COACH Trial: A Randomized Controlled Trial of Nurse Practitioner/Community Health Worker Cardiovascular Disease Risk Reduction in Urban Community Health Centers (original) (raw)
. Author manuscript; available in PMC: 2012 Nov 1.
Published in final edited form as: Circ Cardiovasc Qual Outcomes. 2011 Sep 27;4(6):595–602. doi: 10.1161/CIRCOUTCOMES.111.961573
Abstract
Background
Despite well-publicized guidelines on the appropriate management of cardiovascular disease (CVD) and type 2 diabetes, the implementation of risk-reducing practices remains poor. This paper describes the results of a randomized controlled clinical trial evaluating the effectiveness of a comprehensive program of cardiovascular disease risk reduction delivered by nurse practitioner/community health worker (NP/CHW) teams versus enhanced usual care (EUC) to improve lipids, blood pressure, glycated hemoglobin (HbA1c), and patients’ perceptions of the quality of their chronic illness care in patients in urban community health centers.
Methods and Results
A total of 525 patients with documented cardiovascular disease, type 2 diabetes, hypercholesterolemia, or hypertension and levels of LDL-cholesterol, blood pressure or HbA1c that exceeded goals established by national guidelines were randomized to NP/CHW (n=261) or EUC (n=264) groups. The NP/CHW intervention included aggressive pharmacologic management and tailored educational and behavioral counseling for lifestyle modification and problem solving to address barriers to adherence and control. As compared to EUC, patients in the NP/CHW group had significantly greater 12 month improvement in total cholesterol (difference, 19.7mg/dL), LDL cholesterol (difference,15.9 mg/dL), triglycerides (difference, 16.3 mg/dL), systolic blood pressure (difference, 6.2 mm Hg), diastolic blood pressure (difference, 3.1 mm Hg), HbA1c (difference, 0.5%), and perceptions of the quality of their chronic illness care (difference, 1.2 points).
Conclusions
An intervention delivered by a NP/CHW team using individualized treatment regimens based on treat-to-target algorithms can be an effective approach to improve risk factor status and perceptions of chronic illnes care in high risk patients.
Keywords: Randomized trial, Cardiovascular disease, Diabetes, Prevention
INTRODUCTION
Approximately 831,000 Americans die annually from cardiovascular disease (CVD), with lower income, prior coronary heart disease (CHD), and diabetes populations differentially represented in these deaths.1 Despite well-publicized guidelines on the appropriate management of cardiovascular disease (CVD) and type 2 diabetes, implementation of risk-reducing practices remains poor. Several different models of chronic disease case management have emerged to respond to growing concerns about the quality and increasing costs of health care; however, evaluation of their impact on patient outcomes or cost is limited.
Case management by a specially trained nurse-led team, including community health workers, has been shown to be among the most efficacious strategies to improve management of CVD risk factors in many studies.2–6 Several studies have shown that nurse management clinics are at least as beneficial in achieving goals as are other clinics managed by physicians, and in many cases actually result in marked improvement in the outcomes including patient satisfaction and utilization of healthcare services, compared with usual care. For example, trained nurses providing care have demonstrated successful strategies for improving lipid levels in patients with elevated low-density lipoprotein cholesterol (LDL-C) and blood pressure (BP).4–9 In the nurse management models, factors such as patient education and counseling and even regular telephone follow-up by a nurse showed marked sustained improvement in medication adherence and goal achievement. Nurse case managers have been shown to improve adherence to guidelines in part by serving as a bridge to physician care and by adhering more strictly to management algorithms, including many counseling features that are not within the time frame of a busy physician in practice. Several studies suggest that a nurse-led team management program is the most effective strategy to date for reducing LDL-C.6, 10
Nurses managing patients with diabetes also have a more favorable impact on chronic disease parameters, including adherence to recommendations for diet and for renal testing.11 Nurse case management improves control of diabetes in clinical settings, with significant reductions in fasting blood glucose, body weight, glycosylated hemoglobin, and LDL-C.12 Telephone management of diabetic patients by a nurse has been shown to markedly improve CHD risk factors, including lipids. Diabetic patients were more likely to be appropriately treated with a lipid lowering therapy when managed by the nurse over the phone than patients managed solely with usual care.13
In low income and minority populations, community health workers (CHWs) or lay health advisors have often participated in team-based care for the management of CVD risk factors, particularly hypertension and diabetes.14, 15 While there are too few randomized clinical trials of the role of these individuals, there is sufficient collective experience to suggest that this role can be an important one in improving adherence in high risk subsets of the population.9, 16–18 Trained CHWs, front line health and human service care providers, most often share the same ethnicity, geographic community, and socioeconomic background of the patients they serve. The theoretical rationale for using CHWs is a shared perspective and experience that enhances trust between CHW and the patient, and enables the CHW to effectively link underserved populations to healthcare resources where traditional health education and outreach efforts have failed.19, 20 CHWs also bridge the communication barriers between patients and health care providers which can catalyze provider and health system changes.21, 22 CHWs have been shown to improve quality of care, satisfaction with care, increase access to care, reduce healthcare costs, strengthen local economies and families, and foster community capacity building.15, 20, 23–25 CHWs also have been shown to be effective in research as interviewers and interventionists.9, 17, 21, 26
The aim of this study was to evaluate the effectiveness of a comprehensive program of CVD risk reduction delivered by nurse practitioner (NP)/CHW teams versus enhanced usual care to improve lipids, blood pressure, and HbA1c levels in patients in urban community health centers. This effectiveness research is one of the first studies testing a model of NP/CHW team care in urban federally-qualified community health centers. We used community based participatory research establishing a true academic health center-community practice partnership to enhance the applicability and sustainability of the intervention.
METHODS
Study design
The complete methods of the Community Outreach and Cardiovascular Health (COACH) study have been detailed elsewhere.27 Briefly, we used community-based participatory research (CBPR) as a theoretical framework for this study. CBPR is a methodology that promotes active community involvement in the processes that shape research and intervention strategies, as well as the conduct of research studies.28. This research utilized a Community-Provider Advisory Committee to guide all aspects of the study.
COACH was a randomized controlled trial in which 525 patients were randomly assigned to one of two groups: comprehensive intensive management of cardiovascular disease (CVD) risk factors by a NP/CHW team or an enhanced usual care (EUC) control group. Individuals in the control group received usual care from their primary provider which was enhanced by feedback regarding CVD risk factors provided to the patient and their provider. Those in the intensive intervention group received enhanced usual care plus management by the NP/CHW team. The program included aggressive pharmacologic management, tailored educational and behavioral counseling for lifestyle modification, identification of barriers to adherence and control, phone follow-ups between visits and pre-appointment reminders.
Participants
Patients were recruited between July 2006 and July 2009 from two community health centers which are part of the federally - qualified community health center entitled Baltimore Medical Systems Incorporated (BMS). The focus of these clinics is on primary care in communities designated as medically underserved areas.
Patients identified from clinic-based computerized ICD 9 codes were eligible if they were African American or Caucasian and had diagnosed CVD defined as a prior MI, revascularization procedure for coronary disease, ischemic heart disease, stroke, peripheral vascular disease, or hypercholesterolemia, hypertension, or had diagnosed type 2 diabetes receiving any therapy. They had to be ≥ 21 years of age, and be able to speak and understand English. Patients were enrolled in the trial if they had at least one of the following criteria within the past six months at the time of the medical record reviews: (1) an LDL-C ≥ 100 mg/dl or LDL-C ≥ 130 mg/dl if no diagnosed CVD or diabetes, (2) a blood pressure > BP 140/90 mm Hg or > 130/80 mm Hg if diabetic or renal insufficiency, or (3) if diabetic, a HbA1c 7% or greater or glucose ≥ 125 mg. Patients were excluded if they had a serious life-threatening non-cardiac co-morbidity with a life expectancy of less than 5 years (AIDS or cancer for example), had a serious physician-recorded psychiatric morbidity that would preclude participating in their own care, or were sufficiently neurologically impaired to preclude participation in their own care.
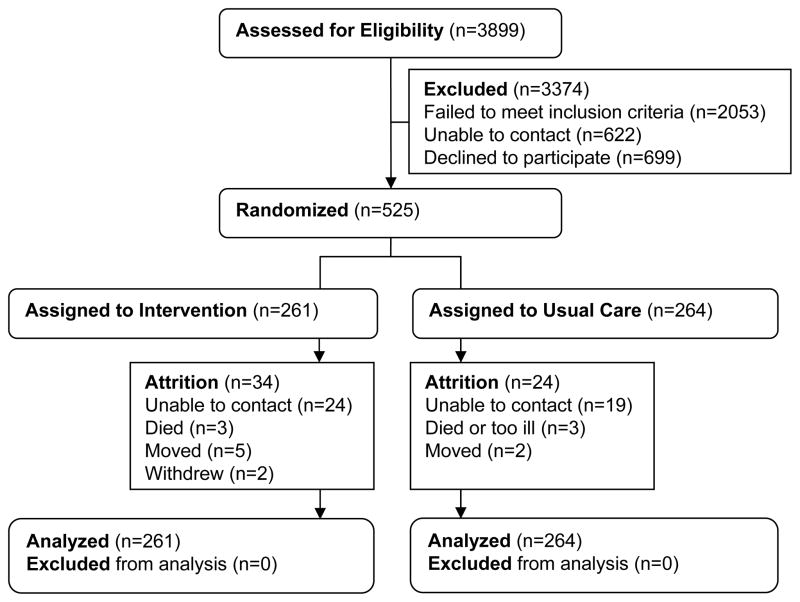
Of the 3899 screened for eligibility, 525 were enrolled in the trial (Figure 1). The participants were randomly assigned, stratified by race and sex, to receive the NP/CHW intervention or EUC. All participants provided written informed consent. The protocol was approved by the Johns Hopkins University Institutional Review Board.
Figure 1.
CONSORT diagram of COACH Trial
Intervention
The NP/CHW intervention focused on behavioral interventions to effect therapeutic lifestyle changes (TLC) and adherence to medications and appointments as well as the prescription and titration of medications. Patients were followed for one year. The NP and CHW worked as a team. The NP functioned as the case coordinator for each study participant. She oversaw the initial assessment and tailored the intervention plan, conducted the intervention including lifestyle modification, counseling and medication titration and prescription, consulted with the physician, and supervised the CHW. Specific algorithms for drug treatment of hyperlipidemia, hypertension (HBP), hyperglycemia, as well for ACE, and β-blocker therapy were developed for this study based on current guidelines and standards of care. (Algorithms can be found in the Appendix)
In addition to meeting with the NP, patients and their support person met with the CHW who spent additional time problem solving anticipated barriers to treatment adherence, including issues important to the patient’s life which might not be directly related to cardiovascular health. The CHW also reinforced instructions by the NP related to integration of lifestyle modifications and medication therapies and assisted patients in designing a set of reminders, prompts, logs, pill organizers, alarm clocks, or whatever the individual believed would work for them to assist in following complex regimens. The intensity of the nurse/CHW intervention was greater among those who had not yet achieved goals. Follow-up algorithms guided the frequency and type of follow-up. Those patients not making progress towards their goal levels received more frequent telephone follow-up from the CHW.
A low-literacy Wellness Guide was developed specifically for the study as a behavioral tool for the NP, CHW and patient team to promote TLC. The patient received the Guide at the first encounter, took it home as a tool for making changes and was asked to bring it to each visit. The Wellness Guide had sections focusing on the patient’s laboratory results and therapeutic goals for weight, blood pressure, lipids, and HbA1c (for patients with diabetes); medication reconciliation and customized tips for taking medicine; healthy eating, including strategies for portion control; increasing physical activity and a customized walking program; smoking cessation; and a place to record questions for future visits. Each section had a place for recording the patient’s goals, potential barriers, strategies to deal with difficult situations, ways to reward oneself; and identification of support people to help facilitate meeting goals. This section was completed during the counseling sessions with the NP and CHW.
The lifestyle behaviors of healthy low-fat, low sodium diet, regular moderate-intensity physical activity, and smoking cessation were the focus of TLC counseling interventions. The nurse initiated recommendations for healthy low fat, low sodium eating recommended in the TLC diet, adapted for diabetics according to standards of the American Diabetes Association. 29 The importance of dietary adherence was emphasized as an adjunct to pharmacotherapy. Recognition of food preferences were important along with how to choose low-fat, low sodium foods, modify recipes, self-monitor fat and sodium intake, and develop individualized low-fat, low-sodium eating plans. Some areas of focus included reducing portion size, reducing fast food intake, avoiding processed foods high in sodium and carbohydrates. Progress review of dietary patterns, strategies for dietary change, and guides for managing difficult situations were addressed with patients by the CHW.
Patients were instructed to participate in a moderate-intensity home-based exercise program. The patient selected the mode of moderate-intensity physical activity and set realistic goals. Telephone contact was initiated by the CHW two weeks after inception of the program and once a month until the sixth month to monitor progress, answer questions, and provide individualized feedback and positive reinforcement.
The intervention teams included NPs who were certified adult nurse practitioners with experience in the delivery of primary care and CHWs with experience working with underserved minority populations. The NPs completed additional continuing education in the management of hypertension, hypercholesterolemia, and diabetes and the CHWs were trained in the disease pathophysiology of CHD and diabetes and therapeutic lifestyle management approaches of nutrition and physical activity. Both NPs and CHWs were trained in motivational interviewing behavior change techniques.
Documenting the team’s adherence to protocols was important to assure intervention fidelity. Encounter forms for the NP and the CHW tracked the number, length, and content of the encounters (such as counseling on diet, exercise, medications, smoking cessation, and adherence) to determine the delivered dose of the intervention. In addition there was a COACH Program Intervention Quality Assurance (QA) Plan to assure adherence to study intervention protocols and treatment algorithms to promote intervention integrity throughout the study. QA assessments were conducted on a quarterly basis. The QA assessment included analysis of audio-tape recorded intervention sessions and intervention documentation in medical records. QA assessments were independently conducted by two COACH study investigators. The two independent reviewers discussed assessments and provided feedback to interventionists to provide positive reinforcement and/or a plan for additional training in a timely basis
Patients and their providers in the EUC group received the results of baseline lipids, BP, and HbA1c along with the recommended goal levels and a pamphlet on controlling risk factors published by the American Heart Association. In addition, providers received copies of the AHA/ACC Guidelines for Secondary Prevention.30
Outcome Measures
The primary outcomes were changes from baseline to one year in lipids, BP, HbA1c and patients’ perceptions of the quality of their chronic illness care. The primary outcomes also were operationalized as meeting the goals for secondary prevention or experiencing a clinically significant change as follows: HbA1c < 7% or clinically significant decrease of ≥ 0.5%; systolic BP < 140 mm Hg or < 130 mm Hg if patient had diabetes or kidney disease or clinically significant decrease of ≥ 10 mm Hg; and LDL cholesterol level, < 100 mg/dL or < 130 if no CVD or diabetes or a clinically significant decrease of ≥ 20%. The chemistry laboratory at Johns Hopkins performed all biochemical measures. Total cholesterol, triglycerides, and high-density lipoprotein cholesterol (HDL-C) were measured directly after a 12 hour fast. Low-density lipoprotein cholesterol (LDL-C) was estimated using the Friedewald equation.31 In the event of triglyceride levels greater than 400 mg/dL, direct measurement of LDL-C through ultracentrifugation methods was performed. In participants with diabetes, HbA1c was measured using high pressure liquid chromatography. Blood pressure was measured using the Omron Digital Blood Pressure Monitor HEM-907XL automatic blood pressure device according to JNC VII guidelines, following five minutes of quiet rest, in the right arm with the person seated in a chair with arm supported at heart level. The average of three blood pressures was recorded.
The patient’s ratings of care received from their health care team was measured by the Patient Assessment of Chronic Illness Care (PACIC) Survey, a 20-item patient report instrument that assesses patient’s perceptions of the receipt of clinical services and actions consistent with quality care defined by the Chronic Care Model.32 The five subscales are Patient Activation; Delivery System/Decision Support; Goal Setting; Problem-solving/Contextual Counseling; and Follow-up/Coordination.
Secondary outcomes included the lifestyle behaviors of dietary intake measured by the Habits and History Food Frequency Questionnaire, Block 2005.1,33, 34 and physical activity evaluated with the Stanford 7-Day Physical Activity Recall.35, 36 Quality of life was measured by the 5 item EuroQol questionnaire37 and resource utilization and patients’ health care utilization data were collected to conduct a cost effectiveness analysis which will be reported separately.
Statistical Analysis
The sample size for this study was determined considering the effect sizes observed in the investigators’ preliminary work. Based on the calculations, a minimum of 450 participants (225 per group) were needed to detect clinically significant differences in changes in the primary outcomes of BP, LDL-C, and HbA1c at one year to ensure 80% power at a 0.05 significance level. This sample size accounted for an expected 25% attrition at the one-year follow-up yielding 180 participants per intervention.
The data analysis for this paper was generated using SAS® version 9.2 for Windows. Statistical tests were used to study differences in baseline demographic, clinical, and risk factor characteristics, with a t-test used for continuous variables and a chi-square test for categorical variables. Similar statistical tests were used to compare baseline characteristics for subjects completing the study to those lost to follow-up for any reason.
The primary outcomes are changes from baseline to one year in lipids, BP, HgA1c, and the patient’s perception of chronic illness care. Analysis followed the intention- to- treat model including all randomized participants in the analyses according to their original assignment. Participants who withdrew or did not complete the one year assessment were included in the analysis. Missing data were imputed with multiple imputation. Multiple imputation is an advanced statistical method for handling missing data.38 This computationally intensive approach uses multiple linear regression to predict missing values with observed data. The procedure is repeated with five iterations. Repeatedly imputing missing values allows for quantifying the uncertainty resulting from sampling error.
Generalized linear mixed models (GLMM) using a random patient-level intercept model were used to build multilevel models comparing the effectiveness of the NP/CHW intervention with EUC on each outcome, controlling for the covariates of age, sex, race, body mass index, insurance status which were determined by univariate analyses to be predictive of outcomes. Mixed models are the optimal statistical method to use with pre- and post-intervention repeated measures data, as this modeling approach accounts for the correlated data structure.
RESULTS
The sample was predominantly female (71%) and Black (79%). A majority had at least a high school education; however, a majority had annual incomes less than $20,000 and fewer than half had private health insurance. There were no significant differences in sociodemographic and baseline measures between the two groups except for higher total cholesterol and HbA1c levels in the NP/CHW intervention group compared to the EUC group (Table 1). We did not find statistically significant differential attrition between the two groups. Ninety four percent (n=467) completed the 1-year assessment with no differences between completers and noncompleters in baseline lipids, HbA1c, BP, age, education, race, or sex.
Table 1.
Baseline sample characteristics
| Characteristic | Intervention (n = 261) | Usual Care (n = 264) | P |
|---|---|---|---|
| Age, y, mean (SD)* | 54.3 (12.0) | 54.7 (11.5) | 0.692 |
| Female, n (%) | 187 (71.7) | 187 (70.8) | 0.837 |
| Marital status, n (%) | 0.591 | ||
| Single | 61 (23.4) | 69 (26.1) | |
| Married | 86 (33.0) | 80 (30.3) | |
| Separated | 19 (7.3) | 28 (10.6) | |
| Widowed | 39 (14.9) | 37 (14.0) | |
| Divorced | 56 (21.5) | 50 (18.9) | |
| Race, n (%) | 0.946 | ||
| Non-black | 54 (20.7) | 54 (20.5) | |
| Black | 207 (79.3) | 210 (79.6) | |
| Education, n (%) | 0.051 | ||
| <High School | 76 (29.1) | 94 (35.6) | |
| High school/GED | 118 (45.2) | 92 (34.9) | |
| Some college | 67 (25.7) | 78 (29.6) | |
| Employment status, n (%) | 0.318 | ||
| Employed | 110 (42.2) | 100 (37.9) | |
| Not employed | 151 (57.9) | 164 (62.1) | |
| Type of insurance, n (%) | 0.403 | ||
| Private | 112 (42.9) | 105 (39.8) | |
| Medicare and/or Medicaid | 106 (40.6) | 101 (38.3) | |
| Uninsured | 43 (16.5) | 55 (20.8) | |
| Unknown | 0 (0) | 3 (1.1) | |
| Annual income, n (%) | 0.223 | ||
| <$20,000 | 137 (52.5) | 149 (56.4) | |
| ≥$20,000 | 120 (46.0) | 105 (39.8) | |
| Unknown | 4 (1.5) | 10 (3.8) | |
| Comorbidity score, mean (SD) | 1.6 (1.3) | 1.8)1.4) | 0.193 |
| Diastolic Blood Pressure, mean (SD) | 83.1 (12.6) | 82.3 (13.0) | 0.442 |
| Systolic Blood Pressure, mean (SD) | 139.7 (23.8) | 138.7 (19.9) | 0.587 |
| Total Cholesterol, mean (SD) | 199.7 (46.0) | 191.3 (45.0) | 0.036 |
| LDL-C†, mean (SD) | 121.6 (40.0) | 116.3 (40.5) | 0.132 |
| HDL-C‡, mean (SD) | 50.8 (14.7) | 50.9 (13.6) | 0.92 |
| Triglycerides, median (IQR)§ | 113 (85) | 105 (76) | 0.220 |
| Hemoglobin A1c, mean (SD) | 8.9 (2.2) | 8.3 (1.9) | 0.006 |
| PACIC[| | ](#TFN5), mean (SD) | 1.5 (0.9) | 1.6 (0.9) |
A total of 84 percent of patients randomized to the intervention group completed an initial visit, and 70 percent had at least four in-person visits with the nurse. Patients in the intervention group had a mean of 7 ± 3 in-person visits and 6 ± 5 telephone visits with the NP/CHW team. A comprehensive cost-effectiveness analysis will be published separately.
At 12 months, patients in the intervention group had significantly greater overall improvement in total cholesterol, LDL cholesterol, triglycerides, systolic and diastolic BP, HbA1c, and perceptions of the quality of their chronic illness care compared to patients receiving EUC (Table 2). The analyses using general linear mixed models controlled for age, sex, education, race, body mass index, insurance status, and an indicator of control status at baseline. The estimated between group differences were clinically significant. At the 12 month follow-up, a significantly higher percentage of patients in the intervention group compared to the EUC group had values that reached guideline goals or showed clinically significant improvements in LDL cholesterol (EUC=58%; I=75%, p<0.001), systolic BP (EUC=74%; I=82%, p=0.018), and HbA1c (EUC=47%; I=60%, p=0.016).
Table 2.
Changes in Primary Outcomes by Group
| Outcome | Intervention Group (n=261) | Usual Care Group (n=264) | P Value* | Estimated Between Group Difference (95% CI) | ||
|---|---|---|---|---|---|---|
| Change | Change | |||||
| Systolic BP, mmHg | ||||||
| Baseline | 139.7±23.8 | 8.9±25.1 | 138.7±19.9 | 2.7±22.0 | 0.003 | −6.2 (−10.2, −2.1) |
| One year | 130.8±20.7 | 135.9±20.5 | ||||
| Diastolic BP, mmHg | ||||||
| Baseline | 83.0±12.7 | 5.6±13.6 | 82.3±13.0 | 2.6±12.1 | 0.013 | −3.1 (−5.3, −0.9) |
| One year | 77.4±12.5 | 79.7±12.6 | ||||
| Total Cholesterol†, mg/dL | ||||||
| Baseline | 199.7±46.0 | 27.0±50.7 | 191.3±45.0 | 7.3±44.5 | <0.001 | −19.7 (−27.9, −11.5) |
| One year | 172.7±44.5 | 184.1±41.9 | ||||
| LDL†, mg/dL | ||||||
| Baseline | 121.6±40.0 | 21.6±44.0 | 116.3±40.5 | 5.7±38.9 | <0.001 | −15.9 (−23.0, −8.8) |
| One year | 100.1±39.2 | 110.6±36.8 | ||||
| Triglycerides †‡, mg/dL | ||||||
| Baseline | 138.1±93.4 | 20.1±88.3 | 126.8±71.5 | 3.8±65.6 | 0.013 | −16.3 (−29.6, −3.0) |
| One year | 121.3±81.6 | 123.1±72.2 | ||||
| HDL†, mg/dL | ||||||
| Baseline | 50.8±14.7 | 1.4±10.5 | 50.9±13.6 | 1.0±10.9 | 0.497 | −0.4 (−2.2, 1.4) |
| One year | 49.4±13.5 | 49.9±12.9 | ||||
| Hemoglobin A1c, % | ||||||
| Baseline | 8.9±2.2 | 0.6±2.3 | 8.3±1.9 | 0.1±1.8 | 0.034 | −0.5 (−0.9, −0.2) |
| One year | 8.3±2.2 | 8.2±2.1 | ||||
| PACIC | ||||||
| Baseline | 1.6±0.9 | −1.4±1.0 | 1.6±1.0 | −0.2±0.9 | <0.001 | 1.2 (1.0, 1.3) |
| One year | 2.9±0.9 | 1.8±1.0 |
Patients’ assessments of their chronic illness care improved significantly from baseline to one year in the intervention group (Table 3). This increase was significantly greater than the modest increase in the EUC group. These significantly different changes were present for the total score on the PACIC instrument as well as the five subscales of Patient Activation, Delivery System Design/Decision Support, Goal Setting, Problem Solving/Contextual Counseling, and Follow-up Coordination.
Table 3.
Changes in Patient Assessment of Chronic Illness Care (PACIC) Scores by Group
| Outcome | Intervention Group (n=261) | Usual Care Group (n=264) | P Value* | ||
|---|---|---|---|---|---|
| Change | Change | ||||
| Total PACIC | |||||
| Baseline | 1.6±0.9 | −1.4±1.0 | 1.6±1.0 | −0.2±0.9 | <0.001 |
| One year | 2.9±0.9 | 1.8±1.0 | |||
| Patient Activation Subscale | |||||
| Baseline | 1.5±1.2 | −1.3±1.5 | 1.4±1.2 | −0.2±1.3 | <0.001 |
| One year | 2.7±1.2 | 1.6±1.2 | |||
| Delivery System Subscale | |||||
| Baseline | 2.2±1.1 | −1.3±1.3 | 2.2±1.1 | −0.1±1.2 | <0.001 |
| One year | 3.5±0.8 | 2.4±1.1 | |||
| Goal Setting Subscale | |||||
| Baseline | 1.4±1.1 | −1.5±1.3 | 1.5±1.1 | −0.2±1.1 | <0.001 |
| One year | 3.0±0.9 | 1.7±1.2 | |||
| Problem Solving Subscale | |||||
| Baseline | 1.9±1.2 | −1.3±1.3 | 1.8±1.3 | −0.2±1.3 | <0.001 |
| One year | 3.2±1.0 | 2.0±1.3 | |||
| Follow-Up Subscale | |||||
| Baseline | 1.1±1.0 | −1.2±1.3 | 1.1±1.1 | −0.2±1.0 | <0.001 |
| One year | 2.4±1.0 | 1.4±1.1 |
Although there were greater changes in the recommended direction in the intervention group compared to EUC, there were no statistically significant differences in changes between groups in the level of physical activity, body mass index, total energy intake, saturated fat or sodium intake from baseline to one year of follow-up.
DISCUSSION
This study demonstrated that vulnerable patients with uncontrolled CVD risk factors managed by a NP/CHW intervention team achieved significant improvement in their CVD risk profiles. The improvements in the primary outcomes in this study compare favorably with changes in other studies targeting improvement in clinical outcomes and quality of care in patients with CVD and/or diabetes. In a meta-analysis of 66 trials to improve the outcomes of diabetes care, the HbA1c level decreased by a mean of 0.42% (95% CI, 0.29 to 0.54)39 versus a mean of 0.50% (95% CI, 0.2 to 0.9) in this trial. In a recent review of 11 studies of nurse-led interventions used to improve control of high blood pressure in people with diabetes, meta-analysis showed greater reductions in blood pressure in favor of nurse-led interventions (systolic weighted mean difference −5.8 mmHg, 95% CI, −9.6 to −2.0; diastolic weighted mean difference −4.2 mmHg, 95% CI, −7.6 to −0.7).40 In a systematic review of 44 trials, systolic BP decreased by a mean of 4.5 mm Hg (95% CI, 1.8 to 6.6)41 versus a mean of 6.2 (95% CI, 2.1 to 10.2) in this trial. The changes in HbA1c, BP, total and LDL cholesterol and triglycerides in this study are clinically meaningful. On a population level, they should lead to a meaningful decreases in macrovascular and microvascular disease in people with diabetes42, 43 and decreases in events in people with CVD.1
Patients in the intervention group rated the quality of care that they received for the management of their chronic conditions as increasing significantly more than patients who received EUC. Whether this translates into greater satisfaction with care is unclear; however, we know that satisfaction with care predicts better self-care and more favorable outcomes.44 The NP/CHW team enhanced patient self-care by encouraging self-monitoring, mutual goal-setting and decision-making, addressing barriers to improve adherence to medications and appointment keeping, and making proactive contact with patients to assess progress. These types of interventions are consistent with the strategies described by the Chronic Care Model to improve the performance of health care systems.45
The results of this trial support the potential for nurse-led patient-centered medical homes (PCMH) to improve the quality of care in high risk underserved populations. The concept of a PCMH is receiving increased attention as a means to improve care and potentially reduce costs. The PCMH has its origins in care for children with chronic conditions.46 In March 2007, the American Academy of Pediatrics, American Academy of Family Practice, American College of Physicians, and American Osteopathic Association published a joint statement of principles calling for accessible, continuous, team-based care that focuses on the whole person, with the PCMH taking responsibility for care coordination.47 In 2009, the American College of Physicians endorsed the inclusion of NP-led practices to test different PCMH models within the Medical Home Demonstration Project.48 As the costs of health care for chronic diseases continues to increase, NPs are in pivotal positions to address the need for safe, effective, patient-centered, efficient, and equitable health care.49
This study also provides evidence that a nurse-led team which includes CHWs is an effective model of care. However, adoption and sustainability of this model of care will require financing mechanisms for CHWs. Funding, reimbursement and payment policies for CHWs must be established to ensure that CHW models are adopted in mainstream health care.14, 50
The limitations of the COACH Trial include the fact that it was conducted in one federally-qualified community health system and used highly trained NPs and CHWs, which may limit generalizability. Second, the recruitment and screening process resulted in the inclusion of a sample of predominately Black women. However this represents the majority of patients seen in these and other similar community health clinics which increases confidence in the generalizability of findings to similar settings. Third, physicians had patients in both the intervention and EUC groups. This may have resulted in a change in the level of care provided to their patients in the EUC group as they received laboratory reports at baseline and tended to become more vigilant with the assessment, treatment and follow-up for cardiovascular risk factor management. This may explain the improvements in clinical measures in the EUC group. Nevertheless, improvements in clinical outcomes and perceptions of the quality of care were significantly greater among patients in the intervention group compared to the EUC group. Finally, there was a higher attrition rate in the intervention group (13%) as compared to the EUC group, 9%. However, the study was powered to account for a dropout rate of 25%. The slightly differential dropout rate in the intervention group may be due to the increased commitment to participate in the intervention group, including more visits to the clinic resulting in more costs to the participant.
CONCLUSIONS
In summary, an intervention delivered by a NP/CHW team using individualized treatment regimens based on treat-to-target algorithms can be an effective approach to improve risk factor status and perceptions of chronic illness care in high risk patients. The translation of new knowledge and efficacious interventions into the care of populations, particularly those at highest risk of multiple chronic diseases, disability and mortality, remains a national problem. This study developed a partnership with Baltimore Medical Systems, specifically to implement a program to reach this high risk population. Moreover, the design and intervention were developed in collaboration with the Community Health Centers within this System, so that the program, if found efficacious, would be sustained for long term effectiveness. Further analyses will evaluate the cost effectiveness of NP/CHW model. Further study is needed to determine if this translates into improved morbidity and mortality from CVD.
Supplementary Material
1
Acknowledgments
We gratefully thank the patients who participated in the program and the administration and staff of Baltimore Medical Systems for their collaboration in the design and implementation of the program. We also thank Margaret Denny for her assistance in the preparation of this manuscript.
Funding Sources: This study was supported by the National Heart Lung and Blood Institute, National Institutes of Health grant # R01HL082638.
Footnotes
Conflict of Interest Disclosures: None.
References
- 1.Roger VL, Go AS, Lloyd-Jones DM, Adams RJ, Berry JD, Brown TM, Carnethon MR, Dai S, De Simone G, Ford ES, Fox CS, Fullerton HJ, Gillespie C, Greenlund KJ, Hailpern SM, Heit JA, Ho PM, Howard VJ, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Makuc DM, Marcus GM, Marelli A, Matchar DB, McDermott MM, Meigs JB, Moy CS, Mozaffarian D, Mussolino ME, Nichol G, Paynter NP, Rosamond WD, Sorlie PD, Stafford RS, Turan TN, Turner MB, Wong ND, Wylie-Rosett J. Heart disease and stroke statistics--2011 update: a report from the American Heart Association. Circulation. 2011;123:e18–e209. doi: 10.1161/CIR.0b013e3182009701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Allen JK. Cholesterol management: an opportunity for nurse case managers. J Cardiovasc Nurs. 2000;14:50–58. doi: 10.1097/00005082-200001000-00007. [DOI] [PubMed] [Google Scholar]
- 3.Allen JK, Dennison CR. Randomized trials of nursing interventions for secondary prevention in patients with coronary artery disease and heart failure: systematic review. J Cardiovasc Nurs. 2010;25:207–220. doi: 10.1097/JCN.0b013e3181cc79be. [DOI] [PubMed] [Google Scholar]
- 4.Becker DM, Raqueno JV, Yook RM, Kral BG, Blumenthal RS, Moy TF, Bezirdjian PJ, Becker LC. Nurse-mediated cholesterol management compared with enhanced primary care in siblings of individuals with premature coronary disease. Arch Intern Med. 1998;158:1533–1539. doi: 10.1001/archinte.158.14.1533. [DOI] [PubMed] [Google Scholar]
- 5.DeBusk RF, Miller NH, Superko HR, Dennis CA, Thomas RJ, Lew HT, Berger WE, III, Heller RS, Rompf J, Gee D. A case-management system for coronary risk factor modification after acute myocardial infarction. Ann Intern Med. 1994;120:721–729. doi: 10.7326/0003-4819-120-9-199405010-00001. [DOI] [PubMed] [Google Scholar]
- 6.Allen JK, Blumenthal RS, Margolis S, Young DR, Miller ER, III, Kelly K. Nurse case management of hypercholesterolemia in patients with coronary heart disease: results of a randomized clinical trial. Am Heart J. 2002;144:678–686. doi: 10.1067/mhj.2002.124837. [DOI] [PubMed] [Google Scholar]
- 7.Allison TG, Squires RW, Johnson BD, Gau GT. Achieving National Cholesterol Education Program goals for low-density lipoprotein cholesterol in cardiac patients: importance of diet, exercise, weight control, and drug therapy. Mayo Clin Proc. 1999;74:466–473. doi: 10.4065/74.5.466. [DOI] [PubMed] [Google Scholar]
- 8.Brown AS, Cofer LA. Lipid management in a private cardiology practice (the Midwest Heart experience) Am J Cardiol. 2000;85:18A–22A. doi: 10.1016/s0002-9149(99)00934-0. [DOI] [PubMed] [Google Scholar]
- 9.Hill MN, Han HR, Dennison CR, Kim MT, Roary MC, Blumenthal RS, Bone LR, Levine DM, Post WS. Hypertension care and control in underserved urban African American men: behavioral and physiologic outcomes at 36 months. Am J Hypertens. 2003;16:906–913. doi: 10.1016/s0895-7061(03)01034-3. [DOI] [PubMed] [Google Scholar]
- 10.Shaffer J, Wexler LF. Reducing low-density lipoprotein cholesterol levels in an ambulatory care system. Results of a multidisciplinary collaborative practice lipid clinic compared with traditional physician-based care. Arch Intern Med. 1995;155:2330–2335. [PubMed] [Google Scholar]
- 11.Sikka R, Waters J, Moore W, Sutton DR, Herman WH, Aubert RE. Renal assessment practices and the effect of nurse case management of health maintenance organization patients with diabetes. Diabetes Care. 1999;22:1–6. doi: 10.2337/diacare.22.1.1. [DOI] [PubMed] [Google Scholar]
- 12.Ridgeway NA, Harvill DR, Harvill LM, Falin TM, Forester GM, Gose OD. Improved control of type 2 diabetes mellitus: a practical education/behavior modification program in a primary care clinic. South Med J. 1999;92:667–672. doi: 10.1097/00007611-199907000-00004. [DOI] [PubMed] [Google Scholar]
- 13.Kirkman MS, Weinberger M, Landsman PB, Samsa GP, Shortliffe EA, Simel DL, Feussner JR. A telephone-delivered intervention for patients with NIDDM. Effect on coronary risk factors. Diabetes Care. 1994;17:840–846. doi: 10.2337/diacare.17.8.840. [DOI] [PubMed] [Google Scholar]
- 14.Brownstein JN, Bone LR, Dennison CR, Hill MN, Levine DM. Community health workers as interventionists in research and practice for the prevention of heart disease and stroke. American Journal of Preventative Medicine. 2005;29:128–133. doi: 10.1016/j.amepre.2005.07.024. [DOI] [PubMed] [Google Scholar]
- 15.Fedder DO, Chang RJ, Curry S, Nichols G. The effectiveness of a community health worker outreach program on healthcare utilization of west Baltimore City Medicaid patients with diabetes, with or without hypertension. Ethn Dis. 2003;13:22–27. [PubMed] [Google Scholar]
- 16.Batts ML, Gary TL, Huss K, Hill MN, Bone L, Brancati FL. Patient priorities and needs for diabetes care among urban African American adults. Diabetes Educ. 2001;27:405–412. doi: 10.1177/014572170102700310. [DOI] [PubMed] [Google Scholar]
- 17.Hill MN, Becker DM. Roles of nurses and health workers in cardiovascular health promotion. Am J Med Sci. 1995;310(suppl 1):S123–S126. doi: 10.1097/00000441-199512000-00022. [DOI] [PubMed] [Google Scholar]
- 18.Hill MN, Bone LR, Hilton SC, Roary MC, Kelen GD, Levine DM. A clinical trial to improve high blood pressure care in young urban black men: recruitment, follow-up, and outcomes. Am J Hypertens. 1999;12:548–554. doi: 10.1016/s0895-7061(99)00007-2. [DOI] [PubMed] [Google Scholar]
- 19.Bird JA, Otero-Sabogal R, Ngoc-The H, McPhee SJ. Tailoring lay health worker interventions for diverse cultures: Lessons learned from Vietnamese and Latina communities. Health Educ & Behav. 1996;23:S105–S122. [Google Scholar]
- 20.Brownstein JN, Rosenthal EL. The final report of the National Advisor Study: Weaving the Future. Tucson, AZ: University of Arizona; 1998. The challenge of evaluating CHA services; pp. 50–74. [Google Scholar]
- 21.Love MB, Gardner K. The emerging role of the community health worker in California: results of a statewide university survey and San Francisco Bay Area focus group on the Community Health Workers in California’s public health system. San Francisco, CA: California Department of Health Services, Health Promotion Section; 1992. [Google Scholar]
- 22.Stone RI, Wiener J. Who will care for us? Addressing the long-term care workforce crisis. Washington, DC: The Urban Institute and the American Association of Homes and Services for the Aging; 2001. [Google Scholar]
- 23.Koch E, Thompson A, Keegan P. Community health workers: a leadership brief on preventive health programs. Washington, DC: The CivicHealth Institute at Codman Square Health Center and the Harrison Institute for Public Law at Georgetown University Law Center and the Center for Policy Alternatives; 1998. [Google Scholar]
- 24.Levine DM, Bone LR, Hill MN, Stallings R, Gelber AC, Barker A, Harris EC, Zeger SL, Felix-Aaron KL, Clark JM. The effectiveness of a community/academic health center partnership in decreasing the level of blood pressure in an urban African-American population. Ethn Dis. 2003;13:354–361. [PubMed] [Google Scholar]
- 25.Witmer A, Seifer SD, Finocchio L, Leslie J, O’Neil EH. Community health workers: integral members of the health care work force. Am J Public Health. 1995;85:1055–1058. doi: 10.2105/ajph.85.8_pt_1.1055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hill MN, Bone LR, Butz AM. Enhancing the role of community-health workers in research. Image J Nurs Sch. 1996;28:221–226. doi: 10.1111/j.1547-5069.1996.tb00355.x. [DOI] [PubMed] [Google Scholar]
- 27.Allen JK, Himmelfarb CR, Szanton SL, Bone L, Hill MN, Levine DM. COACH trial: A randomized controlled trial of nurse practitioner/community health worker cardiovascular disease risk reduction in urban community health centers: Rationale and design. Contemp Clin Trials. 2011;32:403–411. doi: 10.1016/j.cct.2011.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Green L, Daniel M, Novack L. Partnerships and coalitions for community-based research. Public Health Reports. 2001;116(suppl 1):20–31. doi: 10.1093/phr/116.S1.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nutrition recommendations and principles for people with diabetes mellitus. American Diabetes Association. Tenn Med. 2000;93:430–433. [PubMed] [Google Scholar]
- 30.Smith SC, Jr, Allen J, Blair SN, Bonow RO, Brass LM, Fonarow GC, Grundy SM, Hiratzka L, Jones D, Krumholz HM, Mosca L, Pearson T, Pfeffer MA, Taubert KA. AHA/ACC guidelines for secondary prevention for patients with coronary and other atherosclerotic vascular disease: 2006 update endorsed by the National Heart, Lung, and Blood Institute. J Am Coll Cardiol. 2006;47:2130–2139. doi: 10.1016/j.jacc.2006.04.026. [DOI] [PubMed] [Google Scholar]
- 31.Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18:499–502. [PubMed] [Google Scholar]
- 32.Glasgow RE, Wagner EH, Schaefer J, Mahoney LD, Reid RJ, Greene SM. Development and validation of the Patient Assessment of Chronic Illness Care (PACIC) Med Care. 2005;43:436–444. doi: 10.1097/01.mlr.0000160375.47920.8c. [DOI] [PubMed] [Google Scholar]
- 33.Block G, Hartman AM, Dresser CM, Carroll MD, Gannon J, Gardner L. A data-based approach to diet questionnaire design and testing. Am J Epidemiol. 1986;124:453–469. doi: 10.1093/oxfordjournals.aje.a114416. [DOI] [PubMed] [Google Scholar]
- 34.Block G, Thompson FE, Hartman AM, Larkin FA, Guire KE. Comparison of two dietary questionnaires validated against multiple dietary records collected during a 1-year period. J Am Diet Assoc. 1992;92:686–693. [PubMed] [Google Scholar]
- 35.Blair SN, Haskell WL, Ho P, Paffenbarger RS, Jr, Vranizan KM, Farquhar JW, Wood PD. Assessment of habitual physical activity by a seven-day recall in a community survey and controlled experiments. Am J Epidemiol. 1985;122:794–804. doi: 10.1093/oxfordjournals.aje.a114163. [DOI] [PubMed] [Google Scholar]
- 36.Sallis JF, Haskell WL, Wood PD, Fortmann SP, Rogers T, Blair SN, Paffenbarger RS., Jr Physical activity assessment methodology in the Five-City Project. Am J Epidemiol. 1985;121:91–106. doi: 10.1093/oxfordjournals.aje.a113987. [DOI] [PubMed] [Google Scholar]
- 37.EuroQol--a new facility for the measurement of health-related quality of life. The EuroQol Group. Health Policy. 1990;16:199–208. doi: 10.1016/0168-8510(90)90421-9. [DOI] [PubMed] [Google Scholar]
- 38.He Y. Missing data analysis using multiple imputation: getting to the heart of the matter. Circ Cardiovasc Qual Outcomes. 2010;3:98–105. doi: 10.1161/CIRCOUTCOMES.109.875658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Shojania KG, Ranji SR, McDonald KM, Grimshaw JM, Sundaram V, Rushakoff RJ, Owens DK. Effects of quality improvement strategies for type 2 diabetes on glycemic control: a meta-regression analysis. JAMA. 2006;296:427–440. doi: 10.1001/jama.296.4.427. [DOI] [PubMed] [Google Scholar]
- 40.Clark CE, Smith LF, Taylor RS, Campbell JL. Nurse-led interventions used to improve control of high blood pressure in people with diabetes: a systematic review and meta-analysis. Diabet Med. 2011;28:250–261. doi: 10.1111/j.1464-5491.2010.03204.x. [DOI] [PubMed] [Google Scholar]
- 41.Walsh JM, McDonald KM, Shojania KG, Sundaram V, Nayak S, Lewis R, Owens DK, Goldstein MK. Quality improvement strategies for hypertension management: a systematic review. Med Care. 2006;44:646–657. doi: 10.1097/01.mlr.0000220260.30768.32. [DOI] [PubMed] [Google Scholar]
- 42.Skyle JS, Bergenstal R, Bonow RO, Buse J, Deedwania P, Gale EA, Howard BV, Kirkman MS, Kosiborod M, Reaven P, Sherwin RS. Intensive glycemic control and the prevention of cardiovascular events: implications of the ACCORD, ADVANCE, and VA Diabetes Trials: a position statement of the American Diabetes Association and a Scientific Statement of the American College of Cardiology Foundation and the American Heart Association. J Am Coll Cardiol. 2009;53:298–304. doi: 10.1016/j.jacc.2008.10.008. [DOI] [PubMed] [Google Scholar]
- 43.Adler AI, Stratton IM, Neil HA, Yudkin JS, Matthews DR, Cull CA, Wright AD, Turner RC, Holman RR. Association of systolic blood pressure with macrovascular and microvascular complications of type 2 diabetes (UKPDS 36): prospective observational study. BMJ. 2000;321:412–419. doi: 10.1136/bmj.321.7258.412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sherbourne CD, Hays RD, Ordway L, DiMatteo MR, Kravitz RL. Antecedents of adherence to medical recommendations: results from the Medical Outcomes Study. J Behav Med. 1992;15:447–468. doi: 10.1007/BF00844941. [DOI] [PubMed] [Google Scholar]
- 45.Wagner EH, Austin BT, Von Korff M. Organizing care for patients with chronic illness. Milbank Q. 1996;74:511–544. [PubMed] [Google Scholar]
- 46.Cooley WC. Providing a primary care medical home for children and youth with cerebral palsy. Pediatrics. 2004;114:1106–1113. doi: 10.1542/peds.2004-1409. [DOI] [PubMed] [Google Scholar]
- 47.American Academy of Family Physicians, American Academy of Pediatrics, American College of Physicians, American Osteopathic Association. Guidelines for Patient-Centered Medical Home (PCMH) Recognition and Accreditation Programs. [Accessed January 28, 2011.];Guidelines for Patient-Centered Medical Home (PCMH) Recognition and Accreditation Programs. 2011 http://www.acponline.org/running_practice/pcmh/understanding/guidelines_pcmh.pdf.
- 48.American College of Physicians. Nurse Practitioners in Primary Care. Philadelphia, PA: American College of Physicians; 2009. Policy Monograph. (Available from American College of Physicans, 190 N. Independence Mall West, Philadelphia, PA 19106.) [Google Scholar]
- 49.Parsons Schram A. Medical Home and the Nurse Practitioner: A Policy Analysis. The Journal for Nurse Practitioners. 2010;6:132–139. [Google Scholar]
- 50.Dower C, Know M, Lindler V, O’Neil E. Advancing Community Health Worker Practice and Utilization: The Focus on Financing. San Francisco, CA: National Fund for Medical Education; 2006. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
1