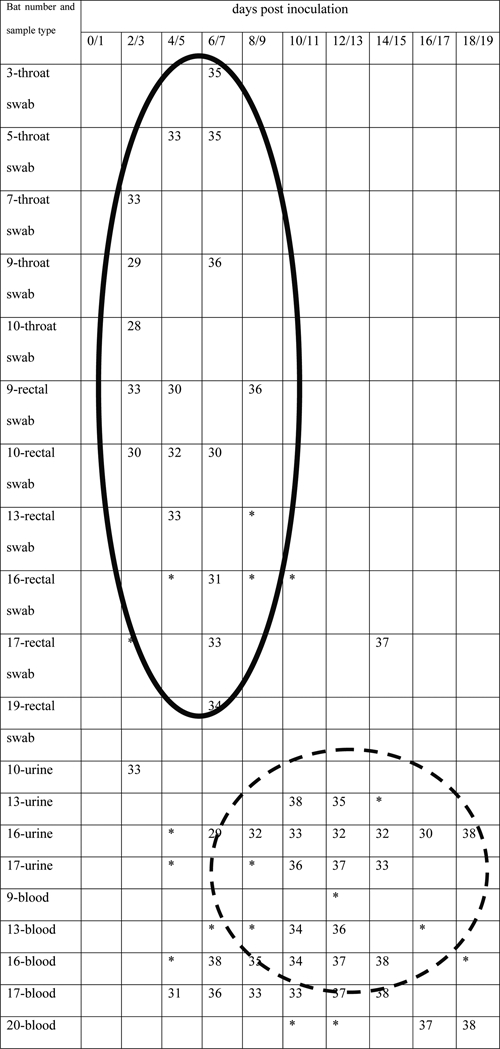
All samples collected were screened by TaqMan RT-PCR for either HeV or NiV genome, depending on the inoculum. Positive HeV TaqMan results for urine, blood, throat, and rectal swab samples are shown in Table 1. The table indicates the average cycle number (CT value) at which the sample was positive for the detection of HeV genome when tested in triplicate. Indeterminate samples, where only one or two wells registered a CT value of < 45 were also recorded. There were 46 samples that were positive for the detection of HeV genome, and an additional 18 indeterminate results.
Table 1.
CT values for the HeV TaqMan positive samples from Pteropus alecto.
At postmortem, a limited range of tissues were positive for the detection of HeV genome and these all came from bats that had samples test positive for HeV genome during the clinical sampling period (Table 2). The data does not indicate an association between virus replication and virus shedding with pregnancy. It should be noted that as animal numbers were unavoidably limited (because of the restrictions working within a BSL-4 environment) no statistical analyses could be undertaken.
Table 2.
Bats that tested positive for the detection of HeV genome during the sampling period and at postmortem, together with their antibody status at postmortem
| Sex (M/F), pregnant (P) | Bat number | TaqMan + ve samples | Sampling day number (postinoculation) of the positive sample | TaqMan + ve PM tissues | Antibody status at post mortem |
|---|---|---|---|---|---|
| F (P) | 3 | Throat swab | 6 | Lung | −ve |
| F (P) | 5 | Throat swab | 4, 6 | None | −ve |
| F (P) | 7 | Throat swab | 2 | None | −ve |
| F (P) | 9 | Throat swab | 3, 7 | Spleen | 1/10 |
| Rectal swab | 3, 5, 9 | ||||
| Blood | 13 | ||||
| F (P) | 10 | Throat swab | 3 | None | −ve |
| Rectal swab | 3, 5, 7 | ||||
| Urine | 3 | ||||
| F | 13 | Rectal swab | 4 | Spleen | 1/20 |
| Urine | 10, 12 | ||||
| Blood | 10, 12 | ||||
| F | 16 | Rectal swab | 7, 15 | Spleen Liver Kidney | −ve |
| Urine | 7, 9, 11, 13, 15, 17, 19 | ||||
| Blood | 7, 9, 11, 13, 15 | ||||
| F | 17 | Rectal swab | 7 | Spleen Lung Liver | 1/40 |
| Urine | 11, 13, 15 | ||||
| Blood | 5, 7, 9, 11, 13, 15 | ||||
| M | 19 | Rectal swab | 7 | None | −ve |
| M | 20 | Blood | 16, 18 | Spleen | −ve |
Only two samples tested positive for NiV genome, both from Bat 22; one from a throat swab on Day 4, and one from a rectal swab on Day 8 (data not shown). No postmortem tissues tested positive for NiV genome (data not shown).
Virus isolation.
Samples positive or indeterminate for henipavirus genome were inoculated onto cells for virus isolation. For Parts 1 and 2, this amounted to 64 premortem samples and 10 postmortem samples (Table 2), and in Part 3, only two samples (throat swab and rectal swab from Bat 22). Virus was isolated from one non-pregnant female bat (Bat 16), on three occasions, twice from urine on consecutive sampling days (Days 6 and 8) and once from a rectal swab on Day 6. The amount of virus recovered was at the limit of detection (virus titer < 1/8).
Postmortem.
No gross abnormalities were identified on gross postmortem examination of the bats. At postmortem Bat 15 was noted to be in the early stages of pregnancy.
Histopathology and immunohistochemistry.
Histopathological abnormalities were few. In the adrenal gland of Bat 8 there was severe, diffuse, subacute necrosis and hemorrhage of the zona fasciculata and zona reticularis extending into the adrenal medulla consistent with the exhaustion phase of a stress response. The fetal liver from Bat 6 had mild periportal mononuclear cell infiltration suggesting antigenic exposure. The endometrial glands of Bats 13 and 16 were distended, indicating possible oestrus, or perioestral activity, and Bat 15 was in the early stages of pregnancy. The testicular tissue was in active spermatogenesis in Bat 18 only. All tissues examined were negative on immunohistochemical staining for HeV or NiV antigen including the kidney and bladder of Bat 16.
Serology.
Table 3 shows a summary of the serology results from Parts 1 and 2 indicating the virus neutralizing titer and day of collection. In Part 1, by postmortem, 50% (6/12) bats had virus neutralizing titers ranging from 1/10 to 1/40. There was an additional bat that showed fleeting virus neutralization in serum at Day 10 with a titer of 1/10. In Part 2, three bats showed virus neutralization by the time of postmortem, with the maximum titer being 1/40. Table 4 shows a summary of the serology from Part 3, where for the first 3 weeks of the experiment, virus neutralization patterns mirrored those seen in the Australian bats and by Day 21 two bats had titers of 1/10. However, 7 days later, this had risen to 5/10 animals. It was at this point that bats in Part 3 were rechallenged. Seven days after this rechallenge another bat showed virus neutralization by serum, and by the conclusion of the experiment (Day 49+), the serum of 7/8 bats neutralized NiV.
Table 3.
The HeV serum neutralizing titers of the Pteropus alecto bats at 10 days postinoculation and at postmortem; all other bats (3, 5, 6, 7, 10, 14, 15, 16, 19, 20) remained seronegative (≤ 1/5) throughout the experiment
| Bat no. | Hendra virus serum neutralizing titer | |
|---|---|---|
| Day 10 pi | Postmortem† | |
| 1 | 1/20 | 1/10 |
| 2 | 1/20 | 1/10 |
| 4 | 1/40 | 1/20 |
| 8 | 1/20 | 1/40 |
| 9 | 1/20 | 1/10 |
| 11 | 1/80 | 1/40 |
| 12 | 1/10 | ≤ 1/5 |
| 13 | ≤ 1/5 | 1/20 |
| 17 | ≤ 1/5 | 1/40 |
| 18 | 1/20 | 1/20 |
Table 4.
NiV serum neutralizing titers of the Pteropus vampyrus bats*
| Bat no. | Nipah virus serum neutralizing titer | |||||
|---|---|---|---|---|---|---|
| Day 14 | Day 21 | Day 28 | Day 35 | Day 42 | Postmortem‡ | |
| 21 | ≤ 1/5 | ≤ 1/5 | 1/10 | 1/10 | 1/80 | 1/80 |
| 22 | ≤ 1/5 | 1/10 | 1/10 | 1/20 | 1/40 | 1/20 |
| 24 | ≤ 1/5 | ≤ 1/5 | ≤ 1/5 | ≤ 1/5 | 1/40 | 1/20 |
| 25 | ≤ 1/5 | ≤ 1/5 | 1/10 | 1/20 | 1/20 | 1/40 |
| 26 | ≤ 1/5 | ≤ 1/5 | ≤ 1/5 | 1/20 | ≤ 1/5 | 1/10 |
| 27 | 1/80 | 1/10 | 1/40 | 1/40 | 1/20 | 1/40 |
| 28 | ≤ 1/5 | ≤ 1/5 | ≤ 1/5 | ≤ 1/5 | ≤ 1/5 | 1/10 |
Discussion
This study confirms that while healthy Pteropus bats can be experimentally infected with henipaviruses productive infections (generation of high titer progeny viruses) were not established. One non-pregnant female P. alecto shed HeV in urine on Day 6 and Day 8 postexposure and had HeV genome in kidney at postmortem examination. Isolation of henipavirus from bat urine is consistent both with previously published laboratory data and field surveillance. In one study using a native Australian bat (P. poliocephalus), NiV was isolated on three occasions from the urine of a single bat.10 Similarly, Chua and others4 recovered the first pteropid NiV isolate from urine collected beneath the roost of P. hypomelanus and, subsequently, NiV was similarly isolated from the urine of P. lylei and from a wild-caught P. vampyrus.5,6 The presence of live virus in a rectal swab of the same bat on Day 6 is quite likely to be a contaminant from urine as the sampling procedure started with urine collection. Urine expression by manual bladder palpation in females did result in some contamination of fur in the urogenital region. Additionally, there was no other rectal swab isolate of HeV from this or any other bat.
In this study NiV was not recovered from exposed Malaysian bats. Nipah virus genome detection in samples was also very low (2/512). Both positive samples were from the same female bat; one being a throat swab on Day 4 and the other a rectal swab on Day 8. Although it is possible these results reflected primary inoculum on mucosal surfaces, it is our experience (in other species) that clearance of henipavirus inoculum occurs within 48 hours of its administration (unpublished data). Detection of genome without the subsequent detection of live virus has been seen in other studies. In a recent study involving P. alecto Japanese encephalitis virus was transmitted from experimentally infected bats to mosquitoes despite the absence of a detectable viraemia.11 In only one experimentally infected bat was Japanese encephalitis virus genome detected by TaqMan RT-PCR and this was at a very high cycle number, indicating very low levels of genome. The sample did not yield viable virus when inoculated onto cells, confirming the very low levels of virus.
The greatest incidence of HeV genome detection in rectal and throat swabs was in the first 7 days post challenge, whereas the majority of urine and blood samples with detectable HeV genome were collected after Day 7 (Table 1). This is consistent with intranasal exposure of HeV being followed by replication in mucosal surfaces with subsequent systemic infection. In this and other experiments virus isolation from exposed Pteropus bats coincided with the timing of the proposed systemic infection, at least 6 days after exposure to the virus.10,12
Only 1 in 20 bats shed infectious HeV. The virus was at low titers and was detected over a narrow time frame. Previous studies have not reported the titer of henipavirus recovered from bats; however, the low frequency of virus isolation is consistent with field data. We conclude that the opportunity for spillover of HeV from healthy bats is limited both by the amount of excreted virus and the time over which it is excreted. It follows that for an outbreak of Hendra virus to occur, a susceptible spillover species would need to be exposed, most likely to urine from an infected bat, within a very narrow window of opportunity. It is possible that this window is enlarged by certain physiological or immunological factors in some individual bats. Our data do not support either pregnancy or stress in the conventional sense being such a factor, however it should be noted that because of low experimental numbers the finding may not reflect the situation in nature. Similarly, when naive colonies are exposed to HeV and many individuals become simultaneously infected, there may be an increased likelihood of a susceptible host receiving an infectious dose. The latter mechanism has been proposed as an explanation for the sporadic nature of HeV outbreaks in horses.13
Inoculated bats survived Nipah virus challenge without developing clinical disease consistent with previous studies.10 We conclude that the opportunity for spillover of NiV from healthy bats is also rare, and similarly constrained by the short infectious period and the low intensity of infection.
Regarding the finding from VNTs on post-challenge serum samples, all positive samples had relatively low titers consistent with previous studies.12 One animal in a previous study did mount a significant antibody response with a titer > 1/640.10 However in this study, an Australian bat species (P. poliocephalus) was infected with heterologous virus (i.e., virus that naturally infects a closely related species of bats; NiV) and this may explain the increased titer seen.
The consistently low virus neutralizing titers in experimental and natural henipavirus infections in bats is in contrast to the high titers often observed during infection of other species.14 In this study, the VNT profile of the NiV-infected bats was similar to that of the HeV-infected bats up to Day 21 pi, with low titers and only a small proportion of bats (2/8) testing positive in the serum neutralizing test. However, by Day 28, 50% of the P. vampyrus had virus neutralization at low serum dilutions. After rechallenge on Day 28, three more bats showed virus neutralization by the termination of the experiment but in neither time frame were the patterns particularly suggestive of either a primary or anamnestic antibody response.
Leonard, Allen, and Sulkin15 suggested that the immune response of bats to (arbovirus) infection enhanced their effectiveness as reservoir hosts. Chakravarty and Sarkar16,17 found a high percentage (∼82%) of peripheral circulating B cells in P. giganteus and suggested that this was evidence, which corroborated earlier suggestions that the immune status of bats could be described as relatively immunodeficient. From our observations we do not believe that the immune status of bats is necessarily compromised, but rather the key immune responses to co-evolved pathogens may require alternate methods of evaluation to those described above.
Plowright and others18 showed that seroprevalence rates in Pteropus scapulatus suggested that pregnancy and lactation are risk factors for viral infection. In our study pregnancy did not influence recovery of live virus from infected bats. Plowright and others18 also reported elevated seroprevalence in a nutritionally stressed population, and suggested that there may be an increased susceptibility to viral infection caused by substantial energetic costs of immune responses. Although the bats used in this study were in good health, and did not lose bodyweight over the course of the experiment, it would be difficult to ascertain whether they were stressed in a physiological sense.
Absence of disease in infected animals is consistent with previous studies. Long-term coexistence of viruses and their hosts has given co-evolution a good chance to reach a relative equilibrium, and consequently many viruses do not cause disease in their reservoir host.19 The theory of viral co-evolution with chiropteran hosts has been previously suggested, and the findings of this study support this.20
Our studies provide valuable insight into aspects of the dynamics of henipavirus infection in the natural flying fox reservoir, but many questions remain unanswered. Current assumptions about serology and conventional host/pathogen relationships, and how such data is fed into models, must be challenged. The most significant finding of this work is that infected animals exhibited little clinical or serological evidence of henipavirus infection or associated disease. The data from this study and others18 show that pteropid bats are susceptible to henipavirus infection but, in general, the infections (experimental and field) are non-pathogenic. Collectively, these characteristics indicate that pteropid bats are true reservoir host species21–27 for henipaviruses. The data may be indicative that for an effective spillover event to occur, ecologically, physiologically or immunologically ‘primed’ bats may be necessary. To test this hypothesis further experimental trials are required to assess the impact of henipavirus infection on such animals. Finally, it must be noted that the inferences gained from the data described in this study are drawn from low numbers of experimental animals.
ACKNOWLEDGMENTS
We acknowledge the assistance of John Muschialli, Don Carlson, Gary Crameri, Jennifer McEachern, Bruce Mungall, and Christine Rootes in husbandry and sampling of the bats. We thank Kevin Lazarus and staff at the Zoo Taiping and Night Safari, Perak, Malaysia for accommodating the Pteropus vampyrus bats and facilitating their export to Australia. We also thank John Mackenzie (Curtin University, Western Australia) for his comments on the manuscript and Peter Kerr (CSIRO Entomology) and Peter Hudson (Pennsylvania State University, USA) for discussions on pathogen co-evolution.
Footnotes
Financial support: This work was supported by a National Institutes of Health/National Science Foundation “Ecology of Infectious Diseases” award (R01-TW05869) from the John E. Fogarty International Center.
Authors' addresses: Kim Halpin, Life Technologies, Singapore, E-mail: kim.halpin@lifetech.com. Alex D. Hyatt, Deborah Middleton, and John Bingham, Australian Animal Health Laboratory, Geelong, Australia, E-mails: alex.hyatt@csiro.au, deborah.middleton@csiro.au, and john.bingham@csiro.au. Rhys Fogarty, Flinders University, Flinders Medical Centre Bedford Park, Australia, E-mail: rhys.fogarty@flinders.edu.au. Jonathan H. Epstein, Tom Hughes, Peter Daszak, and the Henipavirus Ecology Research Group, EcoHealth Alliance, New York, NY, E-mails: epstein@ecohealthalliance.org, Tom.hughes@ecohealthalliance.org, and daszak@ecohealthalliance.org. Sohayati Abdul Rahman, Veterinary Research Institute, Jalan Sultan Azlan Shah 31400 Ipoh, Malaysia, E-mail: sohayati@jphvri.po.my. Craig Smith and Hume E. Field, Biosecurity Queensland, Department of Employment, Economic Development and Innovation, Animal Research Institute, Yeerongpilly, Australia, E-mails: craig.smith@deedi.qld.gov.au and hume.field@deedi.qld.gov.au.
References
- 1.Young PL, Halpin K, Selleck PW, Field H, Gravel JL, Kelly MA, Mackenzie JS. Serologic evidence for the presence in Pteropus bats of a paramyxovirus related to equine morbillivirus. Emerg Infect Dis. 1996;2:239–240. doi: 10.3201/eid0203.960315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Halpin K, Young P, Field H, Mackenzie J. Isolation of Hendra virus from pteropid bats: a natural reservoir of Hendra virus. J Gen Virol. 2000;81:1927–1932. doi: 10.1099/0022-1317-81-8-1927. [DOI] [PubMed] [Google Scholar]
- 3.Johara M, Field H, Rashdi A, Morrissy C, van der Heide B, Rota P, Adzhar A, White J, Daniels P, Jamaluddin A, Ksiazek T. Nipah virus infection in bats (order Chiroptera) in Peninsular Malaysia. Emerg Infect Dis. 2001;7:439–441. doi: 10.3201/eid0703.010312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chua KB, Koh CL, Hooi PS, Wee KF, Khong JH, Chua BH, Chan YP, Lim ME, Lam SK. Isolation of Nipah virus from Malaysian Island flying-foxes. Microbes Infect. 2002;4:145–151. doi: 10.1016/s1286-4579(01)01522-2. [DOI] [PubMed] [Google Scholar]
- 5.Rahman SA, Hassan SS, Olival KJ, Mohamed M, Chang LY, Hassan L, Saad NM, Shohaimi SA, Mamat ZC, Naim MS, Epstein JH, Suri AS, Field HE, Daszak P. Characterization of Nipah virus from naturally infected Pteropus vampyrus bats, Malaysia. Emerg Infect Dis. 2010;16:1990–1993. doi: 10.3201/eid1612.091790. Henipavirus Ecology Research Group. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Reynes JM, Counor D, Ong S, Faure C, Seng V, Molia S, Walston J, Georges-Courbot MC, Deubel V, Sarthou JL. Nipah virus in Lyle's flying foxes, Cambodia. Emerg Infect Dis. 2010;11:1042–1047. doi: 10.3201/eid1107.041350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mungall BA, Middleton D, Crameri G, Bingham J, Halpin K, Russell G, Green D, McEachern J, Pritchard I, Eaton BT, Wang LF, Bossart KN, Broder CC. Feline model of acute Nipah virus infection and protection with a soluble glycoprotein-based subunit vaccine. J Virol. 2006;80:12293–12302. doi: 10.1128/JVI.01619-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mungall BA, Schopman NC, Lambeth L, Doran TJ. Inhibition of Henipavirus infection by RNA interference. Antiviral Res. 2008;80:324–331. doi: 10.1016/j.antiviral.2008.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Middleton DJ, Westbury HA, Morrissy CJ, van der Heide BM, Russell GM, Braun MA, Hyatt AD. Experimental Nipah virus infection in pigs and cats. J Comp Pathol. 2002;126:124–136. doi: 10.1053/jcpa.2001.0532. [DOI] [PubMed] [Google Scholar]
- 10.Middleton DJ, Morrissy CJ, van der Heide BM, Russell GM, Braun MA, Westbury HA, Halpin K, Daniels PW. Experimental Nipah virus infection in pteropid bats (Pteropus poliocephalus) J Comp Pathol. 2007;136:266–272. doi: 10.1016/j.jcpa.2007.03.002. [DOI] [PubMed] [Google Scholar]
- 11.van den Hurk AF, Smith CS, Field HE, Smith IL, Northill JA, Taylor CT, Jansen CC, Smith GA, Mackenzie JS. Transmission of Japanese encephalitis virus from the black flying fox, Pteropus alecto, to Culex annulirostris mosquitoes, despite the absence of detectable viremia. Am J Trop Med Hyg. 2009;81:457–462. [PubMed] [Google Scholar]
- 12.Williamson M, Hooper P, Selleck P, Westbury H, Slocombe R. Experimental Hendra virus infection in pregnant guinea-pigs and fruit bats (Pteropus poliocephalus) J Comp Pathol. 1999;122:201–207. doi: 10.1053/jcpa.1999.0364. [DOI] [PubMed] [Google Scholar]
- 13.Plowright RK, Foley P, Field HE, Dobson AP, Foley JE, Eby P, Daszak P. Urban habituation, ecological connectivity and epidemic dampening: the emergence of Hendra virus from flying foxes (Pteropus species) Proceedings of the Royal Society B. 2011 doi: 10.1098/rspb.2011.0522. DOI:10.1098/rspb.2011.0522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Williamson M, Hooper P, Selleck P, Gleeson L, Daniels P, Westbury H, Murray K. Transmission studies of Hendra virus (equine morbillivirus) in fruit bats, horses and cats. Aust Vet J. 1998;76:813–818. doi: 10.1111/j.1751-0813.1998.tb12335.x. [DOI] [PubMed] [Google Scholar]
- 15.Leonard LL, Allen R, Sulkin SE. Bat immunoglobulins formed in response to experimental japanese B encephalitis (JBE) virus infection. J Immunol. 1968;101:1168–1175. [PubMed] [Google Scholar]
- 16.Chakravarty AK, Sarkar SK. Immunofluorescence analysis of immunoglobulin bearing lymphocytes in the Indian fruit bat: Pteropus giganteus. Lymphology. 1994;27:97–104. [PubMed] [Google Scholar]
- 17.Chakraborty AK, Chakravarty AK. Antibody-mediated immune response in the bat, Pteropus giganteus. Dev Comp Immunol. 1984;8:415–423. doi: 10.1016/0145-305x(84)90048-x. [DOI] [PubMed] [Google Scholar]
- 18.Plowright RK, Field HE, Smith C, Divljan A, Palmer C, Tabor G, Daszak P, Foley JE. Reproduction and nutritional stress are risk factors for Hendra virus infection in little red flying foxes (Pteropus scapulatus) Proc R Soc Lond B Biol Sci. 2008;275:861–869. doi: 10.1098/rspb.2007.1260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Domingo E. Mechanisms of viral emergence. Vet Res. 2010;41:38. doi: 10.1051/vetres/2010010. [Epub 2010 Feb 5] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Halpin K, Hyatt AD, Plowright RK, Epstein JH, Daszak P, Field HE, Wang L, Daniels PW. Emerging viruses: coming in on a wrinkled wing and a prayer. Clin Infect Dis. 2007;44:711–717. doi: 10.1086/511078. Henipavirus Ecology Research Group. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dorland WAN. Dorland's Illustrated Medical Dictionary. London: W.B. Saunders; 1994. [Google Scholar]
- 22.Henderson IF, Henderson WD. Henderson's Dictionary of Biological Terms. London: Longman Scientific & Technical; 1989. [Google Scholar]
- 23.Swinton J, Harwood J, Grenfell BT, Gilligan CA. Persistence thresholds for phocine distemper virus infection in harbour seal Phoca vitulina metapopulations. J Anim Ecol. 1998;67:54–68. [Google Scholar]
- 24.Swinton J, Woolhouse MEJ, Begon ME, Dobson AP, Ferroglio E, Grenfell BT, Guberti V, Hails RS, Heesterbeek JAP, Lavazza A, Roberts MG, White PJ, Wilson K. In: The Ecology of Wildlife Diseases. Hudson PJ, editor. Oxford: Oxford University Press; 2001. pp. 83–101. (Microparasite transmission and persistence). [Google Scholar]
- 25.Ashford RW. What it takes to be a reservoir host. Belg J Zool. 1997;127:85–90. [Google Scholar]
- 26.Mosier DA, Oberst RD. Cryptosporidiosis—a global challenge. Ann NY. 2000;916:102–111. doi: 10.1111/j.1749-6632.2000.tb05279.x. [DOI] [PubMed] [Google Scholar]
- 27.Hiroshi N, Hoye B, Klaassen M, Bauer S, Heesterbeek H. How to find natural reservoir hosts from endemic prevalence in a multi-host population: a case study of influenza in waterfowl. Epidemics. 2009;1:118–128. doi: 10.1016/j.epidem.2009.04.002. [DOI] [PubMed] [Google Scholar]