ILAE Classification of the Epilepsies Position Paper of the ILAE Commission for Classification and Terminology (original) (raw)
. Author manuscript; available in PMC: 2018 Apr 1.
Published in final edited form as: Epilepsia. 2017 Mar 8;58(4):512–521. doi: 10.1111/epi.13709
Summary
The ILAE Classification of the Epilepsies has been updated to reflect our gain in understanding of the epilepsies and their underlying mechanisms following the major scientific advances which have taken place since the last ratified classification in 1989. As a critical tool for the practising clinician, epilepsy classification must be relevant and dynamic to changes in thinking, yet robust and translatable to all areas of the globe. Its primary purpose is for diagnosis of patients, but it is also critical for epilepsy research, development of antiepileptic therapies and communication around the world. The new classification originates from a draft document submitted for public comments in 2013 which was revised to incorporate extensive feedback from the international epilepsy community over several rounds of consultation. It presents three levels, starting with seizure type where it assumes that the patient is having epileptic seizures as defined by the new 2017 ILAE Seizure Classification. After diagnosis of the seizure type, the next step is diagnosis of epilepsy type, including focal epilepsy, generalized epilepsy, combined generalized and focal epilepsy, and also an unknown epilepsy group. The third level is that of_epilepsy syndrome_ where a specific syndromic diagnosis can be made. The new classification incorporates etiology along each stage, emphasizing the need to consider etiology at each step of diagnosis as it often carries significant treatment implications. Etiology is broken into six subgroups, selected because of their potential therapeutic consequences. New terminology is introduced such as developmental and epileptic encephalopathy. The term benign is replaced by the terms self-limited and pharmacoresponsive, to be used where appropriate. It is hoped that this new framework will assist in improving epilepsy care and research in the 21st century.
Keywords: Classification, Epilepsy syndromes, Terminology, Etiology
Introduction
Ongoing efforts to refine the classification of the epilepsies have been made by the International League Against Epilepsy (ILAE) almost since its inception in 1909 and gained special momentum in the early sixties when new concepts of classification were proposed by Henri Gastaut 1–3. Intense debate and acquisition of new knowledge in the next two decades led to the landmark 1985 ILAE ‘_Classification of Epilepsies and Epileptic Syndromes_’ 4, which was soon followed by a revised version ratified by the ILAE General Assembly in 1989 5. The 1989 Classification has been highly influential worldwide and has had a major impact on epilepsy care and research. The work presented here builds on the efforts of many over more than a century; we acknowledge their seminal contributions in the development of the classification of the epilepsies.
Although many concepts outlined in the 1989 ILAE classification remain valid to this day, it has become increasingly clear that a revision is needed to account for subsequent scientific discoveries that over the last few decades have fundamentally changed our understanding of the epilepsies as well as our approach to the diagnosis and management of individuals with epilepsy.
Epilepsy classification is the key clinical tool in evaluating an individual presenting with seizures. It influences every clinical consultation yet its impact stretches far beyond the clinical domain to clinical and basic epilepsy research and to the development of novel therapies. Classification serves many purposes: providing a framework for understanding the type of seizures that the patient has, the other seizure types that are more likely to occur in that individual, the potential triggers for their seizures and often their prognosis. Classification also informs the risks of co-morbidities including learning difficulties, intellectual disability, psychiatric features such as autism spectrum disorder, and mortality risk such as sudden unexpected death in epilepsy (SUDEP). Importantly, classification often guides the selection of antiepileptic therapies.
Classification of the epilepsies has evolved dramatically since its inception in the 1960s 6–9. The many iterations in classification reflect advances in understanding phenotypic patterns and underlying mechanisms, based on major contributions from clinical and basic research from around the world. These insights are incorporated into the many facets of clinical care for patients and lead to progress in the development of innovative treatments be they pharmacological or dietary therapies, surgical approaches or device development. Classification will always be a dynamic process, iterative to the new insights gained through research and improved understanding of this heterogeneous group of diseases. Its continued evolution into the future promises to lead to further advances in patient care.
Classification engenders passionate debate. This is partly because it is built on the complex clinical constructs underpinning epilepsy diagnosis and partly because it is so critical to our daily practice. Classification has been based on expert opinion drawing together epileptologists and related experts from around the world. While there is no doubt that the desired endpoint is a scientifically-based classification, our understanding is not sufficiently advanced to construct a classification on a scientifically rigorous basis 9. Thus current proposals are based on a combination of the latest scientific understanding coupled with high level expert opinion, including an extensive consultation with epilepsy professionals and the wider epilepsy community worldwide.
When a patient presents with seizures, the clinician works through several critical steps in making a diagnosis. Before attempting to classify a seizure, the physician must determine whether the paroxysmal event is indeed an epileptic seizure with a myriad of differential diagnoses being possible. These include convulsive syncope, parasomnias, movement disorders and other non-epileptic events (https://www.epilepsydiagnosis.org/epilepsy-imitators.html). This diagnostic step is taken as already established at the point of beginning to classify the patient’s epilepsy.
In terms of epilepsy classification, the clinician starts by classifying the type of seizure. This is the subject of the companion paper on the new classification of seizure types 10. Then, the patient’s type of epilepsy needs to be classified and, in many cases, a specific epilepsy syndrome diagnosis can be made. Just as importantly, strenuous attempts to identifiy the etiology of their epilepsy should be made at each step in the diagnostic pathway. Classification of seizure type and epilepsy type both take into account the results of investigations such as EEG and neuroimaging studies together with other studies exploring the underlying etiology of the epilepsy. Here, we present the first major Classification of the Epilepsies since the last ratified ILAE Classification in 1989.
Methods
In the past, ILAE position papers on fundamental matters such terminology, definition and classification of seizures and epilepsy required ratification by the General Assembly through a vote by the representatives of the ILAE Chapters from around the world 5. This approach is no longer optimal, since it does not permit adequate engagement of the greatly expanded constituency of epilepsy experts around the world and fails to exploit opportunities offered by impressive advances in communication tools.
Consequently, in 2013 the League set in place a new process for the finalization and approval of position documents, i.e. documents which reflect the ILAE position on topics that involve adoption of a common language or set of definitions (e.g. defining epilepsy, classification)11. This process is highly iterative and involves initial production of the document by a group of experts selected by the League, posting the document on the ILAE website, soliciting comments and criticism by all stakeholders, and appointing a separate expert panel to review and incorporate the public comments. This process takes place in parallel with the peer review conducted by the journal to which the document is submitted for publication (http://www.ilae.org/Visitors/Documents/Guideline-PublPolicy-2013Aug.pdf)
In the case of the revised Classification, a first proposal which preceded implementation of the procedure outlined above was published by the ILAE Commission on Classification and Terminology in 2010 9. The emphasis was on employing transparent terminology, where words mean what they say. The 2010 publication triggered extensive discussion and commentaries 12–29. A new Commission on Classification and Terminology was subsequently appointed by the ILAE Executive and tasked to produce a revised Classification through the procedure outlined for ILAE position documents. The Commission submitted the initial document in 2013, and the document was posted online inviting discussion (supplementary material for Scheffer et al 2016 30). Avid community engagement and debate occurred, with 128 comments received from 43 countries. The response was so extensive and the feedback on important concepts so conflicting that the panel in charge for reviewing the public comments determined that further pubic engagement was necessary to ensure the highest possible level of agreement. The roadmap followed by the panel to solicit further engagement and to respond to feedback from stakeholders is described in an article published in Epilepsia Open in 2016, which again invited feedback from the global community30. Further comments and opinions were then deliberated and considered in finalizing the present position document which defines the Classification of the Epilepsies in 2017.
Classification of the Epilepsies
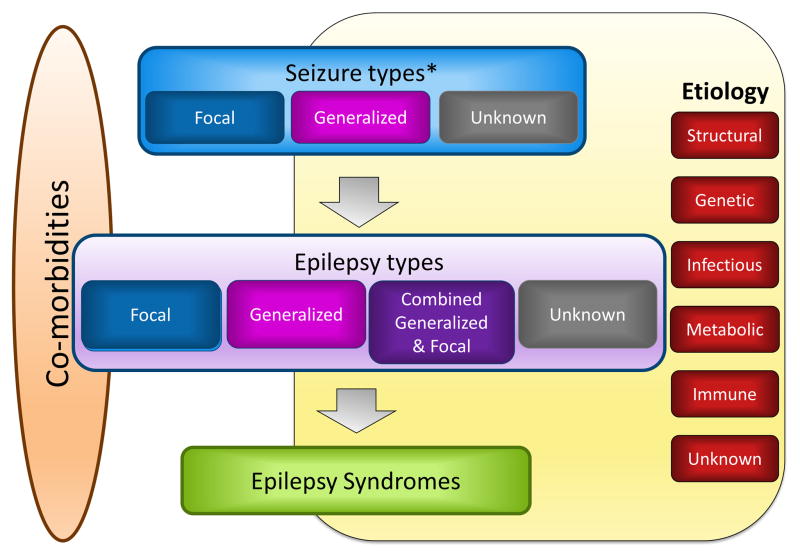
The new Classification of the Epilepsies is a multi-level classification, designed to cater for classifying epilepsy in different clinical environments (Figure). This is in acknowledgement of the wide variation in resources around the world meaning that different levels of classification will be possible depending on the resources available to the clinician making the diagnosis. Where possible, a diagnosis at all three levels should be sought as well as the etiology of the individual’s epilepsy.
Figure.
Framework for Classification of the Epilepsies. * Denotes onset of seizure
1. Seizure Type
The starting point of the Epilepsy classification framework is the Seizure Type; it assumes that the clinician has already made a definite diagnosis of an epileptic seizure and is not meant to be a diagnostic algorithm to distinguish epileptic from non-epileptic events. The Seizure Type Classification is determined according to the new nomenclature in the accompanying paper10. Seizures are classified into focal onset, generalized onset and unknown onset.
In some settings, classification according to Seizure Type may be the maximum level possible for diagnosis as there may be no access to EEG, video and imaging studies. In other cases, there may simply be too little information available to be able to make a higher level diagnosis, such as when a patient has only had a single seizure.
2. Epilepsy Type
The second level is that of Epilepsy Type and assumes that the patient has a diagnosis of epilepsy based on the 2014 definition31. The Epilepsy Type level includes a new category of “Combined Generalized and Focal Epilepsy” in addition to the well-established Generalized Epilepsy and Focal Epilepsies. It also includes an Unknown category. Many epilepsies will include multiple types of seizures.
For a diagnosis of Generalized Epilepsy, the patient would typically show generalized spike-wave activity on EEG. Individuals with generalized epilepsies may have a range of seizure types including absence, myoclonic, atonic, tonic and tonic-clonic seizures. The diagnosis of generalized epilepsy is made on clinical grounds, supported by the finding of typical interictal EEG discharges. Caution needs to be exercised for a patient with generalized tonic-clonic seizures and a normal EEG. In this case, supportive evidence would need to be present to make a diagnosis of generalized epilepsy, such as myoclonic jerks or a relevant family history.
Focal Epilepsies include unifocal and multifocal disorders as well as seizures involving one hemisphere. A range of seizure types can be seen including focal aware seizures, focal impaired awareness seizures, focal motor seizures, focal non-motor seizures, and focal to bilateral tonic-clonic seizures. The interictal EEG typically shows focal epileptiform discharges but the diagnosis is made on clinical grounds, supported by EEG findings.
The new group of Combined Generalized and Focal Epilepsies exists as there are patients who have both generalized and focal seizures. The diagnosis is made on clinical grounds, supported by EEG findings. Ictal recordings are helpful but not essential. The interictal EEG may show both generalized spike-wave and focal epileptiform discharges, but epileptiform activity is not required for the diagnosis. Common examples in which both types of seizures occur are Dravet syndrome and Lennox-Gastaut syndrome.
The Epilepsy type may also be the final level of diagnosis achievable where the clinician is unable to make an Epilepsy Syndrome diagnosis. Examples include: the common situation of a child or adult with non-lesional temporal lobe epilepsy who has Focal Epilepsy with no known etiology; a 5 year old child presenting with generalized tonic-clonic seizures and generalized spike-wave activity on EEG who cannot be classified into a known epilepsy syndrome but has a clear-cut diagnosis of Generalized Epilepsy; or the less common scenario of a 20 year old woman with both focal impaired awareness seizures and absence seizures with both focal discharges and generalized spike wave on EEG recordings and normal MRI, therefore, she would have a diagnosis of Combined Generalized and Focal Epilepsy.
The term “Unknown” is used to denote where it is understood that the patient has Epilepsy but the clinician is unable to determine if the Epilepsy Type is focal or generalized because there is insufficient information available. This may be for a variety of reasons. There may be no access to EEG or the EEG studies may have been uninformative e.g. normal. If the Seizure Type(s) are unknown, then the Epilepsy Type may be unknown for similar reasons although the two may not always be concordant. For example, the patient may have had several symmetrical tonic-clonic seizures without focal features and normal EEG recordings. Thus the onset of the seizures is unknown and the person has an unknown epilepsy type.
3. Epilepsy Syndrome
The third level is an Epilepsy Syndrome diagnosis. An epilepsy syndrome refers to a cluster of features incorporating seizure types, EEG and imaging features that tend to occur together. It often has age-dependent features such as age of onset and remission (where applicable), seizure triggers, diurnal variation and sometimes prognosis 4;5. It may also have distinctive co-morbidities such as intellectual and psychiatric dysfunction, together with specific findings on EEG and imaging studies. It may have associated etiological, prognostic and treatment implications. Importantly, an epilepsy syndrome does not have a one-to-one correlation with an etiological diagnosis and serves a different purpose such as guiding management. There are many well recognised syndromes, such as childhood absence epilepsy, West and Dravet syndromes, although it should be noted that there has never been a formal classification of syndromes by the ILAE 9. The recently developed educational ILAE website, epilepsydiagnosis.org, provides an excellent resource to understand the parameters for diagnosis, review videos of seizure types and the EEG features of many established syndromes and has been devised as a teaching tool.
Idiopathic Generalized Epilepsies
Within the Generalized Epilepsies is the well-recognised and common subgroup of the Idiopathic Generalized Epilepsies (IGEs). The IGEs encompass four well-established epilepsy syndromes: Childhood Absence Epilepsy, Juvenile Absence Epilepsy, Juvenile Myoclonic Epilepsy and Generalized Tonic-Clonic Seizures Alone (formerly known as Generalized Tonic-Clonic Seizures on Awakening but modified in recognition that seizures can occur at any time of day). The intention to remove the term “idiopathic” from the nomenclature of Epilepsy Classification was suggested as its definition was “no known or suspected etiology other than possible hereditary predisposition”5. The Greek term “idios” refers to self, own and personal, and is thus meant to reflect the genetic etiology without explicitly saying so. Idiopathic may therefore be regarded as an imprecise term given our increasing recognition and discovery of the genes involved in many epilepsies, including those with monogenic (with inherited or de novo pathogenic variants) or complex (polygenic with or without environmental factors) inheritance. Also, the word ‘genetic’ may sometimes be wrongly interpreted as synonymous with ‘inherited’.
It is therefore more meaningful to refer to this group of syndromes as Genetic Generalized Epilepsies (GGEs) where the clinician feels there is sufficient evidence for this classification. Such evidence is drawn from meticulous clinical research of the inheritance of these syndromes in twin and family studies and does not mean that specific genetic mutations have been identified. Indeed, it is currently rarely the case that the genetic mutation(s) causing a patient’s epilepsy has been determined, perhaps with the exception of the infantile onset developmental and epileptic encephalopathies where many patients have been shown to have a_de novo_ pathogenic variant 32.
There has been, however, considerable desire to retain the term IGE. The Task Force has therefore decided that the term IGE will be acceptable specifically for the group of four epilepsy syndromes: Childhood Absence Epilepsy, Juvenile Absence Epilepsy, Juvenile Myoclonic Epilepsy and Generalized Tonic-Clonic Seizures Alone. In individual cases, the term Genetic Generalized Epilepsy may be used where the clinician is comfortable with invoking a genetic etiology.
Self-limited focal epilepsies
There are several self-limited focal epilepsies, typically beginning in childhood. The most common is self-limited epilepsy with centrotemporal spikes, formerly called “benign epilepsy with centrotemporal spikes”. Others included in this broad group are the self-limited occipital epilepsies of childhood, with the early-onset form described by Panayiotopoulos and the late-onset form by Gastaut33. Other self-limited frontal lobe34, temporal35 and parietal lobe epilepsies 36 have been described with some beginning in adolescence and even adult life.
Etiology
From the moment that the patient presents with their first epileptic seizure, the clinician should be aiming to determine the etiology of the patient’s epilepsy. A range of etiological groups has been recognised with emphasis on those that have implications for treatment. Often the first investigation carried out involves neuroimaging, ideally MRI where available. This enables the clinician to decide if there is a structural etiology for the patient’s epilepsy. The five additional etiological groups are genetic, infectious, metabolic and immune, as well as an unknown group (Figure). A patient’s epilepsy may be classified into more than one etiological category; the etiologies are not hierarchical and the importance given to the patient’s etiological group may depend on the circumstance. For instance, a patient with tuberous sclerosis has both a structural and a genetic etiology; the structural etiology is critical for epilepsy surgery while the genetic etiology is key for genetic counselling and consideration of novel therapies such as mTOR inhibitors.
1. Structural etiology
The concept behind a structural etiology is that a structural abnormality has a substantially increased risk of being associated with epilepsy based on appropriately designed studies 9. A structural etiology refers to abnormalities visible on structural neuroimaging where the electro-clinical assessment together with the imaging findings lead to a reasonable inference that the imaging abnormality is the likely cause of the patient’s seizures. Structural etiologies may be acquired such as stroke, trauma and infection, or genetic such as many malformations of cortical development. Despite there being a genetic basis with such malformations, the structural correlate underpins the person’s epilepsy. Identification of a subtle structural lesion requires appropriate MRI studies using specific epilepsy protocols 37.
There are well recognized associations within the epilepsies with a structural etiology. These include the relatively frequent finding of mesial temporal lobe seizures with hippocampal sclerosis. Other key associations include gelastic seizures with hypothalamic hamartoma, Rasmussen syndrome, and hemiconvulsion-hemiplegia-epilepsy. Recognition of these associations is important to ensure that the patient’s imaging is carefully examined for a specific structural abnormality. This in turn highlights the need for consideration for epilepsy surgery should the patient fail medical therapy.
The underlying basis for a structural abnormality may be genetic or acquired or both. For example, polymicrogyria may be secondary to mutations in genes such as GPR56, or acquired, secondary to intrauterine cytomegalovirus infection 38. Acquired structural causes include hypoxic-ischemic encephalopathy, trauma, infection and stroke. Where a structural etiology has a well-defined genetic basis such as tuberous sclerosis complex, which is caused by mutations in the genes_TSC1_ and TSC2 encoding hamartin and tuberin respectively, both etiological terms, structural and genetic can be used.
2. Genetic etiology
The concept of a genetic epilepsy is that it directly results from a known or presumed genetic mutation in which seizures are a core symptom of the disorder. The epilepsies in which a genetic etiology has been implicated are quite diverse and, in most cases, the underlying genes are_not_ yet known.
First, the inference of a genetic etiology may be based solely on a family history of an autosomal dominant disorder. For example, in the syndrome of Benign Familial Neonatal Epilepsy, most families have mutations of one of the potassium channel genes, KCNQ2 or_KCNQ3_ 39. Conversely, in the syndrome of Autosomal Dominant Nocturnal Frontal Lobe epilepsy, the underlying mutation is only known in a small proportion of individuals at this time 40.
Second, a genetic etiology may be suggested by clinical research in populations with the same syndrome such as Childhood Absence Epilepsy or Juvenile Myoclonic Epilepsy. Evidence for a genetic basis comes from elegant studies such as Lennox’s twin studies in the 1950s and familial aggregation studies 41;42.
Third, a molecular basis may have been identified and implicate a single gene or copy number variant of major effect. There is an increasing number of patients with known genetic abnormalities causing both severe and mild epilepsies. Molecular genetics has led to identification of the causative mutation in a large number of epilepsy genes, most frequently arising de novo, in 30% to 50% of infants with severe developmental and epileptic encephalopathies 32.
The best known example is Dravet syndrome in which more than 80% of patients have a pathogenic variant of SCN1A. Importantly, a monogenic etiology may cause a spectrum of mild to severe epilepsies, such as SCN1A mutations which are associated with Dravet syndrome and Genetic Epilepsy with Febrile Seizures Plus (GEFS+), and may have implications for treatment 43;44. Understanding the phenotypic spectrum associated with mutations of a specific gene is critical information as the finding of a mutation in a specific gene may not, on its own, enable prediction of the outcome. Interpretation of its significance needs to be considered in the context of the electroclinical presentation. Thus, to date, the majority of genes show phenotypic heterogeneity and the majority of syndromes reveal genetic heterogeneity.
Where epilepsy follows complex inheritance, which implies multiple genes with/without an environmental contribution, susceptibility variants may be identified which contribute to causation but are insufficient alone to cause epilepsy 45;46. In this setting, there may be no family history of seizures as other family members do not have enough epilepsy genetic variants to be affected.
Importantly, genetic does not equate to inherited. An increasing number of de novo mutations is being identified in both severe and mild epilepsies 47–52. This means that the patient has a new mutation that has arisen in him or her, and therefore is unlikely to have a family history of seizures and has not inherited the genetic mutation. Nevertheless, this patient may now have a heritable form of epilepsy. For example if the individual has a de novo dominant mutation, their offspring will have a 50% risk of inheriting the mutation. This does not necessarily mean that their children will have epilepsy as its expression will depend on the penetrance of the mutation.
Drilling down further, patients may be mosaic for a mutation. This means they have two populations of cells, with one population having the mutation and the other having the wild type (normal) allele. Mosaicism may impact on the severity of their epilepsy with lower mosaicism rates resulting in a milder severity of their epilepsy, as shown in_SCN1A_ studies 53.
A genetic etiology does not exclude an environmental contribution. It is well accepted that environmental factors contribute to seizure disorders; for example, many individuals with epilepsy are more likely to have seizures with sleep deprivation, stress and illness. A genetic etiology refers to a pathogenic variant (mutation) of significant effect in causing the individual’s epilepsy.
3. Infectious etiology
The commonest etiology worldwide is where epilepsy occurs as a result of an infection 54. The concept of an infectious etiology is that it directly results from a known infection in which seizures are a core symptom of the disorder. An infectious etiology refers to a patient with epilepsy, rather than with seizures occurring in the setting of acute infection such as meningitis or encephalitis. Common examples in specific regions of the world include neurocysticercosis, tuberculosis, HIV, cerebral malaria, subacute sclerosing panencephalitis, cerebral toxoplasmosis and congenital infections such as Zika virus and cytomegalovirus. These infections sometimes have a structural correlate. An infectious etiology carries specific treatment implications. An infectious etiology may also refer to the post-infectious development of epilepsy, such as viral encephalitis leading to seizures in the aftermath of the acute infection.
4. Metabolic etiology
A range of metabolic disorders is associated with epilepsy. This area is expanding and a greater understanding of the phenotypic spectrum emerging. The concept of a metabolic epilepsy is that it directly results from a known or presumed metabolic disorder in which seizures are a core symptom of the disorder. Metabolic causes refer to a well delineated metabolic defect with manifestations or biochemical changes throughout the body such as porphyria, uremia, amino-acidopathies or pyridoxine dependent seizures. In many cases, metabolic disorders will have a genetic defect. It is likely that the vast majority of metabolic epilepsies will have a genetic basis but some may be acquired such as cerebral folate deficiency. The identification of specific metabolic causes of epilepsy is extremely important due to implications for specific therapies and potential prevention of intellectual impairment.
5. Immune etiology
The concept of an immune epilepsy is that it directly results from an immune disorder in which seizures are a core symptom of the disorder. A range of immune epilepsies has been recently recognized with characteristic presentations in both adults and children 54. An immune etiology can be conceptualized as where there is evidence of autoimmune-mediated central nervous system inflammation. Diagnosis of these autoimmune encephalitides is rapidly increasing, particularly with greater access to antibody testing. Examples include anti-NMDA receptor encephalitis and anti-LGI1 encephalitis55. With the emergence of these entities, this etiological subgroup deserves a specific category particularly given the treatment implications with targeted immunotherapies.
6. Unknown etiology
Unknown means that the cause of the epilepsy is not yet known. There remain many patients with epilepsy for whom the cause is not known. In this category it is not possible to make a specific diagnosis apart from the basic electroclinical semiology such as frontal lobe epilepsy. The extent to which a cause can be found depends on the extent of the evaluation available to the patient. This differs across different health care settings and countries and hopefully will improve over time in resource poor countries.
Co-morbidities
There is increasing awareness that many of the epilepsies are associated with co-morbidities such as learning, psychological and behavioural problems (Figure, left hand vertical oval). These range in type and severity, from subtle learning difficulties to intellectual disability, to psychiatric features such as autism spectrum disorders and depression, to psychosocial concerns. In the more severe epilepsies, a complex range of co-morbidities may be seen, including motor deficits such as cerebral palsy or deterioration in gait, movement disorders, scoliosis, sleep and gastro-intestinal disorders. Like etiology, it is important that the presence of co-morbidities be considered for every patient with epilepsy at each stage of classification, enabling early identification, diagnosis and appropriate management.
New terminology and definitions
Developmental and epileptic encephalopathies
The term “epileptic encephalopathy” was re-defined in the Berg et al. 2010 9 report as where the epileptic activity itself contributes to severe cognitive and behavioral impairments above and beyond what might be expected from the underlying pathology alone (e.g. cortical malformation). Global or selective impairments can worsen over time. These impairments can be seen along a spectrum of severity and across all epilepsies and can occur at any age.
The concept of the epileptic encephalopathy may be applicable to epilepsies at all ages and should be utilised more widely than just for the severe epilepsies with onset in infancy and childhood. Many epilepsy syndromes associated with encephalopathy have a genetic etiology, such as West syndrome where there is marked genetic heterogeneity, and Epileptic encephalopathy with continuous spike-and-wave during sleep (CSWS), where the first genes have begun to emerge 32. Equally, such syndromes may have an acquired cause such as hypoxic-ischemic encephalopathy or stroke, or may be associated with a malformation of cortical development that may also have a genetic or acquired etiology.
The concept of an epileptic encephalopathy can also be applied to single gene disorders, such as CDKL5 encephalopathy and_CHD2_ encephalopathy. However, a single gene may cause an epileptic encephalopathy in some individuals and a self-limited epilepsy in others; examples include SCN1A, SCN2A, SLC2A1, KCNQ2, KCNA2 and_CHD2_. In an epileptic encephalopathy, the abundant epileptiform activity interferes with development resulting in cognitive slowing and often regression, and sometimes is associated with psychiatric and behavioural consequences. The epileptiform activity can cause regression in an individual with normal development or pre-existing developmental delay, who then shows developmental plateauing or regression. A key component of the concept is that amelioration of the epileptiform activity may have the potential to improve the developmental consequences of the disorder. This is a critical issue from a clinical perspective and one often mirrored in the observations of families and clinicians.
Many of these severe genetic disorders also have developmental consequences arising directly from the effect of the genetic mutation, in addition to the effect of the frequent epileptic activity on development. There are several ways in which this may manifest. There may be pre-existing developmental delay, complicated by plateauing or regression with seizure onset or with prolonged seizures. In other disorders, developmental slowing may occur on a background of normal development, with the slowing emerging prior to the presence of frequent epileptic activity on the EEG. A well-known example is the relatively common encephalopathy of Dravet syndrome, in which developmental slowing or regression occurs between one and two years of age, at a time when epileptiform activity on EEG is typically not yet frequent. This suggests a developmental component in addition to an epileptic component, with both occurring secondary to the underlying sodium channel subunit gene (SCN1A) mutation found in >80% of cases. In a third group, the epilepsy may settle down relatively early in the child’s history but the developmental consequences may remain profound as seen in some patients with KCNQ2 encephalopathy or_STXBP1_ encephalopathy. These observations, pertinent to many of the genetic encephalopathies, suggest that a broadening of the terminology, where appropriate, to include the word “developmental” acknowledges that both aspects may be playing a role in the clinical presentation. These concepts are crucial to understanding the disease process for both families and clinicians.
It is therefore suggested that the term “developmental_and_ epileptic encephalopathy” be used where appropriate and can be applied to individuals of any age. This allows for the use of either or both descriptors: developmental encephalopathy where there is just developmental impairment without frequent epileptic activity associated with regression or further slowing of development; epileptic encephalopathy where there is no pre-existing developmental delay and the genetic mutation is not thought to cause slowing in its own right; and developmental and epileptic encephalopathy where both factors play a role. Often it may not be possible to disentangle whether the epileptic or developmental component is more important in contributing to a patient’s presentation.
Many patients with these disorders have previously been classified as ‘symptomatic generalized epilepsies’; however, this term will no longer be used as it was applied to a highly heterogeneous group of patients. This term has been applied to patients with developmental encephalopathies and epilepsy (eg. static intellectual disability and mild epilepsy), those with epileptic encephalopathies, those with developmental and epileptic encephalopathies as well as some patients with generalized epilepsy or combined generalized and focal epilepsy. The new classification will allow more precise classification of these individuals’ epilepsy.
In many instances, where a genetic mutation of major effect is identified, the terms ‘developmental and epileptic encephalopathy’ may be subsumed by using the name of the underlying condition. For example, many of the well recognised developmental and epileptic encephalopathies can now be called by their gene name together with the word encephalopathy, such as “STXBP1 encephalopathy” or “KCNQ2 encephalopathy”. This is particularly important when referring to a genetic disease where genes are associated with both severe and self-limited, pharmacoresponsive epilepsies, such as_KCNQ2_ or SCN2A. Then the term “encephalopathy” can be used to denote the severe form of the disease associated with developmental impairment.
Self-limited and pharmacoresponsive
With increasing recognition of the impact of these co-morbidities on an individual’s life, there has been considerable concern that the term “benign” underestimates this burden particularly in the milder epilepsy syndromes such as benign epilepsy with centrotemporal spikes (BECTS) and childhood absence epilepsy (CAE). Despite the gestalt of a benign syndrome, BECTS may be associated with transient or long-lasting cognitive effects56;57 and CAE with significant psychosocial consequences such as increased risk of early pregnancy 58.
The Berg et al report 9suggested new terms to distil the elements implied in the term “benign”. Thus “benign”, as a descriptor for epilepsy, is replaced by both “self-limited” and “pharmacoresponsive”, each replacing different components of the meaning of benign. “Self-limited” refers to the likely spontaneous resolution of a syndrome. “Pharmacoresponsive” means that the epilepsy syndrome will be likely to be controlled with appropriate anti-epileptic therapy. It is important to acknowledge, however, that there will be individuals with these syndromes who are not pharmacoresponsive. As noted previously there is no formal ILAE classification of syndromes however we expect the word benign in time will be replaced in the names of specific syndromes. The terms “malignant” and “catastrophic” will no longer be used; they will be removed from the epilepsy lexicon because of their serious and devastating connotations.
It is hoped that this new Classification of the Epilepsies will serve the epilepsy community well, leading to improved diagnosis, understanding of etiology and targeted therapies to the patient’s disease. It is notable that even where the etiology is clearly defined, the underlying mechanism producing recurrent seizures still requires elucidation. With the advent of significant advances in understanding the neurobiology of seizures and epileptic diseases, there have been major paradigm shifts in the concepts underpinning classification. This Classification is designed to mirror current understanding, so that it is relevant to clinical practice as the pre-eminent tool for communication in both clinical and research domains.
Key points.
- The ILAE presents a revised framework for the Classification of the Epilepsies, designed to work with the classification of seizure types.
- Levels of diagnosis: seizure type, epilepsy type (focal, generalized, combined generalized and focal, unknown) and epilepsy syndrome.
- An etiological diagnosis should be considered from when the patient first presents, and at each step along the diagnostic pathway. A patient’s epilepsy may be classified into more than one etiological category.
- The term ‘benign’ is replaced by the terms self-limited and pharmacoresponsive to be used where appropriate.
- The term ‘developmental and epileptic encephalopathy’ can be applied in whole or in part where appropriate.
APPENDIX
Disclosures
Ingrid Scheffer received support from, and/or has served as a paid consultant for UCB, Eisai, Athena Diagnostics, GlaxoSmithKline, Transgenomics and Biocodex. She serves on the editorial board of _Neurology_and Epileptic Disorders. She has received grants from the NHMRC, ARC, NIH, HRC, CURE, US Department of Defense, and March of Dimes.
Samuel Berkovic discloses payments from UCB Pharma, Novartis Pharmaceuticals, Sanofi-Aventis, and Jansen Cilag for advisory board and educational activities and a patent for SCN1A testing held by Bionomics Inc licensed to various diagnostic companies.
Giuseppe Capovilla serves on the editorial board of the European Journal of Pediatric Neurology.
Mary Connolly has received research grants and/or speakers honoraria from UCB, Novartis, Biocodex, Eisai and Sage Therapeutics. All honoraria are donated to the Epilepsy Research and Development Fund. She has also received research grants from CIHR (Canadian Institute for Health Research) and The Alva Foundation. She is Co-Chair of the Canadian Paediatric Epilepsy Network.
Jacqueline French: The Epilepsy Study Consortium pays her university employer for her consultant time related to Acorda, Anavex, Brabant Pharma, Bio-Pharm Solutions, Eisai Medical Research, Glaxo Smith-Kline, GW Pharma, Impax, Johnson and Johnson, Marinus, Neusentis, Novartis, Roivant, Pfizer, Sage, Sunovion, SK life sciences, Supernus Pharmaceuticals, Takeda, UCB, Upsher-Smith, Ultragenyx, Vertex, Zogenix, Zynerba, Scientific Advisory Board for Anavex, UCB, grants and research from Acorda, Alexza, LCGH, Eisai Medical Research, Lundbeck, Pfizer, SK life sciences, UCB, Upsher-Smith, Vertex, grants from NINDS, Epilepsy Therapy Project, Epilepsy Research Foundation, Epilepsy Study Consortium; She is on the editorial board of Lancet Neurology, Neurology Today and Epileptic disorders, and is an Associate Editor of Epilepsia, for which she receives a fee.
Laura Guilhoto: serves on the editorial board of Seizure - European Journal of Epilepsy.
Edouard Hirsch has received support from UCB, and/or has served as a paid consultant for UCB, ESAI, BIAL.
Satish Jain has no disclosures.
Gary Mathern is partially supported by the Davies/Crandall Chair for Epilepsy Research at UCLA and is co-editor in chief for_Epilepsia_ and Epilepsia Open. He is also on the editorial board of Neurology, and the Data Management Committee for NeuroPace, Inc.
Solomon L. Moshé MD is the Charles Frost Chair in Neurosurgery and Neurology and funded by grants from NIH NS43209 and 1U54NS100064-01, CURE Infantile Spasms Initiative, US Department of Defense (W81XWH-13-1-0180), the Heffer Family and the Segal Family Foundations and the Abbe Goldstein/Joshua Lurie and Laurie Marsh/Dan Levitz families. He serves as Associate Editor of Neurobiology of Disease, and is on the editorial board of Brain and Development, Pediatric Neurology and Physiological Research. He receives from Elsevier an annual compensation for his work as Associate Editor in Neurobiology of Disease and royalties from 2 books he co-edited. He received a consultant’s fee from Eisai and UCB.
Douglas Nordli: is funded from NIH (1-RO1-NS43209) and CURE. He is an Associate Editor for UpToDate.
Emilio Perucca has received speaker’s or consultancy fees and/or research grants from the following pharmaceutical companies: Eisai, Biopharm Solutions, GW Pharma, Mylan, Sanofi, SK life sciences, Sun Pharma, Takeda, and UCB Pharma.
Torbjörn Tomson has received research grants and/or speakers honoraria to his institution from the following pharmaceutical companies: Eisai, GlaxoSmithKline, Novartis, Bial, and UCB. He has also received research grants from CURE, Stockholm County Council, and EU (DG Sante).
Samuel Wiebe has received speaker’s or consultancy fees and/or research/educational grants from UCB, Electrocore and Sunovion.
Yue-Hua Zhang has no disclosures.
Sameer Zuberi has received research support and or speaker’ honoraria/consultancy fees from Epilepsy Research UK, Dravet Syndrome UK, UCB Pharma, Yorkhill Children’s Charity, GW Pharma, Brabant Pharma and Zogenix. He is Editor-in-Chief of the European Journal of Paediatric Neurology.
Footnotes
We confirm that we have read the Journal’s position on issues involved in ethical publication and affirm that this report is consistent with those guidelines.
References
- 1.Gastaut H, Caveness WF, Landolt W, et al. A proposed international classification of epileptic seizures. Epilepsia. 1964;5:297–306. doi: 10.1111/j.1528-1157.1964.tb03337.x. [DOI] [PubMed] [Google Scholar]
- 2.Gastaut H. Clinical and electroencephalographical classification of epileptic seizures. Epilepsia. 1969;10(Suppl):2–13. [PubMed] [Google Scholar]
- 3.Gastaut H. Classification of the epilepsies. Proposal for an international classification. Epilepsia. 1969;10(Suppl):14–21. [PubMed] [Google Scholar]
- 4.Commission on Classification and Terminology of the International League Against Epilepsy. Proposal for classification of epilepsies and epileptic syndromes. Epilepsia. 1985;26:268–278. [PubMed] [Google Scholar]
- 5.Commission on Classification and Terminology of the International League Against Epilepsy. Proposal for revised classification of epilepsies and epileptic syndromes. Epilepsia. 1989;30:389–399. doi: 10.1111/j.1528-1157.1989.tb05316.x. [DOI] [PubMed] [Google Scholar]
- 6.Commission on Classification and Terminology of the International League Against Epilepsy. Proposal for revised clinical and electroencephalographic classification of epileptic seizures. Epilepsia. 1981;22:489–501. doi: 10.1111/j.1528-1157.1981.tb06159.x. [DOI] [PubMed] [Google Scholar]
- 7.Engel J., Jr A proposed diagnostic scheme for people with epileptic seizures and with epilepsy: report of the ILAE Task Force on Classification and Terminology. Epilepsia. 2001;42:796–803. doi: 10.1046/j.1528-1157.2001.10401.x. [DOI] [PubMed] [Google Scholar]
- 8.Engel J. Report of the ILAE classification core group. Epilepsia. 2006;47:1558–1568. doi: 10.1111/j.1528-1167.2006.00215.x. [DOI] [PubMed] [Google Scholar]
- 9.Berg AT, Berkovic SF, Brodie MJ, et al. Revised terminology and concepts for organization of seizures and epilepsies: report of the ILAE Commission on Classification and Terminology, 2005–2009. Epilepsia. 2010;51:676–685. doi: 10.1111/j.1528-1167.2010.02522.x. [DOI] [PubMed] [Google Scholar]
- 10.Fisher RS, Cross JH, French JA, et al. Operational classification of seizure types by the International League Against Epilepsy. Epilepsia. 2017 Mar 8; doi: 10.1111/epi.13671. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 11.Epilepsy ILa. [Accessed 2nd July 2015];Guidelines for Publications from League Commissions and Task Forces. 2014 Available at: http://www.ilae.org/visitors/centre/guidelines.cfm.
- 12.Avanzini G. A sound conceptual framework for an epilepsy classification is still lacking. Epilepsia. 2010;51:720–722. doi: 10.1111/j.1528-1167.2010.02531.x. [DOI] [PubMed] [Google Scholar]
- 13.Beghi E. New classification proposals for epilepsy: a real advancement in the nosography of the disease? Epilepsia. 2011;52:1197–1198. doi: 10.1111/j.1528-1167.2011.03090.x. discussion 1205–1199. [DOI] [PubMed] [Google Scholar]
- 14.Berg AT, Scheffer IE. New concepts in classification of the epilepsies: entering the 21st century. Epilepsia. 2011;52:1058–1062. doi: 10.1111/j.1528-1167.2011.03101.x. [DOI] [PubMed] [Google Scholar]
- 15.Berg AT, Scheffer IE. What is at stake in a classification? Epilepsia. 2011;52:1205–1208. [Google Scholar]
- 16.Camfield P. Issues in epilepsy classification for population studies. Epilepsia. 2012;53(Suppl 2):10–13. doi: 10.1111/j.1528-1167.2012.03552.x. [DOI] [PubMed] [Google Scholar]
- 17.Duncan JS. The evolving classification of seizures and epilepsies. Epilepsia. 2011;52:1204–1205. doi: 10.1111/j.1528-1167.2011.03106.x. discussion 1205–1209. [DOI] [PubMed] [Google Scholar]
- 18.Engel J., Jr The etiologic classification of epilepsy. Epilepsia. 2011;52:1195–1197. doi: 10.1111/j.1528-1167.2011.03065.x. discussion 1205–1209. [DOI] [PubMed] [Google Scholar]
- 19.Ferrie CD. Terminology and organization of seizures and epilepsies: radical changes not justified by new evidence. Epilepsia. 2010;51:713–714. doi: 10.1111/j.1528-1167.2010.02540.x. [DOI] [PubMed] [Google Scholar]
- 20.Fisher RS. What is a classification essay? Epilepsia. 2010;51:714–715. doi: 10.1111/j.1528-1167.2010.02541.x. [DOI] [PubMed] [Google Scholar]
- 21.Guerrini R. Classification concepts and terminology: is clinical description assertive and laboratory testing objective? Epilepsia. 2010;51:718–720. doi: 10.1111/j.1528-1167.2010.02530.x. [DOI] [PubMed] [Google Scholar]
- 22.Jackson G. Classification of the epilepsies 2011. Epilepsia. 2011;52:1203–1204. doi: 10.1111/j.1528-1167.2011.03093.x. discussion 1205–1209. [DOI] [PubMed] [Google Scholar]
- 23.Moshe SL. In support of the ILAE Commission classification proposal. Epilepsia. 2011;52:1200–1201. doi: 10.1111/j.1528-1167.2011.03077.x. discussion 1205–1209. [DOI] [PubMed] [Google Scholar]
- 24.Luders HO, Amina S, Baumgartner C, et al. Modern technology calls for a modern approach to classification of epileptic seizures and the epilepsies. Epilepsia. 2012;53:405–411. doi: 10.1111/j.1528-1167.2011.03376.x. [DOI] [PubMed] [Google Scholar]
- 25.Panayiotopoulos CP. The new ILAE report on terminology and concepts for the organization of epilepsies: critical review and contribution. Epilepsia. 2012;53:399–404. doi: 10.1111/j.1528-1167.2011.03381.x. [DOI] [PubMed] [Google Scholar]
- 26.Shinnar S. The new ILAE classification. Epilepsia. 2010;51:715–717. doi: 10.1111/j.1528-1167.2010.02542.x. [DOI] [PubMed] [Google Scholar]
- 27.Shorvon SD. The etiologic classification of epilepsy. Epilepsia. 2011;52:1052–1057. doi: 10.1111/j.1528-1167.2011.03041.x. [DOI] [PubMed] [Google Scholar]
- 28.Wolf P. Much ado about nothing? Epilepsia. 2010;51:717–718. doi: 10.1111/j.1528-1167.2010.02529.x. [DOI] [PubMed] [Google Scholar]
- 29.Wong M. Epilepsy is both a symptom and a disease: a proposal for a two-tiered classification system. Epilepsia. 2011;52:1201–1203. doi: 10.1111/j.1528-1167.2011.03078.x. discussion 1205–1209. [DOI] [PubMed] [Google Scholar]
- 30.Scheffer I, French J, Hirsch E, et al. Clasification of the epilepsies: New concepts for discussion and debate - Special report of the ILAE Classification Task Force of the Commission for Classification and Terminology. Epilepsia Open. 2016;1:37–44. doi: 10.1002/epi4.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fisher RS, Acevedo C, Arzimanoglou A, et al. ILAE official report: a practical clinical definition of epilepsy. Epilepsia. 2014;55:475–482. doi: 10.1111/epi.12550. [DOI] [PubMed] [Google Scholar]
- 32.McTague A, Howell KB, Cross JH, et al. The genetic landscape of the epileptic encephalopathies of infancy and childhood. Lancet Neurol. 2016;15:304–316. doi: 10.1016/S1474-4422(15)00250-1. [DOI] [PubMed] [Google Scholar]
- 33.Guerrini R, Pellacani S. Benign childhood focal epilepsies. Epilepsia. 2012;53(Suppl 4):9–18. doi: 10.1111/j.1528-1167.2012.03609.x. [DOI] [PubMed] [Google Scholar]
- 34.Beaumanoir A, Nahory A. Benign partial epilepsies: 11 cases of frontal partial epilepsy with favorable prognosis. Rev Electroencephalogr Neurophysiol Clin. 1983;13:207–211. doi: 10.1016/s0370-4475(83)80029-x. [DOI] [PubMed] [Google Scholar]
- 35.Berkovic SF, McIntosh A, Howell RA, et al. Familial temporal lobe epilepsy: a common disorder identified in twins. Ann Neurol. 1996;40:227–235. doi: 10.1002/ana.410400214. [DOI] [PubMed] [Google Scholar]
- 36.Sveinbjornsdottir S, Duncan JS. Parietal and occipital lobe epilepsy: a review. Epilepsia. 1993;34:493–521. doi: 10.1111/j.1528-1157.1993.tb02590.x. [DOI] [PubMed] [Google Scholar]
- 37.Gaillard WD, Chiron C, Cross JH, et al. Guidelines for imaging infants and children with recent-onset epilepsy. Epilepsia. 2009;50:2147–2153. doi: 10.1111/j.1528-1167.2009.02075.x. [DOI] [PubMed] [Google Scholar]
- 38.Guerrini R, Dobyns WB. Malformations of cortical development: clinical features and genetic causes. Lancet Neurol. 2014;13:710–726. doi: 10.1016/S1474-4422(14)70040-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Grinton BE, Heron SE, Pelekanos JT, et al. Familial neonatal seizures in 36 families: Clinical and genetic features correlate with outcome. Epilepsia. 2015;56:1071–1080. doi: 10.1111/epi.13020. [DOI] [PubMed] [Google Scholar]
- 40.Tinuper P, Bisulli F, Cross JH, et al. Definition and diagnostic criteria of sleep-related hypermotor epilepsy. Neurology. 2016;86:1834–1842. doi: 10.1212/WNL.0000000000002666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lennox WG. The genetics of epilepsy. American Journal of Psychiatry. 1947;103:457–462. doi: 10.1176/ajp.103.4.457. [DOI] [PubMed] [Google Scholar]
- 42.Lennox WG. The heredity of epilepsy as told by relatives and twins. Journal of the American Medical Association. 1951;146:529–536. doi: 10.1001/jama.1951.03670060005002. [DOI] [PubMed] [Google Scholar]
- 43.Brunklaus A, Dorris L, Ellis R, et al. The clinical utility of an SCN1A genetic diagnosis in infantile-onset epilepsy. Dev Med Child Neurol. 2013;55:154–161. doi: 10.1111/dmcn.12030. [DOI] [PubMed] [Google Scholar]
- 44.Mullen SA, Scheffer IE. Translational research in epilepsy genetics: sodium channels in man to interneuronopathy in mouse. Arch Neurol. 2009;66:21–26. doi: 10.1001/archneurol.2008.559. [DOI] [PubMed] [Google Scholar]
- 45.Helbig I, Mefford H, Sharp A, et al. 15q13. 3 microdeletions increase risk of idiopathic generalized epilepsy. Nat Genet. 2009;41:160–162. doi: 10.1038/ng.292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Dibbens LM, Mullen S, Helbig I, et al. Familial and sporadic 15q13. 3 microdeletions in idiopathic generalized epilepsy: precedent for disorders with complex inheritance. Hum Mol Genet. 2009;18:3626–3631. doi: 10.1093/hmg/ddp311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Claes L, Del-Favero J, Ceulemans B, et al. De novo mutations in the sodium-channel gene SCN1A cause severe myoclonic epilepsy of infancy. Am J Hum Genet. 2001;68:1327–1332. doi: 10.1086/320609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Weckhuysen S, Mandelstam S, Suls A, et al. KCNQ2 encephalopathy: Emerging phenotype of a neonatal epileptic encephalopathy. Ann Neurol. 2012;71:15–25. doi: 10.1002/ana.22644. [DOI] [PubMed] [Google Scholar]
- 49.Depienne C, Bouteiller D, Keren B, et al. Sporadic infantile epileptic encephalopathy caused by mutations in PCDH19 resembles Dravet syndrome but mainly affects females. PLoS Genet. 2009;5:e1000381. doi: 10.1371/journal.pgen.1000381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Arsov T, Mullen SA, Rogers S, et al. Glucose transporter 1 deficiency in the idiopathic generalized epilepsies. Ann Neurol. 2012;72:807–815. doi: 10.1002/ana.23702. [DOI] [PubMed] [Google Scholar]
- 51.Scheffer IE, Grinton BE, Heron SE, et al. PRRT2 phenotypic spectrum includes sporadic and fever-related infantile seizures. Neurology. 2012;79:2104–2108. doi: 10.1212/WNL.0b013e3182752c6c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Carvill GL, Heavin SB, Yendle SC, et al. Targeted resequencing in epileptic encephalopathies identifies de novo mutations in CHD2 and SYNGAP1. Nature Genetics. 2013;45:825–830. doi: 10.1038/ng.2646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Depienne C, Trouillard O, Gourfinkel-An I, et al. Mechanisms for variable expressivity of inherited SCN1A mutations causing Dravet syndrome. J Med Genet. 2010;47:404–410. doi: 10.1136/jmg.2009.074328. [DOI] [PubMed] [Google Scholar]
- 54.Vezzani A, Fujinami RS, White HS, et al. Infections, inflammation and epilepsy. Acta Neuropathol. 2016;131:211–234. doi: 10.1007/s00401-015-1481-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lancaster E, Dalmau J. Neuronal autoantigens--pathogenesis, associated disorders and antibody testing. Nat Rev Neurol. 2012;8:380–390. doi: 10.1038/nrneurol.2012.99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Staden UE, Isaacs E, Boyd SG, et al. Language dysfunction in children with rolandic epilepsy. Neuropediatrics. 1998;29:242–248. doi: 10.1055/s-2007-973569. [DOI] [PubMed] [Google Scholar]
- 57.Lillywhite LM, Saling MM, Harvey AS, et al. Neuropsychological and functional MRI studies provide converging evidence of anterior language dysfunction in BECTS. Epilepsia. 2009;50:2276–2284. doi: 10.1111/j.1528-1167.2009.02065.x. [DOI] [PubMed] [Google Scholar]
- 58.Wirrell EC, Camfield CS, Camfield PR, et al. Long-term psychosocial outcome in typical absence epilepsy. Sometimes a wolf in sheeps’ clothing. Arch Pediatr Adolesc Med. 1997;151:152–158. doi: 10.1001/archpedi.1997.02170390042008. [DOI] [PubMed] [Google Scholar]