Endosomal Proteolysis of the Ebola Virus Glycoprotein Is Necessary for Infection (original) (raw)
. Author manuscript; available in PMC: 2016 Mar 18.
Published in final edited form as: Science. 2005 Apr 14;308(5728):1643–1645. doi: 10.1126/science.1110656
Abstract
Ebola virus (EboV) causes rapidly fatal hemorrhagic fever in humans and there is currently no effective treatment. We found that the infection of African green monkey kidney (Vero) cells by vesicular stomatitis viruses bearing the EboV glycoprotein (GP) requires the activity of endosomal cysteine proteases. Using selective protease inhibitors and protease-deficient cell lines, we identified an essential role for cathepsin B (CatB) and an accessory role for cathepsin L (CatL) in EboV GP-dependent entry. Biochemical studies demonstrate that CatB and CatL mediate entry by carrying out proteolysis of the EboV GP subunit GP1 and support a multistep mechanism that explains the relative contributions of these enzymes to infection. CatB and CatB/CatL inhibitors diminish the multiplication of infectious EboV-Zaire in cultured cells and may merit investigation as anti-EboV drugs.
Ebola virus (EboV) is a member of the Filoviridae family of enveloped viruses with nonsegmented negative-sense RNA genomes (1). EboV infection is initiated by the fusion between viral and host cell membranes, which is mediated by the viral membrane glycoprotein (GP) (2, 3). Mature GP is a trimer of three disulfide-linked GP1-GP2 heterodimers that are generated by the proteolytic cleavage of the GP0 precursor polypeptide during virus assembly (4–6). The membrane-distal subunit, GP1, mediates viral adhesion to host cells and is proposed to regulate the transmembrane subunit GP2, which carries out membrane fusion (7–9). The processing and function of EboV GP are analogous to those of other type-I envelope glycoproteins, such as Env of the human immunodeficiency virus (HIV) and HA of the influenza virus (4, 7, 10–12). Current models of infection by these viruses (11) indicate that a specific signal within susceptible cells, such as receptor binding or exposure to acid pH, triggers the destabilization of intersubunit contacts, conformational rearrangement of the transmembrane subunits, and membrane fusion.
The triggering signal for the EboV GP1-GP2 trimer is unknown. Specifically, an essential EboV receptor analogous to CD4/CCR5 for HIV Env has not been identified (13). EboV infection is blocked by inhibitors of endosomal acidification (2, 3), indicating that this virus uses an acid-dependent pathway to enter cells. However, acid pH does not induce GP-dependent cell membrane fusion (8), as might be expected from studies of acid pH–triggered influenza virus and retroviruses (14, 15). These findings suggest the possibility that a critical host factor for EboV entry is dependent on acid pH. The nonenveloped mammalian reoviruses provide such a precedent: They require the activity of acid-dependent endosomal proteases to enter cells (16–18).
To test the possibility that acid-dependent endosomal proteases are also host factors for EboV GP-dependent entry, we assessed the capacity of broad-spectrum protease inhibitors to block infection by vesicular stomatitis virus (VSV) particles pseudotyped with EboV GP (VSV-GP). The cysteine protease inhibitor E-64d specifically reduced VSV-GP infection in Vero African green monkey kidney epithelial cells by >99.9% (fig. S1). A similar profile of inhibition was observed with more highly infectious VSV particles containing a form of EboV GP that lacks the mucin-like/variable (Muc) domain in GP1 (VSV-GPΔMuc) (6, 19). These findings indicate that one or more cysteine proteases in Vero cells are required for EboV GP-dependent entry.
Cathepsin B (CatB) and cathepsin L (CatL) are E-64d–sensitive cysteine proteases that are present in endosomes and lysosomes and are active at acid pH in the broad range of mammalian cells susceptible to EboV infection (2, 20, 21). To examine the roles of these enzymes, we studied the effect of a selective CatB inhibitor [CA074 (22)] and a CatL/CatB inhibitor [FYdmk (23)] on VSV-GPΔMuc infection of Vero cells. Infection was inhibited in a manner that correlated closely with the inactivation of CatB but not CatL (Fig. 1, A and B). We next measured VSV-GPΔMuc infectivity in murine embryo fibroblasts (MEFs) derived from wild-type and CatB-deficient (_CatB_−/− CatL+/+) mice (24, 25) (Fig. 1C). We observed a >90% reduction in EboV GPΔMuc-dependent infection of _CatB_−/− CatL+/+ MEFs but no reduction in infection dependent on VSV’s own glycoprotein (VSV G) (26). VSV-GPΔMuc infection was enhanced by the expression of CatB but not CatL. Together, these results indicate that CatB is an essential host factor for EboV GP-dependent entry.
Fig. 1.
Endosomal cysteine proteases CatB and CatL are host factors for VSV-GPΔMuc infection. (A and B) (Top) Effect of CatB-selective inhibitor CA074 (A) and CatL/CatB inhibitor FYdmk (B) on infectivities of VSV-G and VSV-GPΔMuc in Vero cells. (Bottom) CatB (A) and CatL (B) enzymatic activities in CA074- and FYdmk-treated Vero cells. Infectivities [infectious units (iu)/ml] are relative to the infectivity of the same virus in dimethyl sulfoxide (DMSO)–treated Vero cells (set to 100%) (25). (C) Wild-type (WT) and CatB-deficient (_CatB_−/− CatL+/+) MEFs were not transfected (none) or transfected with plasmid DNAs encoding β-galactosidase (β-gal), CatB (CatB), or CatL (CatL). After 24 hours, cells were exposed to VSV-GPΔMuc (~1 iu per cell), and the percentage of infected cells was determined 24 hours later by flow cytometry (25). (D) Capacity of VSV-GPΔMuc to infect CatB/CatL-deficient (_CatB_−/−_CatL_−/−) MEFs was determined as in (C). Infectivities from two replicates are shown in (A) and (B) and are representative of four independent experiments. Error bars, SD from at least three replicates.
The inactivation of both CatB and CatL with high concentrations of FYdmk (Fig. 1B) or with a combination of CA074 and FYdmk (fig. S5) inhibited VSV-GPΔMuc infection more effectively than did the inactivation of CatB alone with CA074 (Fig. 1A and table S1), suggesting a role for CatL in entry. To investigate this possibility, we measured VSV-GPΔMuc infectivity in MEFs derived from CatB/CatL-deficient (_CatB_−/−_CatL_−/−) mice (Fig. 1D) (27). We observed a >99% reduction in EboV GPΔMuc-dependent infection of _CatB_−/−_CatL_−/− MEFs but no reduction in VSV G–dependent infection (26). VSV-GPΔMuc infection was enhanced by the expression of CatB but not CatL, providing additional evidence for the essential role of CatB. Although CatL is neither necessary nor sufficient for entry, we observed a synergistic increase in infection upon coexpression of CatL with CatB, suggesting that CatL enhances infection by contributing to the CatB-dependent entry mechanism.
To further investigate the roles of CatB and CatL in EboV GP-dependent entry, we examined the effect of the purified enzymes on VSV-GPΔMuc at pH 5.5 and 37°C (Fig. 2, A and B). Both enzymes cleaved the GP1 subunit to yield an ~18-kD N-terminal fragment (GP118K); however, CatL mediated GP1→GP118K cleavage much more efficiently than did CatB under these selected conditions. After complete GP1→GP118K cleavage by CatL, VSV particles remained fully infectious and dependent on cellular CatB activity in Vero cells (Fig. 2C) and MEFs (26), indicating that GP1→ GP118K cleavage is not the step in entry that specifically requires CatB.
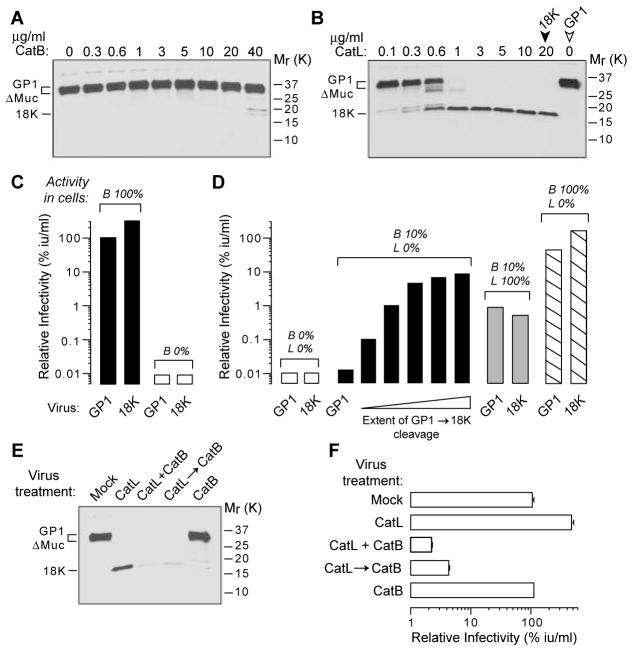
Fig. 2.
Endosomal cysteine proteases act directly on EboV GPΔMuc to mediate infection of Vero cells. (A and B) Purified CatB (A) and CatL (B) cleave GPΔMuc to GP118K. VSV-GPΔMuc was incubated with enzyme for 1 hour at pH 5.5 and 37°C. Mock-treated VSV particles containing GP1 (open arrowhead) and CatL-treated VSV particles containing GP118K (18K) (solid arrowhead) were used in (C) and (D). (C) VSV particles containing GP118K are highly infectious and fully dependent on cellular CatB activity. Cells were not treated (solid bars) or pretreated with E-64d (300 μM) (open bars) to inactivate CatB. Approximate CatB activity (B%) in these cells is indicated above the bars. (D) VSV particles containing GP118K bypass a block to GP1 cleavage within cells. Cells were treated with inhibitors to obtain the approximate levels of cellular CatB (B%) and CatL (L%) activity shown (also see Fig. 1 and table S1). Open bars, 300 μM E-64d; solid black bars, 10 μM FYdmk; solid gray bars, 40 μM CA074; striped bars, 1 μM FYdmk. Cells were then infected with VSV-GPΔMuc containing GP1 only, GP118K only, or increasing amounts of GP118K (wedge) (generated by incubation with increasing concentrations of CatL for 1 hour at pH 5.5 and 37°C). (E) Purified CatB efficiently digests CatL-derived GP118K. VSV-GPΔMuc was incubated with the indicated enzymes for 1 hour at pH 5.5 and 37°C {CatB, 40 μg/ml; CatL, 20 μg/ml; CatB and CatL together (CatB + CatL); or CatL followed by CatB [CatL→CatB (30 min each)]}. (F) Digestion of CatL-derived GP118K by CatB inactivates VSV-GPΔMuc. Infectivities of VSV particles from (E) are shown. Averages of two replicates are shown in (C) and (D) and are representative of three independent experiments. Error bars, SD from three replicates; _M_r, relative molecular weight in kilodaltons (K).
On the basis of these findings, we pursued the hypothesis that VSV particles containing GP118K are an intermediate in the CatB-dependent entry pathway. This hypothesis predicts that the GP118K-containing particles should bypass a block to infection of cells in which presumptive GP1 cleavage by cellular CatB and/or CatL is inhibited. Accordingly, we treated cells with inhibitor to reduce CatB activity to ~10% and CatL activity to undetectable levels, and we then challenged those cells with CatL-treated VSV particles containing increasing amounts of GP118K (Fig. 2D). Infection of these cells was enhanced in a GP118K-dependent manner, indicating that GP1 cleavage is an essential step in entry. In contrast, we observed little or no GP118K-dependent enhancement of infection in cells with ~100% CatL or ~100% CatB, indicating that the required intracellular cleavage of GP1 that is mimicked by in vitro GP1→GP118K cleavage is mediated by CatL and/or CatB.
VSV particles containing GP118K remain dependent on cellular CatB (Fig. 2, C and D), indicating the existence of a downstream CatB-dependent step. Purified CatB but not CatL efficiently digested CatL-derived GP118K to fragments not detected by immunoblot (Fig. 2E) and inactivated infectivity by >90% (Fig. 2F). More work is needed to uncover the mechanistic details of this CatB-dependent step, but our results are consistent with a simple model in which CatB-mediated digestion of GP118K in vitro inactivates VSV particles by relieving GP1-dependent constraints on GP2 and inducing premature deployment of the fusion machinery. In this scheme, EboV GP1 digestion by cellular CatB and CatL is functionally equivalent to fusion-triggering signals for other viruses, such as the binding of retroviruses to receptors (15) and the exposure of influenza virus to acidic pH (14, 25).
Taken together, our findings indicate that GP1 proteolysis by CatB and CatL during entry is a multistep process. We propose that this process is initiated by cleavages of GP1 by CatB and/or CatL to remove C-terminal sequences (figs. S3 and S4) (25) and to generate an N-terminal GP118K-like species, which is then digested by CatB to trigger membrane fusion and entry. Our data suggest that CatL contributes to infection, particularly when CatB activity is low, by virtue of its ability to mediate initial GP1 cleavages, but is insufficient for entry because further digestion of GP1 requires CatB. The C-terminal region of GP1 contains highly variable and heavily glycosylated sequences, including the Muc domain (6), which promote viral adhesion (9) and may shield viral particles from immune recognition, but may have to be removed first to allow further GP1 digestion. An analogous multistep strategy is used by HIV: CD4-receptor binding is required for Env to be triggered by the CCR5 coreceptor (11). Even more striking parallels exist between the enveloped Ebola virus and the nonenveloped mammalian reovirus: reovirus entry also requires stepwise proteolysis of viral surface proteins by endosomal cysteine proteases (16–18).
Human fatalities from EboV infection range from 50 to 90% and treatment is currently restricted to supportive care (1). The development of an antiviral therapy for EboV is therefore a high priority. To examine whether endosomal cysteine proteases are potential anti-EboV targets, we measured the effects of E-64d and CA074 on growth of the Zaire strain of Ebola virus. Vero cells were pretreated with these inhibitors and exposed to virus for 1 hour. Inhibitor and unbound virus were then removed and viral growth was monitored. The yields of infectious EboV progeny (Fig. 3A) and expression of cell-associated GP1 (Fig. 3B) were markedly reduced in inhibitor-treated cells, suggesting that EboV multiplication in Vero cells is sensitive to inhibitors of endosomal cysteine proteases in general and of CatB in particular. Further investigation of the antiviral efficacy of such inhibitors may therefore be warranted. The wealth of existing knowledge regarding the design (21) and in vivo pharmacology (28) of these inhibitors may facilitate development of an anti-EboV therapy.
Fig. 3.
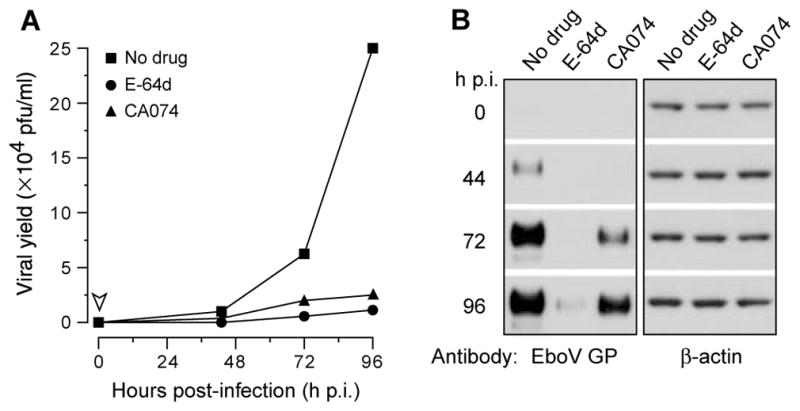
Endosomal cysteine protease inhibitors diminish EboV-Zaire multiplication in Vero cells. (A) Yields of infectious EboV-Zaire released from cells treated with DMSO (no drug), 300 μM E-64d (to inactivate endosomal cysteine proteases), or 80 μM CA074 (to selectively inactivate CatB) for 4 hours are shown. Growth medium containing inhibitors was removed from cells at the indicated time (arrowhead) and replaced with fresh medium lacking inhibitors. pfu/ml, plaque-forming units per milliliter; h p.i., hours post infection. Averages from two replicates are shown. (B) GP expression in EboV-infected cells from (A). β-actin was used as a loading control.
Supplementary Material
Supplemental Online Material
Acknowledgments
We thank J-Y. Yang, V. Spivak, and P. Popernack for technical support; C. Peters and AstraZeneca for knockout mice; T. S. Dermody and N. Fehrenbacher for protease plasmids and MEFs; and M. A. Agosto, S. C. Harrison, T. W. Geisbert, T. Ivanovic, P. B. Jahrling, J. Jané-Valbuena, M. Lazar, W. Mothes, G. J. Nabel, M. L. Nibert, T. Raz, and S. Viswanathan for helpful discussions. Supported by grants from NIH (J.M.C., N.J.S., and S.P.W.), the Cystic Fibrosis Foundation (S.P.W), and departmental funds (S.P.W.). K.C. is supported by the New England Regional Center of Excellence for Biodefense and Emerging Infectious Diseases Research. U.F. is supported by an Emmy Noether grant from the Deutsche Forschungsgemeinschaft.
Footnotes
References and Notes
- 1.Geisbert TW, Jahrling PB. Nat Med. 2004;10:S110. doi: 10.1038/nm1142. [DOI] [PubMed] [Google Scholar]
- 2.Wool-Lewis RJ, Bates P. J Virol. 1998;72:3155. doi: 10.1128/jvi.72.4.3155-3160.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Takada A, et al. Proc Natl Acad Sci USA. 1997;94:14764. doi: 10.1073/pnas.94.26.14764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Volchkov VE. Curr Top Microbiol Immunol. 1999;235:35. doi: 10.1007/978-3-642-59949-1_3. [DOI] [PubMed] [Google Scholar]
- 5.Sanchez A, et al. J Virol. 1998;72:6442. doi: 10.1128/jvi.72.8.6442-6447.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jeffers SA, Sanders DA, Sanchez A. J Virol. 2002;76:12463. doi: 10.1128/JVI.76.24.12463-12472.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Weissenhorn W, Carfi A, Lee KH, Skehel JJ, Wiley DC. Mol Cell. 1998;2:605. doi: 10.1016/s1097-2765(00)80159-8. [DOI] [PubMed] [Google Scholar]
- 8.Ito H, Watanabe S, Sanchez A, Whitt MA, Kawaoka Y. J Virol. 1999;73:8907. doi: 10.1128/jvi.73.10.8907-8912.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Simmons G, et al. Virology. 2003;305:115. doi: 10.1006/viro.2002.1730. [DOI] [PubMed] [Google Scholar]
- 10.Skehel JJ, Wiley DC. Annu Rev Biochem. 2000;69:531. doi: 10.1146/annurev.biochem.69.1.531. [DOI] [PubMed] [Google Scholar]
- 11.Earp LJ, Delos SE, Park HE, White JM. Curr Top Microbiol Immunol. 2005;285:25. doi: 10.1007/3-540-26764-6_2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Malashkevich VN, et al. Proc Natl Acad Sci USA. 1999;96:2662. doi: 10.1073/pnas.96.6.2662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Simmons G, et al. J Virol. 2003;77:13433. doi: 10.1128/JVI.77.24.13433-13438.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Boulay F, Doms RW, Wilson I, Helenius A. EMBO J. 1987;6:2643. doi: 10.1002/j.1460-2075.1987.tb02555.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mothes W, Boerger AL, Narayan S, Cunningham JM, Young JA. Cell. 2000;103:679. doi: 10.1016/s0092-8674(00)00170-7. [DOI] [PubMed] [Google Scholar]
- 16.Ebert DH, Deussing J, Peters C, Dermody TS. J Biol Chem. 2002;277:24609. doi: 10.1074/jbc.M201107200. [DOI] [PubMed] [Google Scholar]
- 17.Nibert ML. thesis. Harvard University; 1993. [Google Scholar]
- 18.Chandran K, Nibert ML. Trends Microbiol. 2003;11:374. doi: 10.1016/s0966-842x(03)00178-1. [DOI] [PubMed] [Google Scholar]
- 19.Experiments in Figs. 1 and 2 were performed with VSV-GPΔMuc, and similar results with VSV-GP are reported in figs. S1 to S5.
- 20.Turk B, Turk V, Turk D. Biol Chem. 1997;378:141. [PubMed] [Google Scholar]
- 21.Otto HH, Schirmeister T. Chem Rev. 1997;97:133. doi: 10.1021/cr950025u. [DOI] [PubMed] [Google Scholar]
- 22.Murata M, et al. FEBS Lett. 1991;280:307. doi: 10.1016/0014-5793(91)80318-w. [DOI] [PubMed] [Google Scholar]
- 23.Shaw E. Methods Enzymol. 1994;244:649. doi: 10.1016/0076-6879(94)44048-4. [DOI] [PubMed] [Google Scholar]
- 24.Deussing J, et al. Proc Natl Acad Sci USA. 1998;95:4516. doi: 10.1073/pnas.95.8.4516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Materials and methods are available as supporting material on Science Online.
- 26.Chandran K, Cunningham JM. data not shown. [Google Scholar]
- 27.Felbor U, et al. Proc Natl Acad Sci USA. 2002;99:7883. doi: 10.1073/pnas.112632299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhang T, et al. Immunology. 2000;100:13. doi: 10.1046/j.1365-2567.2000.00000.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Online Material