Safety of Acupuncture: Overview of Systematic Reviews (original) (raw)
Abstract
Acupuncture is increasingly used worldwide. It is becoming more accepted by both patients and healthcare providers. However, the current understanding of its adverse events (AEs) is fragmented. We conducted this overview to collect all systematic reviews (SRs) on the AEs of acupuncture and related therapies. MEDLINE and EMBASE were searched from inception to December 2015. Methodological quality of included reviews was assessed with a validated instrument. Evidence was narratively reported. Seventeen SRs covering various types of acupuncture were included. Methodological quality of the reviews was overall mediocre. Four major categories of AEs were identified, which are organ or tissue injuries (13 reviews, median: 36 cases, median deaths: 4), infections (11 reviews, median: 17 cases, median deaths: 0.5), local AEs or reactions (12 reviews, median: 8.5 cases, no deaths were reported), and other complications such as dizziness or syncope (11 reviews, median: 21 cases, no deaths were reported). Minor and serious AEs can occur during the use of acupuncture and related modalities, contrary to the common impression that acupuncture is harmless. Serious AEs are rare, but need significant attention as mortality can be associated with them. Referrals should consider acupuncturists’ training credibility, and patient safety should be a core part of acupuncture education.
Introduction
In China, it is estimated that nine hundred million traditional Chinese Medicine consultations took place in 2009, of which acupuncture is a significant part of ref. 1. Often, related therapies, such as electro-acupuncture, auricular therapy, moxibustion, cupping, and transcutaneous electrical nerve stimulation (TENS) are also used in conjunction with acupuncture or on their own as a modality of treatment for various ailments and medical diseases. Traditional needle acupuncture has been gaining increasing popularity beyond China, as patients are becoming increasingly aware of and accepting of said acupuncture and its related modalities in the West. In the UK, approximately 4 million acupuncture sessions were offered to patients in 2009, with about two-third provided beyond the National Health Service2. In America, 3.1 million adults and 150,000 children used acupuncture in 20073, which increased approximately by 1 million since 20024. In 2003, 11% of Canadian adults sought help from complementary and alternative medicine (CAM), 2% of whom visited acupuncturists5.
In the UK, acupuncture and related therapies are most popular amongst patients with musculoskeletal pain and neurological conditions like headache and migraine2. Besides acupuncturists, it is also practiced by doctors, nurses, and physiotherapists with varying levels of training2. Although it is a common impression that acupuncture and related therapies are safe procedures, both minor and serious adverse events can occur during its use. Many publications have reported these adverse events but they are hard for clinicians to digest as they were written in inconsistent formats. The goal of this overview is to synthesize comprehensively existing systematic reviews on adverse events associated with acupuncture and related therapies, thus informing clinicians, acupuncturists, and patients alike on applying such treatments in a clinically mindful manner.
Results
Results on literature search and selection
Electronic database search identified 1,597 citations, with 387 duplicates that were excluded before the screening process. Among the remaining 1,210 records, 1,183 were excluded based on title and abstract screening, leaving 17 publications for full text assessments. All of the 17 were found to be eligible and were included in the present overview. See Fig. 1 for the flow diagram of literature search and selection.
Figure 1.
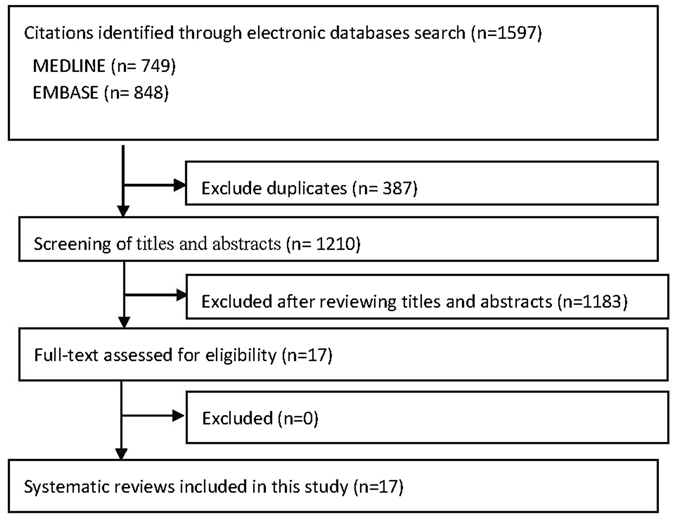
Flowchart of literature selection on systematic reviews of acupuncture related adverse events.
Characteristics of included reviews
The 17 reviews were published between 1996 to 2015. The included reviews reported adverse events from a median of 43 primary studies (range, 9 to 167) and a median of 279 patients (range, 21 to 111,692). All 17 reviews were published in English. Seven (41.2%) reviews included only case reports, and the rest (10, 58.8%) included multiple study designs, including randomized or non-randomized clinical trials, cohort studies, case-control studies, cross-sectional studies, and case series. One review (5.9%) focused only on auricular acupuncture and related auricular therapies6, one (5.9%) focused only on electro-acupuncture7, six (35.3%) focused only on needle acupuncture8–13, three (17.6%) did not limit the type of acupuncture or related intervention that were included14–16, and the remaining six (35.3%) included two or more modalities, including needle acupuncture, electro-acupuncture, cupping, moxibustion, laser acupuncture, indwelling needles, dry needling, bee venom acupuncture, acupuncture point injection, and acupressure17–22. Four reviews (23.5%) included studies from China only7, 10, 17, 19, one (5.9%) included studies from the United States only8, one (5.9%) included studies from Norway only13, one (5.9%) included studies from Japan only12, and one (5.9%) included studies from the UK only11. The remaining reviews (9, 52.9%) included studies from two or more countries. See Table 1 for full details.
Table 1.
Characteristics of included systematic reviews on acupuncture related adverse events.
| First author and year of publication | Included study designs | Country of origin of included studies | Search period | Nature of acupuncture and related interventions | No. of studies (No. of patients) included |
|---|---|---|---|---|---|
| Norheim, 1996 | Case reports | Norway | 1981–1994 | Needle acupuncture | 78 (193) |
| Ernst, 2001 | Prospective studies | 5 countries in Europe, 4 countries in the Far East (Czechoslovakia, Sweden, Germany, Singapore, and Taiwan were reported) | Inception - 1999 | Needle acupuncture, electro-acupuncture, cupping, moxibustion, laser acupuncture, or indwelling needles | 9 (111, 692; including control group) |
| Yamashita, 2001 | Case reports | Japan | 1987–1999 | Needle acupuncture | 89 (124) |
| Ernst, 2003 | Cohort, case-control, and cross sectional studies | United Kingdom | Inception – 2001 | Needle acupuncture | 15 (45922; including control group) |
| Lao, 2003 | Case reports | United Kingdom, Germany, Belgium, United States, Israel, Ireland, New Zealand, Korea, Scotland, France, Norway, Japan, Taiwan, Australia, Canada, Brazil, Turkey, Italy, Spain, Nigeria, India, and China | 1965–1999 | Not stated | 98 (202) |
| Bergqvist, 2008 | Case reports | Not stated | Inception - NS | Needle acupuncture or electro-acupuncture | 21 (21) |
| Zhang, 2010 | Case reports and case series | China | 1980–2009 | Needle acupuncture | 115 (479) |
| Adam, 2011 | RCTs, cohort studies, case reports, and case series | Israel, China, France, Taiwan, Japan, United States, Canada, Hong Kong, Germany, United Kingdom | 1950–2010 | Needle acupuncture | 37 (279) |
| Ernst, 2011a | Case reports and case series | Taiwan, Kapan, Hong Kong, China, Korea, Lima, United States, Canada, Malaysia, Australia, Croatia, Spain, France, Thailand, Ireland, United Kingdom, Spain, Holland, Singapore, Germany, and Switzerland | 2000–2009 | Needle acupuncture, dry needling, electro-acupuncture, bee venom acupuncture, laser acupuncture | 94 (95) |
| Ernst, 2011b | Case reports and case series | China, Austria, Canada, France, India, Japan, Korea, Norway, and the United States | Inception - NS | Not stated | 17 (26) |
| He, 2012 | Case reports | China | 1949–2010 | Needle acupuncture, moxibustion, cupping, electro-acupuncture, laser acupuncture, auricular acupuncture, wrist and ankle acupuncture, acupuncture point injection, or acupressure | 167 (1038) |
| Zheng, 2012 | Case reports, case series, and surveys | China | 1950–2010 | Electro-acupuncture | 15 (44) |
| Gnatta, 2013 | No study design restrictions; all publications that reported infections caused by atypical mycobacteria after needle acupuncture were included | China, Spain, Portugal, South Korea, Canada, Venezuela, and Brazil | Inception - NS | Not stated | 16 (406 including control group) |
| Xu, 2013 | Case reports | Japan, Hong Kong, United Kingdom, United States, Ireland, Spain, Korea, France, Thailand, Australia, Canada, Malaysia, Taiwan, Croatia, Scotland, Venezuela, Brazil, Germany, Singapore, New Zealand, Iran, Austria, Greece, Italy, China, and Turkey | 2000–2011 | Needle acupuncture, moxibustion, or cupping | 117 (308) |
| Tan, 2014 | Case reports, case series, prospective and retrospective surveys, and all types of clinical trials | Australia, Austria, Canada, China, Germany, Hong Kong, Malaysia, Spain, Sweden, Taiwan, United Kingdom and United States | Inception - 2014 | Auricular needle acupuncture, auricular electro-acupuncture, auricular acupressure, or auricular bloodletting therapy | 43 (4203 including control group) |
| McCulloch, 2015 | Case reports, case series, practice descriptions, and RCTs | United States | NS | Needle acupuncture | 11 (>6000 including control group) |
| Wu, 2015 | Case reports | China | 1980–2013 | Needle acupuncture or electro-acupuncture | 133 (182) |
Methodological quality of included reviews
Fifteen (88.2%) reviews conducted a comprehensive literature search. No review provided an a priori design to their reviews via protocol publication. Thirteen (76.5%) review provided characteristics of their included studies. No review provided lists of both included and excluded studies. Eleven (64.7%) reviews reported the presence or absence of conflict of interests on the review itself. Only one (5.9%) review assessed the scientific quality of the included primary studies. The use of appropriate statistical methods and assessment on the likelihood of publication bias were not applicable as no meta-analysis was conducted amongst all included reviews. See Table 2 for full details.
Table 2.
Methodological quality of included systematic reviews on acupuncture and its adverse events and/or complications.
| First author and publication year | AMSTAR Item | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | |
| Norheim, 1996 | N | NR | N | NR | N | N | NR | N | NA | NA | N |
| Ernst, 2001 | N | Y | Y | Y | N | Y | NR | Y | NA | NA | N |
| Yamashita, 2001 | N | NR | N | N | N | N | NR | N | NA | NA | N |
| Ernst, 2003 | N | Y | Y | Y | N | Y | NR | Y | NA | NA | N |
| Lao, 2003 | N | NR | Y | N | N | N | NR | Y | NA | NA | Y |
| Bergqvist, 2008 | N | NR | Y | Y | N | Y | NR | Y | NA | NA | N |
| Zhang, 2010 | N | Y | Y | N | N | Y | NR | Y | NA | NA | Y |
| Adams, 2011 | N | Y | Y | Y | N | Y | NR | Y | NA | NA | Y |
| Ernst, 2011a | N | NR | Y | Y | N | Y | NR | Y | NA | NA | Y |
| Ernst, 2011b | N | Y | Y | Y | N | Y | NR | N | NA | NA | Y |
| He, 2012 | N | Y | Y | N | N | N | NR | N | NA | NA | Y |
| Zheng, 2012 | N | Y | Y | NR | N | Y | NR | N | NA | NA | Y |
| Gnatta, 2013 | N | NR | Y | Y | Y | Y | NR | Y | NA | NA | N |
| Xu, 2013 | N | Y | Y | N | N | Y | NR | N | NA | NA | Y |
| Tan, 2014 | Y | Y | Y | Y | N | Y | Y | Y | NA | NA | Y |
| McCulloch, 2015 | N | Y | Y | NR | N | Y | NR | Y | NA | NA | Y |
| Wu, 2015 | N | NR | Y | N | N | Y | NR | N | NA | NA | Y |
Adverse Events
Major results are narratively presented in this section and detailed information about the cases, including age and sex, reason for treatment, training background of practitioner, site of treatment, and follow-up time and outcome can be found in Table 3. A full list of results can be found in the Appendix 2.
Table 3.
Most common adverse events and complications associated with acupuncture.
| First author and publication year | Number of cases (age/sex) | Reason for acupuncture | Punctured Site | Practitioner | Follow-up Time and Outcome |
|---|---|---|---|---|---|
| Organ or Tissue Injuries | |||||
| Pneumothorax | |||||
| Norheim, 1996 | 23 (NS/NS) | NS | NS | Acupuncturists (at least half were conventional medical doctors) | NS |
| Yamashita, 2001 | 25 (NS/NS) | NS | NS | NS | NS |
| Lao, 2003 | 26 (NS/NS) | NS | Left nipple, above clavicle, back, intercostal space, parasternal, neck, paraspinal, chest below clavicle, supraclavicular, paravertebral, posterior aspect of shoulder, upper back, anterior chest, midthorax paraspine, chest, supraclavicular fossa, pericardial area | 3 cases treated by non-medically trained acupuncturists, 1 chiropractor, 1 health clinic, 5 acupuncturists, 1 physician, 1 acupuncture office, 14 NS | 23 recovered, 1 died, 2 NS |
| Zhang, 2010 | 201 (NS/NS) | NS | Shoulder, scapula, chest | NS | 2–30 days, 197 recovered, 4 died |
| Ernst, 2011a | 21 (25–72y/6M, 20F, 1 NS) | Pain (shoulder, neck, back), shoulder stiffness, algodystrophy, asthma, chronic cough, tension headache, 6 cases NS | NS | NS | 17 recovered, 4 died |
| He, 2012 | 307 (NS/NS) | Periarthritis of the shoulders, cervical spondylosis, stiff neck, intercostal neuralgia, “others” (as reported by authors) | BL13, GB21, BL18, CV22, LI17, CV15, SI13, LI18, EX-B1, ST12, LU1, BL12, BL43, SP21, KI25 | 7 cases treated by acupuncturists, 23 private clinics, 4 barefoot doctors, 1 self, 272 NS | 252 recovered, 6 died, 49 NS |
| Xu, 2013 | 13 (25–72y/3M, 10F) | Pain (back, shoulder, neck, musculoskeletal), asthma, stiff neck, breathing problem, chronic bronchitis, 1 case NS | Thoracic spine bilaterally, thoracic cavity, chest, upper back, back region, right scapular region, LU1, BL13, BL14, BL15, BL16 | 2 cases treated by acupuncturists, 1 acupuncture clinic, 1 medical acupuncturist, 1 registered TCM practitioner, 2 physiotherapists, 6 NS | 2–12 days, 11 recovered, 1 died, 1 NS |
| Wu, 2015 | 30 (21–65y/13M, 17F) | Pain (shoulder, chest, back, cervical, neck, leg), gastroptosis, numbness of shoulders and chest, stiff neck, bronchitis, chronic bronchitis and emphysema, pulmonary heart disease, chronic asthmatic disease, hysteria, cough, spasmodic torticollis, scapulohumeral periarthritis, intercostal neuralgia, chronic hepatitis B, cervical spondylopathy | Shoulder, back, chest, supraclavicular fossa, scapular region, 6th intercostal space anterior axillar line, RN15, GB21, BL13, EX-B2, RN22, BL12, SI13, BL18, LI17, BL23, SI11, 2 NS | 5 cases treated by acupuncturists, 3 factory doctors, 2 clinics, 1 hospital, 1 itinerant doctor, 3 individual clinics, 1 country doctor, 1 health center, 13 NS | 3 days–1 month, 25 recovered, 2 died, 3 NS |
| Central Nervous System Injury / Spinal Cord Injury | |||||
| Norheim, 1996 | 13 (NS/NS) | NS | NS | NS | NS |
| Yamashita, 2001 | 25 (NS/NS) | NS | NS | NS | NS |
| Lao, 2003 | 13 (NS/NS) | Pain (lumbar, low back, neck, shoulder, cervical, posterior neck), neck stiffness, migraine, easily fatigued, bronchial asthma, stiff and painful shoulder, nervousness | NS | NS | 8 recovered, 2 improved, 1 recovery of strength but not sensation, 2 sensory impairment remained |
| Zheng, 2012 | 2 (19–23y/2F) | Schizophrenia | GB20, GV15, GV14 | NS | 2 died |
| Xu, 2013 | 9 (29–74y/7M, 2F) | Pain (neck, lower back, quadi-paresis associated neck), stiff neck, 3 cases NS | Neck, lumbar region, upper back, posterior neck, GV16 | 3 cases treated by acupuncturists (1 unauthorized), 1 nonmedical practitioner, 1 oriental medicine clinic, 1 family physician, 3 NS | 10 days–1 year, 8 recovered, 1 NS |
| Wu, 2015 | 37 (4.5–77y/21M, 16F) | Pain (neck, low back, lumbago, headache, migraine, toothache), impaired vision, schizophrenia, eyelid muscle twitch, bulbar palsy, headache, hysteria, chronic tracheitis, facial spasm, deaf-mute, psychosis, cerebral agenesis with apahasia, weakness of limbs, acid swells of the neck, aural vertigo, head stuffiness, facial paralysis, stiff neck, cold, neurosis, stroke, insomnia, cerebral hemorrhage, cervical spondylopathy, ankylosing spondylitis | Neck, posterior neck, back, waist, Ashi points near C3, T2-T3, GB20, DU16, DU14, DU15, EX-HN18, EX-HN21, LI11, LI4, GB30, ST36, GB39, GB14, ST2, BL37, KI01, RN16, RN10, RN9, RN4 | NS | 2–47 days, 23 recovered, 2 recovered after surgery, 12 died |
| Subarachnoid / Intracranial Hemorrhage | |||||
| Zhang, 2010 | 35 (NS/NS) | NS | GB20, GV15, GV16, GV14, BL10 | NS | 1–8 weeks, 32 recovered, 3 died |
| He, 2012 | 64 (NS/NS) | Headache, insomnia, neurasthenia, epilepsy, spasm of face | GB20, GV16, EX-HN14, HN13 | 1 case treated by acupuncturist, 63 NS | 50 recovered, 12 NS, 2 died |
| McCulloch, 2015 | 4 (42–74y/NS) | NS | Scalp, GB20 | NS | NS |
| Cardiac Tamponade / Heart Injury | |||||
| Bergqvist, 2008 | 7 (25–83y/2M, 5F) | NS | Breast, back, shoulder | NS | 5 recovered, 2 congenital sternal foramen |
| Ernst, 2011b | 26 (9–83y/6M, 8F, 12 NS) | Pain (chronic epigastric, back, multiple sites), fibromyalgia, intercostal neuralgia, chronic bronchitis, oesophagitis, dyspnea, diabetes, various, 7 cases NS | NS | NS | 18 recovered, 6 died, 2 NS |
| Zheng, 2012 | 1 (30y/F) | Schizophrenia | CV15 | NS | 1 died |
| Pseudoaneurysm | |||||
| Bergqvist, 2008 | 7 (43–72y/5M, 2F) | Pain (abdominal and back), mass, pulsating mass, swelling, bleeding, fever | Shoulder, left knee, thigh, back, popliteal fossa, calf | NS | 7 recovered |
| Hematoma | |||||
| Adams, 2011 | 44 (NS/NS) | Headache or chronic lower back pain or arthrosis | NS | 44 cases treated by MDs trained in acupuncture | NS |
| Broken needle / needle fragment | |||||
| Ernst, 2011a | 4 (29–70y/3M, 1F) | Dizziness, low back pain, sciatica, 1 case NS | NS | NS | 4 recovered |
| Soft-tissue injury | |||||
| McCulloch, 2015 | 3 (60–82y/1M, 2F) | NS | NS | NS | NS |
| Thumb deformity | |||||
| Adams, 2011 | 12 (3–11y/4M, 8F) | NS | NS | NS | NS |
| Infections | |||||
| Hepatitis | |||||
| Norheim, 1996 | 100 (NS/NS) | NS | NS | NS | NS |
| Yamashita, 2001 | 11 (NS/NS) | NS | NS | NS | NS |
| Lao, 2003 | 94 (NS/NS) | NS | NS | 36 cases treated by persons with no recognized medical qualification, 8 physicians practicing acupuncture, 6 chiropractic clinics, 35 licensed acupuncturists, 9 NS | 42 recovered, 3 mild to severe liver failure, 3 chronic, 4 unknown, 1 died 41 NS |
| Abscesses | |||||
| Yamashita, 2001 | 6 (NS/NS) | NS | NS | NS | NS |
| Zhang, 2010 | 8 (19–52y/7M, 2F) | Tooth ache, gluteal numbness, insomnia, dizziness, headache, psoatic strain | Buccal, gluteal, cephalic, lower back | NS | 8 recovered |
| Ernst, 2011a | 8 (16–78y/5M, 3F) | No restriction of disease/symptoms (Pain (low back, hip, epigastric), weight loss, muscle strain, 1 case NS | NS | NS | 8 recovered |
| Wu, 2015 | 4 (19–28y/2M, 2F) | Migraine, lumbar muscle strain | EX-HN5, GB14, DU20, Loin | 1 case treated by health worker in the army, 1 NS | 3–6 months, 4 recovered |
| Tetanus | |||||
| Zhang, 2010 | 2 (2F) | Pain (leg), headache | Cephalic, NS | NS | 2 recovered |
| He, 2012 | 14 (NS/NS) | NS | NS | 2 cases treated by barefoot doctors, 12 NS | 5 recovered, 8 died, 1 NS |
| Wu, 2015 | 6 (2–62y/2M, 4F) | Pain (leg), malnutritional stagnation, headache, facioplegia, fever, rheumatoid arthritis | Knee, EX-UE19, EX-HN05, DU20, GB20, LI4, GB21, SJ5, 2 NS | 2 cases treated by illegal treatment, 1 village acupuncturist, 1 private practitioner, 1 health-center, 1 NS | 3 days–1 month, 3 recovered, 3 died |
| Auricular Infections | |||||
| Norheim, 1996 | 16 (NS/NS) | NS | NS | NS | NS |
| Lao, 2003 | 9 (NS/NS) | NS | NS | 1 case treated by acupuncturist, 8 NS | 4 residual deformities, 2 recovered, 3 NS |
| Adams, 2011 | 1 (16y/F) | Weight loss | NS | NS | NS |
| Septic Arthritis | |||||
| Adams, 2011 | 1 (13y/M) | Lumbar pain | NS | 1 case treated by acupuncturist | NS |
| Ernst, 2011a | 7 (13–78y/4F, 2M, 1 NS) | Pain (knee), rheumatoid arthritis, post-operative recovery, 1 case NS | NS | NS | 7 recovered |
| Local Infection | |||||
| He, 2012 | 12 (NS/NS) | NS | NS | 1 case treated by acupuncturist, 1 barefoot doctor, 10 NS | 12 recovered |
| Tan, 2014 | 3 (NS/NS) | Smoking cessation, acute tonsillitis | Shenmen, lung, mouth, sympathetic, Ashi point | 1 case treated by acupuncturist, 2 NS | NS |
| Mycobacterial infection | |||||
| Gnatta, 2013 | 295 (mean age 43–55y/162F, 33M, 100 NS) | NS | NS | NS | NS |
| Xu, 2013 | 193 (58–79y (4 participants, 189 NS)/3F, 1M, 189 NS) | Pain (ankle), knee osteoarthritis, obesity | GB38, abdomen, thigh, limb, 189 NS | NS | 3 weeks to 4 months, 4 recovered, 189 NS |
| Staphylococcal infection | |||||
| Xu, 2013 | 29 (15–79 (11)/7M, 5F, 11 NS) | Pain (hip, low back, nuchal, knee and subscapular), postoperative recovery, shoulder stiffness, eczema | Low limb, around tibia, back, lower back, cervical paraspinal and medial scapular, shoulder and arm, hip, thigh, around the knee, bilateral paraspinal muscles | 7 cases treated by acupuncturist, 1 practitioner, 1 TCM doctor, 20 NS | 4 weeks–5 months, 12 recovered, 17 NS |
| Local Adverse Events or Adverse Reactions | |||||
| Contact Dermatitis / Allergy | |||||
| Norheim, 1996 | 3 (NS/NS) | NS | NS | NS | NS |
| Yamashita, 2001 | 2 (NS/NS) | NS | NS | NS | NS |
| Lao, 2003 | 7 (NS/NS) | NS | NS | NS | NS |
| Zhang, 2010 | 4 (11–52y/1M, 3F) | Cervical spondylosis, coxarthritis, abdominal pain | GB20, BL57, BL40, 1 NS | NS | 4 recovered |
| Adams, 2011 | 11 (11–12y/1F, 10 NS) | Hip pain, emesis from general anaesthesia | NS | 10 cases treated by anaesthesiologists trained by acupuncturist, 1 NS | NS |
| Ernst, 2011a | 1 (65y/F) | Shoulder stiffness | NS | NS | NS |
| He, 2012 | 6 (NS/NS) | NS | NS | 1 case treated by acupuncturist, 5 NS | 6 recovered |
| Tan, 2014 | ~63 (NS/NS) | Post-operative pain, chronic low back pain, smoking cessation, insomnia, neurasthenia, obesity in female patients, vascular dementia, myopia, constipation, chemotherapy-induced nausea and vomiting, persistent allergic rhinitis, functional constipation | Shenmen, lung, mouth, brain, liver, kidney, heel, lesser occipital nerve, sympathetic, endocrine, heart, subcortex, stomach, spleen, pancreas, gallbladder, anterior ear lobe, San Jiao, great auricular nerve, hunger, colon, apex of ear, eye, large intestine, rectum, internal nose, wind stream, lumbar spine, cushion | 2 cases treated by TCM practitioners, 2 acupuncturists, 1 therapist, 1 nurse, 57 NS | 28 recovered, ~35NS |
| Wu, 2015 | 3 (54–72y/1M, 1F, 1 NS) | Scapulohumeral periarthritis, nerve root cervical spondylopathy, cervical type cervical spondylopathy | EX-UE01, GB21, LI11, SJ5, EX-B2 | 1 case treated by acupuncturist, 2 NS | 10 minutes to 1 week, 3 recovered |
| Argyria | |||||
| Norheim, 1996 | 5 (NS/NS) | NS | NS | NS | NS |
| Yamashita, 2001 | 10 (NS/NS) | NS | NS | NS | NS |
| Ernst, 2011a | 1 (66y/F) | Skin lesions | NS | NS | NS |
| Xu, 2013 | 1 (66y/F) | Arthralgia | Extremities | NS | NS |
| Local Bleeding | |||||
| Adams, 2011 | ~47 (10−<18y/1M, 1F, ~42NS) | Nocturnal enuresis, autism spectrum disorder, various, cerebral palsy, paralytic strabismus | NS | 1 case treated by MD, ~40 acupuncturists, ~6 NS | NS |
| McCulloch, 2015 | 51 (NS/NS) | NS | NS | NS | NS |
| Local Pain / Tenderness | |||||
| Zhang, 2010 | 4 (NS/NS) | NS | SI3, LI11, hand | NS | 4 recovered |
| Tan, 2014 | ~139 (NS/NS) | Drug dependence, chronic low back pain, obesity, pregnant women with low back pain and posterior pelvic pain, women with concurrent substance use problems and anxiety and depressive symptoms, substance abuse problem, smoking cessation, post-operative pain, alcohol withdrawal, drug use problem, psychological symptoms, physical discomfort in prison inmates | Shenmen, sympathetic, kidney, liver, lung, lumbar spine, cushion, stomach, hunger, endocrine, analgesia, mouth, knee joint, thalamus, hip joint, Ashi point, lumbosacral vertebrae, subcortex, unknown number of NS | 8 cases treated by acupuncturists, 2 psychiatrists, 2 nurses, 1 physiotherapist, 121 NS | NS |
| Local Burns | |||||
| Lao, 2003 | 2 (NS/NS) | NS | NS | 2 acupuncture clinics | NS |
| Zheng, 2012 | 1 (54y/M) | Leg pain | Right leg | NS | NS |
| He, 2012 | 1 (NS/NS) | NS | NS | NS | NS |
| Xu, 2013 | 2 (30, 32y/2M) | Pain (back) | Back | 1 mother, 1 self | 11 days, 2 recovered |
| Local Bruising | |||||
| McCulloch, 2015 | 1 (NS/NS) | NS | NS | NS | NS |
| Other Complications | |||||
| Dizziness / Syncope | |||||
| Norheim, 1996 | 2 (NS/NS) | NS | NS | NS | NS |
| Yamashita, 2001 | 1 (NS/NS) | NS | NS | NS | NS |
| Lao, 2003 | 2 (NS/NS) | NS | NS | 1 acupuncturist | NS |
| Zhang, 2010 | 150 (30–57y/2M, 6F, 142NS) | Pain (low back, shoulder), stomach ache, cervical spondylosis, 146 cases NS | Shoulder, cervical, 148 NS | NS | 150 recovered |
| He, 2012 | 468 (NS/NS) | NS | NS | 194 cases treated by acupuncturists, 274 NS | 394 recovered, 74 NS |
| Xu, 2013 | 3 (25–72y/2M, 1F) | Pain (arm, ankle), healthy volunteer for a clinical study | ST36, LI11, TB5, GB34, B40 | NS | NS |
| Tan, 2014 | ~55 (48y, NS/1F, 51 NS) | Constipation, drug dependence, state anxiety before dental treatment, obesity, smoking cessation, post-operative pain, heroin addiction, cholecystolithiasis | Shenmen, kidney, liver, spleen, stomach, temple, subcortex, forehead, occiput, sympathetic, lung, relaxation, tranquilizer, master cerebral, hunger, endocrine, mouth, knee, joint, large intestine, rectum, San Jiao, extra, gallbladder, duodenum | 1 case treated by physician, ~26 acupuncturists, 26 investigator with a diploma of acupuncture, unknown TCM practitioners 2 NS | 2 withdrew from treatment, 3 recovered, ~50 NS |
| Wu, 2015 | 18 (24–78y/6M, 12F) | Pain (lumbago, shoulder, right thumb, stomache ache), facioplegia, myotenositis of long head of biceps brachii, scapulohumeral periarthritis, waist sprain, insomnia, prosopalgia, stroke, cervical spondylopathy, acute lumbar sprain, gouty arthritis, cervical spondylopathy radiculaire, facial paralysis | GB14, ST6, ST4, SJ17, LI20, LI14, LI15, LI11, Ashi, LI3, ST36, PC6, EX-UE01, GB21, LI14, LI11, SJ5, LI4, BL40, acupoint of bladder meridian, PC6, HT7, BL23, BL40, DU3, GB30, KI17, LI15, SJ5, SJ14, EX-HN5, SP6, EX-UE17, EX-LE11, BL10, GB20, SJ3, EX-B5, GB14, ST2, EX-HN16 | 18 cases treated by acupuncturists | 10 minutes to 2 days, 18 recovered |
| Nausea and vomiting | |||||
| Lao, 2003 | 1 (NS/NS) | NS | NS | NS | 1 recovered |
| Tan, 2014 | ~22 (NS/NS) | Drug dependence, smoking cessation, post-operative pain, heroin addiction, cholecystolithiasis | Shenmen, sympathetic, kidney, lung, liver, mouth, sympathetic, knee, joint, gallbladder, duodenum, stomach | ~22 cases treated by acupuncturists, unknown number treated by TCM practitioners | 1 recovered, ~21 NS |
| Reduced bowel movements | |||||
| Norheim, 1996 | 2 (NS/NS) | NS | NS | NS | NS |
| Atrioventricular Block | |||||
| Zheng, 2012 | 17 (NS/NS) | Psychosis | Between SJ17 and GB20 | NS | 17 recovered |
| Epilepsy | |||||
| Ernst, 2011a | 2 (63–72y/1M, 1F) | Pain (forearm, ankle) | NS | NS | 2 recovered |
| He, 2012 | 1 (NS/NS) | NS | NS | NS | NS |
| Wu, 2015 | 3 (35–53y/3M) | Soft tissue injury, epilepsy, cervical spondylosis | Ashi point, 2 NS | 3 cases treated by acupuncturists | 1 minute to 2 minutes, 3 recovered |
| Factitial panniculitis | |||||
| Ernst, 2011a | 2 (22–24y/2F) | Weight loss | NS | NS | NS |
| Aggravation of Bell’s Palsy | |||||
| Zheng, 2012 | 13 (NS/NS) | Bell’s palsy | NS | NS | NS |
| Galactorrhea | |||||
| Xu, 2013 | 2 (32–41y/2F) | Pain (cancer, foot) | Upper back, foot | NS | NS |
| Initial crying with fear and possible minor pain | |||||
| Adams, 2011 | ~62 (NS/NS) | Cerebral palsy, autism spectrum disorder, persistent drooling | NS | ~62 cases treated by acupuncturists | NS |
| Vasovagal reaction | |||||
| Adams, 2011 | 13 (NS/NS) | Headache, chronic lower back pain, arthrosis | NS | 13 cases treated by MDs trained in acupuncture | NS |
| Aphonia | |||||
| Zhang, 2010 | 2 (36y, 46y/1M, 1F) | Hiccups | PC6 | NS | 2 recovered |
Organ or tissue injuries (including complications from broken or remnant needles) associated with acupuncture
A median of 36 organ or tissue injuries were reported amongst 13 reviews7–10, 12, 13, 15–20, 22. A median of 4 deaths were reported across reviews, but four reviews did not report any data on outcomes8, 9, 12, 13. The most common organ or tissue injuries that occurred in patients included pneumothorax (8 reviews10, 12, 13, 15, 17–19, 22, median, 25.5, median number of deaths, 3), central nervous system or spinal cord injury (6 reviews7, 12, 13, 16–18, median, 13), subarachnoid or intracranial hemorrhage (3 reviews8, 10, 19, median, 35, median number of deaths, 2.5, with 1 review not providing outcome data19), and cardiac tamponade or heart injury (3 reviews7, 15, 20, median, 7, median number of deaths, 1). Respectively, one review reported each of the following as one of the most common organ or tissue injuries: pseudoaneurysm (7 cases)20, hematoma (44 cases)9, broken needle/needle fragment (4 cases)22, soft tissue injury (3 cases)8, and thumb deformity (12 cases)9. No deaths were reported for any of these complications. See Table 3 for full details.
Infections associated with acupuncture
A median of 17 infections were reported amongst 11 reviews6, 9, 10, 12–14, 16–19, 22. A median of 0.5 deaths was reported, but 5 reviews did not report any data on outcomes6, 9, 12–14. The most common infections that occurred in patients included hepatitis (3 reviews12, 13, 16, median, 94, 1 death in total), abscesses (4 reviews10, 12, 17, 22, median, 7), tetanus (3 reviews10, 17, 19, median, 6, median number of deaths, 3), auricular infections (3 reviews9, 13, 16, median, 9), septic arthritis (2 reviews9, 22, median, 4), local infections (2 reviews6, 19, median, 7.5), Mycobacterial infection (2 reviews9, 22, median, 244), Staphylococcal infection (1 review18, 29 cases). See Table 3 for full details.
Local adverse events or reactions associated with acupuncture
A median of 8.5 local adverse events or reactions were reported amongst 12 reviews6–10, 12, 13, 16–19, 22. No deaths were reported. The most common local adverse events or reactions that occurred in patients included contact dermatitis or local allergic reactions (9 reviews6, 9, 10, 12, 13, 16, 17, 19, 22, median, 4), argyria (4 reviews12, 13, 18, 22, median, 3), local bleeding (2 reviews8, 9, median, approximately 44), local pain or tenderness (2 reviews6, 10, median, approximately 71.5), local burns (4 reviews7, 16, 18, 19, median 1.5), and local bruising (1 review8, 1 case). See Table 3 for full details.
Other complications associated with acupuncture
A median of 21 other complications were reported amongst 11 reviews6, 7, 9, 10, 12, 13, 16–19, 22. No deaths were reported. The most common other complications that occurred in patients included dizziness or syncope (8 reviews6, 10, 12, 13, 16–19, median, 10.5), nausea and vomiting (2 reviews6, 16, median, approximately 11.5), and epilepsy (3 reviews, median, 2). Respectively, one review reported each of the following as one of the most common other complications: reduced bowel movements (2 cases)13, atrioventricular block (17 cases)7, factitial panniculitis (2 cases)22, aggravation of Bell’s palsy (13 cases)7, galactorrhea (2 cases)18, initial crying with fear and possible minor pain (approximately 62 cases)9, vasovagal reaction (13 cases)9, and aphonia (2 cases)10. See Table 3 for full details.
Discussion
This overview provided a comprehensive summary of all the adverse events and complications associated with acupuncture and related therapies that have been reported to date in published systematic reviews, with the majority coming from case reports, case series, and randomized controlled trials across 17 publications. The number of included primary studies in these publications ranged from 9 to 167. Amongst these primary studies, the number of included patients ranging from 21 to 111,692. In general, the results show that both minor and serious adverse events can occur from the use of acupuncture. Incidence rates, related confidence intervals (CIs), and p values could not be calculated because many adverse events came from case reports and many of the reviews did not include full details about the number of participants in their included studies. However, all the reviews have suggested that adverse events are rare and often minor.
Although serious complications were rare, they require significant attention as mortalities are associated with these adverse events. There was insufficient data to determine which body sites or whether patient predispositions were associated with these events, but it is clear that patients can be at great risk. Practitioners should pay ample attention to risk stratifying patients based on their medical history and other relevant characteristics. Other potential areas of improvement include enforcing stricter sterile needle practices, improving patient education about common and/or serious risks, and enhancing practitioner recognition of acute complications. Better communication should exist between physicians treating complications and the practitioner that administered the acupuncture, so that practitioners can become more cognizant of issues that can arise from their practice.
The methodological quality of the included reviews was mediocre. The majority of the included reviews conducted a comprehensive literature search. Most reviews also included the characteristics of their included studies and stated any conflicts of interest. However, no studies provided an a priori design, and only one study6 thoroughly assessed the scientific quality of included studies, which might be caused by lack of appropriate methodological quality assessment tools for case reports23. Regardless, the reviews provided a tantamount of information on the existence of adverse events in the literature across studies from around the world. A major limitation of the presented information was that no causality could be determined. In the reviews that commented on the scientific quality of included studies, concern was raised regarding the ability to ascertain that acupuncture resulted in the adverse outcome8, 10, 11, 14, 22. One review classified reported cases on a causality scale, and only a minority of adverse events were classified as certainly caused by acupuncture19. Future studies need to be more rigorous in their assessment of causality, and document their means of determining causality. Ideally, prospective cohort studies or randomized controlled trials should be reporting all the adverse events that occur during their investigations, as these provide the best evidence for causality. For rarer adverse events, case-control studies would be the ideal design. Another limitation is that a significant number of adverse events were not followed up. Although most complications were minor, practitioners and researchers should still follow up with the patient so that meaningful and definitive data can be derived. It is improper to assume that minor complications resolve spontaneously, or that major complications result in long-term implications. More attention needs to paid on the documentation and follow-up of all adverse events that occur during a study. Furthermore, a standardized template should be developed in the near future so that practitioners around the world can use it to track and report complications for research and clinical purposes.
Due to the diversity in study designs (e.g. case report, case series, case control studies, cohort studies, and clinical trials), populations, and data collection methods included in the identified systematic reviews, none of them conducted a meta-analysis to generate a pooled incidence rate with CI24. Although systematic reviews on adverse events are recommended to summarize evidence in a qualitative manner, a quantitative estimation of the upper limit of the 95% CI for the probability of the adverse events will help the clinicians to estimate what the worst-case scenario could be24. Future systematic reviews on this topic should use available statistical method25 to provide such a quantitative estimation. For primary studies, case control studies is the preferred method give the rare occurrence of adverse events.
Another concern raised by most reviews was the issue of underreporting10, 11, 13, 15, 16, 19–21. Often, only medically interesting findings are reported as many case reports are published by the physicians treating them16. Minor, less significant adverse events are often not published. Some reviews found that no adverse events were reported by acupuncturists12, raising the question of whether some practitioners are even aware of complications in their patients. Many journals restrict the type of publications that are accepted, and thus publication bias can also limit the number of adverse events reported20. This is a systemic issue, and regulatory bodies around the world need to create a convenient platform for which practitioners providing acupuncture and physicians treating complications can report known adverse events and the surrounding circumstances which can help with epidemiological and clinical research. In addition to providing a comprehensive summary, this overview serves as an important step towards furthering the knowledge, safety, and application of acupuncture. The overview may inform practitioners around the world about and modify the way they practice acupuncture, given that many acupuncturists may not be fully aware of the full breadth and depth of risk their treatments can pose. Usage of acupuncture is increasing worldwide, and more acupuncturists are being trained to match the demand. Thus, the need to pay careful attention towards the risks of acupuncture is becoming increasingly paramount as more patients become subject to it.
Methods
Inclusion criteria
Any systematic review (SR) that summarized adverse effects of acupuncture and related therapies, including electro-acupuncture, cupping, moxibustion, laser acupuncture, indwelling needles, dry needling, bee venom acupuncture, acupuncture point injection and acupressure, were considered eligible for this overview. To be included, the SR must have a primary objective of identifying adverse events instead of investigating its treatment efficacy or effectiveness. We had no restriction for the type of patients included, as long as they received acupuncture or related therapies for the management of any diseases or symptoms. We did not set any restriction on the control treatment as long as adverse effects of acupuncture were reported. However, SRs on adverse effects specifically caused by injected drugs through acupoint injections were excluded.
Literature search
MEDLINE and EMBASE were searched from their inception to December 2015. Published search filters related to SR26, 27 and adverse effects28 were used during the literature search, in addition to search keywords for acupuncture and related therapies. Details on search strategies as well as the retrieved results from the electronic databases could be found in Appendix 1.
Literature selection, data extraction and assessments of the methodological quality
Literature search was conducted by one researcher, and retrieved results were equally distributed to 4 pairs of trained research assistants. Each pair of assistants independently screened and evaluated the eligibility of citations that were assigned to them, and extracted data from the included reviews using a standardized, piloted template. The template was designed according to the requirement of the PRISMA harm checklist29. Disagreements were resolved via discussion and consensus within each pair. A senior researcher was consulted when disagreement was unresolvable.
Methodological quality of included SRs were evaluated with the validated Methodological Quality of Systematic Reviews (AMSTAR)30 instrument by two researchers independently. It includes 11 items, with each item being assessed as yes, no, cannot answer, or not applicable based on information provided by the SRs. Disagreements between assessors were discussed to reach consensus. A third reviewer was consulted if necessary.
Data synthesis
Adverse effects of acupuncture and related therapies and their outcomes were narratively reported according to each adverse event. Protocol of this overview has been registered in PROSPERO (http://www.crd.york.ac.uk/PROSPERO/printPDF.php?RecordID=43943&UserID=6569).
Electronic supplementary material
Acknowledgements
This study did not receive any grant support.
Author Contributions
Study concept and design: V.C., S.W., J.W. Acquisition of data: X.Y.W., M.C. Analysis and interpretation of data: X.Y.W., M.C. Drafting of the manuscript: X.Y.W., M.C. Critical revision of the manuscript for important intellectual content: V.C., S.W., J.W. Administrative, technical, or material support: S.W., J.W. All authors reviewed the manuscript.
Competing Interests
The authors declare that they have no competing interests.
Footnotes
Malcolm W. C. Chan and Xin Yin Wu contributed equally to this work.
Electronic supplementary material
Supplementary information accompanies this paper at doi:10.1038/s41598-017-03272-0
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Burton, A., Falkenberg, T., Smith, M., Zhang, Q. & Zhang, X. WHO Traditional Medicine Strategy 2014_–_2023 Available at: http://apps.who.int/iris/bitstream/10665/92455/1/9789241506090\_eng.pdf?ua=1 (Assessed: 9th July 2016) (2013).
- 2.Hopton AK, Curnoe S, Kanaan M, MacPherson H. Acupuncture in practice: mapping the providers, the patients and the settings in a national cross-sectional survey. BMJ Open. 2012;2:1–9. doi: 10.1136/bmjopen-2011-000456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cheng, X. Chinese Acupuncture and Moxibustion (Foreign Languages Pres, 2010).
- 4.Barnes, P. M., Bloom, B. & Nahin, R. L. Complementary and alternative medicine use among adults and children: United States, 2007. National health statistics reports 1–23 (2008). [PubMed]
- 5.Statistics Canada. Health reports: use of alternative health care. The Daily16 (2004).
- 6.Tan, J. Y., Molassiotis, A., Wang, T. & Suen, L. K. P. Adverse events of auricular therapy: A systematic review. Evid Based Complement Alternat Med2014, doi: 10.1155/2014/506758 (2014). [DOI] [PMC free article] [PubMed]
- 7.Zheng W, Zhang J, Shang H. Electro-acupuncture-related adverse events: A systematic review. Med Acupunct. 2012;24:77–81. doi: 10.1089/acu.2011.0858. [DOI] [Google Scholar]
- 8.McCulloch M, Nachat A, Schwartz J, Casella-Gordon V, Cook J. Acupuncture safety in patients receiving anticoagulants: a systematic review. Perm J. 2015;19:68–73. doi: 10.7812/TPP/14-057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Adams D, et al. The safety of pediatric acupuncture: A systematic review. Pediatrics. 2011;128:e1575–e1587. doi: 10.1542/peds.2011-1091. [DOI] [PubMed] [Google Scholar]
- 10.Zhang J, Shang H, Gao X, Ernst E. Acupuncture-related adverse events: A systematic review of the chinese literature. Bull World Health Organ. 2010;88:915–921. doi: 10.2471/BLT.10.076737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ernst E, Sherman KJ. Is acupuncture a risk factor for hepatitis? Systematic review of epidemiological studies. J Gastroenterol Hepatol. 2003;18:1231–1236. doi: 10.1046/j.1440-1746.2003.03135.x. [DOI] [PubMed] [Google Scholar]
- 12.Yamashita H, et al. Systematic review of adverse events following acupuncture: The Japanese literature. Complement Ther Med. 2001;9:98–104. doi: 10.1054/ctim.2001.0446. [DOI] [PubMed] [Google Scholar]
- 13.Norheim AJ. Adverse effects of acupuncture: a study of the literature for the years 1981–1994. J Altern Complement Med. 1996;2:291–297. doi: 10.1089/acm.1996.2.291. [DOI] [PubMed] [Google Scholar]
- 14.Gnatta JR, Kurebayashi LFS, Paes da Silva MJ. Atypical mycobacterias associated to acupuncuture: an integrative review. Rev Lat Am Enfermagem. 2013;21:450–458. doi: 10.1590/S0104-11692013000100022. [DOI] [PubMed] [Google Scholar]
- 15.Ernst E, Zhang J. Cardiac tamponade caused by acupuncture: a review of the literature. Int J Cardiol. 2011;149:287–289. doi: 10.1016/j.ijcard.2010.10.016. [DOI] [PubMed] [Google Scholar]
- 16.Lao L, Hamilton GR, Fu J, Berman BM. Is acupuncture safe? A systematic review of case reports. Altern Ther Health Med. 2003;9:72–83. [PubMed] [Google Scholar]
- 17.Wu, J. et al. Systematic Review of Adverse Effects: A Further Step towards Modernization of Acupuncture in China. Evid Based Complement Alternat Med2015, doi:10.1155/2015/432467 (2015). [DOI] [PMC free article] [PubMed]
- 18.Xu, S. et al. Adverse events of acupuncture: A systematic review of case reports. Evid Based Complement Alternat Med2013, doi:10.1155/2013/581203. Epub 2013 Mar 20 (2013). [DOI] [PMC free article] [PubMed]
- 19.He W, Zhao X, Li Y, Xi Q, Guo Y. Adverse events following acupuncture: A systematic review of the chinese literature for the years 1956–2010. J Altern Complement Med. 2012;18:892–901. doi: 10.1089/acm.2011.0825. [DOI] [PubMed] [Google Scholar]
- 20.Bergqvist D. Vascular injuries caused by acupuncture. Eur J Vasc Endovasc Surg. 2008;36:160–163. doi: 10.1016/j.ejvs.2008.04.004. [DOI] [PubMed] [Google Scholar]
- 21.Ernst E, White AR. Prospective studies of the safety of acupuncture: A systematic review. Am J Med. 2001;110:481–485. doi: 10.1016/S0002-9343(01)00651-9. [DOI] [PubMed] [Google Scholar]
- 22.Ernst E, Lee MS, Choi T-Y. Acupuncture: does it alleviate pain and are there serious risks? A review of reviews. Pain. 2011;152:755–764. doi: 10.1016/j.pain.2010.11.004. [DOI] [PubMed] [Google Scholar]
- 23.Zeng X, et al. The methodological quality assessment tools for preclinical and clinical studies, systematic review and meta-analysis, and clinical practice guideline: a systematic review. J Evid Based Med. 2015;8:2–10. doi: 10.1111/jebm.12141. [DOI] [PubMed] [Google Scholar]
- 24.Loke YK, Price D, Herxheimer A. Systematic reviews of adverse effects: framework for a structured approach. BMC Med Res Methodol. 2007;7:32. doi: 10.1186/1471-2288-7-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Eypasch E, Lefering R, Kum CK, Troidl H. Probability of adverse events that have not yet occurred: a statistical reminder. BMJ. 1995;311:619–620. doi: 10.1136/bmj.311.7005.619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wilczynski NL, Haynes RB. EMBASE search strategies achieved high sensitivity and specificity for retrieving methodologically sound systematic reviews. J Clin Epidemiol. 2007;60:29–33. doi: 10.1016/j.jclinepi.2006.04.001. [DOI] [PubMed] [Google Scholar]
- 27.Montori VM, Wilczynski NL, Morgan D, Haynes RB. Optimal search strategies for retrieving systematic reviews from Medline: analytical survey. BMJ. 2005;330:68. doi: 10.1136/bmj.38336.804167.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Golder S, Loke YK. Sensitivity and precision of adverse effects search filters in MEDLINE and EMBASE: a case study of fractures with thiazolidinediones. Health Info Libr J. 2012;29:28–38. doi: 10.1111/j.1471-1842.2011.00972.x. [DOI] [PubMed] [Google Scholar]
- 29.Zorzela, L. et al. PRISMA harms checklist: improving harms reporting in systematic reviews. BMJ352, doi:10.1136/bmj.i157 (2016). [DOI] [PubMed]
- 30.Shea BJ, et al. Development of AMSTAR: a measurement tool to assess the methodological quality of systematic reviews. BMC Med Res Methodol. 2007;7:1–7. doi: 10.1186/1471-2288-7-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.