Fracture Prevalence among Human Immunodeficiency Virus (HIV)-Infected Versus Non-HIV-Infected Patients in a Large U.S. Healthcare System (original) (raw)
Abstract
Context: Reduced bone mineral density has been demonstrated among HIV-infected patients, but fracture prevalence is unknown.
Objective: The objective of the study was to compare fracture prevalence in HIV-infected and non-HIV-infected patients.
Design: This was a population-based study.
Setting: The study was conducted at a large U.S. health care system.
Patients: A total of 8525 HIV-infected and 2,208,792 non-HIV-infected patients with at least one inpatient or outpatient encounter between October 1, 1996, and March 21, 2008, was compared.
Main Outcome Measure: Fracture prevalence using specific International Classification of Diseases, Ninth Revision, Clinical Modification fracture codes was measured.
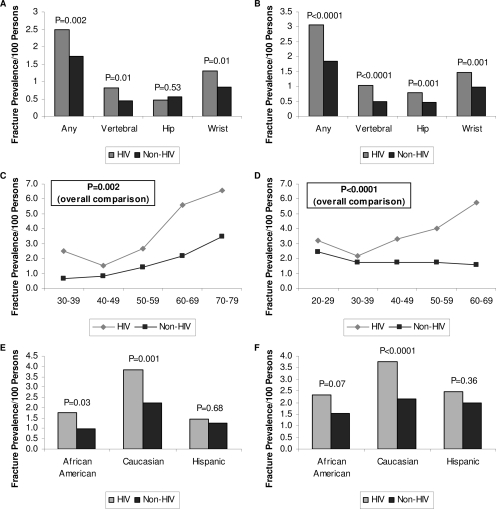
Results: The overall fracture prevalence was 2.87 vs. 1.77 patients with fractures per 100 persons in HIV-infected, compared with non-HIV-infected patients (P < 0.0001). Among females, the overall fracture prevalence was 2.49 vs. 1.72 per 100 persons in HIV-infected vs. non-HIV-infected patients (P = 0.002). HIV-infected females had a higher prevalence of vertebral (0.81 vs. 0.45; P = 0.01) and wrist (1.31 vs. 0.83; P = 0.01) fractures per 100 persons, compared with non-HIV-infected females but had a similar prevalence of hip fractures (0.47 vs. 0.56; P = 0.53). Among males, the fracture prevalence per 100 persons was higher in HIV-infected vs. non-HIV-infected patients for any fracture (3.08 vs. 1.83; P < 0.0001), vertebral fractures (1.03 vs. 0.49; P < 0.0001), hip fractures (0.79 vs. 0.45; P = 0.001), and wrist fractures (1.46 vs. 0.99; P = 0.001). Fracture prevalence was higher relative to non-HIV-infected patients among African-American and Caucasian females and Caucasian males.
Conclusions: Fracture prevalence is increased in HIV-infected compared with non-HIV-infected patients.
The database review of a large U.S. healthcare system demonstrates that fracture prevalence is increased among HIV-infected vs. non HIV-infected males and females. These data also suggest that fracture prevalence may increase more with age among the HIV-infected group.
An increased prevalence of osteoporosis and osteopenia has been reported in both men and women infected with HIV, but the mechanism and consequences of these changes are unknown. Numerous studies have evaluated bone density among patients with HIV infection (1,2,3,4,5,6,7) and have found the prevalence of osteoporosis and osteopenia to be elevated in HIV-infected compared with control groups (8,9,10,11,12,13,14). A metaanalysis of studies comparing bone mineral density in HIV-infected with non-HIV-infected patients demonstrated a pooled odds ratio of 3.7 for osteoporosis (15).
Although the increased prevalence of osteoporosis and osteopenia among HIV-infected patients has raised concern for increased fracture risk, few investigations have evaluated fracture rates among HIV-infected patients, and studies are largely limited to the case report level (16). Two smaller studies compared fracture rates in HIV vs. non-HIV-infected patients (17,18) by patient interview.
To our knowledge, fracture prevalence in HIV-infected patients has not been compared with that of control patients within a large health care system, using specific coded diagnoses for outcome ascertainment assessing fracture site and demographic subgroups.
Patients and Methods
Data source and patient sample
Data were obtained from the Research Patient Data Registry (RPDR), a clinical care data registry capturing all data from the Partners HealthCare System, which includes two primary hospitals, Brigham and Women’s Hospital (BWH) and Massachusetts General Hospital (MGH). Complex queries can be created and submitted to the RPDR, and a set of patients matching the search criteria is returned as an aggregate deidentified summary number that is within three patients of the actual value for security purposes. We queried the RPDR for all patients with at least one encounter at BWH or MGH between October 1, 1996, and March 21, 2008, conducting separate searches for patients with and without HIV infection. Inpatient and outpatient encounters were included. Within the HIV-stratified groups, we identified patients with vertebral, hip, or wrist fracture, or any of the three sites of fracture, at any time during the study period. Patients with multiple fractures were counted only once. All searches were stratified by gender and further stratified by age group and race using RPDR search functions.
Exposure and outcome ascertainment
HIV infection was identified using International Classification of Diseases (ICD), Ninth Revision, Clinical Modification codes of either 042 (human immunodeficiency virus disease) or V08 (asymptomatic HIV infection status) recorded at any time. Patients with no code of 042 or V08 were presumed to be HIV negative. Fracture outcomes were determined using ICD-9-CM codes selected on the basis of the likelihood of their being related to osteoporosis (19). Vertebral fractures were identified using codes 805.2 [closed fracture of dorsal (thoracic) vertebra], 805.3 [open fracture of dorsal (thoracic) vertebra], 805.4 (closed fracture of lumbar vertebra), 805.5 (open fracture of lumbar vertebra), 805.6 (closed fracture of sacrum and coccyx), and 805.7 (open fracture of sacrum and coccyx). Hip fractures were identified using codes 820.0 (transcervical fracture, closed), 820.1 (transcervical fracture, open), 820.2 (pertrochanteric fracture of femur, closed), 820.3 (pertrochanteric fracture of femur, open), 820.8 (fracture of unspecified part of neck of femur, closed), and 820.9 (fracture of unspecified part of neck of femur, open). Wrist fractures were identified using codes 814.0 (closed fractures of carpal bones), 814.1 (open fractures of carpal bones), 813.4 (fracture of lower end of radius and ulna, closed), and 813.5 (fracture of lower end of radius and ulna, open). A chart review validation of ICD-based fracture ascertainment was performed by a trained clinical research nurse on a subset of charts. The sensitivity was 100% for both hip and vertebral fractures, and the specificity was 84% for hip fractures and 79% for vertebral fractures.
Data analysis
This population-based study used database query to identify patient groups for comparison of fracture prevalence according to HIV status and gender, age, race, and site of fracture. Period prevalence between October 1, 1996, and March 21, 2008, was calculated as the number of patients with fractures per 100 persons during the given time period for each subgroup. Searches returned the number of unique patients who met search criteria. χ2 analysis was used to calculate P values for dichotomous variables. Demographic differences between the background HIV-infected and non-HIV-infected populations were accounted for by a series of stratified analyses comparing prevalences. Statistical analysis was conducted using JMP statistical software version 5.0.1 (1989–2003, SAS Institute, Cary, NC). The study was approved by the Partners Human Research Committee. P < 0.05 was considered to indicate statistical significance.
Results
The background population who presented for care at either BWH or MGH during the study period was comprised of 8525 HIV-infected and 2,208,792 non-HIV-infected patients. The demographic characteristics of these groups stratified by gender are shown in Table 1. A greater proportion of HIV-infected patients were male compared with the non-HIV-infected patients. Within both female and male groups, there were higher proportions of HIV-infected patients in the 30–39, 40–49, and 50–59 yr age groups, compared with non-HIV-infected patients. In gender-stratified comparisons, the HIV-infected group also had higher proportions of African-American and Hispanic and lower proportions of Caucasian patients compared with the non-HIV-infected group.
Table 1.
Demographics according to HIV status
| HIV infected (n = 8525) | Non-HIV infected (n = 2,208,792) | |||
|---|---|---|---|---|
| n | Percentage | n | Percentage | |
| Female | 2971 | 34.9 | 1,233,549 | 55.8 |
| Age (yr) | ||||
| 30–39 | 754 | 25.4 | 222,657 | 18.1 |
| 40–49 | 998 | 33.6 | 212,509 | 17.2 |
| 50–59 | 598 | 20.1 | 178,318 | 14.5 |
| 60–69 | 143 | 4.8 | 131,747 | 10.7 |
| 70–79 | 76 | 2.6 | 88,960 | 7.2 |
| Race | ||||
| African-American | 910 | 30.6 | 79,508 | 6.4 |
| Caucasian | 1168 | 39.3 | 772,040 | 62.6 |
| Hispanic | 555 | 18.7 | 86,953 | 7.0 |
| Male (yr) | 5555 | 65.2 | 975,158 | 44.1 |
| Age | ||||
| 20–29 | 217 | 3.9 | 103,537 | 10.6 |
| 30–39 | 959 | 17.3 | 144,189 | 14.8 |
| 40–49 | 2128 | 38.3 | 152,070 | 15.6 |
| 50–59 | 1564 | 28.2 | 135,118 | 13.9 |
| 60–69 | 451 | 8.1 | 112,526 | 11.5 |
| Race | ||||
| African-American | 994 | 17.9 | 59,251 | 6.1 |
| Caucasian | 3062 | 55.1 | 626,721 | 64.3 |
| Hispanic | 856 | 15.4 | 79,076 | 8.1 |
Table 2 summarizes fracture prevalence comparing HIV-infected with non-HIV-infected patients. Overall fracture prevalence (including any of the three sites: vertebral, hip, or wrist) was 2.87 patients with fractures per 100 persons [95% confidence interval (CI) 2.52–3.23] in the HIV-infected group, compared with 1.77 (95% CI 1.75–1.79; P < 0.0001) in the non-HIV-infected group. All data shown represent number of unique patients with the specified type of fracture. Similar significant differences between HIV and non-HIV-infected patients were seen for vertebral [1.01 (0.80–1.22) vs. 0.47 (0.46–0.48); P < 0.0001], hip [0.72 (0.54–0.89) vs. 0.51 (0.50–0.52); P = 0.01], and wrist [1.38 (1.14–1.63) vs. 0.90 (0.89–0.91); P < 0.0001] fractures. Overall fracture prevalence (HIV vs. non-HIV-infected) was 2.49 per 100 persons (95% CI 1.93–3.05) vs. 1.72 (95% CI 1.69–1.74; P = 0.002) for women and 3.08 (95% CI 2.62–3.53) vs. 1.83 (95% CI 1.81–1.86; P < 0.0001) for men.
Table 2.
Fracture prevalence according to HIV status
| HIV infected | Non-HIV infected | |||
|---|---|---|---|---|
| n | Prevalence (95% CI) | n | Prevalence (95% CI) | |
| Total | 245 | 2.87 (2.52–3.23) | 39,073 | 1.77 (1.75–1.79) |
| Vertebral | 86 | 1.01 (0.80–1.22) | 10,300 | 0.47 (0.46–0.48) |
| Hip | 61 | 0.72 (0.54–0.89) | 11,222 | 0.51 (0.50–0.52) |
| Wrist | 118 | 1.38 (1.14–1.63) | 19,889 | 0.90 (0.89–0.91) |
| Female | 74 | 2.49 (1.93–3.05) | 21,185 | 1.72 (1.69–1.74) |
| Site | ||||
| Vertebral | 24 | 0.81 (0.49–1.13) | 5502 | 0.45 (0.43–0.46) |
| Hip | 14 | 0.47 (0.22–0.72) | 6854 | 0.56 (0.54–0.57) |
| Wrist | 39 | 1.31 (0.90–1.72) | 10,277 | 0.83 (0.82–0.85) |
| Age (yr) | ||||
| 30–39 | 19 | 2.52 (1.40–3.64) | 1396 | 0.63 (0.59–0.66) |
| 40–49 | 15 | 1.50 (0.75–2.26) | 1708 | 0.80 (0.77–0.84) |
| 50–59 | 16 | 2.68 (1.38–3.97) | 2519 | 1.41 (1.36–1.47) |
| 60–69 | 8 | 5.59 (1.83–9.36) | 2826 | 2.15 (2.07–2.22) |
| 70–79 | 5 | 6.58 (1.01–12.15) | 3085 | 3.47 (3.35–3.59) |
| Race | ||||
| African-American | 16 | 1.76 (0.90–2.61) | 773 | 0.97 (0.90–1.04) |
| Caucasian | 45 | 3.85 (2.75–4.96) | 17,308 | 2.24 (2.21–2.27) |
| Hispanic | 8 | 1.44 (0.45–2.43) | 1081 | 1.24 (1.17–1.32) |
| Male | 171 | 3.08 (2.62–3.53) | 17,887 | 1.83 (1.81–1.86) |
| Site | ||||
| Vertebral | 57 | 1.03 (0.76–1.29) | 4799 | 0.49 (0.48–0.51) |
| Hip | 44 | 0.79 (0.56–1.03) | 4368 | 0.45 (0.43–0.46) |
| Wrist | 81 | 1.46 (1.14–1.77) | 9611 | 0.99 (0.97–1.01) |
| Age (yr) | ||||
| 20–29 | 7 | 3.23 (0.87–5.58) | 2535 | 2.45 (2.35–2.54) |
| 30–39 | 21 | 2.19 (1.26–3.12) | 2477 | 1.72 (1.65–1.78) |
| 40–49 | 70 | 3.29 (2.53–4.05) | 2617 | 1.72 (1.66–1.79) |
| 50–59 | 63 | 4.03 (3.05–5.00) | 2323 | 1.72 (1.65–1.79) |
| 60–69 | 26 | 5.76 (3.61–7.92) | 1777 | 1.58 (1.51–1.65) |
| Race | ||||
| African-American | 23 | 2.31 (1.38–3.25) | 915 | 1.54 (1.44–1.64) |
| Caucasian | 115 | 3.76 (3.08–4.43) | 13,505 | 2.15 (2.12–2.19) |
| Hispanic | 21 | 2.45 (1.42–3.49) | 1577 | 1.99 (1.90–2.09) |
Fracture prevalence according to anatomical site is shown in Fig. 1, A and B. In gender-stratified comparisons of HIV-infected vs. non-HIV-infected patients, HIV-infected patients had significantly higher fracture prevalence in all categories, with the exception of hip fractures among women, in which prevalence between HIV-infected and non-HIV-infected patients was similar. Fracture prevalence according to gender and further stratified by age (Fig. 1, C and D) or race (Fig. 1, E and F) was also determined. Fracture prevalence was relatively higher across all age categories in each gender, although confidence intervals (Table 2) were wide for a number of specific age groups. P values for the overall comparison among men and women, including data from all age groups, was highly significant for women (P = 0.002) and men (P < 0.0001). Fracture prevalence was higher for HIV-infected than non-HIV-infected patients for African-American and Caucasian women and Caucasian men.
Figure 1.
Fracture prevalence comparing HIV-infected and non-HIV-infected patients by gender and site of fracture, age group, and race. Panels A, C, and E represent females. Panels B, D, and F represent males. A and B, Comparison of fracture prevalence in HIV-infected vs. non-HIV-infected patients according to gender and site of fracture. C and D, Comparison of fracture prevalence in HIV-infected vs. non-HIV-infected patients according to gender and age group. E and F, Comparison of fracture prevalence in HIV-infected vs. non-HIV-infected patients according to gender and race. Light bars and lines represent HIV-infected patients; dark bars and lines represent non-HIV-infected patients. In C and D, the P values are for the comparison of overall fracture prevalence between HIV-infected and non-HIV-infected patients.
In a secondary analysis stratified by gender, followed by age group and race, HIV-infected patients demonstrated a similar pattern of higher fracture prevalence, compared with non-HIV-infected patients in every group, with the exception of Hispanic men aged 50–59 yr (data not shown). A series of secondary analyses were conducted limiting the study duration to 3-yr periods (1997–1999, 2001–2003, and 2005–2007) to minimize the potential time difference between HIV diagnosis and fracture, and the results were similar to the primary analysis, demonstrating higher fracture prevalence in HIV-infected patients, compared with non-HIV-infected patients (3.91 vs. 2.77 in 1997–1999; 3.61 vs. 2.51 in 2001–2003; and 3.25 vs. 2.09 in 2005–2007, HIV-infected vs. non-HIV-infected). A significant temporal time trend in fractures was not observed comparing fractures by individual study year, from 1996 to 2008, among the HIV-infected patients. We also assessed the proportion of patients in each group with coded outpatient visits, and this proportion was more than 90% in both the HIV-infected and non-HIV-infected groups.
Discussion
Fracture prevalence was higher in HIV-infected patients, compared with non-HIV-infected patients, in this large population-based study drawing from more than 11 yr of data from a large U.S. health care system. HIV-infected patients had a significantly higher prevalence of vertebral, hip, wrist, and combined fractures, compared with non-HIV-infected patients. Within both genders, fracture prevalence was higher in HIV-infected vs. non-HIV-infected patients for the majority of sites assessed, across age categories, and most race categories.
The results of multiple studies have established an increased prevalence of osteoporosis and osteopenia in patients with HIV disease, and reduced bone mineral density (BMD) is likely to translate to an increased risk of fracture. For example, in non-HIV-infected patients, fracture risk is thought to increase approximately 2-fold for each 1 sd reduction in BMD (20). However, very few studies have focused on the outcome of fracture, comparing HIV-infected with non-HIV-infected patients (17,18). Furthermore, the studies comparing fracture rates examined relatively small cohorts of patients and used history-based outcome ascertainment.
We used a large clinical care data registry of more than 2.2 million patients, including more than 8000 HIV-infected patients, to obtain a global estimate of fracture prevalence in HIV-infected patients, compared with a background population receiving care in the same health care system. Using ICD codes for outcome ascertainment avoids the potential for recall bias or inaccurate patient information obtained in history-based outcome ascertainment. Furthermore, we selected specific ICD codes to reduce the likelihood of misclassification. Our results demonstrate modest but significant increases in fracture prevalence, among both men and women, consistent with data demonstrating moderate but significant reductions in bone density in these groups (2,11).
Of note, fracture prevalence appears to increase with age in both HIV-infected men and women. Comparison with a control population is critical in this regard. Fracture rates in the background population of more than 2 million patients increase to a greater extent with age in women, and this increase is shown to occur as anticipated at the time of the perimenopausal transition (21). Among both HIV-infected men and women, age-related increases in fracture rates appear to be greater than in the control population, suggesting that fractures may increase as the HIV-infected population lives longer and ages.
Due to database constraints, we could not investigate antiretroviral medication use, smoking, alcohol use, body mass index, socioeconomic status, or medications affecting bone metabolism such as estrogens or steroids. However, we were able to perform gender-, age-, and race-stratified analyses demonstrating increased fracture rates among Caucasian males and females and African-American females at most age ranges. We could not assess whether fractures were specifically trauma related, but the prevalence of trauma by ICD code was less than 1% for both the HIV-infected and non-HIV-infected groups. Moreover, this was a population-based fracture prevalence study, and individual bone density data were not available, preventing formal multivariable regression analyses. Therefore, our data provide novel information on prevalence but do not permit determination of mechanism, and further studies will be necessary to assess specific causes. In this regard, it will be critical to investigate factors related to the menopausal transition in women and aging in men as well as factors related to use of specific antiretroviral drugs and metabolic abnormalities associated with use of antiretroviral therapies (10,22). Mitochondrial dysfunction has been associated with the use of nucleoside reverse transcriptase inhibitors (23), and it is interesting to speculate that this may contribute to a premature aging in HIV-infected patients which may contribute to reduced BMD and increased fracture rates.
In both HIV-infected and control populations, fracture prevalence was greater for Caucasian patients, consistent with the known differences in bone density in African-American and Caucasian patients (24). Among women, a greater increase was seen for vertebral fractures relative to control than for hip fractures, potentially suggesting factors that affect trabecular bone. However, wrist fractures were also increased relative to controls in women, and all three categories (hip, wrist, and vertebral) were increased for HIV-infected men.
To our knowledge, these data are the first to compare fracture prevalence between HIV-infected and non-HIV-infected patients with a large patient sample using ICD-based outcome ascertainment. The results provide strong evidence that HIV-infected patients have a higher prevalence of fractures than non-HIV-infected patients across both genders and critical fracture sites. Moreover, our data suggest that the relative difference in fracture prevalence between HIV-infected and non-HIV- infected patients increases with age for both genders. As the HIV-infected population ages, reduced BMD and increased fracture risk may become an even greater problem. Whether increased fractures are the sequelae of antiretroviral therapy, increased rates of traditional risk factors such as low weight among HIV-infected patients, or HIV infection, and its accompanying metabolic and inflammatory disturbances, itself remains to be determined. This study suggests the importance of assessing bone density and minimizing factors contributing to increased fracture risk in the HIV-infected population.
Acknowledgments
We thank Shawn Murphy and the Partners HealthCare Research Patient Data Registry group for facilitating use of their database and Jo Ann David-Kasdan for assistance with validation substudies.
Footnotes
This work was supported in part by Grants T32 AI07387 (to V.A.T., Massachusetts General Hospital), K23 AT002862 (to T.T.B., Johns Hopkins Medical Center), and K24 DK064545 (to S.K.G., Massachusetts General Hospital).
The authors have nothing to disclose.
First Published Online July 1, 2008
Abbreviations: BMD, Bone mineral density; BWH, Brigham and Women’s Hospital; CI, confidence interval; ICD, International Classification of Diseases; MGH, Massachusetts General Hospital; RPDR, Research Patient Data Registry.
References
- Tebas P, Powderly WG, Claxton S, Marin D, Tantisiriwat W, Teitelbaum SL, Yarasheski KE 2000 Accelerated bone mineral loss in HIV-infected patients receiving potent antiretroviral therapy. AIDS 14:F63–F67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carr A, Miller J, Eisman JA, Cooper DA 2001 Osteopenia in HIV-infected men: association with asymptomatic lactic acidemia and lower weight pre-antiretroviral therapy. AIDS 15:703–709 [DOI] [PubMed] [Google Scholar]
- Gold J, Pocock N, Li Y 2002 Bone mineral density abnormalities in patients with HIV infection. J Acquir Immune Defic Syndr 30:131–132 [DOI] [PubMed] [Google Scholar]
- Mondy K, Yarasheski K, Powderly WG, Whyte M, Claxton S, DeMarco D, Hoffmann M, Tebas P 2003 Longitudinal evolution of bone mineral density and bone markers in human immunodeficiency virus-infected individuals. Clin Infect Dis 36:482–490 [DOI] [PubMed] [Google Scholar]
- Bongiovanni M, Fausto A, Cicconi P, Menicagli L, Melzi S, Ligabo VE, Cornalba G, Bini T, Sardanelli F, Monforte AD 2005 Osteoporosis in HIV-infected subjects: a combined effect of highly active antiretroviral therapy and HIV itself? J Acquir Immune Defic Syndr 40:503–504 [DOI] [PubMed] [Google Scholar]
- Cazanave C, Dupon M, Lavignolle-Aurillac V, Barthe N, Lawson-Ayayi S, Mehsen N, Mercie P, Morlat P, Thiebaut R, Dabis F 2008 Reduced bone mineral density in HIV-infected patients: prevalence and associated factors. AIDS 22:395–402 [DOI] [PubMed] [Google Scholar]
- Rivas P, Gorgolas M, Garcia-Delgado R, Diaz-Curiel M, Goyenechea A, Fernandez-Guerrero ML 2008 Evolution of bone mineral density in AIDS patients on treatment with zidovudine/lamivudine plus abacavir or lopinavir/ritonavir. HIV Med 9:89–95 [DOI] [PubMed] [Google Scholar]
- Bruera D, Luna N, David DO, Bergoglio LM, Zamudio J 2003 Decreased bone mineral density in HIV-infected patients is independent of antiretroviral therapy. AIDS 17:1917–1923 [DOI] [PubMed] [Google Scholar]
- Amiel C, Ostertag A, Slama L, Baudoin C, N′Guyen T, Lajeunie E, Neit-Ngeilh L, Rozenbaum W, De Vernejoul MC 2004 BMD is reduced in HIV-infected men irrespective of treatment. J Bone Miner Res 19:402–409 [DOI] [PubMed] [Google Scholar]
- Brown TT, Ruppe MD, Kassner R, Kumar P, Kehoe T, Dobs AS, Timpone J 2004 Reduced bone mineral density in human immunodeficiency virus-infected patients and its association with increased central adiposity and postload hyperglycemia. J Clin Endocrinol Metab 89:1200–1206 [DOI] [PubMed] [Google Scholar]
- Dolan SE, Huang JS, Killilea KM, Sullivan MP, Aliabadi N, Grinspoon S 2004 Reduced bone density in HIV-infected women. AIDS 18:475–483 [DOI] [PubMed] [Google Scholar]
- Yin M, Dobkin J, Brudney K, Becker C, Zadel JL, Manandhar M, Addesso V, Shane E 2005 Bone mass and mineral metabolism in HIV+ postmenopausal women. Osteoporos Int 16:1345–1352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dolan SE, Carpenter S, Grinspoon S 2007 Effects of weight, body composition, and testosterone on bone mineral density in HIV-infected women. J Acquir Immune Defic Syndr 45:161–167 [DOI] [PubMed] [Google Scholar]
- Jones S, Restrepo D, Kasowitz A, Korenstein D, Wallenstein S, Schneider A, Keller MJ 2007 Risk factors for decreased bone density and effects of HIV on bone in the elderly. Osteoporos Int 19:913–918 [DOI] [PubMed] [Google Scholar]
- Brown TT, Qaqish RB 2006 Antiretroviral therapy and the prevalence of osteopenia and osteoporosis: a meta-analytic review. AIDS 20:2165–2174 [DOI] [PubMed] [Google Scholar]
- Guaraldi G, Ventura P, Albuzza M, Orlando G, Bedini A, Amorico G, Esposito R 2001 Pathological fractures in AIDS patients with osteopenia and osteoporosis induced by antiretroviral therapy. AIDS 15:137–138 [DOI] [PubMed] [Google Scholar]
- Arnsten JH, Freeman R, Howard AA, Floris-Moore M, Lo Y, Klein RS 2007 Decreased bone mineral density and increased fracture risk in aging men with or at risk for HIV infection. AIDS 21:617–623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prior J, Burdge D, Maan E, Milner R, Hankins C, Klein M, Walmsley S 2007 Fragility fractures and bone mineral density in HIV-positive women: a case-control population-based study. Osteoporos Int 18:1345–1353 [DOI] [PubMed] [Google Scholar]
- Gage BF, Birman-Deych E, Radford MJ, Nilasena DS, Binder EF 2006 Risk of osteoporotic fracture in elderly patients taking warfarin: results from the National Registry of Atrial Fibrillation 2. Arch Intern Med 166:241–246 [DOI] [PubMed] [Google Scholar]
- Cauley JA, Hochberg MC, Lui LY, Palermo L, Ensrud KE, Hillier TA, Nevitt MC, Cummings SR 2007 Long-term risk of incident vertebral fractures. JAMA 298:2761–2767 [DOI] [PubMed] [Google Scholar]
- 2002 Incidence of vertebral fracture in Europe: results from the European Prospective Osteoporosis Study (EPOS). J Bone Miner Res 17:716–724 [DOI] [PubMed] [Google Scholar]
- Huang JS, Rietschel P, Hadigan CM, Rosenthal DI, Grinspoon S 2001 Increased abdominal visceral fat is associated with reduced bone density in HIV-infected men with lipodystrophy. AIDS 15:975–982 [DOI] [PubMed] [Google Scholar]
- Caron M, Auclairt M, Vissian A, Vigouroux C, Capeau J 2008 Contribution of mitochondrial dysfunction and oxidative stress to cellular premature senescence induced by antiretroviral thymidine analogues. Antivir Ther 13:27–38 [PubMed] [Google Scholar]
- Arnsten JH, Freeman R, Howard AA, Floris-Moore M, Santoro N, Schoenbaum EE 2006 HIV infection and bone mineral density in middle-aged women. Clin Infect Dis 42:1014–1020 [DOI] [PubMed] [Google Scholar]