Clinical evidence of inflammation driving secondary brain injury: A systematic review (original) (raw)
. Author manuscript; available in PMC: 2015 Jan 16.
Published in final edited form as: J Trauma Acute Care Surg. 2015 Jan;78(1):184–191. doi: 10.1097/TA.0000000000000468
Abstract
Background
Despite advances in both prevention and treatment, traumatic brain injury (TBI) remains one of the most burdensome diseases; 2% of the US population currently lives with disabilities resulting from TBI. Recent advances in the understanding of inflammation and its impact on the pathophysiology of trauma have increased the interest in inflammation as a possible mediator in TBI outcome.
Objectives
The goal of this systematic review is to address the question: “What is the evidence in humans that inflammation is linked to secondary brain injury?” As the experimental evidence has been well described elsewhere, this review will focus on the clinical evidence for inflammation as a mechanism of secondary brain injury.
Data Sources
Medline database (1996-Week 1 June 2014), Pubmed and Google Scholar databases were queried for relevant studies.
Study Eligibility Criteria
Studies were eligible if participants were adults and/or children who sustained moderate or severe TBI in the acute phase of injury, published in English. Studies published in the last decade (since 2004) were preferentially included. Trials could be observational or interventional in nature.
Appraisal and Synthesis Methods
To address the quality of the studies retrieved, we applied the Grades of Recommendation, Assessment, Development, and Evaluation (GRADE) criteria to assess the limitations of the included studies.
Results
Trauma initiates local central nervous system as well as systemic immune activation. Numerous observational studies describe elevation of pro-inflammatory cytokines that are associated with important clinical variables including neurologic outcome and mortality. A small number of clinical trials have included immunomodulating strategies, but no intervention to date has proven effective in improving outcomes after TBI.
Limitations
Inclusion of studies not initially retrieved by the search terms may have biased our results. Additionally, some reports may have been inadvertently excluded due to use of non-search term key words. Conclusions and Implications of Key Findings Clinical evidence of inflammation causing secondary brain injury in humans is gaining momentum. While inflammation is certainly present, it is not clear from the literature at what juncture inflammation becomes maladaptive, promoting secondary injury rather than facilitating repairand identifying patients with maladaptive inflammation (neuro-inflammation, systemic, or both) after TBI remains elusive. Direct agonism/antagonism represents an exciting target for future study.
Level of Evidence
Systematic review, level III.
Background: Secondary Brain Injury—A Role for Inflammation?
Despite advances in both prevention and treatment, traumatic brain injury (TBI) remains one of the most burdensome diseases; 2% of the US population currently lives with disabilities resulting from TBI.1 Public attention to TBI has been heightened by the prevalence of brain injury in the military and professional sports. Thus, brain trauma remains a key public health issue in need of innovative therapies aimed at improving functional outcomes. Recent advances in the understanding of inflammation and its impact on the pathophysiology of trauma have increased the interest in inflammation as a possible mediator in TBI outcome.
After the initial trauma, a second phase of brain injury begins. Secondary brain injury results from a complex sequence of events that begins just after the initial insult and continues through the acute hospitalization. Mitigating secondary brain injury represents a key target in the fight to limit disability incurred from TBI. Secondary brain injury results from a diverse host of etiologies, including (but not limited to) edema, ischemia, excitotoxicity, and inflammation.2 Excitotoxicity occurs when a neuron is destructively stimulated with excess amounts of neurotransmitter, especially glutamate. In experimental conditions, inflammation is increasingly recognized to be an important source of secondary brain injury. In the clinical setting, however, inflammation's contribution to secondary TBI is less well established. Trauma, with or without TBI, results in a dysregulation of the immune system, predisposing patients to nosocomial infections and worse outcomes. Investigators are just beginning to appreciate immunologic dysfunction or dissonance as a source of worsening neurologic injury. Clinical evidence in humans has lagged behind the observations made in animal models. Advances in technology allow markers of inflammation such as cytokines and chemokines to be measured in the clinical setting, providing an emerging body of clinical research.
Objectives
The goal of this systematic review was to address the question, “What is the evidence in humans that inflammation is linked to secondary brain injury?” As the experimental evidence has been well described elsewhere,3 this systematic review will focus on the clinical evidence for inflammation as a mechanism of secondary brain injury. The review will unfold in three parts as follows: (1) pathophysiology of the injured brain, (2) observational associations between inflammation and secondary brain injury, and (3) clinical trials addressing, at least in part, inflammation as a mechanism of secondary injury. We adhered to the PRISMA criteria4 for the structure of this systematic review.
Data Sources and Study Eligibility Criteria
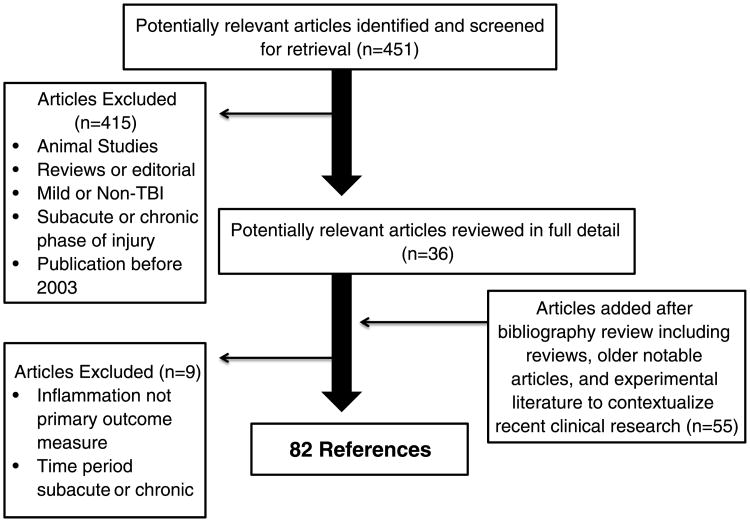
MEDLINE (1996 to Week 1 of June 2014), PubMed, and Google Scholar databases were queried for relevant studies in both adults and children sustaining moderate or severe TBI in the acute phase of injury, published in English, and with an emphasis on studies conducted in the last decade. All TBI moderate/severe subtypes (diffuse axonal injury, hemorrhagic contusion, etc.) were included. Patients with isolated TBI and patients with TBI and other injuries were included. Secondary brain injury was defined as any process that disturbs the metabolism of neurons, thus creating further injury and/or cell death. OVID search terms included (traumatic brain injury or brain injuries) AND (Inflammation Mediators/ or Inflammation/ or Neurogenic Inflammation/) AND (human). PubMed and Google Scholar database searches also included the terms secondary injury and cytokine. In addition, we inspected the reference lists of identified articles and included relevant articles for completeness. Search results are summarized in Figure 1.
Figure 1.
Search algorithm and results.
Study Appraisal and Synthesis Methods
To address the quality of the studies retrieved, we applied the Grades of Recommendation, Assessment, Development, and Evaluation (GRADE) criteria to assess the limitations of the included studies.5 We performed descriptive synthesis of results.
The studies included in the sections on “Observational Associations Between Immune Dysregulation and Secondary Brain Injury” and “The Injured Brain: Both an Immunologic Target and an Effector Organ” were observational in nature and largely uncontrolled, making comparison across studies challenging and contributing to a low grade of evidence (Grade 2C). The section on “Future Directions: Therapies and Trials” contains data from controlled clinical trials, which as a whole provides stronger levels of evidence, but few strong recommendations may be made. Each trial is assessed individually in the section on “Future Directions: Therapies and Trials.”
The Injured Brain: Both an Immunologic Target and an Effector Organ
In the brain, local and systemic inflammation work in concert to contribute to secondary brain injury, the cerebral analog to the systemic inflammatory response/compensatory anti-inflammatory response phenomenon described peripherally. The protection or “immunologic privilege” the brain usually enjoys is disrupted in moderate-to-severe TBI. In the absence of the relative fortification of the blood-brain barrier (BBB), a bidirectional flow of inflammatory mediators transits between the systemic circulation and the brain.6 The brain is both a target and an effector organ, as glial cells and neurons both produce immunologic mediators (i.e., complement, acute phase proteins, and cytokines) and exhibit receptors for these substances.7 This interchange produces local tissue damage and a systemic response.
BBB Breakdown
The initial moments after a traumatic injury can be categorized in two concurrent phases as follows: (1) metabolic crisis and (2) excitotoxicity. In response to direct tissue injury, the cerebral metabolism is deranged, leading to the accumulation of lactic acid due to anaerobic glycolysis, increased membrane permeability, and edema formation.8 Autoregulation of cerebral blood flow is impaired, promoting energy failure. In parallel, there is massive release of excitatory neurotransmitters, resulting in oxidative damage. The consequence of these processes is membrane degradation and BBB compromise.9 Membrane degradation fosters unregulated transit of immune molecules in and out of the injured brain. BBB breakdown is present even in diffuse injury.10
Local Inflammation
In response to the primary injury, the brain's support cells, the microglia, are activated,11 subsequently releasing a host of small signaling proteins. Those signaling proteins include cytokines (including chemokines12) and danger-associated molecular pattern (DAMP) molecules. Most of these factors are principally produced in the central nervous system by the microglia and have roles in inflammation and repair after injury.13,14 In addition, neurons themselves seem to synthesize chemokines.15 Cytokines signal peripheral immune cells to flow through the compromised BBB into the brain. The timing of up-regulation plays a critical role in the function of the various cytokines, dictating the direction of their actions. Damaged or dying cells may also release DAMPs, which activate the innate immune system, reinforcing cytokine production. DAMPs are a diverse group of molecules; examples include S100B16 and mitochondrial DNA.17 All of the signaling proteins may serve as biomarkers, alerting investigators to immune activation.
Observational Associations Between Immune Dysregulation and Secondary Brain Injury
Investigators and clinicians desire reliable biomarkers that reflect the immunologic status after acute TBI. Reliable biomarkers might empower clinicians to selectively administer personalized therapies, as it seems that single treatment ameliorates all secondary brain injury. The heterogeneity of injury after TBI is often cited as a reason that large-scale clinical trials have thus far failed to produce effective therapies. While intriguing, human data regarding inflammatory markers remain mixed and challenging to interpret. Table 1 summarizes the most frequently studied immune-modulating markers and the clinically relevant associations. Higher levels of proinflammatory markers are linked to poor outcome, although this has not been observed in every study. Some themes do emerge: proinflammatory cytokines interleukin 1β (IL-1β), IL-6, and IL-8 (considered as chemokine) as well as anti-inflammatory IL-10 shows linkage to important parameters after TBI, often worsened outcome. Elevation of certain markers may portend an improved prognosis, rather than a worsened one. For example, the expression of the chemokine fractalkine is associated with lower intracranial pressure (ICP) after TBI.18 A few noncytokine protein markers also relay information about inflammation after brain injury: glial fibrillary acidic protein (GFAP), SBDP145, and the so-called inflammasome, a protein complex whose activation leads to the downstream production of mature IL-1β and IL-18.
Table 1. Summary of the Most Investigated Immune-Modulating Biomarkers After Severe TBI.
| Mediator | Admission GCS Score | Increased ICP | Worse Outcome | Mortality |
|---|---|---|---|---|
| IL-1β | +19 | +39,57 | ||
| IL-1ra | −57 | |||
| IL-6 | +29 | +27,30 | +36 | |
| −31, 42,56 | ||||
| IL-8 | +21,22 | +23,24 | +25–28,26,41 | |
| IL-10 | +43 | +43 | +44,45 | |
| −46 | ||||
| TNF-α | +21,22 | +48, −21 | ||
| Other signalers, GFAP | +35 | +32–34 | +32–34 | |
| Inflammasome | +50 | |||
| Mitochondrial DNA | +51 |
An additional challenge is where to measure the marker (blood vs. cerebrospinal fluid [CSF] vs. extracellular fluid), as well as when after injury to measure. Most studies measure a single level within the first 72 hours or take the highest absolute value in the acute period. Different methods make comparing results between studies challenging. Finally, the complexity of the resultant data is not to be underestimated. Proteins interact with each other at each time point in this complex, dynamic system. One way to address the complexity is via statistical methods such as principal components analysis to account for covariance of markers.19
Peripheral Blood
As a result of the compromised BBB, investigators have measured centrally generated markers of inflammation in the peripheral blood. During the last decade, several studies associating elevated proinflammatory cytokines and markers of neurologic deterioration after TBI have been published—for example, increased ICP, decreased cerebral perfusion pressure, poor outcome in the form of a lower Glasgow Outcome Scores (GOSs), and mortality. At the same time, immunosuppressive cytokines are also up-regulated by activated T lymphocytes.20 Generally, proinflammatory markers seem to be associated with the severity of injury on admission and might predict future deterioration. Proinflammatory IL-1β levels within 6 hours of injury inversely correlate with admission Glasgow Coma Scale (GCS) score.21 The β-chemokine RANTES seems to track with radiographic head injury severity on computed tomographic scan.22 Serum IL-8 and Tumor necrosis factor α (TNF-α) have been associated with elevated ICP; specifically, higher levels seem to correlate with the “dose” (pressure × time) of ICP greater than 20 mm Hg.23 In a later work, the same investigators observed that these elevations preceded the events of intracranial hypertension and cerebral hypoperfusion, leading them to conclude that these inflammatory markers might be used to predict neurologic deterioration.24 However, there does not seem to be a direct link between serum TNF-α and outcome.23 Serum IL-8 at Day 1 after injury may be a good predictor of outcome when combined with postresuscitation GCS score.25 Likewise, IL-8 seems to be inversely associated with GOS when measured on Day 7 after injury.26 Several studies have found higher peripheral IL-8 levels in nonsurvivors versus survivors.27–30 The data are mixed with regard to IL-6, with some studies indicating that elevated levels are associated with elevated ICP31 and poor outcome,29,32 while others found no relationship with out-come.33 In severe TBI patients, serum GFAP levels seem to predict mortality and outcome.34–36 In mild and moderate TBI, GFAP-BDPs correlate with injury severity as gauged by GCS and associate with injury burden seen on head computed to-mographic scan.37 One possible explanation for the link between elevated proinflammatory cytokines and poor outcome might be as association with multiorgan failure. A large, prospective observational study of polytrauma with or without TBI found a multiphasic peak in IL-6 and IL-8 with late multiorgan failure and mortality.38 Another possibility is that inflammation induces worsening coagulopathy, as rising IL-6 covaries with coagulation abnormalities after TBI, although causality must still be proven.39
Cerebrospinal Fluid
CSF is usually obtained from a ventricular drain, although a few studies have relied on lumbar puncture. The patterns of markers of inflammation observed in the peripheral blood tend to be echoed in CSF, but these levels are orders of magnitude more pronounced, although the expression in CSF may lag behind plasma expression.40 For example, in one study, the authors compared levels of IL-6 and IL-1 in serum and CSF, finding that levels of each were twice as high in the CSF compared with blood levels.41 IL-10 also seems to follow this pattern in patients after TBI.42 Observations such as these have led investigators to believe that the higher levels of these markers in the CSF represent intrathecal production. Indeed, in postmortem samples, brain tissue samples after acute, severe TBI IL-6, IL-8, TNF-α, and IL-1β and their mRNA levels are all significantly increased following injury, further supporting the notion of synthesis in the central nervous system.13 IL-8 in the CSF has also been linked with mortality in children and adults.30,43 The ratio between CSF and peripheral markers may represent a quantification of BBB breakdown, although systemic production of cytokines should not be discounted. Most groups observe higher proinflammatory markers to accompany poor outcomes, but one found that higher peak CSF IL-6 concentrations predicted good clinical outcome following TBI.44 To reconcile the apparent contradiction, this group hypothesized that local cerebral production of IL-6 might be protective, while massive systemic release might provoke systemic inflammatory response syndrome and ultimately be destructive. Another group found that high levels of anti-inflammatory cytokines (IL-1ra, sTNFr-I, and IL-10) correlated with higher ICP and worse outcome, leading these investigators to conclude that anti-inflammatory cytokine levels might reflect the severity of brain injury, rather than the cause of ongoing injury.45 Elevation of CSF IL-10 has been linked to mortality in several studies,46,47 although not in others.48
In addition, there seem to be associations between elevations of certain proinflammatory cytokines and biomarkers that reflect outcome. One group found a strong association between elevated CSF IL1-β and elevated CSF S100B, an accepted biomarker for outcome after neural injury. Both were significantly elevated in patients with poor outcome.41 In addition, the expression of αII-spectrin breakdown product 145 (SBDP145) was measured in the CSF and correlated significantly with a 6-month mortality.49 Combinations of markers have proven more fruitful in the CSF after TBI; for example, S100B, myelin basic protein, and neuron-specific enolase and to a lesser extent TNF were significantly higher in hypoxic patients with unfavorable outcome in one cohort.50 Elevated collections of proinflammatory cytokines may even predict depression.51 The complexity of measuring multiple markers has motivated some investigators to create scores, assigning each marker a point value and evaluating an overall summation with clinically meaningful outcomes as a way of addressing this intricacy.48
The complex protein termed the inflammasome may also prove to be a useful brain injury biomarker. In a recent study, CSF was collected from 23 patients who had experienced a moderate or severe TBI, and levels of inflammasome proteins were measured. Inflammasome levels correlated with outcome as measured by GOS at 5 months.52 Finally, it was recently demonstrated that children with TBI have elevated levels of mitochondrial DNA (an emerging DAMP in neurotrauma) in their CSF as compared with controls and that levels of mitochondrial DNA correlated with poor outcome in the TBI group.53
Microdialysis
Microdialysis is the most specifically cerebral of all the measurements, removing extracellular fluid from a small target area around the end of the probe in the brain.54 In the absence of injury, cytokines are not usually observed in the extracellular space.55 However, after TBI, a robust inflammatory response is observed in the extracellular space similar to serum and CSF, dominated by IL-6 and IL-8.56 Observationally, IL-6 seems to be linked to macroscopic tissue injury,57 yet one group found that elevated IL-6 in microdialysate was linked to improved outcome, similar to the results in CSF.58 If certain proinflammatory cytokines (IL-1β) are balanced by anti-inflammatory cytokines thought to promote repair (IL-1ra), subjects' outcomes seem to be improved. For example, when IL-1β and IL-1ra were measured in brain microdialysates of 15 TBI patients, better outcomes were reported in patients with a high IL-1ra/IL-1β ratio.59 Others have found no relationship between IL-1β, IL-6, IL-8, and IL-10 and important clinical variables such as ICP or brain tissue oxygenation.60 However, almost all patients in this specific case series received either steroidal or nonsteroidal anti-inflammatories, which may have blunted the neuroinflammatory response.61 Another challenge for microdialysis is probe placement. It is possible that the local area sampled in an investigation might be anatomically removed from active, ongoing injury. As microdialysis becomes more available, future data will help address such controversies.
Future Directions: Therapies and Trials
Investigators are gaining a growing appreciation for the immunomodulatory properties of neuroprotectant strategies. Several promising neuroprotectants have been developed to promote immunomodulation as part of the strategy to preserve the central nervous system after trauma. Importantly, clinical outcomes should be impacted by restoring immunologic balance—it is not sufficient to show decreases in inflammatory cytokines. Interventions must change clinically meaningful parameters (e.g., ICP, GOS). Several previous and ongoing clinical trials have endeavored to do just that.
Steroids
Despite some early enthusiasm, corticosteroids have not been shown to be beneficial in the treatment of TBI. The CRASH trial, a multicenter, international, randomized controlled trial that enrolled more than 10,000 patients with acute TBI, which was terminated in 2004, provided high-quality evidence that corticosteroid use in head trauma is contra-indicated given the higher mortality of the treatment group compared with placebo (Grade 1A). The authors were unable to provide a definitive answer as to why mortality was higher, but it did not seem to be caused by infection or gastrointestinal bleeding.62 It is possible that corticosteroids bluntly provide indiscriminate immunosuppression, overwhelming the potentially beneficial limbs of immune activation. Better insight into injury-specific mechanisms might provide a selective role for corticosteroids in the future.
Hypertonic Saline
Hypertonic saline (HS) exhibits numerous beneficial properties in TBI including improved cerebral perfusion and decreased ICP.63 In animals, HS seems to enhance T-cell function and reverse immunosuppression seen in trauma.64,65 When compared with TBI patients receiving normal saline, TBI patients receiving HS showed peripheral blood reductions of TNF-α and IL-10, adding clinical evidence for im-munomodulation.66 Yet, despite these encouraging findings, a large-scale clinical trial was unable to show outcome modification. In 2010, the results of a double-blind, three-group, randomized controlled clinical trial comparing a 250-mL bolus of 7.5% saline (HS) versus 7.5% saline/6% dextran 70 (HS/ dextran) versus 0.9% saline (normal saline) as the initial resuscitation fluid administered to patients suspected of having a severe TBI (GCS score ≤ 8) were published. Patients in hypovolemic shock were excluded. The investigators hypothesized that early control of ICP combined with improved immune function might improve outcomes. However, the authors observed the primary outcome, 6-month Glasgow Outcome Scale Extended scores, to be similar among the groups.67 HS is still helpful in the acute care of cerebral edema but should not be administered indiscriminately to all patients suspected of TBI in the field (Grade 1A).
Hypothermia
Despite encouraging experimental evidence that temperature reduction quells inflammation,68 hypothermia for TBI has not operated as expected clinically. For example, the application of moderate therapeutic hypothermia (32–33°C) in children after severe TBI did not dampen the increase in CSF levels of proinflammatory cytokines as compared with normothermic controls.69 It is possible that induction of hypothermia does not have the same predictable effect on the immune system clinically when compared with rigorous experimental conditions or its benefits are overshadowed by associated complications, such as the metabolic strain of shivering or infections. Even when applied very early, hypothermia does not seem to confer any mortality benefit to patients with severe head injury.70 These results have been echoed in children with severe TBI.71,72 At present, hypothermia is reserved for special circumstances, such as refractory elevated ICP (Grade 1B).
Sex Steroids
There is a wealth of data indicating female animals fare better than males exposed to the same brain injury.73 In humans, there are sex differences in the pattern of inflammation after TBI, specifically that women seem to show a more robust and sustained inflammatory response.55 These observations are attributed to hormonal differences, particularly estrogen and progesterone. Among its neuro protective effects, progesterone down-regulates the synthesis of proinflammatory cytokines as well as decreasing immune cell migration and proliferation after TBI.74 Tw o Phase II clinical trials suggest that progesterone administration in humans may improve survival; however, a Phase III efficacy trial was recently halted for futility (ProTECT III).75,76 One important criticism of both the HS trial and ProTECT III has been the use of Glasgow Outcome Scale Extended as the primary outcome. It may be that this blunt neurologic outcome measure does not relay subtle differences in outcome. Another might be patient selection, enrolling heterogeneous injury types governed only by the admission GCS score and not adjusting for injury subtype (e.g., diffuse axonal injury vs. focal hemorrhagic contusion). Future large-scale clinical trials will do well to address these concerns (Grade 1B).
Mesenchymal Stem Cells
In addition to potentially promoting neuronal growth after TBI, mesenchymal stem cells (MSCs) may also modulate the inflammatory response. In animals, intravenous infusions of MSCs are associated with reduced infiltration of peripheral leukocytes and reduced proinflammatory cytokines.77 MSCs likely function through several pathways, including expressing an IL-1 receptor antagonist, signaling to macrophages to reduce TNF-α (via TSG-6), and secreting prostaglandin (PGE-2) that signals macrophages to produce IL-10 among other me-diators.78 MSCs may also help to repair the BBB.79 In humans, investigators are recruiting patients for safety trials of infusions of MSCs for moderate-to-severe TBI (NCT01575470).
Eicosanoids
Another strategy to modulate inflammation harnesses one of the body's intrinsic substances, namely, prostacyclin. Prostacyclin inhibits platelet activation and serves as a vasodilator. Experimentally, prostacyclin modulates leukocyte behavior, limiting aggregation and adhesion.80 One patient with severe TBI had improvement in microdialysis parameters of ischemia after an intravenous infusion of prostacyclin was in-troduced.81 Recently, a group in Sweden performed a randomized, placebo-controlled trial of epoprostenol, a commercially available prostacyclin, in TBI.82 In a substudy, inflammatory mediators IL-6, IL-8, and C-reactive protein were measured in both groups.83 The epoprostenol-treated group had significantly lower IL-6 and C-reactive protein 73 hours to 96 hours after the trauma, but there were no significant differences in outcomes among the groups (Grade 2A).
Direct Antagonism of Cytokines
A more recent addition to the clinical therapeutics in TBI is the increasing ability to provide direct agonism or antagonism to biomarkers of interest. A group from Cambridge recently conducted an open-label, randomized control trial of a recombinant human IL-1 receptor antagonist daily for 5 days in a small cohort of critically ill TBI patients. Their results suggest that this strategy is safe, penetrates the brain, and seems to impact the cytokine milieu of the microdialysate compared with the control group.84 What effect such a single-agent strategy will have on outcomes is uncertain, but this investigation represents an exciting proof of the concept that systemic administration of an immune modulating agent may have direct intracerebral effects. These results should be replicated in a larger population with outcome data (Grade 2B).
Limitations
The inclusion of studies not initially retrieved by the search terms may have biased our results, although we chose to include these additional studies to add context and completeness to the results section. In addition, some reports may have been inadvertently excluded because of the use of nonsearch term key words.
Conclusion
Investigators have made promising strides forward in understanding the molecular mechanisms underlying secondary brain injury after trauma. Clinical evidence of inflammation causing secondary brain injury in humans is gaining momentum. Markers of inflammation are altered in every readily measured compartment, including serum, CSF, and the extracellular space. While inflammation is certainly present, it is not clear from the literature at what juncture inflammation becomes maladaptive, promoting secondary injury rather than facilitating repair, and identifying patients with maladaptive inflammation (neuroinflammation, systemic, or both) after TBI remains elusive. Direct agonism/antagonism represents an exciting target for future study. Tilting the balance of neuro-inflammation after injury toward cellular repair will be the goal for future therapies. Limiting disability from TBI, not just mortality, will be the next decade's challenge.
Acknowledgments
Disclosure: The project described was supported in part by Award Number 5K12HL108974-03 from the National Heart, Lung, and Blood Institute.
Footnotes
The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the National Heart, Lung, and Blood Institute or the National Institutes of Health.
Authorship: H.E.H. contributed to data abstraction and revision. M.S. contributed to study supervision. All authors contributed to study design and draft writing.
Contributor Information
Holly E. Hinson, Departments of Neurology and Neurocritical Care, Oregon Health and Science University, Portland, Oregon.
Susan Rowell, Department of Surgery, Oregon Health and Science University, Portland, Oregon.
Martin Schreiber, Department of Surgery, Oregon Health and Science University, Portland, Oregon.
References
- 1.Langlois JA, Rutland-Brown W, Wald MM. The epidemiology and impact of traumatic brain injury: a brief overview. J Head Trauma Rehabil. 2006;21(5):375–378. doi: 10.1097/00001199-200609000-00001. [DOI] [PubMed] [Google Scholar]
- 2.Algattas H, Huang JH. Traumatic brain injury pathophysiology and treatments: early, intermediate, and late phases post-injury. Int J Mol Sci. 2014;15(1):309–341. doi: 10.3390/ijms15010309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lenzlinger PM, Morganti-Kossmann MC, Laurer HL, McIntosh TK. The duality of the inflammatory response to traumatic brain injury. Mol Neurobiol. 2001;24(1–3):169–181. doi: 10.1385/MN:24:1-3:169. [DOI] [PubMed] [Google Scholar]
- 4.Moher D, Liberati A, Tetzlaff J, Altman DG The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA Statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. Br Med J. 2008;336(7650):924–926. doi: 10.1136/bmj.39489.470347.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Szmydynger-Chodobska J, Strazielle N, Gandy JR, Keefe TH, Zink BJ, Ghersi-Egea JF, et al. Posttraumatic invasion of monocytes across the blood-cerebrospinal fluid barrier. J Cereb Blood Flow Metab. 2012;32(1):93–104. doi: 10.1038/jcbfm.2011.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kossmann T, Stahel PF, Lenzlinger PM, Redl H, Dubs RW, Trentz O, et al. Interleukin-8 released into the cerebrospinal fluid after brain injury is associated with blood-brain barrier dysfunction and nerve growth factor production. J Cereb Blood Flow Metab. 1997;17(3):280–289. doi: 10.1097/00004647-199703000-00005. [DOI] [PubMed] [Google Scholar]
- 8.Werner C, Engelhard K. Pathophysiology of traumatic brain injury. Br J Anaesth. 2007;99(1):4–9. doi: 10.1093/bja/aem131. [DOI] [PubMed] [Google Scholar]
- 9.Das M, Mohapatra S, Mohapatra SS. New perspectives on central and peripheral immune responses to acute traumatic brain injury. J Neuroinflammation. 2012;9:236. doi: 10.1186/1742-2094-9-236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kelley BJ, Lifshitz J, Povlishock JT. Neuroinflammatory responses after experimental diffuse traumatic brain injury. J Neuropathol Exp Neurol. 2007;66(11):989–1001. doi: 10.1097/NEN.0b013e3181588245. [DOI] [PubMed] [Google Scholar]
- 11.Israelsson C, Bengtsson H, Kylberg A, Kullander K, Lewén A, Hillered L, et al. Distinct cellular patterns of upregulated chemokine expression supporting a prominent inflammatory role in traumatic brain injury. J Neurotrauma. 2008;25(8):959–974. doi: 10.1089/neu.2008.0562. [DOI] [PubMed] [Google Scholar]
- 12.Stefini R, Catenacci E, Piva S, Sozzani S, Valerio A, Bergomi R, et al. Chemokine detection in the cerebral tissue of patients with posttraumatic brain contusions. J Neurosurg. 2008;108(5):958–962. doi: 10.3171/JNS/2008/108/5/0958. [DOI] [PubMed] [Google Scholar]
- 13.Frugier T, Morganti-Kossmann MC, O'Reilly D, McLean CA. In situ detection of inflammatory mediators in post mortem human brain tissue after traumatic injury. J Neurotrauma. 2010;27(3):497–507. doi: 10.1089/neu.2009.1120. [DOI] [PubMed] [Google Scholar]
- 14.Goodman JC, Van M, Gopinath SP, Robertson CS. Pro-inflammatory and pro-apoptotic elements of the neuroinflammatory response are activated in traumatic brain injury. Acta Neurochir Suppl. 2008;102:437–439. doi: 10.1007/978-3-211-85578-2_85. [DOI] [PubMed] [Google Scholar]
- 15.Coughlan CM, McManus CM, Sharron M, Gao Z, Murphy D, Jaffer S, et al. Expression of multiple functional chemokine receptors and monocyte chemoattractant protein-1 in human neurons. Neuroscience. 2000;97(3):591–600. doi: 10.1016/s0306-4522(00)00024-5. [DOI] [PubMed] [Google Scholar]
- 16.Michetti F, Corvino V, Geloso MC, Lattanzi W, Bernardini C, Serpero L, et al. The S100B protein in biological fluids: more than a lifelong bio-marker of brain distress. J Neurochem. 2012;120(5):644–659. doi: 10.1111/j.1471-4159.2011.07612.x. [DOI] [PubMed] [Google Scholar]
- 17.Zhang Q, Raoof M, Chen Y, Sumi Y, Sursal T, Junger W, et al. Circulating mitochondrial DAMPs cause inflammatory responses to injury. Nature. 2010;464(7285):104–107. doi: 10.1038/nature08780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gaetani P, Pisano P, Solinas G, Colombo P, Destro A, Levi D, et al. Immunohistohemical expression of the chemokine fractalkine and its receptor in the human brain cortex after severe traumatic brain injury and brain hemorrhage. J Neurosurg Sci. 2013;57(1):55–62. [PubMed] [Google Scholar]
- 19.Helmy A, Antoniades CA, Guilfoyle MR, Carpenter KL, Hutchinson PJ. Principal component analysis of the cytokine and chemokine response to human traumatic brain injury. PLoS One. 2012;7(6):e39677. doi: 10.1371/journal.pone.0039677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cadosch D, Al-Mushaiqri MS, Gautschi OP, Chan E, Jung FJ, Skirving AP, et al. Immune response deviation and enhanced expression of chemokine receptor CCR4 in TBI patients due to unknown serum factors. Injury. 2010;41(6):e4–e9. doi: 10.1016/j.injury.2009.09.001. [DOI] [PubMed] [Google Scholar]
- 21.Taşçi A, Okay O, Gezici AR, Ergün R, Ergüngör F. Prognostic value of interleukin-1 beta levels after acute brain injury. Neurol Res. 2003;25(8):871–874. doi: 10.1179/016164103771953998. [DOI] [PubMed] [Google Scholar]
- 22.Lumpkins K, Bochicchio GV, Zagol B, Ulloa K, Simard JM, Schaub S, et al. Plasma levels of the beta chemokine regulated upon activation, normal T cell expressed, and secreted (RANTES) correlate with severe brain injury. J Trauma. 2008;64(2):358–361. doi: 10.1097/TA.0b013e318160df9b. [DOI] [PubMed] [Google Scholar]
- 23.Stein DM, Lindell A, Murdock KR, Kufera JA, Menaker J, Keledjian K, et al. Relationship of serum and cerebrospinal fluid biomarkers with intra-cranial hypertension and cerebral hypoperfusion after severe traumatic brain injury. J Trauma. 2011;70(5):1096–1103. doi: 10.1097/TA.0b013e318216930d. [DOI] [PubMed] [Google Scholar]
- 24.Stein DM, Lindel AL, Murdock KR, Kufera JA, Menaker J, Scalea TM. Use of serum biomarkers to predict secondary insults following severe traumatic brain injury. Shock. 2012;37(6):563–568. doi: 10.1097/SHK.0b013e3182534f93. [DOI] [PubMed] [Google Scholar]
- 25.Lo TYM, Jones PA, Minns RA. Combining coma score and serum bio-marker levels to predict unfavorable outcome following childhood brain trauma. J Neurotrauma. 2010;27(12):2139–2145. doi: 10.1089/neu.2010.1387. [DOI] [PubMed] [Google Scholar]
- 26.Sohrevardi SM, Ahmadinejad M, Said K, Sarafzadeh F, Zadeh SS, Yousefi M, et al. Evaluation of TGF A1, IL-8 and nitric oxide in the serum of diffuse axonal injury patients and its association with clinical status and outcome. Turk Neurosurg. 2013;23(2):151–154. doi: 10.5137/1019-5149.JTN.5858-12.2. [DOI] [PubMed] [Google Scholar]
- 27.Gopcevic A, Mazul-Sunko B, Marout J, Sekulic A, Antoljak N, Siranovic M, et al. Plasma interleukin-8 as a potential predictor of mortality in adult patients with severe traumatic brain injury. Tohoku J Exp Med. 2007;211(4):387–393. doi: 10.1620/tjem.211.387. [DOI] [PubMed] [Google Scholar]
- 28.Rhodes J, Sharkey J, Andrews P. Serum IL-8 and MCP-1 concentration do not identify patients with enlarging contusions after traumatic brain injury. J Trauma. 2009;66(6):1591–1597. doi: 10.1097/TA.0b013e31819a0344. discussion 1598. [DOI] [PubMed] [Google Scholar]
- 29.Venetsanou K, Vlachos K, Moles A, Fragakis G, Fildissis G, Baltopoulos G. Hypolipoproteinemia and hyperinflammatory cytokines in serum of severe and moderate traumatic brain injury (TBI) patients. Eur Cytokine Netw. 2007;18(4):206–209. doi: 10.1684/ecn.2007.0112. [DOI] [PubMed] [Google Scholar]
- 30.Kushi H, Saito T, Makino K, Hayashi N. IL-8 is a key mediator of neuroinflammation in severe traumatic brain injuries. Acta Neurochir Suppl. 2003;86:347–350. doi: 10.1007/978-3-7091-0651-8_74. [DOI] [PubMed] [Google Scholar]
- 31.Hergenroeder GW, Moore AN, McCoy JP, Jr, Samsel L, Ward NH, 3rd, Clifton GL, et al. Serum IL-6: a candidate biomarker for intracranial pressure elevation following isolated traumatic brain injury. J Neuroinflammation. 2010;7:19. doi: 10.1186/1742-2094-7-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Woiciechowsky C, Schöning B, Cobanov J, Lanksch WR, Volk HD, Döcke WD. Early IL-6 plasma concentrations correlate with severity of brain injury and pneumonia in brain-injured patients. J Trauma. 2002;52(2):339–345. doi: 10.1097/00005373-200202000-00021. [DOI] [PubMed] [Google Scholar]
- 33.Kalabalikis P, Papazoglou K, Gouriotis D, Papadopoulos N, Kardara M, Papageorgiou F, et al. Correlation between serum IL-6 and CRP levels and severity of head injury in children. Intensive Care Med. 1999;25(3):288–292. doi: 10.1007/s001340050837. [DOI] [PubMed] [Google Scholar]
- 34.Pelinka LE, Kroepfl A, Leixnering M, Buchinger W, Raabe A, Redl H. GFAP versus S100B in serum after traumatic brain injury: relationship to brain damage and outcome. J Neurotrauma. 2004;21(11):1553–1561. doi: 10.1089/neu.2004.21.1553. [DOI] [PubMed] [Google Scholar]
- 35.Nylén K, Ost M, Csajbok LZ, Nilsson I, Blennow K, Nellgård B, et al. Increased serum-GFAP in patients with severe traumatic brain injury is related to outcome. J Neurol Sci. 2006;240(1–2):85–91. doi: 10.1016/j.jns.2005.09.007. [DOI] [PubMed] [Google Scholar]
- 36.Vos PE, Jacobs B, Andriessen TM, Lamers KJB, Borm GF, Beems T, et al. GFAP and S100B are biomarkers of traumatic brain injury: an observational cohort study. Neurology. 2010;75(20):1786–1793. doi: 10.1212/WNL.0b013e3181fd62d2. [DOI] [PubMed] [Google Scholar]
- 37.Papa L, Lewis LM, Falk JL, Zhang Z, Silvestri S, Giordano P, et al. Elevated levels of serum glial fibrillary acidic protein breakdown products in mild and moderate traumatic brain injury are associated with intracranial lesions and neurosurgical intervention. Ann Emerg Med. 2012;59(6):471–483. doi: 10.1016/j.annemergmed.2011.08.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Maier B, Lefering R, Lehnert M, Laurer HL, Steudel WI, Neugebauer EA, et al. Early versus late onset of multiple organ failure is associated with differing patterns of plasma cytokine biomarker expression and outcome after severe trauma. Shock. 2007;28(6):668–674. [PubMed] [Google Scholar]
- 39.Nekludov M, Antovic J, Bredbacka S, Blombäck M. Coagulation abnormalities associated with severe isolated traumatic brain injury: cerebral arterio-venous differences in coagulation and inflammatory markers. J Neurotrauma. 2007;24(1):174–180. doi: 10.1089/neu.2006.0173. [DOI] [PubMed] [Google Scholar]
- 40.Maier B, Lehnert M, Laurer HL, Mautes AE, Steudel WI, Marzi I. Delayed elevation of soluble tumor necrosis factor receptors p75 and p55 in cerebrospinal fluid and plasma after traumatic brain injury. Shock. 2006;26(2):122–127. doi: 10.1097/01.shk.0000223127.41641.f4. [DOI] [PubMed] [Google Scholar]
- 41.Hayakata T, Shiozaki T, Tasaki O, Ikegawa H, Inoue Y, Toshiyuki F, et al. Changes in CSF S100B and cytokine concentrations in early-phase severe traumatic brain injury. Shock. 2004;22(2):102–107. doi: 10.1097/01.shk.0000131193.80038.f1. [DOI] [PubMed] [Google Scholar]
- 42.Csuka E, Morganti-Kossmann MC, Lenzlinger PM, Joller H, Trentz O, Kossmann T. IL-10 levels in cerebrospinal fluid and serum of patients with severe traumatic brain injury: relationship to IL-6, TNF-alpha, TGF-beta1 and blood-brain barrier function. J Neuroimmunol. 1999;101(2):211–221. doi: 10.1016/s0165-5728(99)00148-4. [DOI] [PubMed] [Google Scholar]
- 43.Whalen MJ, Carlos TM, Kochanek PM, Wisniewski SR, Bell MJ, Clark RS, et al. Interleukin-8 is increased in cerebrospinal fluid of children with severe head injury. Crit Care Med. 2000;28(4):929–934. doi: 10.1097/00003246-200004000-00003. [DOI] [PubMed] [Google Scholar]
- 44.Singhal A, Baker AJ, Hare GMT, Reinders FX, Schlichter LC, Moulton RJ. Association between cerebrospinal fluid interleukin-6 concentrations and outcome after severe human traumatic brain injury. J Neurotrauma. 2002;19(8):929–937. doi: 10.1089/089771502320317087. [DOI] [PubMed] [Google Scholar]
- 45.Shiozaki T, Hayakata T, Tasaki O, Hosotubo H, Fuijita K, Mouri T, et al. Cerebrospinal fluid concentrations of anti-inflammatory mediators in early-phase severe traumatic brain injury. Shock. 2005;23(5):406–410. doi: 10.1097/01.shk.0000161385.62758.24. [DOI] [PubMed] [Google Scholar]
- 46.Bell MJ, Kochanek PM, Doughty LA, Carcillo JA, Adelson PD, Clark RS, et al. Interleukin-6 and interleukin-10 in cerebrospinal fluid after severe traumatic brain injury in children. J Neurotrauma. 1997;14(7):451–457. doi: 10.1089/neu.1997.14.451. [DOI] [PubMed] [Google Scholar]
- 47.Kirchhoff C, Buhmann S, Bogner V, Stegmaier J, Leidel BA, Braunstein V, et al. Cerebrospinal IL-10 concentration is elevated in non-survivors as compared to survivors after severe traumatic brain injury. Eur J Med Res. 2008;13(10):464–468. [PubMed] [Google Scholar]
- 48.Lo TYM, Jones PA, Minns RA. Pediatric brain trauma outcome prediction using paired serum levels of inflammatory mediators and brain-specific proteins. J Neurotrauma. 2009;26(9):1479–1487. doi: 10.1089/neu.2008.0753. [DOI] [PubMed] [Google Scholar]
- 49.Czeiter E, Mondello S, Kovacs N, Sandor J, Gabrielli A, Schmid K, et al. Brain injury biomarkers may improve the predictive power of the IMPACT outcome calculator. J Neurotrauma. 2012;29(9):1770–1778. doi: 10.1089/neu.2011.2127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Yan EB, Satgunaseelan L, Paul E, Bye N, Nguyen P, Agyapomaa D, et al. Post-traumatic hypoxia is associated with prolonged cerebral cytokine production, higher serum biomarker levels, and poor outcome in patients with severe traumatic brain injury. J Neurotrauma. 2014;31(7):618–629. doi: 10.1089/neu.2013.3087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Juengst SB, Kumar RG, Failla MD, Goyal A, Wagner AK. Acute inflammatory biomarker profiles predict depression risk following moderate to severe traumatic brain injury. Shock. 2014;41:499–503. doi: 10.1097/HTR.0000000000000031. [DOI] [PubMed] [Google Scholar]
- 52.Adamczak S, Dale G, de Rivero Vaccari JP, Bullock MR, Dietrich WD, Keane RW. Inflammasome proteins in cerebrospinal fluid of brain-injured patients as biomarkers of functional outcome: clinical article. J Neurosurg. 2012;117(6):1119–1125. doi: 10.3171/2012.9.JNS12815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Walko TD, 3rd, Bola RA, Hong JD, Au AK, Bell MJ, Kochanek PM, et al. Cerebrospinal fluid mitochondrial DNAVa novel DAMP in pediatric traumatic brain injury. Shock. 2014 doi: 10.1097/SHK.0000000000000160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Helmy A, Carpenter KLH, Skepper JN, Kirkpatrick PJ, Pickard JD, Hutchinson PJ. Microdialysis of cytokines: methodological considerations, scanning electron microscopy, and determination of relative recovery. J Neurotrauma. 2009;26(4):549–561. doi: 10.1089/neu.2008.0719. [DOI] [PubMed] [Google Scholar]
- 55.Mellergård P, Åneman O, Sjögren F, Säberg C, Hillman J. Differences in cerebral extracellular response of interleukin-1A, interleukin-6, and interleukin-10 after subarachnoid hemorrhage or severe head trauma in humans. Neurosurgery. 2011;68(1):12–19. doi: 10.1227/NEU.0b013e3181ef2a40. discussion 19. [DOI] [PubMed] [Google Scholar]
- 56.Roberts DJ, Jenne CN, Léger C, Kramer AH, Gallagher CN, Todd S, et al. Association between the cerebral inflammatory and matrix metalloproteinase responses after severe traumatic brain injury in humans. J Neurotrauma. 2013;30(20):1727–1736. doi: 10.1089/neu.2012.2842. [DOI] [PubMed] [Google Scholar]
- 57.Hillman J, Aneman O, Persson M, Andersson C, Dabrosin C, Mellergård P. Variations in the response of interleukins in neurosurgical intensive care patients monitored using intracerebral microdialysis. J Neurosurgeon. 2007;106(5):820–825. doi: 10.3171/jns.2007.106.5.820. [DOI] [PubMed] [Google Scholar]
- 58.Winter CD, Pringle AK, Clough GF, Church MK. Raised parenchymal interleukin-6 levels correlate with improved outcome after traumatic brain injury. Brain. 2004;127(Pt 2):315–320. doi: 10.1093/brain/awh039. [DOI] [PubMed] [Google Scholar]
- 59.Hutchinson PJ, O'Connell MT, Rothwell NJ, Hopkins SJ, Nortje J, Carpenter KLH, et al. Inflammation in human brain injury: intracerebral concentrations of IL-1alpha, IL-1beta, and their endogenous inhibitor IL-1ra. J Neurotrauma. 2007;24(10):1545–1557. doi: 10.1089/neu.2007.0295. [DOI] [PubMed] [Google Scholar]
- 60.Perez-Barcena J, Ibáñez J, Brell M, Crespí C, Frontera G, Llompart-Pou JA, et al. Lack of correlation among intracerebral cytokines, intracranial pressure, and brain tissue oxygenation in patients with traumatic brain injury and diffuse lesions. Crit Care Med. 2011;39(3):533–540. doi: 10.1097/CCM.0b013e318205c7a4. [DOI] [PubMed] [Google Scholar]
- 61.Sharma D, Vavilala MS. Intracerebral cytokines in traumatic brain injury: clinical and radiological correlates. Crit Care Med. 2011;39(3):599–601. doi: 10.1097/CCM.0b013e31820a5148. [DOI] [PubMed] [Google Scholar]
- 62.Roberts I, Yates D, Sandercock P, Farrell B, Wasserberg J, Lomas G, et al. Effect of intravenous corticosteroids on death within 14 days in 10008 adults with clinically significant head injury (MRC CRASH trial): randomised placebo-controlled trial. Lancet. 2004;364(9442):1321–1328. doi: 10.1016/S0140-6736(04)17188-2. [DOI] [PubMed] [Google Scholar]
- 63.Dias C, Silva MJ, Pereira E, Silva S, Cerejo A, Smieleweski P, et al. Post-traumatic multimodal brain monitoring: response to hypertonic saline. Acta Pharmacol Sin. 2014;34:1485–1490. doi: 10.1089/neu.2014.3376. [DOI] [PubMed] [Google Scholar]
- 64.Junger WG, Liu FC, Loomis WH, Hoyt DB. Hypertonic saline enhances cellular immune function. Circ Shock. 1994;42(4):190–196. [PubMed] [Google Scholar]
- 65.Coimbra R, Hoyt DB, Junger WG, Angle N, Wolf P, Loomis W, et al. Hypertonic saline resuscitation decreases susceptibility to sepsis after hemorrhagic shock. J Trauma. 1997;42(4):602–606. doi: 10.1097/00005373-199704000-00004. discussion 606–607. [DOI] [PubMed] [Google Scholar]
- 66.Rhind SG, Crnko NT, Baker AJ, Morrison LJ, Shek PN, Scarpelini S, et al. Prehospital resuscitation with hypertonic saline-dextran modulates inflammatory, coagulation and endothelial activation marker profiles in severe traumatic brain injured patients. J Neuroinflammation. 2010;7:5. doi: 10.1186/1742-2094-7-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Bulger EM, May S, Brasel KJ, Schreiber M, Kerby JD, Tisherman SA, et al. Out-of-hospital hypertonic resuscitation following severe traumatic brain injury: a randomized controlled trial. JAMA. 2010;304(13):1455–1464. doi: 10.1001/jama.2010.1405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ma H, Sinha B, Pandya RS, Lin N, Popp AJ, Li J, et al. Therapeutic hypothermia as a neuroprotective strategy in neonatal hypoxic-ischemic brain injury and traumatic brain injury. Curr Mol Med. 2012;12(10):1282–1296. doi: 10.2174/156652412803833517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Buttram SDW, Wisniewski SR, Jackson EK, Adelson PD, Feldman K, Bayir H, et al. Multiplex assessment of cytokine and chemokine levels in cerebrospinal fluid following severe pediatric traumatic brain injury: effects of moderate hypothermia. J Neurotrauma. 2007;24(11):1707–1717. doi: 10.1089/neu.2007.0349. [DOI] [PubMed] [Google Scholar]
- 70.Clifton GL, Valadka A, Zygun D, Coffey CS, Drever P, Fourwinds S, et al. Very early hypothermia induction in patients with severe brain injury (the National Acute Brain Injury Study: Hypothermia II): a randomised trial. Lancet Neurol. 2011;10(2):131–139. doi: 10.1016/S1474-4422(10)70300-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Adelson PD, Wisniewski SR, Beca J, Brown SD, Bell M, Muizelaar JP, et al. Comparison of hypothermia and normothermia after severe traumatic brain injury in children (Cool Kids): a phase 3, randomised controlled trial. Lancet Neurol. 2013;12(6):546–553. doi: 10.1016/S1474-4422(13)70077-2. [DOI] [PubMed] [Google Scholar]
- 72.Hutchison JS, Guerguerian AM. Cooling of children with severe traumatic brain injury. Lancet Neurol. 2013;12(6):527–529. doi: 10.1016/S1474-4422(13)70058-9. [DOI] [PubMed] [Google Scholar]
- 73.Alkayed NJ, Murphy SJ, Traystman RJ, Hurn PD, Miller VM. Neuroprotective effects of female gonadal steroids in reproductively senescent female rats. Stroke. 2000;31(1):161–168. doi: 10.1161/01.str.31.1.161. [DOI] [PubMed] [Google Scholar]
- 74.Wei J, Xiao GM. The neuroprotective effects of progesterone on traumatic brain injury: current status and future prospects. Acta Pharmacol Sin. 2013 doi: 10.1038/aps.2013.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Wright DW, Kellermann AL, Hertzberg VS, Clark PL, Frankel M, Goldstein FC, et al. ProTECT: a randomized clinical trial of progesterone for acute traumatic brain injury. Ann Emerg Med. 2007;49(4):391–402. 402.e1–2. doi: 10.1016/j.annemergmed.2006.07.932. [DOI] [PubMed] [Google Scholar]
- 76.Xiao G, Wei J, Yan W, Wang W, Lu Z. Improved outcomes from the administration of progesterone for patients with acute severe traumatic brain injury: a randomized controlled trial. Crit Care. 2008;12(2):R61. doi: 10.1186/cc6887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Zhang R, Liu Y, Yan K, Chen L, Chen XR, Li P, et al. Anti-inflammatory and immunomodulatory mechanisms of mesenchymal stem cell transplantation in experimental traumatic brain injury. J Neuroinflammation. 2013;10(1):106. doi: 10.1186/1742-2094-10-106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Prockop DJ, Oh JY. Mesenchymal stem/stromal cells (MSCs): role as guardians of inflammation. Mol Ther. 2012;20(1):14–20. doi: 10.1038/mt.2011.211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Menge T, Zhao Y, Zhao J, Wataha K, Gerber M, Zhang J, et al. Mesen-chymal stem cells regulate blood-brain barrier integrity through TIMP3 release after traumatic brain injury. Sci Transl Med. 2012;4(161):161ra150. doi: 10.1126/scitranslmed.3004660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Jones G, Hurley JV. The effect of prostacyclin on the adhesion of leucocytes to injured vascular endothelium. J Pathol. 1984;142(1):51–59. doi: 10.1002/path.1711420110. [DOI] [PubMed] [Google Scholar]
- 81.Reinstrup P, Nordström CH. Prostacyclin infusion may prevent secondary damage in pericontusional brain tissue. Neurocrit Care. 2011;14(3):441–446. doi: 10.1007/s12028-010-9486-3. [DOI] [PubMed] [Google Scholar]
- 82.Olivecrona M, Rodling-Wahlström M, Naredi S, Koskinen LO. Prostacyclin treatment in severe traumatic brain injury: a microdialysis and outcome study. J Neurotrauma. 2009;26(8):1251–1262. doi: 10.1089/neu.2008.0605. [DOI] [PubMed] [Google Scholar]
- 83.Wahlström MR, Olivecrona M, Ahlm C, Bengtsson A, Koskinen LO, Naredi S, et al. Effects of prostacyclin on the early inflammatory response in patients with traumatic brain injury—a randomised clinical study. Springerplus. 2014;3:98. doi: 10.1186/2193-1801-3-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Helmy A, Guilfoyle MR, Carpenter KLH, Pickard JD, Menon DK, Hutchinson PJ. Recombinant human interleukin-1 receptor antagonist in severe traumatic brain injury: a phase II randomized control trial. J Cereb Blood Flow Metab. 2014;34(5):845–851. doi: 10.1038/jcbfm.2014.23. [DOI] [PMC free article] [PubMed] [Google Scholar]