Reduced Incidence of Lower-Extremity Amputations in People With Diabetes in Scotland: A nationwide study (original) (raw)
Abstract
OBJECTIVE
To establish the incidence of nontraumatic lower-extremity amputation (LEA) in people with diabetes in Scotland.
RESEARCH DESIGN AND METHODS
This cohort study linked national morbidity records and diabetes datasets to establish the number of people with diabetes who underwent nontraumatic major and minor LEA in Scotland from 2004 to 2008.
RESULTS
Two thousand three hundred eighty-two individuals with diabetes underwent a nontraumatic LEA between 2004 and 2008; 57.1% (n = 1,359) underwent major LEAs. The incidence of any LEA among persons with diabetes fell over the 5-year study period by 29.8% (3.04 per 1,000 in 2004 to 2.13 per 1,000 in 2008, P < 0.001). Major LEA rates decreased by 40.7% from 1.87 per 1,000 in 2004 to 1.11 per 1,000 in 2008 (P < 0.001).
CONCLUSIONS
There has been a significant reduction in the incidence of LEA in persons with diabetes in Scotland between 2004 and 2008, principally explained by a reduction in major amputation.
Diabetes-related foot disease results in major morbidity and mortality (1). National and global amputation rates vary considerably (2,3) because of confounding factors, such as ethnicity, case definition, and ascertainment of diabetes prevalence (4).The aim of this study was to establish any change in the incidence of diabetes-related nontraumatic lower-extremity amputation (LEA) in Scotland from 2004 to 2008.
RESEARCH DESIGN AND METHODS
We performed a cohort study of all people in Scotland with diabetes between January 2004 and December 2008. The Scottish Morbidity Record was the primary data source using predefined codes for categorization of amputation type (OCPS-4 codes ×07–11). This was linked with the Scottish Care Information–Diabetes Collaboration (SCI-DC) National Diabetes Register (5).
Approval for the dataset was from SCI-DC, Scottish multicenter research ethics committee, Privacy Advisory Committee of NHS National Services Scotland, and Caldicott guardians.
An LEA was defined as a complete loss in the transverse anatomical plane of any part of the limb. Major amputation was any through or proximal to the ankle and minor distal to the ankle. In patients with more than one procedure, the highest level of amputation was analyzed. Traumatic and tumor-related amputations were excluded. A diabetes-related LEA was any in a person known to have diabetes at the time of amputation or registered with diabetes within 3 months of amputation.
The national population was taken from the General Register Office for Scotland’s midpoint population estimates. The diabetes population was taken from SCI-DC. Incidence of amputation was expressed as number of amputations in people with diabetes per 1,000 individuals with diabetes and per 100,000 general population.
Chi-square test methods were used to assess changes in amputations over time. The significances of linear trends were investigated using Kendall τb. This cohort study has been reported using Strengthening the Reporting of Observational Studies in Epidemiology guidance (6).
RESULTS
The Scottish diabetes population increased by 12.8% from 183,311 in 2004 to 206,818 in 2008. This represents an increase in crude prevalence of diabetes from 3.6 to 4.0%. The mean age of people with diabetes increased from 59.4 to 62.7 years from 2004 to 2008. Diabetes duration increased from 7.6 to 8.7 years over 5 years. Other parameters including HbA1c, BMI, and estimated glomerular filtration rate remained stable.
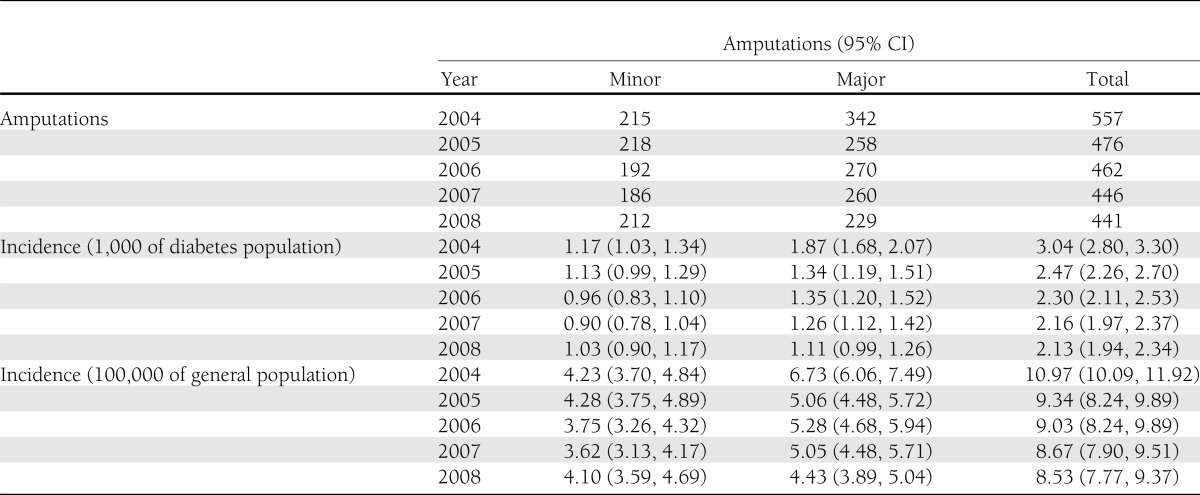
Two thousand three hundred eighty-two people with diabetes underwent nontraumatic LEAs between 2004 and 2008. The number of people undergoing major and minor amputations over 5 years were 1,359 and 1,023, respectively (Table 1). This corresponded to a total, major, and minor amputation rate of 2.42, 1.39, and 1.04 per 1,000 individuals with diabetes per year, respectively.
Table 1.
Minor, major, and total amputations and incidence in the diabetes and general population in Scotland from 2004 to 2008
The incidence of major and total amputations (per 1,000 of the diabetes population) fell steadily over 5 years (P < 0.001). There was a 29.8% reduction in individuals with diabetes undergoing any LEA from 3.04 to 2.13 per 1,000. The most pronounced fall was in major LEAs, with a reduction of 40.7% from 1.87 per 1,000 in 2004 to 1.11 per 1,000 in 2008. There was a 1.7-fold variation in diabetes-related amputation rates between different health boards (range 1.1–1.9%, P < 0.001).
The incidence of diabetes-related amputations per 100,000 of the general population fell by 22.2% from 10.97 to 8.53. The decreasing trend was statistically significant for major and total (P < 0.001 in both cases) but not minor amputations. The largest fall was in those undergoing major LEAs, in which there was a reduction of 34.2% from 6.73 to 4.43 per 100,000 from 2004 to 2008.
CONCLUSIONS
The incidence of LEA in persons with diabetes in Scotland has decreased by 30% over 5 years. The greatest reduction was in major amputation, which fell by 41%.
A potential confounding factor contributing to the decreased incidence of amputations in our study could be improved registration of diabetes rather than a true increase in the prevalence of new cases. Establishing accurate amputation incidence is difficult because of variability in the denominator and misclassification of cases (7). Although it is important to consider case ascertainment, it is unlikely to be a major factor in our study because the Scottish information system for diabetes diagnosis has been established for a number of years, and the annual increase in prevalence of 0.2% indicates an established stable population.
Because amputation rates are susceptible to many confounding variables, it has been suggested that to demonstrate a genuine improvement both incidence and absolute number of amputations should fall (4). We have shown both to be the case and feel that the decrease in amputation rate is therefore genuine. Several regional studies have demonstrated significant reductions in diabetes-related amputations (8–10); however, this is not reflected at a national level (11,12). Further studies have shown significant geographic variation within countries (13) and highlight the benefit of national data in determining accurate amputation rates.
Countries that have shown a reduction in diabetes-related amputations include the Netherlands (2), Finland (14), and the U.S. (15), with a decrease in total amputations of 37, 49, and 65%, respectively. These studies were hampered with methodological problems, including estimates from a projected diabetes population, failure to provide the incidence for amputation subtypes, and reporting relative risk compared with nondiabetic subjects. This raises the possibility that a significant proportion of any decrease was a result of diabetes case ascertainment or an increased rate of amputation in people without diabetes. These studies highlight the problems of comparing amputation rates when the number of subjects in the denominator changes significantly or there is failure to report transparent data on amputation types. There is an urgent need to devise a consistent approach to reporting amputation incidence. Similar to others (4), we would advocate that total, major, and minor amputation incidences are reported per 1,000 subjects with diabetes and per 100,000 of the general population. This would allow comparisons between countries, and inclusion of general population rates helps negate any numerator/denominator bias relating to identification of diabetes cases.
We believe that Scotland is the fourth nation to show a significant reduction in the incidence of diabetes-related LEAs. However, Scotland is the first to provide information on amputation subtypes and rates from an actual rather than estimated diabetes population.
Acknowledgments
These data were available for analysis by members of the Scottish Diabetes Research Network (SDRN) thanks to the hard work and dedication of NHS staff across Scotland who enter the data and people and organizations (SCI-DC Steering Group, the Scottish Diabetes Group, the Scottish Diabetes Survey Group, the managed clinical network managers and staff in each health board) involved in setting up, maintaining, and overseeing SCI-DC. The SDRN receives core support from the Chief Scientist’s Office at the Scottish Government Health Department. The costs of data linkage were covered by the Scottish Government Health Department. This work was funded by the Wellcome Trust through the Scottish Health Informatics Programme (SHIP) Grant (Ref WT086113). SHIP is a collaboration between the universities of Aberdeen, Dundee, Edinburgh, Glasgow, and St. Andrews, and the Information Services Division of NHS Scotland. Statistical analysis was funded from the Tayside Health Board Research Endowments.
All authors have completed the Unified Competing Interest form at www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) and declare no support from any organization for the submitted work; no financial relationships with any organizations that might have an interest in the submitted work in the previous 3 years; and no other relationships or activities that could appear to have influenced the submitted work.
No potential conflicts of interest relevant to this article were reported.
B.K., G.P.L., and L.C. were involved in the conception, design, analysis, and interpretation of the data as well as the initial draft and final approval of the manuscript. H.C., S.W., D.S., N.S., D.P., R.S.L., and A.D.M. contributed to the interpretation of the data, revision, and final approval of the manuscript. S.L. contributed to the data analysis and interpretation of the data. M.Y., J.M., and S.C. contributed to the interpretation of the data, revision, and final approval of the manuscript. B.K. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
See accompanying commentary, p. 2419.
References
- 1.Boulton AJ, Vileikyte L, Ragnarson-Tennvall G, Apelqvist J. The global burden of diabetic foot disease. Lancet 2005;366:1719–1724 [DOI] [PubMed] [Google Scholar]
- 2.van Houtum WH, Rauwerda JA, Ruwaard D, Schaper NC, Bakker K. Reduction in diabetes-related lower-extremity amputations in The Netherlands: 1991-2000. Diabetes Care 2004;27:1042–1046 [DOI] [PubMed] [Google Scholar]
- 3.Moxey PW, Gogalniceanu P, Hinchliffe RJ, et al. Lower extremity amputations—a review of global variability in incidence. Diabet Med 2011;28:1144–1153 [DOI] [PubMed] [Google Scholar]
- 4.Jeffcoate WJ, van Houtum WH. Amputation as a marker of the quality of foot care in diabetes. Diabetologia 2004;47:2051–2058 [DOI] [PubMed] [Google Scholar]
- 5.Cunningham S, McAlpine R, Leese G, et al. Using web technology to support population-based diabetes care. J Diabetes Sci Tech 2011;5:523–534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, STROBE Initiative The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol 2008;61:344–349 [DOI] [PubMed] [Google Scholar]
- 7.Rayman G, Krishnan ST, Baker NR, Wareham AM, Rayman A. Are we underestimating diabetes-related lower-extremity amputation rates? Results and benefits of the first prospective study. Diabetes Care 2004;27:1892–1896 [DOI] [PubMed] [Google Scholar]
- 8.Krishnan S, Nash F, Baker N, Fowler D, Rayman G. Reduction in diabetic amputations over 11 years in a defined U.K. population: benefits of multidisciplinary team work and continuous prospective audit. Diabetes Care 2008;31:99–101 [DOI] [PubMed] [Google Scholar]
- 9.Schofield CJ, Yu N, Jain AS, Leese GP. Decreasing amputation rates in patients with diabetes-a population-based study. Diabet Med 2009;26:773–777 [DOI] [PubMed] [Google Scholar]
- 10.Larsson J, Eneroth M, Apelqvist J, Stenström A. Sustained reduction in major amputations in diabetic patients: 628 amputations in 461 patients in a defined population over a 20-year period. Acta Orthop 2008;79:665–673 [DOI] [PubMed] [Google Scholar]
- 11.Vamos EP, Bottle A, Edmonds ME, Valabhji J, Majeed A, Millett C. Changes in the incidence of lower extremity amputations in individuals with and without diabetes in England between 2004 and 2008. Diabetes Care 2010;33:2592–2597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ringborg A, Lindgren P, Martinell M, Yin DD, Schön S, Stålhammar J. Prevalence and incidence of Type 2 diabetes and its complications 1996-2003—estimates from a Swedish population-based study. Diabet Med 2008;25:1178–1186 [DOI] [PubMed] [Google Scholar]
- 13.Margolis DJ, Hoffstad O, Nafash J, et al. Location, location, location: geographic clustering of lower-extremity amputation among Medicare beneficiaries with diabetes. Diabetes Care 2011;34:2363–2367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ikonen TS, Sund R, Venermo M, Winell K. Fewer major amputations among individuals with diabetes in Finland in 1997-2007: a population-based study. Diabetes Care 2010;33:2598–2603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Li Y, Burrows NR, Gregg EW, Albright A, Geiss LS. Declining rates of hospitalization for nontraumatic lower-extremity amputation in the diabetic population aged 40 years or older: U.S., 1988-2008. Diabetes Care 2012;35:273–277 [DOI] [PMC free article] [PubMed] [Google Scholar]