Poverty and common mental disorders in low and middle income countries: A systematic review✩ (original) (raw)
. Author manuscript; available in PMC: 2016 Aug 19.
Abstract
In spite of high levels of poverty in low and middle income countries (LMIC), and the high burden posed by common mental disorders (CMD), it is only in the last two decades that research has emerged that empirically addresses the relationship between poverty and CMD in these countries. We conducted a systematic review of the epidemiological literature in LMIC, with the aim of examining this relationship. Of 115 studies that were reviewed, most reported positive associations between a range of poverty indicators and CMD. In community-based studies, 73% and 79% of studies reported positive associations between a variety of poverty measures and CMD, 19% and 15% reported null associations and 8% and 6% reported negative associations, using bivariate and multivariate analyses respectively. However, closer examination of specific poverty dimensions revealed a complex picture, in which there was substantial variation between these dimensions. While variables such as education, food insecurity, housing, social class, socio-economic status and financial stress exhibit a relatively consistent and strong association with CMD, others such as income, employment and particularly consumption are more equivocal. There are several measurement and population factors that may explain variation in the strength of the relationship between poverty and CMD. By presenting a systematic review of the literature, this paper attempts to shift the debate from questions about whether poverty is associated with CMD in LMIC, to questions about which particular dimensions of poverty carry the strongest (or weakest) association. The relatively consistent association between CMD and a variety of poverty dimensions in LMIC serves to strengthen the case for the inclusion of mental health on the agenda of development agencies and in international targets such as the millenium development goals.
Keywords: Mental health, Poverty, Developing countries, Depression, Anxiety, Development, Systematic review
Introduction
Common mental disorders (CMD), which include depression, anxiety and somatoform disorders, make a significant contribution to the burden of disease and disability in low and middle income countries (LMIC) (Lopez, Mathers, Ezzati, Jamison, & Murray, 2006; WHO, 2001). In spite of high levels of poverty in LMIC, and the high burden posed by CMD in these countries, it is only in the last two decades that research has emerged that empirically addresses the relationship between poverty and CMD in these settings (Araya, Lewis, Rojas, & Fritsch, 2003; Patel, Araya, de Lima, Ludermir, & Todd, 1999; Patel & Kleinman, 2003).
Recently, there has been debate in the literature regarding the strength of this relationship. Narrative reviews of 5 epidemiological studies from Brazil, Chile, India and Zimbabwe (Patel et al., 1999) and of a further 11 studies from a range of LMIC (Patel & Kleinman, 2003), suggest that CMD is strongly associated with lower levels of education and socio-economic status, as well as factors such as rapid social change, violence and insecurity, particularly among women. However, other reviews have concluded that when using measures of poverty such as consumption (defined as household per capita expenditure) or level of education, there is no consistent association with indicators of poor mental health (Das, Do, Friedman, McKenzie, & Scott, 2007).
The debate regarding the consistency and strength of the association between CMD and poverty is important, not only for conceptual reasons. A clear association between mental ill-health and poverty in LMIC would strengthen the case for the inclusion of mental health on the agenda of development agencies and on international targets such as the millenium development goals (MDGs) (Miranda & Patel, 2005; Sachs & Sachs, 2007). On the other hand, a weak association might suggest that interventions that target the purported social determinants of CMD would exert a limited effect (Das et al., 2007). In this instance, interventions might be better directed towards protecting individuals and households from adverse events (Das et al., 2007), as well as secondary and tertiary prevention.
This debate has taken place against the backdrop of a relatively well established field of study regarding poverty and mental health in high income countries (HIC) (Saraceno & Barbui, 1997; Saraceno, Levav, & Kohn, 2005). Unemployment (Weich & Lewis, 1998); adverse neighbourhood characteristics (Truong & Ma, 2006); low income, education, social class and socio-economic status (SES) (Lorant et al., 2003); and more recently income inequality (Pickett, James, & Wilkinson, 2006) have been shown to be associated with negative mental health outcomes in these countries. Theory regarding the mechanisms of this relationship is broadly divided into the “social causation” hypothesis, in which the conditions of poverty, such as stress, increased negative life events, worse physical health, reduced access to health care and stigma are thought to precipitate or maintain mental ill-health; and the “social selection” or “social drift” hypothesis, in which people living with mental illness are thought to drift into, or remain in, conditions of poverty, as a result of increased health expenditure, reduced income and lost employment (Dohrenwend et al., 1992; Saraceno et al., 2005). It has been hypothesised that the former theory may more readily apply to depression, whereas the latter may be more appropriate for schizophrenia (Saraceno et al., 2005).
In both HIC and LMIC, the definition of poverty appears to be central to examining its association with mental health. Traditionally, “absolute” poverty refers to a fixed income level and “relative” poverty refers to the level of income in relation to the mean or median income of a population (Toye & Infanti, 2004). A further distinction has been made between poverty and deprivation. Townsend argued that while deprivation refers to people’s unmet needs for a number of basic commodities, poverty refers to the lack of resources required to meet those needs (Townsend, 1979, 1987). The subsequent development of the term “multiple deprivation” has come to refer to a range of indicators of social and economic deprivation and exclusion in poverty studies (Barnes, Wright, Noble, & Dawes, 2007; Toye & Infanti, 2004). Attempts have also been made to develop composite deprivation indices, such as the Index of Multiple Deprivation (IMD) (Department of the Environment, 2000) and the Human Development Index (HDI) (United Nations Development Programme, 2006).
In the light of the apparently contradictory findings from existing literature in LMIC, and the complex relationship between poverty and mental health, we carried out a systematic review of the literature to further elucidate the relationship between a variety of poverty indicators and CMD in LMIC. In particular, we aimed to describe the strength and nature of any association, and the type of poverty indicators most predictive of this relationship. These may inform national and international policy interventions.
Methods
Search strategies
This review was part of a broader systematic review examining the association between poverty and various mental illnesses. The search strategies therefore reflect that of the broader review, from which studies on CMD were subsequently selected. We searched the MEDLINE, EconLit and PsycINFO databases, using Medical Subject Heading (MeSH) terms (or equivalent terms for EconLit and PsycINFO) in February 2008 and again in January 2009 for published peer-review journal articles. Terms used to capture articles relating to mental illness were “mental disorders” and all terms included in MESH as sub-headings of mental disorders. Those for capturing poverty-related studies included: “social class”, “social environment”, “community networks”, “social support”, “violence”, “poverty”, “education”, “educational status”, “employment”, “unemployment”, “income”, “housing”, “health expenditures”, “socioeconomic factors” and “social conditions”. Those for capturing studies carried out in LMIC included “developing countries”, and the names of all the individual countries classified as low or middle income countries by the World Bank (World Bank, 2001).
Searches were conducted for studies published in all languages between 1 January 1990 and 31 December 2008. This period was selected because prior to 1990 there were few epidemiological studies conducted in LMIC with sufficiently robust methodologies to examine the association between CMD and poverty-related variables.
Reference sections of key articles were reviewed and hand searches were conducted to review tables of contents for Social Science and Medicine; British Journal of Psychiatry; Social Psychiatry and Psychiatric Epidemiology; and The Journal of Mental Health Policy and Economics from 1 January 1990 to 31 December 2008.
Types of studies and samples
Observational and intervention studies reporting epidemiological data on measures of poverty and CMD and their relationship among adults in one or more LMIC were eligible for review. The studies had to include an internal comparison group of individuals who represent one level of social or economic status in relation to another. Comparison to reference data was not eligible for inclusion in this review.
Types of poverty measures
With the understanding that a range of poverty and deprivation variables exert a complex and varied influence on mental health outcomes, we elected to report on a range of these measures separately, as they had been reported in the studies we reviewed, rather than creating a composite poverty index. The following indices were selected as exposure variables: education; income; employment; housing and living environment (structural), which included the physical condition of housing and living environments and access to electricity, water and sanitation; housing and living environment (overcrowding); financial stress; consumption; food insecurity; social class and socio-economic status (SES). We excluded studies that only examined exposures related to social capital, violence and war.
Types of mental illness measures
Given the wide range of measures to assess CMD, we compiled a list of conventionally used categories that would allow for a meaningful comparison of studies examining the same outcomes. These categories included: depression; anxiety; common mental disorders (defined as anxiety, depression and somatoform disorders, usually measured by a screening tool designed to detect all three of these disorders, such as the Self-Reporting Questionnaire (SRQ-20) (Harding et al., 1980) or the General Health Questionnaire (GHQ) (Goldberg & Hillier, 1979)); posttraumatic stress disorder (PTSD) and postnatal depression. We excluded psychosis; dementias; child and adolescent mental disorders; conversion disorders; body dysmorphic disorders; personality disorders; eating disorders; suicide; self harm; substance use disorders; intellectual disability; epilepsy and developmental disorders.
Identification of studies
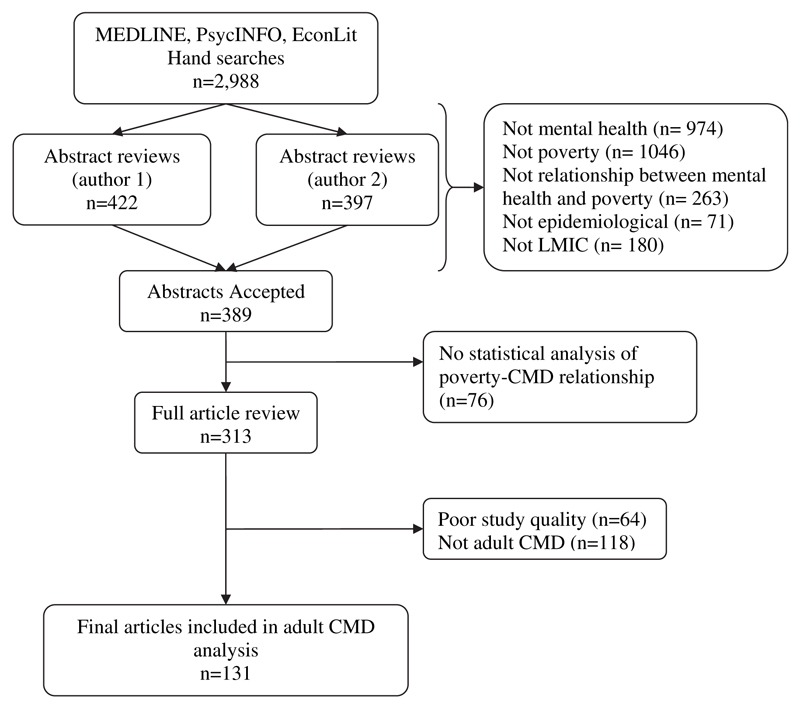
Using the above search methods, we identified 2988 articles (Fig. 1). The first two authors (CL and AB) independently reviewed the abstracts of these articles, using a hierarchical set of exclusion criteria: “not mental health”, “not poverty”, “not relationship between mental health and poverty”, “not epidemiological”, “not low or middle income country”. Inter-rater reliability between the two reviewers was moderate (Cohen’s kappa = 0.75 for 359 articles published in 2008). Once compared, the first two authors discussed discordant results to reach agreement, and 389 articles were included. Having obtained the full articles of these studies, we excluded a further 76 articles as they did not provide statistical analysis of the relationship between mental health and poverty.
Fig. 1.
Flow chart of literature search.
Data extraction
Data from the 313 articles to be included were extracted into a spreadsheet, which included 5 dimensions: (1) study characteristics: author, year, country, rural versus urban, single versus multicentre, single versus two-stage design, setting (community-based, clinic-based, hospital-based, registers), main purpose of the study, design, sample size, sampling procedure, participation rate, duration of the study (if a cohort study), exclusion criteria, age, age unit, ethnicity, % female, adult or child and adolescent; (2) poverty measures (as listed above) and instruments used; (3) mental illness measures (as listed above) and instruments used; (4) analysis: proportion by poverty measure, proportion by mental health measure, crude odds ratios (OR) (95% confidence intervals) for poverty and mental health indicators, adjusted OR (95% confidence intervals) for poverty and mental health indicators, variables adjusted for, and interactions tested; and (5) quality assessment.
Quality assessment
Quality assessments of all of the eligible studies were carried out independently by two reviewers (a data extractor and the first author (CL)). We evaluated studies for methodological quality and appropriateness for inclusion, without consideration of their results, based on a set of pre-determined criteria derived from the SIGN50 guidelines (http://www.sign.ac.uk/guidelines/fulltext/50/annexc.html). The criteria for assessing the quality of the studies are set out in Table 1. Studies rated as “_” were excluded from the review, leaving 249 articles. Of these, 118 articles that did not report adult CMD as an outcome were removed from the analysis for this paper.
Table 1.
Study quality assessment criteria.
| Study design | |
|---|---|
| All study designs | Presentation of an appropriate research question, risk for bias due to selection, confounding and/or measurement, and reporting of confidence intervals. |
| Case control studies | Comparable cases and controls, same exclusion criteria, participation rate, similarities at baseline, clear case-control definitions, clear establishment of controls, blindness to exposure, reliability of exposure measure, identification of potential confounders and use of sensitivity analysis. |
| Cross-sectional studies | Participation rate, blindness to exposure, reliability of exposure measure, identification of potential confounders and use of sensitivity analysis. |
| Cohort studies | Comparable baseline, response rate, outcome present at baseline, losses to follow-up, impact of losses to follow-up, clearly defined outcome, blind outcome assessment, acknowledgement of impact of non-blind assessment, reliable exposure assessment, validity of outcome assessment and reliability of exposure measure. |
| Overall ratings | |
| ++ | All or almost all of the above criteria were fulfilled, and those criteria that were not fulfilled were thought unlikely to alter the conclusions of the study. |
| + | Some of the above criteria were fulfilled, and those criteria that were not fulfilled were thought unlikely to alter the conclusions of the study. |
| − | Few or no criteria were fulfilled, and the conclusions of the study were thought likely or very likely to alter with their inclusion. |
Data analysis
Recognizing that the results of a single study can be published in multiple publications and that a single article can include results of more than one study, care was taken to ensure that the unit of analysis was the study rather than the article to avoid over/under-counting studies in the analysis. We stratified the included studies by poverty indicator, by study design, by setting and by those that conducted bivariate and multivariate analysis. To explore specific hypotheses we grouped studies by instrumentation, for example comparing the strength of the poverty-CMD association between screening instruments and structured diagnostic tools. Using these stratifications, we calculated proportions of studies that demonstrated positive, null and negative associations between poverty and mental health variables. Our analysis focused on four main issues: (1) definitions and measures of poverty; (2) definitions and measures of CMD; (3) the consistency of the association between poverty and CMD; and (4) possible causal mechanisms.
Given the heterogeneity of the studies’ design, measurement and analysis it was not possible to pool the data to generate summary estimates. Not all studies reported odds ratios, and those that did used a variety of methods for measuring both the independent and dependent variables. For example, in the case of education studies, educational level was measured by literacy versus no-literacy, tertiles (e.g., primary, secondary, tertiary), quartiles (e.g., no education, primary, secondary, tertiary), quintiles (no education, Grades 1–4, 5–7, 8–12, 13 and over) and years of education (as a numerical variable). Pooling odds ratios from these varying methods, while statistically possible, would have limited validity.
Results
Overview of studies
A total of 131 published articles representing 115 studies from 33 countries were included in the final analysis (Table 2). Among these, 18 studies were published in multiple articles and 3 articles reported on multiple studies within a single article. Details of all included studies are set out in Appendices.
Table 2.
Study characteristics.
| Variable | Number of studiesa | % |
|---|---|---|
| Setting | ||
| Community-based | 76 | 67 |
| Clinic-based | 25 | 22 |
| Hospital-based | 10 | 9 |
| Registries, prisons or military | 4 | 3 |
| Location | ||
| Rural | 13 | 11 |
| Urban | 54 | 47 |
| Both | 48 | 42 |
| Disorderb | ||
| Anxiety | 26 | |
| Depression | 71 | |
| CMD | 30 | |
| Poverty indicatorb | ||
| Income | 34 | |
| Education | 90 | |
| Employment | 44 | |
| SES | 13 | |
| Social class | 6 | |
| Financial stress | 8 | |
| Housing/living environment (structural) | 11 | |
| Housing/living environment (overcrowding) | 8 | |
| Food insecurity | 7 | |
| Consumption | 4 | |
| Study design | ||
| Case control | 6 | 5 |
| Cohort | 11 | 10 |
| Cross-sectional | 98 | 85 |
| Sampling procedure | ||
| Consecutive | 23 | 20 |
| Random | 70 | 61 |
| Selective | 12 | 10 |
| Otherc | 10 | 9 |
| Quality | ||
| ++ | 25 | 22 |
| + | 90 | 78 |
| Sample sizesa | ||
| Minimum value | 49 | |
| First quartile (25th percentile) | 303 | |
| Median (50th percentile) | 718 | |
| Third quartile (75th percentile) | 1350 | |
| Maximum value | 35014 |
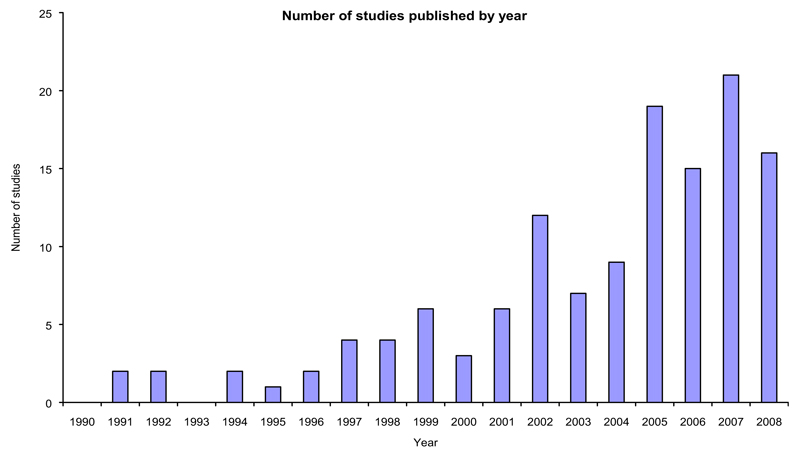
Most of the studies were published in English, with 6 Portuguese, 5 Spanish and 1 Hebrew study. Most of the studies (77%) had as their primary purpose the reporting of the prevalence or incidence of CMD and their socio-economic correlates. The number of eligible studies published per year increased steadily over the review period, with 108 (82%) studies published between 2000 and 2008 (Fig. 2).
Fig. 2.
Number of studies published by year.
Poverty measures
There was variation in the manner in which each poverty variable was defined. For example in the case of income, some reported individual income, some household income and some developed aggregates per household member. For SES, some aggregated education, income and residential area, others created ill-defined categories of “high, medium and low”. We elected to report SES as it was defined by the authors of the studies, but evidence of measurement bias counted against the study in the quality assessment (described above). For example if a study reported SES categories of “high, medium and low” but did not provide any indication of how these categories were derived or what measures were used to assess SES, the study was marked as having a risk of measurement bias.
Mental illness measures
Various tools were used to assess CMD as a whole, such as the General Health Questionnaire (GHQ) (including a mixture of short and full versions), Self-Reporting Questionnaire (SRQ-20) and the Revised Clinical Interview Schedule (CIS-R). Other screening tools were used to assess depression, such as the Edinburgh Postnatal Depression Scale (EPDS), Beck Depression Inventory (BDI) and the Centre for Epidemiologic Studies-Depression scale (CES-D). Structured diagnostic tools were used, such as the Composite International Diagnostic Interview (CIDI) to detect depressive or anxiety disorders according to DSM-IV, ICD-10 or DSM III-R criteria. Several studies used clinical interviews, frequently as a second-stage assessment. Overall, 18% used a two-stage assessment design.
Poverty-CMD associations
Most studies reported positive associations between a range of poverty indicators and CMD (Odds ratios (OR) with 95%CI > 1, or p < 0.05). In community-based studies, 73% and 79% of studies reported positive associations between a variety of poverty measures and CMD, 19% and 15% reported null associations and 8% and 6% reported negative associations, using bivariate and multivariate analyses respectively (Table 3). In facility-based studies (clinic and hospital-based studies), trends were similar, with 76% and 69% of studies reporting positive associations, 22% and 31% reported null associations and 1% and 0% reported negative associations, using bivariate and multivariate analyses respectively. Among those studies that did report positive associations, poverty measures were associated not only with increased prevalence of CMD, but also with increased severity, longer course and worse outcome. However, closer examination of specific poverty dimensions revealed a complex picture, in which there was substantial variation between poverty indicators.
Table 3.
Proportions of studies showing positive, null and negative associations between poverty measures and CMD, by setting.
| Poverty indicator | Settinga | Analysis | Association with CMD | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Positive | Null | Negative | Unknown | Total | |||||||
| n | % | n | % | n | % | n | % | ||||
| Lower income | Community-based | Bivariate | 17 | 77 | 5 | 23 | 0 | 0 | 0 | 0 | 22 |
| Multivariate | 8 | 62 | 4 | 31 | 1 | 8 | 0 | 0 | 13 | ||
| Facility-based | Bivariate | 7 | 78 | 2 | 22 | 0 | 0 | 0 | 0 | 9 | |
| Multivariate | 2 | 50 | 2 | 50 | 0 | 0 | 0 | 0 | 4 | ||
| Lower education | Community-based | Bivariate | 35 | 66 | 13 | 25 | 5 | 9 | 0 | 0 | 53 |
| Multivariate | 20 | 67 | 9 | 30 | 0 | 0 | 1 | 3 | 30 | ||
| Facility-based | Bivariate | 20 | 61 | 12 | 36 | 1 | 3 | 0 | 0 | 33 | |
| Multivariate | 9 | 64 | 5 | 36 | 0 | 0 | 0 | 0 | 14 | ||
| Unemployment | Community-based | Bivariate | 12 | 60 | 7 | 35 | 1 | 5 | 0 | 0 | 20 |
| Multivariate | 13 | 59 | 8 | 36 | 0 | 0 | 1 | 5 | 22 | ||
| Facility-based | Bivariate | 11 | 50 | 9 | 41 | 1 | 5 | 1 | 5 | 22 | |
| Multivariate | 2 | 33 | 4 | 67 | 0 | 0 | 0 | 0 | 6 | ||
| Lower SES | Community-based | Bivariate | 6 | 100 | 0 | 0 | 0 | 0 | 0 | 0 | 6 |
| Multivariate | 5 | 100 | 0 | 0 | 0 | 0 | 0 | 0 | 5 | ||
| Facility-based | Bivariate | 3 | 43 | 4 | 57 | 0 | 0 | 0 | 0 | 7 | |
| Multivariate | 2 | 67 | 1 | 33 | 0 | 0 | 0 | 0 | 3 | ||
| Lower social class | Community-based | Bivariate | 4 | 100 | 0 | 0 | 0 | 0 | 0 | 0 | 4 |
| Multivariate | 4 | 100 | 0 | 0 | 0 | 0 | 0 | 0 | 4 | ||
| Facility-based | Bivariate | 1 | 100 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | |
| Multivariate | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | ||
| Increased financial stress | Community-based | Bivariate | 4 | 80 | 1 | 20 | 0 | 0 | 0 | 0 | 5 |
| Multivariate | 3 | 100 | 0 | 0 | 0 | 0 | 0 | 0 | 3 | ||
| Facility-based | Bivariate | 3 | 75 | 1 | 25 | 0 | 0 | 0 | 0 | 4 | |
| Multivariate | 2 | 100 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | ||
| Worse housing/living | Community-based | Bivariate | 11 | 92 | 0 | 0 | 1 | 8 | 0 | 0 | 12 |
| environment (structural) | Multivariate | 3 | 100 | 0 | 0 | 0 | 0 | 0 | 0 | 3 | |
| Facility-based | Bivariate | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Multivariate | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | ||
| Worse housing/living | Community-based | Bivariate | 4 | 67 | 2 | 33 | 0 | 0 | 0 | 0 | 6 |
| environment (overcrowding) | Multivariate | 1 | 50 | 1 | 50 | 0 | 0 | 0 | 0 | 2 | |
| Facility-based | Bivariate | 2 | 100 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | |
| Multivariate | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | ||
| Food insecurity | Community-based | Bivariate | 2 | 67 | 0 | 0 | 1 | 33 | 0 | 0 | 3 |
| Multivariate | 1 | 50 | 0 | 0 | 1 | 50 | 0 | 0 | 2 | ||
| Facility-based | Bivariate | 4 | 100 | 0 | 0 | 0 | 0 | 0 | 0 | 4 | |
| Multivariate | 3 | 100 | 0 | 0 | 0 | 0 | 0 | 0 | 3 | ||
| Reduced consumption | Community-based | Bivariate | 1 | 25 | 2 | 50 | 1 | 25 | 0 | 0 | 4 |
| Multivariate | 1 | 100 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | ||
| Facility-based | Bivariate | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Multivariate | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | ||
| Mean | Community-based | Bivariate | 10 | 73 | 3 | 19 | 1 | 8 | 0 | 0 | |
| Multivariate | 6 | 79 | 2 | 15 | 0 | 6 | 0 | 1 | |||
| Facility-based | Bivariate | 7 | 76 | 4 | 22 | 0 | 1 | 0 | 1 | ||
| Multivariate | 3 | 69 | 2 | 31 | 0 | 0 | 0 | 0 |
Income
Community-based studies that employed bivariate analyses showed a relatively consistent positive association between low income and CMD (77% of studies). However, when other variables were controlled for in multivariate analyses, the positive association dropped to 62% of studies. For example, in Santiago, Chile, income was not associated with CMD after adjusting for age, sex, physical disease, working status, social support, education, income decrease and quality of housing. Only recent income decrease (OR: 2.14, 95% CI: 1.70–2.70), lower level of education (OR: 2.44, 95% CI: 1.50–3.97) and poorer housing quality (OR: 1.53, 95% CI: 1.05–2.23) showed independent and statistically significant associations with an increased prevalence of CMD after adjusting for other explanatory variables (Araya et al., 2003). In the only study which reported a negative association, this association was reported when comparing depression scores between 2nd and 4th highest income quartiles of 500–1490and>500–1490 and >500–1490and>3000 (OR: 1.7, 95% CI: 1.1–2.7) in South Korea (Cho et al., 2007).
Only 2 community-based cohort studies examined income, and both reported positive associations between low income and CMD, over 12-month periods in India (Patel, Kirkwood, Pednekar, Weiss, & Mabey, 2006) and Taiwan (Seplaki, Goldman, Weinstein, & Lin, 2006). In the one cohort study that reported both bivariate and multivariate analyses, the strength of the association was reduced from OR: 0.23 (95% CI: 0.1–0.7) to OR: 0.41 (95% CI: 0.1–1.3) (the latter significant for trend: p = 0.04) when adjusting for socio-economic, reproductive and physical health risk factors (Patel, Kirkwood, et al., 2006).
In facility-based studies, trends were similar: while bivariate analyses showed a relatively consistent positive association between low income and CMD (78% of studies), in multivariate analyses the association was more equivocal (only 50% of studies showed this association).
Education
Of the 53 community-based studies that examined education, most (66% of bivariate and 67% of multivariate analyses) found that less education was associated with higher rates of CMD. A small proportion of studies reported a null association (25% of bivariate and 30% of multivariate analyses), while 9% of bivariate analyses noted that less education was associated with less CMD. These latter findings appear to be at least partially a factor of study quality. In the 15 high quality (++) studies using bivariate analysis, only one study showed a negative association and 2 showed null associations. Of the 12 multivariate high quality studies, 11 reported a significant association between low education level and CMD, after controlling for a range of social, economic and demographic variables.
Similarly, all 3 of the community-based cohort studies that explored educational status and CMD in bivariate analysis found that less education was associated with higher rates of CMD. Women with more education had lower risk of postpartum depression in Turkey (p = 0.001) (Gulseren et al., 2006) and CMD in India (OR: 0.11, 95% CI: 0.0–0.9) (Patel, Kirkwood, et al., 2006). However, in Pakistan, the association was with the husbands’ educational level (OR: 1.7, 95% CI: 1.3–2.2), but not the educational level of the women themselves (Rahman & Creed, 2007).
In the 33 facility-based studies that examined education, findings were similar. Of the 2 facility-based cohort studies, one demonstrated a similar association between higher educational level and reduced CMD after 12 months (OR: 0.8, 95% CI: 0.7–0.9), after controlling for sex, age and site of recruitment in Zimbabwe (Todd et al., 1999). The other study reported a positive association in bivariate analysis in the rural area (p = 0.04) but not the urban area (p = 0.26), and a null association in multivariate analysis (OR: 1.98, 95% CI: 0.7–5.6) after controlling for psychosocial, pregnancy and delivery related factors in Lebanon (Chaaya et al., 2002).
Unlike income, the consistency of the association between education and CMD was not attenuated in multivariate analysis: a similar proportion of studies that carried out bivariate and multivariate analyses reported positive, null and negative associations. This was the case in both community and facility-based settings.
Employment status
Just over half of the community-based studies reported a positive association between employment status (unemployment and under-employment) and CMD (60% of bivariate and 59% of multivariate analyses). Many of these studies did not specifically compare employed and unemployed groups – for example examining differences between several employed occupational categories (Adelekan, Ndom, Ekpo, & Oluboka, 1999) or comparing “blue collar” and “white collar” workers (Liu et al., 1998). When we analysed only the 16 studies that compared employed and unemployed groups, 11 studies showed a positive association between unemployment and CMD, 4 studies found null associations and one study found a negative association. Two of the null associations were from samples of Taiwanese earthquake victims and their PTSD outcomes, which limits the generalisability of these findings (Kuo, Wu, Ma, Chiu, & Chou, 2007; Lai, Chang, Connor, Lee, & Davidson, 2004). Overall, the trend suggests that unemployment is associated with CMD, but that this may vary depending on local contextual and measurement factors.
As with income, controlling for other variables such as age, gender, education and physical health appears to diminish the association between unemployment and CMD. Among multivariate analyses, 12 of 17 studies reported a positive association, and the remainder reported null associations.
In facility-based studies, the association was less evident. Only 11 of the 22 studies that conducted bivariate analyses, and 2 of the 6 studies that conducted multivariate analyses showed a positive association between reduced employment and CMD. In the latter studies, the association was weakened when controlling for age, sex, marital status, education, income, clinic, pregnancy-related factors, relationship status and ethnicity.
Housing
In community-based studies that reported structural housing conditions, 11 of the 12 studies showed a positive association between worse housing conditions and CMD, using bivariate analyses, and one study showed a negative association. The negative association was found in a study from Nigeria that classified housing on the basis of “hard” versus “earth” floors, with those living in houses with earth floors at decreased risk (Gureje, Kola, & Afolabi, 2007). In multivariate analysis, 2 of the 3 studies showed a positive association: in Nigeria low scores on the GHQ-12 were associated with below average living conditions (OR: 3.3, 95% CI: 1.99–5.50) (Amoran, Lawoyin, & Oni, 2005); and in South Korea low scores on the Korean Geriatric Depression Scale were associated with rented accommodation (OR: 1.75, 95% CI: 1.18–2.60) (Kim, Shin, Yoon, & Stewart, 2002). There was only one cohort study that examined structural housing, where lack of access to tap water in the house was associated with higher 12-month incidence of CMD among women in India (OR: 2.09, 95% CI: 1.0–4.2) (Patel, Kirkwood, et al., 2006).
Regarding overcrowding and CMD, the trend was towards worse mental health in situations of overcrowding. Among the 6 studies that examined overcrowding, 4 reported a positive association between overcrowded housing and CMD based on bivariate analyses, and 2 a null association. Both of the latter studies reported PTSD outcomes: one was a sample of 314 villagers affected by the 2004 tsunami in Tamil Nadu, India (Kumar et al., 2007) and the other was of mothers of under-fives in Kabul, Afghanistan (Seino, Takano, Mashal, Hemat, & Nakamura, 2008). Of the 2 studies that conducted multivariate analyses, 1 reported a positive association in Mexico (OR: 3.69, 95% CI: 1.19–11.39) (Sabin, Lopes, Nackerud, Kaiser, & Varese, 2003) and 1 a null association in Zimbabwe (OR: 1.66, 95% CI: 0.83–3.30) (Abas & Broadhead, 1997).
Only two facility-based studies reported structural and over-crowding housing variables, neither of which conducted multi-variate analyses. These studies reported positive associations between the number of people per room in households and CMD in India (p = 0.04) (Patel, Pereira, et al., 1998) and living in a squatter area and postnatal depression in Turkey (p = 0.003) (Danaci, Dinc, Deveci, Sen, & Icelli, 2002).
Socio-economic status (SES)
Five of the 6 studies reported a positive association between low SES and CMD, based on bivariate analyses. The exceptional study was among elderly Nigerians where SES was inversely associated with lifetime depression (OR: 0.5, 95% CI: 0.3–0.8) measured using the CIDI (Gureje et al., 2007). All 5 of the studies that reported multivariate analyses showed a positive association between low SES and CMD. Multivariate analyses therefore showed that people from low SES groups in these countries are more likely to have CMD, even after adjusting for a range of health and demographic variables. There is also evidence that SES may be temporally linked to CMD: a cohort study in Pakistan showed that women in the low SES category are three times as likely to have postnatal depression at 12-month follow-up than women in a higher SES category, after adjusting for SRQ score, BDI score and life events (OR: 3.1, 95% CI: 1.2–8.4) (Rahman & Creed, 2007).
Among facility-based studies the findings for SES were more equivocal. In bivariate analyses, 4 of the 8 studies reported null associations and the remaining 4 reported positive associations. In the 3 studies that conducted multivariate analyses, one reported an inverse association between SES and refractory obsessive-compulsive disorder in a small sample in Brazil (OR: 20.72, 95% CI: 1.42–303.32) (Ferrao et al., 2006); one reported an inverse association between SES and postpartum depression in Turkey (OR: 4.1 95% CI: 1.83–9.17) (Dindar & Erdogan, 2007) and one reported a null association for CMD (OR: 1.68, 95% CI: 0.94–3.01) (Liu, Prince, Blizard, & Mann, 2002). It should be noted that in the Turkey study high SES was also associated with increased risk, compared to middle SES (OR: 2.09, 95% CI: 1.03–4.23) (Dindar & Erdogan, 2007).
Social class
All 4 community-based studies showed positive bivariate associations between low social class and CMD. Similarly, 3 of the 4 studies with multivariate analyses showed this association, while one study reported null associations for mood disorders and anxiety disorders, using the CIDI in Sao Paulo, Brazil (Andrade, Walters, Gentil, & Laurenti, 2002).
Among facility-based studies, there was a similar trend. Only one study examined this variable, and in bivariate analysis reported a positive association between low social class and postpartum depression in Pelotas, Brazil (OR: 3.89, 95% CI: 1.28–1.78) (Moraes et al., 2006).
Food insecurity
Two of three community-based studies reported a positive bivariate association between food insecurity and CMD. Food insecurity was associated with PTSD among both those who had (OR: 2.04, 95% CI: 1.45–2.88) and those who had not experienced armed conflict (OR: 1.86, 95% CI: 1.07–3.23) in Afghanistan (Seino et al., 2008); and hunger in the last 3 months was associated with CMD in India (OR: 3.37, 95% CI: 1.3–8.8) (Patel, Kirkwood, et al., 2006). In multivariate analyses, one study reported a positive association between not having food in the house for the next meal and CMD in Agincourt, South Africa (OR: 2.59, 95% CI: 1.12–5.98), but a null association for a sample from Khayelitsha, South Africa (OR: 0.66, 95% CI: 0.31–1.43) (Havenaar, Geerlings, Vivian, Collinson, & Robertson, 2008). One study showed a negative association between lack of food and PTSD with both bivariate and multivariate analyses among Guatemalan refugees living in Mexico 20 years after civil conflict (Sabin et al., 2003).
Among facility-based studies, all 4 studies with bivariate analyses and all 3 studies with multivariate analyses showed a positive association between food insecurity and CMD. Food insecurity was associated with the onset of an episode of depression and the persistence of an existing episode in Harare, Zimbabwe (Patel et al., 1997).
Three cohort studies examined food insecurity: one community-based and two clinic-based, all of which demonstrated positive associations between CMD and food insecurity. In the community-based study, 12-month incidence of CMD was associated with hunger in the past 3 months (OR: 3.37, 95% CI: 1.3–8.8) (Patel, Kirkwood, et al., 2006). In the clinic-based studies, hunger during the past month was associated with postpartum depression, but only among mothers of female infants in Goa, India (RR: 3.0, 95% CI: 1.7–5.1) (Patel, Rodrigues, & DeSouza, 2002). The other clinic-based study in Zimbabwe, demonstrated an association between being unable to buy food and CMD at 6 months, but not at 12 months, after controlling for age, sex and site of recruitment (Patel, Todd, et al., 1998; Todd et al., 1999).
Consumption
In a study examining community-based data in 5 countries, mental health status was marginally worse for low consumption households in 2 countries (Bosnia and Tonga), but was improved for low consumption households in one country (Mexico) and there was no association in 2 countries (Indonesia and India) (Das et al., 2007).
Financial stress
Most of the community-based studies demonstrated a positive association between financial stress and CMD: in 4 of 5 studies with bivariate analyses and 3 studies with multivariate analyses. In one study, financial stress was not associated with depression among incarcerated offenders in Nigeria (Fatoye, Fatoye, Oyebanji, & Ogunro, 2006).
In facility-based studies, 3 of the 4 studies with bivariate analyses, and both of the studies with multivariate analyses reported a positive association between financial stress and CMD. In one, the negative impact of finance-related life events was related to major depressive episodes among clinic attenders in Uganda, but this was not statistically significant (Muhwezi, Agren, Neema, Maganda, & Musisi, 2008).
Two cohort studies explored financial stress. Among women in India, those expressing difficulty making ends meet were more likely to have CMD at 12-months follow-up (OR: 2.39, 95% CI: 1.2–4.9), after adjusting for socio-economic, reproductive and health risk factors (Patel, Kirkwood, et al., 2006). In Taiwan, difficulty meeting expenses was associated with increased score of approximately 1.2 on the CES-D score for depression in the aftermath of an earthquake (Ordinary least squares regression coefficient: 1.2, 95% CI: 0.4–2.0, p < 0.01), after adjusting for health, earthquake experience, social and economic characteristics, demographic characteristics with or without significant interaction terms (Seplaki et al., 2006).
Discussion
Summary of main results
This review presents findings on a complex body of epidemiological literature with heterogeneous methods, instrumentation, study settings and populations, published between 1990 and 2008. Despite the heterogeneity, the literature shows a relatively consistent trend in which CMD is associated with a range of poverty dimensions in LMIC. Among community-based studies that conducted multivariate analysis, 79% reported positive associations between a variety of poverty measures and CMD, and 6% reported negative associations. This finding is consistent with previous narrative reviews (Patel et al., 1999; Patel & Kleinman, 2003) although it reports on a wider range of studies, poverty measures and countries, over a longer time period.
However, there are important differences in the consistency and strength of the association between poverty and CMD, across poverty indicators. While variables such as education, food insecurity, housing, social class, SES and financial stress exhibit a relatively consistent and strong association with CMD, others such as income, employment and particularly consumption are more equivocal. This latter finding may provide some explanation for studies that have questioned the association between poverty and mental ill-health in LMIC (Das et al., 2007).
For example, in the case of income, while most studies showed a significant association between low income and CMD, we were not able to draw clear conclusions regarding this trend, particularly as many of the studies that do show associations do not use multivariate analyses. It may be the case that relative poverty, sudden changes in income level, adverse life events and the stress associated with low income, rather than absolute poverty, are stronger predictors of mental health status, particularly when other variables are controlled (Myer, Stein, Grimsrud, Seedat, & Williams, 2008; Patel & Kleinman, 2003). Nevertheless, caution should be exercised in the interpretation of null associations that are found after multivariate analyses. The weakening of an association may indicate that variables such as education, housing, food insecurity and SES are mediators of the relationship between income and CMD, and that low income may exert its effect on CMD through these other dimensions of deprivation.
Measurement factors
The reasons for differences in the consistency of the association between CMD and poverty are an important point of discussion. These may be divided into measurement and population factors. In relation to measurement of CMD, studies that assess CMD as a whole through a screening tool (such as the SRQ-20, GHQ and EPDS), appear to show more consistent associations than studies that use more complex, multi-faceted diagnostic instruments to assess individual disorders, such as the CIDI. For example all 6 of the studies using the SRQ-20 showed a positive relationship between CMD (including depression) and lower education in bivariate analysis (De Lima et al., 1999; Faria, Facchini, Fassa, & Tomasi, 1999; Hackett, Sagdeo, & Creed, 2007; Ludermir, 2000; Marín-León, de Oliveira, de Azevedo Barros, Dalgalarrondo, & Botega, 2007; Reichenheim & Harpham, 1991) whereas only 2 of the 5 studies that used the CIDI to assess the relationship between depression and education reported a positive association (Cho et al., 2007; Vorcaro, Lima-Costa, Barreto, & Uchoa, 2001) and 3 reported a null association (Gureje et al., 2007; Karam et al., 2006; Robison et al., 2003). This may indicate that the association of CMD with poverty may be stronger for CMD as a whole than for individual diagnostic categories such as anxiety or depression. Broader measures may assess “psychological distress” whereas more specific diagnostic tools may detect more “biological” forms of disorder, which are less likely to be socially determined. Furthermore, broader measures contain items which reflect somatic concerns and it is possible that poor physical health status combined with poor access to health care may lead to higher scores. These hypotheses are supported when comparing outcomes for psychological distress with diagnostic categories, within the same sample in a study. For example, in the South African Stress and Health Survey a strong association was found between SES and psychological distress (measured by the Kessler-10) after adjusting for demographic characteristics, social constructs and life events (OR 2.11, 95% CI: 1.36–3.29) (Myer et al., 2008), but no significant association was reported for 12-month or lifetime depression or anxiety disorders (Stein et al., 2008; Williams et al., 2008).
In addition, there was considerable heterogeneity in the manner in which poverty variables were measured. For example income included both household and personal income, and annual and monthly income; different cut-offs and income categories were employed; and it is difficult to compare findings between 1990 and 2008 when inflation impacts on the value of the income. Similar inconsistencies were evident for other poverty variables. These variations make it difficult to compare the findings from different studies and draw consistent conclusions regarding the relationship between these poverty variables and CMD.
Population factors
Aside from measurement factors, a number of population factors may explain the variability in associations. Given the broad nature of this review, it is not possible to analyse their specific role in detail, but it is important to at least note their potential influence. These may be divided into proximal and distal factors. Among proximal factors, studies in this review indicate that women are more likely than men to have CMD in LMIC and that women living in poverty are particularly vulnerable (Harpham, Snoxell, Grant, & Rodriguez, 2005). Further analysis is required of the role of gender in weakening or strengthening the associations reported here. Secondly, physical health lies in the causal pathway between poverty and CMD and is likely to influence variability in the relationship (Adewuya, Ola, Aloba, Mapayi, & Okeniyi, 2006; Harpham, Huttly, De Silva, & Abramsky, 2005; Patel, DeSouza, et al., 2003; Rahman, Iqbal, Bunn, Lovel, & Harrington, 2004). Thirdly, individual genetic and psychological factors are crucial in mediating the extent to which poverty-related variables, such as sudden loss of income, are translated into symptoms of mental disorder, such as depressed mood, poor concentration, insomnia and fatigue associated with major depression (Patel, Flisher, & Cohen, 2006). Further research is required regarding the intermediate steps between socioeconomic risk factors and specific mental health outcomes.
Among more distal factors, firstly, access to health care is likely to influence the relationship between poverty and CMD (WHO Commission on Social Determinants of Health, 2005). Inadequate access to health care is likely to adversely affect mental health status, given evidence of a high degree of comorbidity between physical and mental disorders (Prince et al., 2007), and increased risk for physical health problems among people living in conditions of poverty (Inandi et al., 2002; Patel, 2001; Patel, Flisher, et al., 2006; Sale & Gadanya, 2009; WHO, 2001; WHO Commission on Social Determinants of Health, 2005). Secondly, the presence or absence of violence, including civil conflict, crime and domestic violence, is also likely to influence the extent to which poor communities are vulnerable to CMD (Cardozo et al., 2004; Ceballo, Ramirez, Castillo, Caballero, & Lozoff, 2004; Harpham, Snoxell, et al., 2005; Seedat, Nyamai, Njenga, Vythilingum, & Stein, 2004; Stein, Seedat, & Emsley, 2002; Ward, Flisher, Zissis, Muller, & Lombard, 2001; WHO, 2002). Thirdly, income inequality may be a factor which is likely to influence the poverty-CMD relationship. For example, settings like Chile and Brazil, with high levels of inequality show strong associations between poverty variables and mental health (Araya, Rojas, Fritsch, Acuna, & Lewis, 2001; Ludermir & Lewis, 2001). Conversely, settings with relatively homogenous socioeconomic strata, such as Ethiopia (Kebede & Alem, 1999a, 1999b) and Nigeria, (Gureje et al., 2007) show relatively weak associations. Additionally, perceptions or experience of deprivation, and comparison of one’s own status with that of others may inform mental health status, particularly for depression (Patel & Kleinman, 2003). Cifuentes et al. (2008) found that the Gini index was positively associated with major depressive episodes, but only in high HDI countries (Cifuentes et al., 2008). Fourthly, urbanisation may be a factor which may explain variability. Populations undergoing rapid urbanisation may be hypothesised as being more vulnerable to mental disorder (Harpham & Blue, 1997), through factors such as overcrowding, inadequate housing, crime, unemployment, breakdown of traditional family structures, hazardous environmental conditions, and insufficient access to clean water, sanitation, education, health and other basic services (Blue & Harpham, 1996; Flisher & Chalton, 2001; Gillis, Welman, Koch, & Joyi, 1991; Harpham, 1994; Harpham & Molyneux, 2001; Ludermir & Harpham, 1998; National Academies Press, 2003). Fifthly, poverty-related variables may be context-specific and dependent on the social and cultural meaning attributed to them (Sabin et al., 2003). Finally, macro-economic contextual factors are likely to have a substantial impact on all of the poverty indicators chosen for this study. Situations such as the 1999–2002 economic crisis in Argentina, the economic crisis in Zimbabwe, the 1997 Asian financial crisis are all likely to have informed the poverty – mental health relationship in these countries during these periods.
Mechanisms of the relationship
Given that the vast majority of studies are cross-sectional, it is difficult to draw clear conclusions regarding the direction of the poverty-CMD relationship. The findings of this review are consistent with the conceptualisation of poverty and mental health as interacting in a “vicious cycle” (Patel, 2001). In this model, people living in poverty are at increased risk of developing CMD, through social exclusion, high stressors, reduced social capital, malnutrition, obstetric risks and increased risk of violence and trauma, all of which increase the risk for higher prevalence of mental disorders, inadequate care and a more severe course of the condition (Saraceno & Barbui, 1997). Conversely, people with CMD may be more likely to drift into poverty, due to increased health expenditure, reduced productivity, lost employment, school dropout, reduced social support and stigma associated with these conditions (Patel & Kleinman, 2003).
Based on the evidence from the limited number of cohort studies in this review, there appears to be some support for the first causal pathway, namely that some poverty conditions (particularly low education, food insecurity and financial stress) may lead to CMD. There is high consistency across studies examining the associations (with the exception of income, employment and household consumption) and many findings from the cross-sectional and case-control studies are supported by longitudinal studies. Furthermore, many of the associations in cohort studies are strong (odds ratios greater than 2) and in one instance (education) there is evidence of a dose–response relationship (Araya et al., 2003). This finding is consistent with findings from other studies in high income countries, which show that CMD is more likely to fit with social causation theory whereas conditions such as schizo-phrenia are more likely to apply to social selection or social drift theory (Dohrenwend et al., 1992; Saraceno & Barbui, 1997). However, the evidence for poverty causing CMD does not preclude the possibility that CMD may cause poverty. The absence of evidence from cohort studies that explored the impact of CMD on poverty status does not imply that there is evidence of the absence of this causal pathway.
Limitations
There are several limitations to this review. Firstly, the review focused only on published peer-review journal articles and a systematic review of grey literature was not undertaken. Secondly, the studies in this review are taken from only 33 countries, and there are limits to which these findings can be generalised to other LMIC. Thirdly, by focusing on variation between poverty predictors, we were not able, within the limited space available, to explore variation between outcomes, such as those between depression and anxiety. Fourthly, publication bias may limit the conclusions that can be drawn from this review, as studies that show a positive association may be more likely to be published than those that show a null association (Dwan et al., 2008). Fifthly, in the case of diffuse multiple associations, aggregate variables tend to yield higher associations than more specific variables. It was not possible to disaggregate these due to the nature of the studies we included, but the effect of possibly over-stating the strength of the associations in some instances, needs to be acknowledged. Sixthly, we were not able to explore the impact of macro-economic factors on the relationship between poverty and CMD in these countries. There are also several limitations to the field currently, namely that the vast majority of studies are cross-sectional, no intervention studies met the inclusion criteria for this review, and most studies focus on risk rather than resilience.
Future research
Four major areas can be identified for future research. Firstly, epidemiological studies need to disaggregate patterns of comorbidity between different disorders, including between mental disorders and physical health, and to explore in more detail the interrelationship between biological, personal, social and economic factors as they impact on mental health in poor communities. This should include the adoption of a multiple deprivation rather than absolute poverty approach, by which indicators of deprivation are sequentially added to regression models not to see if the association is nullified, but rather to see how much each changes the strength of the association. Secondly, longitudinal epidemiological studies are required to provide further clarity on the direction of causality in the relationship between CMD and poverty. A critical research question in this context is what factors provide protection of people living in circumstances of multiple deprivation from developing CMD. These studies are complex and expensive to mount, but are essential if more targeted policy-directed interventions are to be developed. Thirdly, qualitative studies are essential to understand complex local realities and lived experiences. These are likely to yield important differences within and between different developing country contexts and support the development of theory. Fourthly, interventions that aim to break the vicious cycle of poverty and mental ill-health need to be developed and evaluated. These may be aimed at either “end” of the cycle: by reducing the impact of the poverty related risk factors that increase the prevalence or severity of CMD, (Ahmed, Rana, Chowdhury, & Bhuiya, 2002; Case, 2004; McKenzie, Patel, & Araya, 2004) or by reducing the likelihood that people with mental disorders will slide into poverty, for example through secondary prevention (Patel, Chisholm, et al., 2003). It would be helpful to measure variables as continuous, rather than categorical, or at least with sufficient categories to allow rigorous evaluation of dose—response relationships.
Conclusion
The epidemiological literature of the last 19 years indicates that the social and economic conditions of poverty are linked with CMD in LMIC. The mechanisms by which the cycle of poverty and CMD is maintained are complex and multi-dimensional. By presenting a systematic review of the literature, this paper has attempted to shift the debate from questions about whether poverty is associated with CMD in LMIC, to questions about which particular dimensions of poverty carry the strongest (or weakest) association.
For policy makers, a major conclusion from this review is that efforts to address the burden of CMD in LMIC will be limited if they only target individual-level interventions (Truong & Ma, 2006). The relatively consistent association between CMD and poverty in LMIC serves to strengthen the case for the inclusion of mental health on the agenda of development agencies and on international targets such as the MDGs (Miranda & Patel, 2005; Sachs & Sachs, 2007). More specifically, the findings of this review call for increasing precision in the targeting and evaluation of interventions. For example strategies for housing improvements in urban settings should include assessments of mental health consequences of such interventions, with a view to reducing health service burden and costs, and improving mental health of communities.
This implies that development policies aimed at economic growth, measured for example by increased gross domestic product (GDP), are unlikely to carry mental health benefits for populations if the result is to increase food insecurity and adverse living circumstances, and worsen educational outcomes within a given society. Crucially, it is interventions that promote security, education and social, welfare and health safety nets that are more likely to protect the mental health of populations, and allow for the full development of human potential.
Appendix. Supplementary data
Supplementary data associated with this article can be found in online version at doi:10.1016/j.socscimed.2010.04.027.
Appendix Table 1
Appendix Table 2
✩.
This paper was produced as part of the work of the Mental Health and Poverty Project, funded by the UK Department for International Development (DfID) for the benefit of LMIC. VP is supported by a Wellcome Trust Senior Research Fellowship in Tropical Medicine. JC is funded by the Western Cape Department of Health, South Africa. Initial drafting of this review was conducted as part of the Municipal Services Project, funded by the International Development Research Council. The views expressed are not necessarily those of the funders. We would like to thank Sara Cooper and Sarah Skeen for their assistance with the data extraction and Stephen Stansfeld for commenting on an earlier draft of this paper.
Footnotes
We declare that we have no conflicts of interest.
References
- Abas MA, Broadhead JC. Depression and anxiety among women in an urban setting in Zimbabwe. Psychological Medicine. 1997;27:59–71. doi: 10.1017/s0033291796004163. [DOI] [PubMed] [Google Scholar]
- Adelekan ML, Ndom RJ, Ekpo M, Oluboka O. Epidemiology of childhood behavioural disorders in Ilorin, Nigeria–findings from parental reports. West African Journal of Medicine. 1999;18:39–48. [erratum appears in West African Journal of Medicine 1999 Apr–Jun; 18(2):152] [PubMed] [Google Scholar]
- Adewuya AO, Ola BA, Aloba OO, Mapayi BM, Okeniyi JAO. Impact of postnatal depression on infants’ growth in Nigeria; African Psychiatric Association and Allied Professionals meeting, Addis Ababa, Ethiopia; 2006. [Google Scholar]
- Ahmed SM, Rana AKMM, Chowdhury M, Bhuiya A. Measuring perceived health outcomes in non-western culture: does SF-36 have a place? Journal of Health, Population and Nutrition. 2002;20:334–342. [PubMed] [Google Scholar]
- Amoran OE, Lawoyin TO, Oni OO. Risk factors associated with mental illness in Oyo State, Nigeria: a community based study. Annals of General Psychiatry. 2005;4 doi: 10.1186/1744-859X-4-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrade L, Walters EE, Gentil V, Laurenti R. Prevalence of ICD-10 mental disorders in a catchment area in the city of Sao Paulo, Brazil. Social Psychiatry & Psychiatric Epidemiology. 2002;37:316–325. doi: 10.1007/s00127-002-0551-x. [DOI] [PubMed] [Google Scholar]
- Araya R, Lewis G, Rojas G, Fritsch R. Education and income: which is more important for mental health? Journal of Epidemiology and Community Health. 2003;57:501–505. doi: 10.1136/jech.57.7.501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Araya R, Rojas G, Fritsch R, Acuna J, Lewis G. Common mental disorders in Santiago, Chile: prevalence and socio-demographic correlates. British Journal of Psychiatry. 2001;178:228–233. doi: 10.1192/bjp.178.3.228. [DOI] [PubMed] [Google Scholar]
- Barnes H, Wright G, Noble M, Dawes A. The South African index of multiple deprivation for children: Census 2001. Cape Town: HSRC Press; 2007. [Google Scholar]
- Blue I, Harpham T. Urbanization and mental health in developing countries. Current Issues in Public Health. 1996;2:181–185. [PubMed] [Google Scholar]
- Cardozo BL, Bilukha OO, Crawford CAG, Shaikh I, Wolfe MI, Gerber ML, et al. Mental health, social functioning, and disability in Postwar Afghanistan. JAMA: The Journal Of The American Medical Association. 2004;292:575–584. doi: 10.1001/jama.292.5.575. [DOI] [PubMed] [Google Scholar]
- Case A. Does money protect health status? Evidence from South African pensions. In: Wise D, editor. Perspectives on the economics of Aging. Chicago: University of Chicago Press; 2004. pp. 287–305. [Google Scholar]
- Ceballo R, Ramirez C, Castillo M, Caballero GA, Lozoff B. Domestic violence and women’s mental health in Chile. Psychology of Women Quarterly. 2004;28:298–308. [Google Scholar]
- Chaaya M, Campbell OM, El KF, Shaar D, Harb H, Kaddour A. Postpartum depression: prevalence and determinants in Lebanon. Archives of Women’s Mental Health. 2002;5:65–72. doi: 10.1007/s00737-002-0140-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cho MJ, Kim JK, Jeon HJ, Suh T, Chung IW, Hong JP, et al. Lifetime and 12-month prevalence of DSM-IV psychiatric disorders among Korean adults. Journal of Nervous & Mental Disease. 2007;195:203–210. doi: 10.1097/01.nmd.0000243826.40732.45. [DOI] [PubMed] [Google Scholar]
- Cifuentes M, Sembajwe G, Tak S, Gore R, Kriebel D, Punnett L. The association of major depressive episodes with income inequality and the human development index. Social Science & Medicine. 2008;67:529–539. doi: 10.1016/j.socscimed.2008.04.003. [DOI] [PubMed] [Google Scholar]
- Danaci AE, Dinc G, Deveci A, Sen FS, Icelli I. Postnatal depression in turkey: epidemiological and cultural aspects. Social Psychiatry & Psychiatric Epidemiology. 2002;37:125–129. doi: 10.1007/s001270200004. [DOI] [PubMed] [Google Scholar]
- Das J, Do QT, Friedman J, McKenzie D, Scott K. Mental health and poverty in developing countries: revisiting the relationship. Social Science & Medicine. 2007;65:467–480. doi: 10.1016/j.socscimed.2007.02.037. [DOI] [PubMed] [Google Scholar]
- De Lima MS, Hotopf M, Mari JJ, Beria JU, De Bastos AB, Mann A. Psychiatric disorder and the use of benzodiazepines: an example of the inverse care law from Brazil. Social Psychiatry & Psychiatric Epidemiology. 1999;34:316–322. doi: 10.1007/s001270050150. [DOI] [PubMed] [Google Scholar]
- Department of the Environment, T. a. t. RD. Measuring multiple deprivation at the small area level the indices of deprivation 2000. London: DETR; 2000. [Google Scholar]
- Dindar I, Erdogan S. Screening of Turkish women for postpartum depression within the first postpartum year: the risk profile of a community sample. Public Health Nursing. 2007;24:176–183. doi: 10.1111/j.1525-1446.2007.00622.x. [DOI] [PubMed] [Google Scholar]
- Dohrenwend BP, Levav I, Shrout PE, Schwartz S, Naveh G, Link BG, et al. Socioeconomic status and psychiatric disorders: the causation-selection issue. Science. 1992;255:946–952. doi: 10.1126/science.1546291. [DOI] [PubMed] [Google Scholar]
- Dwan K, Altman DG, Arnaiz JA, Bloom J, Chan AW, Cronin E, et al. Systematic review of the empirical evidence of study publication bias and outcome reporting bias. PloS ONE. 2008;3 doi: 10.1371/journal.pone.0003081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faria NM, Facchini LA, Fassa AG, Tomasi E. A cross-sectional study about mental health of farm-workers from Serra Gaucha (Brazil) Revista de Saude Publica. 1999;33:391–400. doi: 10.1590/s0034-89101999000400011. (in Portuguese) [DOI] [PubMed] [Google Scholar]
- Fatoye FO, Fatoye GK, Oyebanji AO, Ogunro AS. Psychological characteristics as correlates of emotional burden in incarcerated offenders in Nigeria. East African Medical Journal. 2006;83:545–552. doi: 10.4314/eamj.v83i10.9467. [DOI] [PubMed] [Google Scholar]
- Ferrao YA, Shavitt RG, Bedin NR, de Mathis ME, Carlos LA, Fontenelle LF, et al. Clinical features associated to refractory obsessive-compulsive disorder. Journal of Affective Disorders. 2006;94:199–209. doi: 10.1016/j.jad.2006.04.019. [DOI] [PubMed] [Google Scholar]
- Flisher A, Chalton D. Urbanisation and adolescent risk behaviour. South African Medical Journal. 2001;91:243–249. [PubMed] [Google Scholar]
- Gillis LS, Welman M, Koch A, Joyi M. Psychological distress and depression in urbanising elderly black persons. South African Medical Journal. 1991;79:490–495. [PubMed] [Google Scholar]
- Goldberg D, Hillier VF. A scaled version of the General Health Questionnaire. Psychological Medicine. 1979;9:139–145. doi: 10.1017/s0033291700021644. [DOI] [PubMed] [Google Scholar]
- Gulseren L, Erol A, Gulseren S, Kuey L, Kilic B, Ergor G. From antepartum to postpartum: a prospective study on the prevalence of peripartum depression in a semiurban Turkish community. Journal of Reproductive Medicine. 2006;51:955–960. [PubMed] [Google Scholar]
- Gureje O, Kola L, Afolabi E. Epidemiology of major depressive disorder in elderly Nigerians in the Ibadan study of ageing: a community-based survey. Lancet. 2007;370:957–964. doi: 10.1016/S0140-6736(07)61446-9. [see comment] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hackett RJ, Sagdeo D, Creed FH. The physical and social associations of common mental disorder in a tribal population in South India. Social Psychiatry and Psychiatric Epidemiology. 2007;42:712–715. doi: 10.1007/s00127-007-0223-y. [DOI] [PubMed] [Google Scholar]
- Harding TW, De Aravango V, Baltazar J, Climent CE, Ibrahim HHA, Ladrido-Ignacio L, et al. Mental disorders in primary health care: a study of their frequency and diagnosis in four developing countries. Psychological Medicine. 1980;10:231–241. doi: 10.1017/s0033291700043993. [DOI] [PubMed] [Google Scholar]
- Harpham T. Urbanization and mental health in developing countries: a research role for social scientists, public health professionals and social psychiatrists. Social Science & Medicine. 1994;39:233–245. doi: 10.1016/0277-9536(94)90332-8. [DOI] [PubMed] [Google Scholar]
- Harpham T, Blue I. Linking health policy and social policy in urban settings: the new development agenda. Transactions of the Royal Society of Tropical Medicine and Hygiene. 1997;91:497–498. doi: 10.1016/s0035-9203(97)90001-8. [DOI] [PubMed] [Google Scholar]
- Harpham T, Huttly S, De Silva MJ, Abramsky T. Maternal mental health and child nutritional status in four developing countries. BMJ Publishing Group; 2005. (Rep. No. 59) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harpham T, Molyneux C. Urban health in developing countries: a review. Progress in Development Studies. 2001;1:113–137. [Google Scholar]
- Harpham T, Snoxell S, Grant E, Rodriguez C. Common mental disorders in a young urban population in Colombia. The British Journal Of Psychiatry: The Journal Of Mental Science. 2005;187:161–167. doi: 10.1192/bjp.187.2.161. [DOI] [PubMed] [Google Scholar]
- Havenaar JM, Geerlings MI, Vivian L, Collinson M, Robertson B. Common mental health problems in historically disadvantaged urban and rural communities in South Africa: prevalence and risk factors. Social Psychiatry & Psychiatric Epidemiology. 2008;43:209–215. doi: 10.1007/s00127-007-0294-9. [DOI] [PubMed] [Google Scholar]
- Inandi T, Elci OC, Ozturk A, Egri M, Polat A, Sahin TK. Risk factors for depression in postnatal first year, in eastern Turkey. International Journal of Epidemiology. 2002;31:1201–1207. doi: 10.1093/ije/31.6.1201. [DOI] [PubMed] [Google Scholar]
- Karam EG, Mneimneh ZN, Karam AN, Fayyad JA, Nasser SC, Chatterji S, et al. Prevalence and treatment of mental disorders in Lebanon: a national epidemiological survey. Lancet. 2006;367:1000–1006. doi: 10.1016/S0140-6736(06)68427-4. [see comment] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kebede D, Alem A. Major mental disorders in Addis Ababa, Ethiopia. II. Affective disorders. Acta Psychiatrica Scandinavica, Supplementum. 1999a;397:18–23. doi: 10.1111/j.1600-0447.1999.tb10689.x. [DOI] [PubMed] [Google Scholar]
- Kebede D, Alem A. Major mental disorders in Addis Ababa, Ethiopia. III. Neurotic and somatoform disorders. Acta Psychiatrica Scandinavica, Supplementum. 1999b;397:24–29. doi: 10.1111/j.1600-0447.1999.tb10690.x. [DOI] [PubMed] [Google Scholar]
- Kim JM, Shin IS, Yoon JS, Stewart R. Prevalence and correlates of late-life depression compared between urban and rural populations in Korea. International Journal of Geriatric Psychiatry. 2002;17:409–415. doi: 10.1002/gps.622. [DOI] [PubMed] [Google Scholar]
- Kumar MS, Murhekar MV, Hutin Y, Subramanian T, Ramachandran V, Gupte MD. Prevalence of posttraumatic stress disorder in a coastal fishing village in Tamil Nadu, India, after the December 2004 tsunami. American Journal of Public Health. 2007;97:99–101. doi: 10.2105/AJPH.2005.071167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuo HW, Wu SJ, Ma TC, Chiu MC, Chou SY. Posttraumatic symptoms were worst among quake victims with injuries following the Chi-Chi quake in Taiwan. Journal of Psychosomatic Research. 2007;62:495–500. doi: 10.1016/j.jpsychores.2004.11.012. [DOI] [PubMed] [Google Scholar]
- Lai TJ, Chang CM, Connor KM, Lee LC, Davidson JR. Full and partial PTSD among earthquake survivors in rural Taiwan. Journal of Psychiatric Research. 2004;38:313–322. doi: 10.1016/j.jpsychires.2003.08.005. [DOI] [PubMed] [Google Scholar]
- Liu CK, Lai CL, Tai CT, Lin RT, Yen YY, Howng SL. Incidence and subtypes of dementia in southern Taiwan: impact of socio-demographic factors. Neurology. 1998;50:1572–1579. doi: 10.1212/wnl.50.6.1572. [DOI] [PubMed] [Google Scholar]
- Liu SI, Prince M, Blizard B, Mann A. The prevalence of psychiatric morbidity and its associated factors in general health care in Taiwan. Psychological Medicine. 2002;32:629–637. doi: 10.1017/s0033291701005074. [DOI] [PubMed] [Google Scholar]
- Lopez DA, Mathers DC, Ezzati M, Jamison TD, Murray JLC. Global burden of disease and risk factors. New York: Oxford University Press/The World Bank; 2006. [Google Scholar]
- Lorant V, Deliege D, Eaton W, Robert A, Philippot P, Ansseau M. Socio-economic inequalities in depression: a meta-analysis. American Journal of Epidemiology. 2003;157:98–112. doi: 10.1093/aje/kwf182. [DOI] [PubMed] [Google Scholar]
- Ludermir AB. Productive employment, gender and mental health. Cadernos de Saude Publica. 2000;16:647–659. doi: 10.1590/s0102-311x2000000300013. (in Portuguese) [DOI] [PubMed] [Google Scholar]
- Ludermir AB, Harpham T. Urbanization and mental health in Brazil: social and economic dimensions. Health & Place. 1998;4:223–232. doi: 10.1016/s1353-8292(98)00017-3. [DOI] [PubMed] [Google Scholar]
- Ludermir AB, Lewis G. Links between social class and common mental disorders in Northeast Brazil. Social Psychiatry & Psychiatric Epidemiology. 2001;36:101–107. doi: 10.1007/s001270050297. [DOI] [PubMed] [Google Scholar]
- Marín-León L, de Oliveira HB, de Azevedo Barros MB, Dalgalarrondo P, Botega NJ. Social inequality and common mental disorders. Revista Brasileira de Psiquiatria. 2007;29 doi: 10.1590/s1516-44462006005000060. [DOI] [PubMed] [Google Scholar]
- McKenzie K, Patel V, Araya R. Learning from low income countries: mental health. BMJ: British Medical Journal. 2004;329:1138–1140. doi: 10.1136/bmj.329.7475.1138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miranda JJ, Patel V. Achieving the millennium development goals: does mental health play a role? PloS Medicine. 2005 doi: 10.1371/journal.pmed.0020291. [On-line]. Available: www.plosmedicine.org. [DOI] [PMC free article] [PubMed]
- Moraes IG, Pinheiro RT, Silva RA, Horta BL, Sousa PL, Faria AD. Prevalence of postpartum depression and associated factors. Revista de Saude Publica. 2006;40:65–70. doi: 10.1590/s0034-89102006000100011. [see comment], (in Portuguese) [DOI] [PubMed] [Google Scholar]
- Muhwezi WW, Agren H, Neema S, Maganda AK, Musisi S. Life events associated with major depression in Ugandan primary healthcare (PHC) patients: issues of cultural specificity. International Journal of Social Psychiatry. 2008;54:144–163. doi: 10.1177/0020764007083878. [DOI] [PubMed] [Google Scholar]
- Myer L, Stein DJ, Grimsrud A, Seedat S, Williams DR. Social determinants of psychological distress in a nationally-representative sample of South African adults. Social Science & Medicine. 2008;66:1828–1840. doi: 10.1016/j.socscimed.2008.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Academies Press. Cities transformed: demographic change and its implications in the developing world. 2003 http://books.nap.edu/catalog/10693.html [On-line].
- Patel V. Poverty, inequality, and mental health in developing countries. In: Leon DA, Walt G, editors. Poverty, inequality and health: An international perspective. Oxford: Oxford University Press; 2001. pp. 247–262. [Google Scholar]
- Patel V, Araya R, de Lima M, Ludermir A, Todd C. Women, poverty and common mental disorders in four restructuring societies. Social Science & Medicine. 1999;49:1461. doi: 10.1016/s0277-9536(99)00208-7. [DOI] [PubMed] [Google Scholar]
- Patel V, Chisholm D, Rabe-Hesketh S, Dias-Saxena F, Andrew G, Mann A. The efficacy and cost-effectiveness of a drug and psychological treatment for common mental disorders in general health care in Goa, India: a randomised controlled trial. Lancet. 2003;361:33–39. doi: 10.1016/S0140-6736(03)12119-8. [DOI] [PubMed] [Google Scholar]
- Patel V, DeSouza N, Rodrigues M. Postnatal depression and infant growth and development in low income countries: a cohort study from Goa, India. Archives of Disease in Childhood. 2003;88:34–37. doi: 10.1136/adc.88.1.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel V, Flisher A, Cohen A. Social and cultural determinants of mental health. In: Murray R, Kendler K, McGuffin P, Wessely S, Castle D, editors. Essentials of psychiatry. (2 ed.) Cambridge: Cambridge University Press; 2006. [Google Scholar]
- Patel V, Kirkwood BR, Pednekar S, Weiss H, Mabey D. Risk factors for common mental disorders in women. Population-based longitudinal study. British Journal of Psychiatry. 2006;189:547–555. doi: 10.1192/bjp.bp.106.022558. [DOI] [PubMed] [Google Scholar]
- Patel V, Kleinman A. Poverty and common mental disorders in developing countries. Bulletin of the World Health Organization. 2003;81:609–615. [PMC free article] [PubMed] [Google Scholar]
- Patel V, Pereira J, Coutinho L, Fernandes R, Fernandes J, Mann A. Poverty, psychological disorder and disability in primary care attenders in Goa, India. British Journal of Psychiatry. 1998a;172:533–536. doi: 10.1192/bjp.172.6.533. [DOI] [PubMed] [Google Scholar]
- Patel V, Rodrigues M, DeSouza N. Gender, poverty, and postnatal depression: a study of mothers in Goa, India. American Journal of Psychiatry. 2002;159:43–47. doi: 10.1176/appi.ajp.159.1.43. [see comment] [DOI] [PubMed] [Google Scholar]
- Patel V, Todd C, Winston M, Gwanzura F, Simunyu E, Acuda W, et al. Common mental disorders in primary care in Harare, Zimbabwe: associations and risk factors. The British Journal of Psychiatry. 1997;171:60–64. doi: 10.1192/bjp.171.1.60. [DOI] [PubMed] [Google Scholar]
- Patel V, Todd C, Winston M, Gwanzura F, Simunyu E, Acuda W, et al. Outcome of common mental disorders in Harare, Zimbabwe. British Journal of Psychiatry. 1998;172:53–57. doi: 10.1192/bjp.172.1.53. [DOI] [PubMed] [Google Scholar]
- Pickett KE, James OW, Wilkinson RG. Income inequality and the prevalence of mental illness: a preliminary international analysis. Journal of Epidemiology and Community Health. 2006;60:646–647. doi: 10.1136/jech.2006.046631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prince M, Patel V, Saxena S, Maj M, Maselko J, Phillips MR, et al. No health without mental health – a slogan with substance. Lancet. 2007;370:859–877. doi: 10.1016/S0140-6736(07)61238-0. [DOI] [PubMed] [Google Scholar]
- Rahman A, Creed F. Outcome of prenatal depression and risk factors associated with persistence in the first postnatal year: prospective study from Rawalpindi, Pakistan. Journal of Affective Disorders. 2007;100:115–121. doi: 10.1016/j.jad.2006.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahman A, Iqbal Z, Bunn J, Lovel H, Harrington R. Impact of maternal depression on infant nutritional status and illness: a cohort study. Archives of General Psychiatry. 2004;61:946–952. doi: 10.1001/archpsyc.61.9.946. [DOI] [PubMed] [Google Scholar]
- Reichenheim ME, Harpham T. Maternal mental health in a squatter settlement in Rio de Janeiro. The British Journal Of Psychiatry: The Journal Of Mental Science. 1991;159:683–690. doi: 10.1192/bjp.159.5.683. [DOI] [PubMed] [Google Scholar]
- Robison J, Curry L, Gruman C, Covington T, Gaztambide S, Blank K. Depression in later-life Puerto Rican primary care patients: the role of illness, stress, social integration, and religiosity. International Psychogeriatrics. 2003;15:239–251. doi: 10.1017/s1041610203009505. [DOI] [PubMed] [Google Scholar]
- Sabin M, Lopes CB, Nackerud L, Kaiser R, Varese L. Factors associated with poor mental health among Guatemalan refugees living in Mexico 20 years after civil conflict. JAMA. 2003;290:635–642. doi: 10.1001/jama.290.5.635. [see comment] [DOI] [PubMed] [Google Scholar]
- Sachs SE, Sachs JD. Mental health in the millennium development goals: not ignored. PLoS Medicine/Public Library of Science. 2007;4:e56. doi: 10.1371/journal.pmed.0040056. [comment], author. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sale S, Gadanya M. Prevalence and factors associated with depression in HIV/AIDS patients aged 15–25 years at Aminu Kano Teaching Hospital, Nigeria. Journal of Child and Adolescent Mental Health. 2009;20(2):95–99. doi: 10.2989/JCAMH.2008.20.2.5.688. [DOI] [PubMed] [Google Scholar]
- Saraceno B, Barbui C. Poverty and mental illness. Canadian Journal of Psychiatry. 1997;42:285–290. doi: 10.1177/070674379704200306. [DOI] [PubMed] [Google Scholar]
- Saraceno B, Levav I, Kohn R. The public mental health significance of research on socio-economic factors in schizophrenia and major depression. World Psychiatry. 2005;4:181–185. [PMC free article] [PubMed] [Google Scholar]
- Seedat S, Nyamai C, Njenga F, Vythilingum B, Stein D. Trauma exposure and post-traumatic stress symptoms in urban African schools. Survey in Cape Town and Nairobi. British Journal of Psychiatry. 2004;184:169–175. doi: 10.1192/bjp.184.2.169. [DOI] [PubMed] [Google Scholar]
- Seino K, Takano T, Mashal T, Hemat S, Nakamura K. Prevalence of and factors influencing posttraumatic stress disorder among mothers of children under five in Kabul, Afghanistan, after decades of armed conflicts. Health & Quality of Life Outcomes. 2008;6:29. doi: 10.1186/1477-7525-6-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seplaki CL, Goldman N, Weinstein M, Lin YH. Before and after the 1999 Chi-Chi earthquake: traumatic events and depressive symptoms in an older population. Social Science & Medicine. 2006;62:3121–3132. doi: 10.1016/j.socscimed.2005.11.059. [DOI] [PubMed] [Google Scholar]
- Stein DJ, Seedat S, Herman A, Moomal H, Heeringa SG, Kessler RC, et al. Lifetime prevalence of psychiatric disorders in South Africa. British Journal of Psychiatry. 2008;192:112–117. doi: 10.1192/bjp.bp.106.029280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein D, Seedat S, Emsley R. Violence in the world and in South Africa: what is a doctor to do? South African Medical Journal. 2002;92:789–790. [PubMed] [Google Scholar]
- Todd C, Patel V, Simunyu E, Gwanzura F, Acuda W, Winston M, et al. The onset of common mental disorders in primary care attenders in Harare, Zimbabwe. Psychological Medicine. 1999;29:97–104. doi: 10.1017/s0033291798007661. [DOI] [PubMed] [Google Scholar]
- Townsend P. Poverty in the United Kingdom. Harmondsworth, Middlesex: Penguin Books; 1979. [Google Scholar]
- Townsend P. Deprivation. Journal of Social Policy. 1987;16:125–146. [Google Scholar]
- Toye M, Infanti J. Social inclusion and community economic development: Literature review. Victoria, BC: The Canadian CED Network; 2004. [Google Scholar]
- Truong KD, Ma S. A systematic review of relations between neighborhoods and mental health. Journal of Mental Health Policy and Economics. 2006;9:137–154. [PubMed] [Google Scholar]
- United Nations Development Programme. Human development report 2006. Beyond scarcity: Power, poverty and global water crisis. New York: MacMillan; 2006. [Google Scholar]
- Vorcaro CM, Lima-Costa MF, Barreto SM, Uchoa E. Unexpected high prevalence of 1-month depression in a small Brazilian community: the Bambui Study. Acta Psychiatrica Scandinavica. 2001;104:257–263. doi: 10.1034/j.1600-0447.2001.00440.x. [DOI] [PubMed] [Google Scholar]
- Ward C, Flisher F, Zissis C, Muller ML, Lombard C. Exposure to violence and its relationship to psychopathology in adolescents. Injury Prevention. 2001;7:297–301. doi: 10.1136/ip.7.4.297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weich S, Lewis G. Poverty, unemployment, and common mental disorders: population based cohort study. British Medical Journal. 1998;317:115–119. doi: 10.1136/bmj.317.7151.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO. World health report 2001, mental health: New understanding, new hope. Geneva: WHO; 2001. [Google Scholar]
- WHO. World report on violence and health. Geneva: WHO; 2002. [Google Scholar]
- WHO Commission on Social Determinants of Health. Action on the social determinants of health: Learning from previous experiences. Geneva: WHO; 2005. [Google Scholar]
- Williams DR, Herman A, Stein DJ, Heeringa SG, Jackson PB, Moomal H, et al. Twelve-month mental disorders in South Africa: prevalence, service use and demographic correlates in the population-based South African Stress and Health Study. Psychological Medicine. 2008;38:211–220. doi: 10.1017/S0033291707001420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Bank. World development report 2000/2001-attacking poverty. New York: Oxford University Press for the World Bank; 2001. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix Table 1
Appendix Table 2