The SEARCH for Diabetes in Youth Study: Rationale, Findings, and Future Directions (original) (raw)
Abstract
The SEARCH for Diabetes in Youth (SEARCH) study was initiated in 2000, with funding from the Centers for Disease Control and Prevention and support from the National Institute of Diabetes and Digestive and Kidney Diseases, to address major knowledge gaps in the understanding of childhood diabetes. SEARCH is being conducted at five sites across the U.S. and represents the largest, most diverse study of diabetes among U.S. youth. An active registry of youth diagnosed with diabetes at age <20 years allows the assessment of prevalence (in 2001 and 2009), annual incidence (since 2002), and trends by age, race/ethnicity, sex, and diabetes type. Prevalence increased significantly from 2001 to 2009 for both type 1 and type 2 diabetes in most age, sex, and race/ethnic groups. SEARCH has also established a longitudinal cohort to assess the natural history and risk factors for acute and chronic diabetes-related complications as well as the quality of care and quality of life of persons with diabetes from diagnosis into young adulthood. Many youth with diabetes, particularly those from low-resourced racial/ethnic minority populations, are not meeting recommended guidelines for diabetes care. Markers of micro- and macrovascular complications are evident in youth with either diabetes type, highlighting the seriousness of diabetes in this contemporary cohort. This review summarizes the study methods, describes key registry and cohort findings and their clinical and public health implications, and discusses future directions.
Introduction
Significant gaps existed at the start of the 21st century in our understanding of diabetes in youth, including limited data on the burden of diabetes and trends in incidence and prevalence by type, age, sex, and race/ethnicity, the natural history and etiologic classification of childhood diabetes, the burden and risk factors for diabetes-related early complications, and the quality of health care and quality of life of youth with diabetes. The SEARCH for Diabetes in Youth (SEARCH) study was initiated in 2000 with funding from the Division of Diabetes Translation of the Centers for Disease Control and Prevention and the National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health to address these gaps and respond to emerging issues in the field of childhood diabetes. SEARCH has brought together multiple facets of childhood diabetes research: an active epidemiologic surveillance component to assess trends in incidence, prevalence, and clinical course and a health services research component to evaluate the processes and quality of care using both clinical and public health perspectives. We provide a description of the methods used and an overview of major findings to date as well as future questions and challenges to be addressed to develop a more complete picture of diabetes in youth.
Design of Search
Recruitment
Phase 1 (2000–2005) (1) and 2 (2005–2010) included six recruitment centers, four geographic-based sites based in Ohio (eight counties including Cincinnati, OH); the entire state of Colorado; five counties around Seattle, Washington; the entire state of South Carolina; two health plan–based sites in Hawaii and California (health plan enrollees in one plan from seven counties); and under the direction of Colorado, American Indian reservation-based populations in Arizona and New Mexico. Each site identified prevalent (in 2001 and 2009) and incident cases (ongoing since 2002) of diagnosed diabetes (excluding gestational diabetes) in youth <20 years of age. Phase 3 began in 2010 and continues to the present with five of the six original centers (excluding Hawaii).
Study Components
SEARCH includes a registry and a cohort study (Fig. 1). The registry study identifies incident cases each year since 2002 through the present with ∼5.5 million children <20 years of age (∼6% of the U.S. population <20 years) under surveillance annually. Approximately 3.5 million children <20 years of age were under surveillance in 2001 at the six SEARCH recruitment centers, with approximately the same number at the five centers under surveillance in 2009. Denominators representing the population at risk for the geographic-based sites use race-bridged postcensal estimates of the nonmilitary, noninstitutionalized midyear populations in the center catchment areas. The health plans use end-of-year membership rolls, and Indian Health Service beneficiary rolls provide American Indian site denominators. Compared with U.S. Census data, the SEARCH surveillance population is similar to the U.S. youth population with respect to race/ethnicity, age, household income, and parental education (2).
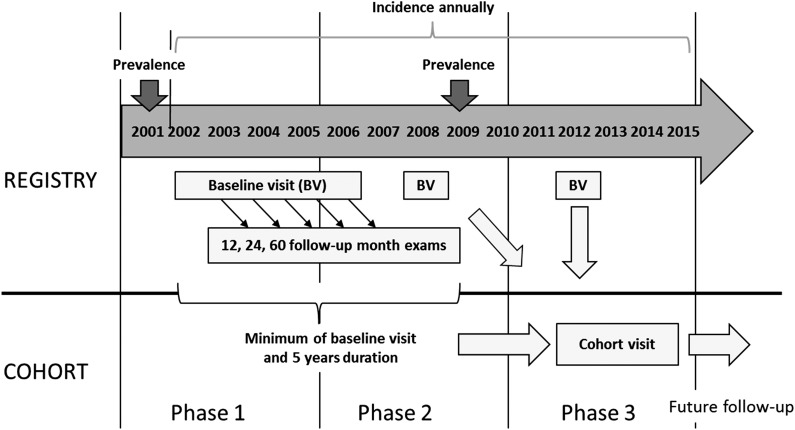
Figure 1.
Summary of the SEARCH study design. The registry began in 2001 measuring prevalence, which was repeated in 2009. Incidence has been measured annually starting in 2002. Youth diagnosed in 2002–2006, 2008, and 2012 had a baseline in-person visit for measurement of diabetes autoantibodies, albuminuria, BMI, cardiovascular risk factors, and sociodemographic, quality of care, and quality of life questionnaires. Youth with baseline visits (incident cases in 2002–2005) were invited to return in 12, 24, and 60 months after their baseline visit for additional visits. Those with a baseline visit and at least 5 years of duration were asked to join the cohort study, started in 2012, which added measures of early complications (retinopathy, cardiac autonomic and peripheral neuropathy, and arterial stiffness). Future follow-up of the cohort is planned.
Centers conduct active surveillance under Health Insurance Portability and Accountability Act waivers of consent using networks of endocrinologists (pediatric and adult), as well other health care providers, hospitals, community health centers, clinical and administrative data systems, and electronic medical records. Cases are determined to be valid (diabetes is confirmed in the medical record or by the referring physician), eligible (based on age, residence, nonmilitary, noninstitutionalized, and health plan membership at diagnosis [health plan sites]), and unique (duplicates are removed) locally and are then registered anonymously with the Coordinating Center at Wake Forest University. A high degree of case ascertainment (generally >90%), for both type 1 and type 2 diabetes has been obtained, estimated using capture-recapture methods (2–4).
The cohort study was developed by recruiting incident cases in 2002–2006, 2008, and 2012 that had a baseline visit near diagnosis and at least 5 years of diabetes duration at the cohort visit assessment (Fig. 1). The cohort study will allow estimates of the prevalence and incidence of acute and chronic complications as well as the degree to which processes of care impact glycemia, blood pressure, and lipid control and diabetes-related outcomes. A biospecimen repository has also been developed and is available for the conduct of ancillary studies.
Study Findings
Diabetes Is Frequent Among U.S. Youth, and Both Type 1 and Type 2 Diabetes Are Increasing in Most Racial/Ethnic Populations and Sex and Age Groups
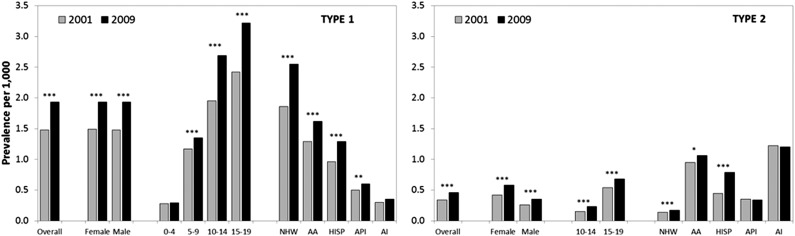
The prevalence of all types of diabetes was 1.8/1,000 youth in 2001 and was 2.2/1,000 youth in 2009, which translated to at least 154,000 children/youth in the U.S. with diabetes in 2001 (5) and at least 192,000 in 2009 (6). Overall, between 2001 and 2009, prevalence of type 1 diabetes in youth increased by 21.1% (95% CI 15.6–27.0), with similar increases for boys and girls and in most racial/ethnic and age groups (2) (Fig. 2). The prevalence of type 2 diabetes also increased significantly over the same time period by 30.5% (95% CI 17.3–45.1), with increases observed in both sexes, 10–14- and 15–19-year-olds, and among Hispanic and non-Hispanic white and African American youth (2). These data on changes in type 2 are consistent with smaller U.S. studies (7–11).
Figure 2.
Prevalence (per 1,000) of diabetes by type, sex, age group, and race/ethnic group in 2001 and 2009 (2). P values for change between years: *P < 0.05; **P < 0.01; ***P < 0.001. AA, African American; AI, American Indian; API, Asian Pacific Islander; HISP, Hispanic; NHW, non-Hispanic white.
The incidence of diabetes (per 100,000/year) in 2002 to 2003 was 24.6/100,000/year (12), representing ∼15,000 new patients every year with type 1 diabetes and 3,700 with type 2 diabetes, increasing to 18,436 newly diagnosed type 1 and 5,089 with type 2 diabetes in 2008 to 2009 (13). Among non-Hispanic white youth, the incidence of type 1 diabetes increased by 2.7% (95% CI 1.2–4.3) annually between 2002 and 2009. Significant increases were observed among all age groups except the youngest age group (0–4 years) (14). These increases for non-Hispanic whites are consistent with data worldwide (15,16), with the highest increase in the 0–4-year age group (5.4% per year) (17), something not seen in SEARCH results. The underlying factors responsible for this increase have not yet been identified. Potential trends in incidence of type 1 and type 2 diabetes among other racial/ethnic groups are currently being explored.
Diabetes presents a significant burden to the health of U.S. youth and represents a major clinical and public health challenge, especially with increasing burden of both types of diabetes in minority youth and unique challenges in proper diagnosis and management (18), given excess obesity in minorities.
Many Youth With Diabetes, Particularly Those of Racial and Ethnic Minority Groups, Are at Risk for Acute and Chronic Complications
Over 50% of youth are hospitalized at diabetes onset, and ∼30% of children newly diagnosed with diabetes present with diabetic ketoacidosis (DKA) (19). Prevalence of DKA at diagnosis was three times higher among youth with type 1 diabetes (29.4%) compared with youth with type 2 diabetes (9.7%) and was lowest in Asian/Pacific Islanders (16.2%) and highest among Hispanics (27.0%).
A substantial proportion of youth with diabetes, particularly African American and American Indian youth and especially youth with type 2 diabetes, come from low-resourced homes (60–70%) (20–24). Overweight [85–94% of U.S. BMI distribution (25)] and obesity (≥95% of the U.S. BMI distribution) are common among youth with type 2 diabetes regardless of race/ethnicity (80–90%). However, a surprisingly large proportion of youth with type 1 diabetes (35–50%) were also overweight or obese across all racial/ethnic groups (20–24). This high rate of overweight/obesity is at least partly due to low rates of physical activity (26) and low consumption of fruits and vegetables (27).
A significant proportion of youth with diabetes, particularly those with type 2 diabetes, have very poor glycemic control (Table 1) (28): 17% of youth with type 1 diabetes and 27% of youth with type 2 diabetes had A1C levels ≥9.5% (≥80 mmol/mol). Minority youth were significantly more likely to have higher A1C levels compared with non-Hispanic white youth, regardless of diabetes type. Table 1 also shows that cardiovascular disease risk factors were also elevated, including high blood pressure and dyslipidemia (29–31), elevated apolipoprotein B (apoB) levels and small, dense LDL particles (32). Early signs of kidney disease (33), retinopathy (34), neuropathy (35,36), as well as increased arterial stiffness (37–39) were also identified. This was especially true for youth with type 2 diabetes and for racial and ethnic minority youth with type 1 diabetes. Youth with worse glycemic control had poorer levels of each of these outcomes. These data stress the need to enhance screening efforts for risk factors and preclinical disease in these high-risk populations to delay the long-term impact of these complications.
Table 1.
Prevalence of elevated glycemia, CVD risk factors, and early complications, SEARCH 2006–2013
| Type 1 | P value | Type 2 | P value | |
|---|---|---|---|---|
| Glycemia (28) | N = 3,947 | N = 552 | ||
| A1C ≥9.5% (≥80 mmol/mol), all races (%) | 16.8 | 26.6 | ||
| Non-Hispanic white | 12.3 | <0.0001* | 12.2 | <0.0001* |
| African American | 35.5 | 22.3 | ||
| Hispanic | 27.3 | 27.4 | ||
| Asian Pacific Islander | 26.0 | 36.4 | ||
| American Indian | 52.2 | 43.8 | ||
| CVD risk factors†, age 10–19 years (30) | N = 1,376 | N = 63 | ||
| Hypertension (%) | 22.0 | 73.0 | ||
| Elevated triglycerides (%) | 14.0 | 65.0 | ||
| Decreased HDL (%) | 9.0 | 60.0 | ||
| Increased waist circumference (%) | 15.0 | 95.0 | ||
| N = 2,657 | N = 345 | |||
| Elevated apoB (%) (32) | 10.6 | 36.3 | <0.0001‡ | |
| Dense LDL (%) (32) | 7.9 | 36.3 | ||
| Retinopathy (34) | N = 222 | N = 43 | ||
| Any (%) | 17.0 | 42.0 | 0.40‡ | |
| Mild/moderate/proliferative (%) | 2.7 | 16.3 | ||
| Nephropathy (33) | N = 2,885 | N = 374 | ||
| Elevated ACR ≥30 μg/mg (%) | 9.2 | 22.2 | <0.0001‡ | |
| Neuropathy | N = 329 | N = 70 | ||
| Peripheral neuropathy MNSE >2 (%) (35) | 8.2 | 25.7 | <0.0001‡ | |
| Heart rate variability (%) (36) | −11.6 | 0.003†† | ||
| Arterial stiffness (37) | N = 535 | N = 60 | ||
| Pulse wave velocity (m/sec) | 5.3 | 6.4 | <0.01‡ | |
| BrachD (%/mmHg) | 6.1 | 5.2 | <0.01‡ |
While Many Youth With Diabetes Are Receiving Quality Care, a Significant Proportion of Youth Who Are Racial/Ethnic Minorities and “Emerging Adults” Are Not
Optimal care is an important component of successful long-term management for youth with diabetes. While there are high levels of adherence for some diabetes care indicators such as blood pressure checks (95%), urinary protein tests (83%), and lipid assessments (88%), approximately one-third of youth had no documentation of eye or A1C values at appropriate intervals and therefore were not meeting the American Diabetes Association (ADA)-recommended screening for diabetic control and complications (40). Participants ≥18 years old, particularly those with type 2 diabetes, and minority youth with type 1 diabetes had fewer tests of all kinds performed. Challenges in the transition from pediatric to adult care were also observed. There was a ∼2.5 times greater odds of poor glycemic control among youth with type 1 transitioning to adult care compared with those who remained in pediatric care, suggesting that this period requires a high level of support to ensure success (41). Importantly, using basal-bolus therapies and higher frequency of glucose monitoring were associated with lower A1C in youth with type 1 diabetes (42).
These data highlight the challenges associated with achieving recommended goals for appropriate diabetes management in youth and indicate that some subgroups are particularly vulnerable.
A Simple Etiologic Classification of Diabetes Type Is Possible for Youth-Onset Diabetes
Because recognition of the broader spectrum of diabetes in children and adolescents is recent, there are no gold-standard definitions for differentiating the types of diabetes in this population, either for research or clinical purposes or for public health surveillance. The ADA classification of diabetes as type 1 and type 2 does not include operational definitions for the specific etiologic markers of diabetes type, such as types and numbers of diabetes autoantibodies or measures of insulin resistance, hallmarks of type 1 and 2 diabetes, respectively (43). Moreover, obese adolescents with a clinical phenotype suggestive of type 2 diabetes can present with ketoacidosis (44) or have evidence of autoimmunity (45).
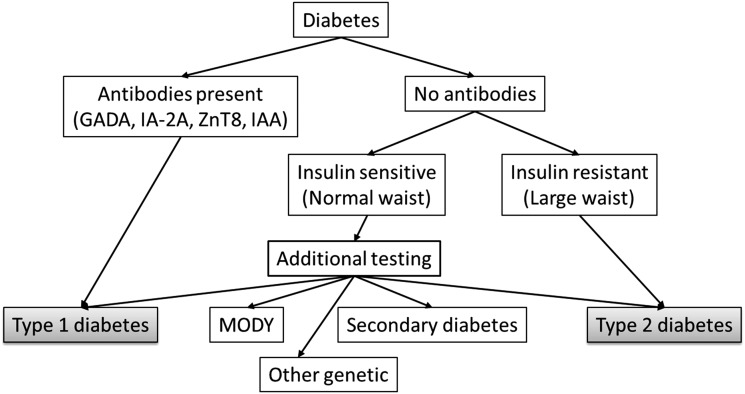
Using the ADA framework (43), we operationalized definitions of two main etiologic markers, autoimmunity and insulin sensitivity, to identify four etiologic subgroups based on the presence or absence of markers. Autoimmunity was based on presence of one or more diabetes autoantibodies (GAD65 and IA2). Insulin sensitivity was estimated using clinical variables (A1C, triglyceride level, and waist circumference) from a formula that was highly associated with estimated insulin sensitivity measured using a euglycemic-hyperinsulinemic clamp among youth with type 1 and 2 and normal control subjects (46). Participants were categorized as insulin resistant (estimated insulin sensitivity <8.15, representing the lowest 25th percentile among National Health and Nutrition Examination Survey youth) and insulin sensitive (47). Using this approach, 54.5% of SEARCH cases were classified as typical type 1 (autoimmune, insulin-sensitive) diabetes, while 15.9% were classified as typical type 2 (nonautoimmune, insulin-resistant) diabetes. Cases that were classified as autoimmune and insulin-resistant likely represent individuals with type 1 autoimmune diabetes and concomitant obesity, a phenotype becoming more prevalent as a result of the recent increase in the frequency of obesity, but is unlikely to be a distinct etiologic entity. This is supported by the following: 1) the phenotype represented ∼26% of all autoimmune cases, a proportion similar to that expected, given that the definition of insulin resistance was based on the lowest 25th percentile for the National Health and Nutrition Examination Survey, and 2) there was a similar prevalence and titers of diabetes autoantibodies and similar distribution of HLA DR-DQ risk genotypes to those observed in the typical type 1 case (autoimmune and insulin sensitive), suggesting a similar contribution of immune-mediated disease processes (47).
Ten percent of SEARCH participants had no evidence of either autoimmunity or insulin resistance and thus require additional testing, including additional measurements of diabetes-related autoantibodies (only two antibodies were measured in SEARCH) as well as testing for monogenic forms of diabetes to clarify etiology. Among antibody-negative youth, 8% of those tested had a mutation in one or more of the hepatocyte nuclear factor-1α (HNF-1α), glucokinase, and HNF-4α genes, an estimated monogenic diabetes population prevalence of at least 1.2% (48).
These findings allowed us to propose a straightforward clinical classification scheme (Fig. 3) without a requirement for a new etiologic category (i.e., type 1.5 or double diabetes). With some additional clinical data collection (especially antibodies and waist circumference), the vast majority of cases can be readily classified.
Figure 3.
Proposed algorithm for classification of pediatric diabetes. Presence of any antibodies indicates type 1 diabetes. Absence of antibodies and a large waist [or insulin sensitivity score <8.15 units (47)] indicates type 2 diabetes. Individuals with no antibodies and a normal waist (or insulin sensitivity score ≥8.15 units) require additional testing for potential monogenic forms of diabetes or other defects. GADA, GAD antibody; IAA, insulin autoantibody; MODY, maturity-onset diabetes of the young.
A summary of major topics and references from SEARCH and the ancillary studies is shown in Table 2.
Table 2.
Major topics and papers from the SEARCH study and ancillary studies*
| Burden of diabetes (prevalence/1,000) |
|---|
| 2001 (5); 2009 (6); changes in prevalence 2001–2009 (2); projections of diabetes burden to 2050 (50) |
| Risk of diabetes (incidence/100,000) |
| 2002 to 2003 (12); 2008 to 2009 (13); trends in incidence, non-Hispanic whites (2002–2009) (14) |
| Race/ethnicity–specific characteristics |
| Navajo (21); Asian, Pacific Islander (23); Hispanic (22); African American (24); non-Hispanic white (20) |
| Adiposity |
| Prevalence of overweight and obesity (25) |
| Weight-loss practices and weight-related issues (58) |
| Clinical, biochemical, and genetic findings |
| Glycemic control |
| Lipids and glycemic control (59) |
| Glycemic control and change in lipids (61) |
| Psychosocial burden and glycemic control (63) |
| HLA and genetics |
| HLA-associated phenotypes (60) |
| Time trends in HLA susceptibility among type 1 in Colorado (62) |
| Prevalence of MODY due to HNF1A, HNF4A, glucokinase (48), JDRF Monogenic Study* |
| Prevalence of permanent neonatal diabetes (64), JDRF Monogenic Study* |
| TCF7L2 and type 2 in multiethnic youth (66) |
| β-Cell function |
| Preservation of β-cell function in autoantibody positive youth (65) |
| Evolution of β-cell function (67) |
| Testing the accelerator hypothesis: body size, β-cell function, age at onset among type 1 (68) |
| Type of diabetes |
| Development of an insulin sensitivity score (46) |
| Etiologic approach to characterization of diabetes type (47) |
| CVD risk factors |
| CVD risk factor clustering (69) |
| Prevalence of elevated apoB and small, dense LDL (32) |
| Lipids among type 1 and control subjects (71), SEARCH CC* |
| CVD risk factors among type 2 and controls (73), SEARCH CC* |
| Prevalence of tobacco use and CVD risk factors (75) |
| Developmental origins |
| Maternal diabetes in utero and age at diagnosis among type 2 (70) |
| Maternal obesity and diabetes in utero and type 2 (72), SEARCH CC* |
| Breast-feeding and type 2 in three ethnic groups (74), SEARCH CC* |
| Behavioral factors |
| Physical activity and self-concept (76), SEARCH CC* |
| Physical activity and electronic media use (26), SEARCH CC* |
| TV and computer use (79) |
| Cardiovascular health among type 1 (81), SEARCH CVD* |
| Nutrition |
| Dietary intake (27) |
| Correlates of dietary intake (77) |
| DASH diet and CVD risk factors (78) |
| Change in DASH diet and CVD risk factors (80) |
| Sugar sweetened beverages and CVD risk profile (82) |
| DASH diet and hypertension (83) |
| Vitamin D insufficiency prevalence and association with insulin resistance (85), SNAS* |
| Nutritional factors and preservation of C-peptide among type 1 (87), SNAS* |
| Fructose intake and CVD risk factors among type 1 (89), SNAS* |
| Dietary intake patterns and arterial stiffness (91), SNAS* and CVD* |
| Quality of life |
| Health-related quality of life (84) |
| Demographic and clinical correlates of quality of life among type 1 (86) |
| Longitudinal associations among sex, self-care, and quality of life (88) |
| Prevalence and correlates of depressed mood (90) |
| Metabolic and inflammatory links with depression (92) |
| Acute complications |
| Prevalence of DKA at onset (19) |
| Trends in DKA at onset (44) |
| Risk factors and early complications |
| Carotid structure and function among type 1 (39), SEARCH CVD* |
| CVD risk factors associated with increased arterial stiffness among type 1 (93), SEARCH CVD* |
| Smoking and arterial stiffness among type 1 (95), SEARCH CVD* |
| Reduced HRV in type 1 and control subjects (36), SEARCH CVD* |
| Glycemic control and HRV (94), SEARCH CVD* |
| Reduced HRV is associated with increased arterial stiffness among type 1 (96), SEARCH CVD* |
| Quality of care |
| Barriers to care among type 1 (97) |
| Treatment patterns among type 2 (99) |
| Transition from childhood to adult care among type 1 (41) |
| Insulin regimens and clinical outcomes (42) |
| Predictors of insulin regimens among type 1 (102) |
| Spatial epidemiology and built environment |
| Neighborhood level risk factors among type 1 (98), SPATIAL* |
| Geographic variation in type 1 and 2 in four U.S. regions (100) |
| Surveillance |
| Ascertainment of diabetes using EHRs (54,101) |
| Adherence to treatment guidelines (40) |
Future Challenges and Opportunities
SEARCH has begun to clarify gaps in the understanding of diabetes among youth but challenges remain. Type 1 diabetes is not uncommon among minority youth as previously assumed, and type 2 diabetes is diagnosed among youth from all racial/ethnic groups. Both type 1 and type 2 diabetes are increasing over time, signaling a major challenge for the provision of health care resources. While recent evidence suggests that obesity rates may be plateauing among youth (49), this will at best result in a future plateauing of the rates of type 2 diabetes in this population, though not necessarily disease burden. A recent analysis suggests that given current population projections and observed trends, the number of youth with type 1 diabetes will nearly triple and type 2 diabetes prevalence will quadruple by 2050 (50).
Continued surveillance is needed to answer important questions:
- Will type 1 diabetes incidence continue to rise across all race and ethnicity groups in the U.S., or will there be a leveling off, as recently reported in Scandinavia (51–53)?
- Will type 2 diabetes incidence rise across all race and ethnicity groups in the U.S., or will there be a plateauing as obesity rates plateau?
Challenges to “sustainable” surveillance (e.g., relatively inexpensive, rapid, and more geographically diverse) must be faced. There is frequent movement of youth with diabetes between health care providers and systems over short time spans, making ascertainment, especially of type 2 diabetes, surprisingly difficult. While implementation of electronic health record (EHR) systems is rapidly occurring, the harmonization of multiple data systems and the identification of crucial information (e.g., date of diagnosis and type of diabetes) remain difficult (54). Absence of testing for diabetic antibodies and measurement of waist circumference are also common and limit the use of existing records. The increasing use of EHRs may permit easier surveillance, but substantial work remains to realize significant efficiencies.
The SEARCH cohort study was designed to explore the clinical evolution of diabetes and its complications on a sample of youth with type 1 and type 2 diabetes in contemporary care. Despite current treatment options, the prevalence of poor glycemic control is high, particularly among minority youth. Our initial findings suggest that a substantial number of youth with diabetes will develop serious, debilitating complications early in life, which is likely to have significant implications for their quality of life, as well as economic and health care implications. An especially high burden was noted among youth with type 2 diabetes, consistent with data from the TODAY study (55–57), and youth of minority racial/ethnic groups. Therefore, important questions remain:
- Are diabetic complications more frequent in youth with type 2 than type 1 of similar race/ethnicity and diabetes duration? Are such complications more frequent in minority youth regardless of diabetes type?
- Are there differences in the onset, diabetes duration, and clustering of complications between type 1 and type 2 diabetes?
- Do known risk factors explain observed differences or must other factors be identified?
- Are the sequence and severity of diabetic complications similar in youth with type 1 and type 2 diabetes, or are different mechanisms involved?
- What will the impact be of the Affordable Care Act implementation on the care of youth and young adults with diabetes, particularly those with type 2 diabetes?
Conclusions
Our findings to date have contributed to a better understanding of the complex nature of diabetes in youth; however, the increasing trends in the burden of type 1 and type 2 diabetes suggest that there is a pressing need to continue high-level, comprehensive surveillance efforts. Given the evidence of early complications despite current therapeutic approaches, continuing long-term follow-up of youth with diabetes is necessary to expand our understanding of its natural history, so the most appropriate approaches to primary, secondary, and tertiary prevention of diabetes and its complications in youth can occur.
A listing of all SEARCH publications is available at www.searchfordiabetes.org. The Supplementary Data lists the SEARCH investigators and staff at each of the sites.
Supplementary Material
Supplementary Data
Article Information
Acknowledgments. The SEARCH study thanks the many youth, families, and health care providers whose participation made this study possible.
Funding. SEARCH is funded by the Centers for Disease Control and Prevention (PA numbers 00097, DP-05-069, and DP-10-001) and supported by the National Institute of Diabetes and Digestive and Kidney Diseases. Support was also provided by General Clinical Research Centers at the South Carolina Clinical & Translational Research Institute, at the Medical University of South Carolina (National Institutes of Health [NIH]/National Center for Research Resources grant UL1-RR-029882), Seattle Children’s Hospital (NIH Clinical and Translational Science Award grant UL1-TR-000423 of the University of Washington), University of Colorado Pediatric Clinical and Translational Research Center (grant UL1-TR-000154), the Barbara Davis Center at the University of Colorado at Denver (Diabetes Endocrinology Research Centers NIH P30-DK-057516), the National Center for Research Resources and the National Center for Advancing Translational Sciences, NIH, through grant 8-UL1-TR-000077, and the Children with Medical Handicaps program managed by the Ohio Department of Health. Site contract numbers are as follows: Kaiser Permanente Southern California (U48/CCU919219, U01-DP-000246, and U18-DP-002714), University of Colorado Denver (U48/CCU819241-3, U01-DP-000247, and U18-DP-000247-06A1), Kuakini Medical Center (U58CCU919256 and U01-DP-000245), Children’s Hospital Medical Center (Cincinnati) (U48/CCU519239, U01-DP-000248, and 1-U18-DP-002709), University of North Carolina at Chapel Hill (U48/CCU419249, U01-DP-000254, and U18-DP-002708), University of Washington School of Medicine (U58/CCU019235-4, U01-DP-000244, and U18-DP-002710-01), and Wake Forest University School of Medicine (U48/CCU919219, U01-DP-000250, and 200-2010-35171).
Duality of Interest. No potential conflicts of interest relevant to this article were reported.
Author Contributions. R.F.H., R.A.B., D.D., R.B.D., L.D., J.M.L., S.M.M., E.J.M.-D., C.P., and B.L.R. researched data, reviewed and edited the manuscript, and contributed to discussion. G.I., B.L., and S.S. reviewed and edited the manuscript and contributed to discussion.
Footnotes
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention and the National Institute of Diabetes and Digestive and Kidney Diseases.
References
- 1.SEARCH Study Group . SEARCH for Diabetes in Youth Study: a multicenter study of the prevalence, incidence and classification of diabetes mellitus in youth. Control Clin Trials 2004;25:458–471 [DOI] [PubMed] [Google Scholar]
- 2.Dabelea D, Mayer-Davis EJ, Saydah S, et al. SEARCH for Diabetes in Youth Study . Prevalence of type 1 and type 2 diabetes among children and adolescents from 2001 to 2009. JAMA 2014;311:1778–1786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hamman RF, Dabelea D, Liese AD, et al. Estimation of Completeness of Case Ascertainment Using Capture-Recapture (Technical Report) [internet], 2013. Available from https://www.searchfordiabetes.org/public/dspPubs.cfm. Accessed 2 July 2014
- 4.Verlato G, Muggeo M. Capture-recapture method in the epidemiology of type 2 diabetes: a contribution from the Verona Diabetes Study. Diabetes Care 2000;23:759–764 [DOI] [PubMed] [Google Scholar]
- 5.Liese AD, D’Agostino RB, Jr, Hamman RF, et al. SEARCH for Diabetes in Youth Study Group . The burden of diabetes mellitus among US youth: prevalence estimates from the SEARCH for Diabetes in Youth Study. Pediatrics 2006;118:1510–1518 [DOI] [PubMed] [Google Scholar]
- 6.Pettitt DJ, Talton J, Dabelea D, et al. SEARCH for Diabetes in Youth Study Group . Prevalence of diabetes in U.S. youth in 2009: the SEARCH for diabetes in youth study. Diabetes Care 2014;37:402–408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lipman TH, Ratcliffe SJ, Cooper R, Levitt Katz LE. Population-based survey of the prevalence of type 1 and type 2 diabetes in school children in Philadelphia. J Diabetes 2013;5:456–461 [DOI] [PubMed] [Google Scholar]
- 8.Pinhas-Hamiel O, Dolan LM, Daniels SR, Standiford D, Khoury PR, Zeitler P. Increased incidence of non-insulin-dependent diabetes mellitus among adolescents. J Pediatr 1996;128:608–615 [DOI] [PubMed] [Google Scholar]
- 9.Smith TL, Drum ML, Lipton RB. Incidence of childhood type I and non-type 1 diabetes mellitus in a diverse population: the Chicago Childhood Diabetes Registry, 1994 to 2003. J Pediatr Endocrinol Metab 2007;20:1093–1107 [DOI] [PubMed] [Google Scholar]
- 10.Dabelea D, Hanson RL, Bennett PH, Roumain J, Knowler WC, Pettitt DJ. Increasing prevalence of Type II diabetes in American Indian children. Diabetologia 1998;41:904–910 [DOI] [PubMed] [Google Scholar]
- 11.Lipman TH, Katz LL, Ratcliffe S, et al. Continued Marked Rise in the Incidence of Type 1 Diabetes in Young Children in Philadelphia. Diabetes 2014;63(Suppl. 1):A45 [Google Scholar]
- 12.Dabelea D, Bell RA, D’Agostino RB, Jr, et al. Writing Group for the SEARCH for Diabetes in Youth Study Group . Incidence of diabetes in youth in the United States. JAMA 2007;297:2716–2724 [DOI] [PubMed] [Google Scholar]
- 13.Lawrence JM, Imperatore G, Pettitt DJ, et al. SEARCH for Diabetes in Youth Study Group Incidence of diabetes in United States youth by diabetes type, race/ethnicity, and age, 2008-2009. Diabetes 2014;63(Suppl. 1):A407 [Google Scholar]
- 14.Lawrence JM, Imperatore G, Dabelea D, et al. SEARCH for Diabetes in Youth Study Group Trends in incidence of type 1 diabetes among non-Hispanic white youth in the U.S., 2002-2009. Diabetes 2014;63:3938–3945 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Karvonen M, Viik-Kajander M, Moltchanova E, Libman I, LaPorte R, Tuomilehto J. Incidence of childhood type 1 diabetes worldwide. Diabetes Mondiale (DiaMond) Project Group. Diabetes Care 2000;23:1516–1526 [DOI] [PubMed] [Google Scholar]
- 16.Patterson CC, Gyürüs E, Rosenbauer J, et al. Trends in childhood type 1 diabetes incidence in Europe during 1989-2008: evidence of non-uniformity over time in rates of increase. Diabetologia 2012;55:2142–2147 [DOI] [PubMed] [Google Scholar]
- 17.Patterson CC, Dahlquist GG, Gyürüs E, Green A, Soltész G, EURODIAB Study Group . Incidence trends for childhood type 1 diabetes in Europe during 1989-2003 and predicted new cases 2005-20: a multicentre prospective registration study. Lancet 2009;373:2027–2033 [DOI] [PubMed] [Google Scholar]
- 18.Klingensmith GJ, Pyle L, Arslanian S, et al. TODAY Study Group . The presence of GAD and IA-2 antibodies in youth with a type 2 diabetes phenotype: results from the TODAY study. Diabetes Care 2010;33:1970–1975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rewers A, Klingensmith G, Davis C, et al. Presence of diabetic ketoacidosis at diagnosis of diabetes mellitus in youth: the Search for Diabetes in Youth Study. Pediatrics 2008;121:e1258–e1266 [DOI] [PubMed] [Google Scholar]
- 20.Bell RA, Mayer-Davis EJ, Beyer JW, et al. SEARCH for Diabetes in Youth Study Group Diabetes in non-Hispanic white youth: prevalence, incidence, and clinical characteristics: the SEARCH for Diabetes in Youth Study. Diabetes Care 2009;32(Suppl. 2):S102–S111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dabelea D, DeGroat J, Sorrelman C, et al. Diabetes in Navajo youth: prevalence, incidence, and clinical characteristics: the SEARCH for Diabetes in Youth Study. Diabetes Care 2009;32(Suppl. 2):S141–S147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lawrence JM, Mayer-Davis EJ, Reynolds K, et al. Diabetes in Hispanic American youth: prevalence, incidence, demographics, and clinical characteristics: the SEARCH for Diabetes in Youth Study. Diabetes Care 2009;32(Suppl. 2):S123–S132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Liu LL, Yi JP, Beyer J, et al. Type 1 and Type 2 diabetes in Asian and Pacific Islander U.S. youth: the SEARCH for Diabetes in Youth Study. Diabetes Care 2009;32(Suppl. 2):S133–S140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mayer-Davis EJ, Beyer J, Bell RA, et al. SEARCH for Diabetes in Youth Study Group Diabetes in African American youth: prevalence, incidence, and clinical characteristics: the SEARCH for Diabetes in Youth Study. Diabetes Care 2009;32(Suppl. 2):S112–S122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Liu LL, Lawrence JM, Davis C, et al. SEARCH for Diabetes in Youth Study Group . Prevalence of overweight and obesity in youth with diabetes in USA: the SEARCH for Diabetes in Youth study. Pediatr Diabetes 2010;11:4–11 [DOI] [PubMed] [Google Scholar]
- 26.Lobelo F, Liese AD, Liu J, et al. Physical activity and electronic media use in the SEARCH for diabetes in youth case-control study. Pediatrics 2010;125:e1364–e1371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mayer-Davis EJ, Nichols M, Liese AD, et al. SEARCH for Diabetes in Youth Study Group . Dietary intake among youth with diabetes: the SEARCH for Diabetes in Youth Study. J Am Diet Assoc 2006;106:689–697 [DOI] [PubMed] [Google Scholar]
- 28.Petitti DB, Klingensmith GJ, Bell RA, et al. SEARCH for Diabetes in Youth Study Group . Glycemic control in youth with diabetes: the SEARCH for diabetes in Youth Study. J Pediatr 2009;155:668–672.e1-e3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kershnar AK, Daniels SR, Imperatore G, et al. Lipid abnormalities are prevalent in youth with type 1 and type 2 diabetes: the SEARCH for Diabetes in Youth Study. J Pediatr 2006;149:314–319 [DOI] [PubMed] [Google Scholar]
- 30.Rodriguez BL, Fujimoto WY, Mayer-Davis EJ, et al. Prevalence of cardiovascular disease risk factors in U.S. children and adolescents with diabetes: the SEARCH for diabetes in youth study. Diabetes Care 2006;29:1891–1896 [DOI] [PubMed] [Google Scholar]
- 31.Rodriguez BL, Dabelea D, Liese AD, et al. SEARCH Study Group . Prevalence and correlates of elevated blood pressure in youth with diabetes mellitus: the SEARCH for diabetes in youth study. J Pediatr 2010;157:245–251.e1 [DOI] [PubMed] [Google Scholar]
- 32.Albers JJ, Marcovina SM, Imperatore G, et al. Prevalence and determinants of elevated apolipoprotein B and dense low-density lipoprotein in youths with type 1 and type 2 diabetes. J Clin Endocrinol Metab 2008;93:735–742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Maahs DM, Snively BM, Bell RA, et al. Higher prevalence of elevated albumin excretion in youth with type 2 than type 1 diabetes: the SEARCH for Diabetes in Youth study. Diabetes Care 2007;30:2593–2598 [DOI] [PubMed] [Google Scholar]
- 34.Mayer-Davis EJ, Davis C, Saadine J, et al. SEARCH for Diabetes in Youth Study Group . Diabetic retinopathy in the SEARCH for Diabetes in Youth Cohort: a pilot study. Diabet Med 2012;29:1148–1152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jaiswal M, Lauer A, Martin CL, et al. SEARCH for Diabetes in Youth Study Group . Peripheral neuropathy in adolescents and young adults with type 1 and type 2 diabetes from the SEARCH for Diabetes in Youth follow-up cohort: a pilot study. Diabetes Care 2013;36:3903–3908 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jaiswal M, Urbina EM, Wadwa RP, et al. Reduced heart rate variability among youth with type 1 diabetes: the SEARCH CVD study. Diabetes Care 2013;36:157–162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wadwa RP, Urbina EM, Anderson AM, et al. SEARCH Study Group . Measures of arterial stiffness in youth with type 1 and type 2 diabetes: the SEARCH for diabetes in youth study. Diabetes Care 2010;33:881–886 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Urbina EM, Wadwa RP, Davis C, et al. Prevalence of increased arterial stiffness in children with type 1 diabetes mellitus differs by measurement site and sex: the SEARCH for Diabetes in Youth Study. J Pediatr 2010;156:731–737.e1 [DOI] [PubMed] [Google Scholar]
- 39.Urbina EM, Dabelea D, D’Agostino RB, Jr, et al. Effect of type 1 diabetes on carotid structure and function in adolescents and young adults: the SEARCH CVD study. Diabetes Care 2013;36:2597–2599 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Waitzfelder B, Pihoker C, Klingensmith G, et al. SEARCH for Diabetes in Youth Study Group . Adherence to guidelines for youths with diabetes mellitus. Pediatrics 2011;128:531–538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lotstein DS, Seid M, Klingensmith G, et al. SEARCH for Diabetes in Youth Study Group . Transition from pediatric to adult care for youth diagnosed with type 1 diabetes in adolescence. Pediatrics 2013;131:e1062–e1070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pihoker C, Badaru A, Anderson A, et al. SEARCH for Diabetes in Youth Study Group . Insulin regimens and clinical outcomes in a type 1 diabetes cohort: the SEARCH for Diabetes in Youth study. Diabetes Care 2013;36:27–33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.American Diabetes Association . Diagnosis and classification of diabetes mellitus. Diabetes Care 2014;37(Suppl. 1):S81–S90 [DOI] [PubMed] [Google Scholar]
- 44.Dabelea D, Rewers A, Stafford JM, et al. SEARCH for Diabetes in Youth Study Group . Trends in the prevalence of ketoacidosis at diabetes diagnosis: the SEARCH for diabetes in youth study. Pediatrics 2014;133:e938–e945 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hathout EH, Thomas W, El-Shahawy M, Nahab F, Mace JW. Diabetic autoimmune markers in children and adolescents with type 2 diabetes. Pediatrics 2001;107:E102. [DOI] [PubMed] [Google Scholar]
- 46.Dabelea D, D’Agostino RB, Jr, Mason CC, et al. Development, validation and use of an insulin sensitivity score in youths with diabetes: the SEARCH for Diabetes in Youth study. Diabetologia 2011;54:78–86 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Dabelea D, Pihoker C, Talton JW, et al. SEARCH for Diabetes in Youth Study . Etiological approach to characterization of diabetes type: the SEARCH for Diabetes in Youth Study. Diabetes Care 2011;34:1628–1633 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Pihoker C, Gilliam LK, Ellard S, et al. SEARCH for Diabetes in Youth Study Group . Prevalence, characteristics and clinical diagnosis of maturity onset diabetes of the young due to mutations in HNF1A, HNF4A, and glucokinase: results from the SEARCH for Diabetes in Youth. J Clin Endocrinol Metab 2013;98:4055–4062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA 2014;311:806–814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Imperatore G, Boyle JP, Thompson TJ, et al. SEARCH for Diabetes in Youth Study Group . Projections of type 1 and type 2 diabetes burden in the U.S. population aged <20 years through 2050: dynamic modeling of incidence, mortality, and population growth. Diabetes Care 2012;35:2515–2520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Berhan Y, Waernbaum I, Lind T, Möllsten A, Dahlquist G, Swedish Childhood Diabetes Study Group . Thirty years of prospective nationwide incidence of childhood type 1 diabetes: the accelerating increase by time tends to level off in Sweden. Diabetes 2011;60:577–581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Harjutsalo V, Sund R, Knip M, Groop PH. Incidence of type 1 diabetes in Finland. JAMA 2013;310:427–428 [DOI] [PubMed] [Google Scholar]
- 53.Skrivarhaug T, Stene LC, Drivvoll AK, Strøm H, Joner G, Norwegian Childhood Diabetes Study Group . Incidence of type 1 diabetes in Norway among children aged 0-14 years between 1989 and 2012: has the incidence stopped rising? Results from the Norwegian Childhood Diabetes Registry. Diabetologia 2014;57:57–62 [DOI] [PubMed] [Google Scholar]
- 54.Zhong VW, Pfaff ER, Beavers DP, et al. for the Search for Diabetes in Youth Study Group . Use of administrative and electronic health record data for development of automated algorithms for childhood diabetes case ascertainment and type classification: the SEARCH for Diabetes in Youth Study. Pediatr Diabetes 9 June 2014 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.TODAY Study Group . Rapid rise in hypertension and nephropathy in youth with type 2 diabetes: the TODAY clinical trial. Diabetes Care 2013;36:1735–1741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.TODAY Study Group . Lipid and inflammatory cardiovascular risk worsens over 3 years in youth with type 2 diabetes: the TODAY clinical trial. Diabetes Care 2013;36:1758–1764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.TODAY Study Group . Retinopathy in youth with type 2 diabetes participating in the TODAY clinical trial. Diabetes Care 2013;36:1772–1774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lawrence JM, Liese AD, Liu L, et al. Weight-loss practices and weight-related issues among youth with type 1 or type 2 diabetes. Diabetes Care 2008;31:2251–2257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Petitti DB, Imperatore G, Palla SL, et al. SEARCH for Diabetes in Youth Study Group . Serum lipids and glucose control: the SEARCH for Diabetes in Youth study. Arch Pediatr Adolesc Med 2007;161:159–165 [DOI] [PubMed] [Google Scholar]
- 60.Black MH, Lawrence JM, Pihoker C, et al. SEARCH for Diabetes in Youth Study Group . HLA-associated phenotypes in youth with autoimmune diabetes. Pediatr Diabetes 2013;14:121–128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Maahs DM, Dabelea D, D’Agostino RB, Jr, et al. SEARCH for Diabetes in Youth Study . Glucose control predicts 2-year change in lipid profile in youth with type 1 diabetes. J Pediatr 2013;162:101–107.e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Vehik K, Hamman RF, Lezotte D, et al. Trends in high-risk HLA susceptibility genes among Colorado youth with type 1 diabetes. Diabetes Care 2008;31:1392–1396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Hood KK, Beavers DP, Yi-Frazier J, et al. Psychosocial Burden and Glycemic Control During the First 6 Years of Diabetes: Results From the SEARCH for Diabetes in Youth Study. J Adolesc Health 9 May 2014 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kanakatti Shankar R, Pihoker C, Dolan LM, et al. SEARCH for Diabetes in Youth Study Group . Permanent neonatal diabetes mellitus: prevalence and genetic diagnosis in the SEARCH for Diabetes in Youth Study. Pediatr Diabetes 2013;14:174–180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Greenbaum CJ, Anderson AM, Dolan LM, et al. SEARCH Study Group . Preservation of beta-cell function in autoantibody-positive youth with diabetes. Diabetes Care 2009;32:1839–1844 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Dabelea D, Dolan LM, D’Agostino R, Jr, et al. Association testing of TCF7L2 polymorphisms with type 2 diabetes in multi-ethnic youth. Diabetologia 2011;54:535–539 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Dabelea D, Mayer-Davis EJ, Andrews JS, et al. Clinical evolution of beta cell function in youth with diabetes: the SEARCH for Diabetes in Youth study. Diabetologia 2012;55:3359–3368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Dabelea D, D’Agostino RB, Jr, Mayer-Davis EJ, et al. SEARCH for Diabetes in Youth Study Group . Testing the accelerator hypothesis: body size, β-cell function, and age at onset of type 1 (autoimmune) diabetes. Diabetes Care 2006;29:290–294 [DOI] [PubMed] [Google Scholar]
- 69.Mayer-Davis EJ, Ma B, Lawson A, et al. SEARCH for Diabetes in Youth Study Group . Cardiovascular disease risk factors in youth with type 1 and type 2 diabetes: implications of a factor analysis of clustering. Metab Syndr Relat Disord 2009;7:89–95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Pettitt DJ, Lawrence JM, Beyer J, et al. Association between maternal diabetes in utero and age at offspring’s diagnosis of type 2 diabetes. Diabetes Care 2008;31:2126–2130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Guy J, Ogden L, Wadwa RP, et al. Lipid and lipoprotein profiles in youth with and without type 1 diabetes: the SEARCH for Diabetes in Youth case-control study. Diabetes Care 2009;32:416–420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Dabelea D, Mayer-Davis EJ, Lamichhane AP, et al. Association of intrauterine exposure to maternal diabetes and obesity with type 2 diabetes in youth: the SEARCH Case-Control Study. Diabetes Care 2008;31:1422–1426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.West NA, Hamman RF, Mayer-Davis EJ, et al. Cardiovascular risk factors among youth with and without type 2 diabetes: differences and possible mechanisms. Diabetes Care 2009;32:175–180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Mayer-Davis EJ, Dabelea D, Lamichhane AP, et al. Breast-feeding and type 2 diabetes in the youth of three ethnic groups: the SEARCH for diabetes in youth case-control study. Diabetes Care 2008;31:470–475 [DOI] [PubMed] [Google Scholar]
- 75.Reynolds K, Liese AD, Anderson AM, et al. Prevalence of tobacco use and association between cardiometabolic risk factors and cigarette smoking in youth with type 1 or type 2 diabetes mellitus. J Pediatr 2011;158:594–601.e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.O’Neill JR, Liese AD, McKeown RE, et al. Physical activity and self-concept: the SEARCH for diabetes in youth case control study. Pediatr Exerc Sci 2012;24:577–588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Bortsov A, Liese AD, Bell RA, et al. Correlates of dietary intake in youth with diabetes: results from the SEARCH for diabetes in youth study. J Nutr Educ Behav 2011;43:123–129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Liese AD, Bortsov A, Günther AL, et al. Association of DASH diet with cardiovascular risk factors in youth with diabetes mellitus: the SEARCH for Diabetes in Youth study. Circulation 2011;123:1410–1417 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Li C, Beech B, Crume T, et al. Longitudinal association between television watching and computer use and risk markers in diabetes in the SEARCH for Diabetes in Youth Study. Pediatr Diabetes 12 July 2014 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Barnes TL, Crandell JL, Bell RA, Mayer-Davis EJ, Dabelea D, Liese AD. Change in DASH diet score and cardiovascular risk factors in youth with type 1 and type 2 diabetes mellitus: The SEARCH for Diabetes in Youth Study. Nutr Diabetes 2013;3:e91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Alman AC, Talton JW, Wadwa RP, et al. Cardiovascular health in adolescents with type 1 diabetes: The SEARCH CVD Study. Pediatr Diabetes 22 January 2014 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Bortsov AV, Liese AD, Bell RA, et al. Sugar-sweetened and diet beverage consumption is associated with cardiovascular risk factor profile in youth with type 1 diabetes. Acta Diabetol 2011;48:275–282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Günther AL, Liese AD, Bell RA, et al. Association between the dietary approaches to hypertension diet and hypertension in youth with diabetes mellitus. Hypertension 2009;53:6–12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Naughton MJ, Ruggiero AM, Lawrence JM, et al. SEARCH for Diabetes in Youth Study Group . Health-related quality of life of children and adolescents with type 1 or type 2 diabetes mellitus: SEARCH for Diabetes in Youth Study. Arch Pediatr Adolesc Med 2008;162:649–657 [DOI] [PubMed] [Google Scholar]
- 85.The NS, Crandell JL, Lawrence JM, et al. Vitamin D in youth with Type 1 diabetes: prevalence of insufficiency and association with insulin resistance in the SEARCH Nutrition Ancillary Study. Diabet Med 2013;30:1324–1332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Lawrence JM, Yi-Frazier JP, Black MH, et al. SEARCH for Diabetes in Youth Study Group . Demographic and clinical correlates of diabetes-related quality of life among youth with type 1 diabetes. J Pediatr 2012;161:201–207.e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Mayer-Davis EJ, Dabelea D, Crandell JL, et al. Nutritional factors and preservation of C-peptide in youth with recently diagnosed type 1 diabetes: SEARCH Nutrition Ancillary Study. Diabetes Care 2013;36:1842–1850 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Naughton MJ, Yi-Frazier JP, Morgan TM, et al. SEARCH for Diabetes in Youth Study Group . Longitudinal associations between sex, diabetes self-care, and health-related quality of life among youth with type 1 or type 2 diabetes mellitus. J Pediatr 2014;164:1376–1383.e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Couch SC, Crandell JL, Shah AS, et al. Fructose intake and cardiovascular risk factors in youth with type 1 diabetes: SEARCH for diabetes in youth study. Diabetes Res Clin Pract 2013;100:265–271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Lawrence JM, Standiford DA, Loots B, et al. SEARCH for Diabetes in Youth Study . Prevalence and correlates of depressed mood among youth with diabetes: the SEARCH for Diabetes in Youth study. Pediatrics 2006;117:1348–1358 [DOI] [PubMed] [Google Scholar]
- 91.Lamichhane AP, Liese AD, Urbina EM, et al. Associations of dietary intake patterns identified using reduced rank regression with markers of arterial stiffness among youth with type 1 diabetes. Eur J Clin Nutr 28 May 2014 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Hood KK, Lawrence JM, Anderson A, et al. SEARCH for Diabetes in Youth Study Group . Metabolic and inflammatory links to depression in youth with diabetes. Diabetes Care 2012;35:2443–2446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Dabelea D, Talton JW, D’Agostino R, Jr, et al. Cardiovascular risk factors are associated with increased arterial stiffness in youth with type 1 diabetes: the SEARCH CVD study. Diabetes Care 2013;36:3938–3943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Jaiswal M, Fingerlin TE, Urbina EM, et al. Impact of glycemic control on heart rate variability in youth with type 1 diabetes: the SEARCH CVD study. Diabetes Technol Ther 2013;15:977–983 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Shah AS, Dabelea D, Talton JW, et al. Smoking and arterial stiffness in youth with type 1 diabetes: The SEARCH Cardiovascular Disease Study. J Pediatr 2014;165:110–116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Jaiswal M, Urbina EM, Wadwa RP, et al. Reduced heart rate variability is associated with increased arterial stiffness in youth with type 1 diabetes: the SEARCH CVD study. Diabetes Care 2013;36:2351–2358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Valenzuela JM, Seid M, Waitzfelder B, et al. SEARCH for Diabetes in Youth Study Group . Prevalence of and disparities in barriers to care experienced by youth with type 1 diabetes. J Pediatr 2014;164:1369–1375.e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Liese AD, Puett RC, Lamichhane AP, et al. Neighborhood level risk factors for type 1 diabetes in youth: the SEARCH case-control study. Int J Health Geogr 2012;11:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Badaru A, Klingensmith GJ, Dabelea D, et al. Correlates of treatment patterns among youth with type 2 diabetes. Diabetes Care 2014;37:64–72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Liese AD, Lawson A, Song HR, et al. Evaluating geographic variation in type 1 and type 2 diabetes mellitus incidence in youth in four US regions. Health Place 2010;16:547–556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Lawrence JM, Black MH, Zhang JL, et al. Validation of pediatric diabetes case identification approaches for diagnosed cases by using information in the electronic health records of a large integrated managed health care organization. Am J Epidemiol 2014;179:27–38 [DOI] [PubMed] [Google Scholar]
- 102.Paris CA, Imperatore G, Klingensmith G, et al. Predictors of insulin regimens and impact on outcomes in youth with type 1 diabetes: the SEARCH for Diabetes in Youth study. J Pediatr 2009;155:183–189.e1 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Data