Anxiety and depression in patients with gastroesophageal reflux disease and their effect on quality of life (original) (raw)
Abstract
AIM: To explore the role of psychological factors in gastroesophageal reflux disease (GERD) and their effect on quality of life (QoL) of GERD patients.
METHODS: A total of 279 consecutive patients with typical symptoms and 100 healthy controls were enrolled in the study. All of the participants were evaluated with the Zung Self-Rating Anxiety Scale (ZSAS), the Zung Self-Rating Depression Scale (ZSDS) and the SF-36 questionnaire. The scores for anxiety, depression and QoL of the two groups were analyzed. The correlation between psychological factors and QoL was also analyzed.
RESULTS: Compared with healthy controls (34.70 ± 8.00), the scores of ZSAS in the non-erosive reflux disease (NERD) group (48.27 ± 10.34) and the reflux esophagitis (RE) group (45.38 ± 10.27) were significantly higher (P < 0.001). The mean ZSAS score of the NERD group was significantly higher than that of the RE group (P = 0.01). Compared with healthy controls (37.61 ± 8.44), the mean ZSDS scores were significantly higher in the NERD group (49.65 ± 11.09, P < 0.001) and the RE group (46.76 ± 11.83, P < 0.001). All dimensions of the SF-36 form were negatively correlated with the SAS and SDS scores in patients with NERD and RE (P < 0.05). According to the SF-36 form, vitality, mental health and social functioning were significantly correlated with symptoms of depression in patients with NERD and RE. General health was obviously affected by symptoms of depression in patients with NERD (P < 0.05).
CONCLUSION: Anxiety and depression may play an important role in the occurrence of GERD and especially that of NERD. The QoL of patients with GERD is reduced by anxiety and depression.
Keywords: Anxiety, Depression, Gastroesophageal reflux disease, Zung Self-Rating Anxiety Scale, Zung Self-Rating Depression Scale, SF-36, Quality of life
Core tip: In our study, the degree of anxiety and depression in non-erosive reflux disease (NERD) and reflux esophagitis patients was significantly higher than that of healthy controls, especially for the NERD group. The quality of life was negatively correlated with the degree of anxiety and depression.
INTRODUCTION
Gastroesophageal reflux disease (GERD) is a condition characterized by the reflux of stomach contents into the esophagus, which causes several symptoms, such as heartburn and regurgitation. It is typically divided into three subtypes: reflux esophagitis (RE), non-erosive reflux disease (NERD) and Barrett’s esophagus. GERD has been shown to have a significant negative impact on the quality of life (QoL) of affected patients and may even disrupt their daily activities. On a weekly basis, GERD affects up to 20% of the population in the United States and Europe[1], 12% to 15% in Australia, and 2% to 5% in Asia[2]. Therefore, a diagnosis of GERD is easily made based on the symptoms of the patients, which typically include heartburn and regurgitation and/or other atypical acid reflux-related symptoms. Meanwhile, a diagnosis can also be obtained from gastroendoscopic findings of visible esophageal mucosal injury. NERD has been defined as the presence of acid reflux-related symptoms with no esophageal mucosal injury.
The etiology of GERD is multifactorial. The disease results from an imbalance between the harmful properties of refluxed stomach contents, mechanisms of esophageal clearance, and esophageal mucosal resistance[3]. Common risk factors for GERD including the absence of a hiatus hernia, a low body mass index (BMI) and the presence of Helicobacter pylori, indicate that this condition is a milder form of disease within the GERD spectrum. The majority of patients with GERD use antacid drugs to control their symptoms. However, the symptoms of GERD are sometimes impossible to control, and these patients tend to have a lower response rate, even to the most potent proton-pump inhibitors (PPIs)[4,5]. Some studies have already demonstrated that up to 40% of patients with heartburn reported either a partial or complete lack of response to PPIs taken once daily[6-8]. According to clinical data, apart from the common risk factors listed above, psychological factors, including anxiety and depression, can also develop in patients with GERD. We supposed that the psychological factors associated with NERD may distinguish NERD from RE and Barrett’s esophagus.
We hypothesized that psychological factors may comprise some of the essential influencing factors and that they might impair the QoL of individuals with GERD. However, it remains unknown how psychological factors induce GERD and affect the QoL in patients with GERD in China. To explore the link between psychological factors and the pathophysiology of GERD, this study evaluated the psychological status of patients with GERD and its effect on QoL.
MATERIALS AND METHODS
Subjects
A total of 279 consecutive patients with typical symptoms of heartburn or regurgitation from the Division of Gastroenterology (Union Hospital, Tongji Medical College) and 100 healthy controls selected among the staff of Union Hospital and medical students of Tongji Medical College were enrolled in this study.
Procedure
All subjects agreed to participate and signed an informed consent form. Subsequently, subjects underwent gastroendoscopy to evaluate for the presence of esophageal mucosal lesions. Based on the results of the gastroendoscopy, the patients were divided into two major groups: RE (including Barrett’s esophagus; males = 71; females = 63) and NERD (males = 66; females = 79). GERD was diagnosed according to the previously proposed Rome III criteria. Patients were excluded for the following reasons: use of prescribed non-steroidal anti-inflammatory drugs (NSAIDs) and aspirin; previous treatment with a proton pump inhibitor (patients who were treated with H2-blockers were allowed to participate if the treatment had been discontinued 14 d prior to the initial evaluation); incidence of a peptic stricture or duodenal and/or gastric ulcer visible on upper endoscopy; a history of upper gastrointestinal surgery; comorbidities, such as scleroderma, diabetes mellitus, autonomic or peripheral neuropathy, myopathy, functional bowel disorder or any underlying disease (or medication) that might affect the lower esophageal sphincter pressure or increase the acid clearance time; inability or unwillingness to fully complete all stages of the study; and inability or unwillingness to provide informed consent. This protocol was approved by the Ethics Committee of Tongji Medical College (No. 104).
Measures
The Zung Self-Rating Anxiety Scale (ZSAS) was designed by William WK Zung to evaluate the level of anxiety in patients who experience anxiety-related symptoms[9]. The ZSAS contains 20 questions. Each question is scored on a scale of 1-4 (never, some of the time, relatively often, most of the time). Fifteen questions involve the assessment of increasing anxiety levels, and five questions involve decreasing anxiety levels. The ZSAS scores were used to define four categories of anxiety severity: within normal range or no significant psychopathology (20-44 points); presence of mild to moderate anxiety levels (45-59 points); severe anxiety levels (60-74 points); and presence of extreme depression (75-80 points).
Similarly, the Zung Self-Rating Depression Scale (ZSDS) was used to assess the severity of depression in the patients[10]. The ZSDS includes 10 positively worded items and 10 negatively worded items that assess symptoms of depression. Item responses are ranked from 1 to 4, and higher scores correspond to more frequent symptoms. Therefore, for each item, patients give a score according to whether the item has occurred: 1 = never/very rarely/rarely; 2 = once in a while/some of the time/occasionally; 3 = relatively often/very often/often; 4 = most of the time/always/almost always. The ZSDS scores were used to define four categories of depression severity: within normal range or no significant psychopathology (below 40 points); presence of minimal to mild depression (40-47 points); presence of moderate to marked depression (48-55 points); and presence of severe to extreme depression (56 points and above). Total scores on the ZSDS do not correspond with a clinical diagnosis of depression but rather indicate the level of depressive symptoms that may be clinically relevant.
The 36-item Short-Form Health Survey (SF-36) is a commonly used generic questionnaire that includes 36 items clustered into eight dimensions (bodily pain, general health, mental health, physical functioning, role-emotional, role-physical, social functioning, and vitality)[11]. The item scores for each dimension are coded, summed and transformed to a scale from 0 (worst possible health status) to 100 (best possible health status). The SF-36 is well-documented in terms of reliability and validity in all available language versions. Each raw scale score is linearly transformed to t scores. The transformed scores range from 0 to 100; higher scores indicate a better health-related QoL. These physical and mental summary scores served as the dependent variables in our analysis. We performed a separate analysis for each score.
Statistical analysis
The statistical analyses were performed using SPSS software (SPSS, Version 18; Chicago, IL, United States). For all continuous variables, the mean and standard deviation are presented. One-way analysis of variance was used to compare the parametric quantitative variables, followed by LSD or Tamhane’s T2 test for a post-hoc analysis to further examine the differences among the groups. A χ2 test or Fisher’s exact test was used to compare the proportions. All _P_-values were two-tailed, and the level of significance was defined at 0.05.
RESULTS
Demographic and clinical characteristics
A total of 279 patients and 100 healthy controls were included in this study. Patient demographics and clinical characteristics are shown in Table 1. No significant differences were observed with respect to sex or age among the three groups.
Table 1.
Patient demographics and clinical data (n = 379)
| Healthy controls | RE patients | NERD patients | |
|---|---|---|---|
| n | 100 | 134 | 145 |
| Gender (M/F)1 | 49/51 | 71/63 | 66/79 |
| mean age (yr)2 | 40.04 ± 12.22 | 41.07 ± 10.61 | 39.68 ± 10.80 |
| Age range (yr) | 19-67 | 23-68 | 16-71 |
Prevalence of anxiety symptoms in patients with NERD
A total of 379 people completed the ZSAS questionnaire. The characteristics of the anxiety symptoms according to the ZSAS are detailed in Table 2. The results of the χ2 test revealed a significant difference in the constituent ratio of the three groups (P < 0.001). Compared with healthy controls, the constituent ratios of both the NERD group and the RE group presented a significant difference (P < 0.001). The incidence of anxiety was significantly higher in the NERD group than in the RE group (Fisher’s exact test, P = 0.050). As shown in Figure 1, the mean scores of the ZSAS in the NERD group (48.27 ± 10.34) and in the RE group (45.38 ± 10.27) were significantly higher than that of the healthy control group (34.70 ± 8.00) (P < 0.001). Moreover, the mean score of the NERD group was significantly higher than that of the RE group (P = 0.01), suggesting that patients with NERD experienced more severe anxiety than did patients with RE, despite the fact that patients with NERD lacked esophageal erosions.
Table 2.
Characteristics of anxiety symptoms according to the Zung self-rating anxiety scale n (%)
| Group | Normal | Mild to moderate | Severe | Extreme |
|---|---|---|---|---|
| Healthy control | 86 (86) | 13 (13) | 1 (1) | 0 (0) |
| RE | 61 (45.52) | 59 (44.03) | 14 (10.44) | 0 (0) |
| NERD | 49 (33.79) | 72 (49.66) | 24 (16.55) | 0 (0) |
Figure 1.
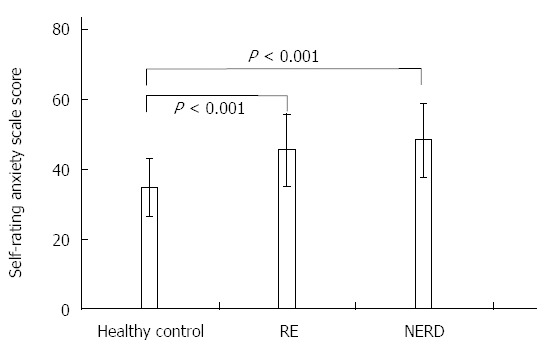
Comparison of the Zung self-rating anxiety scale scores in the three groups. RE: Reflux esophagitis; NERD: Non-erosive reflux disease.
Prevalence of depressive symptoms in patients with NERD
A significant difference was observed in the constituent ratios of the three groups (P < 0.001). The SDS scores were significantly higher in patients with NERD (49.65 ± 11.09, P < 0.001) and in patients with RE (46.76 ± 11.83, P < 0.001) compared with those of healthy controls (37.61 ± 8.44) (Figure 2). However, the constituent ratios between patients with NERD and patients with RE were not significantly different (χ2 = 6.556, P = 0.085) (Table 3). In addition, the incidence of depression in patients with NERD was higher than that in patients with RE (Fisher’s exact test, P = 0.020).
Figure 2.
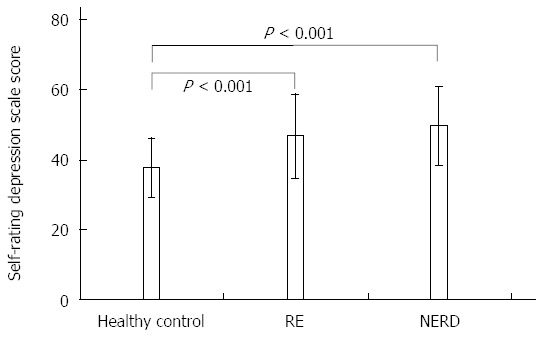
Comparison of Zung self-rating depression scale scores in the three groups. RE: Reflux esophagitis; NERD: Non-erosive reflux disease.
Table 3.
Characteristics of anxiety symptoms according to the Zung self-rating depression scale n (%)
| SDS | Normal | Mild to moderate | Severe | Extreme |
|---|---|---|---|---|
| Healthy, control | 80 (86) | 11 (13) | 8 (1) | 1 (0) |
| RE | 42 (31.34) | 43 (32.09) | 26 (19.40) | 23 (17.16) |
| NERD | 32 (22.07) | 38 (26.21) | 35 (24.14) | 40 (27.59) |
QoL in the three groups
The standardized component scales of the SF36 are reported in this text as summary information on QoL shown in Figure 3. Compared with the healthy controls, all of the dimensions had statistically lower scores in the NERD and RE groups (P < 0.05), indicating that the QoL of patients with both NERD and RE was inferior to that of the healthy controls. In the NERD group, the scores of vitality and mental health were statistically lower than those of RE patients, which means that part dimensions of QoL in NERD patients were more decreased than those of RE patients (P < 0.05).
Figure 3.
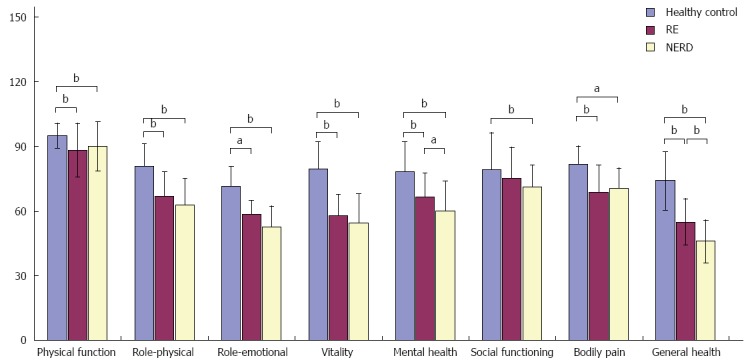
Comparison of the quality of life in the three groups. a_P <_ 0.05, b_P <_ 0.01. RE: Reflux esophagitis; NERD: Non-erosive reflux disease.
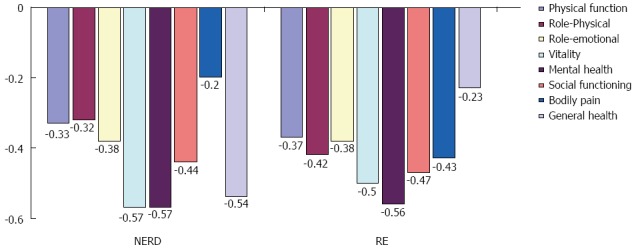
Negative correlation of the ZSAS scores with the SF-36 survey in NERD and RE patients
Correlations between the scores of SAS and SF-36 are shown in Figure 4. All of the dimensions of the SF-36 survey were significantly negatively correlated with the SAS anxiety scores in patients with NERD and RE, which means that QoL of patients with GERD was decreased by anxiety. At the same time, general health and mental health of patients with NERD seemed to decrease more readily due to anxiety symptoms compared with these same dimensions in patients with RE (P < 0.05). The correlation coefficients between the ZSAS scores and the other dimensions of the SF-36 survey, such as physical function, role-physical, role-emotional, and social functioning, were similar in both groups.
Figure 4.
Negative correlations between the Zung self-rating anxiety scale scores and the SF-36 survey. All items of the SF-36 were significantly negatively correlated with the SAS anxiety scores in NERD and RE group (P < 0.05). RE: Reflux esophagitis; NERD: Non-erosive reflux disease.
Negative correlation of the SDS scores with the SF-36 survey in patients with NERD and RE
Correlations between the scores of SDS and SF-36 are shown in Figure 5. All of the dimensions of the SF-36 form were significantly negatively correlated with the SDS scores. As a result of the negative correlation between the ZSAS and the SF-36 form, vitality, mental health and social functioning were significantly correlated with depressive symptoms in both groups. Although bodily pain was significantly correlated with symptoms of depression in both groups, it appeared that patients with RE were more easily troubled by depression. However, the general health dimension was more likely to be lowered by symptoms of depression in patients with NERD (P < 0.05). The correlation coefficients between the ZSDS scores and the other dimensions of the SF-36 form, such as physical function, role-physical, and role-emotional, were similar in both groups.
Figure 5.
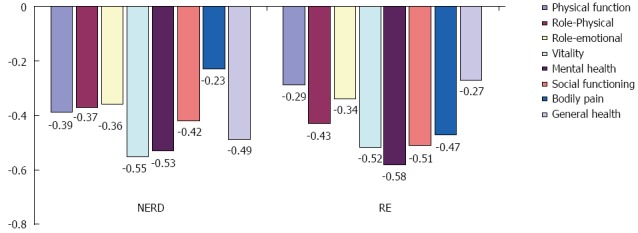
Negative correlations between the Zung self-rating depression scale scores and the SF-36 survey. All items of the SF-36 were significantly negatively correlated with the SDS depression scores in NERD and RE group (P < 0.05). RE: Reflux esophagitis; NERD: Non-erosive reflux disease.
DISCUSSION
According to previous epidemiological surveys, psychological factors play an important role in patients with GERD and have been shown to decrease QoL[12]. Although there have been some studies on the morbidity of GERD in China[13-16], no surveys have been reported on the role of psychological factors in GERD and their negative impact on QoL. In the current study, we analyzed the roles of both anxiety and depression symptoms on the incidence of GERD, as well as their negative impact on QoL in patients with GERD. The results suggested that the incidence of GERD was correlated with anxiety and depression, and QoL of patients with GERD was reduced statistically.
GERD is associated with anxiety and depression. Another study showed that the psychological scores for neuroticism, anxiety and depression were higher in patients with GERD than in healthy controls[13,17]. Moreover, psychological disorders were found to be positively correlated with symptoms of heartburn[18]. In our study, anxiety and depression scores of patients with NERD and RE were obviously higher than those of healthy controls. The difference in the constituent ratios of the three groups also implied a moderate to severe degree of anxiety and depression in the patients with NERD and RE, suggesting an important role of anxiety and depression in the pathogenesis of GERD. Other studies have shown that patients with anxiety or depression are at an increased risk for the development of reflux symptoms[19-22]. Jansson et al[23] reported that patients with anxiety but no depression had a 3.2-fold (95%CI: 2.7-3.8) increased risk of reflux symptoms and that those with depression but no anxiety had a 1.7-fold (95%CI: 1.4-2.1) increased risk; subjects with both anxiety and depression presented a 2.8-fold (95%CI: 2.4-3.2) increased risk compared with subjects without anxiety/depression. Two explanations have been offered on the correlation between psychological factors and GERD. The first theory is that anxiety and depression develop secondary to the reflux and then cause increased sensitivity to the reflux symptoms. The second explanation is that the severity of reflux is greater in patients with psychiatric diseases[24].
Moreover, the scores of anxiety and depression in patients with NERD were significantly higher than those in patients with RE, which may indicate a different pathogenesis of NERD in our study. A large number of epidemiological investigations have also found that anxiety, depression, and chronic stress can lead to NERD[12]. NERD accounts for an estimated 50% to 70% of GERD cases[25,26]. NERD is considered a heterogeneous group because of the various characteristics and symptom patterns of acid reflux. Studies have also shown that RE and NERD respond differently to PPIs because of their distinct pathogenesis[27-29]. On one hand, NERD is significantly more refractory than RE to PPI treatment[30,31]. On the other hand, some studies have indicated that anxiety and depression can worsen the symptoms of reflux[23]. Patients with typical GERD symptoms were more likely to have atypical symptoms, dyspepsia and higher scores on psychological symptoms (e.g., somatization, obsessive-compulsion and phobic anxiety) than those without GERD symptoms[32].
Apart from reflux symptoms, anxiety and depression can also decrease the QoL in patients with GERD. It has been reported that all dimensions of health-related QoL, as measured using the SF-36 questionnaire, were meaningfully impaired in subjects with symptomatic GERD compared with subjects without[33]. Those results are consistent with the results of our study, which indicate a lower QoL score in patients with GERD compared with healthy controls. In our study, the SF-36 questionnaire was employed to evaluate the QoL of the subjects. Generally, the scores for items of the SF-36 form were significantly decreased in patients with NERD and RE compared with the healthy controls. Interestingly, all of the scores for items in patients with NERD were more severely lowered than the scores in patients with RE, especially with respect to mental health and general health. Therefore, we suggest that psychological factors play important roles in the development of GERD, especially that of NERD. In addition, the study by Kovács et al[34] also reported that, along with anxiety, the symptoms of depression caused by persistent living pressure were elevated; the QoL of patients with GERD was also decreased. However, Lee reported that venlafaxine, an SNRI antidepressant, significantly improved symptoms in young adult patients with functional chest pain[35]. The results also indicated that GERD symptom was reversible by antidepressant. In our study, anxiety and depression were negatively correlated with all dimensions of the SF-36 questionnaire. However, Boltin et al[36] reported that lack of response to PPI was associated with lower life satisfaction but not anxiety or depression. Therefore, we posited that, except acid reflux symptoms, the increased anxiety and depression in patients with NERD and RE were other factors that lowered the QoL.
In summary, psychological factors, including anxiety and depression, play an essential role in the development of GERD and especially that of NERD. Meanwhile, they have obvious negative effects on QoL. Consequently, anti-anxiety and anti-depression medications may be alternative therapies for patients with NERD and RE if antacids cannot produce a satisfactory effect. This issue requires further study to identify the patients who might benefit from anti-anxiety and anti-depression therapy in the future. Moreover, this study was conducted in a university hospital. Therefore, the results may be different from those visiting a general physician. If this was a multicenter study, the results should be more reasonable.
COMMENTS
Background
Gastroesophageal reflux disease (GERD) has been shown to have a significant negative impact on the quality of life (QoL) of affected patients and may even disrupt their daily activities. The etiology of GERD is multifactorial. Common risk factors for GERD including the absence of a hiatus hernia, a low BMI and the presence of Helicobacter pylori, indicate that this condition is a milder form of disease within the GERD spectrum. The majority of patients with GERD use antacid drugs to control their symptoms. However, the symptoms of GERD are sometimes impossible to control, and these patients tend to have a lower response rate, even to the most potent proton-pump inhibitors (PPIs). According to clinical data, apart from the common risk factors listed above, psychological factors, including anxiety and depression, can also develop in patients with GERD. So, this study investigated the role of anxiety and depression in GERD and their effect on quality of life.
Research frontiers
Functional gastrointestinal disease is always concerned with psychological factors. The quality of life of patients is often reduced. As for GERD, PPIs are not always effective. So, it is necessary to explore the course of GERD and its correlation with psychological factors.
Innovations and breakthroughs
Anxiety and depression were concerned with incidence of functional gastrointestinal disease. Our study results indicated the incidence and degree of anxiety in the NERD group were significantly higher than those in the reflux esophagitis (RE) group. As for depression in the NERD group, the results were the same. SF36 was employed to evaluate the quality of life, and the results indicated that QoL of patients with both NERD and RE was inferior to that of the healthy controls. The QoL of NERD and RE patients was significantly correlated with anxiety and depression.
Applications
This study may help gastroenterologist to understand the role of psychological factors in GERD. The results may help them to focus on other pathogenic factors for GERD, and try new therapy.
Peer-review
In this study, anxiety and depression scores of patients with NERD and RE were higher than those of healthy controls. The QoL of NERD and RE patients was significantly decreased, especially for NERD ones. The QoL was negatively correlated with anxiety and depression significantly.
Footnotes
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: July 31, 2014
First decision: August 15, 2014
Article in press: December 8, 2014
P- Reviewer: Nishida T S- Editor: Yu J L- Editor: Wang TQ E- Editor: Liu XM
References
- 1.Sonnenberg A, El-Serag HB. Clinical epidemiology and natural history of gastroesophageal reflux disease. Yale J Biol Med. 1999;72:81–92. [PMC free article] [PubMed] [Google Scholar]
- 2.Locke GR, Talley NJ, Fett SL, Zinsmeister AR, Melton LJ. Prevalence and clinical spectrum of gastroesophageal reflux: a population-based study in Olmsted County, Minnesota. Gastroenterology. 1997;112:1448–1456. doi: 10.1016/s0016-5085(97)70025-8. [DOI] [PubMed] [Google Scholar]
- 3.Kongara K, Varilek G, Soffer EE. Salivary growth factors and cytokines are not deficient in patients with gastroesophageal reflux disease or Barrett’s esophagus. Dig Dis Sci. 2001;46:606–609. doi: 10.1023/a:1005615703009. [DOI] [PubMed] [Google Scholar]
- 4.Dean BB, Gano AD, Knight K, Ofman JJ, Fass R. Effectiveness of proton pump inhibitors in nonerosive reflux disease. Clin Gastroenterol Hepatol. 2004;2:656–664. doi: 10.1016/s1542-3565(04)00288-5. [DOI] [PubMed] [Google Scholar]
- 5.Galmiche JP. Non-erosive reflux disease and atypical gastro-oesophageal reflux disease manifestations: treatment results. Drugs. 2006;66 Suppl 1:7–13; discussion 29-33. doi: 10.2165/00003495-200666001-00003. [DOI] [PubMed] [Google Scholar]
- 6.Hershcovici T, Fass R. Management of gastroesophageal reflux disease that does not respond well to proton pump inhibitors. Curr Opin Gastroenterol. 2010;26:367–378. doi: 10.1097/MOG.0b013e32833ae2be. [DOI] [PubMed] [Google Scholar]
- 7.Hershcovici T, Fass R. An algorithm for diagnosis and treatment of refractory GERD. Best Pract Res Clin Gastroenterol. 2010;24:923–936. doi: 10.1016/j.bpg.2010.10.004. [DOI] [PubMed] [Google Scholar]
- 8.Fass R. Proton pump inhibitor failure--what are the therapeutic options? Am J Gastroenterol. 2009;104 Suppl 2:S33–S38. doi: 10.1038/ajg.2009.50. [DOI] [PubMed] [Google Scholar]
- 9.Zung WW. A rating instrument for anxiety disorders. Psychosomatics. 1971;12:371–379. doi: 10.1016/S0033-3182(71)71479-0. [DOI] [PubMed] [Google Scholar]
- 10.Zung WW. A self-rating depression scale. Arch Gen Psychiatry. 1965;12:63–70. doi: 10.1001/archpsyc.1965.01720310065008. [DOI] [PubMed] [Google Scholar]
- 11.Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–483. [PubMed] [Google Scholar]
- 12.Hartono JL, Mahadeva S, Goh KL. Anxiety and depression in various functional gastrointestinal disorders: do differences exist? J Dig Dis. 2012;13:252–257. doi: 10.1111/j.1751-2980.2012.00581.x. [DOI] [PubMed] [Google Scholar]
- 13.Li YM, Du J, Zhang H, Yu CH. Epidemiological investigation in outpatients with symptomatic gastroesophageal reflux from the Department of Medicine in Zhejiang Province, east China. J Gastroenterol Hepatol. 2008;23:283–289. doi: 10.1111/j.1440-1746.2007.05045.x. [DOI] [PubMed] [Google Scholar]
- 14.Chen T, Lu M, Wang X, Yang Y, Zhang J, Jin L, Ye W. Prevalence and risk factors of gastroesophageal reflux symptoms in a Chinese retiree cohort. BMC Gastroenterol. 2012;12:161. doi: 10.1186/1471-230X-12-161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee SW, Chang CM, Chang CS, Kao AW, Chou MC. Comparison of presentation and impact on quality of life of gastroesophageal reflux disease between young and old adults in a Chinese population. World J Gastroenterol. 2011;17:4614–4618. doi: 10.3748/wjg.v17.i41.4614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.He J, Ma X, Zhao Y, Wang R, Yan X, Yan H, Yin P, Kang X, Fang J, Hao Y, et al. A population-based survey of the epidemiology of symptom-defined gastroesophageal reflux disease: the Systematic Investigation of Gastrointestinal Diseases in China. BMC Gastroenterol. 2010;10:94. doi: 10.1186/1471-230X-10-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lee YC, Wang HP, Chiu HM, Liao SC, Huang SP, Lai YP, Wu MS, Chen MF, Lin JT. Comparative analysis between psychological and endoscopic profiles in patients with gastroesophageal reflux disease: a prospective study based on screening endoscopy. J Gastroenterol Hepatol. 2006;21:798–804. doi: 10.1111/j.1440-1746.2005.04034.x. [DOI] [PubMed] [Google Scholar]
- 18.Haug TT, Mykletun A, Dahl AA. Are anxiety and depression related to gastrointestinal symptoms in the general population? Scand J Gastroenterol. 2002;37:294–298. doi: 10.1080/003655202317284192. [DOI] [PubMed] [Google Scholar]
- 19.Jansson C, Wallander MA, Johansson S, Johnsen R, Hveem K. Stressful psychosocial factors and symptoms of gastroesophageal reflux disease: a population-based study in Norway. Scand J Gastroenterol. 2010;45:21–29. doi: 10.3109/00365520903401967. [DOI] [PubMed] [Google Scholar]
- 20.Kim JY, Kim N, Seo PJ, Lee JW, Kim MS, Kim SE, Jo SY, Lee DH, Jung HC. Association of sleep dysfunction and emotional status with gastroesophageal reflux disease in Korea. J Neurogastroenterol Motil. 2013;19:344–354. doi: 10.5056/jnm.2013.19.3.344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Niu XP, Yu BP, Wang YD, Han Z, Liu SF, He CY, Zhang GZ, Wu WC. Risk factors for proton pump inhibitor refractoriness in Chinese patients with non-erosive reflux disease. World J Gastroenterol. 2013;19:3124–3129. doi: 10.3748/wjg.v19.i20.3124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jiang C, Shen YH, Qin XY, Li Y, Cai W, Li YL, Wu X, Hu YH. [A community-based epidemiologic study on gastroesophageal reflux disease in Haidian district of Beijing] Zhonghua Yufang Yixue Zazhi. 2010;44:516–521. [PubMed] [Google Scholar]
- 23.Jansson C, Nordenstedt H, Wallander MA, Johansson S, Johnsen R, Hveem K, Lagergren J. Severe gastro-oesophageal reflux symptoms in relation to anxiety, depression and coping in a population-based study. Aliment Pharmacol Ther. 2007;26:683–691. doi: 10.1111/j.1365-2036.2007.03411.x. [DOI] [PubMed] [Google Scholar]
- 24.Oh JH, Kim TS, Choi MG, Lee H, Jeon EJ, Choi SW, Lee C, Chung IS. Relationship between Psychological Factors and Quality of Life in Subtypes of Gastroesophageal Reflux Disease. Gut Liver. 2009;3:259–265. doi: 10.5009/gnl.2009.3.4.259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tack J, Caenepeel P, Arts J, Lee KJ, Sifrim D, Janssens J. Prevalence of acid reflux in functional dyspepsia and its association with symptom profile. Gut. 2005;54:1370–1376. doi: 10.1136/gut.2004.053355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang K, Duan LP, Chen H, Xia ZW, Lin SR. [Comparison of esophageal acid exposure characteristics between reflux oesophagitis and non-erosive reflux diseases] Zhonghua Neike Zazhi. 2005;44:5–8. [PubMed] [Google Scholar]
- 27.Fujiwara Y, Higuchi K, Shiba M, Yamamori K, Watanabe Y, Sasaki E, Tominaga K, Watanabe T, Oshitani N, Arakawa T. Differences in clinical characteristics between patients with endoscopy-negative reflux disease and erosive esophagitis in Japan. Am J Gastroenterol. 2005;100:754–758. doi: 10.1111/j.1572-0241.2005.40966.x. [DOI] [PubMed] [Google Scholar]
- 28.Wu JC. Gastroesophageal reflux disease: an Asian perspective. J Gastroenterol Hepatol. 2008;23:1785–1793. doi: 10.1111/j.1440-1746.2008.05684.x. [DOI] [PubMed] [Google Scholar]
- 29.Fass R. Erosive esophagitis and nonerosive reflux disease (NERD): comparison of epidemiologic, physiologic, and therapeutic characteristics. J Clin Gastroenterol. 2007;41:131–137. doi: 10.1097/01.mcg.0000225631.07039.6d. [DOI] [PubMed] [Google Scholar]
- 30.Lee ES, Kim N, Lee SH, Park YS, Kim JW, Jeong SH, Lee DH, Jung HC, Song IS. Comparison of risk factors and clinical responses to proton pump inhibitors in patients with erosive oesophagitis and non-erosive reflux disease. Aliment Pharmacol Ther. 2009;30:154–164. doi: 10.1111/j.1365-2036.2009.04021.x. [DOI] [PubMed] [Google Scholar]
- 31.Hiyama T, Yoshihara M, Tanaka S, Haruma K, Chayama K. Strategy for treatment of nonerosive reflux disease in Asia. World J Gastroenterol. 2008;14:3123–3128. doi: 10.3748/wjg.14.3123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lee SP, Lee KN, Lee OY, Lee HL, Choi HS, Yoon BC, Jun DW, Sohn W, Cho SC. The relationship between existence of typical symptoms and psychological factors in patients with erosive esophagitis. J Neurogastroenterol Motil. 2012;18:284–290. doi: 10.5056/jnm.2012.18.3.284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Masoumi SJ, Khademolhosseini F, Mehrabani D, Moradi F, Mostaghni AA, Zare N, Montazeri A, Saberi-Firoozi M. Correlation of quality of life with gastroesophageal reflux disease amongst Qashqai nomads in Iran. Arch Iran Med. 2012;15:747–750. [PubMed] [Google Scholar]
- 34.Kovács Z, Seres G, Kerékgyártó O, Czobor P. Psychopathological symptom dimensions in patients with gastrointestinal disorders. J Clin Psychol Med Settings. 2010;17:378–386. doi: 10.1007/s10880-010-9212-5. [DOI] [PubMed] [Google Scholar]
- 35.Lee H, Kim JH, Min BH, Lee JH, Son HJ, Kim JJ, Rhee JC, Suh YJ, Kim S, Rhee PL. Efficacy of venlafaxine for symptomatic relief in young adult patients with functional chest pain: a randomized, double-blind, placebo-controlled, crossover trial. Am J Gastroenterol. 2010;105:1504–1512. doi: 10.1038/ajg.2010.82. [DOI] [PubMed] [Google Scholar]
- 36.Boltin D, Boaz M, Aizic S, Sperber A, Fass R, Niv Y, Dickman R. Psychological distress is not associated with treatment failure in patients with gastroesophageal reflux disease. J Psychosom Res. 2013;75:462–466. doi: 10.1016/j.jpsychores.2013.08.008. [DOI] [PubMed] [Google Scholar]