Association of Age and Sex With Myocardial Infarction Symptom Presentation and In-Hospital Mortality (original) (raw)
. Author manuscript; available in PMC: 2015 Jul 7.
Published in final edited form as: JAMA. 2012 Feb 22;307(8):813–822. doi: 10.1001/jama.2012.199
Abstract
Context
Women are generally older than men at hospitalization for myocardial infarction (MI) and also present less frequently with chest pain/discomfort. However, few studies have taken age into account when examining sex differences in clinical presentation and mortality.
Objective
To examine the relationship between sex and symptom presentation and between sex, symptom presentation, and hospital mortality, before and after accounting for age in patients hospitalized with MI.
Design, Setting, and Patients
Observational study from the National Registry of Myocardial Infarction, 1994-2006, of 1 143 513 registry patients (481 581 women and 661 932 men).
Main Outcome Measures
We examined predictors of MI presentation without chest pain and the relationship between age, sex, and hospital mortality.
Results
The proportion of MI patients who presented without chest pain was significantly higher for women than men (42.0% [95% CI, 41.8%-42.1%] vs 30.7% [95% CI, 30.6%-30.8%]; P< .001). There was a significant interaction between age and sex with chest pain at presentation, with a larger sex difference in younger than older patients, which became attenuated with advancing age. Multivariable adjusted age-specific odds ratios (ORs) for lack of chest pain for women (referent, men) were younger than 45 years, 1.30 (95% CI, 1.23-1.36); 45 to 54 years, 1.26 (95% CI, 1.22-1.30); 55 to 64 years, 1.24 (95% CI, 1.21-1.27); 65 to 74 years, 1.13 (95% CI, 1.11-1.15); and 75 years or older, 1.03 (95% CI, 1.02-1.04). Two-way interaction (sex and age) on MI presentation without chest pain was significant (P<.001). The in-hospital mortality rate was 14.6% for women and 10.3% for men. Younger women presenting without chest pain had greater hospital mortality than younger men without chest pain, and these sex differences decreased or even reversed with advancing age, with adjusted OR for age younger than 45 years, 1.18 (95% CI, 1.00-1.39); 45 to 54 years, 1.13 (95% CI, 1.02-1.26); 55 to 64 years, 1.02 (95% CI, 0.96-1.09); 65 to 74 years, 0.91 (95% CI, 0.88-0.95); and 75 years or older, 0.81 (95% CI, 0.79-0.83). The 3-way interaction (sex, age, and chest pain) on mortality was significant (P< .001).
Conclusion
In this registry of patients hospitalized with MI, women were more likely than men to present without chest pain and had higher mortality than men within the same age group, but sex differences in clinical presentation without chest pain and in mortality were attenuated with increasing age.
Optimal Recognition and timely management of myocardial infarction (MI), especially for reducing patient delay in seeking acute medical care, is critical. The presence of chest pain/discomfort is the hallmark symptom of MI. Despite this well-accepted phenomenon, previous analyses from the National Registry of Myocardial Infarction (NRMI) have demonstrated that a large number of patients with MI lack chest pain/discomfort at presentation.1 Furthermore, patients without chest pain/discomfort tend to present later, are treated less aggressively, and have almost twice the short-term mortality compared with those presenting with more typical symptoms of MI.1 In addition, younger women with MI may have higher mortality risk than men,2,3 and the lack of chest pain/discomfort may contribute to that risk. Thus, we sought to answer the question of whether lack of chest pain was associated with the higher mortality observed in younger women with MI.
Women are generally older than men at hospitalization for MI. It is plausible that women's older age at presentation is related to whether they present with chest pain, as well as subsequent hospital mortality. However, a limited number of studies have taken age into account in examining sex differences in MI clinical presentation.4 This analysis from a large and clinically rich NRMI database aims to examine the relationship among patients hospitalized with MI between sex and symptom presentation (primary objective) and sex, symptom presentation, and hospital mortality (secondary objective), after accounting for age.
Methods
Patient Population and Data Collection
The NRMI is an industry-sponsored national registry, the largest of its kind in the world, collecting, analyzing, and reporting hospital data on 2 160 671 patients admitted with confirmed MI at 1977 participating hospitals from 1994-2006. Because the NRMI was a quality improvement initiative and patient information was deidentified, it was exempt from the requirement of institutional review board approval of data collection unless required by the local hospital.
In the NRMI, the diagnosis of acute MI was based on a clinical presentation (ischemic symptoms) consistent with acute MI and was determined by trained health care providers at each local hospital. This primarily involved an International Classification of Diseases, Ninth Revision, Clinical Modification diagnosis code of 410.X1 or supporting evidence of MI, to include elevated cardiac biomarker level, electrocardiographic evidence of acute MI, or alternative enzymatic, nuclear cardiac imaging, or autopsy evidence indicative of acute MI. No independent on-site validation of acute MI was performed, although case ascertainment and clinical data were previously validated by comparison with the Medicare cohort of the NRMI and Medicare Cooperative Cardiovascular Project, the latter of which used detailed hospital record review.5
All transferred patients were excluded from the present analyses because of incomplete reporting at initial hospital or subsequent outcome. Also excluded were patients with missing information on sex, age, or symptom presentation and patients with a secondary diagnosis of MI.
Study Variables
Among patients presenting with acute MI, the only symptom recorded was presence/absence of chest pain/discomfort. Chest pain/discomfort was defined as any symptom of chest discomfort, sensation or pressure, or tightness; or arm, neck, or jaw pain occurring before hospital arrival or preceding a diagnosis of acute MI. The chest pain/discomfort variable was classified as present or absent before admission, during admission, or both and may have included (but was not limited to) patients presenting with shortness of breath, nausea/vomiting, palpitations, syncope, or cardiac arrest. However, in the absence of chest pain/discomfort, the specific symptom (other than chest pain/discomfort) was not abstracted from the medical record. In addition to sex and age, information on race/ethnicity and payer status was also collected. Race/ethnicity was determined by chart review of the admission profile and medical record by trained abstractors.
Statistical Methods
The descriptive results were displayed by the presence or absence of chest pain/discomfort, sex, and age dichotomized at 65 years. Differences between study groups were assessed by χ2 test for categorical variables, the t test for continuous variables, and the nonparametric Wilcoxon rank sum test for median comparisons. Age-specific analyses and multivariable adjusted regression models were developed to assess the factors associated with MI presentation without chest pain/discomfort. The overall population and 5 age intervals were examined: younger than 45 years, 45 to 54 years, 55 to 64 years, 65 to 74 years, and 75 years or older. Preexisting variables that may have preceded the development of presenting symptoms, including other baseline characteristics, cardiovascular risk factors, medical history, and cardiac history, were adjusted for in each model and are listed in Table 1.
Table 1. Characteristics of Patients With MI, With and Without Chest Pain/Discomfort, Stratified by Sex and Age: NRMI, 1994-2006.
| Variable | Age <65 y (n = 400 336) | Age ≥65 y (n = 743177) | ||||||
|---|---|---|---|---|---|---|---|---|
| Women Without Chest Pain (n = 27 370) | Women With Chest Pain (n = 80 929) | Men Without Chest Pain (n = 52 974) | Men With Chest Pain (n = 239 063) | Women Without Chest Pain (n = 174 786) | Women With Chest Pain (n = 198 496) | Men Without Chest Pain (n = 150 281) | Men With Chest Pain (n = 219 614) | |
| Demographic and baseline characteristics, % | ||||||||
| Age, mean (SD), y | 56.2 (6.1) | 54.6 (6.3) | 55.2 (6.2) | 53.5 (6.3) | 80.5 (7.3) | 78.3 (7.4) | 78.0 (7.2) | 75.5 (7.0) |
| Median (IQR) | 58.0 (52.0-62.0) | 55.0 (49.0-60.0) | 56.0 (50.0-61.0) | 54.0 (48.0-59.0) | 81.0 (75.0-87.0) | 78.0 (72.0-84.0) | 78.0 (72.0-84.0) | 75.0 (70.0-81.0) |
| Race/ethnicity | ||||||||
| White | 73.1 | 76.1 | 78.0 | 81.6 | 85.3 | 86.9 | 86.4 | 87.8 |
| Black | 17.5 | 15.3 | 11.2 | 8.2 | 7.8 | 6.3 | 5.8 | 4.4 |
| Hispanic | 2.6 | 4.2 | 3.5 | 4.4 | 4.3 | 2.7 | 4.4 | 3.0 |
| Asian | 2.3 | 1.4 | 1.6 | 1.8 | 2.1 | 1.4 | 2.3 | 1.7 |
| Other | 3.0 | 3.0 | 3.2 | 3.9 | 2.9 | 2.7 | 4.1 | 3.1 |
| Payer status | ||||||||
| Commercial/PPO | 34.5 | 40.0 | 41.5 | 46.2 | 19.8 | 19.7 | 21.9 | 22.3 |
| HMO | 16.9 | 18.8 | 18.9 | 19.6 | 10.9 | 11.4 | 12.9 | 13.5 |
| Medicare | 21.0 | 12.5 | 17.3 | 9.2 | 86.5 | 84.5 | 83.5 | 80.7 |
| Medicaid | 17.4 | 12.3 | 8.8 | 5.3 | 8.2 | 6.1 | 4.6 | 3.2 |
| Self-pay | 10.3 | 12.5 | 10.6 | 13.1 | 1.3 | 1.3 | 1.5 | 1.6 |
| Weight, mean (SD), kg | 79.0 (24.1) | 80.7 (22.4) | 91.1 (23.8) | 92.6 (21.7) | 64.9 (18.1) | 68.5 (18.1) | 78.7 (18.9) | 82.6 (18.7) |
| Coronary heart disease risk factors, % | ||||||||
| Diabetes | 46.7 | 31.9 | 33.4 | 20.0 | 34.0 | 31.2 | 34.0 | 28.3 |
| Hypertension | 60.0 | 55.8 | 52.7 | 46.2 | 66.3 | 67.2 | 57.3 | 56.7 |
| Smoker | 34.5 | 48.0 | 39.2 | 49.7 | 8.8 | 11.5 | 12.7 | 15.3 |
| Dyslipidemia | 30.0 | 38.2 | 33.5 | 39.5 | 20.2 | 29.4 | 21.6 | 30.4 |
| Family history of CAD | 25.4 | 38.1 | 29.0 | 38.4 | 13.4 | 21.2 | 14.5 | 21.1 |
| Previous angina | 10.7 | 12.5 | 11.8 | 11.6 | 12.2 | 19.1 | 13.8 | 19.8 |
| Previous MI | 20.0 | 18.9 | 23.5 | 21.9 | 23.8 | 26.8 | 30.9 | 32.6 |
| Previous heart failure | 19.6 | 8.0 | 13.5 | 4.2 | 33.3 | 22.2 | 29.7 | 16.3 |
| Previous PCI | 8.4 | 11.2 | 10.9 | 14.0 | 5.2 | 9.3 | 8.1 | 14.0 |
| Previous CABG | 9.1 | 8.5 | 12.5 | 11.1 | 8.4 | 11.6 | 18.3 | 23.2 |
| Previous stroke | 10.1 | 5.1 | 7.5 | 3.2 | 17.3 | 11.7 | 17.5 | 10.7 |
| Presenting characteristics | ||||||||
| Systolic blood pressure, mean (SD), mm Hg | 140.3 (35.9) | 145.1 (32.1) | 139.8 (32.9) | 145.0 (29.6) | 141.0 (35.3) | 147.2 (33.4) | 137.4 (33.6) | 145.2 (31.9) |
| Pulse, mean (SD), beats/min | 96.7 (26.8) | 85.1 (21.8) | 91.7 (26.3) | 81.3 (20.6) | 95.5 (26.0) | 88.1 (23.9) | 93.5 (26.2) | 84.5 (23.8) |
| Symptom onset to arrival, mean (SD), h | 7.3 (11.8) | 5.1 (8.1) | 7.8 (12.4) | 4.6 (7.7) | 7.2 (11.7) | 5.6 (8.7) | 7.1 (11.8) | 5.1 (8.2) |
| Median (IQR) | 2.3 (1.0-8.0) | 2.1 (1.1-5.3) | 2.4 (1.0-8.6) | 1.9 (1.0-4.4) | 2.4 (1.0-7.3) | 2.5 (1.3-5.8) | 2.3 (1.0-7.2) | 2.2 (1.1-5.0) |
| Killip classification, % | ||||||||
| I | 67.2 | 87.3 | 74.7 | 91.2 | 54.1 | 69.5 | 56.7 | 75.5 |
| II | 18.1 | 8.4 | 14.1 | 6.0 | 28.6 | 20.9 | 27.2 | 17.0 |
| III | 12.1 | 3.3 | 8.7 | 2.0 | 15.5 | 8.3 | 14.0 | 6.2 |
| IV | 2.7 | 1.0 | 2.5 | 0.8 | 1.8 | 1.4 | 2.1 | 1.3 |
| Electrocardiogram, % | ||||||||
| ST-segment elevation | 21.6 | 43.1 | 24.6 | 50.3 | 18.0 | 35.8 | 16.0 | 35.9 |
| Left BBB | 5.3 | 2.5 | 4.4 | 1.8 | 10.6 | 8.1 | 10.3 | 7.2 |
| Right BBB | 4.0 | 2.4 | 5.3 | 3.5 | 6.6 | 5.6 | 11.1 | 9.3 |
| Type of MI, % | ||||||||
| STEMI | 37.9 | 54.9 | 40.1 | 61.6 | 38.1 | 52.9 | 36.8 | 52.3 |
| Non-STEMI | 62.1 | 45.1 | 59.9 | 38.4 | 61.9 | 47.1 | 63.2 | 47.7 |
| Location of MI, % | ||||||||
| Anterior | 21.6 | 23.6 | 20.9 | 24.9 | 20.2 | 24.4 | 17.7 | 22.7 |
| Lateral | 10.9 | 13.7 | 10.5 | 13.9 | 9.4 | 13.4 | 8.7 | 12.3 |
| Inferior | 21.6 | 35.8 | 26.5 | 41.2 | 16.5 | 27.7 | 17.5 | 29.5 |
| Right ventricle | 0.5 | 0.9 | 0.5 | 0.8 | 0.4 | 0.7 | 0.3 | 0.6 |
| Mortality, % | 16.1 | 3.7 | 12.5 | 2.4 | 21.2 | 13.0 | 22.0 | 6.6 |
We calculated the odds ratio (OR) for MI presentation without chest pain/discomfort in each age stratum for women compared with men (reference group). A 2-way interaction term was calculated between sex and age. Sensitivity analyses were performed by restricting the analysis to ST-segment elevation myocardial infarction (STEMI) cohort and by excluding patients who died within 24 hours and 48 hours.
Similarly, age-specific multivariable logistic regression models were used to assess sex differences in hospital mortality. Multivariable adjusted hospital case-fatality rates were determined within 5 age intervals. To assess the interaction of sex and symptom presentation, the following 4 dummy variables were created: men who presented without chest pain/discomfort, women who presented without chest pain/discomfort, women who presented with chest pain/discomfort, and men who presented with chest pain/discomfort (reference group). Variables were entered into a stepwise model that included comorbidities and clinical characteristics, prehospital delay, hospital characteristics (Table 1 and Table 2), medications and invasive procedures (Table 3), and the year the patient was enrolled in the study (to account for temporal trends in care and definition of MI). Two-tailed tests were used and _P_≤.001 was considered to be statistically significant. All statistical analyses were conducted with SAS version 9.13.
Table 2. Hospital Characteristics, Stratified by Patient Sex and Age: NRMI, 1994-2006.
| Hospital Characteristics, % | Age <65 y (n = 400 336) | Age ≥65 y (n = 743177) | ||||||
|---|---|---|---|---|---|---|---|---|
| Women Without Chest Pain (n = 27 370) | Women With Chest Pain (n = 80 929) | Men Without Chest Pain (n = 52 974) | Men With Chest Pain (n = 239 063) | Women Without Chest Pain (n = 174 786) | Women With Chest Pain (n = 198 496) | Men Without Chest Pain (n = 150 281) | Men With Chest Pain (n = 219 614) | |
| Bed size | ||||||||
| <151 | 14.6 | 11.0 | 13.1 | 10.5 | 20.6 | 17.1 | 19.4 | 15.1 |
| 151-250 | 21.7 | 20.8 | 21.5 | 20.3 | 24.3 | 23.2 | 24.0 | 22.7 |
| >250 | 63.7 | 68.2 | 65.4 | 69.2 | 55.1 | 59.8 | 56.6 | 62.2 |
| Census region | ||||||||
| West | 22.9 | 23.1 | 25.0 | 25.4 | 23.0 | 24.2 | 25.5 | 27.2 |
| South | 33.6 | 35.9 | 32.7 | 34.4 | 27.4 | 30.1 | 26.8 | 30.2 |
| Midwest | 30.0 | 30.6 | 29.5 | 29.9 | 29.9 | 29.7 | 29.5 | 28.5 |
| Northeast | 13.4 | 10.4 | 12.8 | 10.2 | 19.8 | 15.9 | 18.2 | 14.1 |
| Facility type | ||||||||
| Noninvasive | 9.7 | 5.4 | 8.4 | 4.8 | 16.7 | 11.9 | 15.3 | 9.8 |
| Catheterization | 18.6 | 12.2 | 15.0 | 10.1 | 22.8 | 17.9 | 20.8 | 15.0 |
| Catheterization/PCI/open heart surgery | 65.9 | 76.5 | 71.5 | 79.6 | 54.2 | 64.7 | 58.0 | 70.1 |
| Catheterization/PCI | 5.8 | 5.9 | 5.1 | 5.5 | 6.3 | 5.5 | 5.9 | 5.0 |
| Teaching hospital | 15.3 | 15.5 | 15.1 | 14.8 | 11.1 | 11.5 | 11.7 | 11.9 |
| Urban hospital | 91.0 | 92.8 | 92.1 | 93.3 | 88.2 | 89.0 | 88.7 | 90.3 |
| MI volume/y | 285.6 | 312.9 | 304.5 | 322.4 | 256.2 | 277.3 | 268.5 | 296.3 |
Table 3. Process of Care for MI Patients With and Without Chest Pain, Stratified by Sex and Age: NRMI, 1994-2006.
| Variable | Age <65 y (n = 400 336) | Age ≥65 y (n = 743 177) | ||||||
|---|---|---|---|---|---|---|---|---|
| Women Without Chest Pain (n = 27 370) | Women With Chest Pain (n = 80 929) | Men Without Chest Pain (n = 52 974) | Men With Chest Pain (n = 239 063) | Women Without Chest Pain (n = 174 786) | Women With Chest Pain (n = 198 496) | Men Without Chest Pain (n = 150 281) | Men With Chest Pain (n = 219 614) | |
| Initial reperfusion among eligible candidates, % | ||||||||
| Fibrinolytic treatment | 17.4 | 42.2 | 18.0 | 43.6 | 8.9 | 31.7 | 9.5 | 34.4 |
| Primary PCI | 16.3 | 31.9 | 21.7 | 36.3 | 5.9 | 19.3 | 7.8 | 24.2 |
| Immediate CABG | 0.6 | 0.9 | 1.2 | 1.3 | 0.3 | 0.8 | 0.6 | 1.3 |
| Any reperfusion | 34.6 | 75.3 | 41.4 | 81.5 | 15.2 | 52.0 | 18.1 | 60.2 |
| Intervals after hospital arrival | ||||||||
| First electrocardiogram, mean (SD), min | 34.2 (33.2) | 18.1 (21.2) | 28.8 (31.1) | 13.8 (17.4) | 34.4 (32.9) | 18.4 (21.1) | 31.1 (31.7) | 15.5 (18.9) |
| Median (IQR) | 22.0 (10.0-48.0) | 11.0 (5.0-22.0) | 17.0 (8.0-39.0) | 9.0 (4.0-16.0) | 23.0 (10.0-48.0) | 12.0 (6.0-22.0) | 20.0 (9.0-42.0) | 10.0 (5.0-19.0) |
| Fibrinolytic treatment, mean (SD), min | 81.2 (83.2) | 49.5 (49.2) | 61.6 (64.7) | 42.5 (42.2) | 80.2 (77.6) | 54.0 (52.3) | 72.8 (75.3) | 48.9 (47.4) |
| Median (IQR) | 56.0 (36.0-100.0) | 38.0 (26.0-58.0) | 44.0 (27.0-75.0) | 33.0 (22.0-50.0) | 60.0 (37.0-97.0) | 42.0 (29.0-64.0) | 52.0 (32.0-88.0) | 38.0 (25.0-58.0) |
| Primary PCI, mean (SD), min | 153.3 (115.4) | 121.4 (95.8) | 140.2 (121.6) | 110.6 (82.5) | 155.6 (113.1) | 126.5 (92.4) | 151.4 (121.2) | 121.0 (92.3) |
| Median (IQR) | 126.0 (94.0-175.0) | 102.0 (78.0-136.0) | 112.0 (83.0-156.0) | 95.0 (73.0-124.0) | 129.0 (93.0-181.0) | 107.0 (82.0-141.0) | 123.0 (90.0-175.0) | 102.5 (79.0-136.0) |
| Medications within 24 h, % | ||||||||
| Overall | ||||||||
| Aspirin/antiplatelets | 72.1 | 90.7 | 77.9 | 93.2 | 68.3 | 85.1 | 69.7 | 87.4 |
| Heparin | 51.0 | 74.0 | 55.8 | 78.7 | 39.2 | 63.5 | 42.2 | 67.8 |
| β-Blocker | 46.6 | 64.6 | 53.8 | 68.4 | 42.0 | 56.8 | 41.6 | 57.8 |
| Calcium blocker | 16.2 | 13.6 | 14.3 | 10.2 | 18.2 | 18.0 | 16.9 | 16.0 |
| ACE inhibitor | 27.5 | 26.0 | 27.0 | 25.5 | 29.6 | 28.8 | 28.3 | 29.6 |
| STEMI | ||||||||
| Aspirin/antiplatelets | 68.2 | 91.3 | 75.4 | 93.7 | 66.1 | 85.5 | 66.6 | 87.9 |
| Heparin | 60.8 | 84.3 | 64.9 | 86.4 | 47.2 | 74.1 | 49.8 | 78.2 |
| β-Blocker | 42.1 | 63.5 | 50.4 | 68.1 | 36.7 | 54.3 | 36.7 | 55.7 |
| Calcium blocker | 13.0 | 10.5 | 11.1 | 8.0 | 14.7 | 13.6 | 13.9 | 12.1 |
| ACE inhibitor | 23.9 | 24.4 | 23.6 | 24.9 | 27.2 | 26.4 | 25.9 | 25.6 |
| Non-STEMI | ||||||||
| Aspirin/antiplatelets | 74.5 | 90.0 | 79.5 | 92.5 | 69.7 | 84.7 | 71.5 | 86.9 |
| Heparin | 45.0 | 61.3 | 49.6 | 66.3 | 34.2 | 51.6 | 37.9 | 56.4 |
| β-Blocker | 49.3 | 65.8 | 56.2 | 68.7 | 45.2 | 59.7 | 44.4 | 60.1 |
| Calcium blocker | 18.2 | 17.3 | 16.4 | 13.7 | 20.3 | 23.0 | 18.6 | 20.3 |
| ACE inhibitor | 29.8 | 27.9 | 29.3 | 26.5 | 31.1 | 31.5 | 29.7 | 30.0 |
| Invasive cardiac procedures, % | ||||||||
| Overall | ||||||||
| Catheterization | 49.7 | 78.4 | 59.3 | 82.8 | 20.1 | 46.0 | 27.5 | 57.5 |
| PCI | 20.8 | 45.2 | 29.0 | 53.0 | 7.8 | 24.8 | 10.8 | 31.0 |
| CABG | 7.9 | 9.5 | 12.7 | 12.3 | 3.2 | 7.2 | 6.3 | 11.7 |
| STEMI | ||||||||
| Catheterization | 51.3 | 80.9 | 60.1 | 84.3 | 20.7 | 48.7 | 28.4 | 61.1 |
| PCI | 26.3 | 53.6 | 33.2 | 59.0 | 9.6 | 30.3 | 12.8 | 37.5 |
| CABG | 8.4 | 9.3 | 13.1 | 11.5 | 3.3 | 7.1 | 6.5 | 11.8 |
| Non-STEMI | ||||||||
| Catheterization | 48.8 | 75.4 | 58.8 | 80.3 | 19.7 | 43.0 | 27.0 | 53.5 |
| PCI | 17.5 | 34.9 | 26.1 | 43.4 | 6.8 | 18.6 | 9.6 | 23.7 |
| CABG | 7.6 | 9.6 | 12.4 | 13.6 | 3.2 | 7.4 | 6.3 | 11.7 |
Results
Study Population
NRMI enrolled 2 160 671 patients between 1994 and 2006. After the exclusion of 901 375 transfer patients, 68 768 patients with a secondary diagnosis of MI, and 47 015 patients with missing age, sex, or symptom presentation information, our final study population included 1 143 513 MI patients. Of these, 481 581 (42.1%) were women. Women with MI were significantly older than men at hospital presentation: mean age 73.9 vs 66.5 years (SD, 12.4 vs 13.2 years), respectively (P< .001).
Baseline, Presenting, and Hospital Characteristics
Table 1 and Table 2 show the baseline, presenting, and hospital characteristics of the study patients, further stratified by the presence/absence of chest pain/discomfort and by sex and age; these characteristics were used in our multivariable models to probe potential explanations for sex differences in chest pain presentation and mortality. Myocardial infarction patients without chest pain/discomfort were more likely to have diabetes and delay hospital arrival, irrespective of age or sex, and were more likely to present with Killip classification III and IV. Myocardial infarction patients with chest pain/discomfort were more likely to present with STEMI and anterior MI, and those without chest pain/discomfort were more likely to present with non-STEMI, irrespective of age and sex.
Processes of Care and Treatments
Myocardial infarction patients without chest pain/discomfort were less likely to receive any acute reperfusion therapies such as fibrinolytic therapies or primary percutaneous coronary intervention and were significantly less likely to receive these lifesaving therapies in a timely manner compared with the MI cohort with chest pain/discomfort (P<.001) (Table 3). In addition, this same cohort was less likely to receive aspirin, other antiplatelet agents, heparin, and β-blocker therapies during hospitalization, which was especially evident in the older cohort (>65 years). Myocardial infarction patients with chest pain/discomfort were more likely to receive cardiac catheterization and any percutaneous coronary intervention, which was especially evident among men and women younger than 65 years. However, coronary artery bypass graft surgery was more likely to be performed in men with chest pain/discomfort regardless of age or men without chest pain/discomfort who were younger than 65 years. Analysis of the medications and invasive procedures by MI type (STEMI and non-STEMI) did not yield any additional insights to that observed in the overall study population further stratified according to age and sex.
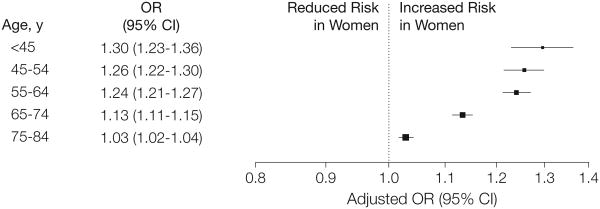
Sex Differences in MI Presentation Without Chest Pain/Discomfort
The overall proportion of MI patients who presented without chest pain/discomfort was 35.4% (95% CI, 35.4%-35.5%) and was significantly higher for women than men (42.0% vs 30.7%; 95% CI, 41.8%-42.1% vs 30.6%-30.8%; P<.001). Age-specific and multivariable analyses indicated a significant interaction between age and sex such that sex-specific differences in MI presentation without chest discomfort became progressively smaller with advancing age (Figure). Separate models were performed within each age stratum to calculate the age-stratum-specific OR of women vs men, which resulted in the following: younger than 45 years, 1.30 (95% CI, 1.23-1.36); 45 to 54 years, 1.26 (95% CI, 1.22-1.30); 55 to 64 years, 1.24 (95% CI, 1.21-1.27); 65 to 74 years, 1.13 (95% CI, 1.11-1.15); and 75 years or older, 1.03 (95% CI, 1.02-1.04). The statistical significance for trend of the OR by increasing age and for the interaction between sex and age was significant (P< .001).
Figure. Sex Differences in Myocardial Infarction Presentation Without Chest Pain/Discomfort, Stratified by Age.
P< .001 for all comparisons. In these multivariable models, candidate variables for inclusion in the model include demographics, baseline characteristics, cardiovascular risk factors, and medical history (Table 1). Separate adjusted models were performed within each age stratum to find the age-stratum-specific odds ratio (OR) for women vs men, and within each age stratum, the reference group was men.
Sensitivity analyses were performed to examine the potential influence of several factors pertinent to our results: the introduction of troponin assays in the registry by restricting the analysis to the STEMI cohort who would not be directly affected by this change in MI definition, and possible bias caused by earlier deaths (such as cardiac arrest) and potential for incomplete symptom characterization in this group by excluding individuals who died within 24 hours and 48 hours. In each case, the results from the sensitivity analyses on symptom presentation did not change materially, and the adjusted sex-specific differences in MI presentation without chest discomfort were evident and became progressively smaller with advancing age (Tables 4 and 5).
Table 4. Differences in MI Presentation Without Chest Pain Among Patients Receiving a Diagnosis of MI, Crude Proportions Stratified by Age and Sex: NRMI, 1994-2006.
| Patients, % | |||
|---|---|---|---|
| Age, y | No. | Chest Pain/Discomfort (n = 738 102) | No Chest Pain/Discomfort (n = 405 411) |
| Overall | |||
| <45 | 66 540 | 85.8 | 14.2 |
| 45-54 | 132 777 | 82.9 | 17.1 |
| 55-64 | 201 019 | 76.1 | 23.9 |
| 65-74 | 267 480 | 65.2 | 34.8 |
| 75-84 | 475 697 | 51.3 | 48.7 |
| Women | |||
| <45 | 15 236 | 81.5 | 18.5 |
| 45-54 | 31 899 | 78.4 | 21.6 |
| 55-64 | 61 164 | 71.1 | 28.9 |
| 65-74 | 107 877 | 62.1 | 37.9 |
| 75-84 | 265 405 | 49.6 | 50.4 |
| Men | |||
| <45 | 51 304 | 87.0 | 13.0 |
| 45-54 | 100 878 | 84.3 | 15.7 |
| 55-64 | 139 855 | 78.2 | 21.8 |
| 65-74 | 159 603 | 67.3 | 32.7 |
| 75-84 | 210 292 | 53.4 | 46.6 |
Table 5. Sex Differences in MI Presentation Without Chest Pain Among Patients Receiving a Diagnosis of MI, Stratified by Age: NRMI, 1994-2006a.
| Odds Ratio (95% CI) Stratified by Age, y | |||||
|---|---|---|---|---|---|
| <45 | 45-54 | 55-64 | 65-74 | 75-84 | |
| Women vs men | |||||
| Unadjusted odds ratio | 1.53 (1.45-1.60) | 1.48 (1.43-1.53) | 1.46 (1.43-1.49) | 1.26 (1.24-1.28) | 1.17 (1.15-1.18) |
| Adjusted odds ratio | 1.30 (1.23-1.36) | 1.26 (1.22-1.30) | 1.24 (1.21-1.27) | 1.13 (1.11-1.15) | 1.03 (1.02-1.04) |
| ST-segment elevation myocardial infarction only | 1.45 (1.34-1.56) | 1.30 (1.24-1.37) | 1.32 (1.28-1.37) | 1.15 (1.12-1.18) | 1.05 (1.03-1.07) |
| After excluding patients who died within 24 h | 1.40 (1.30-1.52) | 1.28 (1.22-1.35) | 1.31 (1.26-1.36) | 1.15 (1.12-1.18) | 1.06 (1.04-1.08) |
| After excluding patients who died within 48 h | 1.38 (1.27-1.50) | 1.27 (1.20-1.34) | 1.30 (1.25-1.35) | 1.15 (1.12-1.18) | 1.06 (1.04-1.08) |
Adjusted Hospital Case-Fatality Rates by Chest Pain/Discomfort on Presentation, Age, and Sex
The in-hospital mortality rate was 14.6% for women and 10.3% for men. In the fully adjusted models, younger women presenting without chest pain/discomfort had greater hospital case-fatality rates than men, a trend that reversed with increasing age (Table 6). This may be more clearly depicted in examination of the fully adjusted model when the reference group is men without chest pain. However, younger women presenting with chest pain/discomfort had a greater hospital case-fatality rate than men with chest pain/discomfort in the same age group, but differences in hospital death rates between men and women decreased with advancing age (no longer significant in the oldest group). The 3-way interaction (sex, age, and chest pain) on mortality was significant (P< .001). These data suggest that the absence of chest pain may be a more important predictor of death in younger women with MI compared with other similarly aged groups.
Table 6. Hospital Mortality for Myocardial Infarction Patients, by Chest Pain/Discomfort on Presentation, Age, and Sex: NRMI, 1994-2006a.
| Age, y | Men With Chest Pain | Women With Chest Pain | Men Without Chest Pain | Women Without Chest Pain | P Value |
|---|---|---|---|---|---|
| Crude rate, No. (%) | |||||
| <45(n = 66540) | 562/44 651 (1.3) | 246/12 413 (2.0) | 679/6653 (10.2) | 432/2823 (15.3) | <.001 |
| 45-54 (n = 132 777) | 1476/85 029 (1.7) | 679/25 006 (2.7) | 1680/15 849 (10.6) | 997/6893 (14.5) | |
| 55-64 (n = 201 019) | 3621/109 383 (3.3) | 2066/43 510 (4.7) | 4254/30 472 (14.0) | 2974/17 654 (16.8) | |
| 65-74 (n = 267 480) | 7378/107 347 (6.9) | 5746/66 942 (8.6) | 9888/52 256 (18.9) | 7891/40 935) (19.3) | |
| ≥75(n = 475 697) | 15 330/112 267 (13.7) | 19 962/131 554 (15.2) | 23 148/98 025 (23.6) | 29 141/133 851 (21.8) | |
| Unadjusted OR (95% CI) | c Statistic | ||||
| <45 | 1 [Reference] | 1.59 (1.36-1.85) | 8.92 (7.95-10.00) | 14.17 (12.42-16.17) | .74 |
| 45-54 | 1 [Reference] | 1.58 (1.44-1.73) | 6.71 (6.24-7.21) | 9.57 (8.80-10.42) | .72 |
| 55-64 | 1 [Reference] | 1.46 (1.38-1.54) | 4.74 (4.52-4.96) | 5.92 (5.62-6.23) | .69 |
| 65-74 | 1 [Reference] | 1.27 (1.23-1.32) | 3.16 (3.06-3.27) | 3.24 (3.13-3.35) | .64 |
| ≥75 | 1 [Reference] | 1.13 (1.11-1.16) | 1.95 (1.91-2.00) | 1.76 (1.72-1.80) | .57 |
| Adjusted OR (95% CI) | |||||
| Comorbidity and admission clinical characteristics | |||||
| <45 | 1 [Reference] | 1.26 (16-1.49) | 4.71 (4.08-5.43) | 5.51 (4.63-6.56) | .90 |
| 45-54 | 1 [Reference] | 1.33 (1.20-1.47) | 3.78 (3.46-4.12) | 4.37 (3.92-4.87) | .88 |
| 55-64 | 1 [Reference] | 1.26 (1.18-1.34) | 3.11 (2.94-3.29) | 3.22 (3.02-3.44) | .84 |
| 65-74 | 1 [Reference] | 1.13 (1.09-1.18) | 2.43 (2.34-2.52) | 2.23 (2.14-2.32) | .78 |
| ≥75 | 1 [Reference] | 0.99 (0.97-1.02) | 1.76 (1.72-1.81) | 1.43 (1.39-1.46) | .72 |
| Above plus patient delay | |||||
| <45 | 1 [Reference] | 1.26 (1.07-1.50) | 4.41 (3.81-5.11) | 5.13 (4.29-6.13) | .91 |
| 45-54 | 1 [Reference] | 1.34 (1.21-1.48) | 3.48 (3.18-3.81) | 4.01 (3.59-4.48) | .88 |
| 55-64 | 1 [Reference] | 1.26 (1.18-1.34) | 2.82 (2.67-2.99) | 2.92 (2.73-3.12) | .84 |
| 65-74 | 1 [Reference] | 1.13 (1.09-1.18) | 2.21 (2.13-2.29) | 2.03 (1.95-2.12) | .78 |
| ≥75 | 1 [Reference] | 0.99 (0.97-1.02) | 1.61 (1.57-1.65) | 1.30 (1.27-1.34) | .72 |
| Above plus hospital characteristics | |||||
| <45 | 1 [Reference] | 1.27 (1.07-1.51) | 4.30 (3.71-4.98) | 5.07 (4.24-6.07) | .91 |
| 45-54 | 1 [Reference] | 1.32 (1.19-1.46) | 3.38 (3.09-3.70) | 3.83 (3.43-4.28) | .88 |
| 55-64 | 1 [Reference] | 1.25 (1.18-1.33) | 2.75 (2.60-2.91) | 2.82 (2.64-3.01) | .84 |
| 65-74 | 1 [Reference] | 1.13 (1.08-1.17) | 2.16 (2.07-2.24) | 1.97 (1.89-2.06) | .78 |
| ≥75 | 1 [Reference] | 0.99 (0.96-1.01) | 1.59 (1.55-1.64) | 1.29 (1.25-1.32) | .72 |
| Final adjusted model (above plus treatments) | |||||
| <45 | 1 [Reference] | 1.28 (1.07-1.52) | 2.87 (2.44-3.39) | 3.06 (2.51-3.73) | .93 |
| 45-54 | 1 [Reference] | 1.26 (1.13-1.40) | 2.25 (2.03-2.48) | 2.37 (2.10-2.68) | .91 |
| 55-64 | 1 [Reference] | 1.22 (1.15-1.30) | 1.88 (1.77-2.00) | 1.92 (1.79-2.06) | .88 |
| 65-74 | 1 [Reference] | 1.11 (1.06-1.16) | 1.60 (1.54-1.67) | 1.47 (1.40-1.53) | .83 |
| ≥75 | 1 [Reference] | 0.98 (0.95-1.00) | 1.32 (1.28-1.36) | 1.08 (1.05-1.11) | .77 |
| Adjusted model (above minus treatments) | |||||
| <45 | 0.23 (0.20-0.27) | 0.30 (0.25-0.35) | 1 [Reference] | 1.18 (1.00-1.39) | .91 |
| 45-54 | 0.30 (0.27-0.32) | 0.39 (0.35-0.44) | 1 [Reference] | 1.13 (1.02-1.26) | .88 |
| 55-64 | 0.36 (0.34-0.39) | 0.46 (0.43-0.49) | 1 [Reference] | 1.02 (0.96-1.09) | .84 |
| 65-74 | 0.46 (0.45-0.48) | 0.52 (0.50-0.54) | 1 [Reference] | 0.91 (0.88-0.95) | .78 |
| ≥75 | 0.63 (0.61-0.64) | 0.62 (0.60-0.63) | 1 [Reference] | 0.81 (0.79-0.83) | .72 |
| Final adjusted model (above plus treatments) | 1 [Reference] | ||||
| <45 | 0.35 (0.30-0.41) | 0.44 (0.37-0.54) | 1 [Reference] | 1.07 (0.89-1.27) | .93 |
| 45-54 | 0.45 (0.40-0.49) | 0.56 (0.50-0.63) | 1 [Reference] | 1.06 (0.95-1.18) | .91 |
| 55-64 | 0.53 (0.50-0.57) | 0.65 (0.61-0.70) | 1 [Reference] | 1.02 (0.96-1.09) | .88 |
| 65-74 | 0.62 (0.60-0.65) | 0.69 (0.66-0.72) | 1 [Reference] | 0.91 (0.88-0.95) | .83 |
| ≥75 | 0.76 (0.74-0.78) | 0.74 (0.72-0.76) | 1 [Reference] | 0.82 (0.80-0.84) | .77 |
In the stepwise modeling, adjustment for comorbidity and clinical characteristics clearly accounted for the majority of excess mortality in younger women and younger men without chest pain/discomfort. Further adjustments for patient delay or hospital characteristics had little influence on sex-specific mortality differences by age. In contrast, adjustment for treatments (initial medications within 24 hours and invasive cardiac procedures) accounted for a modest excess of mortality in the MI cohort without chest pain/discomfort, which was most evident among women younger than 55 years.
Comment
To our knowledge, this analysis represents the largest study to date examining the relationship of age and sex to the presence or absence of chest pain/discomfort at admission for MI and index hospital survival. Overall, women with MI were more likely than men to present without chest pain/discomfort. Adjusted sex differences in presentation without chest pain/discomfort were more pronounced in younger MI patients, a finding that became attenuated and nearly disappeared with increasing age. Our data also suggest that the absence of chest pain is associated with increased mortality, especially among younger women with MI, and may explain in part the excess mortality risk in this high-risk group. In fact, younger women presenting without chest pain/discomfort had higher hospital death rates than similarly aged men, but this finding reversed with increasing age.
Previous studies have suggested that women may have a different symptom presentation than men with MI, typically with more nonspecific acute symptoms and fewer “classic” ones.4,6 However, many studies lacked standardization for characterizing MI presentation, data collection, and reporting on women's symptoms, making it difficult to provide definitive conclusions or recommendations.4 In addition, although women are generally older than men when they experience MI, a limited number of studies have had a sufficient population to fully adjust for the effect of age when explaining sex-based differences in clinical presentation.4
We observed sex differences in presenting symptoms of MI in the current study. Chest pain/discomfort was the most common symptom of MI in both women (58%) and men (69%); however, women, especially those younger than 45 years, were less likely to report chest pain/discomfort. Although there may be true differences in symptom presentation by age and sex, the first step in MI care is recognizing any significant new symptoms and seeking medical care promptly, rather than focusing on simplistic generalizations of MI symptom presentation among women and men.
Our results show that age is an important factor of sex-based differences in MI presentation, which is especially relevant because women are older than men when they present with an acute coronary syndrome. After simultaneous adjusting for age and sex, age may be a more important factor in MI presentation in the absence of chest pain/discomfort. This difference should be confirmed in other studies, ideally a prospectively designed observational investigation that includes careful inquiry into the symptoms associated with MI.
Although MI in women occurs predominantly in older age, previous reports (including one from the NRMI) have shown that MI occurring at a younger age is associated with a substantial risk of mortality in women compared with men, especially those younger than 60 years.2,3 In the current study, comorbidity, clinical characteristics, and, to a modest extent, differences in treatments accounted for the majority of excess mortality in MI patients without chest pain/discomfort, which was especially notable in women younger than 55 years. More recently, another NRMI study showed remarkable reductions in hospital mortality after MI during the past decade for both sexes, especially women, possibly in part because of better recognition and management of cardiovascular risk factors in women before acute MI.7 As a result, the sex gap revealing higher mortality of younger women compared with men, although still present, has substantially decreased.7
The reasons for sex-based differences in MI symptom presentation observed in our study are largely unknown. It is plausible, or even likely, that the pathophysiology or pathobiology of higher mortality observed in younger women also accounts for the apparent differences in MI symptom presentation in this premenopausal or middle-aged group.
A number of studies support a biological mechanism of sex-based differences in clinical presentation. For example, in the Framingham Heart Study, sex-based differences in initial clinical manifestations of coronary artery disease revealed that women were more likely to manifest with stable or unstable angina, and men were more likely to manifest with MI or sudden cardiac death.8-10 Epidemiologic data have indicated that women, on average, are almost a decade older than men at their initial MI11-14 and are relatively spared from clinically significant coronary artery disease up to age 75 years, possibly because of the protective effects of estrogen.8 However, women in whom coronary atherosclerosis develops before age 75 years may be predisposed to a particularly aggressive disease or may have more risk factors for coronary heart disease, which might override the protective effect of estrogen.2
These findings emphasize that premenopausal or middle-aged women and older women who experience MI may represent a heterogeneous group. Younger women who experience MI may have significantly less narrowing of the coronary arteries than older women or men,15-17 possibly because of a hypercoagulable state, inflammation, coronary spasm, or plaque erosion vs rupture.
Other investigators have hypothesized that differences between men and women in coronary artery disease presentation and prognosis may be explained by sex differences in cardiovascular risk factors.18-20 For example, the mechanisms of sudden coronary death appear to differ in older women compared with premenopausal or middle-aged women, and risk factors may play different roles in these groups of patients.21 Young women who die from coronary artery thrombosis are often smokers with plaque erosions and relatively little coronary narrowing, whereas older women who die from coronary artery thrombosis often have high cholesterol levels and subsequent plaque rupture, with relatively severe coronary narrowing. Although the pathobiological mechanisms underlying sex-based differences in the descriptive epidemiology of coronary artery disease are intriguing, their relevance in explaining sex differences in symptom presentation with MI remains unclear.
Further research is needed to enhance the current understanding of underlying pathophysiology and potentially sex-tailored health messages to the general public and health care providers to encourage men and women with signs and symptoms of acute coronary syndromes to seek care promptly, with resultant improvements in the care and survival of women. Our results of sex-based differences in MI symptom presentation in younger patients are provocative and should be confirmed by others with clinical databases of MI or acute coronary syndromes. From a public health perspective, it is appropriate to target high-risk groups for delay (young women) with information on the American Heart Association/National Institutes of Health heart attack message, but until additional research is conducted, the current chest pain/discomfort heart attack symptom message, which targets women and men equally irrespective of age, should remain unchanged.
Our study had several limitations. The NRMI patients and hospitals enrolled may not be representative of all MI patients and hospitals in the United States. The NRMI is an observational study, and our results may be limited by various biases and unmeasured or inadequately measured potential confounders. Patients who died before hospital arrival were not included in our study and do not compromise our overall finding of age and sex differences in acute symptom presentation among those who presented to the hospital. The description of other MI symptoms in the absence of chest pain/discomfort was not identified in our data set. We did not have a cohort of patients without MI with which to compare symptom presentation and thus cannot generalize our findings to all patients with suspected acute coronary syndrome. Ascertainment of symptoms was obtained through medical record review, with a lack of standardization for the collection and recording of these data at participating study hospitals. In addition, the latest universal definition of MI, which was updated in 2007 to include 5 separate MI categories,22 was not available during the era of NRMI 2 to 5 (1994-2006). The current report included data from 1994-2006, and the diagnosis and treatment of acute MI have changed substantially during that time.
Conclusions
Women were more likely than men to present without chest pain and had higher mortality than men, especially among younger age groups, but sex differences in clinical presentation without chest pain and in mortality were attenuated with increasing age. Age is an important factor in examining sex differences in MI presentation and subsequent mortality. Further qualitative and quantitative research is needed to more fully clarify the development of premonitory and acute symptoms of coronary disease in men and women of different ages and the role of these symptoms in patients' care-seeking behavior and treatment practices, as well as in hospital and long-term outcomes.
Acknowledgments
Funding/Support: The National Registry of Myocardial Infarction was supported by Genentech.
Role of the Sponsors: The study sponsor approved the final manuscript but did not participate in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Footnotes
Author Contributions: Dr Canto had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Canto. Acquisition of data: Canto.
Analysis and interpretation of data: Canto, Rogers, Peterson, Wenger, Vaccarino, Kiefe, Frederick, Sopko, Zheng.
Drafting of the manuscript: Canto. Critical revision of the manuscript for important intellectual content: Canto, Rogers, Goldberg, Peterson, Wenger, Vaccarino, Kiefe, Frederick, Sopko, Zheng.
Statistical analysis: Canto, Peterson, Frederick. Supervision: Canto.
Conflict of Interest Disclosures: All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Dr Kiefe reports receiving partial funding from the National Institutes of Health (grants U01HL 105268 and U54 RR 026088). Mr Frederick reports being an employee of ICON Clinical Research, which received support from Genentech, to provide biostatistical and analytic services. Dr Peterson reported receiving research grants from Bristol-Myers Squibb, sanofi-aventis, Eli Lilly, Schering Plough/Merck, Johnson & Johnson, and St Jude Inc and consultant fees from Bayer and Pfizer. Dr Wenger reported receiving research grants and/or trial committee or data and safety monitoring board compensation from Pfizer, Merck, NHLBT, Gilead Sciences, Abbott, and Eli Lilly; she also reported receiving consultant fees from Gilead Sciences, AstraZeneca, Abbott Women's Advisory Board, Merck, and Pfizer.
Online-Only Material: The Author Video Interview is available at http://www.jama.com.
Publisher's Disclaimer: Disclaimer: The views expressed in this article are those of the authors and do not necessarily reflect the opinions of the funding organizations. Dr Peterson, a contributing editor for JAMA, was not involved in the editorial review of or decision to publish this article.
References
- 1.Canto JG, Shlipak MG, Rogers WJ, et al. Prevalence, clinical characteristics, and mortality among patients with myocardial infarction presenting without chest pain. JAMA. 2000;283(24):3223–3229. doi: 10.1001/jama.283.24.3223. [DOI] [PubMed] [Google Scholar]
- 2.Vaccarino V, Parsons L, Every NR, Barron HV, Krumholz HM National Registry of Myocardial Infarction 2 Participants. Sex-based differences in early mortality after myocardial infarction. N Engl J Med. 1999;341(4):217–225. doi: 10.1056/NEJM199907223410401. [DOI] [PubMed] [Google Scholar]
- 3.Vaccarino V, Krumholz HM, Yarzebski J, Gore JM, Goldberg RJ. Sex differences in 2-year mortality after hospital discharge for myocardial infarction. Ann Intern Med. 2001;134(3):173–181. doi: 10.7326/0003-4819-134-3-200102060-00007. [DOI] [PubMed] [Google Scholar]
- 4.Canto JG, Goldberg RJ, Hand MM, et al. Symptom presentation of women with acute coronary syndromes: myth vs reality. Arch Intern Med. 2007;167(22):2405–2413. doi: 10.1001/archinte.167.22.2405. [DOI] [PubMed] [Google Scholar]
- 5.Every NR, Frederick PD, Robinson M, Sugarman J, Bowlby L, Barron HV. A comparison of the National Registry of Myocardial Infarction 2 with the Cooperative Cardiovascular Project. J Am Coll Cardiol. 1999;33(7):1886–1894. doi: 10.1016/s0735-1097(99)00113-8. [DOI] [PubMed] [Google Scholar]
- 6.Shin JY, Martin R, Suls J. Meta-analytic evaluation of gender differences and symptom measurement strategies in acute coronary syndromes. Heart Lung. 2010;39(4):283–295. doi: 10.1016/j.hrtlng.2009.10.010. [DOI] [PubMed] [Google Scholar]
- 7.Vaccarino V, Parsons L, Peterson ED, Rogers WJ, Kiefe CI, Canto J. Sex differences in mortality after acute myocardial infarction: changes from 1994 to 2006. Arch Intern Med. 2009;169(19):1767–1774. doi: 10.1001/archinternmed.2009.332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lerner DJ, Kannel WB. Patterns of coronary heart disease morbidity and mortality in the sexes: a 26-year follow-up of the Framingham population. Am Heart J. 1986;111(2):383–390. doi: 10.1016/0002-8703(86)90155-9. [DOI] [PubMed] [Google Scholar]
- 9.Hochman JS, Tamis JE, Thompson TD, et al. Global Use of Strategies to Open Occluded Coronary Arteries in Acute Coronary Syndromes IIb Investigators. Sex, clinical presentation, and outcome in patients with acute coronary syndromes. N Engl J Med. 1999;341(4):226–232. doi: 10.1056/NEJM199907223410402. [DOI] [PubMed] [Google Scholar]
- 10.Hsia J, Aragaki A, Bloch M, LaCroix AZ, Wallace R WHI Investigators. Predictors of angina pectoris versus myocardial infarction from the Women's Health Initiative Observational Study. Am J Cardiol. 2004;93(6):673–678. doi: 10.1016/j.amjcard.2003.12.002. [DOI] [PubMed] [Google Scholar]
- 11.Chandra NC, Ziegelstein RC, Rogers WJ, et al. Observations of the treatment of women in the United States with myocardial infarction: a report from the National Registry of Myocardial Infarction-I. Arch Intern Med. 1998;158(9):981–988. doi: 10.1001/archinte.158.9.981. [DOI] [PubMed] [Google Scholar]
- 12.Maynard C, Every NR, Martin JS, Kudenchuk PJ, Weaver WD. Association of gender and survival in patients with acute myocardial infarction. Arch Intern Med. 1997;157(12):1379–1384. [PubMed] [Google Scholar]
- 13.Canto JG, Rogers WJ, Chandra NC, et al. National Registry of Myocardial Infarction 2 Investigators. The association of sex and payer status on management and subsequent survival in acute myocardial infarction. Arch Intern Med. 2002;162(5):587–593. doi: 10.1001/archinte.162.5.587. [DOI] [PubMed] [Google Scholar]
- 14.Blomkalns AL, Chen AY, Hochman JS, et al. CRUSADE Investigators. Gender disparities in the diagnosis and treatment of non-ST-segment elevation acute coronary syndromes: large-scale observations from the CRUSADE (Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes With Early Implementation of the American College of Cardiology/American Heart Association Guidelines) National Quality Improvement Initiative. J Am Coll Cardiol. 2005;45(6):832–837. doi: 10.1016/j.jacc.2004.11.055. [DOI] [PubMed] [Google Scholar]
- 15.Johansson S, Bergstrand R, Ulvenstam G, et al. Sex differences in preinfarction characteristics and longterm survival among patients with myocardial infarction. Am J Epidemiol. 1984;119(4):610–623. doi: 10.1093/oxfordjournals.aje.a113778. [DOI] [PubMed] [Google Scholar]
- 16.Albert CM, McGovern BA, Newell JB, Ruskin JN. Sex differences in cardiac arrest survivors. Circulation. 1996;93(6):1170–1176. doi: 10.1161/01.cir.93.6.1170. [DOI] [PubMed] [Google Scholar]
- 17.Burke AP, Farb A, Malcom GT, Liang Y, Smialek J, Virmani R. Effect of risk factors on the mechanism of acute thrombosis and sudden coronary death in women. Circulation. 1998;97(21):2110–2116. doi: 10.1161/01.cir.97.21.2110. [DOI] [PubMed] [Google Scholar]
- 18.Hochman JS, McCabe CH, Stone PH, et al. TIMI Investigators. Outcome and profile of women and men presenting with acute coronary syndromes: a report from TIMI IIIB. J Am Coll Cardiol. 1997;30(1):141–148. doi: 10.1016/s0735-1097(97)00107-1. [DOI] [PubMed] [Google Scholar]
- 19.Robinson K, Conroy RM, Mulcahy R, Hickey N. Risk factors and in-hospital course of first episode of myocardial infarction or acute coronary insufficiency in women. J Am Coll Cardiol. 1988;11(5):932–936. doi: 10.1016/s0735-1097(98)90048-1. [DOI] [PubMed] [Google Scholar]
- 20.Benderly M, Behar S, Reicher-Reiss H, Boyko V, Goldbourt U SPRINT Study Group. Long-term prognosis of women after myocardial infarction. Am J Epidemiol. 1997;146(2):153–160. doi: 10.1093/oxfordjournals.aje.a009246. [DOI] [PubMed] [Google Scholar]
- 21.Virmani R, Burke AP, Farb A, Kolodgie FD. Pathology of the vulnerable plaque. J Am Coll Cardiol. 2006;47(8 suppl):C13–C18. doi: 10.1016/j.jacc.2005.10.065. [DOI] [PubMed] [Google Scholar]
- 22.Thygesen K, Alpert JS, White HD, et al. Joint ESC/ACCF/AHA/WHF Task Force for the Redefinition of Myocardial Infarction. Universal definition of myocardial infarction. Circulation. 2007;116(22):2634–2653. doi: 10.1161/CIRCULATIONAHA.107.187397. [DOI] [PubMed] [Google Scholar]