Contagious Diseases in the United States from 1888 to the Present (original) (raw)
. Author manuscript; available in PMC: 2014 Sep 26.
Published in final edited form as: N Engl J Med. 2013 Nov 28;369(22):2152–2158. doi: 10.1056/NEJMms1215400
Public health programs — especially vaccination — have led to dramatic declines in the incidence of contagious diseases in the United States over the past century.1–3 However, some contagious diseases are now on the rise despite the availability of vaccines. Pertussis vaccines have been available since the 1920s, but the worst pertussis epidemic since 1959 occurred in 2012, with more than 38,000 cases nationwide reported by last December.4,5 Outbreaks of measles also continue to occur, even though a measles vaccine has been licensed in the United States since 1963.6
The current low overall incidence of contagious diseases has resulted in a perception that the risk of these diseases is low — and paradoxically — in increased concerns about the costs and consequences of vaccination programs (e.g., adverse events, expenses, and inconvenience).7–9 Low perceived risk of disease at the individual level can lead to lower participation in control programs, with negative consequences for the entire community — a well-known game-theory principle that applies to vaccination programs as well.10,11 Parents who question the risk–benefit balance of vaccination may refuse or delay immunization of their children, which leads to local variations in vaccine coverage and increased risk of disease outbreaks due to localized disruptions of herd immunity.12 Both pertussis and measles outbreaks have been attributed at least in part to intentional undervaccination.7,8,13 Organized antivaccination movements amplify these problems.14,15 The medical community needs to seriously address parental concerns about the value of immunization at the individual and community levels by introducing scientific evidence in the context of trusting clinician–parent relationships.8,9,16
The interpretation of long-term disease patterns at the local level has heretofore been hampered by a lack of access to high-resolution historical data in computable form. In cases in which detailed long-term data have been available (e.g., with regard to measles and pertussis in the United Kingdom or dengue in Thailand), pattern analysis has yielded new insights into disease-transmission dynamics.17–20 In the United States, cases of contagious diseases have been reported to health authorities for more than a century, but these data have not been available in a computable format, so their use and value have been limited.
Data and Analysis
In an effort to overcome these limitations, we digitized all weekly surveillance reports of notifiable diseases for U.S. cities and states published between 1888 and 2011. This data set, which we have made publicly available (www.tycho.pitt.edu), consists of 87,950,807 reported individual cases, each localized in space and time. We used these data to derive a quantitative history of disease reduction in the United States over the past century, focusing particularly on the effect of vaccination programs.
We obtained all weekly notifiable disease surveillance tables published between 1888 and 2011 in the Morbidity Mortality Weekly Report and its precursor journals from various online and hardcopy sources.21–24 We digitized all data available in tabular format that listed etiologically defined cases or deaths by week for locations in the United States. Reported counts (weekly tallies) of cases or deaths and the reporting locations, periods, and diseases were extracted from these data and standardized. Then we selected eight vaccine-preventable contagious diseases for more detailed analysis and computed weekly incidence rates, deriving a quantitative history of each disease.
The number of cases prevented since vaccine introduction was estimated for seven of the eight diseases; because there were no data from the pre-smallpox-vaccination era (before 1800), we could not quantify the number of smallpox cases prevented by vaccines. We estimated the numbers of cases of polio, measles, rubella, mumps, hepatitis A, diphtheria, and pertussis that were prevented by subtracting the reported number of weekly cases after vaccine introduction from a simulated counterfactual number of cases that would have occurred in the absence of vaccination, assuming no other changes affecting incidence rates occurred. We used the year of vaccine licensure as the cutoff year to separate the prevaccine period from the vaccination period. Counterfactuals were estimated by multiplying the median weekly incidence rate from prevaccine years with population estimates for vaccination years. (A full description of data sources and methods, along with additional figures and tables, are provided in the Supplementary Appendix available with the full text of this article at NEJM.org.)
A total of 56 notifiable diseases were reported at some time between 1888 and the present in U.S. cities, counties, and states. No single disease was reported continuously throughout this interval. Changes in which conditions were reportable reflected shifting public health challenges and priorities (Fig. 1).
Figure 1.
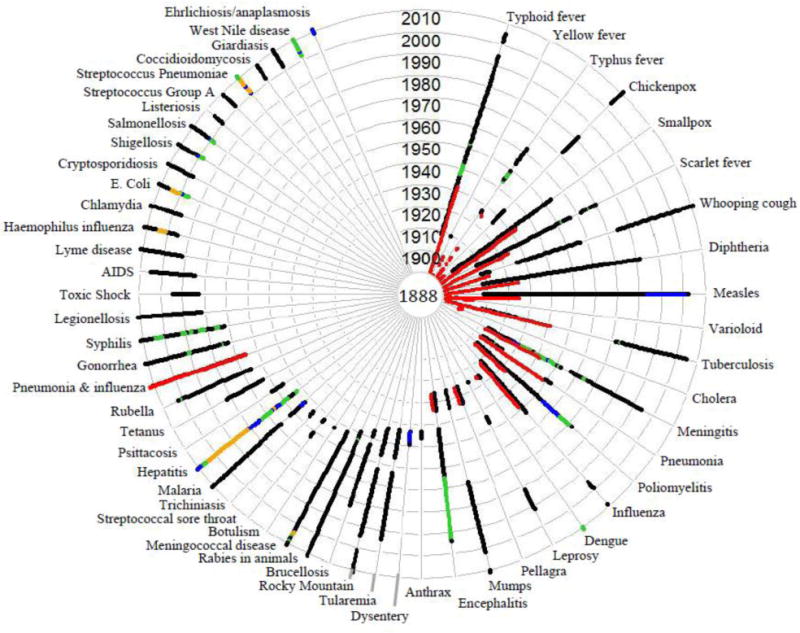
Availability of Weekly Counts of Cases of Reported Diseases from Any U.S. Location, 1888–2011. Each concentric circle represents a decade, starting with 1888 in the center. No single disease was reported weekly throughout the entire period, and for many diseases, the type of reports changed over time, as represented by different colors: red represents mortality reports and black, green, blue, and orange represent reporting of cases for 1, 2, 3, or more than 3 disease subcategories, respectively.
Decline of Contagious Diseases
We examined historical temporal transmission patterns at the state or city level for eight vaccine-preventable diseases. For each disease, temporal patterns started with high incidence rates and (often seasonally recurring) disease epidemics, followed by a period of persisting reduced transmission (Fig. 2). The smallpox vaccine was introduced in the United States around 1800 by Dr. Benjamin Waterhouse at Harvard University who received the vaccine from Dr. John Haygarth of Bath, Sommerset who received it from Edward Jenner. Severe smallpox disease caused by the Variola major virus was already eliminated from the United States by 1927, but annual epidemics of the less severe Variola minor virus continued until the disease was eradicated in the late 1940s.
Figure 2.
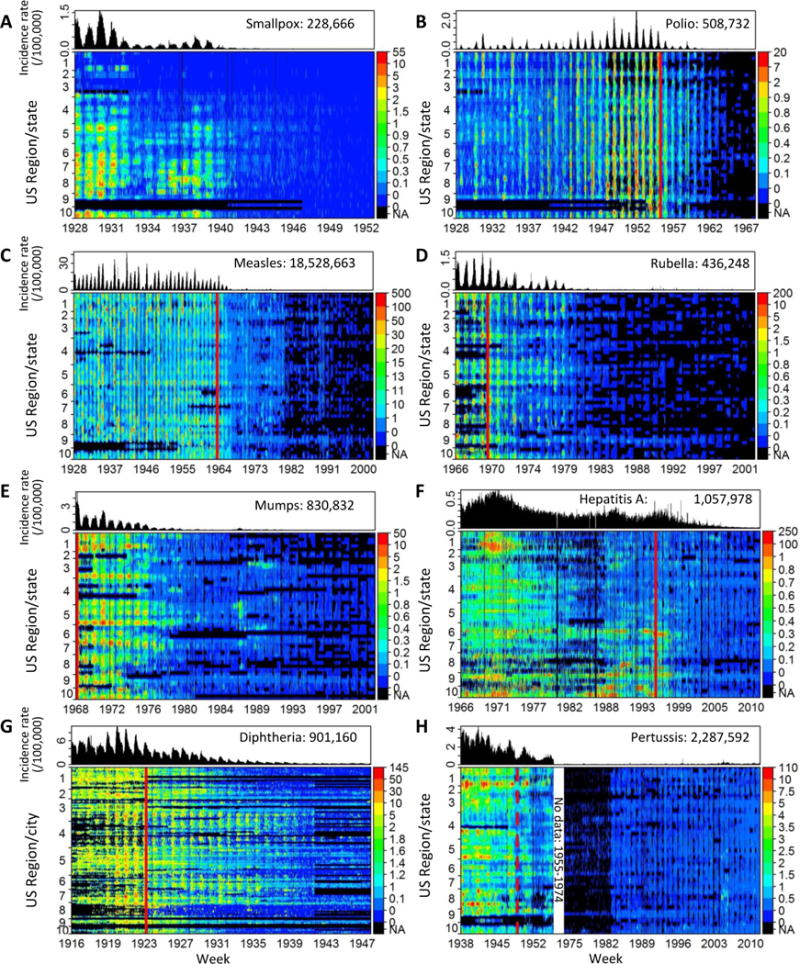
Snapshots of Disease Elimination in the United States. Weekly incidence rates per 100,000 population are displayed for the entire country (top of each panel) and per state (for all diseases except diphtheria) or city (for diphtheria) grouped by US epidemiological region in the following order: region 1= Connecticut, Maine, Massachusetts, New Hampshire, Rhode Island, Vermont; 2= New Jersey, New York; 3= Delaware, District of Columbia, Maryland, Pennsylvania, Virginia, West Virginia; 4= Alabama, Florida, Georgia, Kentucky, Mississippi, North Carolina, South Carolina, Tennessee; 5= Illinois, Indiana, Michigan, Minnesota, Ohio, Wisconsin; 6= Arkansas, Louisiana, New Mexico, Oklahoma, Texas; 7= Iowa, Kansas, Missouri, Nebraska; 8= Colorado, Montana, North Dakota, South Dakota, Utah, Wyoming; 9= Arizona, California, Hawaii, Nevada; 10= Alaska, Idaho, Oregon, Washington. The year of vaccine licensure is indicated by a vertical red line, and the total number of cases displayed is listed for each disease. The smallpox vaccine was introduced in the United States around 1800. Weekly reports for pertussis were unavailable from 1955 to 1974 (white space), and an approximate year of vaccine licensure was used (dashed line). NA denotes data not available (i.e. not included in weekly reports).
The inactivated Salk polio vaccine was licensed in 1955, and polio incidence rates decreased substantially in the succeeding years. An additional reduction followed the licensure of the Sabin live oral polio vaccine in 1961, until eradication was achieved in 1979.
Measles, rubella, and mumps occurred in well-characterized annual and biannual epidemics, with a median incidence rate before the introduction of a vaccine of 317.1, 28.1, and 89.5 cases per 100,000 population, respectively. The Edmonston measles vaccine was licensed in 1963, and measles incidence rates declined rapidly afterward, whereas rubella and mumps persisted until the late 1970s despite vaccine licensure in 1969 and 1967, respectively. Vaccination programs that started in the late 1970s (the Measles Immunization Initiative and the National Childhood Immunization Initiative) and the introduction of the combined measles–mumps–rubella (MMR) vaccine in 1978 led to major reductions in transmission of these diseases.
Incidence rates of hepatitis A infection declined across large parts of the United States in the late 1970s, presumably because of improved water and sanitation, but high transmission rates (a yearly median incidence ratio of 24.5; 10th percentile–90th percentile, 12.3–40.2) continued in some regions (e.g., the South, the Northwest, and the Pacific Coast). Hepatitis A vaccine was licensed in 1995, and its routine use in 11 states with elevated transmission was recommended 4 years later. In 2006, this vaccine was recommended for all states, leading to a wide-scale reduction in hepatitis A throughout the United States.
Diphtheria immunization started with the use of toxin–antitoxin around 1914, but annual epidemics continued until the introduction of heat-inactivated diphtheria toxoid discovered by Gaston Ramon in 1923. Only city-level data were available for the years before and after 1923. Large variation was found in diphtheria-reduction rates among cities after the toxoid became available, probably owing to varying policies on vaccine introduction. The whole-cell pertussis vaccine was already licensed in the United States around 1914 but not widely recommended until it was combined with diphtheria toxoid and tetanus toxoid in the diphtheria–tetanus–pertussis (DTP) vaccine in 1948. Until then, major pertussis epidemics occurred annually throughout the country.
Assuming that the difference between prevaccine and vaccine disease incidence rates was attributable solely to vaccination programs, we estimate that a total of 103.1 million cases of these contagious diseases have been prevented since 1924 (10th–90th percentiles, 72.3 million–147.8 million); of those hypothetical cases, approximately 26 million were prevented in the past decade. Sensitivity analysis using different methods for imputing missing data and for simulating counterfactual cases resulted in estimates ranging from about 75 million to 106 million prevented cases. The number of cases prevented per disease depended on the incidence rate before vaccination and the duration of the vaccination program. Diphtheria had the greatest estimated number of cases prevented (about 40 million), having had the second-highest prevaccination incidence rate (237 cases per 100,000 population per year) and the longest-standing vaccination program (since 1924). An estimated 35 million measles cases have been prevented, even though vaccination started relatively recently (1963). The measles incidence rate before the vaccine was introduced (318 cases per 100,000 population per year) was the highest among the diseases we studied, and the proportion of cases prevented increased rapidly in the years following vaccine licensure, which suggests that the vaccine rollout program was fast and widespread.
The proportion of cases of each disease that were prevented increased in the years after vaccine licensure, but the rates of decrease varied. The disease with the most rapid increase was measles, with 22.2% more cases prevented each year, on average, during the first 5 years after vaccine licensure (10th–90th percentiles, 12.8–29.7%); rubella and polio were next, with annual increases in prevented cases of 16.2% and 15.3%, respectively. By year 5 after vaccine licensure, 95% of measles cases were prevented, a milestone reached for polio in year 8 — as compared with 19 years for diphtheria and 17 for pertussis, presumably owing to much slower vaccine rollouts in a different era.
Recent Resurgences
Despite successful vaccination programs, multiple resurgences of measles, rubella, mumps, and pertussis have occurred since the 1980s. Measles outbreaks were continuously reported throughout the country during the 1980s, and a major resurgence in 1989–1990 affected the entire country. Since the early 1980s, the rubella incidence rate has been elevated in California, and a large outbreak occurred in 1990–1991. A major resurgence of mumps occurred in 1986–1987 in multiple states, and the incidence rate has continued to be elevated in some of those states ever since. Pertussis is the only vaccine-preventable disease that has been consistently on the rise in the United States, with yearly incidence rates increasing since 1976. In 2003–2005 and again in 2010, there were resurgences of pertussis throughout the country, with the highest incidence rates in the Midwest to Northwest and in the Northeast. Last year (2012), the largest pertussis outbreak since 1959 was reported in the United States with over 38,000 cases nationwide.
Implications for Immunization Programs
Our digitization project, Project Tycho (named after Tycho Brahe, the Danish astronomer whose comprehensive data set was used by Johannes Kepler to derive the laws of planetary motion25), led to descriptions of population-scale disease patterns that provide strong evidence of the value of vaccination programs. We estimate that 103 million cases of childhood diseases (95% of those that would otherwise have occurred) have been prevented since 1924; in the past decade alone, 26 million cases (99% of those that would otherwise have occurred) were prevented. These results are consistent with previous estimates of 92 to 100% of cases prevented in 2006 and 86 to 100% of cases prevented in 2010.1,3
For some diseases including measles, hepatitis A, diphtheria, and pertussis, incidence rates had variable baseline patterns before the vaccine-introduction years, possibly owing to non–vaccine-related factors (e.g., sanitation, hygiene, or demographic factors) or to the use of early vaccine formulations (diphtheria toxin–antitoxin or early whole-cell pertussis vaccines). In the absence of clear-cut trends, and given known seasonal and multi-year dynamics and complex interactions, the causes of variable baselines in incidence cannot be disentangled without detailed historical data that are currently not available.
In contrast, the striking and persistent reductions in disease incidence rates after vaccine licensure (Fig. 2) strongly support the conclusion that vaccination programs were a leading cause. As in previous studies,1,26 we made the simplifying assumption of attributing the entire difference between prevaccine and vaccine incidence rates to immunization programs. The range of 75 million to 106 million cases prevented by vaccines is probably an underestimate, since we could not include all vaccine-preventable diseases. We also could not adjust for underreporting of cases but this would have increased the number of cases prevented,given that the underreporting rate was probably higher in the prevaccine period than in the later vaccine period. Detailed historical demographic data such as birth rates and age-specific disease incidence rates would enable such adjustment but are currently only available for a small number of locations and for limited time periods.
Multiple resurgences of four contagious diseases (measles, rubella, mumps, and pertussis) have occurred despite vigorous ongoing vaccination programs. Local gaps in vaccine coverage can disrupt local herd immunity, resulting in outbreaks when people come into contact with pathogens because of imported cases or relocation (e.g., college enrollment).6,27 Reported rates of vaccine refusal or delay are increasing.7–9,12,13 The 1989–1990 measles resurgence occurred mostly among preschool children in minority ethnic groups in which the vaccination rate was only 19%. Other outbreaks have been linked to similarly low immunization rates.28–30 Failure to vaccinate is believed to contribute to the reemergence of pertussis, including the large 2012 epidemic. Between 1980 and 1989, 64% of almost 10,000 U.S. children with pertussis had not been appropriately vaccinated, and 37% of them had never even received one dose of the DTP vaccine.31
Our analysis demonstrates how high-resolution spatiotemporal data can be effectively used to illustrate these trends at the national and local levels and to inform public opinion about the necessity of vaccination programs. Detailed spatiotemporal public health data have too often remained inaccessible and therefore underutilized. Lack of access to historical epidemiologic data constrains scientific understanding of the dynamics of disease transmission, hampers disease-control programs, and limits public health education programs. We believe that open access to large disease surveillance data sets in computable form should become a worldwide norm.
Supplementary Material
Tycho supplement
Acknowledgments
Supported by research awards from the Bill and Melinda Gates Foundation (Grant 49276, Evaluation of Candidate Vaccine Technologies Using Computational Models) and from the US National Institute of General Medical Sciences (Grant 5U54GM088491, Computational Models of Infectious Disease Threats).
We thank the following people and institutions for their assistance: Stephen Wisniewski (data management), David Galloway (database design), Ying-Feng Hsu (informatics), Divyasheel Sharma (informatics), Stephen Ostroff (epidemiology), Ronald Rosenfeld (manuscript review), Sharon Crow (manuscript review), Digital Divide Data (data entry), the U.S. Centers for Disease Control and Prevention Office of Surveillance, Epidemiology, and Laboratory Services (scientific discussions) and the Centers for Disease Control and Prevention and its precursor institutions (data collection), and the state health departments (scientific input and data collection).
Footnotes
Disclosure forms provided by the authors are available with the full text of this article at NEJM.org.
References
- 1.Roush SW, Murphy TV. Historical comparisons of morbidity and mortality for vaccine-preventable diseases in the United States. JAMA. 2007;298:2155–63. doi: 10.1001/jama.298.18.2155. [DOI] [PubMed] [Google Scholar]
- 2.Ten great public health achievements–United States, 2001–2010. MMWR Morb Mortal Wkly Rep. 2011;60:619–23. [PubMed] [Google Scholar]
- 3.Hinman AR, Orenstein WA, Schuchat A. Vaccine-preventable diseases, immunizations, and MMWR–1961–2011. MMWR Surveill Summ. 2011;60(Suppl 4):49–57. [PubMed] [Google Scholar]
- 4.Cherry JD. Epidemic pertussis in 2012–the resurgence of a vaccine-preventable disease. N Engl J Med. 2012;367:785–7. doi: 10.1056/NEJMp1209051. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. Notifiable Diseases and Mortality Tables. Morbidity and Mortality Weekly Report. 2012;61:ND-663–ND-76. [Google Scholar]
- 6.Vaccination coverage among children in kindergarten–United States, 2011–12 school year. MMWR Morb Mortal Wkly Rep. 2012;61:647–52. [PubMed] [Google Scholar]
- 7.Omer SB, Salmon DA, Orenstein WA, deHart MP, Halsey N. Vaccine refusal, mandatory immunization, and the risks of vaccine-preventable diseases. N Engl J Med. 2009;360:1981–8. doi: 10.1056/NEJMsa0806477. [DOI] [PubMed] [Google Scholar]
- 8.Diekema DS. Improving childhood vaccination rates. N Engl J Med. 2012;366:391–3. doi: 10.1056/NEJMp1113008. [DOI] [PubMed] [Google Scholar]
- 9.Larson HJ, Cooper LZ, Eskola J, Katz SL, Ratzan S. Addressing the vaccine confidence gap. Lancet. 2011;378:526–35. doi: 10.1016/S0140-6736(11)60678-8. [DOI] [PubMed] [Google Scholar]
- 10.Fine PE, Clarkson JA. Individual versus public priorities in the determination of optimal vaccination policies. Am J Epidemiol. 1986;124:1012–20. doi: 10.1093/oxfordjournals.aje.a114471. [DOI] [PubMed] [Google Scholar]
- 11.Shim E, Grefenstette JJ, Albert SM, Cakouros BE, Burke DS. A game dynamic model for vaccine skeptics and vaccine believers: measles as an example. J Theor Biol. 2012;295:194–203. doi: 10.1016/j.jtbi.2011.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gust DA, Strine TW, Maurice E, et al. Underimmunization among children: effects of vaccine safety concerns on immunization status. Pediatrics. 2004;114:e16–22. doi: 10.1542/peds.114.1.e16. [DOI] [PubMed] [Google Scholar]
- 13.Sugerman DE, Barskey AE, Delea MG, et al. Measles outbreak in a highly vaccinated population, San Diego, 2008: role of the intentionally undervaccinated. Pediatrics. 2010;125:747–55. doi: 10.1542/peds.2009-1653. [DOI] [PubMed] [Google Scholar]
- 14.Gangarosa EJ, Galazka AM, Wolfe CR, et al. Impact of anti-vaccine movements on pertussis control: the untold story. Lancet. 1998;351:356–61. doi: 10.1016/s0140-6736(97)04334-1. [DOI] [PubMed] [Google Scholar]
- 15.Kata A. Anti-vaccine activists, Web 2.0, and the postmodern paradigm–an overview of tactics and tropes used online by the anti-vaccination movement. Vaccine. 2012;30:3778–89. doi: 10.1016/j.vaccine.2011.11.112. [DOI] [PubMed] [Google Scholar]
- 16.Stokley S, Cohn A, Dorell C, et al. Adolescent vaccination-coverage levels in the United States: 2006–2009. Pediatrics. 2011;128:1078–86. doi: 10.1542/peds.2011-1048. [DOI] [PubMed] [Google Scholar]
- 17.Grenfell BT, Bjornstad ON, Kappey J. Travelling waves and spatial hierarchies in measles epidemics. Nature. 2001;414:716–23. doi: 10.1038/414716a. [DOI] [PubMed] [Google Scholar]
- 18.Rohani P, Earn DJ, Grenfell BT. Opposite patterns of synchrony in sympatric disease metapopulations. Science. 1999;286:968–71. doi: 10.1126/science.286.5441.968. [DOI] [PubMed] [Google Scholar]
- 19.Cummings DA, Iamsirithaworn S, Lessler JT, et al. The impact of the demographic transition on dengue in Thailand: insights from a statistical analysis and mathematical modeling. PLoS Med. 2009;6:e1000139. doi: 10.1371/journal.pmed.1000139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cummings DA, Irizarry RA, Huang NE, et al. Travelling waves in the occurrence of dengue haemorrhagic fever in Thailand. Nature. 2004;427:344–7. doi: 10.1038/nature02225. [DOI] [PubMed] [Google Scholar]
- 21.Hathi Trust Digital Library. Morbidity and Mortality Weekly Report : MMWR / Center for Disease Control. [Website online] [cited 2012 March 22]; Available from: http://catalog.hathitrust.org/Record/003910026.
- 22.Hathi Trust Digital Library. Morbidity and mortality / Federal Security Agency, Public Health Service, National Office of Vital Statistics. [Website online] 2009 [cited 2009; Available from: http://catalog.hathitrust.org/Record/003843660.
- 23.National Center for Biotechnology Information. Public Health Reports. [Website online] 2012 [cited 2012 March 1]; Available from: http://www.ncbi.nlm.nih.gov/pmc/journals/333/
- 24.Centers for Disease Control and Prevention. Morbidity and Mortality Weekly Report (MMWR). [Website online] 2009 [cited 2009; Available from: http://www.cdc.gov/mmwr/mmwr_wk/wk_pvol.html.
- 25.Ferguson K. Tycho and Kepler: The Unlikely Partnership That Forever Changed Our Understanding of the Heavens. New York: Walker and Company; 2002. [Google Scholar]
- 26.About Anti-Vaccination. Cal State J Med. 1909;7:157–8. [PMC free article] [PubMed] [Google Scholar]
- 27.Omer SB, Pan WK, Halsey NA, et al. Nonmedical exemptions to school immunization requirements: secular trends and association of state policies with pertussis incidence. JAMA. 2006;296:1757–63. doi: 10.1001/jama.296.14.1757. [DOI] [PubMed] [Google Scholar]
- 28.Atkinson WL, Orenstein WA, Krugman S. The resurgence of measles in the United States, 1989–1990. Annu Rev Med. 1992;43:451–63. doi: 10.1146/annurev.me.43.020192.002315. [DOI] [PubMed] [Google Scholar]
- 29.The measles epidemic. The problems, barriers, and recommendations. The National Vaccine Advisory Committee. JAMA. 1991;266:1547–52. [PubMed] [Google Scholar]
- 30.Hinman AR, Orenstein WA, Schuchat A. Vaccine-preventable diseases, immunizations, and the Epidemic Intelligence Service. Am J Epidemiol. 2011;174:S16–22. doi: 10.1093/aje/kwr306. [DOI] [PubMed] [Google Scholar]
- 31.Farizo KM, Cochi SL, Zell ER, Brink EW, Wassilak SG, Patriarca PA. Epidemiological features of pertussis in the United States, 1980–1989. Clin Infect Dis. 1992;14:708–19. doi: 10.1093/clinids/14.3.708. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Tycho supplement