Hospital Utilization and Characteristics of Patients Experiencing Recurrent Readmissions Within Children’s Hospitals (original) (raw)
. Author manuscript; available in PMC: 2012 Feb 16.
Published in final edited form as: JAMA. 2011 Feb 16;305(7):682–690. doi: 10.1001/jama.2011.122
Abstract
Context
Early hospital readmission is emerging as an indicator of care quality. Some children with chronic illnesses may be readmitted on a recurrent basis, but there are limited data describing their rehospitalization patterns and impact.
Objectives
To describe the inpatient resource utilization, clinical characteristics, and admission reasons of patients recurrently readmitted to children’s hospitals.
Design, Setting, and Patients
Retrospective cohort analysis of 317 643 patients (n=579 504 admissions) admitted to 37 US children’s hospitals in 2003 with follow-up through 2008.
Main Outcome Measure
Maximum number of readmissions experienced by each child within any 365-day interval during the 5-year follow-up period.
Results
In the sample, 69 294 patients (21.8%) experienced at least 1 readmission within 365 days of a prior admission. Within a 365-day interval, 9237 patients (2.9%) experienced 4 or more readmissions; time between admissions was a median 37 days (interquartile range [IQR], 21–63). These patients accounted for 18.8% (109 155 admissions) of all admissions and 23.2% ($3.4 billion) of total inpatient charges for the study cohort during the entire follow-up period. Tests for trend indicated that as the number of readmissions increased from 0 to 4 or more, the prevalences increased for a complex chronic condition (from 22.3% [n=55 382/248 349] to 89.0% [n=8225/9237]; P <.001), technology assistance (from 5.3% [n = 13 163] to 52.6% [n=4859]; P <.001), public insurance use (from 40.9% [n = 101 575] to 56.3% [n=5202]; P <.001), and non-Hispanic black race (from 21.8% [n=54 140] to 34.4% [n=3181]; P <.001); and the prevalence decreased for readmissions associated with an ambulatory care–sensitive condition (from 23.1% [62 847/272 065] to 14.0% [15 282/109 155], P<.001). Of patients readmitted 4 or more times in a 365-day interval, 2633 (28.5%) were rehospitalized for a problem in the same organ system across all admissions during the interval.
Conclusions
Among a group of pediatric hospitals, 18.8% of admissions and 23.2% of inpatient charges were accounted for by the 2.9% of patients with frequent recurrent admissions. Many of these patients were rehospitalized recurrently for a problem in the same organ system.
Hospital readmission is increasingly considered an indicator of care quality and a leverage point for reimbursement reform to reduce excessive health care costs.1,2 Risk factors for readmission in children include the presence of a complex chronic health condition, black race, and Medicaid insurance use.3–6 Children assisted with medical technology, such as a tracheostomy or a cerebrospinal fluid ventricular shunt, are also at risk for readmission because of a fragile medical state and risk of technology malfunction.7,8 Children with these attributes are routinely cared for within children’s hospitals.9
Prior studies of readmissions in children focus mainly on an index admission and a subsequent, early readmission experience, often within 30 days.3–6 This approach may underestimate the impact of patients experiencing recurrent readmissions during the weeks and months after hospitalization. Adults experiencing recurrent readmissions tend to experience a dense cluster of multiple hospitalizations and quickly accumulate substantial inpatient health care costs.10–12 It is unknown whether children experience this same phenomenon.
Strategies to reduce admissions must distinguish between readmissions that are potentially avoidable and those that may in fact indicate higher quality of care. Children with chronic conditions may require multiple, unavoidable, and necessary hospitalizations (such as chemotherapy for leukemia) to improve their health status. On the other hand, repeat admissions felt to be amenable to high-quality outpatient care (asthma- and seizure-related admissions, for example) or related to the same medical problem (such as repeated admissions for sickle cell crisis) may be considered potentially avoidable.13,14
The objectives of this study were to describe the inpatient resource utilization of children experiencing recurrent readmissions within 37 children’s hospitals, compare the clinical and demographic characteristics of patients by their readmission frequency, and evaluate the reasons for readmission.
METHODS
This was a retrospective cohort analysis of the Pediatric Health Information System (PHIS), an administrative database containing combined hospitalization data from 37 tertiary care pediatric hospitals in the US West (n=8, 21.6%), Midwest (n=11, 29.7%), South (n=14, 37.8%), and Northeast (n=4, 10.8%). These hospitals are designated freestanding children’s hospitals by the National Association of Children’s Hospitals and Related Institutions and are members of Child Health Corporation of America (CHCA), a business alliance of noncompeting children’s hospitals.15 Data are maintained through CHCA and Thomson Reuters Healthcare (New York, New York). Children were followed up across multiple admissions to the same PHIS hospital using unique numerical patient identifiers. This study was approved by the institutional review board at Children’s Hospital Boston with an informed consent waiver.
Patients of all ages admitted to one of the PHIS children’s hospitals at least once during calendar year 2003 were included and followed up through 2008 to examine their readmissions. Patients 18 years and older who used children’s hospitals were included because many have pediatric chronic health conditions that may predispose them to experience readmission.16
Hospital Resource Utilization
The number of hospitalizations, days spent in the hospital, and aggregate hospital charges accrued for each patient during the follow-up period were assessed. Weexcluded hospitalizations associated with use of primary inpatient rehabilitation, psychiatry or psychological service, and normal newborn and obstetric care because these services were not consistently available to patients across the different hospitals. We also excluded chemotherapy hospitalizations (APR-DRG [All Patient Refined Diagnosis Related Groups] version 24 of 693 or a principal procedure of International Classification of Diseases, Ninth Revision, Clinical Modification [_ICD-9-CM_] codes 99.25, 99.28, or 00.10). Chemotherapy may be indicative of protocol-driven, scheduled repeated admissions. Individual patients who experienced one of these admission types were not excluded from analysis unless all of their admissions were attributable to the admission types.
Recurrent Readmission Frequency
We evaluated the maximum recurrent readmission frequency for each child, defined as the maximum number of rehospitalizations experienced by each child within any 365-day interval within the follow-up period. There were 1460 full 365-day intervals during the study period. Interval 1 was January 1, 2003, to December 31, 2003. Interval 2 was January 2, 2003, to January 1, 2004, etc. This strategy permits readmission identification not captured by calendar-year intervals (eg, a child hospitalized once in December 2003 and readmitted in January 2004). We counted the number of rehospitalizations that each child experienced during each interval following an index admission and classified each child into 1 of 5 categories based on the maximum number of readmissions experienced during any interval: 0, 1, 2, 3, and 4 or more re-admissions. Patients with 4 or more readmissions represented the 97th percentile in the distribution of recurrent readmissions among the study cohort.
Characteristics of Children
Demographic characteristics analyzed were age (neonate, 0–30 days; infancy, 31–365 days; early childhood, 1–4 years; late childhood, 5–12 years; adolescence, 13–18 years; or adulthood, >18 years), sex, race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, Asian, or other), and insurance type (public, commercial, self-pay and no charge, other, or missing). Race/ethnicity was classified by patients or their parents or legal guardians with predefined options within the data set. Race/ethnicity was assessed because it may contribute to readmission risk.6
We categorized chronic diagnoses into 2 clinical characteristic categories hypothesized to be more prevalent among children experiencing frequent readmissions: complex chronic conditions (CCCs)3,17–19 and technology assistance.7,8,20,21 Each hospital provided up to 21 ICD-9-CM diagnosis and procedure codes per admission for category assignment.
CCCs were chosen as a clinically meaningful diagnostic category because they represent defined ICD-9-CM code groupings of pediatric respiratory, renal, gastrointestinal, metabolic, hematologic, congenital or genetic defect, malignancy, cardiovascular, and neuromuscular diagnoses that (1) are expected to last longer than 12 months and (2) involve either several different organ systems or 1 organ system severely enough to require specialty pediatric care and hospitalization.17–19 Technology assistance was defined as medical technology used to maintain a child’s health status, such as gastrostomy, tracheostomy, cerebro-spinal fluid ventricular shunt, permanent indwelling catheter, and pace-maker.7,8,20,21
Reasons for Hospitalization
To assess potentially preventable readmissions, we evaluated the principal ICD-9-CM diagnosis code for each hospitalization throughout the entire follow-up period to see if it was associated with an ambulatory care–sensitive condition (ACSC). ACSCs are conditions for which treatment with timely and appropriate ambulatory care may prevent a hospitalization.13 For instance, in the primary care setting, appropriate asthma chronic management therapy coupled with the use of an asthma action plan may mitigate an acute exacerbation and prevent an admission.14,22
We also evaluated readmissions during a patient’s maximum readmission frequency interval that are speculated to reflect a continuation or recurrence of the reason for the prior admission and therefore may be potentially avoidable.23 The Medicare Payment Advisory Commission (MedPAC) and payers have used major diagnostic categories to help identify these readmission situations from administrative health data.23 The major diagnostic categories represent 25 mutually exclusive organ system domains (nervous system, respiratory system, etc). One major diagnostic category is assigned to each hospitalization from the principal ICD-9-CM diagnosis code.
Statistical Analyses
Hospital resource utilization accrued during the entire follow-up period was summarized for patients within each readmission frequency category using median and interquartile range (IQR) as these data were not normally distributed. Charges were converted to 2008 dollars using the consumer price index for hospital and related services.24 We used a Mantel-Haenszel χ2 trend test to determine if prevalence rates of each characteristic varied with readmission frequency among whole categories (eg, patients with and without a CCC) and within specific subgroups (eg, non-Hispanic black race).
In multivariate analysis, generalized estimating equations were used with a multinomial distribution and a cumulative logit link function to analyze the likelihood of a characteristic being associated with an incrementally increasing number of recurrent admissions while clustering patients’ data within individual hospitals. The model was built using a backward elimination, eliminating attributes with P values greater than .05. A 2-sided _P_≤.001 was considered statistically significant to account for multiple comparisons (Bonferroni adjusted level of significance = .0013). All analyses were performed using SAS version 9.2 (SAS Institute, Cary, North Carolina).
RESULTS
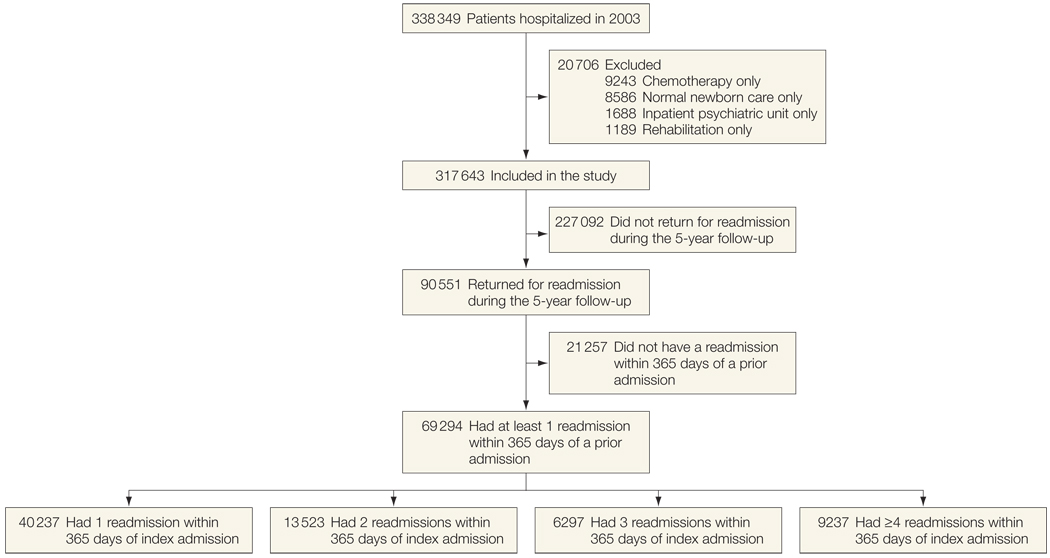
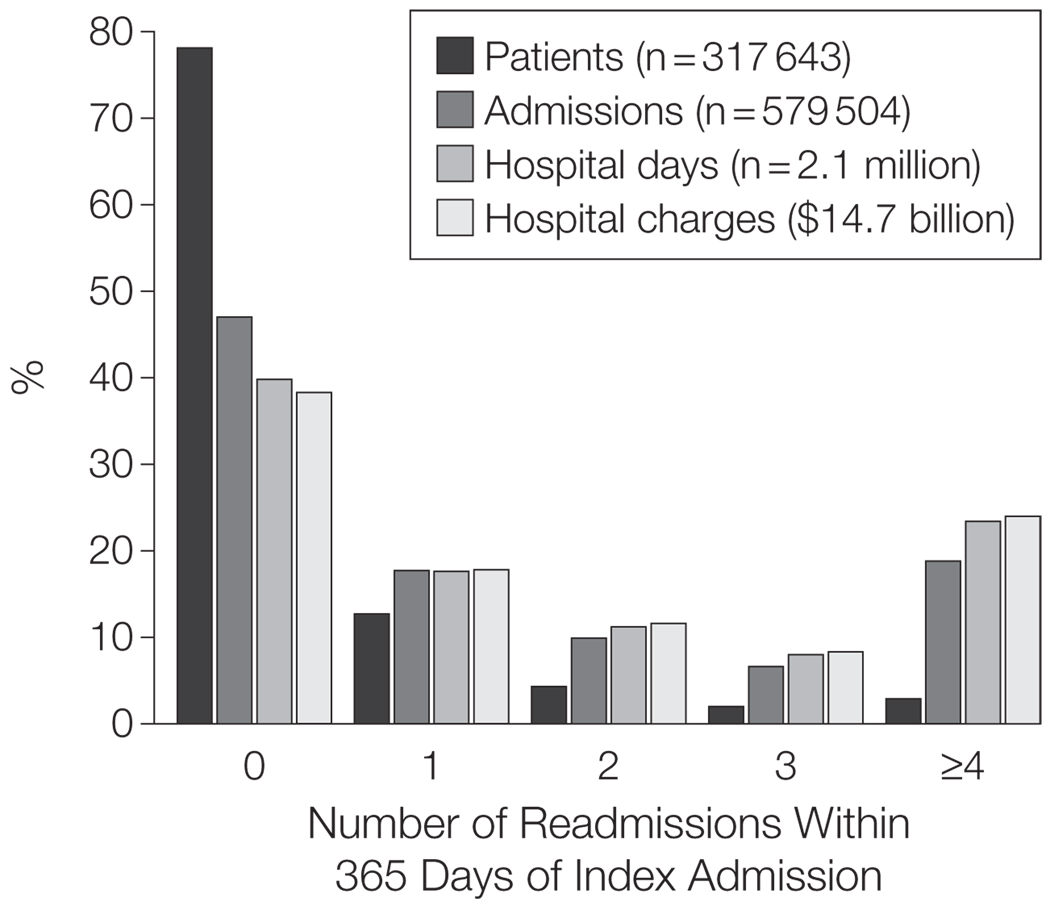
There were 317 643 patients hospitalized during the year 2003 who were included for analysis. Among that sample, 69 294 patients (21.8%) experienced 1 or more readmission within 365 days of a prior admission. Among them, 9237 patients (2.9%) experienced 4 or more readmissions within a 365-day interval (Figure 1) with a median of 37 days (IQR, 21–63) between their admissions (Table 1). Despite accounting for only 2.9% of patients in the cohort, these patients accounted for 18.8% (109 155) of admissions, 23.4% (491 815) of bed-days, and 23.2% ($3.42 billion) of total aggregate charges of the study cohort during the entire follow-up period (2003–2008) (Figure 2). The prevalence of these patients (range, 1.5%–4.9%) and hospital charges attributable to them (range, 14.1%-34.3%) varied among the individual hospitals.
Figure 1.
Readmission Experiences of Children Admitted to 37 US Children’s Hospitals in 2003 With Follow-up Through 2008
Shown are the numbers of patients hospitalized in 2003 with different readmission experiences during the follow-up period.
Table 1.
Inpatient Resource Utilization of Patients Admitted to 37 Children’s Hospitals in 2003 With Follow-up Through 2008
| Readmission Frequency, Median (IQR)a | |||||
|---|---|---|---|---|---|
| 0(n = 248 349) | 1(n = 40 237) | 2(n = 13 523) | 3(n = 6297) | ≥4(n = 9237) | |
| Total admissions per patient, No. | 1 (1–1) | 2 (2–3) | 4 (3–5) | 6 (4–7) | 10 (7–14) |
| Time between admissions, d | NA | 209 (43–352) | 142 (72–204) | 107 (62–148) | 37 (21–63) |
| Time spent in the hospital across admissions per patient, d | 2 (1–3) | 6 (4–11) | 12 (7–21) | 20 (12–33) | 38 (23–64) |
| Total charges accrued across admissions per patient, $b | 9931(5563–19 138) | 25660(13 550–52 953) | 55 758(29 138–110 899) | 93907(51 716–173 739) | 184510(99 437–346 958) |
Figure 2.
Inpatient Health Services Effect of Children Recurrently Readmitted to 37 US Children’s Hospitals in 2003 With Follow-up Through 2008
Percentages shown were attributable to children categorized by their maximum recurrent readmission frequency (0 to ≥4) during a 365-day interval following an index hospitalization.
Resource Utilization Timing
Patients’ maximum readmission frequency 365-day interval began a median of 0.7 years (IQR, 0.3–1.5) from the beginning of the study. During this interval, patients with 4 or more readmissions experienced 39.8% (43 444) of their total admissions and 40.0% ($1.37 billion) of their total hospital charges accrued during the entire follow-up period. Following this interval until the end of the study period, they experienced 44.6% (48 693) of their admissions and 41.2% ($1.41 billion) of their total hospital charges.
Demographic Characteristics
As readmission frequency increased from 0 to 4 or more, there was an increase in the percentage of children aged 13 to 18 years (from 14.0% [34 769] to 24.1% [2235], P<.001), adult patients older than 18 years (from 2.7% [6705] to 11.1% [1029], P<.001), patients who had public insurance (40.9% [101 575] to 56.3% [5202],P< .001), patients who changed their insurance from commercial to public (8.3% [20 613] to 18.4% [1706], P<.001), and non-Hispanic black patients (21.8% [54 140] to 34.4% [3181],P< .001) (Table 2). Older age, public insurance use, and non-Hispanic black race remained significantly associated with higher readmission frequency in multivariate analysis after controlling for the presence of a CCC, including sickle cell disease (Table 3).
Table 2.
Demographic Characteristics, In-Hospital Mortality, and Readmission Frequency of Children Admitted to 37 Children’s Hospitals in 2003 With Follow-up Through 2008
| Readmission Frequencya | _P_Valueb | |||||
|---|---|---|---|---|---|---|
| 0(n = 248349) | 1(n = 40 237) | 2(n = 13 523) | 3(n = 6297) | ≥4(n = 9237) | ||
| Age, No. (%) of patients Neonate, 0–30 d | 22 351 (9.0) | 1408 (3.5) | 257 (1.9) | 63 (1.0) | 37 (0.4) | <.001 |
| Infant, 31–365 d | 44 702 (18.0) | 6478 (16.1) | 1785 (13.2) | 623 (9.9) | 559 (6.1) | <.001 |
| 1–4 y | 71 027 (28.6) | 11 548 (28.7) | 3854 (28.5) | 1732 (27.5) | 2318 (25.1) | <.001 |
| 5–12 y | 68 792 (27.7) | 12 071 (30.0) | 4300 (31.8) | 2072 (32.9) | 3059 (33.2) | <.001 |
| 13–18 y | 34 769 (14.0) | 6760 (16.8) | 2421 (17.9) | 1310 (20.8) | 2235 (24.1) | <.001 |
| >18y | 6705 (2.7) | 1972 (4.9) | 906 (6.7) | 497 (7.9) | 1029 (11.1) | <.001 |
| Race/ethnicity, No. (%) of patients Non-Hispanic white | 125 168 (50.4) | 19 917 (49.5) | 6491 (48.0) | 3111 (49.4) | 4240 (45.6) | <.001 |
| Non-Hispanic black | 54 140 (21.8) | 10 784 (26.8) | 4111 (30.4) | 1902 (30.2) | 3181 (34.4) | <.001 |
| Hispanic | 45 448 (18.3) | 6398 (15.9) | 2015 (14.9) | 856 (13.6) | 1289 (13.9) | <.001 |
| Asian | 5215 (2.1) | 765 (1.9) | 203 (1.5) | 107 (1.7) | 158 (1.7) | <.001 |
| Other | 18 378 (7.4) | 2373 (5.9) | 703 (5.2) | 321 (5.1) | 399 (4.3) | <.001 |
| Female sex, No. (%) of patients | 110 019 (44.3) | 17 905 (44.5) | 6234 (46.1) | 2934 (46.6) | 4423 (47.9) | <.001 |
| Insurance, No. (%) of patients Public | 101 575 (40.9) | 18 509 (46.0) | 6748 (49.9) | 3224 (51.2) | 5202 (56.3) | <.001 |
| Commercial | 81 210 (32.7) | 12 272 (30.5) | 3827 (28.3) | 1751 (27.8) | 2400 (26.1) | <.001 |
| Other | 50 415 (20.3) | 7404 (18.4) | 2353 (17.4) | 1045 (16.6) | 1303 (14.1) | <.001 |
| Self-pay/no chargec | 14 900 (6.0) | 2011 (5.0) | 595 (4.4) | 271 (4.3) | 325 (3.5) | <.001 |
| Missing data | 248 (0.1) | 40 (0.1) | 0 | 6 (0.1) | 7 (0.1) | .86 |
| In-hospital mortality, No. (%) of patients | 2732 (1.1) | 241 (0.6) | 68 (0.5) | 38 (0.6) | 46 (0.5) | <.001 |
Table 3.
Multivariate Analysis of Demographic and Clinical Characteristics With Increasing Readmission Frequency
| Characteristic | Odds Ratio(95% Confidence Interval)a | _P_Value |
|---|---|---|
| Race/ethnicity | ||
| Non-Hispanic black | 1.65 (1.59–1.70) | <.001 |
| Asian | 1.03 (0.95–1.14) | .45 |
| Hispanic | 0.96 (0.93–0.99) | .05 |
| Other | 0.85 (0.81–0.89) | <.001 |
| Non-Hispanic white | 1 [Reference] | |
| Age | ||
| >18 y | 7.03 (6.51–7.58) | <.001 |
| 13–18 y | 5.87 (5.61–6.14) | <.001 |
| 5–12 y | 4.57 (4.39–4.76) | <.001 |
| 1–4 y | 4.02 (3.87–4.17) | <.001 |
| Infant, 31–365 d | 2.74 (2.64–2.84) | <.001 |
| Neonate, 0–31 d | 1 [Reference] | |
| Public vs commercial insurance | 1.36 (1.33–1.40) | <.001 |
| Complex chronic condition vs no complex chronic condition | 5.61 (5.45–5.78) | <.001 |
| Technology assistance vs no technology assistance | 2.85 (2.74–2.96) | <.001 |
Clinical Characteristics
As readmission frequency increased from 0 to 4 or more, there was an increase in the percentage of patients with 1 or more CCC (from 22.3% [55 382] to 89.0% [8225], P< .001). The most prevalent CCCs among patients with 4 or more readmissions were neuromuscular (39.6%, n = 3654), malignancy (22.4%, n = 2068), and cardiovascular (20.1%, n = 1855). Central nervous system degenerative disorders (n = 792, 8.6%), brain malformations (n = 793, 8.6%), and cerebral palsy (n=741, 8.0%) were the most common individual neuromuscular diagnoses among patients with 4 or more readmissions. The percentage of patients with multiple CCCs also increased with readmission frequency (P<.001): 27.0% (n = 2494) of patients with 4 or more readmissions had 2 different CCCs and 17.4% (n= 1604) had 3 or more CCCs (Table 4).
Table 4.
Clinical Characteristics and Readmission Frequency of Children Admitted to 37 Children’s Hospitals in 2003 With Follow-up Through 2008
| Characteristic | Readmission Frequen cya | _P_Valueb | ||||
|---|---|---|---|---|---|---|
| 0(n = 248 349) | 1(n = 40 237) | 2(n = 13 523) | 3(n = 6297) | ≥4(n = 9237) | ||
| CCCs, No. (%) of patients Any CCC | 55 382 (22.3) | 19 636 (48.8) | 9371 (69.3) | 4941 (78.5) | 8225 (89.0) | <.001 |
| Neuromuscular | 24 090 (9.7) | 8651 (21.5) | 4233 (31.3) | 2200 (34.9) | 3654 (39.6) | |
| Malignancy | 5960 (2.4) | 2696 (6.7) | 1474 (10.9) | 983 (15.6) | 2068 (22.4) | |
| Cardiovascular | 17 384 (7.0) | 5110 (12.7) | 2326 (17.2) | 1131 (18.0) | 1855 (20.1) | |
| Hematology and immunodeficiency | 4719 (1.9) | 2012 (5.0) | 1285 (9.5) | 738 (11.7) | 1818 (19.7) | |
| Other congenital/genetic disorder | 9686 (3.9) | 3621 (9.0) | 1866 (13.8) | 102 (1.6) | 1660 (18.0) | |
| Metabolic | 2484 (1.0) | 1086 (2.7) | 703 (5.2) | 510 (8.1) | 1474 (16.0) | |
| Respiratory | 4470 (1.8) | 2253 (5.6) | 1285 (9.5) | 725 (11.5) | 1205 (13.0) | |
| Gastrointestinal | 2732 (1.1) | 1408 (3.5) | 838 (6.2) | 492 (7.8) | 1020 (11.0) | |
| Renal | 3477 (1.4) | 1288 (3.2) | 636 (4.7) | 339 (5.4) | 918 (9.9) | |
| Multiple CCCs, No. (%) of patients 2 CCCs | 7202 (2.9) | 4024 (10.0) | 2326 (17.2) | 1328 (21.1) | 2494 (27.0) | <.001 |
| ≥3 CCCs | 1242 (0.5) | 1006 (2.5) | 879 (6.5) | 633 (10.1) | 1604 (17.4) | <.001 |
| Technology assistance, No. (%) of patients Any technology | 13 163 (5.3) | 7927 (19.7) | 4733 (35.0) | 2741 (43.5) | 4859 (52.6) | <.001 |
| Digestive | 4967 (2.0) | 3702 (9.2) | 2502 (18.5) | 1530 (24.3) | 2837 (30.7) | |
| Neurologic | 6209 (2.5) | 3902 (9.7) | 2272 (16.8) | 1309 (20.8) | 2180 (23.6) | |
| Renal | 745 (0.3) | 643 (1.6) | 527 (3.9) | 424 (6.7) | 1280 (13.9) | |
| Pulmonary | 1490 (0.6) | 1086 (2.7) | 771 (5.7) | 529 (8.4) | 974 (10.5) | |
| Cardiac | 993 (0.4) | 402 (1.0) | 189 (1.4) | 98 (1.6) | 102 (1.1) | |
| Endocrinology | 0 | 40 (0.1) | 27 (0.2) | 12 (0.2) | 37 (0.4) | |
| CCC and technology combinations, No. (%) of patients Any CCC plus any technology | 9686 (3.9) | 6599 (16.4) | 4246 (31.4) | 2538 (40.3) | 4618 (50.0) | <.001 |
| Neuromuscular CCC Plus any technology | 5215 (2.1) | 3702 (9.2) | 2475 (18.3) | 1475 (23.4) | 2634 (28.5) | |
| Plus digestive technology | 2732 (1.1) | 2052 (5.1) | 1501 (11.1) | 910 (14.5) | 1706 (18.5) | |
| Plus neurologic technology | 2732 (1.1) | 2052 (5.1) | 1352 (10.0) | 830 (13.2) | 1372 (14.9) | |
| Plus pulmonary technology | 745 (0.3) | 604 (1.5) | 500 (3.7) | 344 (5.5) | 705 (7.6) |
As readmission frequency increased from 0 to 4 or more, the percentage of technology assistance increased (from 5.3% [13 163] to 52.6% [4859], P< 001). The most prevalent technologies among the patients with 4 or more readmissions were digestive related (30.7%, n=2837), including gastrostomy tube, and neurologically related (23.6%, n = 2180), including cerebrospinal fluid shunt. As readmission frequency increased from 0 to 4 or more, the percentage of patients with both technology assistance and a CCC increased (from 3.9% [9686] to 50.0% [4618], P<.001). A neuromuscular CCC with digestive (18.5%, n=1706) or neurologic (14.9%, n=1372) technology was the most common pairing among patients with 4 or more readmissions (Table 4). Among patients with cerebral palsy readmitted 4 or more times, 77.1% (n = 571) had a gastrostomy tube.
Hospitalization Characteristics
As readmission frequency increased from 0 to 4 or more, the percentage of hospitalizations associated with an ACSC decreased (from 23.1% [62 847] to 14.0% [15 282], P< .001). Asthma was the most frequent ACSC-related hospitalization (3.8%, n=4148) among the patients with 4 or more readmissions, followed by pneumonia (2.9%, n=3165) and seizure (2.2%, n = 2401). In children with 4 or more readmissions, 21.6% (n = 23 577) of hospitalizations were elective (Table 5).
Table 5.
Hospitalization Characteristics and Readmission Frequency of Children Admitted to Children’s Hospitals in 2003 With Follow-up Through 2008
| Characteristic | Readmission Frequenc ya | _P_Valueb | ||||
|---|---|---|---|---|---|---|
| 0(n = 272 065) | 1(n = 102 470) | 2(n = 57 459) | 3(n = 38 355) | ≥4(n = 109155) | ||
| ACSCs, No. (%) of admissionsc No ACSC | 209 218 (76.9) | 77 160 (75.3) | 44 129 (76.8) | 30 684 (80.0) | 93 873 (86.0) | <.001 |
| ACSC | 62 847 (23.1) | 25 310 (24.7) | 13 331 (23.2) | 7671 (20.0) | 15 282 (14.0) | |
| Asthma | 20 949 (7.7) | 10 862 (10.6) | 5459 (9.5) | 2493 (6.5) | 4148 (3.8) | |
| Cellulitis | 8434 (3.1) | 1639 (1.6) | 575 (1.0) | 307 (0.8) | 764 (0.7) | |
| Gastroenteritis and dehydration | 11 970 (4.4) | 3484 (3.4) | 1666 (2.9) | 1036 (2.7) | 2511 (2.3) | |
| Pneumonia | 8978 (3.3) | 3689 (3.6) | 2183 (3.8) | 1573 (4.1) | 3165 (2.9) | |
| Seizure | 3536 (1.3) | 2869 (2.8) | 1953 (3.4) | 1342 (3.5) | 2401 (2.2) | |
| Upper respiratory tract infection | 8978 (3.3) | 2766 (2.7) | 1551 (2.7) | 959 (2.5) | 2183 (2.0) | |
| Elective admissions, No. (%) of admissionsc Overall | 57 678 (21.2) | 25 208 (24.6) | 13 790 (24.0) | 8630 (22.5) | 23 577 (21.6) | <.001 |
| Medical | 28 295 (10.4) | 13 526 (13.2) | 8217 (14.3) | 5907 (15.4) | 18 883 (17.3) | |
| Surgical | 29 383 (10.8) | 11 682 (11.4) | 2762 (9.7) | 2761 (7.2) | 4803 (4.4) |
Respiratory-related diagnoses (14.0%, n = 6082) and procedures (9.0%, n =3910) and hematology-related diagnoses (9.8%, n=4257) and procedures (15.4%, n=6690) were among the most common principal reasons for admissions for patients during the interval when they experienced 4 or more readmissions. Admissions for diagnostic testing (14.9%, n=6472) and technology complications (8.7%, n=3779) were also prevalent (eTable, available at http://www.jama.com).
Among patients with 4 or more readmissions within a 365-day interval, 28.5% (n=2633) were hospitalized for a problem in the same organ system during the interval. Blood and immunological problems (23.1%, n=608), respiratory system problems (20.4%, n=537), and nervous system problems (17.5%, n=461) were the most prevalent consistent problems encountered by these patients.
COMMENT
This study suggests that a small cohort of recurrently readmitted pediatric patients is a major contributor to inpatient utilization and expenditures within a group of children’s hospitals: nearly one-fourth of all inpatient bed-days and charges were attributable to 3% of admitted patients who experienced 4 or more readmissions within a 1-year period. Some of the readmissions may have been potentially avoidable: nearly one-third of patients readmitted 4 or more times were rehospitalized for a problem in the same organ system during the interval they were most frequently readmitted. If these patients were prospectively identified and received effective readmission prevention services before they accumulated multiple readmissions, there would be potential for substantial inpatient expenditure reduction.
The study findings support the importance of monitoring the number of times individual pediatric patients are readmitted. With a median of 37 days between readmissions, the majority of rehospitalizations experienced by patients with the highest readmission frequency would not have been recorded or reviewed using traditional 30-day hospital readmission metrics.25,26 The readmissions may be underrecognized by primary care clinicians if they are not actively involved in the patients’ hospital or immediate postdischarge care. High rates of absent postdischarge primary care follow-up are reported among adults experiencing readmission.27
The attributes of pediatric patients at risk for recurrent readmissions observed in this study suggest that heightened complexity of discharge care planning may be needed to ensure their safe transition from the hospital.28 Those patients with multiple CCCs and technology assistance may require communication, proactive care planning, and follow-up appointments with multiple outpatient specialty providers, equipment specialists, and home nurses at discharge.29 High-quality discharge care planning, including timely communication with outpatient providers regarding hospitalization course and postdischarge care instructions, may be an important mitigating factor to minimize readmission.30 However, this planning may not prevent multiple future readmissions in children at risk for them if the outpatient providers and health system are underequipped to meet their health care needs, optimally manage their acute illnesses, and minimize their chronic illness exacerbations.
Further investigation is needed to determine whether there is a greater opportunity to break the readmission cycle of patients recurrently readmitted or target patients at risk for a single readmission. In the present study, one-fourth of patients experienced a single readmission within 6 weeks of a prior admission. Although these patients accounted for less hospital resource use than patients with recurrent readmissions, it may be easier to mitigate their readmissions because they have a higher prevalence of ACSC hospitalizations and a lower prevalence of CCCs.
Neuromuscular CCCs were the most prevalent disease group among patients frequently readmitted. Children with these conditions are at risk for uncoordinated care and unmet health care needs.31–33 This care could be contributing to their high rates of emergency department use and subsequent hospitalization.34,35 Young adults with pediatric neuromuscular conditions may be particularly vulnerable for unmet health care needs and overuse of inpatient health services when attempting to transfer their care from pediatric to adult providers.36 This may help explain the rising prevalence of adults 18 years and older with increasing readmission frequency.
Even if the highest care quality is delivered throughout inpatient and outpatient care to children at risk for recurrent readmissions, further investigation is needed to determine which readmissions may be truly avoided. Readmissions for ACSCs and for the same major diagnostic category are currently under discussion for being potentially avoidable.13,37 In the present study, asthma was the most common ACSC and a respiratory problem was one of the most common major diagnostic categories encountered repeatedly across patients’ multiple readmissions. Ambulatory action plans that mitigate worsening respiratory illnesses have been successful in decreasing respiratory-related hospitalizations for asthma and other chronic lung diseases.22,38,39
There may be additional respiratory problems among children with CCCs that could be considered ambulatory care–sensitive but are not included within the current ACSC set. Multiple readmissions for aspiration pneumonia in a child with cerebral palsy may be considered care-sensitive if clinicians feel the readmissions are potentially reducible with optimized surgical and ambulatory reflux, digestive motility, and oromotor dysfunction management.40 Establishing a complementary set of ACSCs for children with CCCs that account for this (and other related) clinical situations and designate care management responsibilities between a child’s family and ambulatory health care providers may help inform strategies to identify and reduce potentially avoidable pediatric readmissions.
Our study has several limitations related to PHIS inpatient administrative data. Clinical data are preferable to uncover the true reasons for readmission and identify hospitalizations that are potentially avoidable. Although the diagnosis codes used to exclude planned chemotherapy admissions may have reputable accuracy,41 it is possible that some were unplanned and incorrectly excluded. Outpatient data were unavailable, including access to a medical home, long-term care facility, home nursing, case management, and respite care. Psychosocial factors were unavailable, including home environment stability and family empowerment of chronic illness self-management. Advanced directives with a do-not-hospitalize attribute were not available. We were unable to identify hospitalized children who died in settings beyond a PHIS hospital, such as at home. We could not identify situations where a patient was admitted to a non-PHIS hospital or to a different PHIS hospital, and therefore readmission frequency may be underestimated for some children.
A small number of patients with Medicaid-managed care may have been assigned to the commercial insurance category, underestimating the prevalence of Medicaid users. PHIS data contain hospital charge data that may not reflect the true cost of a hospitalization. The generalizability of the results may be limited to freestanding children’s hospitals. Our sample contains data from 37 of approximately 50 freestanding US children’s hospitals.42 Nationally, it is estimated that 25% of children’s hospitalizations occur within children’s hospitals.43 Children treated at children’s hospitals have a higher prevalence of single and multiple CCCs than children treated at other hospitals.44 Variation was present in the prevalence of patients experiencing recurrent readmissions among the hospitals. Individual hospitals may have their own distinctive discharge care planning and care coordination policies that influence readmission prevalence.
Despite these limitations, this study suggests that a small group of children is accounting for a substantial proportion of inpatient expenditures because they are experiencing recurrent readmissions. There is a need to monitor the number of times individual pediatric patients are readmitted over time so that children’s hospitals and outpatient providers within their local health care environments may understand the true reasons why many of these children are recurrently readmitted, which reasons are associated with contributory illness and health system problems that are ameliorable, and how to identify and help the children who are the most likely to experience future recurrent readmissions given the readmission frequency variation they may experience over time.
It is important to approach the entire continuum of care to best understand and optimally support children at risk for recurrent readmissions. Health care reform initiatives are underway to evaluate the shared accountability for patient outcomes and inpatient utilization among integrated community- and hospital-based clinician teams.45,46 Episode-of-care experiments with a bundled payment for inpatient surgical and outpatient posthospitalization care have been associated with improved patient outcomes, reduced hospital readmission up to 90 days after discharge, and reduced costs.47 Longer-term case management interventions within pediatric medical homes have lowered hospitalization rates in medically complex cases of children with neuromuscular CCCs and technology assistance.48 Further investigation of these strategies among pediatric patients at risk for recurrent readmissions may yield important insight on how to optimize the health and well-being of these children, reduce their readmissions, and keep them safe in their home and community environments.
Acknowledgments
Funding/Support: Dr Berry was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development career development award (K23 HD058092). Dr Kuo was supported by grant KL2RR029883 from the Arkansas Biosciences Institute National Health Center for Research Resources.
Role of the Sponsor: These funders had no role in the design and conduct of the study; in the collection, analysis, and interpretation of the data; or in the preparation, review, or approval of the manuscript.
Footnotes
Author Contributions: Dr Berry had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Berry, D. E. Hall, Kuo, Cohen, Agrawal, M. Hall, Kueser, Neff.
Acquisition of data: Agrawal, M. Hall.
Analysis and interpretation of data: Berry, D. E. Hall, Kuo, Cohen, Agrawal, Feudtner, M. Hall, Kueser, Kaplan.
Drafting of the manuscript: Berry, D. E. Hall, Cohen, Agrawal, M. Hall, Kaplan.
Critical revision of the manuscript for important intellectual content: Berry, D. E. Hall, Kuo, Cohen, Agrawal, Feudtner, Kueser.
Statistical analysis: Berry, D. E. Hall, Cohen, Agrawal, Feudtner, M. Hall.
Obtained funding: Berry, Kueser.
Administrative, technical, or material support: Kueser.
Conflict of Interest Disclosures: All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest and none were reported.
Additional Contributions: We thank Gordon Bass, MM, Children’s Memorial Hospital; Pat Hagan, MHSA, Seattle Children’s Hospital; Charles Schleien, MD, MBA, New York–Presbyterian Morgan Stanley Children’s Hospital; and David Miller, BS, MSM, The Children’s Medical Center of Dayton, for their help with the data analysis plan and results interpretation of this work. These persons did not receive compensation for their help with this work.
REFERENCES
- 1.Carrns A. Farewell, and don’t come back: health reform gives hospitals a big incentive to send patients home for good. US News World Rep. 2010;147(7):20–23. [PubMed] [Google Scholar]
- 2.Coye MJ. CMS’ stealth health reform: plan to reduce readmissions and boost the continuum of care. Hosp Health Netw. 2008;82(11):24. [PubMed] [Google Scholar]
- 3.Feudtner C, Levin JE, Srivastava R, et al. How well can hospital readmission be predicted in a cohort of hospitalized children? a retrospective, multicenter study. Pediatrics. 2009;123(1):286–293. doi: 10.1542/peds.2007-3395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mackie AS, Ionescu-Ittu R, Pilote L, Rahme E, Marelli AJ. Hospital readmissions in children with congenital heart disease: a population-based study. Am Heart J. 2008;155(3):577–584. doi: 10.1016/j.ahj.2007.11.003. [DOI] [PubMed] [Google Scholar]
- 5.Frei-Jones MJ, Field JJ, DeBaun MR. Multi-modal intervention and prospective implementation of standardized sickle cell pain admission orders reduces 30-day readmission rate. Pediatr Blood Cancer. 2009;53(3):401–405. doi: 10.1002/pbc.22048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Czaja AS, Zimmerman JJ, Nathens AB. Readmis-sion and late mortality after pediatric severe sepsis. Pediatrics. 2009;123(3):849–857. doi: 10.1542/peds.2008-0856. [DOI] [PubMed] [Google Scholar]
- 7.Berry JG, Graham DA, Graham RJ, et al. Predictors of clinical outcomes and hospital resource use of children after tracheotomy. Pediatrics. 2009;124(2):563–572. doi: 10.1542/peds.2008-3491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shah SS, Hall M, Slonim AD, Hornig GW, Berry JG, Sharma V. A multicenter study of factors influencing cerebrospinal fluid shunt survival in infants and children. Neurosurgery. 2008;62(5):1095–1102. doi: 10.1227/01.neu.0000325871.60129.23. [DOI] [PubMed] [Google Scholar]
- 9.Berry JG, Lieu TA, Forbes PW, Goldmann DA. Hospital volumes for common pediatric specialty operations. Arch Pediatr Adolesc Med. 2007;161(1):38–43. doi: 10.1001/archpedi.161.1.38. [DOI] [PubMed] [Google Scholar]
- 10.Hansagi H, Olsson M, Sjöberg S, Tomson Y, Göransson S. Frequent use of the hospital emergency department is indicative of high use of other health care services. Ann Emerg Med. 2001;37(6):561–567. doi: 10.1067/mem.2001.111762. [DOI] [PubMed] [Google Scholar]
- 11.Kne T, Young R, Spillane L. Frequent ED users: patterns of use over time. Am J Emerg Med. 1998;16(7):648–652. doi: 10.1016/s0735-6757(98)90166-8. [DOI] [PubMed] [Google Scholar]
- 12.Curtis P. “Frequent flyers” costing NHS £2.3bn pounds a year. [Accessed April 4, 2010];The Guardian. http://www.guardian .co.uk/uk/2006/feb/13/health.society.
- 13.Preventable hospitalizations: a window into primary and preventive care. [Accessed January 6, 2011];Agency for Healthcare Research and Quality. http://www.ahrq.gov/data/hcup/factbk5.
- 14.Institute of Medicine. Access to Health Care in America. Washington, DC: National Academy Press; 1993. Committee on Monitoring Access to Personal Health Care Services; Millman ML. [Google Scholar]
- [Accessed March 29, 2010];Child Health Corporation of America: a business alliance of hospitals. http://www.chca.com.
- 16.Goodman DM, Mendez E, Throop C, Ogata ES. Adult survivors of pediatric illness: the impact on pediatric hospitals. Pediatrics. 2002;110(3):583–589. doi: 10.1542/peds.110.3.583. [DOI] [PubMed] [Google Scholar]
- 17.Feudtner C, Christakis DA, Connell FA. Pediatric deaths attributable to complex chronic conditions: a population-based study of Washington State, 1980–1997. Pediatrics. 2000;106(1 pt 2):205–209. [PubMed] [Google Scholar]
- 18.Feudtner C, Hays RM, Haynes G, Geyer JR, Neff JM, Koepsell TD. Deaths attributed to pediatric complex chronic conditions: national trends and implications for supportive care services. Pediatrics. 2001;107(6):E99. doi: 10.1542/peds.107.6.e99. [DOI] [PubMed] [Google Scholar]
- 19.Feudtner C, Silveira MJ, Christakis DA. Where do children with complex chronic conditions die? patterns in Washington State, 1980–1998. Pediatrics. 2002;109(4):656–660. doi: 10.1542/peds.109.4.656. [DOI] [PubMed] [Google Scholar]
- 20.Buescher PA, Whitmire JT, Brunssen S, Kluttz-Hile CE. Children who are medically fragile in North Carolina: using Medicaid data to estimate prevalence and medical care costs in 2004. Matern Child Health J. 2006;10(5):461–466. doi: 10.1007/s10995-006-0081-3. [DOI] [PubMed] [Google Scholar]
- 21.Palfrey JS, Haynie M, Porter S, et al. Prevalence of medical technology assistance among children in Massachusetts in 1987 and 1990. Public Health Rep. 1994;109(2):226–233. [PMC free article] [PubMed] [Google Scholar]
- 22.Bhogal S, Zemek R, Ducharme FM. Written action plans for asthma in children. Cochrane Database Syst Rev. 2006;3:CD005306. doi: 10.1002/14651858.CD005306.pub2. [DOI] [PubMed] [Google Scholar]
- 23.Lubell J. MedPAC targets readmissions: but savings options concern industry executives. Mod Healthc. 2007;37(26):37–38. [PubMed] [Google Scholar]
- 24.Consumer Price Index. [Accessed January 3, 2011];US Bureau of Labor Statistics. http://data.bls.gov/cgi-bin/surveymost?cu.
- 25.Frei-Jones MJ, Field JJ, DeBaun MR. Risk factors for hospital readmission within 30 days: a new quality measure for children with sickle cell disease. Ped-atr Blood Cancer. 2009;52(4):481–485. doi: 10.1002/pbc.21854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Beck CE, Khambalia A, Parkin PC, Raina P, Macarthur C. Day of discharge and hospital readmission rates within 30 days in children: a population-based study. Paediatr Child Health. 2006;11(7):409–412. doi: 10.1093/pch/11.7.409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360(14):1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 28.Lye PS. American Academy of Pediatrics; Committee on Hospital Care and Section on Hospital Medicine. Clinical report: physicians’ roles in coordinating care of hospitalized children. Pediatrics. 2010;126(4):829–832. doi: 10.1542/peds.2010-1535. [DOI] [PubMed] [Google Scholar]
- 29.Srivastava R, Stone BL, Murphy NA. Hospitalist care of the medically complex child. Pediatr Clin North Am. 2005;52(4):1165–1187. doi: 10.1016/j.pcl.2005.03.007. [DOI] [PubMed] [Google Scholar]
- 30.Kripalani S, Jackson AT, Schnipper JL, Coleman EA. Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists. J Hosp Med. 2007;2(5):314–323. doi: 10.1002/jhm.228. [DOI] [PubMed] [Google Scholar]
- 31.Stone BL, Murphy NA, Mundorff MB, Parker HB, Peterson PR, Srivastava R. Children with chronic complex medical illnesses: is inpatient care family-centered? J Pediatr Rehabil Med. 2008;1(3):237–243. [PMC free article] [PubMed] [Google Scholar]
- 32.Sneed RC, May WL, Stencel C. Physicians’ reliance on specialists, therapists, and vendors when prescribing therapies and durable medical equipment for children with special health care needs. Pediatrics. 2001;107(6):1283–1290. doi: 10.1542/peds.107.6.1283. [DOI] [PubMed] [Google Scholar]
- 33.Sneed RC, May WL, Stencel C. Policy versus practice: comparison of prescribing therapy and durable medical equipment in medical and educational settings. Pediatrics. 2004;114(5):e612–e625. doi: 10.1542/peds.2004-1063. [DOI] [PubMed] [Google Scholar]
- 34.Massin MM, Montesanti J, Ge´ rard P, Lepage P. Children with chronic conditions in a paediatric emergency department. Acta Paediatr. 2006;95(2):208–213. doi: 10.1080/08035250500346443. [DOI] [PubMed] [Google Scholar]
- 35.Reynolds S, Desguin B, Uyeda A, Davis AT. Children with chronic conditions in a pediatric emergency department. Pediatr Emerg Care. 1996;12(3):166–168. doi: 10.1097/00006565-199606000-00005. [DOI] [PubMed] [Google Scholar]
- 36.Young NL, Barden WS, Mills WA, Burke TA, Law M, Boydell K. Transition to adult-oriented health care: perspectives of youth and adults with complex physical disabilities. Phys Occup Ther Pediatr. 2009;29(4):345–361. doi: 10.3109/01942630903245994. [DOI] [PubMed] [Google Scholar]
- 37.Report to the Congress: Promoting Greater Efficiency in Medicine. Medicare Payment Advisory Commission; [Accessed January 6, 2011]. http://www.medpac.gov/documents/jun07_entirereport.pdf. [Google Scholar]
- 38.Turnock AC, Walters EH, Walters JA, Wood-Baker R. Action plans for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2005;(4):CD005074. doi: 10.1002/14651858.CD005074.pub2. [DOI] [PubMed] [Google Scholar]
- 39.Rice KL, Dewan N, Bloomfield HE, et al. Disease management program for chronic obstructive pulmonary disease: a randomized controlled trial. AmJ Respir Crit Care Med. 2010;182(7):890–896. doi: 10.1164/rccm.200910-1579OC. [DOI] [PubMed] [Google Scholar]
- 40.Srivastava R, Berry JG, Hall M, et al. Reflux related hospital admissions after fundoplication in children with neurological impairment: retrospective cohort study. BMJ. 2009;339:b4411. doi: 10.1136/bmj.b4411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Aiello Bowles EJ, Tuzzio L, Ritzwoller DP, et al. Accuracy and complexities of using automated clinical data for capturing chemotherapy administrations: implications for future research. Med Care. 2009;47(10):1091–1097. doi: 10.1097/MLR.0b013e3181a7e569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [Accessed January 13, 2011];National Association of Children’s Hospitals and Related Institutions. http://www.childrenshospitals.net.
- 43.National Statistics on Children. [Accessed January 13, 2011];Healthcare Cost and Utilization Project; Agency for Healthcare Research and Quality. http://www.hcupnet.ahrq.gov/
- 44.Simon TD, Berry J, Feudtner C, et al. Children with complex chronic conditions in inpatient hospital settings in the United States. Pediatrics. 2010;126(4):647–655. doi: 10.1542/peds.2009-3266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Moore KD, Coddington DC. Accountable care: the journey begins. Healthc Financ Manage. 2010;64(8):57–63. [PubMed] [Google Scholar]
- 46.Guterman S, Davis K, Stremikis K, Drake H. Innovation in Medicare and Medicaid will be central to health reform’s success. Health Aff (Millwood) 2010;29(6):1188–1193. doi: 10.1377/hlthaff.2010.0442. [DOI] [PubMed] [Google Scholar]
- 47.Berry SA, Doll MC, McKinley KE, Casale AS, Bothe A., Jr ProvenCare: quality improvement model for designing highly reliable care in cardiac surgery. Qual Saf Health Care. 2009;18(5):360–368. doi: 10.1136/qshc.2007.025056. [DOI] [PubMed] [Google Scholar]
- 48.Palfrey JS, Sofis LA, Davidson EJ, Liu J, Freeman L, Ganz ML. Pediatric Alliance for Coordinated Care. The Pediatric Alliance for Coordinated Care: evaluation of a medical home model. Pediatrics. 2004;113(5) suppl:1507–1516. [PubMed] [Google Scholar]