Rift Valley fever vaccines (original) (raw)
. Author manuscript; available in PMC: 2010 Nov 5.
Abstract
Rift Valley fever virus (RVFV), which belongs to the genus Phlebovirus, family Bunyaviridae, is a negative-stranded RNA virus carrying a tripartite RNA genome. RVFV is transmitted by mosquitoes and causes large outbreaks among ruminants and humans in Africa and the Arabian Peninsula. Human patients develop an acute febrile illness, followed by a fatal hemorrhagic fever, encephalitis or ocular diseases, whereas ruminants experience abortions during outbreak. Effective vaccination of both humans and ruminants is the best approach to control Rift Valley fever. This article summarizes the development of inactivated RVFV vaccine, live attenuated vaccine, and other new generation vaccines.
Keywords: Rift Valley fever virus, MP-12, vaccine
1. Introduction
In 1931, Daubney et al. reported an outbreak of enzootic hepatitis in a herd of ewes on a farm in the Rift Valley, Kenya [1]. They also observed a number of abortions in ruminants and the presence of a hyper acute lethal infection, characterized by necrotic hepatitis in lambs, and proposed the name Rift Valley fever (RVF) for the disease [1]. The causative agent of the disease proved to be a virus, now named Rift Valley fever virus (RVFV), which is transmitted by mosquitoes and has caused large outbreaks among ruminants and humans in several countries, including Kenya, South Africa, Senegal, Mauritania, Egypt, Madagascar, Saudi Arabia and Yemen [2, 3]. The disease is characterized as having an incubation period of 2 to 6 days, after which patients have a sudden onset of fever, headache, muscular pain, articular pain, photophobia, and weakness [4, 5]. In most cases, the patients completely recover from the disease after a period of weeks, whereas some patients also develop retinal macular change, which results in defective vision for undefined periods [2, 4, 5]. Furthermore, fewer than 1% of RVF patients develop a complicated form of the illness, characterized by hemorrhagic fever or encephalitis [2].
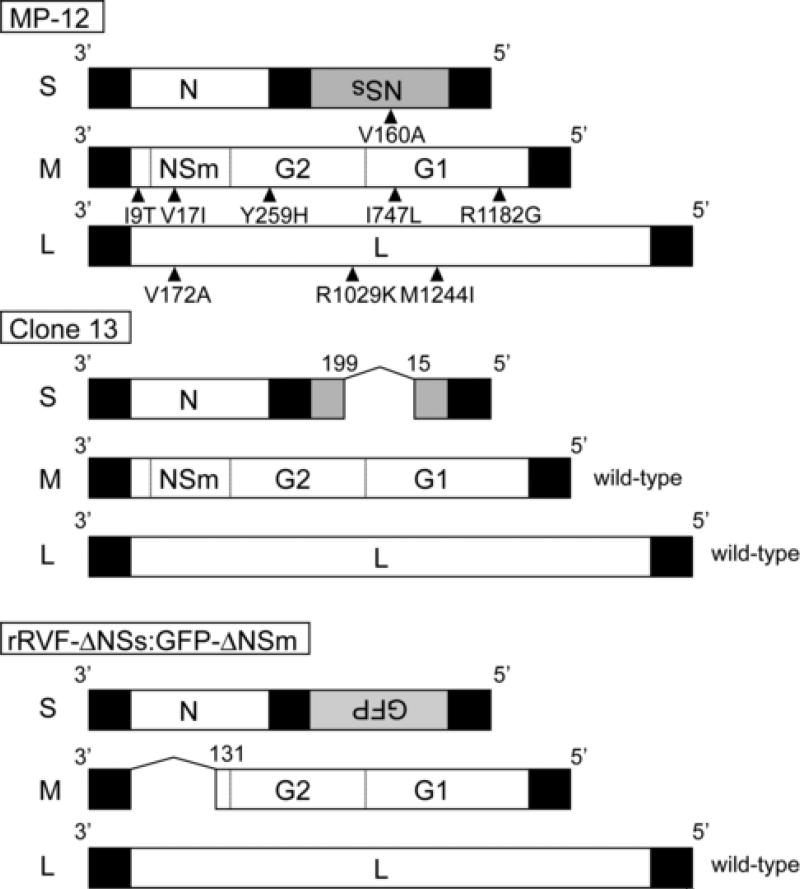
RVFV, belongs to the genus Phlebovirus, family Bunyaviridae and has a tripartite, negative-stranded RNA, consisting of S-, M- and L-segments (Fig.1) [6]. The S-segment (1,690 nt) expresses N protein and NSs protein in an ambi-sense manner. The M-segment (3,885 nt) encodes NSm, 78-kD, G1 (Gc) and G2 (Gn) proteins in a single open reading frame (ORF), and the L-segment (6,404 nt) encodes L protein, a viral RNA-dependent RNA polymerase [6]. Both N and L proteins are required for viral replication and transcription. G1, G2, and 78-kD proteins are incorporated into a viral envelope as glycoproteins, while ribonucleoprotein complex, which are formed by N and viral RNAs, and associated L proteins, are packaged into virions. NSm and NSs are nonstructural proteins [6]. NSs is a major virulence factor of RVFV [7], whereas the contribution of NSm to the virulence of RVFV is less obvious [8].
Figure 1.
Schematic representation of the genetic structure of live attenuated vaccine candidates of RVFV. MP-12 was generated by 12 serial passages of the wild-type ZH548 strain of RVFV in the presence of 5-FU [24]. Amino acid sequence differences between MP-12 and its parental virus ZH548 are shown in the top panel. Clone 13 is a plaque isolate of the wild-type RVFV 74HB59 strain [37]. Clone 13 lacks approximately 70% of the NSs ORF, and expressed truncated NSs is not functional. Although Clone 13 is highly attenuated, the M-and L-segments of clone 13 are the same as those of wild-type RVFV [7, 38]. rRVF-ΔNSs:GFP-ΔNSm was generated by reverse genetics; the NSs ORF was replaced with GFP, and the NSm gene was deleted [40].
In terms of public health, RVF outbreaks outside endemic countries would cause serious health and agricultural problems. Introduction of RVFV into non-endemic countries potentially occurs by the movement of infected travelers, animals and mosquitoes [9]. The intentional spread of RVFV is also a serious concern of national biosecurity. Thus, RVFV is classified as Category A overlap select agent by CDC and USDA [3]. In past, a number of laboratory infections have occurred by the lack of adequate biosafety regulations [4, 5]. Accordingly, the handling of RVFV requires high-containment facilities, including biosafety level (BSL) 4 laboratories or BSL 3 (enhanced) laboratories in the U.S. Although RVFV spread can be prevented by effective vaccination of animals and humans, there are no licensed RVFV vaccines to immunize general citizens in the U.S. or other countries.
A study suggested that humoral immunity is sufficient for protection against RVFV [10]. Furthermore, newborn lamb acquires protective immunity after raising neutralizing antibody by having colostrums of immunized ewes [11]. In contrast, the significance of cell-mediated immunity in protection remains unknown. Another important aspect is that RVFV has relatively small genetic diversities [12]. These past studies provide evidence that the ideal RVFV vaccine for both humans and animals would be one that is safe, elicits rapid humoral immune responses that neutralize known RVFV strains, and induces long-term protective immunity. We summarize the current development of RVFV vaccine candidates and potential problems in this article.
2. Formalin-inactivated RVFV vaccines
Randall et al. reported that immunization of mice with a formalin-inactivated vaccine, which was made from a pantropic Entebbe strain of RVFV, induced higher neutralizing antibody titers than did that made from a neurotropic Smithburn strain [13]. The Entebbe strain of RVFV was initially isolated from mosquitoes in Uganda and had undergone 176 intraperitoneal (i.p.) or intravenous (i.v.) passages in mice. They further showed that the formalin-killed vaccine prepared from chick embryos or chick embryo cell cultures was less immunogenic than that prepared from primary rhesus or African green monkey kidney cells [13, 14]. New formalin-inactivated vaccine, named NDBR 103, was manufactured by using the mouse serum master seed (Entebbe strain, 184th passages) and amplification in primary monkey kidney cells for making the vaccine lot [13]. NDBR 103 was used for immunization of more than 500 human volunteers in 1977 and later [15, 16].
Subsequently, a new lot of formalin-inactivated RVFV vaccine, TSI-GSD 200, was manufactured under rigorous safety regulations by using a new master seed, which was prepared from two passages of the mouse serum master seed of the Entebbe strain in diploid cells (FRhL-2 cells) derived from the lungs of a fetal rhesus monkey [15]. Pittman et al. reported that three subcutaneous injections (s.c.) of TSI-GSD 200 on days 0, 7 and 28 into human volunteers resulted in the development of a neutralizing antibody having a geometric titer of 1: 237 [17]. Further, about 90% of the vaccinees initially responded to the immunization with neutralization antibody titers of 1:40 or more, whereas the remaining 10% were initial non-responders who failed to achieve this titer [17]. A study demonstrated that hamsters that were passively transferred the neutralizing antibodies at a final titer of 1:12 were protected from lethal RVFV challenge [10]. Thus, anti-RVFV neutralizing antibody titers of 1:40 or more was recommended for personnel who would be exposed to wt RVFV [15]. Study by Pittman et al. further suggested that the half life of the 1:40 neutralization titer of initial responders was 287 days [17]. Currently a regular booster administration is deemed necessary for maintaining maximum protection after a series of primary immunization [17, 18].
Immunization side effects of NDBR 103 and TSI-GSD 200 administration to human volunteers were reported to be local reactions, such as erythema, swelling, tenderness or pain at the site of injection, whereas no specific febrile reaction or severe adverse effect related to the vaccination were reported, except for one case of Guillain-Barré syndrome, which might have been due to enterovirus infection [16, 19].
A formalin-inactivated vaccine, derived from a pantropic RVFV strain passaged in baby hamster kidney (BHK) 21 cells, was also used as a veterinary vaccine [20, 21]. The vaccination significantly reduced the abortion of ewes and mortality of newborn lambs during an outbreak and induced immunity in cattle [22].
3. Live attenuated RVFV vaccines
Because inactivated RVFV vaccines require repeated immunizations for inducing and maintaining protective immunity against wild-type RVFV, the development of live attenuated vaccines, which rapidly induce protective immunity without a series of booster administrations, is important.
The Smithburn strain of RVFV, isolated from mosquitoes in Uganda, has been developed as a live attenuated vaccine candidate by serial passages in mouse brains [23]. From 1953 to 58, neuroadapted Smithburn strain was used for vaccination purpose in South Africa, which was passaged 102 times in mouse brains and 50 times in eggs, followed by an additional 16 passages in mouse brain [20, 21]. Since1958, the strain passaged only 102 times in mouse brains had been used for immunization of animals in South Africa, because the latter strain seemed a better immunogen [21]. Smithburn vaccine named modified live virus vaccine (MLVV) was eventually produced in 1971 by amplifying the Smithburn strain-derived viruses, which had undergone the above passages, in BHK cells, and used in African countries including South Africa and Kenya [21]. Although the Smithburn vaccine is significantly attenuated, it has a potential for reversion, and, hence, are not recommended for use in countries where RVFV has not been introduced [20].
Caplen et al attempted to generate a live attenuated vaccine for both human and veterinary use, by performing the serial passage of the ZH548 and ZH501 strains, both wild-type isolates from human patients in Egypt, in the presence of the chemical mutagen, 5-fluorouracil (5FU) [24]. Prior to serial passage in the presence of 5FU, ZH548 had been passaged twice in sucking mice and once in FhRL cells, while ZH501 had been passaged in FhRL cells and undergone plaque cloning in MRC-5 cells in the presence of 5FU. Both strains were independently propagated in the presence of 200 μg/ml of 5FU, and plaques were selected for serial mutagenesis in MRC-5 cells. At 16 serial passages, ZH501 was still virulent to mice, whereas ZH548 had attenuated virulence for mice from passage 5 [24]. The ZH548-derived virus, which was passaged 12 times in the presence of 5FU, has been named MP-12 and selected as a live attenuated vaccine candidate. MP-12 is a temperature-sensitive mutant [25] that carries mutations in all three RNA segments (Fig. 1) [26, 27]. Analysis of reassortant viruses between MP-12 and wt RVFV showed that all three segments contribute to the attenuation phenotype of MP-12 in mice [25], and a recent study further revealed that mutations in the M- and L-segments primarily contribute to the attenuation of MP-12 mouse virulence [28].
MP-12 has been tested for its potential as both veterinary and human vaccines for RVFV. Immunization of ewes at 70 to 100 days of pregnancy with MP-12 induced neutralizing antibodies from 1:80 to 1:320, with no resulting fetus abnormality [29-31]. Newborn lambs from the immunized ewes did not exhibit neutralizing antibodies against RVFV, and the lambs rapidly acquired neutralizing antibodies (1:80 and more) by having the colostrums of the MP-12-vaccinated ewes [11]. In addition, two-days-old to three-months-old lambs survived the MP-12-vaccination and acquired neutralizing antibodies against RVFV [29, 32, 33]. MP-12 vaccination neither induced virus shedding into milk in lactating cows nor caused abortions in cows during 3-, 5- and 8-month gestations [34]. However, MP-12 vaccination of ewes at the 28th day of gestation induced a low level (4%) of abortion and resulted in teratogenic effects in newborn lambs (14%) [35], which may indicate that the use of MP-12 in early pregnancy could cause some loss of lambs. To test MP-12 as a potential human vaccine, it was initially inoculated into more than 100 human volunteers; it has been shown to be safe and immunogenic when adequate dose is administered [36]. MP-12 is currently undergoing further Phase II clinical evaluation in human volunteers.
A plaque isolate (clone 13) of RVFV 74HB59 strain, isolated in Central Africa from a patient having RVF, lacks approximately 70% of an NSs ORF (Fig.1), and is significantly attenuated [37]. Experiments using various reassortant viruses between clone 13 and wild-type ZH548 revealed that the viruses carrying a clone 13-derived S-segment had a low virulence in mice, while the viruses carrying a clone 13-derived M-segment and/or L-segment were virulent in mice. The findings pointed to NSs as the determinant of virulence in mice [7, 38]. In addition, immunization of pregnant ewes with clone 13 induced a protective immunity without causing abortions [20]. A reassortant virus, called the R566 strain, that carries a clone 13 S-segment and MP-12 M- and L-segments, is also under development as a veterinary vaccine candidate [39].
Using a reverse genetics system, Bird et al. generated a ZH501-derived mutant virus (rRVF-ΔNSs:GFP-ΔNSm) lacking the NSm gene in the M-segment and carrying a green fluorescent protein (GFP) in place of the NSs gene in the S-segment (Fig.1)[40]. The rRVF-ΔNSs:GFP-ΔNSm is highly attenuated in rat probably due to the lack of NSs. The s.c. inoculation of 1×103 PFU resulted in the production of high-neutralizing antibody titers at 21 days post immunization without any detectable viremia, while all vaccinated rats survived a wt RVFV challenge at 28 days post vaccination [3]. Accordingly, the use of a live attenuated veterinary RVFV vaccine carrying deletions of a viral gene(s), e.g., an NSs gene and/or NSm gene, and an insertion of a nonviral gene foreign gene is valuable for distinguishing vaccinated animals from those that are naturally infected with wt RVFV, because the immunized animals do not elicit antibodies against the deleted proteins, yet they elicit antibodies for the inserted nonviral gene. The potential problems of vaccine candidates lacking NSs are that the deletion mutant virus may not be able to replicate efficiently in animals, which have normal innate immunity, and may not induce long-term immunity.
4. Recombinant proteins for RVFV vaccination
Dalrymple et al. mapped the protective determinants of RVFV glycoproteins in RVFV G2 regions by using vaccinia virus expressing G1/G2 and those expressing a series of truncated G2 [41]. Thus far, 3 neutralizing epitopes have been mapped in G2 [42]. Accordingly, immunization of animals with purified G2 or expressed G2 would elicit neutralizing antibodies against RVFV.
Several different approaches have been tested to assess the competence of the expressed G1/G2 proteins for eliciting neutralizing antibodies in animals. Schmaljohn et al. reported that s.c. inoculation of mice with lysates of insect Sf9 cells expressing RVFV G1 and G2 induced protective immunity, whereas the inclusion of NSm compromised the immunization [43]. Gorchakov et al. showed that mice were protected from wild-type RVFV challenge following immunization with a Venezuelan equine encephalitis virus (VEEV) replicon expressing G2, but not with Sindbis virus (SINV) replicon expressing G1 and G2 [44]; in both cases, the PRNT titer was <1:80. However, the VEEV replicon expressing G2 failed to efficiently amplify in cell culture in the presence of helper virus due to the negative effect of RVFV G2 on the VEEV replicon. They also reported that immunization with chimeric VEEV expressing partial G2 fused to the N-terminus of VEEV E2 efficiently protected mice from wild-type RVFV challenge [44]. Another study showed that immunization twice with the replicon of a mosquito isolate of SINV (AR86) or that of a human isolate (Girdwood), both of which express RVFV NSm, G1 and G2, induced protective immunity in mice, and the latter also induced neutralizing antibodies in sheep [45]. In South Africa, lumpy skin disease virus (LSDV), belonging to the Capripoxvirus genus, was used for the expression of RVFV G1 and G2 to protect sheep from RVFV as well as sheep poxvirus, closely related to LSDV [46]. These studies suggest that viral vectors are useful for expression of RVFV G1 and G2 and may be further improved as veterinary vaccines.
Virus-like particles (VLP) may be developed as an alternative to traditional formalin-inactivated RVFV vaccines. RVFV VLP is a non-replicable viral particle, and it consists of viral envelope G1, G2 proteins and N protein [47, 48], and can attach target cells like infectious RVFV. After VLP binds to a cellular receptor, the viral envelope proteins are likely digested in endolysosomes, and then antigens are presented by MHC class II molecules. It has been suggested that VLP has an advantage over soluble proteins in terms of its antigens’ stability and its immunogenicity [49]. Näslund et al reported that the co-expression of RVFV N, L, G1, G2, 78kD, NSm proteins and minigenome RNA derived from the M-segment in mammalian cells results in the production of RVFV VLPs [50]. Immunization of mice with the RVFV VLPs elicited neutralizing antibody titers of 1:250 to >1:1250, and the immunized mice were successfully protected from challenge with an RVFV ZH548 strain [50]. The cost reduction and the selection of appropriate cell substrates for the preparation of RVFV VLPs may be needed to develop RVFV VLP as human vaccine candidates.
Immunization with plasmid encoding a viral protein(s) is another approach for inducing immunity against pathogens. An advantage for the immunization with plasmids is that DNA plasmids are stable, and hence a DNA-based immunization method may be suitable for use in tropical areas, where access to refrigeration systems is sometimes difficult. A series of 4 immunizations by gene gun of mice with plasmid encoding RVFV G1 and G2 has elicited neutralizing titers of 1:40 to 1:320 and protected the immunized mice from wild-type RVFV challenge [51]. Another study showed that a series of 4 immunizations by gene gun of mice with plasmid DNA encoding G1 and G2 induced neutralizing antibody titers of 1:25 to 1:75; however, between 25−50% of the immunized mice showed some clinical signs after wild-type RVFV challenge, suggesting the incomplete protection [52].
7. Conclusion
Development of a safe and effective RVFV vaccine is required to protect humans and ruminants from RVFV during outbreaks. Considering the possibility that RVFV may circulate long-term in mosquito populations, an effective vaccination should elicit long-term protective immunity, both in human and animals to prevent further spread of RVFV. Several new generation vaccines are currently under development, and their further improvement will facilitate our preparedness for potential introduction of RVFV into the U.S. and other non-endemic countries. TSI-GSD 200 is a safe vaccine candidate for human; however, primary and follow-up booster administrations are required for maximum protection against RVFV. MP-12, which is highly immunogenic, is under development as both a human and veterinary vaccine.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Daubney R, Hudson JR. Enzootic hepatitis or Rift Valley fever: An undescribed virus disease of sheep cattle and man from east Africa. J Path Bact. 1931;34:545–79. [Google Scholar]
- 2.Peters CJ, Meegan JM. Rift Valley Fever. In: Steele JH, editor. CRC Handbook Series in Zoonoses, Section B: Viral Zoonoses. Vol. 1. CRC Press; Florida: 1981. pp. 403–420. [Google Scholar]
- 3.Bird BH, Ksiazek TG, Nichol ST, Maclachlan NJ. Rift Valley fever virus. J Am Vet Med Assoc. 2009;234(7):883–93. doi: 10.2460/javma.234.7.883. [DOI] [PubMed] [Google Scholar]
- 4.Weiss KE. Rift Valley fever-A review. Bull Epz Dis Afr. 1957;5:431–58. [Google Scholar]
- 5.Easterday BC. Rift Valley fever. Adv Vet Sci. 1965;10:65–127. [PubMed] [Google Scholar]
- 6.Schmaljohn C. Bunyaviridae: the viruses and their replication. In: Knipe DM, Howley PM, editors. Fields Virology. 4th ed. Lippincott, Williams & Wilkins; Maryland: 2001. pp. 1581–602. [Google Scholar]
- 7.Bouloy M, Janzen C, Vialat P, Khun H, Pavlovic J, Huerre M, et al. Genetic evidence for an interferon-antagonistic function of rift valley fever virus nonstructural protein NSs. J Virol. 2001;75(3):1371–7. doi: 10.1128/JVI.75.3.1371-1377.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bird BH, Albarino CG, Nichol ST. Rift Valley fever virus lacking NSm proteins retains high virulence in vivo and may provide a model of human delayed onset neurologic disease. Virology. 2007;25(1):10–5. doi: 10.1016/j.virol.2007.01.046. 362. [DOI] [PubMed] [Google Scholar]
- 9.House JA, Turell MJ, Mebus CA. Rift Valley fever: present status and risk to the Western Hemisphere. Ann N Y Acad Sci. 1992;16:233–42. doi: 10.1111/j.1749-6632.1992.tb19652.x. 653. [DOI] [PubMed] [Google Scholar]
- 10.Niklasson BS, Meadors GF, Peters CJ. Active and passive immunization against Rift Valley fever virus infection in Syrian hamsters. Acta Pathol Microbiol Immunol Scand [C] 1984;92(4):197–200. doi: 10.1111/j.1699-0463.1984.tb00074.x. [DOI] [PubMed] [Google Scholar]
- 11.Morrill JC, Jennings GB, Caplen H, Turell MJ, Johnson AJ, Peters CJ. Pathogenicity and immunogenicity of a mutagen-attenuated Rift Valley fever virus immunogen in pregnant ewes. Am J Vet Res. 1987;48(7):1042–7. [PubMed] [Google Scholar]
- 12.Bird BH, Khristova ML, Rollin PE, Ksiazek TG, Nichol ST. Complete genome analysis of 33 ecologically and biologically diverse Rift Valley fever virus strains reveals widespread virus movement and low genetic diversity due to recent common ancestry. J Virol. 2007;81(6):2805–16. doi: 10.1128/JVI.02095-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Randall R, Gibbs CJ, Jr., Aulisio CG, Binn LN, Harrison VR. The development of a formalin-killed Rift Valley fever virus vaccine for use in man. J Immunol. 1962;89:660–71. [PubMed] [Google Scholar]
- 14.Randall R, Binn LN, Harrison VR. Immunization against Rift Valley Fever Virus. Studies on the Immunogenicity of Lyophilized Formalin-Inactivated Vaccine. J Immunol. 1964;93:293–9. [PubMed] [Google Scholar]
- 15.Eddy GA, Peters CJ, Meadors G, Cole FE., Jr Rift Valley fever vaccine for humans. Contr Epidem Biostatist. 1981;3:124–41. [Google Scholar]
- 16.Niklasson B. Rift Valley fever virus vaccine trial: study of side-effects in humans. Scand J Infect Dis. 1982;14(2):105–9. doi: 10.3109/inf.1982.14.issue-2.06. [DOI] [PubMed] [Google Scholar]
- 17.Pittman PR, Liu CT, Cannon TL, Makuch RS, Mangiafico JA, Gibbs PH, et al. Immunogenicity of an inactivated Rift Valley fever vaccine in humans: a 12-year experience. Vaccine. 2000;18(1−2):181–9. doi: 10.1016/s0264-410x(99)00218-2. [DOI] [PubMed] [Google Scholar]
- 18.Kark JD, Aynor Y, Peters CJ. A Rift Valley fever vaccine trial: 2. Serological response to booster doses with a comparison of intradermal versus subcutaneous injection. Vaccine. 1985;3(2):117–22. doi: 10.1016/0264-410x(85)90060-x. [DOI] [PubMed] [Google Scholar]
- 19.Kark JD, Aynor Y, Peters CJ. A rift Valley fever vaccine trial. I. Side effects and serologic response over a six-month follow-up. Am J Epidemiol. 1982;116(5):808–20. doi: 10.1093/oxfordjournals.aje.a113471. [DOI] [PubMed] [Google Scholar]
- 20.Swanepoel R, Coetzer JAW. Rift Valley fever. In: Coetzer JAW, Thompson GR, Tustin RD, et al., editors. Infectious diseases of livestock with special reference to southern Africa. 2nd ed. Oxford University Press; Cape Town, South Africa: 2004. pp. 1037–1070. [Google Scholar]
- 21.World Health Organization The use of veterinary vaccines for prevention and control of Rift Valley fever: memorandum from a WHO/FAO meeting. Bull World Health Organ. 1983;61(2):261–8. [PMC free article] [PubMed] [Google Scholar]
- 22.Barnard BJ, Botha MJ. An inactivated rift valley fever vaccine. J S Afr Vet Assoc. 1977;48(1):45–8. [PubMed] [Google Scholar]
- 23.Smithburn KC. Rift Valley fever; the neurotropic adaptation of the virus and the experimental use of this modified virus as a vaccine. Br J Exp Pathol. 1949;30(1):1–16. [PMC free article] [PubMed] [Google Scholar]
- 24.Caplen H, Peters CJ, Bishop DH. Mutagen-directed attenuation of Rift Valley fever virus as a method for vaccine development. J Gen Virol. 1985;66(10):2271–7. doi: 10.1099/0022-1317-66-10-2271. [DOI] [PubMed] [Google Scholar]
- 25.Saluzzo JF, Smith JF. Use of reassortant viruses to map attenuating and temperature-sensitive mutations of the Rift Valley fever virus MP-12 vaccine. Vaccine. 1990;8(4):369–75. doi: 10.1016/0264-410x(90)90096-5. [DOI] [PubMed] [Google Scholar]
- 26.Vialat P, Muller R, Vu TH, Prehaud C, Bouloy M. Mapping of the mutations present in the genome of the Rift Valley fever virus attenuated MP12 strain and their putative role in attenuation. Virus Res. 1997;52(1):43–50. doi: 10.1016/s0168-1702(97)00097-x. [DOI] [PubMed] [Google Scholar]
- 27.Takehara K, Min MK, Battles JK, Sugiyama K, Emery VC, Dalrymple JM, et al. Identification of mutations in the M RNA of a candidate vaccine strain of Rift Valley fever virus. Virology. 1989;169(2):452–7. doi: 10.1016/0042-6822(89)90171-2. [DOI] [PubMed] [Google Scholar]
- 28.Billecocq A, Gauliard N, Le May N, Elliott RM, Flick R, Bouloy M. RNA polymerase I-mediated expression of viral RNA for the rescue of infectious virulent and avirulent Rift Valley fever viruses. Virology. 2008;378(2):377–84. doi: 10.1016/j.virol.2008.05.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Morrill JC, Carpenter L, Taylor D, Ramsburg HH, Quance J, Peters CJ. Further evaluation of a mutagen-attenuated Rift Valley fever vaccine in sheep. Vaccine. 1991;9(1):35–41. doi: 10.1016/0264-410x(91)90314-v. [DOI] [PubMed] [Google Scholar]
- 30.Morrill JC, Johnson BK, Hyams C, Okoth F, Tukei PM, Mugambi M, et al. Serological evidence of arboviral infections among humans of coastal Kenya. J Trop Med Hyg. 1991;94(3):166–8. [PubMed] [Google Scholar]
- 31.Baskerville A, Hubbard KA, Stephenson JR. Comparison of the pathogenicity for pregnant sheep of Rift Valley fever virus and a live attenuated vaccine. Res Vet Sci. 1992;52(3):307–11. doi: 10.1016/0034-5288(92)90029-2. [DOI] [PubMed] [Google Scholar]
- 32.Moussa MI, Abdel-Wahab KS, Wood OL. Experimental infection and protection of lambs with a minute plaque variant of Rift Valley fever virus. Am J Trop Med Hyg. 1986;5(3):660–2. doi: 10.4269/ajtmh.1986.35.660. [DOI] [PubMed] [Google Scholar]
- 33.Hubbard KA, Baskerville A, Stephenson JR. Ability of a mutagenized virus variant to protect young lambs from Rift Valley fever. Am J Vet Res. 1991;52(1):50–5. [PubMed] [Google Scholar]
- 34.Morrill JC, Mebus CA, Peters CJ. Safety and efficacy of a mutagen-attenuated Rift Valley fever virus vaccine in cattle. Am J Vet Res. 1997;58(10):1104–9. [PubMed] [Google Scholar]
- 35.Hunter P, Erasmus BJ, Vorster JH. Teratogenicity of a mutagenised Rift Valley fever virus (MVP 12) in sheep. Onderstepoort J Vet Res. 2002;69(1):95–8. [PubMed] [Google Scholar]
- 36.Peters CJ. Emergence of Rift Valley fever. In: Saluzzo JF, Dodet B, editors. Factors in the Emergence of Arbovirus Diseases. Elsevier; Paris: 1997. pp. 253–64. [Google Scholar]
- 37.Muller R, Saluzzo JF, Lopez N, Dreier T, Turell M, Smith J, et al. Characterization of clone 13, a naturally attenuated avirulent isolate of Rift Valley fever virus, which is altered in the small segment. Am J Trop Med Hyg. 1995;53(4):405–11. doi: 10.4269/ajtmh.1995.53.405. [DOI] [PubMed] [Google Scholar]
- 38.Vialat P, Billecocq A, Kohl A, Bouloy M. The S segment of rift valley fever phlebovirus (Bunyaviridae) carries determinants for attenuation and virulence in mice. J Virol. 2000;74(3):1538–43. doi: 10.1128/jvi.74.3.1538-1543.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Thiongane Y, Lena P, Moustapha M, Lo B, Sall B, Martin V, et al. Pathogenicity and immunogenicity of the reassortant attenuated strain R566 of Rift Valley fever virus in sheep.. FAO/IAEA International Symposium on Applications of Gene-based Technologies for Improving Animal Production and Health in Developing Countries.; Vienna, Austria. Oct. 2003. [Google Scholar]
- 40.Bird BH, Albarino CG, Hartman AL, Erickson BR, Ksiazek TG, Nichol ST. Rift valley fever virus lacking the NSs and NSm genes is highly attenuated, confers protective immunity from virulent virus challenge, and allows for differential identification of infected and vaccinated animals. J Virol. 2008;82(6):2681–91. doi: 10.1128/JVI.02501-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Dalrymple JMaC. M.S. Mapping protective determinants of Rift Valley fever virus using recombinant vaccinia virus. In: Lerner RA, Ginsberg H, Chanock RM, Brown F, editors. Vaccines 89' Modern Approaches to New Vaccines Including Prevention of AIDS. Cold Spring Harbor Laboratory; New York: 1989. pp. 371–375. [Google Scholar]
- 42.Keegan K, Collett MS. Use of bacterial expression cloning to define the amino acid sequences of antigenic determinants on the G2 glycoprotein of Rift Valley fever virus. J Virol. 1986;58(2):263–70. doi: 10.1128/jvi.58.2.263-270.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Schmaljohn CS, Parker MD, Ennis WH, Dalrymple JM, Collett MS, Suzich JA, et al. Baculovirus Expression of the M-Genome Segment of Rift-Valley Fever Virus and Examination of Antigenic and Immunogenic Properties of the Expressed Proteins. Virology. 1989;170(1):184–92. doi: 10.1016/0042-6822(89)90365-6. [DOI] [PubMed] [Google Scholar]
- 44.Gorchakov R, Volkova E, Yun N, Petrakova O, Linde NS, Paessler S, et al. Comparative analysis of the alphavirus-based vectors expressing Rift Valley fever virus glycoproteins. Virology. 2007;366(1):212–25. doi: 10.1016/j.virol.2007.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Heise MT, Whitmore A, Thompson J, Parsons M, Grobbelaar AA, Kemp A, et al. An alphavirus replicon-derived candidate vaccine against Rift Valley fever virus. Epidemiol Infect. 2009;137:1–10. doi: 10.1017/S0950268808001696. [DOI] [PubMed] [Google Scholar]
- 46.Wallace DB, Ellis CE, Espach A, Smith SJ, Greyling RR, Viljoen GJ. Protective immune responses induced by different recombinant vaccine regimes to Rift Valley fever. Vaccine. 2006;24:7181–9. doi: 10.1016/j.vaccine.2006.06.041. [DOI] [PubMed] [Google Scholar]
- 47.Habjan M, Penski N, Wagner V, Spiegel M, Overby AK, Kochs G, et al. Efficient production of Rift Valley fever virus-like particles: The antiviral protein MxA can inhibit primary transcription of bunyaviruses. Virology. 2009;385(2):400–8. doi: 10.1016/j.virol.2008.12.011. [DOI] [PubMed] [Google Scholar]
- 48.Liu L, Celma CC, Roy P. Rift Valley fever virus structural proteins: expression, characterization and assembly of recombinant proteins. Virol J. 2008;5:82. doi: 10.1186/1743-422X-5-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ludwig C, Wagner R. Virus-like particles-universal molecular toolboxes. Curr Opin Biotechnol. 2007;18(6):537–45. doi: 10.1016/j.copbio.2007.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Naslund J, Lagerqvist N, Habjan M, Lundkvist A, Evander M, Ahlm C, et al. Vaccination with virus-like particles protects mice from lethal infection of Rift Valley Fever Virus. Virology. 2009;385(2):409–15. doi: 10.1016/j.virol.2008.12.012. [DOI] [PubMed] [Google Scholar]
- 51.Spik K, Shurtleff A, McElroy AK, Guttieri MC, Hooper JW, SchmalJohn C. Immunogenicity of combination DNA vaccines for Rift Valley fever virus, tick-borne encephalitis virus, Hantaan virus, and Crimean Congo hemorrhagic fever virus. Vaccine. 2006;24(21):4657–66. doi: 10.1016/j.vaccine.2005.08.034. [DOI] [PubMed] [Google Scholar]
- 52.Lagerqvist N, Naslund J, Lundkvist A, Bouloy M, Ahlm C, Bucht G. Characterisation of immune responses and protective efficacy in mice after immunisation with Rift Valley Fever virus cDNA constructs. Virol J. 2009;6:6. doi: 10.1186/1743-422X-6-6. [DOI] [PMC free article] [PubMed] [Google Scholar]