mTOR Inhibitors Control the Growth of EGFR Mutant Lung Cancer Even after Acquiring Resistance by HGF (original) (raw)
Abstract
Resistance to epidermal growth factor receptor tyrosine kinase inhibitors (EGFR-TKIs), gefitinib and erlotinib, is a critical problem in the treatment of EGFR mutant lung cancer. Several mechanisms, including bypass signaling by hepatocyte growth factor (HGF)-triggered Met activation, are implicated as mediators of resistance. The mammalian target of rapamycin (mTOR), is a downstream conduit of EGFR and MET signaling, and is thus considered a therapeutically attractive target in the treatment of various types of cancers. The purpose of this study was to examine whether 2 clinically approved mTOR inhibitors, temsirolimus and everolimus, overcome HGF-dependent resistance to EGFR-TKIs in EGFR mutant lung cancer cells. Both temsirolimus and everolimus inhibited the phosphorylation of p70S6K and 4E-BP1, which are downstream targets of the mTOR pathway, and reduced the viability of EGFR mutant lung cancer cells, PC-9, and HCC827, even in the presence of HGF in vitro. In a xenograft model, temsirolimus suppressed the growth of PC-9 cells overexpressing the _HGF_-gene; this was associated with suppression of the mTOR signaling pathway and tumor angiogenesis. In contrast, erlotinib did not suppress this signaling pathway or tumor growth. Multiple mechanisms, including the inhibition of vascular endothelial growth factor production by tumor cells and suppression of endothelial cell viability, contribute to the anti-angiogenic effect of temsirolimus. These findings indicate that mTOR inhibitors may be useful for controlling HGF-triggered EGFR-TKI resistance in EGFR mutant lung cancer, and they provide the rationale for clinical trials of mTOR inhibitors in patients stratified by EGFR mutation and HGF expression status.
Introduction
Lung cancer is the leading cause of malignancy-related death worldwide, and more than 80% of cases are classified as non-small cell lung cancer (NSCLC). Epidermal growth factor receptor (EGFR) activating mutations, such as exon 19 deletion and exon 21 L858R point mutation, are found in a population of NSCLC, and are associated with a clinical response to the EGFR tyrosine kinase inhibitors (EGF-TKIs), gefitinib and erlotinib [1]–[3]. However, almost all responders acquire resistance and develop recurrence after varying periods of time (acquired resistance) [4]. In addition, 20–30% of the patients show unfavorable responses, although their tumors have target mutations (intrinsic resistance) [5]. Many studies have been performed in order to delineate strategies that may overcome acquired and intrinsic resistance. These studies have identified several mechanisms of acquired resistance, including EGFR T790M mutation [6], [7], MET amplification [8], [9], hepatocyte growth factor (HGF) overexpression [10], loss of PTEN [11], transformation to a small cell lung cancer (SCLC) phenotype [12]–[14], epithelial-to-mesenchymal transition (EMT) [15]–[17], activation of the NFkB pathway [18], alteration of microRNA [19], and Gas6-Axl axis activation [20]. The complexity of NSCLC is reflected by the co-occurrence of various combinations of these resistance mechanisms in different individuals. We previously discovered that HGF triggers EGFR-TKI resistance by activating the MET/PI3K/AKT axis [10]. Furthermore, we showed that HGF overexpression is present in tumors from Japanese patients with acquired and intrinsic tumor resistance to EGFR-TKI at frequencies of about 60% and 30%, respectively [21]. This indicates that HGF is an ideal target for overcoming EGFR-TKI resistance in EGFR mutant lung cancer patients. To overcome HGF-triggered resistance, 2 signals from EGFR and HGF-MET should be blocked simultaneously. We already reported that HGF-dependent resistance can be controlled by an anti-HGF neutralizing antibody [22], the HGF antagonist NK4 [22], MET-TKI [23]–[25], and phosphatidylinositol 3-kinase (PI3K) inhibitors [26] in combination with EGFR-TKI. However, these inhibitors are not clinically approved and therefore cannot be used for treatment of cancer patients.
The mammalian target of rapamycin (mTOR), a serine/threonine kinase, is a downstream target of the PI3K and AKT pathways, and it plays a critical role in cell survival and proliferation [27]–[29]. Activation of PI3K/AKT and subsequent phosphorylation of mTOR initiates the phosphorylation of important downstream targets, including ribosomal p70S6 serine/threonine kinase (S6K1) and eukaryotic initiation factor (EIF)-4E binding protein (4E-BP1), resulting in an increase in mRNA translation and cap-dependent protein synthesis, respectively. Thus, mTOR kinase is a key node of the PI3K/AKT signaling pathway [27]–[30]. To date, several mTOR inhibitor rapamycin analogs have been developed, including temsirolimus and everolimus, which have been used to treat renal cell carcinomas and pancreatic neuroendocrine tumors. Rapamycin and its analogs bind FK506-binding protein-12 (FKBP12) and interact with mTOR, inhibiting its kinase activities and halting the translation of proteins critical for cell proliferation and survival.
Because mTOR is downstream of both EGFR and MET, we hypothesized that mTOR inhibition, even as a monotherapy agent, may block EGFR- and MET-mediated signaling simultaneously and overcome HGF-triggered EGFR-TKI resistance. In the present study, we examined whether the clinically approved mTOR inhibitors, temsirolimus and everolimus, circumvent HGF-triggered EGFR-TKI resistance in EGFR mutant lung cancer cells using in vitro and in vivo models, and assessed underlying mechanisms.
Materials and Methods
Cell cultures and reagents
EGFR mutant human lung adenocarcinoma cell lines PC-9 (del E746_A750) and HCC827, with deletions in EGFR exon 19, were purchased from Immuno-Biological Laboratories Co. (Takasaki, Gunma, Japan) and the American Type Culture Collection (Manassas, VA), respectively. Human _HGF_-gene transfectants (PC-9/HGF) and vector control (PC-9/Vec) cells were established as previously described [10]. All cell lines were maintained in RPMI 1640 medium supplemented with 10% FBS and antibiotics. All cells were passaged for less than 3 months before renewal from frozen, early-passage stocks. Cells were regularly screened for mycoplasma by using MycoAlert Mycoplasma Detection Kits (Lonza, Rockland, ME). The cell lines were authenticated at the laboratory of the National Institute of Biomedical Innovation (Osaka, Japan) by short tandem repeat analysis. Erlotinib, everolimus, and temsirolimus were obtained from Selleck Chemicals (Houston, TX). Human recombinant HGF was prepared as previously described [10].
Production of HGF and VEGF in cell culture supernatants
Cells (2×105) were cultured in 2 mL medium with 10% FBS for 24 h, washed with PBS and incubated for 48 h in medium with 10% FBS. In some experiments, HGF was added to the medium. The culture media were harvested and centrifuged, and the supernatants were stored at −70°C until analysis. The concentrations of HGF and VEGF were determined by IMMUNIS HGF EIA (Institute of Immunology, Tokyo, Japan) and Quantikine VEGF ELISA (R&D Systems, Minneapolis, MN), respectively, according to the manufacturers' protocols. All samples were run in duplicate. Color intensity was measured at 450 nm using a spectrophotometric plate reader. Growth factor concentrations were determined by comparison with standard curves. The detection limits for HGF and VEGF were 100 pg/mL and 31 pg/mL, respectively.
Cell viability assay
Cell viability was measured by the MTT dye reduction method. Tumor cells, plated at 2×103/100 µL RPMI 1640 medium plus 10% FBS/well in 96-well plates, were incubated for 24 h. Then, erlotinib, temsirolimus, everolimus, and/or HGF were added to each well, and incubation was continued for an additional 72 h. Cell viability was measured with MTT solution (2 mg/mL; Sigma, St. Louis, MO), as previously described [10]. Each experiment was performed with triplicate samples.
Antibodies and western blotting
Protein aliquots (25 µg each) were resolved by SDS polyacrylamide gel electrophoresis (Bio-Rad, Hercules, CA) and transferred to polyvinylidene difluoride membranes (Bio-Rad). After washing 4 times, the membranes were incubated with Blocking One (Nacalai Tesque, Inc., Kyoto, Japan) for 1 h at room temperature (RT) and overnight at 4°C with primary antibodies to β-actin (13E5), Met (25H2), phospho-MET (anti-p-MET, Y1234/Y1235; 3D7), p-EGFR (Y1068), AKT or p-AKT (S473), mTOR, p-mTOR (S2448), p70S6K, pp70S6K (T389), 4E-BP1, p4E-BP1(T37/46) (Cell Signaling Technology, Beverly, MA), human EGFR (1 µg/mL), human/mouse/rat ERK1/ERK2 (0.2 µg/mL), and p-ERK1/ERK2 (T202/Y204; 0.1 µg/mL) (R&D Systems). After 3 washes, the membranes were incubated for 1 h at RT with species-specific horseradish peroxidase–conjugated secondary antibodies. Immunoreactive bands were visualized with SuperSignal West Dura Extended Duration Substrate, an enhanced chemiluminescent substrate (Pierce Biotechnology, Rockford, IL).
Xenograft studies in SCID mice
Suspensions of PC-9/Vec and PC-9/HGF cells (5×106) were subcutaneously injected into the back of 5-week-old male mice with severe combined immunodeficiency (SCID) (Clea, Tokyo, Japan). After 7 days, the mice were randomized to no treatment (control group), oral erlotinib (20 mg/kg/day), or intravenous temsirolimus (50 mg/kg/week in water). Tumor size was measured twice a week, and tumor volume was calculated (mm3) as [(width)2 × length]/2. All animal experiments complied with the guidelines for the Institute for Experimental Animals, Advanced Science Research Center, Kanazawa University, Kanazawa, Japan (approval no. AP-081088).
Histological analyses
For the detection of proliferating tumor cells (Ki-67), 5-µm-thick sections were deparaffinized in xylene, rehydrated in decreasing concentrations of ethanol, and antigen-retrieved. For detection of endothelial cells (CD31), 5-µm-thick frozen sections of xenograft tumors were fixed with cold acetone and washed with PBS. Then, endogenous peroxidase activity was blocked by incubation in 3% aqueous H2O2 for 10 min. Following treatment with 5% normal horse serum, the sections were incubated with primary antibodies to Ki-67 (MIB-1) (Dako Cytomation, Glostrup, Denmark), and mouse CD31 (MEC13.3) (BD Pharmingen, Franklin Lakes, NJ). After probing with species-specific biotinylated secondary antibodies, the sections were incubated for 30 min with avidin–biotinylated peroxidase complex (ABC) using a Vectastain ABC kit (Vector Laboratories, Burlingame, CA). The DAB (3,3′-diaminobenzidine tetrahydrochloride) Liquid System (Dako Cytomation) was used to detect immunostaining. Omission of primary antibodies served as a negative control. The 5 areas containing the highest numbers of stained cells within a section were selected for histologic quantitation by light or fluorescent microscopy at 400-fold magnification. All results were independently evaluated by 2 two investigators (D.I. and T.N.).
Statistical analysis
Between group comparisons were assessed by two-tailed Student's _t-_tests. All analyses were performed using GraphPad Software. A P value<0.01 was considered statistically significant.
Results
mTOR inhibitors suppress viability of EGFR mutant lung cancer cells in the presence of HGF
PC-9 and HCC827 are human lung adenocarcinoma cell lines with deletions of exon 19 in EGFR, resulting in constitutive activation of this protein. These cell lines were sensitive to erlotinib, whereas HGF induced erlotinib resistance ( Fig. 1 ). Treatment with either mTOR inhibitor (temsirolimus or everolimus) alone discernibly suppressed the viability of these cell lines. Under these experimental conditions, HGF did not decrease the sensitivity of these cell lines to either drug. These results suggest that mTOR inhibitors may effectively control the growth of EGFR mutant lung cancer cells, irrespective of the presence of HGF which would induce EGFR-TKI resistance.
Figure 1. mTOR inhibitors suppressed viability of EGFR mutant lung cancer cells even in the presence of HGF.
PC-9 or HCC827 cells were incubated with or without erlotinib, temsirolimus, or everolimus, in the presence or absence of HGF (20 ng/ml) for 72 h. Then, cell viability was determined by the MTT assay. Bars show SD. The data shown are representative of 5 independent experiments with similar results.
Our previous study demonstrated that, in patients with NSCLC, HGF is primarily detected in cancer cells with acquired resistance to EGFR-TKIs, suggesting that the production of HGF by these cells occurs mainly via an autocrine mechanism. To further explore the effect of mTOR inhibitors on autocrine HGF production, we generated stable _HGF_-gene transfectants in PC-9 cells (PC-9/HGF). PC-9/HGF cells secreted high concentrations of HGF (28±1 ng/48 h), whereas the concentrations of HGF secreted by PC-9- and control vector-transfected PC-9/Vec cells were below the limit of detection. In addition, PC-9/HGF cells became resistant to erlotinib ( Fig. 2 ). We found that temsirolimus or everolimus discernibly reduced the viability of both PC-9/Vec and PC-9/HGF cells to the same extent, whereas the combination of mTOR inhibitor plus erlotinib had no effect in PC-9/Vec cells in the presence of HGF, indicating that the mTOR inhibitors did not further sensitize these cells to erlotinib in vitro (Fig. S1). Knock down of mTOR by siRNA resulted in inhibition of viability of PC-9/Vec and PC-9/HGF cells by 30% (Fig S2 B), indicating that inhibited cell viability by temsirolimus even in the presence of HGF is due to mTOR inhibition. We also performed flow cytometry using Annexin V and found that temsirolimus did not induce discernible apoptosis in PC-9/Vec or PC-9/HGF cells (Fig. S3). These findings indicate that mTOR inhibitors, when used as single agents, suppress growth of EGFR mutant lung cancer cells via inhibition of proliferation rather than induction of apoptosis.
Figure 2. mTOR inhibitors suppressed viability of endogenously HGF-expressing EGFR mutant lung cancer cells via mTOR signal inhibition.
PC-9/Vec and PC-9/HGF cells were incubated with erlotinib (A), temsirolimus (B), or everolimus (C) for 72 h. Then, cell viability was determined using the MTT assay. Bars show SD. (D) PC-9/Vec and PC-9/HGF cells were treated with or without erlotinib (0.3 µM), temsirolimus (0.3 µM), or everolimus (0.3 µM) for 4 h. The cell lysates were harvested and subjected to western blotting. The data shown are representative of 3 independent experiments with similar results.
mTOR inhibitors suppress p70S6K and 4EBP1 phosphorylation even in the presence of HGF
To explore the molecular mechanism by which mTOR inhibitors suppressed cell viability even in the presence of HGF, we examined the protein expression and phosphorylation status of EGFR, MET, and their downstream molecules (ERK1/2, PI3K/AKT, p70S6K, and 4EBP1) in PC-9/Vec and PC-9/HGF cells by western blotting ( Fig. 2D ). PC-9/Vec cells expressed EGFR and MET proteins, whereas only EGFR was discernibly phosphorylated. Erlotinib remarkably inhibited the phosphorylation of EGFR, as well as downstream ERK1/2 and AKT, but it marginally inhibited p70S6K phosphorylation. While neither temsirolimus nor everolimus affected the phosphorylation of EGFR, MET, ERK1/2 or AKT, they inhibited the phosphorylation of p70S6K and 4EBP1, the downstream molecules of mTOR.
In PC-9/HGF cells, MET was also phosphorylated, presumably due to HGF that was produced in an autocrine manner. Erlotinib inhibited EGFR phosphorylation, but it did not remarkably inhibit the phosphorylation of MET, AKT, p70S6K, or 4EBP1. While neither temsirolimus nor everolimus inhibited the phosphorylation of EGFR, MET, ERK1/2, or AKT, they markedly inhibited the phosphorylation of p70S6K and 4EBP1. These results indicate that mTOR inhibitors suppress the phosphorylation of downstream molecules of mTOR, irrespective of the presence of HGF.
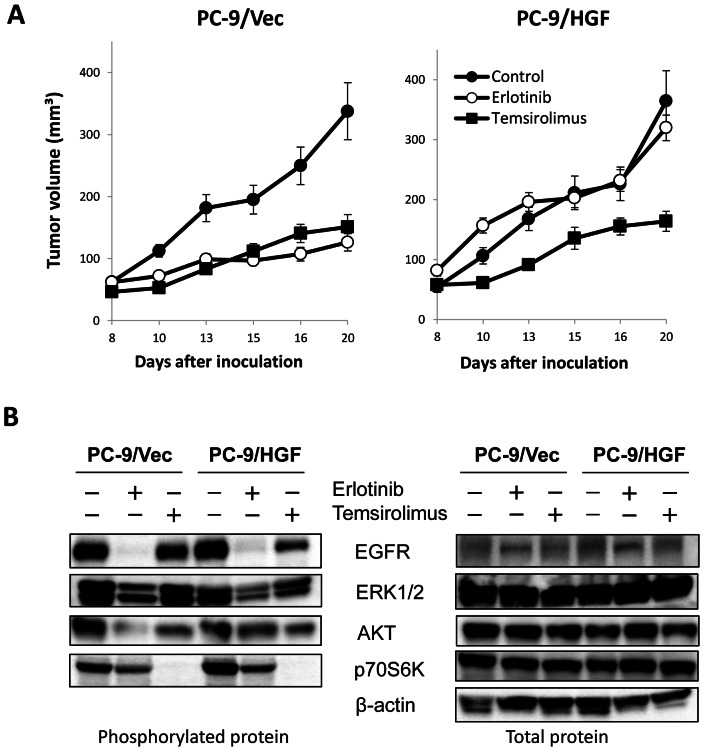
mTOR inhibition suppresses HGF-induced growth of erlotinib-resistant tumors in vivo
We next evaluated whether mTOR inhibitors would control the growth of EGFR mutant lung cancer cells with HGF-triggered EGFR-TKI-resistance in vivo. Oral administration of erlotinib suppressed the growth of PC-9/Vec-tumors, but not PC-9/HGF tumors, indicating resistance of PC-9/HGF tumors to erlotinib in vivo ( Fig. 3A ). On the other hand, intravenous administration of temsirolimus suppressed the growth of both PC-9/Vec tumors and PC-9/HGF tumors. These results indicated that mTOR inhibition may be useful for controlling the growth of HGF-induced resistant tumors in vivo.
Figure 3. Treatment with temsirolimus inhibited the growth of erlotinib-resistant PC-9/HGF tumors in SCID mice.
(A) SCID mice bearing PC-9/Vec or PC-9/HGF tumors were administered 25 mg/kg erlotinib once daily or 50 mg/kg temsirolimus once a week from day 8 to day 20. Tumor volume was measured using calipers on the indicated days. Mean ± SE tumor volumes are shown for groups of 5 mice. *P<0.01 (one-way ANOVA). The data shown are representative of 2 independent experiments with similar results. (B) SCID mice with PC-9/Vec or PC-9/HGF tumors were administered 25 mg/kg erlotinib once daily for 4 days or 50 mg/kg temsirolimus once from day 8. Four hours after final erlotinib administration, tumors were harvested, and the relative levels of proteins in the tumor lysates were determined by western blotting.
We further assessed the molecular mechanisms by which temsirolimus inhibited the growth of PC-9/HGF-tumors. Western blot analyses revealed that erlotinib markedly inhibited the phosphorylation of EGFR, ERK1/2, and AKT, and slightly suppressed the phosphorylation of p70S6K in PC-9/Vec-tumors ( Fig. 3B ). While erlotinib remarkably inhibited EGFR phosphorylation, it only slightly inhibited ERK1/2 and p70S6K phosphorylation, whereas it did not inhibit AKT phosphorylation in PC-9/HGF-tumors. On the other hand, though temsirolimus did not markedly affect the phosphorylation of EGFR or ERK1/2 in both PC-9/Vec tumors and PC-9/HGF tumors, it remarkably inhibited p70S6K phosphorylation, suggesting the mode of action of this drug as a mTOR inhibitor.
Interestingly, temsirolimus slightly inhibited the Akt phosphorylation in PC-9/HGF tumors, but it increased AKT phosphorylation in PC-9/HGF cells in vitro condition ( Fig. 2D ). To clarify the cause of this discrepancy, we examined the time course of mTOR inhibitor treatment on AKT phosphorylation in vivo (Fig S4). We found that in accordance with the results of in vitro experiments, AKT phosphorylation in the tumors was increased 4 h after temsirolimus treatment. But then, the level of AKT phosphorylation was decreased and it was slightly inhibited at 96 h after the treatment, in accordance with the results shown in Fig. 3B. Therefore, the discrepancy of the results between Fig. 2D and Fig. 3B were due to the difference of the timing samples were harvested.
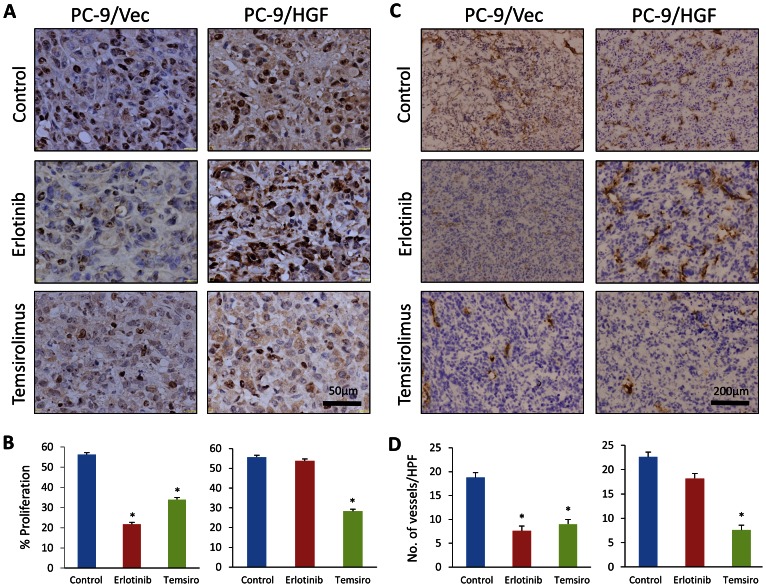
mTOR inhibition suppresses angiogenesis in vivo
We also examined tumor cell proliferation (Ki-67) and angiogenesis (CD31) by immunohistochemistry. Erlotinib treatment markedly inhibited tumor cell proliferation and angiogenesis in PC-9/Vec xenografts, whereas erlotinib did not affect cell proliferation or angiogenesis significantly in PC-9/HGF xenografts ( Fig. 4 ). In contrast, temsirolimus markedly inhibited cell proliferation and angiogenesis in both PC-9/Vec and PC-9/HGF tumors. These findings suggest that temsirolimus inhibits the growth of PC-9/HGF tumors (at least in part) by inhibiting angiogenesis.
Figure 4. Treatment with temsirolimus inhibited tumor-cell proliferation and angiogenesis.
SCID mice with PC-9/Vec or PC-9/HGF tumors were administered as described in Fig. 3B. Four hours after final administration of erlotinib, tumors were harvested, and tumor cell proliferation (A, B: Ki-67) and angiogenesis (C, D: CD31) were determined by immunohistochemistry. B and D show quantification of positive cells. *P<0.01, (one-way ANOVA). Bars show SD.
To further explore the molecular mechanisms by which temsirolimus inhibited angiogenesis, we examined its effect on tumor cell production of VEGF, a prominent pro-angiogenic molecule. Both PC-9 and PC-9/Vec cells constitutively produced detectable levels of VEGF, which was stimulated by HGF ( Fig. 5A ). Consistent with these observations, PC-9/HGF cells produced higher levels of VEGF than PC-9 and PC-9/Vec cells. Temsirolimus suppressed VEGF production in these cancer cells in the presence or absence of HGF. Knock down of mTOR by siRNA resulted in inhibition of VEGF production by PC-9/Vec and PC-9/HGF cells, just like temsirolimus treatment (Fig S2). These results indicate that inhibited VEGF production by temsirolimus even in the presence of HGF is due to mTOR inhibition. We also assessed the direct effect of temsirolimus on the viability of endothelial cells in vitro. Temsirolimus did not inhibit constitutive viability of HMVEC cells in the medium with 10% FBS alone ( Figure 5B ). VEGF and HuMedia-MvG, which contain EGF and fibroblast growth factor-2 (FGF-2), increased the viability of HMVECs. Temsirolimus, at concentrations of 1 nM and higher, inhibited this increase in viability. These results indicate that temsirolimus inhibits angiogenesis by multiple mechanisms.
Figure 5. Temsirolimus inhibited VEGF production by cancer cells and endothelial proliferation.

(A) Tumor cells were incubated with or without HGF (50 ng/ml) in the presence of different concentrations of temsirolimus for 48 h. Then, supernatants were harvested and the number of tumor cells was counted. VEGF concentration in the supernatants was determined by ELISA. VEGF levels corrected by the tumor cell number are shown. (B) HMVECs were incubated in RPMI-1640 medium with 10% FBS (control), RPMI-1640 medium with 10%-FBS plus VEGF, or HuMedia-MvG with different concentrations of temsirolimus for 72 h. Then, cell viability was determined using the MTT assay. Bars show SD. The data shown are 2 independent experiments with similar results.
Discussion
In the present study, we demonstrated that mTOR inhibitors suppressed the growth of EGFR mutant lung cancer cells, even in the presence of HGF, in vitro and in vivo. Our results also indicate that mTOR inhibitors suppress angiogenesis by inhibiting VEGF production and endothelial proliferation stimulated with various pro-angiogenic factors. These observations suggest that mTOR inhibitors, as monotherapeutic agents, are useful for controlling the progression of EGFR mutant lung cancer and HGF-triggered resistance to EGFR-TKIs.
HGF, also called scatter factor, is a multifunctional cytokine [31]. Recent studies showed that HGF is involved in the carcinogenesis, invasion/motility, EMT, angiogenesis, and metastasis in lung cancer, and it is therefore associated with poor prognosis of patients [32]. We previously reported that HGF induces EGFR-TKI-resistance in EGFR mutant lung cancer cells by restoring MET/PI3K/AKT pathway signaling [10]. HGF Overexpression is involved not only in acquired resistance but also intrinsic resistance to EGFR-TKIs [21]. In addition, HGF stimulates VEGF production by EGFR mutant lung cancer cells, as well as facilitates angiogenesis, thereby promoting tumor progression [24]. HGF overexpression is often co-detected with the _EGFR_-T790M gatekeeper mutation in acquired resistant tumors [9], [11], [21]. HGF induces resistance to irreversible EGFR-TKIs and mutant EGFR-selective TKIs [33], which were developed to overcome T790M-mediated EGFR-TKI resistance. Recent clinical trials with irreversible TKI monotherapy failed to demonstrate an objective response in EGFR mutant lung cancer patients that were refractory to treatment with the reversible EGFR-TKIs—gefitinib and erlotinib [34]. These findings suggest that co-existence of altered HGF signaling contributes to the unfavorable response to irreversible EGFR-TKIs in these patients [32]. In addition, the presence of HGF accelerates the growth of pre-existing EGFR-TKI-resistant clones that harbor MET amplification [35]. More recently, HGF was reported to induce resistance to ALK selective inhibitors in EML4-ALK lung cancer [36] and BRAF inhibitors in BRAF mutant melanoma [37]. Such accumulating evidence indicates that HGF is a common target for overcoming resistance to targeted drugs in oncogene-addicted tumors.
Our results also suggest that mTOR inhibitors have advantage of several mechanisms to suppress the growth of EGFR-TKI resistance triggered by HGF in EGFR mutant lung cancer cells. For example, these inhibitors likely block mTOR/p70S6K/4E-BP1 survival signals that are usually engaged during PI3K/AKT activation in cancer cells. The PI3K/AKT/mTOR pathway contributes to the survival of EGFR mutant lung cancer cells [38], [39]. We previously reported that this pathway is also crucial for acquiring HGF-triggered resistance to EGFR-TKIs in EGFR mutant lung cancer cells [40]. In the present study, both temsirolimus and everolimus partially suppressed the phosphorylation of p70S6K and 4E-BP1, as well as inhibited the survival of EGFR mutant cancer cells in vitro. Thus, mTOR inhibitors achieve growth inhibition by suppressing both survival signals from EGFR and resistance signals from MET in cancer cells.
Another possible mechanism is the inhibition of angiogenesis. Recent studies reported that mTOR-mediated signaling stimulates HIF-1α transcription, which regulates VEGF, via 4E-BP1 phosphorylation [41]. mTOR inhibitors suppress HIF-1α transcription and thereby inhibit VEGF production [28], [29], [41]–[43]. We previously reported that HGF activates the MET/GAB1 pathway and increases VEGF production by EGFR mutant lung cancer cells [24]. In the present study, we confirmed this finding and further demonstrated that mTOR inhibitors suppressed both constitutive VEGF production and HGF-stimulated VEGF production. Moreover, we found that while mTOR inhibitors did not affect the viability of unstimulated endothelial cells, they inhibited endothelial proliferation stimulated by various pro-angiogenic factors, including VEGF. mTOR is activated following engagement of several receptor tyrosine kinases such as VEGFR-2, EGFR, and FGFR-1 [41]; hence, mTOR inhibitors may abrogate the stimulation caused by multiple pro-angiogenic factors in endothelial cells. Therefore, mTOR inhibitors may suppress angiogenesis by at least 2 modes of actions. First, they may inhibit VEGF production even in the presence of HGF. Second, they may inhibit endothelial cell proliferation that is stimulated by various pro-angiogenic factors.
Results of recent clinical trials with targeted drugs indicate the importance of patient selection. For example, the response rate of gefitinib was only 10–20% in unselected NSCLC [44], but it was about 80% in EGFR mutation-positive NSCLC [43]. The progression-free survival of EGFR mutant lung cancer patients was also much longer than that of unselected NSCLC patients [45]. While a large number of mTOR inhibitors have been developed and are being evaluated in clinical trials in lung cancer, neither of sirolimus, temsirolimus, or everolimus, when used as monotherapeutic agents, show clinical efficacy in unselected NSCLC [46] [47]. Moreover, recent studies of mTOR inhibitors combined with EGFR-TKI also failed to show clinical benefit in unselected NSCLC [46] [48]–[50]. Our current study is preclinical, and we demonstrated that mTOR inhibitors showed considerable efficacy in lung cancer cells with HGF-mediated resistance to EGFR-TKI resistance both in vitro and in vivo. Dong et al. also reported the anti-tumor activity of mTOR inhibitors against EGFR-TKI-resistant EGFR mutant lung cancer cells with the T790M gatekeeper mutation [51]. Both HGF and T790M gatekeeper mutations are frequently detected in EGFR-TKI resistant tumors, where they contribute to resistance. Therefore, these observations illustrate the necessity of clinical trials with mTOR inhibitors in EGFR mutant lung cancer patients who become refractory to gefitinib and erlotinib. Moreover, since HGF confers resistance to targeted drugs in several tumor types, clinical trials of mTOR inhibitors are warranted.
Supporting Information
Figure S1
mTOR inhibitors did not further sensitize EGFR mutant lung cancer cells to erlotinib in vitro . PC-9/Vec cells were incubated with or without temsirolimus (A) or everolimus (B), in the presence or absence of HGF (20 ng/ml) and erlotinib (0.3 µM) for 72 h. Then, cell viability was determined by the MTT assay. Bars show SD. The data shown are representative of 3 independent experiments with similar results.
(TIF)
Figure S2
Knock-down of mTOR inhibited cell growth and VEGF production. Tumor cells were transfected with mTOR or control siRNA for 24 h and (A) the cell lysates were harvested and subjected to western blotting. (B) cell viability was determined by the MTT assay, (C) VEGF concentration in the supernatants further 48 h after transfection, was determined by ELISA. C shows VEGF levels corrected by the tumor cell number are shown. B and C show quantification of positive cells. *P<0.01, (one-way ANOVA). Bars show SD. The data shown are representative of 5 independent experiments with similar results.
(TIF)
Figure S3
Temsirolimus did not induce apoptosis in PC-9 cells in vitro , irrespective of the presence of HGF. PC-9/Vec and PC-9/HGF cells were treated with cisplatin (as a positive control for apoptosis), erlotinib, or temsirolimus for 48 h. Then, the resultant cells were treated with PE Annexin V Apoptosis Detection Kit I.
(TIF)
Figure S4
Treatment with temsirolimus increased AKT phosphorylation after 4 h treatment, but the phosphorylation was reduced at 96 h. SCID mice with PC-9/HGF tumors were administered 50 mg/kg temsirolimus. After 4 h, 12 h, 48 h and 96 h, the tumors were harvested, and the relative levels of proteins in the tumor lysates were determined by western blotting.
(TIF)
Acknowledgments
We thank Mr Kenji Kita for technical assistance of experiments.
Funding Statement
This study was supported by KAKENHI (Grants-in-Aid for Scientific Research on Innovative Areas ‘Integrative Research on Cancer Microenvironment Network’ (to SY) and Grant-in-Aid for Young Scientists (to TY and ST)), and Grants-in-Aid for Project for Development of Innovative Research on Cancer Therapeutics (P-Direct) from the Ministry of Education, Culture, Sports, Science and Technology (MEXT). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Lynch TJ, Bell DW, Sordella R, Gurubhagavatula S, Okimoto RA, et al. (2004) Activating mutations in the epidermal growth factor receptor underlying responsiveness of non-small-cell lung cancer to gefitinib. N Engl J Med 350: 2129–2139. [DOI] [PubMed] [Google Scholar]
- 2.Paez JG, Jänne PA, Lee JC, Tracy S, Greulich H, et al. (2004) EGFR mutations in lung cancer: correlation with clinical response to gefitinib therapy. Science 304: 1497–1500. [DOI] [PubMed] [Google Scholar]
- 3.Pao W, Miller V, Zakowski M, Doherty J, Politi K, et al. (2004) EGF receptor gene mutations are common in lung cancers from “never smokers” and are associated with sensitivity of tumors to gefitinib and erlotinib. Proc Natl Acad Sci U S A 101: 13306–13311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jackman D, Pao W, Riely GJ, Engelman JA, Kris MG, et al. (2010) Clinical definition of acquired resistance to epidermal growth factor receptor tyrosine kinase inhibitors in non-small-cell lung cancer. J Clin Oncol 28: 357–360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pao W, Chmielecki J (2010) Rational, biologically based treatment of EGFR-mutant non-small-cell lung cancer. Nat Rev Cancer 10: 760–774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kobayashi S, Boggon TJ, Dayaram T, Jänne PA, Kocher O, et al. (2005) EGFR mutation and resistance of non-small-cell lung cancer to gefitinib. N Engl J Med 352: 786–792. [DOI] [PubMed] [Google Scholar]
- 7.Pao W, Miller VA, Politi KA, Riely GJ, Somwar R, et al. (2005) Acquired resistance of lung adenocarcinomas to gefitinib or erlotinib is associated with a second mutation in the EGFR kinase domein. PLoS Med 2: e73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Engelman JA, Zejnullahu K, Mitsudomi T, Song Y, Hyland C, et al. (2007) MET amplification leads to gefitinib resistance in lung cancer by activating ERBB3 signaling. Science 316: 1039–1043. [DOI] [PubMed] [Google Scholar]
- 9.Turke AB, Zejnullahu K, Wu YL, Song Y, Dias-Santagata D, et al. (2010) Preexistence and clonal selection of MET amplification in EGFR mutant NSCLC. Cancer Cell 17: 174–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yano S, Wang W, Li Q, Matsumoto K, Sakurama H, et al. (2008) Hepatocyte growth factor induces gefitinib resistance of lung adenocarcinoma cells with EGF receptor mutation. Cancer Res 68: 9479–9487. [DOI] [PubMed] [Google Scholar]
- 11.Uramoto H, Shimokawa H, Hanagiri T, Kuwano M, Ono M (2011) Expression of selected gene for acquired drug resistance to EGFR-TKI in lung adenocarcinoma. Lung Cancer 73: 361–365. [DOI] [PubMed] [Google Scholar]
- 12.Zakowski MF, Ladanyi M, Kris MG (2006) EGFR mutations in small-cell lung cancers in patients who have never smoked. N Engl J Med 355: 213–215. [DOI] [PubMed] [Google Scholar]
- 13.Morinaga R, Okamoto I, Furuta K, Kawano Y, Sekijima M, et al. (2007) Sequential occurrence of non-small cell and small cell lung cancer with the same EGFR mutation. Lung Cancer 58: 411–413. [DOI] [PubMed] [Google Scholar]
- 14.Shiao TH, Chang YL, Yu CJ, Chang YC, Hsu YC, et al. (2008) Epidermal growth factor receptor mutations in small cell lung cancer. Clin Cancer Res 14: 6092–6096. [DOI] [PubMed] [Google Scholar]
- 15.Frederick BA, Helfrich BA, Coldren CD, Zheng D, Chan D, et al. (2007) Epithelial to mesenchymal transition predicts gefitinib resistance in cell lines of head and neck squamous cell carcinoma and non-small cell lung carcinoma. Mol Cancer Ther 6: 1683–1691. [DOI] [PubMed] [Google Scholar]
- 16.Uramoto H, Iwata T, Onitsuka T, Shimokawa H, Hanagiri T, et al. (2010) Epithelial-mesenchymal transition in EGFR-TKI acquired resistant lung adenocarcinoma. Anticancer Res 30: 2513–2517. [PubMed] [Google Scholar]
- 17.Suda K, Tomizawa K, Fujii M, Murakami H, Osada H, et al. (2011) Maehara Y, Yatabe Y, Sekido Y, Mitsudomi T. Epithelial to mesenchymal transition in an epidermal growth factor receptor-mutant lung cancer cell line with acquired resistance to erlotinib. J Thorac Oncol 6: 1152–1161. [DOI] [PubMed] [Google Scholar]
- 18.Bivona TG, Hieronymus H, Parker J, Chang K, Taron M, et al. (2011) FAS and NF-κB signalling modulate dependence of lung cancers on mutant EGFR. Nature 471: 523–526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Garofalo M, Romano G, Di Leva G, Nuovo G, Jeon YJ, et al. (2011) EGFR and MET receptor tyrosine kinase-altered microRNA expression induces tumorigenesis and gefitinib resistance in lung cancers. Nat Med 18: 74–82. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 20.Zhang Z, Lee JC, Lin L, Olivas V, Au V, et al. (2012) Activation of the AXL kinase causes resistance to EGFR-targeted therapy in lung cancer. Nat Genet 44: 852–860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yano S, Yamada T, Takeuchi S, Tachibana K, Minami Y, et al. (2011) Hepatocyte growth factor expression in EGFR mutant lung cancer with intrinsic and acquired resistance to tyrosine kinase inhibitors in a Japanese cohort. J Thorac Oncol 6: 2011–2017. [DOI] [PubMed] [Google Scholar]
- 22.Wang W, Li Q, Yamada T, Matsumoto K, Matsumoto I, et al. (2009) Crosstalk to stromal fibroblasts induces resistance of lung cancer to epidermal growth factor receptor tyrosine kinase inhibitors. Clin Cancer Res 15: 6630–6638. [DOI] [PubMed] [Google Scholar]
- 23.Wang W, Li Q, Takeuchi S, Yamada T, Koizumi H, et al. (2012) Met kinase inhibitor E7050 reverses three different mechanisms of hepatocyte growth factor-induced tyrosine kinase inhibitor resistance in EGFR mutant lung cancer. Clin Cancer Res 18: 1663–1671. [DOI] [PubMed] [Google Scholar]
- 24.Takeuchi S, Wang W, Li Q, Yamada T, Kita K, et al. (2012) Dual inhibition of Met kinase and angiogenesis to overcome HGF-induced EGFR-TKI resistance in EGFR mutant lung cancer. Am J Pathol 181: 1034–1043. [DOI] [PubMed] [Google Scholar]
- 25.Nakagawa T, Takeuchi S, Yamada T, Nanjo S, Ishikawa D, et al. (2012) Combined therapy with mutant-selective EGFR inhibitor and Met kinase inhibitor for overcoming erlotinib resistance in EGFR-mutant lung cancer. Mol Cancer Ther 11: 2149–2157. [DOI] [PubMed] [Google Scholar]
- 26.Donev IS, Wang W, Yamada T, Li Q, Takeuchi S, et al. (2011) Transient PI3K inhibition induces apoptosis and overcomes HGF-mediated resistance to EGFR-TKIs in EGFR mutant lung cancer. Clin Cancer Res 17: 2260–2269. [DOI] [PubMed] [Google Scholar]
- 27.Helena P, José ML, Paula S (2012) The mTOR signalling pathway in human cancer. Int J Mol Sci 13: 1886–1918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Xiaodong F, William O, David H (2010) Antiangiogenesis therapy: a new strategy for cancer treatment. US Pharm 35 Oncology suppl: 4–9. [Google Scholar]
- 29.Jayashree K, Amit M (2011) PI3K/AKT/mTOR pathway in angiogenesis. Front Mol Neurosci 4: 51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hudson CC, Liu M, Chiang GG, Otterness DM, Loomis DC, et al. (2003) Regulation of hypoxia-inducible factor 1: expression and function by the mammalian target of rapamycin. Mol Cell 11: 1491–1501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Takebayashi T, Iwamoto M, Jikko A, Matsumura T, Enomoto-Iwamoto M, et al. (1995) Hepatocyte growth factor/scatter factor modulates cell motility, proliferation, and proteoglycan synthesis of chondrocytes. J Cell Biol 129: 1411–1419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yano S, Takeuchi S, Nakagawa T, Yamada T (2012) Ligand-triggered resistance to molecular targeted drugs in lung cancer: Roles of hepatocyte growth factor and epidermal growth factor receptor ligands. Cancer Sci 103 1189–1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yamada T, Matsumoto K, Wang W, Li Q, Nishioka Y, et al. (2010) Hepatocyte growth factor reduces susceptibility to an irreversible epidermal growth factor receptor inhibitor in EGFR-T790M mutant lung cancer. Clin Cancer Res 16: 174–183. [DOI] [PubMed] [Google Scholar]
- 34.Yasuda H, Kobayashi S, Costa DB (2012) EGFR exon 20 insertion mutations in non-small-cell lung cancer: preclinical data and clinical implications. Lancet Oncol 2012;13: e23–31. [DOI] [PubMed] [Google Scholar]
- 35.Turke AB, Zejnullahu K, Wu YL, Song Y, Dias-Santagata D, et al. (2010) Preexistence and clonal selection of MET amplification in EGFR mutant NSCLC. Cancer Cell 17: 77–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yamada T, Takeuchi S, Nakade J, Kita K, Nakagawa T, et al. (2012) Paracrine receptor activation by microenvironment triggers bypass survival signals and ALK inhibitor resistance in EML4-ALK lung cancer cells. Clin Cancer Res 18: 3592–3602. [DOI] [PubMed] [Google Scholar]
- 37.Straussman R, Morikawa T, Shee K, Barzily-Rokni M, Qian ZR, et al. (2012) Tumour micro-environment elicits innate resistance to RAF inhibitors through HGF secretion. Nature 487: 500–504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Endoh H, Yatabe Y, Kosaka T, Kuwano H, Mitsudomi T (2006) PTEN and PIK3CA expression is associated with prolonged survival after gefitinib treatment in EGFR-mutated lung cancer patients. J Thorac Oncol 1: 629–634. [PubMed] [Google Scholar]
- 39.Oh MH, Lee HJ, Yoo SB, Xu X, Choi JS, et al. (2012) Clinicopathological correlations of mTOR and pAkt expression in non-small cell lung cancer. Virchows Arch 460: 601–609. [DOI] [PubMed] [Google Scholar]
- 40.Donev IS, Wang W, Yamada T, Li Q, Takeuchi S, et al. (2011) Transient PI3K inhibition induces apoptosis and overcomes HGF-mediated resistance to EGFR-TKIs in EGFR mutant lung cancer. Clin Cancer Res 17: 2260–2269. [DOI] [PubMed] [Google Scholar]
- 41.Yee Koh M, Spivak-Kroizman TR, Powis G (2008) HIF-1 regulation: not so easy come, easy go. Trends Biochem Sci 33: 526–534. [DOI] [PubMed] [Google Scholar]
- 42.Samy LH, Anamika Y, Lenin M, Anthony JV (2011) Regulation of PI 3-K, PTEN, p53, and mTOR in malignant and benign tumors deficient in tuberin. Genes Cancer 2: 1051–1060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Young RM, Wang SJ, Gordan JD, Ji X, Liebhaber SA, et al. (2008) Hypoxia-mediated selective mRNA translation by an internal ribosome entry site-independent mechanism. J Biol Chem 283: 16309–16319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Fukuoka M, Yano S, Giaccone G, Tamura T, Nakagawa K, et al. (2003) Multi-institutional randomized phase II trial of gefitinib for previously treated patients with advanced non-small-cell lung cancer (The IDEAL 1 Trial). J Clin Oncol 21: 2237–2246. [DOI] [PubMed] [Google Scholar]
- 45.Mok TS, Wu YL, Thongprasert S, Yang CH, Chu DT, et al. (2009) Gefitinib or carboplatin-paclitaxel in pulmonary adenocarcinoma. N Engl J Med 361: 947–957. [DOI] [PubMed] [Google Scholar]
- 46.Ekman S, Wynes MW, Hirsch FR (2012) The mTOR pathway in lung cancer and implications for therapy and biomarker analysis. J Thorac Oncol 7: 947–953. [DOI] [PubMed] [Google Scholar]
- 47.Reungwetwattana T, Molina JR, Mandrekar SJ, Allen-ZieglErk, Rowland KM, et al. (2012) Brief report: a phase II “window-of-opportunity” frontline study of the mTOR inhibitor, temsirolimus given as a single agent in patients with advanced NSCLC, an NCCTG study. J Thorac Oncol 7: 919–922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Price KA, Azzoli CG, Krug LM, Pietanza MC, Rizvi NA, et al. (2012) Phase II trial of gefitinib and everolimus in advanced non-small cell lung cancer. J Thorac Oncol 1 1623–1629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Leighl NB, Soria J, Bennouna J, Blais N, Traynor AM, et al. (2012) Phase II study of everolimus plus erlotinib in previously treated patients with advanced non-small cell lung cancer (NSCLC). J Clin Oncol 28 15 suppl: 7524. [DOI] [PubMed] [Google Scholar]
- 50.Papadimitrakopoulou VA, Soria JC, Jappe A, Jehl V, Klimovsky J, et al. (2012) Everolimus and erlotinib as second- or third-line therapy in patients with advanced non-small-cell lung cancer. J Thorac Oncol 7: 1594–1601. [DOI] [PubMed] [Google Scholar]
- 51.Dong S, Zhang XC, Cheng H, Zhu JQ, Chen ZH, et al. (2012) Everolimus synergizes with gefitinib in non-small-cell lung cancer cell lines resistant to epidermal growth factor receptor tyrosine kinase inhibitors. Cancer Chemother Pharmacol 70: 707–716. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1
mTOR inhibitors did not further sensitize EGFR mutant lung cancer cells to erlotinib in vitro . PC-9/Vec cells were incubated with or without temsirolimus (A) or everolimus (B), in the presence or absence of HGF (20 ng/ml) and erlotinib (0.3 µM) for 72 h. Then, cell viability was determined by the MTT assay. Bars show SD. The data shown are representative of 3 independent experiments with similar results.
(TIF)
Figure S2
Knock-down of mTOR inhibited cell growth and VEGF production. Tumor cells were transfected with mTOR or control siRNA for 24 h and (A) the cell lysates were harvested and subjected to western blotting. (B) cell viability was determined by the MTT assay, (C) VEGF concentration in the supernatants further 48 h after transfection, was determined by ELISA. C shows VEGF levels corrected by the tumor cell number are shown. B and C show quantification of positive cells. *P<0.01, (one-way ANOVA). Bars show SD. The data shown are representative of 5 independent experiments with similar results.
(TIF)
Figure S3
Temsirolimus did not induce apoptosis in PC-9 cells in vitro , irrespective of the presence of HGF. PC-9/Vec and PC-9/HGF cells were treated with cisplatin (as a positive control for apoptosis), erlotinib, or temsirolimus for 48 h. Then, the resultant cells were treated with PE Annexin V Apoptosis Detection Kit I.
(TIF)
Figure S4
Treatment with temsirolimus increased AKT phosphorylation after 4 h treatment, but the phosphorylation was reduced at 96 h. SCID mice with PC-9/HGF tumors were administered 50 mg/kg temsirolimus. After 4 h, 12 h, 48 h and 96 h, the tumors were harvested, and the relative levels of proteins in the tumor lysates were determined by western blotting.
(TIF)