Q Fever Pneumonia: Virulence of Coxiella burnetii Pathovars in a Murine Model of Aerosol Infection (original) (raw)
Abstract
Q fever is a worldwide zoonosis caused by Coxiella burnetii, a strictly intracellular bacterium that is a potential bioweapon. Humans usually acquires Q fever after inhalation of dust infected by subclinical animals. We used an aerosol exposure apparatus to challenge immunocompetent (BALB/c) and severe combined immunodeficient (SCID) mice with two different strains (strain Nine Mile and strain Q 212) of C. burnetii at two different inocula. Pathological lesions and dissemination of the bacteria were related to the size of the inoculum. SCID mice showed major pulmonary lesions, whereas similarly infected BALB/c mice were more able to eliminate the bacteria. Pathological differences were found between the strains, with Nine Mile showing more severe histological lesions and quantified spread of bacteria. Our animal model could provide a new tool for the study of acute Q fever pneumonia, the development of Q fever in immunodeficient hosts, and the differentiation of pathogenicity among C. burnetii isolates.
Q fever (“query fever”), a zoonosis caused by the obligate intracellular bacterium Coxiella burnetii, is endemic throughout the world (18). The most common animal reservoirs of C. burnetii are cattle, sheep, cats, and goats, but a variety of other mammalian, avian, and arthropod hosts have been described (13). The heavily infected placenta contaminates the environment at the time of parturition, and microorganisms are viable in the soil for several months (14). C. burnetii is highly infectious, with as little as one organism causing clinical infection; it therefore has high potential for use in biowarfare (17). Human Q fever may be acute or chronic. The acute form generally presents as a self-limiting febrile illness, often associated with pneumonia or hepatitis, whereas chronic Q fever most often presents as endocarditis and is fatal in the absence of appropriate treatment (19, 42). The heterogeneity of C. burnetii strains has been reported (24, 39), and the clinical course of infections may be strain related. Also, the recognition of cases of chronic Q fever in immunocompromised hosts has emphasized the importance of host factors in this disease (24).
In animals, as in humans, aerosols represent the main route of infection. We recently established an animal model in which mice were inoculated intranasally or intraperitoneally. We used this model to demonstrate that the route of infection may contribute to the clinical manifestations of acute Q fever (20). The intranasal inoculation route does not, however, perfectly mimic the aerosol inhalation route, and the size of the inoculum was not standardized. Cynomolgus monkeys have been used as a laboratory animal model for Q fever pneumonia using an aerosol exposure apparatus, but this involves extensive laboratory procedures (46). A suitable, simpler animal model is needed to clarify the pathogenicity of Q fever and its capacity to be used as an aerosolized biological weapon.
C. burnetii is an agent suitable for bioterrorism since it is highly infectious; it is believed that one organism can produce a symptomatic infection in a person (43). Also, C. burnetii can produce a sporelike form resistant to heat and drying and can persist in the environment for long periods. C. burnetii could be used in bioterrorism attacks in an aerosolized form or as a contaminant of food, water, or possibly even postal mail. Ingestion of moderate doses of C. burnetii would be unlikely to produce clinical symptoms, and it has been demonstrated that ingestion of milk contaminated with C. burnetii has resulted in seroconversion, without clinical disease, in human volunteers (4). Release of the aerosolized form of C. burnetii, as studied in the model we report here, in a densely populated area could cause the abrupt onset of an illness similar to that seen with the naturally occurring disease. Madariaga et al. evaluated the effects of 50 kg of C. burnetii being released along a 2-km front upwind of a population of 500,000. The organism would spread over an area of at least 20 km, would cause ca. 150 deaths, and would lead to 125,000 people becoming incapacitated. Of the latter, 9,000 would develop chronic Q fever and an uncertain number would develop acute and chronic psychiatric disorders (17).
The objectives of our study were to create an animal model of aerosol infection with C. burnetii and to determine the pathogenic potential of the organism in terms of the properties of the infecting strain, the inoculum size and the immunological status of the host. We used a device to cause aerosol exposure of immunocompetent BALB/c and severe combined immunodeficient (SCID) mice with two different strains of C. burnetii (strain Nine Mile and strain Q 212) with two different inocula. The pathogenic potential in the two mouse strains was determined by serology, histological, and immunohistological analysis, and detection of bacteria by PCR.
MATERIALS AND METHODS
Animals.
A total of 66 male 6-week-old BALB/c mice and 66 male 6-week-old SCID mice were obtained from the Charles River experimental animal facility (Saint Aubain Les Elbeuf, France). Mice were shipped under legislated travel conditions with certificates of health and origin. All of the animals were kept under controlled conditions in a P3 high-security facility with sterile food and water ad libitum in accordance with the guidelines of the French Council of Animal Care.
Bacteria.
C. burnetii prototype strains Nine Mile phase I and Q 212 phase I, provided by the American Type Culture Collection, were used in the study. Each bacterial strain was first inoculated intraperitoneally in BALB/c mice. Twenty days later, mice were sacrificed, and their spleens were homogenized and inoculated onto L929 monolayers as described previously (41). The organisms were only passaged three times in L929 medium to maintain the bacteria in phase 1 before the monolayers were harvested by using sterile glass beads. The remaining L929 cells were harvested after 0.5% trypsin was added for 30 min at 37°C and the trypsin was heat inactivated at 65°C for 1 h. Harvested organisms were purified by renografin density gradient centrifugation and stored at −80°C in 5- or 10-ml fractions. Titration to provide appropriate inocula was performed in the same manner for both of the strains (45). To establish the number of infecting units per milliliter of the bacterial cell suspensions, dilutions (10−1 to 10−10 of the suspension) were tested by infecting confluent monolayers of HEL cells in centrifugation shell vials. After removing the media from the shell vials, the HEL monolayers were infected with 0.4 ml of the bacterial suspension dilutions and centrifuged at 30°C for 1 h at 700 × g. The supernatant was discarded, 1 ml of fresh medium was added, and the shell vials were incubated for 6 days at 37°C. Infected cells were demonstrated by indirect immunofluorescence with locally prepared rabbit antiserum to C. burnetii. The number of infective C. burnetii per milliliter of inoculum was calculated from the last dilution that resulted in at least one infected cell.
Inoculation experiments.
On day 1, the mice were inoculated by using an aerosolization device with an inoculum of 107 or 108 C. burnetii in 20 ml of sterile phosphate-buffered saline. The mice were placed in the exposure chamber of an airborne infection apparatus (Ysebaert, Frepillon, France), the nebulizer compartment was filled with 20 ml of the appropriate C. burnetii suspension, and the aerosol administered over 45 min.
In all, four groups of 30 mice (15 BALB/c mice and 15 SCID mice) were studied. Group 1 mice received an inoculum of 108 C. burnetii Nine Mile strain, and group 2 mice received 107 of these organisms. Group 3 mice received 108 of C. burnetii Q 212 strain, and group 4 mice received 107 of these organisms. All C. burnetii were in phase I at the time of inoculation. A negative control group of six BALB/c mice and six SCID mice received 20 ml of phosphate-buffered saline containing no organisms. Each group of infected mice and the negative controls were maintained in separate rooms in a P-3 specific-pathogen-free facility. The conditions under which the mice were maintained were in agreement with the European Union laws for the protection of experimental animals. The animals were monitored daily by using a protocol that included monitoring for weight loss, apparent ill health (bristled hair and skin lesions), and behavioral changes (signs of aggressiveness or withdrawal).
For studies of antibody titers to C. burnetii phase I and II antigens, tail blood was obtained from the mice at the beginning of the study. At days 0 (2 h after inoculation), 7, and 14 of the study, five BALB/c mice and five SCID mice were sacrificed, as well as two BALB/c mice and two SCID mice from the control group. Before euthanasia, mice were anesthetized with ether, and blood samples were obtained for serology by puncture of the lung. At necropsy, samples of lung, liver, spleen, heart, and brain were preserved in formalin for histology and immunohistochemistry.
Serology.
Antibodies to phase I and II C. burnetii whole-cell antigens were determined in the sera by a microimmunofluorescence testing with antigens of the Nine Mile strain as described previously (44). The starting dilution for the serum samples was 1:25, and titers of the samples were determined to the endpoint.
Histological and immunohistological analysis.
For each mouse, the left lung, the liver, the spleen, the brain, and the heart were removed, fixed with buffered formalin 4%, and embedded in paraffin. Serial sections (3-μm) of these specimens were obtained for routine hematoxylin-eosin-saffron and immunohistochemical investigations.
The inflammatory granulomas present in each tissue section of the lungs were counted during microscopic examination, and the total area of tissue sections was determined by quantitative image analysis as described previously (15). Briefly, histologic images were digitized and transferred to a computer system. Using the image analyzer SAMBA 2005 (SAMBA Technologies) and a specific interactive program providing visual control of analysis, we quantified the total area of each tissue section. The results were expressed as the number of granulomas found per surface unit (i.e., square millimeters).
Immunohistochemical analysis was performed with a rabbit anti-C. burnetii antibody used at a 1:2,000 dilution. The immunohistological procedure, in which an immunoperoxidase kit was used, has been described elsewhere (12). For each tissue section, a negative control was performed with normal rabbit serum. After immunohistochemical staining, the number of C. burnetii seen by microscopic examination of the lungs was counted. The results were expressed as the number of immunostained bacteria found per surface unit (i.e., square millimeters) as described above.
Counts of granulomas and C. burnetii seen were expressed as the mean ± the standard deviation per square millimeter and compared by using the Student t test. Differences were considered significant when the P value was <0.05.
Detection of C. burnetii by genomic amplification.
Total genomic DNA was extracted from 200 μl of serum by using the QIAamp Blood Kit (Qiagen, Hilden, Germany) as described by the manufacturer. Then, 50 μl of elution buffer was used to resuspend the DNA, and the genomic DNAs were stored at 4°C until PCR assays were performed.
The LightCycler nested PCR assay has been described previously (6). DNA samples were handled carefully to avoid the risk of cross-contamination. DNA extraction, mix preparation, and PCRs were performed in different rooms to prevent PCR carryover contamination. DNA extracted from blood specimens from uninfected mice was used as a negative control. Each 20-μl reaction mixture contained 4 μl of DNA Master SYBR Green; 4.8 μl of 3 mM MgCl2; 1 μl of each of the four primers IS111F1 (5′-ACTGGGTGTTGATATTGC-3′), IS111R1 (5′-CCGTTTCATCCGCGGTG-3′), IS111F2 (5′-GTAAAGTGATCTACACGA-3′), and IS111R2 (5′-TTAACAGCGCTTGAACGT-3′) at 0.5 μM; 5.2 μl of sterile distilled water; and 2 μl of DNA. The IS111F1 and IS111R1 primers, designed to amplify a 485-bp fragment of the htpAB-associated repetitive element (GenBank accession number M80806), were used for the first amplification, and reamplification was performed by using the IS111F2 and IS111R2 primers, which amplify a 260-bp fragment. After an initial denaturation step at 95°C for 8 min, our rapid nested PCR program was performed with 35 cycles of denaturation at 95°C for 15 s (temperature transition, 20°C/s), annealing at 52°C for 5 s, and extension at 72°C for 18 s, followed by 35 cycles of denaturation at 95°C for 15 s (temperature transition, 20°C/s), annealing at 48°C for 5 s, and extension at 72°C for 18 s. The amplification was completed by holding the reaction mixture at 68°C for 10 min to enable complete extension of the PCR products. Since the LightCycler was not able to infer the results from the nested PCR, in particular the melting curve, amplicons from the second amplification were separated by electrophoresis on 1% agarose gels and purified by using a QIAquick PCR purification kit (Qiagen), as described by the manufacturer.
The PCR products obtained from the test samples were sequenced in both directions by using the d-Rhodamine Terminator Cycle Sequencing Ready Reaction kit (Perkin-Elmer, Coignières, France) as described by the manufacturer. Sequencing products were resolved by using an ABI 3100 automated sequencer (Perkin-Elmer). Sequence analysis was performed with the software package ABI Prism DNA Sequencing Analysis Software version 3.0 (Perkin-Elmer), and multisequence alignment was done by using CLUSTAL W software (version 1.81).
RESULTS
C. burnetii infection in mice.
Infected mice became ill 4 to 7 days after infection; their coats became ruffled, and they were inactive. None of the mice died. All infected BALB/c mice sacrificed at days 7 and 14 had developed antibodies to C. burnetii phase I and II antigens (titers from 1:200 to 1:1,600). Mice sacrificed at day 0, SCID mice, and control mice remained seronegative to C. burnetii. Table 1 summarizes the results of our PCR experiments to detect C. burnetii DNA in the blood of the infected mice. C. burnetii was detected at day 0, 7, and 14 in the blood of the group 1 mice but only at day 0 in the blood of the group 2 animals. In the mice in groups 3 and 4, C. burnetii was only detected in a few animals sacrificed at day 0 and day 7. No amplification products were obtained with blood from the control mice.
TABLE 1.
Detection of C. burnetii in blood of BALB/c and SCID mice by PCR
| Strain (bacteria/ml) | Day of sacrifice | Mouse strain | No. of _C. burnetii_-infected mice/total no. of mice tested |
|---|---|---|---|
| Nine Mile (108/ml) group 1 | 0 | SCID | 1/5 |
| BALB/c | 1/5 | ||
| 7 | SCID | 4/5 | |
| BALB/c | 3/5 | ||
| 14 | SCID | 5/5 | |
| BALB/c | 1/5 | ||
| Nine Mile (107/ml) group 2 | 0 | SCID | 1/5 |
| BALB/c | 1/5 | ||
| 7 | SCID | 0/5 | |
| BALB/c | 0/5 | ||
| 14 | SCID | 0/5 | |
| BALB/c | 0/5 | ||
| Q 212 (108/ml) group 3 | 0 | SCID | 1/5 |
| BALB/c | 1/5 | ||
| 7 | SCID | 3/5 | |
| BALB/c | 2/5 | ||
| 14 | SCID | 0/5 | |
| BALB/c | 0/5 | ||
| Q 212 (107/ml) group 4 | 0 | SCID | 1/5 |
| BALB/c | 0/5 | ||
| 7 | SCID | 0/5 | |
| BALB/c | 0/5 | ||
| 14 | SCID | 0/5 | |
| BALB/c | 0/5 | ||
| Negative control | 0 | SCID | 0/2 |
| BALB/c | 0/2 | ||
| 7 | SCID | 0/2 | |
| BALB/c | 0/2 | ||
| 14 | SCID | 0/2 | |
| BALB/c | 0/2 |
Histological findings.
Inflammatory reactions to C. burnetii were only seen in BALB/c and SCID mice infected with 108 Nine Mile strain organisms (group 1). No histological changes were found in the organs ofBALB/c and SCID mice infected with 107 organisms of Nine Mile strain (group 2) or in those infected with 108 (group 3) or 107 (group 4) Q 212 strain organisms.
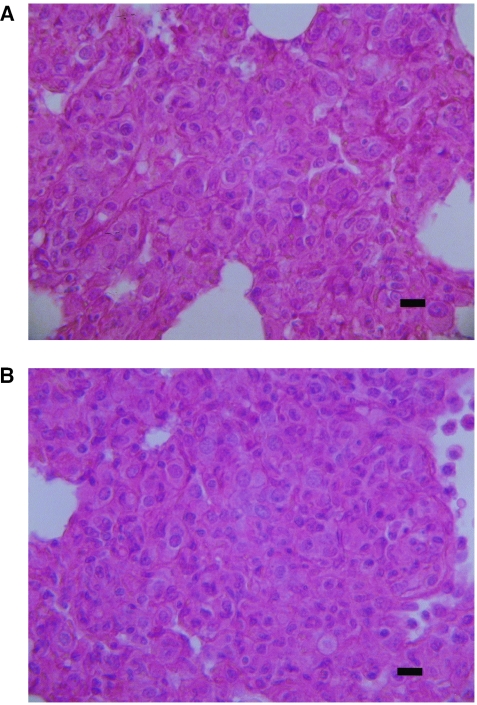
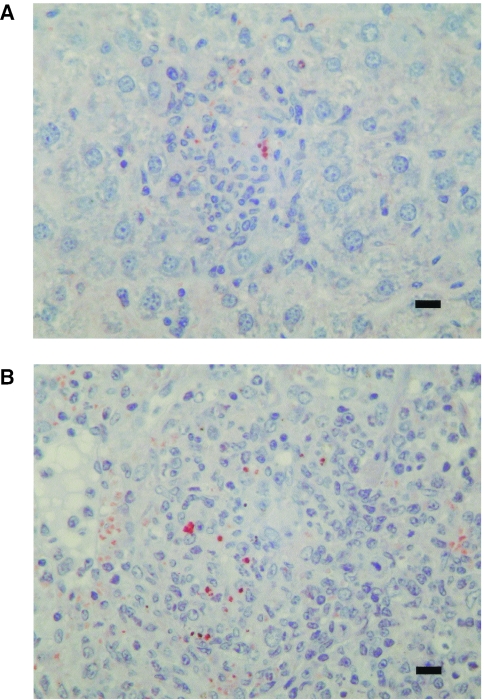
In the lungs, inflammation was observed at days 7 and 14 postinfection. Inflammatory infiltrates were largely confined within the walls of the alveoli. The interalveolar walls were infiltrated by a mononuclear inflammatory infiltrate composed of numerous macrophages and lymphocytes that were often organized as granulomatous interstitial inflammation (Fig. 1). The bronchioalveolar air spaces were relatively free of cellular exudates, but some were filled with alveolar macrophages with pale cytoplasm. Neither necrosis of the lining alveolar epithelium nor suppuration was observed. These findings are consistent with a mixed interstitial and mild alveolar mononuclear cell pneumonia.
FIG. 1.
C. burnetii pneumonia in mice infected with 108 Nine Mile strain organisms. The thickened alveolar walls are heavily infiltrated with mononuclear leukocytes, macrophages, and lymphocytes, with granulomatous interstitial inflammation. (A) BALB/c mouse; (B) SCID mouse. Hematoxylin-eosin-saffron staining was used. Magnification, ×400. Scale bars, 10 μm.
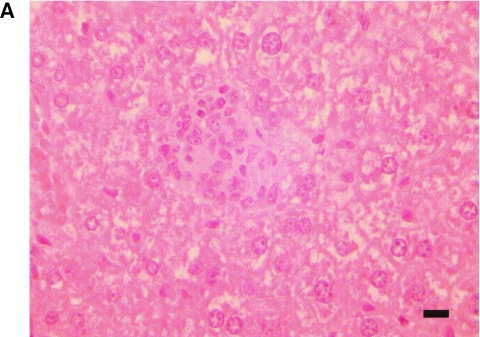
Granulomas were only detected in the liver at day 14 in the BALB/c and SCID mice and in the spleen at day 14 in SCID mice (Fig. 2). The granulomas were randomly distributed in the liver parenchyma (Fig. 2A and B), whereas in spleen they were confined to the red pulp (Fig. 2C). No inflammatory lesions or granulomas were found in the heart or the brain.
FIG. 2.
Sections of _C. burnetii_-induced granulomas at day 14 postinfection in the liver of a BALB/c mouse (A) and in the liver (B) and spleen (C) of a SCID mouse. Granulomas are located in the liver parenchyma and in the splenic red pulp. Hematoxylin-eosin was used. Magnification, ×400. Scale bars, 10 μm.
In the lung parenchyma, granulomas were apparent by day 7 and had decreased by day 14. They were of variable diameter and scattered throughout the interalveolar walls of the lung parenchyma. Since the formation of granulomas is associated with a protective cell-mediated immune response, we counted the granulomas we found in the lung tissue sections (Table 2). The number of inflammatory granulomas was significantly higher in SCID mice infected with the Nine Mile strain than in BALB/c mice infected with Nine Mile strain (P = 0.01) at day 14 but not at day 7 (P > 0.05). Also, there was a significant decrease in the numbers of granulomas between days 7 and 14 in each mouse strain (P = 0.01 and P = 0.01, respectively).
TABLE 2.
Granuloma and bacterium counts in lungs of BALB/c and SCID mice infected with 108 Nine Mile strain organisms
| Mouse group (inoculum) and day postinfection | Mean no./mm2 ± SDa | |
|---|---|---|
| Granulomas | Bacteria | |
| BALB/c mice infected with Nine Mile (108 organisms) | ||
| 7 | 0.84 ± 0.05 | 3.15 ± 1.11 |
| 14 | 0.12 ± 0.02 | 0.24 ± 0.12 |
| SCID mice infected with Nine Mile (108 organisms) | ||
| 7 | 0.86 ± 0.26 | 6.84 ± 2.39 |
| 14 | 0.43 ± 0.18 | 2.21 ± 0.89 |
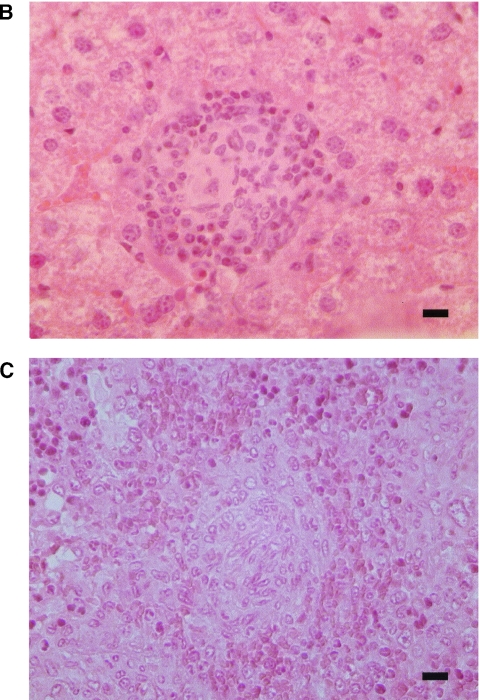
Immunohistochemical analysis.
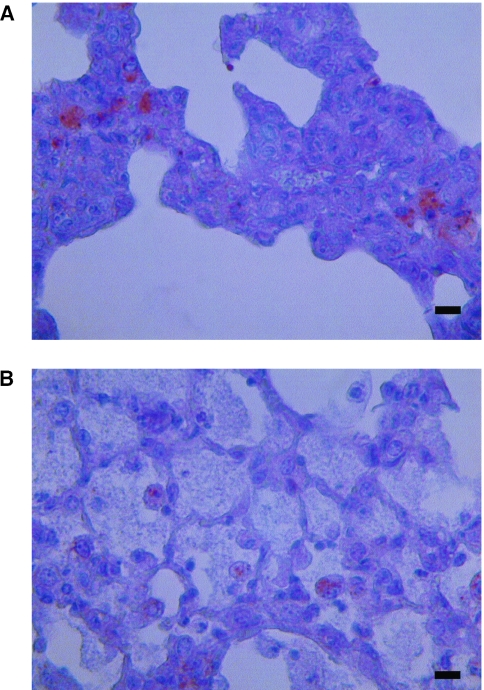
Bacteria were detected by immunohistochemistry in only the lungs, livers, and spleens of BALB/c and SCID mice infected with 108 Nine Mile strain organisms. Bacteria were seen at days 7 and 14 as coarse granular immunopositive material in cells, which had the morphology of macrophages. In the lungs, the macrophages containing organisms were observed in the mononuclear cell inflammatory infiltrates or in granulomas present in interalveolar walls (Fig. 3A) and rarely in bronchioloalveolar air spaces (Fig. 3B). Significantly more bacteria were seen in SCID mice than in BALB/c mice at day 14 (P = 0.01) but not at day 7 (P > 0.05) (Table 2). The number of bacteria in each mouse strain decreased significantly between days 7 and 14 (P = 0.01 and P = 0.01, respectively). Bacteria were seen in macrophages in granulomas in the liver at day 14 in BALB/c and SCID mice (Fig. 4A) and in the spleen at day 14 in SCID mice (Fig. 4B).
FIG. 3.
Demonstration of C. burnetii antigen by immunohistochemistry in the lung of a SCID mouse 7 days after infection with 108 Nine Mile strain organisms. Cytoplasmic vacuoles of macrophages in inflammatory granuloma present in interalveolar walls (A) and in alveolar air spaces (B) are packed with coarse granular immunopositive material. Polyclonal rabbit anti-C. burnetii antibody was used at a dilution of 1:2,000, along with hemalun counterstain. Magnification, ×400. Scale bars, 10 μm.
FIG. 4.
Immunohistochemical demonstration of C. burnetii antigen in liver (A) and spleen (B) of a SCID mouse at day 14 postinfection with 108 Nine Mile strain organisms. Granulomas are composed predominantly of epithelioid macrophages, in part infected. The granulomas and the splenic white pulp are almost completely devoid of lymphoid cells. Polyclonal rabbit anti-C. burnetii antibody at a dilution of 1:2,000 was used, along with hemalun counterstain. Magnification, ×400. Scale bars, 10 μm.
Bacteria were not detected in the organs from mice infected with 107 Nine Mile strain C. burnetii (group 2), from mice infected with 108 (group 3) or 107 (group 4) Q 212 strain organisms, and from the control mice.
DISCUSSION
In our study we were able to design a murine model of aerosol-induced experimental Q fever to assess the effects of two inocula of two isolates of C. burnetii on BALB/c mice and immunocompromised SCID mice. Infected mice became ill between 4 and 7 days after infection, but none of the animals died. This is similar to the situation in humans where Q fever is a mild disease.
As we reported previously (12, 20), in animals the route of infection may determine the predominant manifestations of Q fever, with the lungs having more pronounced pathological changes than the livers and spleens after infection by inhalation of contaminated aerosols. In the present study, we again demonstrated that infections resulting from aerosols can result in liver and spleen lesions. Presumably, infection initially spreads within the lungs as C. burnetii are released from heavily infected dead alveolar macrophages and the organisms are then ingested by macrophages in the same and adjoining alveoli. From the lungs, the infection may spread hematogenously to other organs such as the liver and spleen. This hypothesis is supported by our finding of C. burnetii by PCR in the blood of the infected mice in our experiments (Table 1).
The influence of the inoculum size in pathological changes during experimental Q fever has been demonstrated in guinea pigs (12, 43). A dose-response effect in clinical findings has been described for monkeys (8), for human volunteers (2, 43), and from indirect evidence in outbreaks in which the incubation period ranged from 7 to 30 days according to the intensity of exposure (5). In our model, inoculating 108 C. burnetii Nine Mile strain into mice (group 1) resulted in interstitial pneumonia developing in 7 to 14 days in both immunocompetent and immunocompromised mice. Inoculation with a lower number of organisms (107), however, did not result in the development of pathological lesions. Our study confirms that large numbers of C. burnetii must be present in aerosols before they can lead to the development of Q fever. Infected placentas have been shown to contain at least 109 bacteria/g (26, 28), and high levels of organisms in aerosols are thus likely to be common.
Previous studies have demonstrated the importance of the status of the host in the development of Q fever and, especially in mice, genetic influences are known to affect the expression of Q fever. Sidwell et al. inoculated white mice and deer mice with C. burnetii and observed relapses after irradiation (36, 37) or cortisone injection (36, 37) in white mice only. This showed that both genetic background and immunosuppression play a role in the development of infections with C. burnetii. Several authors have described cases of reactivation of Q fever in immunocompromised people (11, 16, 25, 27). In animals, recrudescence of latent infections has been documented in cattle during parturition (3) and in guinea pigs and mice after pregnancy (35), treatment with methyl-prednisolone (37), and whole-body X irradiation (36). Johnson et al. found that infections with C. burnetii in guinea pigs were reactivated by pregnancy and administration of methyl-prednisolone and cyclophosphamide (10). We recently demonstrated that intraperitoneal infection of female BALB/c mice with C. burnetii, followed by repeated pregnancies over a 2-year period, resulted in persistent infection and endocarditis (40). In the present study, histological examination of infected organs showed that well-developed granulomas formed at sites of C. burnetii implantation and multiplication and that organisms could be detected in the granulomas by using immunohistochemistry. These granulomas were observed in the lungs and livers of both mouse strains used in our experiments. They were, however, only found in the spleens of SCID mice despite their lack of functional T and B lymphocytes and their inability to generate T-cell-mediated immunological responses. These findings contrast with those of Andoh et al. (1), who infected SCID mice with the C. burnetii Nine Mile strain by intraperitoneal inoculation and found that the mice showed acute clinical symptoms and died. Similarly infected immunocompetent mice, however, remained asymptomatic and survived. The 50% lethal dose of C. burnetii for SCID mice was at least 108 times less than that for immunocompetent mice and, despite the inoculum size, the SCID mice could not recover from the disease and died. In the present model the clinical manifestations of animals were less severe, and most of the mice survived, which may open interesting approaches for studies of the comparative pathogenic potential of various C. burnetii strains.
The formation of granulomas has previously been observed in the lungs, livers, and spleens of SCID mice used in other models of infection with intracellular microorganisms such as the Calmette-Guerin bacillus (7, 23). The development of T-cell-independent granulomas in SCID mice has been shown to depend upon the induction of gamma interferon release by natural killer cells (38). In our model, there were more granulomas, and C. burnetii revealed by immunohistochemistry appeared to be more abundant in macrophages in the lungs of SCID mice than was the case with BALB/c mice. From days 7 to 14 of our experiments the numbers of granulomas and the numbers of visible C. burnetii decreased progressively in the lungs of both BALB/c and SCID mice. The decrease, however, was most marked in the BALB/c mice, perhaps because SCID mice have a defect in the bactericidal activity of their macrophages caused by a lack of CD4+ T cells and macrophage-activating products such as gamma interferon (33).
We also compared the pathogenicity of Nine Mile and Q 212 strains. The Nine Mile strain was isolated from a tick in Montana in 1936 and has the QpH1 plasmid (31). The strain Q 212 was isolated from the blood of a Canadian patient suffering from chronic Q fever endocarditis in 1990. This isolate has no plasmid, although the sequences of the QpRS plasmid is integrated into the organisms chromosome (32). The two strains are known to show differences in the composition of their lipopolysaccharides (9) and to have different cytopathic effects in cell cultures (41). Based on this genotypic and phenotypic heterogeneity, the hypothesis was advanced that different isolates strains of C. burnetii may be responsible for the different disease manifestations that can be caused by the organism. Samuel et al. (30) characterized C. burnetii isolates into genomic groups and suggested that organisms causing chronic Q fever would differ genetically from those that cause acute disease. Moos and Hackstadt (22) compared in an animal model the relative infectivity and virulence of lipopolysaccharide variants of the Nine Mile strain with those of the Priscilla strain. More recently the hypothesis was advanced that different strains with different pathogenicities could also be responsible for the different manifestations of acute Q fever (21, 29). When we compared the pathogenicity of the Nine Mile and Q 212 strains of C. burnetii, we found differences in histopathology and when the spread of the bacteria was quantitated. These findings suggest that there are unique pathogenic factors present in different strains that may be involved in the various manifestations of acute Q fever in humans. Different C. burnetii strains, therefore, do not all have the same potential as agents of acute infection and, as a bioterrorism agent, the Nine Mile strain was the most potent in our experiment. The specific factors involved in the pathogenicity of the Nine Mile strain could probably be deduced by comparative genomic studies with the less virulent Q 212 strain. In fact, the genome sequence of Nine Mile was recently published (34), and sequencing Q 212 may help us to understand the physiopathology of C. burnetii infection.
In conclusion, the results of the present study confirm that SCID mice are more susceptible than BALB/c mice to C. burnetii infection. We also found that the titer of the inoculum of C. burnetii is critical for the development of the disease in both immunocompetent and immunodepressed mice and that there are different pathovars among C. burnetii isolates.
.
Acknowledgments
We do not have any commercial or other association that might pose a conflict of interest, and the research described here has not benefited from any external financial support.
Editor: S. H. E. Kaufmann
REFERENCES
- 1.Andoh, M., T. Naganawa, A. Hotta, T. Yamaguchi, H. Fukushi, T. Masegi, and K. Hirai. 2003. SCID mouse model for lethal Q fever. Infect. Immun. 71**:**4717-4723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Anonymous. 1950. Experimental Q fever in man. Br. Med. J. 1:1000. [Google Scholar]
- 3.Babudieri, B. 1959. Q fever: a zoonosis. Adv. Vet. Sci. Comp. Med. 5**:**82-182. [Google Scholar]
- 4.Benson, W. W., D. W. Brock, and J. Mather. 1963. Serologic analysis of a penitentiary group using raw milk from a Q fever infected herd. Public Health Rep. 78**:**707-710. [PMC free article] [PubMed] [Google Scholar]
- 5.Embil, J., J. C. Williams, and T. J. Marrie. 1990. The immune response in a cat-related outbreak of Q fever as measured by the indirect immunofluorescence test and the enzyme-linked immunosorbent assay. Can. J. Microbiol. 36**:**292-296. [DOI] [PubMed] [Google Scholar]
- 6.Fournier, P. E., and D. Raoult. 2003. Comparison of PCR and serology assays for early diagnosis of acute Q Fever. J. Clin. Microbiol. 41**:**5094-5098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Goldmann, T., G. Zissel, R. S. Gupta, M. Schlaak, E. Vollmer, and J. Muller-Quernheim. 2001. Formation of granulomas in the lungs of severe combined immunodeficient mice after infection with bacillus Calmette-Guerin. Am. J. Pathol. 158**:**1890-1891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gonder, J. C., R. A. Kishimoto, M. D. Kastello, C. E. Pedersen, Jr., and E. W. Larson. 1979. Cynomolgus monkey model for experimental Q fever infection. J. Infect. Dis. 139:191-196. [DOI] [PubMed] [Google Scholar]
- 9.Hackstadt, T. 1990. The role of lipopolysaccharides in the virulence of Coxiella burnetii. Ann. N. Y. Acad. Sci. 590**:**27-32. [DOI] [PubMed] [Google Scholar]
- 10.Johnson, J. W., G. A. Eddy, and C. E. Pedersen, Jr. 1976. Biological properties of the M-44 strain of Coxiella burnetii. J. Infect. Dis. 133**:**334-338. [DOI] [PubMed] [Google Scholar]
- 11.Kanfer, E., N. Farrag, C. Price, D. MacDonald, J. Coleman, and A. J. Barrett. 1988. Q fever following bone marrow transplantation. Bone Marrow Transplant. 3**:**165-166. [PubMed] [Google Scholar]
- 12.La Scola, B., H. Lepidi, and D. Raoult. 1997. Pathologic changes during acute Q fever: influence of the route of infection and inoculum size in infected guinea pigs. Infect. Immun. 2443-2447. [DOI] [PMC free article] [PubMed]
- 13.Lang, G. H. 1990. Coxiellosis (Q fever) in animals, p. 23-48. In T. J. Marrie (ed.), Q fever, the disease. CRC Press, Inc., Boca Raton, Fla.
- 14.Langley, J. M. 1990. Perinatal Q fever: is Coxiella burnetii a human perinatal pathogen?, p. 201-212. In T. J. Marrie (ed.), Q fever, the disease. CRC Press, Inc., Boca Raton, Fla.
- 15.Lepidi, H., P. E. Fournier, and D. Raoult. 2000. Quantitative analysis of valvular lesions during Bartonella endocarditis: a case control study. Am. J. Clin. Pathol. 114**:**880-889. [DOI] [PubMed] [Google Scholar]
- 16.Lev, B. I., A. Shachar, S. Segev, P. Weiss, and E. Rubinstein. 1988. Quiescent Q fever endocarditis exacerbated by cardiac surgery and corticosteroid therapy. Arch. Intern. Med. 148**:**1531-1532. [PubMed] [Google Scholar]
- 17.Madariaga, M. G., K. Rezai, G. M. Trenholme, and R. A. Weinstein. 2003. Q fever: a biological weapon in your backyard. Lancet Infect. Dis. 3**:**709-721. [DOI] [PubMed] [Google Scholar]
- 18.Marrie, T. J. 1995. Coxiella burnetii (Q fever) pneumonia. Clin. Infect. Dis. 21**:**S253-S264. [DOI] [PubMed] [Google Scholar]
- 19.Marrie, T. J., and D. Raoult. 1997. Q fever: a review and issues for the next century. Int. J. Antimicrob. Agents 8**:**145-161. [DOI] [PubMed] [Google Scholar]
- 20.Marrie, T. J., A. Stein, D. Janigan, and D. Raoult. 1996. Route of infection determines the clinical manifestations of acute Q fever. J. Infect. Dis. 173**:**484-487. [DOI] [PubMed] [Google Scholar]
- 21.Maurin, M., and D. Raoult. 1999. Q fever. Clin. Microbiol. Rev. 12**:**518-553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Moos, A., and T. Hackstadt. 1987. Comparative virulence of intra- and interstrain lipopolysaccharide variants of Coxiella burnetii in the guinea pig model. Infect. Immun. 55**:**1144-1150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.North, R. J., and A. A. Izzo. 1993. Granuloma formation in severe combined immunodeficient (SCID) mice in response to progressive BCG infection: tendency not to form granulomas in the lung is associated with faster bacterial growth in this organ. Am. J. Pathol. 142**:**1959-1966. [PMC free article] [PubMed] [Google Scholar]
- 24.Raoult, D. 1990. Host factors in the severity of Q fever. Ann. N. Y. Acad. Sci. 590**:**33-38. [DOI] [PubMed] [Google Scholar]
- 25.Raoult, D., P. Brouqui, B. Marchou, and J. A. Gastaut. 1992. Acute and chronic Q fever in patients with cancer. Clin. Infect. Dis. 14**:**127-130. [DOI] [PubMed] [Google Scholar]
- 26.Raoult, D., F. Fenollar, and A. Stein. 2002. Q fever during pregnancy: diagnosis, treatment, and follow-up. Arch. Intern. Med. 162**:**701-704. [DOI] [PubMed] [Google Scholar]
- 27.Raoult, D., P. Y. Levy, H. T. Dupont, C. Chicheportiche, C. Tamalet, J. A. Gastaut, and J. Salducci. 1993. Q fever and HIV infection. AIDS 7**:**81-86. [DOI] [PubMed] [Google Scholar]
- 28.Raoult, D., and D. Stein. 1994. Q fever during pregnancy: a risk for women, fetuses, and obstetricians. N. Engl. J. Med. 330**:**371. [DOI] [PubMed] [Google Scholar]
- 29.Raoult, D., H. Tissot-Dupont, C. Foucault, J. Gouvernet, P. E. Fournier, E. Bernit, A. Stein, M. Nesri, J. R. Harle, and P. J. Weiller. 2000. Q fever 1985-1998: clinical and epidemiologic features of 1,383 infections. Medicine 79**:**109-123. [DOI] [PubMed] [Google Scholar]
- 30.Samuel, J. E., M. E. Frazier, and L. P. Mallavia. 1985. Correlation of plasmid type and disease caused by Coxiella burnetii. Infect. Immun. 49**:**775-779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Samuel, J. E., M. E. Frazier, and L. P. Mallavia. 1988. Stability of plasmid sequences in an acute Q-fever strain of Coxiella burnetii. J. Gen. Microbiol. 134**:**1795-1805. [DOI] [PubMed] [Google Scholar]
- 32.Samuel, J. E., M. E. Frazier, and L. P. Mallavia. 1990. Comparison of Coxiella burnetii plasmids to homologous sequences present in a plasmidless endocarditis causing isolate. Ann. N. Y. Acad. Sci. 590**:**33-38. [DOI] [PubMed] [Google Scholar]
- 33.Sandor, M., J. V. Weinstock, and T. A. Wynn. 2003. Granulomas in schistosome and mycobacterial infections: a model of local immune responses. Trends Immunol. 24**:**44-52. [DOI] [PubMed] [Google Scholar]
- 34.Seshadri, R., I. T. Paulsen, J. A. Eisen, T. D. Read, K. E. Nelson, W. C. Nelson, N. L. Ward, H. Tettelin, T. M. Davidsen, M. J. Beanan, R. T. Deboy, S. C. Daugherty, L. M. Brinkac, R. Madupu, R. J. Dodson, H. M. Khouri, K. H. Lee, H. A. Carty, D. Scanlan, R. A. Heinzen, H. A. Thompson, J. E. Samuel, C. M. Fraser, and J. F. Heidelberg. 2003. Complete genome sequence of the Q-fever pathogen Coxiella burnetii. Proc. Natl. Acad. Sci. USA 100**:**5455-5460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sidwell, R. W., and L. P. Gebhardt. 1997. Studies of latent Q fever infections III. Effects of parturition upon latently infected guinea pigs and white mice. Am. J. Epidemiol. 84**:**132-137. [DOI] [PubMed] [Google Scholar]
- 36.Sidwell, R. W., B. D. Thorpe, and L. P. Gebhardt. 1964. Studies of latent Q fever infections. I. Effects of whole body X irradiation upon latently infected guinea pigs, white mice and deer mice. Am. J. Hyg. 79**:**113-124. [PubMed] [Google Scholar]
- 37.Sidwell, R. W., B. D. Thorpe, and L. P. Gebhardt. 1964. Studies of latent Q fever infections. II. Effects of multiple cortisone injections. Am. J. Hyg. 79**:**320-327. [DOI] [PubMed] [Google Scholar]
- 38.Smith, D., H. Hansch, G. Bancroft, and S. Ehlers. 1997. T-cell-independent granuloma formation in response to Mycobacterium avium: role of tumour necrosis factor-alpha and interferon-gamma. Immunology 92**:**413-421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Stein, A., D. Kruszewska, J. Gouvernet, and D. Raoult. 1997. Study of the 16S-23S ribosomal DNA internal spacer of Coxiella burnetii. Eur. J. Epidemiol. 13**:**471-475. [DOI] [PubMed] [Google Scholar]
- 40.Stein, A., H. Lepidi, J. L. Mege, T. J. Marrie, and D. Raoult. 2000. Repeated pregnancies in BALB/c mice infected with Coxiella burnetii cause disseminated infection resulting in abortion, stillbirth, and endocarditis. J. Infect. Dis. 181**:**188-194. [DOI] [PubMed] [Google Scholar]
- 41.Stein, A., and D. Raoult. 1992. Phenotypic and genotypic heterogeneity of eight new human Coxiella burnetii isolates. Acta Virol. 36**:**7-12. [PubMed] [Google Scholar]
- 42.Stein, A., and D. Raoult. 1995. Q fever endocarditis. Eur. Heart J. 16**:**19-23. [DOI] [PubMed] [Google Scholar]
- 43.Tigertt, W. D., A. S. Benenson, and W. S. Gochenour. 1961. Airborne Q fever. Bacteriol. Rev. 25**:**285-293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tissot-Dupont, H., X. Thirion, and D. Raoult. 1994. Q fever serology: cutoff determination for microimmunofluorescence. Clin. Diagn. Lab. Immunol. 1**:**189-196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Torres, H., and D. Raoult. 1993. In vitro activities of ceftriaxone and fusidic acid against 13 isolates of Coxiella burnetii, determined using the shell vial assay. Antimicrob. Agents Chemother. 37**:**491-494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Waag, D. M., W. R. Byrne, J. Estep, P. Gibbs, M. L. M. Pitt, and C. M. Banfield. 1999. Evaluation of cynomologus (Macaca fascicularis) and rhesus (Macaca mulatta) monkeys as experimental models of acute Q fever after aerosol exposure to phase-I Coxiella burnetii. Lab. Anim. Sci. 49**:**634-938. [PubMed] [Google Scholar]