Bradyarrhythmias in patients with COVID-19: A case series (original) (raw)
Abstract
Novel coronavirus disease (COVID-19) can have variety of cardiac manifestations; however, less is known about the prevalence, clinical characteristics and outcomes of bradyarrhythmias in patients with COVID-19. In the present case series of bradyarrhythmia in patients with COVID-19, we report complete heart block requiring intervention in 5 patients and sinus node dysfunction in 2 patients.
Abbreviations and Acronyms: COVID-19, Coronarvirus disease 2019
Several cardiovascular complications of Coronarvirus disease 2019 (COVID-19) including myocardial infarction, myocarditis, stroke, tachyarrhythmias and pulmonary embolism have been reported during the current pandemic. However, less is known about the prevalence, clinical characteristics and outcomes of bradyarrhythmias in patients with COVID-19 [1].
We report a case series of 7 patients with COVID-19 who presented with bradyarrhythmias. Of them, 5 had complete heart block and 2 had sick sinus syndrome. The clinical characteristics of the patients are summarized in Table 1 The patients were aged between 45 and 80 years. Out of these 3 were women. 2 patients had history of diabetes mellitus, hypertension, or myocardial infarction and 1 had a history of heart failure. None of the patients were on calcium channel blockers, beta-blockers, digoxin or anti-arrhythmic drugs at baseline. In addition, hydroxychloroquine, azithromycin, zinc, remdesivir or convalescent plasma was not given to any of the patients for treatment of COVID-19.
Table 1.
Characteristics of COVID-19 patients with bradyarrhythmias.
| Characteristics | Pt. 1 | Pt. 2 | Pt. 3 | Pt. 4 | Pt. 5 | Pt. 6 | Pt. 7 |
|---|---|---|---|---|---|---|---|
| Age, years | 55 | 56 | 67 | 80 | 45 | 55 | 69 |
| Sex | Female | Female | Male | Male | Female | Male | Male |
| Medical History | |||||||
| Diabetes Mellitus | Yes | No | Yes | No | No | No | No |
| Hypertension | No | No | Yes | Yes | No | No | No |
| Prior Myocardial Infarction | No | No | No | Yes | No | Yes | No |
| Prior Heart Failure | No | No | No | No | No | No | Yes |
| Clinical Presentation | |||||||
| Syncope | Yes | Yes | Yes | Yes | Yes | No | No |
| Fever | No | Yes | Yes | No | No | No | No |
| Cough | No | No | Yes | No | No | No | No |
| Dyspnea | No | No | Yes | Yes | No | No | No |
| Heart rate (bpm) | 40 | 32 | 30 | 42 | 36 | 33 | 40 |
| Escape rhythm | Ventricular | Ventricular | Ventricular | Ventricular | Junctional | Junctional | Junctional |
| Systolic Blood Pressure (mmHg) | 120 | 100 | 110 | 200 | 130 | 90 | 116 |
| Diastolic Blood Pressure (mmHg) | 60 | 60 | 70 | 110 | 80 | 60 | 76 |
| Oxygen Saturation | 98 | 97 | 98 | 98 | 98 | 99 | 98 |
| Laboratory/Imaging Evaluation | |||||||
| White blood count (cells/mm3) | 11,800 | 11,200 | 7400 | 8100 | 5200 | 17,300 | 8400 |
| Neutrophil/Lymphocyte ratio | 75/20 | 75/22 | 76/22 | 63/19 | 65/27 | 84/11 | 71/12 |
| Serum Creatinine (mg/dL) | 0.6 | 0.6 | 1.4 | 0.8 | 0.6 | 1.5 | 1.3 |
| Serum Na mmol/litre) | 138 | 136 | 104 | 136 | 138 | 143 | 134 |
| Serum K (mmol/litre) | 4.7 | 3.4 | 4.2 | 5.1 | 4.0 | 4.8 | 3.9 |
| High-sensitive Troponin T (Upper limit of normal <0.014) | 0.011 | 0.003 | 0.014 | 0.006 | 0.007 | 0.018 | ND |
| NT Pro BNP (pg/ml) | 157 | 143.5 | 3814 | 1515 | 2206 | 677.4 | ND |
| hsCRP (mg/litre) | 57.1 | 48.38 | 81.72 | 106.7 | 395.83 | 74.25 | ND |
| Ferritin (ng/ml) | 80.5 | 280 | 327 | 460 | 520 | 81.4 | ND |
| Infiltrates on Chest-X ray | Absent | Unilateral | Bilateral | Bilateral | Bilateral | Absent | Bilateral |
| LVEF (%) | 60 | 60 | 60 | 50 | 60 | 60 | 40 |
| Bradyarrhythmia | CHB | CHB | CHB | CHB | SSS | CHB | SSS |
| Time from presentation to pacemaker implantation | 14 days | 12 days | 12 days | 15 days | ND | 17 days | ND |
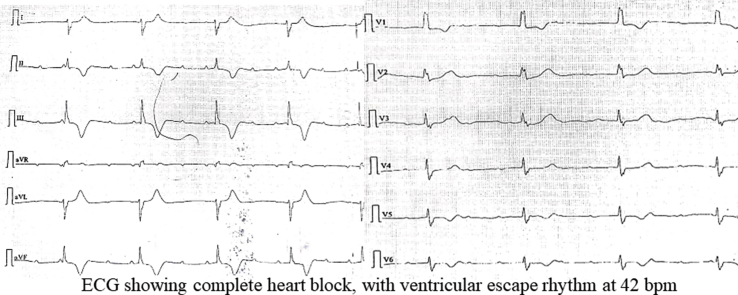
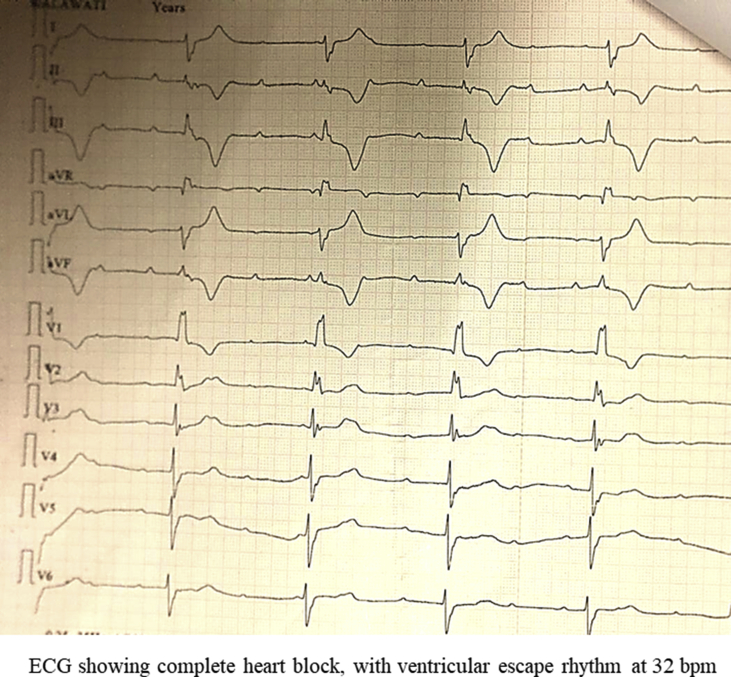
All of the seven patients presented within 24–48 hours of symptom onset. Of these, 5 presented with recent onset syncope and 2 with presyncope. However, only 2 patients had history of fever. All patients were hemodynamically stable and none had hypoxia. Laboratory evaluation demonstrated lymphopenia in all patients and 1 had leucocytosis. High-sensitivity Troponin T levels were mildly elevated in 1 patient and N-terminal-pro hormone BNP (NT-proBNP) levels were elevated in 4 patients. High-sensitivity C-reactive protein (hs-CRP) was elevated in all patients except one and 4 patients had elevated levels of ferritin. Chest X-ray showed infiltrates in five patients. All the patients had bradycardia with a maximum heart-rate of 42 bpm. The escape rhythm was ventricular in 4 out of 5 patients with complete heart block and rest of the patients had junctional escape rhythm. Transthoracic echocardiogram showed preserved left ventricular ejection fraction (LVEF) in 5 patients, while 2 had LVEF ≤ 50%. In view of symptomatic bradycardia and the uncertainty of clinical course of COVID-19, these patients received emergent temporary transvenous pacing. All these patients were strictly monitored for reversion of sinus rhythm, requirement of back up pacing and ventricular arrhythmias for 10–14 days. Five patients with pacing dependent and symptomatic complete heart block, underwent dual-chamber permanent pacemaker implantations approximately 2 weeks after the presentation, with the use of personal protective equipment as per the guidelines of our institution. Two patients with sick sinus syndrome patients were kept under medical follow-up.
COVID-19 has been associated with development of cardiac dysfunction in patients with or without underlying cardiac condition [1]. In this largest case series of bradyarrhythmia in patients with COVID-19, we report complete heart block requiring intervention in 5 patients and sinus node dysfunction in 2 patients. There have been few isolated reports of development of clinically significant bradycardia in few patients with COVID-19 [2,3]. A recent publication reported sinus node dysfunction in 2 patients with COVID-19, both of whom remained in sinus bradycardia after discharge. Another publication reported a solitary case of transient complete heart block in a critically ill patient who died from pulmonary complications of COVID-19 [2,3]. In present series, none of the patient had any reversible cause of complete heart block.
A definitive mechanism for the development of bradyarrhythmia in patients with COVID-19 has not been established yet. Furthermore, it is not known if the virus for COVID-19 has any affinity for the receptors in the myocardial conduction system. As myocarditis has been reported in many patients with COVID-19, it is plausible that myocardial inflammation and injury may affect the conduction system resulting in complete heart block [4]. Autopsies of patients who died secondary to COVID-19 have showed the presence of viral RNA in cardiac myocytes and endothelial cells suggesting direct involvement of the myocardium in this disease. The COVID-19 virus may enter the cardiac myocytes via angiotensin-converting enzyme 2 (ACE2) receptor resulting in myocardial inflammation and injury [5]. Cardiac Magnetic Resonance Imaging (MRI), a definite non-invasive test for myocarditis is currently unavailable at our medical centre due to the COVID-19 pandemic. However, since only 1 patient in our case series had an elevated high-sensitive troponin T, a marker of myocardial injury, we expect that the majority of these patients did not have myocarditis.
In conclusion, patients with COVID-19 may be observed for possible bradyarrhythmias. While, there is no definitive evidence of causality.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Peer review under responsibility of Indian Heart Rhythm Society.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
figs1.
figs2.
References
- 1.Fried J.A., Ramasubbu K., Bhatt R. The variety of cardiovascular presentations of COVID-19. Circulation. 2020;141(23):1930–1936. doi: 10.1161/CIRCULATIONAHA.120.047164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Peigh G., Leya M.V., Baman J.R., Cantey E.P., Knight B.P., Flaherty J.D. Novel coronavirus 19 (COVID-19) associated sinus node dysfunction: a case series. Eur Heart J Case Rep. 2020 doi: 10.1093/ehjcr/ytaa132. ytaa132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Azarkish M., Laleh Far V., Eslami M., Mollazadeh R. Transient complete heart block in a patient with critical COVID-19. Eur Heart J. 2020;41(22):2131. doi: 10.1093/eurheartj/ehaa307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Driggin E., Madhavan M.V., Bikdeli B. Cardiovascular considerations for patients, health care workers, and health systems during the COVID-19 pandemic. J Am Coll Cardiol. 2020;75(18):2352–2371. doi: 10.1016/j.jacc.2020.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Oudit G.Y., Kassiri Z., Jiang C. SARS-coronavirus modulation of myocardial ACE2 expression and inflammation in patients with SARS. Eur J Clin Invest. 2009;39(7):618–625. doi: 10.1111/j.1365-2362.2009.02153.x. [DOI] [PMC free article] [PubMed] [Google Scholar]