Risk Factors for Surgery and Postoperative Recurrence in Crohn’s Disease (original) (raw)
Abstract
Objective
To assess the impact of possible risk factors on intestinal resection and postoperative recurrence in Crohn’s disease (CD) and to evaluate the disease course.
Summary Background Data
The results of previous studies on possible risk factors for surgery and recurrence in Crohn’s disease have been inconsistent. Varying findings may be explained by referral biases and small numbers of patients in some studies.
Methods
Data on initial intestinal resection and postoperative recurrence were evaluated retrospectively in a population-based cohort of 1,936 patients. The influence of concomitant risk factors was assessed using uni- and multivariate analyses.
Results
The cumulative rate of intestinal resection was 44%, 61%, and 71% at 1, 5, and 10 years after diagnosis. Postoperative recurrences occurred in 33% and 44% at 5 and 10 years after resection. The relative risk of surgery was increased in patients with CD involving any part of the small bowel, in those having perianal fistulas, and in those who were 45 to 59 years of age at diagnosis. Female gender and perianal fistulas, as well as small bowel and continuous ileocolonic disease, increase the relative risk of recurrence.
Conclusions
Three of four patients with CD will undergo an intestinal resection; half of them will ultimately relapse. The extent of disease at diagnosis and the presence of perianal fistulas have an impact on the risk of surgery and the risk of postoperative recurrence. Women run a higher risk of postoperative recurrence than men. The frequency of surgery has decreased over time, but the postoperative relapse rate remains unchanged.
Patients with Crohn’s disease (CD) are a heterogeneous group and consequently the individual course of the disease is difficult to predict: some have a rather mild form, but others suffer frequent flare-ups requiring resection, with symptoms recurring soon after surgery. In accordance with the chronic nature of the disease, only 12% of patients with CD have been reported to have experienced a relapse-free course 10 years after diagnosis. 1
To preserve bowel function, a more conservative surgical approach has been adopted during the past few decades. In cases of medical intractabilty, internal fistulas, intestinal obstruction, hemorrhage, toxic dilatation, or acute perforation, however, surgical resection inevitably becomes necessary. 2
Despite the general knowledge of a high probability of intestinal resections in CD patients, few studies since the initial work in the 1970s and 1980s 3 have focused on the risk and risk factors for the initial intestinal resection in CD. 4,5 In contrast, several studies have evaluated the risk and possible risk factors for postoperative recurrent disease, 6,7 but these studies have produced disparate results. 5,8,9 Age, gender, disease localization, preoperative duration of history, and the presence of granulomas have all had different impacts on postoperative recurrence, and thus no sure risk factor, apart from smoking, 10 has yet been established. The varying results may have been mainly attributable to different study designs with reference to the type of patients included and the definition of recurrence.
The aims of this study were to evaluate the probability of undergoing intestinal resection and to assess the risk of postoperative recurrence in a population-based cohort. Included in the assessment were the impact of gender, age, and disease localization at diagnosis, perianal fistulas, duration of disease, and time trends during a 35-year period.
MATERIALS AND METHODS
Case Identification and Criteria for Diagnosis
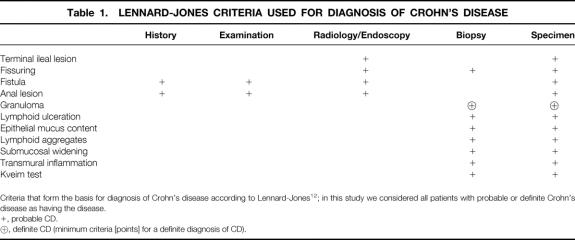
The present study is based on a retrospectively assembled cohort of patients with CD previously described in detail. 11 All inhabitants in Stockholm County diagnosed with CD between 1955 and 1989 were included in the study. Possible cases were sought in diagnosis registers covering hospital admissions from 1955 to 1992 and outpatient visits to internal medicine units during 1993 and 1994. In addition, gastroenterologists in private practice were asked about possible cases and their colonoscopy reports were assessed. The previous diagnoses were reevaluated and confirmed according to the criteria adopted by Lennard-Jones 12 considering history, radiologic and endoscopic examination, macroscopic findings at surgery, and microscopic findings in biopsies and specimens (Table 1). Based on these criteria, a diagnosis of Crohn’s disease is possible on clinical grounds without a final determination from tissue.
Table 1. LENNARD-JONES CRITERIA USED FOR DIAGNOSIS OF CROHN’S DISEASE
Data Management and Definitions
All data were obtained from retrospectively scrutinized case records. To achieve completeness, data were collected until 1995, although December 31, 1989, was the endpoint of the study. Data with reference to gender, date of birth, date of onset of symptoms, date of diagnosis, date of follow-up, disease localization at diagnosis, date and type of surgery, date of postoperative recurrence, and history of perianal disease were extracted and transferred to a data file (File Maker Pro, Claris Inc., Santa Clara, CA).
Age at diagnosis was grouped into 15-year intervals, except for patients over 60 years of age at diagnosis, who constituted a single group.
The primary localization of disease, based on the examinations done at the time of diagnosis, was classified into six groups:
- 1. Orojejunal disease (oral to the ligament of Treitz)
- 2. Small bowel disease (inflammation of the small bowel, excluding the distal 30 cm of the terminal ileum)
- 3. Ileocecal disease (inflammation involving the distal 30 cm of the ileum with or without isolated involvement of the cecum)
- 4. Continuous ileocolonic disease (continuous inflammation of the ileum and the colon)
- 5. Discontinuous ileocolonic disease (inflammation in both the small bowel and the colon but without continuous inflammation in the ileocecal region)
- 6. Colorectal disease (inflammation confined to the colon or rectum or both only)
Patients with only perianal Crohn’s disease were excluded from analysis.
Surgery was defined as any operation leading to intestinal resection and thus strictureplasty (employed in less than 5 cases in the cohort), surgery for perianal disease, and other minor surgical procedures were excluded. Only the first resection for CD was accounted for. The indications for surgery were grouped as acute abdominal pain, medical intractability, intestinal obstruction, palpable mass/abscess, internal fistulas, colonic dilatation, or miscellaneous, which included patients in whom the indication for surgery could not be clarified. The event of postoperative recurrence was considered to be the first day the patient presented with bowel symptoms consistent with CD that was subsequently verified objectively by a diagnostic procedure or was actively treated or both. Changes over time were assessed by comparing patients diagnosed during 1955 to 1974 and 1975 to 1989.
Statistical Methods
Age at onset, age at time of resection, time of follow-up, and time to relapse were calculated as medians. Probabilities for surgery and recurrence after surgery were calculated according to the Kaplan-Meier method. 13,14 The influence of concomitant covariates on the cumulative probability rates was examined using the proportional hazard model described by Cox. 15P values and confidence intervals (CI) were calculated at the 95% confidence level.
RESULTS
In all, 1,936 patients (1,026 women, 910 men) were diagnosed with CD in Stockholm County between 1955 and 1989. Follow-up was complete in 99.2% (1,921) of the patients with a median duration of 14.9 years (range 0–39.7 years). Seventy-three percent (n = 1,415) of the patients had a definite and 27% (n = 521) a possible diagnosis of CD. The localization of disease at diagnosis could be established in all but three patients. Sufficient or reliable information on perianal disease was not available in 75 patients.
First Intestinal Resection
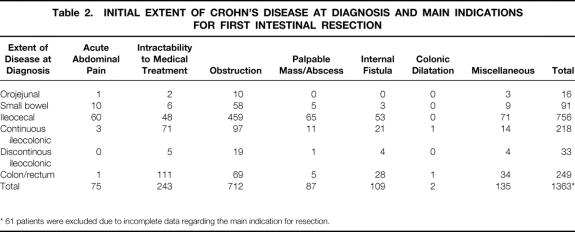
In the total cohort of CD patients, 73.6% (n = 1,424) required at least one intestinal resection. The median age at the time of surgery was 32 years (range 9–85 years). Table 2 shows the indications for surgery in relation to the extent of disease at diagnosis.
Table 2. INITIAL EXTENT OF CROHN’S DISEASE AT DIAGNOSIS AND MAIN INDICATIONS FOR FIRST INTESTINAL RESECTION
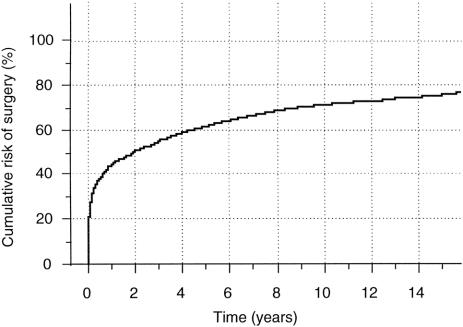
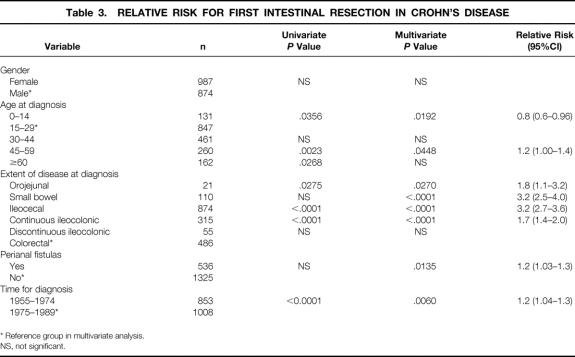
The absolute cumulative frequency of surgery was 44% (95% CI, 42%–47%), 61% (95% CI, 59%–63%) and 71% (95% CI, 69%–73%) 1, 5, and 10 years after diagnosis (Fig. 1). The impact of possible risk factors that may have influenced the frequency of surgery and the numbers is shown in uni- and multivariate analyses in Table 3. Age, disease localization at diagnosis, and perianal fistulas were independent risk factors for surgery. Disease localization at diagnosis had the strongest impact on the probability of surgery. Hence patients with small bowel or solely ileocecal disease had a relative risk of 3.2 (95% CI, 2.5–4.0 and 2.7–3.6) for undergoing surgery compared to the patients with colorectal disease. Moreover, an increased risk was found in patients with orojejunal or continuous ileocolonic disease, the relative risk being 1.8 (95% CI, 1.1–3.2) and 1.7 (95% CI, 1.4–2.0) respectively. Children (< 15 years at diagnosis) had the lowest probability of surgery with a relative risk of 0.8 (95% CI, 0.6–0.96), while the highest probability of surgery was noted in patients aged 45–59 years at diagnosis, who had a relative risk of 1.1 (95% CI, 1.0–1.4) compared to those aged 15 to 29 years at diagnosis. The relative probability of surgery for patients with perianal fistulas (perianal disease) was 1.2 (95% CI, 1.0–1.3), compared to patients without perianal fistulas. Patients diagnosed between 1955 and 1974 had a 1.2 higher relative risk of surgery (95% CI; 1.0–1.3) compared with the patients diagnosed between 1975 and 1989. There was no difference found between the sexes.
Figure 1. Absolute cumulative risk for first intestinal resection in patients with Crohn’s disease, Stockholm County, Sweden, 1955–1989.
Table 3. RELATIVE RISK FOR FIRST INTESTINAL RESECTION IN CROHN’S DISEASE
Furthermore, in an assessment that included only patients with “definite” CD (n = 1,415), a significantly increased risk for primary resection was found in all groups aged over 30 years. Patients aged 30 to 44 years or 45 to 59 years at diagnosis had a relative risk of 1.2 (95% CI, 1.1–1.4 and 1.04–1.5) for resection. Patients aged 60 or more had a relative risk of 1.5 (95% CI, 1.2–1.9). All other variables related to risk for resection remained unchanged, excluding cases with “probable CD.”
Recurrence
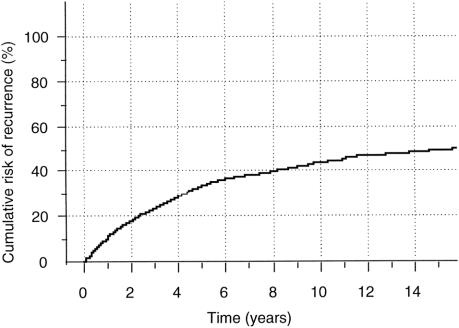
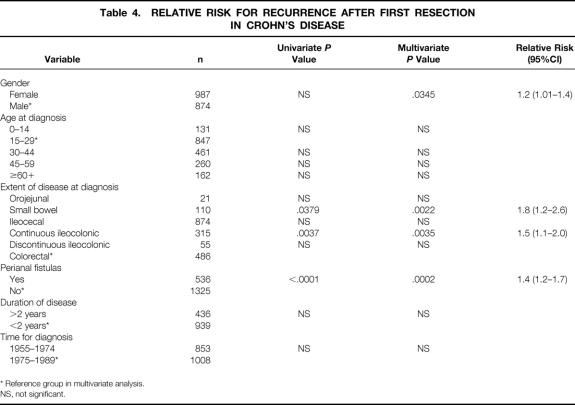
Of the patients who had undergone an intestinal resection, 48% (682/1,424) relapsed subsequently. The cumulative relapse rates were 33% (95% CI, 30%–35%) and 44% (95% CI, 41%–46%), at 5 and 10 years after the first intestinal resection (Fig. 2). Uni- and multivariate analyses of independent risk factors and the numbers for each variable are shown in Table 4. Women had a significantly increased risk of recurrence compared to men, with a relative risk of 1.2 (95% CI, 1.0–1.4). Disease confined to the small bowel or continuous ileocolonic disease increased the relative risk of relapse to 1.8 (95% CI, 1.2–1.6) and 1.5 (95% CI, 1.1–2.0) respectively, compared to colorectal disease. An increased relative risk of 1.4 (95% CI, 1.2–1.7) was also found in patients with perianal fistulas, compared to patients without fistulas. No impact of age at diagnosis or the preoperative duration of disease was found. There was no difference in the recurrence rate between the two periods of time, 1955 to 1974 and 1975 to 1989.
Figure 2. Absolute cumulative risk of recurrence after first intestinal resection in patients diagnosed with Crohn’s disease, Stockholm County, Sweden, 1955–1989.
Table 4. RELATIVE RISK FOR RECURRENCE AFTER FIRST RESECTION IN CROHN’S DISEASE
Moreover, recurrence rates remained unchanged when variables were reevaluated including only patients with “definite” CD (n = 1,415).
DISCUSSION
Risk of Surgery
Retrospective evaluations of the risk of surgery and the risk of recurrence after surgery in Crohn’s disease have been made frequently, 16 but problems pertaining to referrals, insufficient numbers of patients, and a too-short follow-up period contribute to the lack of a consensus so far. 16 The present study, however, is based on a large assembled cohort of patients with CD in a geographically well-defined area over a long period of time; it has a high follow-up rate (99.2%), and possible risk factors for resection and recurrence have been assessed by multivariate analysis.
It is remarkable that the 74% crude rate of at least one intestinal resection found in the present study was identical to figures reported from the Cleveland Clinic in 1985 (74%). 3 Similar results were reported by Truelove et al in 1976, 17 although their definition of surgery also included some patients who had undergone split ileostomy without resection. The lower surgery rate found by Michelassi et al 5 may have been biased by the exclusion of patients previously operated on elsewhere. Furthermore, the length of the follow-up period was not stated.
The majority of patients had been operated on within the first year after diagnosis (44%), indicating a high morbidity during the initial phase of CD. The cumulative probability of surgery leveled off over time, but the rate of 71% at 10 years after diagnosis further stresses the fact that three of four patients with CD require at least one intestinal resection during their lifetime. Moreover, when including only patients with “definite” CD, a further increased risk for primary resection was found in elderly patients, confirming the high risk for resection.
The anatomic site of the disease has been considered to be a determinant of its clinical course. An increased risk of surgery was found in ileal and ileocolic CD in a study by Basilisco et al. 4 Farmer et al 3 demonstrated an increased probability of undergoing surgery for patients with ileocolonic disease, compared to patients with disease confined to other anatomic sites. The lowest probability of surgery found for patients with colorectal disease in the present study is in accord with Farmer’s results. Our findings, however, showed that patients with small bowel disease or disease in the ileocecal region only were more prone to surgery than patients with ileocolonic disease. We were able to show that the occurrence of perianal fistulas was an independent risk factor for surgery by means of a multivariate analysis. Because colorectal disease is strongly associated with perianal fistulas and perianal disease, the high probability of surgery among patients with ileocolonic disease found at the Cleveland Clinic may have been biased by this confounding factor. The differences in the probability of surgery may also have been attributed to differences in the classification of disease in the ileocecal area. The threefold increased risk of surgery for patients with small bowel or ileocecal disease, compared to patients with colorectal disease, may be due to a dissimilar disease pattern (i.e., stenotic vs. inflammatory) as has been proposed elsewhere. 18,19 In our study, 64% (58/91) of the patients with small bowel involvement and 61% (459/756) of those with ileocecal involvement were resected because of mainly obstructive symptoms, whereas this was the case in only 28% (69/249) of the patients with colorectal disease (Table 2).
The increased risk of resection found in patients with perianal fistulas may be due to the poorly documented assumption that removal of a diseased bowel segment decreases the symptoms originating from the fistulas.
Young age at diagnosis has previously been found to be associated with ileal disease and an increased frequency of surgery. 19 Our contradictory results may be explained by the upper limit of 15 years at diagnosis for the youngest age-specific group. The decreased probability of surgery in children can be explained by greater reluctance to resection for this age group, which was also the conclusion drawn in a study from the Children’s Hospital in Stockholm in 1986. 20 Conversely, there are reasons to believe that elderly patients may have been operated on more frequently than young patients partly due to difficulties in distinguishing between CD and malignancy. This assumption was confirmed by both the univariate and multivariate analyses in those aged 45 to 59 years at diagnosis. Too small a number of patients in the >60 years group in the multivariate analysis may have obscured the significantly increased risk found in the univariate analysis.
The long follow-up period enabled an assessment of the risk of surgery over time. Patients diagnosed between 1955 and 1974 were significantly more often subjected to surgery than those diagnosed during the later study period. Thus, time trends have influenced the mode of surgical treatment for Crohn’s disease 21,22 and, in conformity with the apparent risk of recurrence and concomitant introduction of new pharmacologic compounds, 23–25 the mode of surgery may have swung toward a less active approach.
Risk of Recurrence
The postoperative recurrence rate, defined as the risk of a second resection, was 25% to 45% at 10 years from the first resection in two recent studies, 9,26 although postoperative clinical recurrence occurs earlier during the disease course. 27,28 Previous studies have shown that the majority of patients with CD develop an endoscopic recurrence within 3 years after the operation. 29–31 The figures from the present study, in fair agreement with the earlier studies, show that nearly half of all CD patients will have a clinical relapse, and the figures remain unchanged when excluding patients with “probable” CD. However, a relapse-free course during 10 years after surgery seems to imply a high probability of remaining in remission.
The findings of previous studies focusing on possible risk factors for recurrent CD 5,6,8,9 have been inconsistent and the disparate results may be attributable to different study designs, definitions, referrals, and too-small numbers of patients included.
Most studies have indicated that gender does not have any impact on the recurrence rate of CD, 32,33 although a few studies have shown an increased recurrence rate for women, 27,34 and one early study reported an increased recurrence risk for men. 35 In the present study, women had a significantly increased risk of recurrence compared to men. In addition to inheritance, 36 smoking is the most widely recognized risk factor for the initiation and recurrence of CD, 10 although this was not evaluated in the present study. Men have gradually tended to smoke less since the 1960s, but women have tended to smoke more during the same period, 37–39 even though the prevalence of cigarette smoking has generally decreased in Sweden since 1977. Smoking, alone or in combination with the use of oral contraceptives, may therefore have contributed to the increased relapse rate in women. 40
The extent of disease at diagnosis had an impact on recurrence, and increased rates were found in small bowel and continuous ileocolonic CD, in contrast to patients with ileocecal and colorectal disease. Theoretically, ileocecal disease may therefore constitute a subgroup of CD that frequently requires surgery but more rarely exhibits clinical signs of recurrent disease. In this study, the recurrence in relation to the indication for surgery and the type of operation performed was not assessed, because these two variables strongly relate to the initial extent of the inflammatory process.
Another possible subgroup of CD patients may be those with perianal disease. The increased probability of intestinal resection as well as postoperative relapse found for these patients may reflect a subcategory of patients with CD running a more severe disease course.
In previous evaluations, young age at resection increased recurrence rates in some studies, 28,41 but the common finding elsewhere was no impact. 33,42,43 The latter was confirmed in our new analysis, as age at diagnosis was not found to have any impact.
We could not demonstrate any relationship between the preoperative duration of disease and the recurrence rate of CD in the present study, in contrast to a few previous studies. 27,33,44 The date of diagnosis and also the time for the onset of the first CD symptoms are only approximations of the exact times. The true preoperative duration of disease is therefore difficult to establish and thus the value of this risk factor be an issue.
The recurrence rate remained stable over time in spite of the introduction of new pharmacologic compounds. However, azathioprine and its metabolite, 6-mercaptopurine, the most promising drugs for maintaining remission, 45 were not in relatively wide use for CD in Sweden before the late 1980s.
In conclusion, this incidence-based study shows that three of four patients with CD will ultimately require intestinal resection, and half of these patients will relapse clinically. Crohn’s disease involving any part of the small bowel and the presence of perianal fistulas increases the risk of clinical relapse, while solely ileocecal and colorectal disease are associated with a more favorable disease course. A relapse-free course during the 10 years following the first resection implies remission maintenance.
Footnotes
Correspondence: Olle Bernell, MD, Dept. of Surgery, Gastrocentrum K 53, Huddinge University Hospital, S-141 86 Huddinge, Sweden.
Supported by a grant from the Karolinska Institute, Stockholm, Sweden.
Accepted for publication July 30, 1999.
References
- 1.Munkholm P, Langholz E, Davidsen M. Disease activity courses in a regional cohort of Crohn’s disease patients. Scand J Gastroenterol 1995; 30:699–706. [DOI] [PubMed] [Google Scholar]
- 2.Greenstein AJ, Lachman P, Sachar DB, et al. Perforating and non-perforating indications for repeated operations in Crohn’s disease: evidence for two clinical forms. Gut 1988; 29:588–592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Farmer R, Whelan G. Long-term follow-up of patients with Crohn’s disease. Gastroenterology 1985; 88:1818–1825. [DOI] [PubMed] [Google Scholar]
- 4.Basilisco G, Campanini M. Risk factors for first operation in Crohn’s disease. Am J Gastroenterol 1989; 84:749–752. [PubMed] [Google Scholar]
- 5.Michelassi F, Balestracci T, Chappel R, Block G. Primary and recurrent Crohn’s disease: experience with 1379 patients over 18 years. Ann Surg 1991; 214:230–238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Borely N, Mortensen N, Jewell D. Preventing postoperative recurrence of Crohn’s disease. Br J Surg 1997; 84:1493–1502. [PubMed] [Google Scholar]
- 7.Strong S. Prognostic parameters of Crohn’s disease recurrence. Ballieres Clin Gastroenterol 1998; 12:167–177. [DOI] [PubMed] [Google Scholar]
- 8.Caprilli R, Corrao G, Taddei G, et al. Prognostic factors for postoperative recurrence of Crohn’s disease. Dis Colon Rectum 1996; 39:335–341. [DOI] [PubMed] [Google Scholar]
- 9.Heimann T, Greenstein A, Lewis B, et al. Comparison of primary and reoperative surgery in patients with Crohn’s disease. Ann Surg 1998; 227:492–495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cottone M, Rosselli M, Orlando A. Smoking habits and recurrence in Crohn’s disease. Gastroenterology 1994; 106:643–648. [DOI] [PubMed] [Google Scholar]
- 11.Lapidus A, Bernell O, Hellers G, et al. Epidemiology of Crohn’s disease in Stockholm County 1995–89. Gut 1997; 41:480–486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lennard-Jones J. Definition and diagnosis of Crohn’s disease. Scandia International Symposia: Regional Enteritis, 1971.
- 13.Armitage P, Berry G. Statistical methods in medical research. 3rd ed. Oxford: Blackwell Scientific; 1994: 469–492.
- 14.Mantel N. Evaluation of survival data and two new rank order statistics arising in its consideration. Cancer Chemother Rep 1966; 50:163–170. [PubMed] [Google Scholar]
- 15.Cox D. Regression models and life-tables. J R Stat Soc 1972; 34:187–220. [Google Scholar]
- 16.Williams J, Wong W, Rothenberger D, Goldberg S. Recurrence of Crohn’s disease after resection. Br J Surg 1991; 78:10–19. [DOI] [PubMed] [Google Scholar]
- 17.Truelove S, Pena A. Course and prognosis in Crohn’s disease. Gut 1976; 17:192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sachar D, Andrews H, Farmer R. Proposed classification of of patient subgroups in Crohn’s disease. Gastroenterology Int 1992; 5:141–154. [Google Scholar]
- 19.Polito J, Childs B, Mellits E, et al. Crohn’s disease: influence of age at diagnosis on site and clinical type of disease. Gastroenterology 1996; 111:580–586. [DOI] [PubMed] [Google Scholar]
- 20.Lindham S, Bergdahl S. Kirurgisk behandling av inflammatorisk tarmsjukdom hos barn. Läkartidningen 1986; 83:3682–3684. [PubMed] [Google Scholar]
- 21.Alexander-Williams J. Small bowel Crohn’s disease. In: Allan R, Keighley M, Alexander-Williams J, Hawkins C, eds. Inflammatory bowel diseases. 2nd ed. Edinburgh: Churchill Livingstone; 1990: 459–472.
- 22.Winslet M, Keighley M. Surgery for Crohn’s disease of the colon. In: Allan R, Keighley M, Alexander-Williams J, Hawkins C, eds. Inflammatory bowel diseases. 2nd ed. Edinburgh: Churchill Livingstone; 1990: 473–482.
- 23.Azad-Kahn A, Piris J, Truelove S. An experiment to determine the active therapeutic moiety of sulfalazine. Lancet 1977; 2:892–895. [DOI] [PubMed] [Google Scholar]
- 24.Ursing B, Kamme C. Metronidazole for Crohn’s disease. Lancet 1975; 1:775–777. [DOI] [PubMed] [Google Scholar]
- 25.Present D, Korelitz B, Wisch N. Treatment of Crohn’s disease with 6-mercaptopurine: a long-term randomized double blind study. N Engl J Med 1980; 302:981–987. [DOI] [PubMed] [Google Scholar]
- 26.Wettergren A, Christiansson J. Risk of recurrence and reoperation after resection for ileocolic Crohn’s disease. Scand J Gastroenterol 1991; 26:1319–1322. [DOI] [PubMed] [Google Scholar]
- 27.Lennard Jones J, Stalder D. Prognosis after resection of chronic regional ileitis. Gut 1971; 8:332–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hellers G. Crohn’s disease in Stockholm county 1955–74. Acta Chir Scand 1979; 490(suppl):5–81. [PubMed] [Google Scholar]
- 29.Rutgeerts P, Geboes K. Predictability of the postoperative course of Crohn’s disease. Gastroenterology 1990; 99:956–963. [DOI] [PubMed] [Google Scholar]
- 30.Olaison G, Smedh K, Sjödahl R. Natural course of Crohn’s disease after ileocolic resection: endoscopically visualised ileal ulcers preceding symptoms. Gut 1992; 33:331–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McLeod R, Wolff B, Steinhart A. Risk and significance of endoscopic/radiological evidence of recurrent Crohn’s disease. Gastroenterology 1997; 113:1823–1827. [DOI] [PubMed] [Google Scholar]
- 32.Trnka Y, Glotzer D, Kasdon E. Long-term outcome of restorative operation in Crohn’s disease. Ann Surg 1982; 196:345–355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chardavoyne R, Flint G, Pollack S, Wise L. Factors affecting recurrence following resection for Crohn’s disease. Dis Colon Rectum 1986; 29:495–502. [DOI] [PubMed] [Google Scholar]
- 34.Kyle J. Prognosis after ileal resection for Crohn’s disease. Br J Surg 1971; 58:735–737. [DOI] [PubMed] [Google Scholar]
- 35.Atwell J, Duthie H, Goligher J. The outcome of Crohn’s disease. Br J Surg 1965; 52:966–972. [DOI] [PubMed] [Google Scholar]
- 36.Peeters M, Nevens H, Baert F. Familial aggregation in Crohn’s disease: increased age-adjusted risk and concordance in clinical characteristics. Gastroenterology 1996; 111:597–603. [DOI] [PubMed] [Google Scholar]
- 37.Benoni C. Basic research, clinical implications and trends in therapy. Lancaster: Kluwer Academic Publishers; 1994: 319–327.
- 38.Tobacco habits in Sweden. Stockholm: Statistics Sweden; 1986.
- 39.ULF (Examination of life-styles). Stockholm: Statistics Sweden; 1990.
- 40.Sutherland L, Ramcharan S, Bryant H, Fick G. Effects of cigarette smoking on recurrence of Crohn’s disease. Gastroenterology 1990; 98:1123–1128. [DOI] [PubMed] [Google Scholar]
- 41.Fricker M, Segall M. The resectional reoperation rate for Crohn’s disease in general community hospital. Dis Colon Rectum 1983; 26:305–309. [DOI] [PubMed] [Google Scholar]
- 42.Lock M, Farmer R, Fazio V. Recurrence and reoperation for Crohn’s disease: the role of disease location in prognosis. N Engl J Med 1981; 304:1586–1588. [DOI] [PubMed] [Google Scholar]
- 43.Fasth S, Hellberg R, Hulten L, Ahren C. Site of recurrence, extent of ileal disease and magnitude of resection in primary and recurrent Crohn’s disease. Acta Chir Scand 1981; 147:569–576. [PubMed] [Google Scholar]
- 44.Speranza V, Simi M, Leardi S, Del Papa M. Recurrence of Crohn’s disease: are there any risk factors? J Clin Gastroenterol 1986; 8:640–646. [DOI] [PubMed] [Google Scholar]
- 45.O’Donoghue D, Dawson A, Powell-Tuck J. Double-blind withdrawal trial of azathioprine as maintenance treatment for Crohn’s disease. Lancet 1978; 2:955–957. [DOI] [PubMed] [Google Scholar]