Platinum-Based Chemotherapy for Variant Castrate-Resistant Prostate Cancer (original) (raw)
. Author manuscript; available in PMC: 2014 Jul 1.
Abstract
Purpose
Clinical features characteristic of small-cell prostate carcinoma (SCPC), (““anaplastic””) often emerge during the progression of prostate cancer. We sought to determine the efficacy of platinum-based chemotherapy in patients meeting at least one of seven prospectively defined “anaplastic” clinical criteria, including exclusive visceral or predominantly lytic bone metastases, bulky tumor masses, low PSA levels relative to tumor burden or short response to androgen deprivation therapy.
Experimental Design
A 120-patient phase II trial of frontline carboplatin and docetaxel (CD) and second-line etoposide and cisplatin (EP) was designed to provide reliable clinical response estimates under a Bayesian probability model with early stopping rules in place for futility and toxicity.
Results
Seventy-four of 113 (65.4%) and 24 of 71 (33.8%) were progression free after 4 cycles of CD and EP, respectively. Median overall survival (OS) was 16 months (95% CI, 13.6-19.0 months). Of the 7 “anaplastic” criteria, bulky tumor mass was significantly associated with poor outcome. Lactic acid dehydrogenase (LDH) strongly predicted for OS and rapid progression. Serum carcinoembryonic antigen (CEA) concentration strongly predicted OS but not rapid progression. Neuroendocrine markers did not predict outcome or response to therapy.
Conclusion
Our findings support the hypothesis that patients with “anaplastic” prostate cancer are a recognizable subset characterized by a high response rate of short duration to platinum-containing chemotherapies, similar to SCPC. Our results suggest that CEA is useful for selecting therapy in men with CRPC and consolidative therapies to bulky high-grade tumor masses should be considered in this patient population.
Keywords: Small-cell, neuroendocrine, castration-resistant, prostate carcinoma, platinum chemotherapy
Introduction
Volume and extent of cancer dissemination remain the foundation for the classification and prognostication of patients with prostate cancer. However, this anatomy-based classification does not account for the clinical and biologic heterogeneity within the disease and limits our ability to predict individualized outcomes and to conduct efficient studies of promising agents and rational combinations. As part of a broader effort to characterize patients with advanced prostate cancer, we focused on a clinically distinct subset with recognizable features; in particular, we speculated that prostate cancers that display clinical features associated with small-cell carcinoma morphology—a syndrome initially dubbed “anaplastic”—have common underlying biology that may be implicated in the lethality of a significant portion of patients with prostate cancer.
Small-cell prostate cancer (SCPC) is rarely detected at initial diagnosis but is more frequent upon recurrence(1-7). Autopsy series demonstrate its presence in 10-20% of men dying of CRPC (8-10).The diagnosis of small-cell carcinoma morphology is associated with clinical features not considered typical of prostate cancer, e.g., visceral involvement, lytic bone metastases, and low or undetectable prostate-specific antigen (PSA) levels(1-7). It is also associated with a characteristic response profile: it is unresponsive to androgen ablation but experiences frequent (although short-lived) chemotherapy responses(3-7).
Based on our prior experience and that reported by others (1-6) we empirically, but prospectively, defined 7 clinical features that were considered characteristic of SCPC to select patients for this study (C1-C7; Table 1). Men who met one or more of these criteria were treated with carboplatin and docetaxel (CD), and with etoposide and cisplatin (EP) upon progression, in a single-arm sequential phase 2 clinical trial. Our previous studies in patients with documented SCPC histology had shown that, similarly to small-cell lung cancer, SCPC has a high response to EP-based chemotherapy(5, 6) but we had observed that, at the time of disease progression, many patients had prostate adenocarcinoma as the only detected histological type. This spoke to the need to address both histologic components that frequently coexist in this disease. Docetaxel is the standard first-line chemotherapy for CRPC(11, 12) and has shown modest activity in small-cell lung cancer(13, 14). However, it was felt that the combination of EP with docetaxel would result in excessive toxicity. Carboplatin is considered an acceptable alternative to cisplatin for the treatment of small-cell lung cancer(15), has modest single agent activity in CRPC(16) and has been combined with taxanes successfully for its treatment (17). Therefore, we chose to evaluate the efficacy of the combination of CD in patients with “anaplastic” prostate cancer but included EP as salvage therapy in the event that patients failed to respond to CD. This design also allowed careful monitoring of cumulative neurotoxicity, which was a concern when using these two regimens sequentially.
Table 1. Clinical features of “anaplastic” prostate carcinomas (eligibility criteria)
| Castrate-resistanta prostate carcinoma with at least 1 ofthe following: | n (%) |
|---|---|
| C1. Histologic evidence of small-cell prostate carcinoma(pure or mixed). | 29(25.4) |
| C2. Exclusively visceral metastases. | 19(16.7) |
| C3. Radiographically predominant lytic bone metastases byplain x-ray or CT scan. | 16(14.0) |
| C4. Bulky (≥ 5 cm) lymphadenopathy OR bulky (≥5 cm)high-grade (Gleason ≥ 8) tumor mass in prostate/pelvis. | 49(43.0) |
| C5. Low PSA (≤ 10 ng/mL) at initial presentation (prior toADT or at symptomatic progression in the castrate setting)PLUS high volume (≥ 20) bone metastases. | 26(22.8) |
| C6. Presence of neuroendocrine markers on HISTOLOGY(positive staining of chromogranin A or synaptophysin) ORin SERUM (abnormal high serum levels for chromogranin Aor GRP) at initial diagnosis or at progression.PLUS any of the following in the absence of other causes: Elevated serum LDH (≥ 2 × IULN), Malignant hypercalcemia, Elevated serum CEA (≥ 2 × IULN). | 21(18.4) |
| C7. Short interval (≤ 6 months) to androgen-independentprogression following the initiation of hormonal therapy withor without the presence of neuroendocrine markers. | 52(45.6) |
The primary objectives were to estimate the response rate and time to progression for patients with anaplastic prostate carcinoma treated with front-line CD and their response rate and time to progression to second-line EP following treatment with CD. Secondary objectives included the collection of tissues for investigating the underlying biology of this subset, because our broader goal is to contribute to the development of a biologically based, clinically meaningful prognostic and predictive classification of prostate cancer. We also sought to evaluate the toxicity of the regimens and to estimate the overall survival of patients with “anaplastic” prostate carcinoma treated with CD and salvage EP.
The results support our hypothesis that clinical features characteristic of SCPC identify a morphologically heterogeneous but clinically distinct and chemotherapy-responsive variant of prostate cancer.
Patients and Methods
Inclusion and exclusion criteria
Eligibility criteria included the presence of metastatic castrate-resistant prostate cancer with 1 or more of 7 criteria (Table 1). Patients with histologically confirmed SCPC were not required to have received prior androgen-deprivation therapy (ADT), but all others had to have evidence of disease progression during ADT or an unsatisfactory response to ≥ 1 month of castration (i.e., lack of pain control and/or < 20% PSA decrease, confirmed by repeat testing on a different day) and a serum testosterone level of ≤ 1.74 nmol/L. Patients also had to have 0-2 ECOG performance status and adequate organ function, including creatinine clearance ≥ 0.67 mL/s/m2. Men with asymptomatic brain metastases not requiring corticosteroid treatment to control central nervous system symptoms could participate.
Exclusion criteria included grade 2 or greater peripheral neuropathy and treatment with: 2 or more prior chemotherapy regimens; prior platinum-, etoposide-, or taxane-based therapy within 6 months of registration; 2 or more doses of bone-seeking radioisotopes.
The study protocol was approved by the institutional review boards (IRB) of both participating institutions and conducted in accordance with the precepts established by the Helsinki Declaration. Before enrollment, all patients signed IRB-approved written informed consent forms. Clinicaltrials.gov identifier was NCT00514540.
Clinical evaluations
Complete blood counts and serum creatinine, transaminase, and bilirubin concentrations were required within 14 days of enrollment. Complete history and physical examination, serum chemistries, circulating markers (Table 2), electrocardiography, bone scan, and body computed tomography (CT) or MRI scanning were required within 28 days. Contrast-enhanced MRI or CT brain scanning was required within 42 days. Optional procedures included tumor biopsy, bone marrow biopsy, and peripheral blood and urine collection for correlative studies.
Table 2.
Summary of patients’characteristics (n=114) and baseline serum marker values
| n (%)a | ||||
|---|---|---|---|---|
| Age, yearsMedian (range) | At diagnosis | 61 (36–79) | ||
| At registration | 64 (39–80) | |||
| Race | White | 103 (90.4) | ||
| Not white | 11 (9.6) | |||
| Histology at diagnosis | Adenocarcinoma | |||
| GS 5/6 | 5 (4.4) | |||
| GS 7 | 15 (13.2) | |||
| GS 8 | 13 (11.4) | |||
| GS 9 | 53 (46.5) | |||
| GS 10 | 7 (6.0) | |||
| Small-cell carcinoma | 8 (7.0) | |||
| Not available | 13 (11.4) | |||
| Radiation to primary tumor | Yes | 16 (14) | ||
| No | 98 (86) | |||
| Surgery to primary tumor | Yes | 30 (73.7) | ||
| No | 84 (26.3) | |||
| ECOG PS at registration | 0 | 25 (21.9) | ||
| 1 | 74 (64.9) | |||
| 2 | 15 (13.2) | |||
| IULN | No. (%) with Values> IULN | Median (Range) | ||
| ACTH | pmol/L | 10.1 | 4/111 (3.6) | 4.3 (0.88–47.3) |
| ADH | pmol/L | 12.3 | 7/74 (9.5) | 2.9 (0.9–270.4) |
| AVP | pg/mL | 1.7 | 5/36 (13.9) | 0.9 (<0.5–3.6) |
| Alkaline phos | IU/L | 126 | 44/104 (42.3) | 103.5 (40–1107) |
| Calcitonin | pmol/L | 2.5 | 28/88 (31.8) | 1.5 (0.3–1079.8) |
| Bone-sp Alkaline phos | μg/L | 20 | 48/108 (44.4) | 16.95 (1.8-404) |
| CEA | μg/L | 3–6 | 28/113 (24.8) | 2.5 (0–979.4) |
| Chromogranin A | μg/L | 36.4 | 17/74 (23.0) | 16.6 (4–615.7) |
| Chromogranin A,S | μg/L | 225 | 20/35 (57.1) | 251 (4–9850) |
| GRP | pg/mL | 500 | 0/57 (0) | 58 (39–442) |
| Hemoglobin | g/L | 140 | 78/114 (68.4) | 127 (81–159) |
| LDH | IU/L | 546 | 52/114 (45.6) | 527 (111–1942) |
| PAP | ng/mL | 5 | 55/111 (49.5) | 4.5 (0.5–2464.8) |
| PSA | μg/L | 4 | 72/114 (63.2) | 8.7 (0–924.7) |
| Somatostatin | pmol/L | 13.4 | 22/106 (20.8) | 10.7 (3.1–33.6) |
Patients returned for evaluation before each cycle. Imaging and circulating markers were repeated every 2 cycles and every 6-8 weeks after treatment discontinuation.
Chemotherapy
Frontline chemotherapy was CD (carboplatin, area under the curve 5, plus docetaxel, 75 mg/m2) on day 1 every 3 weeks. Second-line EP (etoposide, 120 mg/m2, plus cisplatin, 25 mg/m2) was administered daily for 3 days every 3 weeks upon tumor progression. Treating oncologists could administer the chemotherapy locally, but patients were required to return to the participating institution for evaluation after every 2 cycles.
In the absence of progressive disease (PD), patients received at least 4 cycles of CD or EP. Colony-stimulating factors were administered at the treating physician’s discretion. Dose delays and reductions were within standards for these regimens.
Off-study criteria
Patients were removed from study for documented progression after EP, start of a new systemic treatment, a > 3-week delay in therapy for any reason, unacceptable toxicity that required more than 2 dosing reductions, or patient or physician decision. Data from all patients, whether or not they met eligibility criteria, were evaluated for toxicity if they received at least 1 dose of treatment.
Statistical methods
Sample size
The trial was designed to accrue up to 120 patients to provide reasonably reliable estimates of all relevant parameters based on a Bayesian probability model. This model and decision rules were used to monitor patient outcomes throughout the trial. Interim early stopping rules were applied continuously such that the trial should be stopped for futility (probability of response unacceptably low compared to a target of 30% for CD and 20% for EP following CD) or safety (risk of serious adverse event unacceptably high).
Response evaluation
After 2 and 4 cycles of chemotherapy, response was characterized by the 4-category ordinal variables taking on the values PD, stable disease (SD), partial response (PR), or complete response (CR). With these values, “response” was used in 2 ways:
- “Tumor response” described the tumor’s reaction to the chemotherapy regimens and was reported separately for a) measurable disease (according to RECIST [Response Evaluation Criteria in Solid Tumors] (18)); b) bone disease (an increase in size or number of blastic bone lesions on bone scan, or of lytic lesions on CT, MRI, or plain x-ray, was considered progression); and c) serum tumor marker evaluation (PSA response was defined per PSA Working Group recommendations [(19)]). Carcinoembryonic antigen (CEA) levels were considered evaluable if at least twice the institutional upper limit of normal (IULN), and PSA Working Group criteria were applied to define CEA response. To be evaluable for “tumor response,” eligible patients had to receive at least 2 cycles of treatment and undergo tumor marker and image evaluation.
- “Clinical response,” the primary outcome of the study, was defined as absence of PD (i.e., SD, PR, or CR). To be evaluable for clinical response, patients had to fulfill the eligibility criteria and receive at least 1 chemotherapy cycle. Patients who did not undergo tumor marker and imaging evaluations after 2-4 cycles were counted as having PD.
Statistical methods
Patients’ characteristics were summarized using the median (range) for numeric variables and frequencies (percentages) for categorical variables. Associations between categorical variables were assessed with Fisher’s exact test and its generalizations. The Kaplan-Meier method was used to estimate unadjusted overall survival (OS) and progression-free survival (PFS). Univariate and multivariate Cox proportional hazards models were fit to assess relationships between patient covariates, including our 7 criteria, and OS and PFS. Log transformation was applied for covariates with skewed distributions. The proportional hazards assumption for each fitted Cox model was checked by using the method of Grambsch and Therneau. (20)
All statistical analyses were performed by using SAS 9.0, R2.9.0, or WinBUGS14 software.
Results
Patients
We enrolled 121 patients between June 2006 and October 2010. Seven were ineligible and excluded from the response analysis. Another was eligible but withdrew his consent before treatment, leaving 113 for response to CD analysis. Table 2 highlights baseline characteristics of the 114 eligible patients. Seventy-two (63%) had distant metastatic disease at diagnosis. The median time from diagnosis to registration was 13.9 months (range, 0.2-247.2 months). The median time from initiation of androgen deprivation therapy to registration (data available for n=106) was 9.8 months (95%CI: 8.1-12.4 months). Ninety patients (79%) were symptomatic at registration. Local symptoms (such as perineal pain or urinary obstructive symptoms) were reported by 39 of 96 patients (41%) for whom the information was available.
Sixty-five of the 114 patients (57%) met more than 1 criterion (Table 1) for “anaplastic” prostate cancer. For C6, tissue specimens obtained within 6 months of enrollment and stained for chromogranin A and synaptophysin were available for 51 of the 114 patients (44.7%) and, of these, 29 (56.9%) were positive for 1 and/or the other neuroendocrine (NE) marker. However, of those 29, only 15 (51.7%) also had CEA and/or lactic acid dehydrogenase (LDH) levels twice the IULN needed to meet C6. An additional 6 patients had serum chromogranin A levels above the IULN plus elevated CEA and/or LDH levels, for a total of 21 (18.4%) patients meeting C6. Of the 63 patients (55.3%) for whom stained tissue was unavailable, 57 (90.5%) had neither elevated CEA nor LDH and thus would not have met C6 even if they had had positively staining tissues. Therefore, C6 was unknown for 6 (5.3%) of the 114 patients. As expected, C1 correlated positively with C6 (P = 0. 0001) and negatively with C7 (P = 0.0004).
Table 2 shows baseline serum-marker values. The serum levels of at least 1 of the 6 NE markers (chromogranin A, calcitonin, somatostatin, adrenocorticotropic hormone, antidiuretic hormone, and gastrin-releasing peptide) were elevated in 69 of the 114 patients (60.5%).
Response, PFS, and OS
Table 3 summarizes treatment responses. The median number of cycles of CD administered was 4 (range, 1-12 cycles). At the time of data collection, the median follow-up was 39.1 months (range, 1.07-62.47 months), and 105 patients (92.9%) had experienced PD after CD, with a median time to PD of 5.1 months (95% confidence interval [CI]: 4.2-6.0 months).
Table 3.
Per-course responses to treatment
| Frontline, n (%) | Second-line, n (%) | |||
|---|---|---|---|---|
| Course 1 | Course 2 | Course 1 | Course 2 | |
| RECIST | ||||
| All evaluable | 84 | 69 | 50 | 33 |
| CR | 1(1) | 1(1) | 0 | 0 |
| PD | 4(5) | 4(6) | 5(10) | 6(18) |
| PR | 19(23) | 23(33) | 13(26) | 10(30) |
| SD | 60(71) | 41(59) | 32(64) | 17(52) |
| Bone | ||||
| All evaluable | 85 | 71 | 49 | 25 |
| CR | 0 | 0 | 0 | 0 |
| PD | 7(8) | 3(4) | 10(20) | 5(20) |
| PR | 0 | 0 | 0 | 0 |
| SD | 78(92) | 68(96) | 39(80) | 20(80) |
| PSA | ||||
| All evaluable | 67 | 54 | 43 | 19 |
| CR | 0 | 2(4) | 2(5) | 1(5) |
| PD | 7(10) | 8(15) | 18(42) | 6(32) |
| PR | 19(28) | 23(43) | 5(12) | 5(26) |
| SD | 41(61) | 21(39) | 18(42) | 7(37) |
| CEA | ||||
| All evaluable | 26 | 20 | 20 | 14 |
| CR | 0 | 0 | 0 | 0 |
| PD | 3(12) | 4(20) | 2(10) | 3(21) |
| PR | 1(4) | 5(25) | 4(20) | 5(36) |
| SD | 22(85) | 11(55) | 14(70) | 6(43) |
| Overall | ||||
| All evaluable | 113 | 93 | 74 | 41 |
| PD | 19(17) | 19(20) | 31(42) | 17(41) |
| No PD | 94(83) | 74(80) | 43(58) | 24(59) |
Seventy-four of those 105 patients (70.5%) received second-line EP on study; the remainder withdrew from the study at their physician’s or their own request. Of the 74 patients who received EP, 8 underwent only 1 cycle owing to rapid PD or treatment complications, including 1 death from neutropenic sepsis; their data were inevaluable for “tumor response” but counted as PD for “clinical response.” The median number of EP cycles administered was 4 (range, 1-6 cycles). During the follow-up period, 72 of the 74 patients (97.3%) had experienced PD in a median time of 3.0 months (95% CI: 1.6-3.5 months) after receiving EP.
Among the 113 patients treated on study, 91 (80.5%) have died. The median OS was 16 months (95% CI: 13.6-19.0 months).
We examined the interaction between the chemotherapy regimens delivered sequentially as per protocol. To determine this we assumed that patients with stable or regressing cancers for two cycles of an individual regimen had derived benefit. Of the 74 patients receiving both lines of therapy, 37 (50.0%) benefited from both (median OS 19.33 months, 95%CI: 10.4-23.2) and 5 (6.8%) did not benefit from either (median OS 6.7 months, 95%CI: 19.2-38.2). Twenty-five (33.8%) had a response to CD but not to EP (median OS 14.4 months, 95%CI: 7.5-20.8) and 7 (9.4%) had a response to EP but not to CD (median OS 8.9 months, 95%CI: 13.6-32.2). The 40 patients that only received CD had median OS of 17.4 months (95%CI: 9.7-15.42).
Nine of the 113 patients (7.96%) were found to have brain metastases within the follow-up period. Three of those 9 had primary SCPC at initial diagnosis, and 3 had “secondary” SCPC at re-biopsy; the remaining 3 had no evidence of SCPC on histologic analysis.
Links of Baseline Characteristics with Progression-free and Overall Survival
Table 4 summarizes the effects of baseline clinical and serologic characteristics, including our defined clinical criteria, C1-C7, on PFS and OS. Interpretation of p values should be tempered by the fact that multiple tests were performed for each outcome. (A conservative Bonferroni correction for multiple testing would require an individual p value to be < 0.0015 for each test to control overall type I error at 0.05).
Table 4.
Summary of fitted univariate Cox proportional hazards models for overall survival (OS) and progression-free survival (PFS)
| OS | PFS | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| n | HR | Low 95% | High 95% | P value | HR | Low 95% | High 95% | P value | |
| Race (w vs. not-w) | 114 | 1.066 | 0.514 | 2.211 | 0.863 | 0.973 | 0.490 | 1.935 | 0.939 |
| Mets.at.Diagnosis | 114 | 1.686 | 1.075 | 2.643 | 0.023 | 1.524 | 1.012 | 2.296 | 0.044 |
| log.T.diag | 114 | 0.842 | 0.734 | 0.965 | 0.014 | 0.832 | 0.729 | 0.950 | 0.007 |
| No. of criteria=C1+….+C7 | 114 | 1.410 | 1.126 | 1.766 | 0.003 | 1.211 | 0.970 | 1.511 | 0.092 |
| C1 | 114 | 1.564 | 0.981 | 2.493 | 0.060 | 1.354 | 0.860 | 2.131 | 0.191 |
| C2 | 114 | 1.088 | 0.641 | 1.846 | 0.755 | 1.096 | 0.651 | 1.846 | 0.730 |
| C3 | 114 | 1·230 | 0.693 | 2.182 | 0.479 | 1.362 | 0.786 | 2.362 | 0.271 |
| C4 | 113 | 1.682 | 1.098 | 2.575 | 0.017 | 1.677 | 1.132 | 2.485 | 0.010 |
| C5 | 114 | 1.013 | 0.616 | 1.666 | 0.960 | 0.710 | 0.438 | 1.148 | 0.163 |
| C6 | 108 | 2.150 | 1.235 | 3.741 | 0.007 | 1.126 | 0.673 | 1.882 | 0.651 |
| LDH > 546 | 114 | 2.834 | 1.837 | 4.375 | <0.0001 | 2.472 | 1.645 | 3.714 | <0.0001 |
| CEA > 6 | 114 | 3.241 | 1.973 | 5.325 | <0.0001 | 1.400 | 0.889 | 2.205 | 0.150 |
| IHC (+ vs. −) | 52 | 1.229 | 0.675 | 2.238 | 0.500 | 0.919 | 0.515 | 1.641 | 0.780 |
| C7 | 114 | 0.796 | 0.525 | 1.206 | 0.281 | 0.859 | 0.581 | 1.270 | 0.446 |
| GS≥8 | 101 | 1.203 | 0.730 | 1.984 | 0.470 | 1.393 | 0.864 | 2.244 | 0.170 |
| PS = 0 | 25 | Ref. | Ref. | ||||||
| PS = 1 | 74 | 2.396 | 1.316 | 4.363 | 0.004 | 1.904 | 1.149 | 3.154 | 0.012 |
| PS= 2 | 15 | 3.985 | 1.818 | 8.733 | 0.001 | 3.003 | 1.513 | 5.961 | 0.002 |
| Age | 114 | 1.003 | 0.977 | 1.029 | 0.822 | 0.994 | 0.973 | 1.016 | 0.618 |
| log.ACTH | 101 | 1.134 | 0.774 | 1.662 | 0.517 | 1.121 | 0.775 | 1.621 | 0.545 |
| log.ADH | 74 | 1.159 | 0.930 | 1.444 | 0.190 | 1.094 | 0.872 | 1.372 | 0.436 |
| log.Alk | 104 | 1.249 | 0.953 | 1.636 | 0.107 | 0.896 | 0.681 | 1.178 | 0.431 |
| log.BS.Alk | 108 | 1.292 | 1.040 | 1.605 | 0.021 | 1.002 | 0.815 | 1.233 | 0.983 |
| log.Calcitonin | 88 | 1.581 | 1.202 | 2.079 | 0.001 | 1.566 | 1.196 | 2.050 | 0.001 |
| Calcium | 113 | 0.683 | 0.439 | 1.064 | 0.092 | 1.039 | 0.694 | 1.557 | 0.851 |
| log.CEA | 113 | 1.523 | 1.325 | 1.752 | <0.0001 | 1.263 | 1.083 | 1.474 | 0.003 |
| log.ChrA-1 | 74 | 0.871 | 0.702 | 1.079 | 0.206 | 0.941 | 0.769 | 1.151 | 0.553 |
| log.ChrA-2a | 35 | 1.630 | 1.010 | 2.610 | 0.045 | 1.200 | 0.803 | 1.789 | 0.375 |
| log.GRP | 57 | 0.791 | 0.501 | 1.247 | 0.313 | 0.794 | 0.537 | 1.173 | 0.247 |
| Hb | 114 | 0.804 | 0.709 | 0.912 | 0.001 | 0.915 | 0.817 | 1.025 | 0.127 |
| log.LDH | 114 | 2.714 | 1.698 | 4.340 | <0.0001 | 2.570 | 1.693 | 3.901 | 0.0001 |
| log.PAP | 111 | 1.080 | 0.952 | 1.226 | 0.231 | 1.084 | 0.956 | 1.229 | 0.211 |
| log.PSA | 114 | 1.029 | 0.913 | 1.161 | 0.639 | 1.031 | 0.921 | 1.155 | 0.591 |
| PSA DT | 52 | 1.066 | 0.935 | 1.216 | 0.340 | 1.012 | 0.916 | 1.118 | 0.810 |
| log.Somat | 106 | 2.253 | 1.320 | 3.845 | 0.003 | 1.763 | 1.072 | 2.899 | 0.025 |
| log.uNTX | 61 | 1.404 | 0.970 | 2.031 | 0.072 | 0.986 | 0.699 | 1.392 | 0.936 |
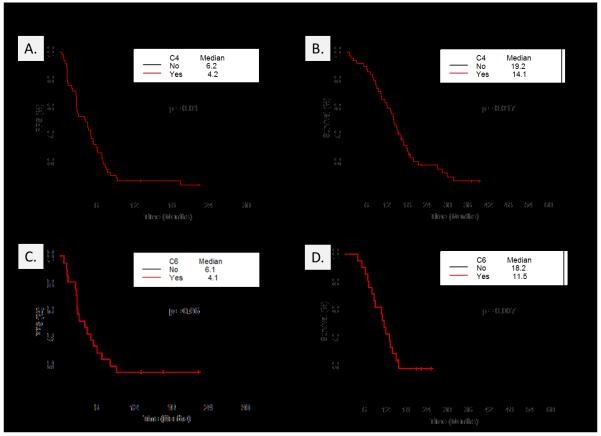
It is noteworthy that of the NE markers, only levels of calcitonin appeared significantly associated with PFS and OS and that levels of LDH and CEA appeared to have greater prognostic value than did levels of circulating chromogranin A and immunohistochemical positivity for either chromogranin A or synaptophysin. Of interest, abnormal CEA levels predicted poor OS (P < 0.0001) but not faster progression (p = 0.150) suggesting a benefit from chemotherapy despite portending a poor prognosis. Among the 7 clinical criteria, only C4 was significantly associated with both OS (p = 0.017) and PFS (p = 0.010), and it predicted faster progression and death, whereas C6 was associated with poor OS (p = 0.007) but not with rapid progression (p = 0.651) (Figs. 1 and 2). Also, the number of the 7 criteria met by a tumor was significantly associated with worse OS (HR = 1.41; p = 0.003).
Figure 1.
Effect of eligibility criteria on outcome. HR (and 95% CI) of the presence of each eligibility criterion (C1-C7, described in Table 1) for OS and PFS. HR = 1 implies no difference in OS/PFS given the presence or absence of the eligibility criterion.
Figure 2.
Kaplan-Meier estimates of OS and PFS for patients meeting eligibility criteria C4 and C6. A, PFS of patients meeting/not meeting eligibility criterion C4 (bulky ≥ 5 cm lymphadenopathy or high-grade tumor mass in prostate/pelvis). B, OS of patients meeting/not meeting eligibility criterion C4. C, PFS of patients meeting/not meeting eligibility criterion C6 (presence of NE markers on histology or serum plus elevated serum LDH and/or malignant hypercalcemia and/or elevated serum CEA). D, OS of patients meeting/not meeting eligibility criterion C6.
The frequency of bulky primary tumor versus bulky lymphadenopathy was determined in 47 of 49 study patients that satisfied C4 to explore associations with outcome. Thirty-six of 47 (76.6%) had bulky primary tumors, 3(6.4%) had both bulky primary tumors and bulky lymphadenopathy and 8(17.0%) had bulky lymph nodes only. No differences were apparent but the numbers are too small to draw any definitive conclusions (data not shown). We also asked whether, within C6, NE differentiation by serum or tissue criteria might be distinct in a predictive/prognostic sense from LDH and CEA. As stated above, immunohistochemistry for chromogranin A and synaptophysin on tumor tissues were only available for 51 (44.7%) of the 114 patients. To explore possible associations, we dichotomized variables based on presence or absence of marker staining or serum levels above/below IULN. In this analysis, no obvious differences were observed (data not shown) although given the number of missing values, significance cannot be reported.
Several of the eligibility criteria were linked as reflected by the correlation analyses. To investigate these connections further we clustered the data by clinical variables (Supplementary Fig. 1) and this pointed to the following associations:
- C4 with metastasis at diagnosis (which would have made treatment of the primary tumor less likely), with measurable disease, and also with elevated serum NE markers.
- C7 with elevated levels of PAP and/or PSA.
- C3 with elevated levels of LDH, alkaline phosphatase and bone-specific alkaline phosphatase.
- A remaining group that includes C1, C2, C5 and C6 and is associated with liver metastases and high levels of CEA.
We also examined the association between time on ADT prior to registration response to therapy (PD/noPD), TTP and OS. Wilcoxon rank test showed a marginally significant difference (p=0.05) in the mean time on ADT prior to registration between patients who progressed after 2 cycles of CD (n=18, 9.5 months) and those who did not (n=88, 20.5 months). No difference was noted (p=0.775) for response to 2 cycles of EP (n=28, 12.3 months vs n=38, 21.7 months respectively). Based on univariate Cox regression on OS, time on ADT (as a continuous variable) was marginally significant on OS (p = 0.09, HR = 0.99 – longer time on ADT had better OS); but not significant on TTP-CD (p = 0.51, HR =0.997) nor TTP-EP (p = 0.14, HR = 0.99).
Toxicity
In all, 544 cycles of CD were administered to 113 patients on study, and 226 cycles of EP were administered to 74. Four men died during treatment: 1 from neutropenic sepsis after EP and 3 from rapid PD after 2 cycles of CD (n = 1) and after 1 cycle of EP (n = 2). We observed no grade 3 or 4 sensory neuropathy. Grade 4 adverse events included thrombosis (n = 2) and thrombocytopenia (n = 1); the most common grade 3 events were infection with normal absolute neutrophil count or grade 1 or 2 neutropenia (n = 8), febrile neutropenia (n = 3), fatigue (n = 2), and vomiting (n = 2).
Discussion
This study is part of our broader effort to characterize patients with aggressive variant prostate cancer. It builds on the observation that prostate cancers that share clinical features with SCPCs also share their sensitivity to chemotherapy and the hypothesis that they are likely to share their underlying biology. We used 7 previously reported characteristics of SCPC (1-6) to select patients for this study. Our observations support the hypothesis that we can prospectively identify a distinct category of patients with castrate-resistant prostate cancer characterized by a distinctive pattern of progression, frequent but fleeting response to platinum-containing chemotherapy, and short survival.
Most of the patients treated experienced clinical benefit from the chemotherapy combinations despite having considerable tumor burden. However, this benefit was not reflected in the tumor-response rates using Prostate Cancer Clinical Trials Working Group (21) or RECIST criteria, which appear similar to response rates reported in first- and second-line clinical trials in castrate-resistant advanced prostate cancer (11, 12, 22, 23). Whether adding platinum agents to the chemotherapy regimen contributed to the high rate of benefit in our population cannot be determined from this trial but is the subject of an ongoing prospective randomized phase 2 study in which patients are stratified for the presence or absence of “anaplastic” criteria.
The clinical similarities between SCPC and the “anaplastic” variant suggest that they share underlying biological mechanisms of tumor progression. Several lines of experimental evidence implicate NE pathways in progression to androgen-independent prostate cancer (24). NE differentiation has primarily been defined as the presence of chromogranin A immunoreactivity and, as such, appears to confer a worse prognosis in castrate-resistant disease(25, 26). However, it has not been shown to define a distinct disease phenotype nor to predict therapy response(23, 27-29). In our patients, serum levels of calcitonin (but not chromogranin A) were associated with worse PFS and OS, suggesting that markers other than chromogranin A, or a combination of NE markers, might show stronger associations and define a distinct phenotype. Nonetheless, NE differentiation was present in slightly more than half of our patients. One plausible explanation is that the expression of NE markers is simply an epiphenomenon and not mechanistically implicated in progression. Another possibility is that the “anaplastic” category contains more than one aggressive variant, which would limit the ability to identify a meaningful association between NE marker expression and the clinical phenotype of the entire group.
This heterogeneity has potential clinical implications. For instance, another important characteristic of SCPCs is that they are androgen-receptor (AR) negative and thus presumably driven by AR-independent mechanisms. Therefore, the “anaplastic” prostate cancers should be enriched for truly AR-independent disease. However, of the 17 patients (14.9%) who met only criterion C7, eight (47.0%) had predominantly bony disease and elevated PSA levels without measurable disease by RECIST (data not shown). These features are closer to those of conventional AR-driven prostate carcinomas and suggest that, among men with “anaplastic” disease, at least some with short responses to ADT have early castrate-resistant AR axis-regulated disease rather than true AR-independent disease. Nonetheless, at least 1 of these patients experienced progression with biopsy-proven SCPC in the primary tumor and the liver after prolonged SD following treatment with CD. Detailed molecular studies of tissues collected from these patients will help elucidate this heterogeneity.
It is noteworthy that increased CEA levels in this study were significantly associated with patient outcome. Blood levels of CEA are increased in 53%-65% of men with biopsy-proven SCPC(5, 6). Additionally, older literature reported serum CEA to be elevated in 23%-80% of patients with prostate carcinoma, without a definite correlation with tumor stage (30), although the cutoffs to define an elevation varied between studies. This marker’s prognostic value was investigated in a National Cancer Institute study that pooled the CEA values of 141 men with “androgen-independent metastatic” prostate cancer participating in clinical trials between 1990 and 1996. In that study, CEA levels > 2.5 μg/L had minimal prognostic value and no usefulness as a response marker (31). However, studies that used higher cutoffs to define an abnormal value found plasma CEA to be a sensitive marker of the clinical status of prostate cancer during chemotherapy(32, 33). Our data showing that high CEA levels are associated with worse OS but not PFS suggest that this marker identifies a population with aggressive disease that nevertheless benefits from chemotherapy.
Another observation in this population is that many patients suffered substantial morbidity from progression at an untreated or radiorecurrent primary site. Some 24%-44% of men treated for prostate cancer with noncurative intent will develop symptomatic local progression requiring intervention(34, 35). Moreover, retrospective studies suggest that control of the primary tumor may improve the outcome of men with metastatic disease (36), a fact borne out in randomized trials in men with locally advanced prostate cancer (37, 38), which is in line with observations in other tumor types (39, 40). These data may justify applying consolidative definitive treatment to the primary tumor despite the presence of distant metastases in this patient population.
Our findings confirm the usefulness of clinical criteria for identifying a subset of patients with prostate cancer with an atypical and aggressive clinical course that may also be characterized by sensitivity to platinum-containing combination chemotherapy. They provide the impetus to further study this unique phenotype, which accounts for a considerable proportion of lethal prostate cancers. Parallel efforts to understand the drivers of these variant prostate cancers are under way in model systems that reflect the salient features observed clinically(41, 42). The ongoing clinical and co-clinical studies should lead to a reclassification of prostate cancer founded on an understanding its underlying biology.
Supplementary Material
1
Translational Relevance.
The clinical application of effective androgen receptor (AR) inhibition has benefitted a large number of men with castrate-resistant prostate carcinoma (CRPC). However, the driver(s) of the disease beyond AR are poorly understood. Small-cell prostate carcinoma (SCPC) is a morphologic variant of prostate cancer that does not express AR and is linked to a short survival. SCPC is rare at initial diagnosis but present in 10-20% of men with lethal CRPC. Moreover clinical features characteristic of SCPC are present in a significant proportion of morphologically heterogeneous CRPCs. We hypothesized that prostate cancers that share clinical features with SCPC (“anaplastic” prostate cancers) also share its responsiveness to chemotherapy and underlying biology. Here we used “anaplastic” criteria to select men with CRPC (plausibly enriched for AR-independent CRPC) for treatment with platinum-based chemotherapies as part of a broader effort to contribute to the development of a clinically meaningful, biologically based classification of prostate cancer.
Acknowledgments
We thank Karen Phillips, ELS(D), of the Department of Genitourinary Medical Oncology, for manuscript editing.
Financial Support: Supported in part by the National Institutes of Health through The University of Texas MD Anderson Cancer Center Support Grant (CA016672), by the David H. Koch Center for Applied Research of Genitourinary Cancers, and by the Department of Defense Prostate Cancer Clinical Trial Consortium.
Footnotes
Disclosure of Potential Conflicts of Interest: The authors have no potential conflicts of interest.
References
- 1.Mahadevia PS, Ramaswamy A, Greenwald ES, Wollner DI, Markham D. Hypercalcemia in prostatic carcinoma. Report of eight cases. Arch Intern Med. 1983;143:1339–42. [PubMed] [Google Scholar]
- 2.Hindson DA, Knight LL, Ocker JM. Small-cell carcinoma of prostate. Transient complete remission with chemotherapy. Urology. 1985;26:182–4. doi: 10.1016/0090-4295(85)90060-3. [DOI] [PubMed] [Google Scholar]
- 3.Tetu B, Ro JY, Ayala AG, Johnson DE, Logothetis CJ, Ordonez NG. Small cell carcinoma of the prostate. Part I. A clinicopathologic study of 20 cases. Cancer. 1987;59:1803–9. doi: 10.1002/1097-0142(19870515)59:10<1803::aid-cncr2820591019>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- 4.Oesterling JE, Hauzeur CG, Farrow GM. Small cell anaplastic carcinoma of the prostate: a clinical, pathological and immunohistological study of 27 patients. J Urol. 1992;147:804–7. doi: 10.1016/s0022-5347(17)37390-1. [DOI] [PubMed] [Google Scholar]
- 5.Amato RJ, Logothetis CJ, Hallinan R, Ro JY, Sella A, Dexeus FH. Chemotherapy for small cell carcinoma of prostatic origin. J Urol. 1992;147:935–7. doi: 10.1016/s0022-5347(17)37427-x. [DOI] [PubMed] [Google Scholar]
- 6.Papandreou CN, Daliani DD, Thall PF, Tu SM, Wang X, Reyes A, et al. Results of a phase II study with doxorubicin, etoposide, and cisplatin in patients with fully characterized small-cell carcinoma of the prostate. J Clin Oncol. 2002;20:3072–80. doi: 10.1200/JCO.2002.12.065. [DOI] [PubMed] [Google Scholar]
- 7.Moore SR, Reinberg Y, Zhang G. Small cell carcinoma of prostate: effectiveness of hormonal versus chemotherapy. Urology. 1992;39:411–6. doi: 10.1016/0090-4295(92)90235-o. [DOI] [PubMed] [Google Scholar]
- 8.Turbat-Herrera EA, Herrera GA, Gore I, Lott RL, Grizzle WE, Bonnin JM. Neuroendocrine differentiation in prostatic carcinomas. A retrospective autopsy study. Arch Pathol Lab Med. 1988;112:1100–5. [PubMed] [Google Scholar]
- 9.Tanaka M, Suzuki Y, Takaoka K, Suzuki N, Murakami S, Matsuzaki O, et al. Progression of prostate cancer to neuroendocrine cell tumor. Int J Urol. 2001;8:431–6. doi: 10.1046/j.1442-2042.2001.00347.x. discussion 7. [DOI] [PubMed] [Google Scholar]
- 10.Shah RB, Mehra R, Chinnaiyan AM, Shen R, Ghosh D, Zhou M, et al. Androgen-independent prostate cancer is a heterogeneous group of diseases: lessons from a rapid autopsy program. Cancer Res. 2004;64:9209–16. doi: 10.1158/0008-5472.CAN-04-2442. [DOI] [PubMed] [Google Scholar]
- 11.Tannock IF, de Wit R, Berry WR, Horti J, Pluzanska A, Chi KN, et al. Docetaxel plus prednisone or mitoxantrone plus prednisone for advanced prostate cancer. N Engl J Med. 2004;351:1502–12. doi: 10.1056/NEJMoa040720. [DOI] [PubMed] [Google Scholar]
- 12.Petrylak DP, Tangen CM, Hussain MH, Lara PN, Jr., Jones JA, Taplin ME, et al. Docetaxel and estramustine compared with mitoxantrone and prednisone for advanced refractory prostate cancer. N Engl J Med. 2004;351:1513–20. doi: 10.1056/NEJMoa041318. [DOI] [PubMed] [Google Scholar]
- 13.Smyth JF, Smith IE, Sessa C, Schoffski P, Wanders J, Franklin H, et al. Activity of docetaxel (Taxotere) in small cell lung cancer. The Early Clinical Trials Group of the EORTC. Eur J Cancer. 1994;30A:1058–60. doi: 10.1016/0959-8049(94)90455-3. [DOI] [PubMed] [Google Scholar]
- 14.Hesketh PJ, Crowley JJ, Burris HA, 3rd, Williamson SK, Balcerzak SP, Peereboom D, et al. Evaluation of docetaxel in previously untreated extensive-stage small cell lung cancer: a Southwest Oncology Group phase II trial. Cancer J Sci Am. 1999;5:237–41. [PubMed] [Google Scholar]
- 15.Rossi A, Martelli O, Di Maio M. Treatment of patients with small-cell lung cancer: From meta-analyses to clinical practice. Cancer Treat Rev. 2012 doi: 10.1016/j.ctrv.2012.09.006. doi: 10.1016/j.ctrv.2012.09.006. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 16.Canobbio L, Guarneri D, Miglietta L, Decensi A, Oneto F, Boccardo F. Carboplatin in advanced hormone refractory prostatic cancer patients. Eur J Cancer. 1993;29A:2094–6. doi: 10.1016/0959-8049(93)90040-m. [DOI] [PubMed] [Google Scholar]
- 17.Graham TR, Yacoub R, Taliaferro-Smith L, Osunkoya AO, Odero-Marah VA, Liu T, et al. Reciprocal regulation of ZEB1 and AR in triple negative breast cancer cells. Breast Cancer Res Treat. 2010;123:139–47. doi: 10.1007/s10549-009-0623-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS, Rubinstein L, et al. European Organization for Research and Treatment of Cancer. National Cancer Institute of the United States. National Cancer Institute of Canada New guidelines to evaluate the response to treatment in solid tumors. J Natl Cancer Inst. 2000;92:205–16. doi: 10.1093/jnci/92.3.205. [DOI] [PubMed] [Google Scholar]
- 19.Bubley GJ, Carducci M, Dahut W, Dawson N, Daliani D, Eisenberger M, et al. Eligibility and response guidelines for phase II clinical trials in androgen-independent prostate cancer: recommendations from the Prostate-Specific Antigen Working Group. J Clin Oncol. 1999;17:3461–7. doi: 10.1200/JCO.1999.17.11.3461. [DOI] [PubMed] [Google Scholar]
- 20.Therneau TM, Grambsch PM. Modeling survival data: extending the Cox model. Springer; New York: 2000. [Google Scholar]
- 21.Scher HI, Halabi S, Tannock I, Morris M, Sternberg CN, Carducci MA, et al. Design and end points of clinical trials for patients with progressive prostate cancer and castrate levels of testosterone: recommendations of the Prostate Cancer Clinical Trials Working Group. J Clin Oncol. 2008;26:1148–59. doi: 10.1200/JCO.2007.12.4487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ross RW, Beer TM, Jacobus S, Bubley GJ, Taplin ME, Ryan CW, et al. A phase 2 study of carboplatin plus docetaxel in men with metastatic hormone-refractory prostate cancer who are refractory to docetaxel. Cancer. 2008;112:521–6. doi: 10.1002/cncr.23195. [DOI] [PubMed] [Google Scholar]
- 23.Loriot Y, Massard C, Gross-Goupil M, Di Palma M, Escudier B, Bossi A, et al. Combining carboplatin and etoposide in docetaxel-pretreated patients with castration-resistant prostate cancer: a prospective study evaluating also neuroendocrine features. Ann Oncol. 2009;20:703–8. doi: 10.1093/annonc/mdn694. [DOI] [PubMed] [Google Scholar]
- 24.di Sant’Agnese PA. Neuroendocrine differentiation in prostatic carcinoma: an update on recent developments. Ann Oncol. 2001;12(Suppl 2):S135–40. [PubMed] [Google Scholar]
- 25.Taplin ME, George DJ, Halabi S, Sanford B, Febbo PG, Hennessy KT, et al. Prognostic significance of plasma chromogranin a levels in patients with hormone-refractory prostate cancer treated in Cancer and Leukemia Group B 9480 study. Urology. 2005;66:386–91. doi: 10.1016/j.urology.2005.03.040. [DOI] [PubMed] [Google Scholar]
- 26.Berruti A, Mosca A, Tucci M, Terrone C, Torta M, Tarabuzzi R, et al. Independent prognostic role of circulating chromogranin A in prostate cancer patients with hormone-refractory disease. Endocr Relat Cancer. 2005;12:109–17. doi: 10.1677/erc.1.00876. [DOI] [PubMed] [Google Scholar]
- 27.Culine S, El Demery M, Lamy PJ, Iborra F, Avances C, Pinguet F. Docetaxel and cisplatin in patients with metastatic androgen independent prostate cancer and circulating neuroendocrine markers. J Urol. 2007;178:844–8. doi: 10.1016/j.juro.2007.05.044. [DOI] [PubMed] [Google Scholar]
- 28.Steineck G, Reuter V, Kelly WK, Frank R, Schwartz L, Scher HI. Cytotoxic treatment of aggressive prostate tumors with or without neuroendocrine elements. Acta Oncol. 2002;41:668–74. doi: 10.1080/028418602321028292. [DOI] [PubMed] [Google Scholar]
- 29.Flechon A, Pouessel D, Ferlay C, Perol D, Beuzeboc P, Gravis G, et al. Phase II study of carboplatin and etoposide in patients with anaplastic progressive metastatic castration-resistant prostate cancer (mCRPC) with or without neuroendocrine differentiation: results of the French Genito-Urinary Tumor Group (GETUG) P01 trial. Ann Oncol. 2011;22:2476–81. doi: 10.1093/annonc/mdr004. [DOI] [PubMed] [Google Scholar]
- 30.Schacht MJ, Garnett JE, Grayhack JT. Biochemical markers in prostatic cancer. Urol Clin North Am. 1984;11:253–67. [PubMed] [Google Scholar]
- 31.Feuer JA, Lush RM, Venzon D, Duray P, Tompkins A, Sartor O, et al. Elevated carcinoembryonic antigen in patients with androgen-independent prostate cancer. J Investig Med. 1998;46:66–72. [PubMed] [Google Scholar]
- 32.Kane RD, Mickey DD, Paulson DF. Serial carcinoembryonic antigen assays in patients with metastatic carcinoma of prostate being treated with chemotherapy. Urology. 1976;8:559–62. doi: 10.1016/0090-4295(76)90517-3. [DOI] [PubMed] [Google Scholar]
- 33.Ihde DC, Bunn PA, Cohen MH, Dunnick NR, Eddy JL, Minna JD. Effective treatment of hormonally-unresponsive metastatic carcinoma of the prostate with adriamycin and cyclophosphamide: methods of documenting tumor response and progression. Cancer. 1980;45:1300–10. doi: 10.1002/1097-0142(19800315)45:6<1300::aid-cncr2820450606>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- 34.Aus G, Hugosson J, Norlen L. Need for hospital care and palliative treatment for prostate cancer treated with noncurative intent. J Urol. 1995;154:466–9. doi: 10.1097/00005392-199508000-00034. [DOI] [PubMed] [Google Scholar]
- 35.Wiegand LR, Hernandez M, Pisters LL, Spiess PE. Surgical management of lymph-node-positive prostate cancer: improves symptomatic control. BJU Int. 2011;107:1238–42. doi: 10.1111/j.1464-410X.2010.09657.x. [DOI] [PubMed] [Google Scholar]
- 36.Qin XJ, Ma CG, Ye DW, Yao XD, Zhang SL, Dai B, et al. Tumor cytoreduction results in better response to androgen ablation--a preliminary report of palliative transurethral resection of the prostate in metastatic hormone sensitive prostate cancer. Urol Oncol. 2012;30:145–9. doi: 10.1016/j.urolonc.2010.02.010. [DOI] [PubMed] [Google Scholar]
- 37.Widmark A, Klepp O, Solberg A, Damber JE, Angelsen A, Fransson P, et al. Endocrine treatment, with or without radiotherapy, in locally advanced prostate cancer (SPCG-7/SFUO-3): an open randomised phase III trial. Lancet. 2009;373:301–8. doi: 10.1016/S0140-6736(08)61815-2. [DOI] [PubMed] [Google Scholar]
- 38.Warde P, Mason M, Ding K, Kirkbride P, Brundage M, Cowan R, et al. Combined androgen deprivation therapy and radiation therapy for locally advanced prostate cancer: a randomised, phase 3 trial. Lancet. 2011;378:2104–11. doi: 10.1016/S0140-6736(11)61095-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Flanigan RC, Salmon SE, Blumenstein BA, Bearman SI, Roy V, McGrath PC, et al. Nephrectomy followed by interferon alfa-2b compared with interferon alfa-2b alone for metastatic renal-cell cancer. N Engl J Med. 2001;345:1655–9. doi: 10.1056/NEJMoa003013. [DOI] [PubMed] [Google Scholar]
- 40.Rapiti E, Verkooijen HM, Vlastos G, Fioretta G, Neyroud-Caspar I, Sappino AP, et al. Complete excision of primary breast tumor improves survival of patients with metastatic breast cancer at diagnosis. J Clin Oncol. 2006;24:2743–9. doi: 10.1200/JCO.2005.04.2226. [DOI] [PubMed] [Google Scholar]
- 41.Aparicio A, Tzelepi V, Araujo JC, Guo CC, Liang S, Troncoso P, et al. Neuroendocrine prostate cancer xenografts with large-cell and small-cell features derived from a single patient’s tumor: morphological, immunohistochemical, and gene expression profiles. Prostate. 2011;71:846–56. doi: 10.1002/pros.21301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tzelepi V, Zhang J, Lu JF, Kleb B, Wu G, Wan X, et al. Modeling a lethal prostate cancer variant with small-cell carcinoma features. Clin Cancer Res. 2012;18:666–77. doi: 10.1158/1078-0432.CCR-11-1867. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
1