Hydrogen sulfide and nitric oxide are mutually dependent in the regulation of angiogenesis and endothelium-dependent vasorelaxation (original) (raw)
Abstract
Hydrogen sulfide (H2S) is a unique gasotransmitter, with regulatory roles in the cardiovascular, nervous, and immune systems. Some of the vascular actions of H2S (stimulation of angiogenesis, relaxation of vascular smooth muscle) resemble those of nitric oxide (NO). Although it was generally assumed that H2S and NO exert their effects via separate pathways, the results of the current study show that H2S and NO are mutually required to elicit angiogenesis and vasodilatation. Exposure of endothelial cells to H2S increases intracellular cyclic guanosine 5′-monophosphate (cGMP) in a NO-dependent manner, and activated protein kinase G (PKG) and its downstream effector, the vasodilator-stimulated phosphoprotein (VASP). Inhibition of endothelial isoform of NO synthase (eNOS) or PKG-I abolishes the H2S-stimulated angiogenic response, and attenuated H2S-stimulated vasorelaxation, demonstrating the requirement of NO in vascular H2S signaling. Conversely, silencing of the H2S-producing enzyme cystathionine-γ-lyase abolishes NO-stimulated cGMP accumulation and angiogenesis and attenuates the acetylcholine-induced vasorelaxation, indicating a partial requirement of H2S in the vascular activity of NO. The actions of H2S and NO converge at cGMP; though H2S does not directly activate soluble guanylyl cyclase, it maintains a tonic inhibitory effect on PDE5, thereby delaying the degradation of cGMP. H2S also activates PI3K/Akt, and increases eNOS phosphorylation at its activating site S1177. The cooperative action of the two gasotransmitters on increasing and maintaining intracellular cGMP is essential for PKG activation and angiogenesis and vasorelaxation. H2S-induced wound healing and microvessel growth in matrigel plugs is suppressed by pharmacological inhibition or genetic ablation of eNOS. Thus, NO and H2S are mutually required for the physiological control of vascular function.
Nitric oxide (NO) and hydrogen sulfide (H2S) are two endogenous gasotransmitters whose regulatory roles in the cardiovascular system include vasorelaxation and stimulation of angiogenesis (1, 2). In endothelial cells, NO is synthesized by the endothelial isoform of NO synthase (eNOS). The principal pathway of NO signaling involves binding to the heme moiety of the soluble guanylyl cyclase (sGC) and production of the second messenger cyclic guanosine 5′-monophosphate (cGMP), followed by the activation of protein kinase G (PKG) (3, 4). However, vascular H2S is generated from l-cysteine by two pyridoxal 5′-phosphate–dependent enzymes, cystathionine-β-synthase (CBS) and cystathionine-γ-lyase (CSE), and by the combined action of cysteine aminotransferase (CAT) and 3-mercaptopyruvate sulfurtransferase (3-MST); activation of the ATP-dependent potassium channel (KATP channel), modulation of cell metabolism, and posttranslational protein modifications via sulfhydration have been identified as some of its key signaling pathways (5–7).
It is generally assumed that the signaling pathways of NO and H2S are independent. In the present study, we describe the unexpected observations showing that the angiogenic and vasorelaxant effects of NO and H2S are dependent on each other's presence. These findings shine a light on the physiological control of vascular tone and have significant implications for the pathogenetic and therapeutic roles of both NO and H2S.
Results
H2S-Induced Angiogenesis Requires NO Biosynthesis.
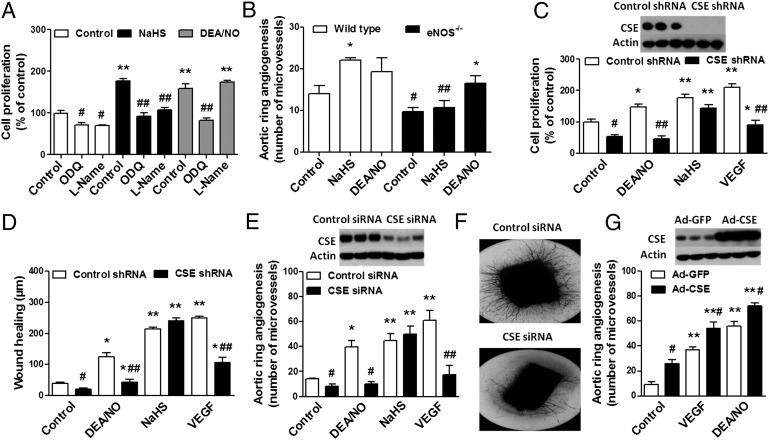
H2S resulted in a concentration-dependent increase in bEnd3 microvascular endothelial cell proliferation (Fig. S1_A_) and migration (Fig. S1 B and C), as well as microvessel sprouting from rat aortic rings (Fig. S1_D_). Similarly, l-cysteine, the substrate of CSE, induced a dose-dependent angiogenic response in vitro (Fig. S2). The sGC inhibitor 1H-[1,2,4]oxadiazolo[4,3,-a]quinoxalin-1-one (ODQ) inhibited both H2S-induced and NO-induced angiogenesis (Fig. 1_A_). Inhibition of endothelial NO biosynthesis with l-NAME abolished the H2S-induced proliferation (Fig. 1_A_). Moreover, aortic rings harvested from eNOS−/− mice exhibited no microvessel outgrowth in response to NaHS, compared with wild-type controls (Fig. 1_B_). These findings demonstrate the absolute requirement of NO in the angiogenic effect of H2S.
Fig. 1.
Mutual requirement of NO and H2S for angiogenesis in vitro. (A) bEnd3 cells were seeded overnight in 12-well plates, pretreated with ODQ (10 μM, 2 h) or l-NAME (4 mM, 40 min), and subsequently incubated with NaHS (30 μM) or DEA/NO (10 μM) for an additional 48 h. Cells were trypsinized and counted using a Neubauer hemocytometer. **P < 0.01 vs. control; ##P < 0.01 vs. NaHS. (B) Aortic rings were harvested from wild-type or eNOS−/− mice, cultured for 7 d in collagen gel in Opti-MEM medium containing 1% FBS, in the presence or absence of NaHS (30 μM) or DEA/NO (10 μM). *P < 0.05 vs. corresponding control; #P < 0.05 and ##P < 0.01 vs. corresponding wild type. (C) The lentiviral shRNA vector targeting CSE was transfected into bEnd3 cells. The shRNA vector effectively inhibited the expression of CSE gene in bEnd3 cell line at the protein level, as shown by Western blot analysis (C Upper). Following CSE silencing, cells were seeded in 12-well cell culture plates, and cell proliferation (C) and wound healing (D) were then evaluated in the presence of vehicle, DEA/NO (10 μM), NaHS (30 μM), or VEGF (20 ng/mL). *P < 0.05 and **P < 0.01 vs. control; #P < 0.05 and ##P < 0.01 vs. corresponding control shRNA. (E) Rat aortic rings were silenced with CSE siRNA for 48 h. Following gene silencing, aortic explants were placed individually on the bottom of 24-well plates, and collagen gel was gently applied. Rings were cultured for 7 d in the presence of vehicle, DEA/NO (10 μM), NaHS (30 μM), or VEGF (20 ng/mL). Western blots confirm efficient CSE silencing in aortic rings. CSE silencing markedly reduced both VEGF- and DEA/NO-induced vessel sprouting. *P < 0.05 and **P < 0.01 vs. control; #P < 0.05 and ##P < 0.01 vs. corresponding control siRNA. (F) Representative images of the 7-d collagen gel cultures of aortic rings exposed to VEGF following CSE gene silencing. (G) Aortic rings were exposed to adenovirus expressing GFP or CSE before embedding in collagen gel. Overexpression of CSE enhanced VEGF- or DEA/NO-induced neovessel growth. **P < 0.01 vs. control; #P < 0.05 vs. corresponding Ad-GFP. (Upper) Representative Western blot for CSE protein in rings exposed to adenovirus expressing GFP or CSE.
NO-Induced Angiogenesis Requires H2S Biosynthesis.
Silencing of CSE in bEnd3 cells with shRNA resulted in a complete inhibition of the in vitro angiogenic response to the NO donor 2-(N,N-diethylamino)-diazenolate-2-oxide, diethylammonium salt (DEA)/NO (Fig. 1 C and D). As expected, CSE silencing failed to affect endothelial cell proliferation and migration in response to authentic H2S (Fig. 1 C and D), but attenuated the angiogenic effect of the CSE substrate l-cysteine (Fig. S3). The angiogenic effect of VEGF was also markedly reduced, whereas that of basic FGF (bFGF) was unaffected by CSE silencing (Fig. 1 C and D and Fig. S3). Similar results were obtained by CSE down-regulation using siRNA in rat aortic rings. CSE knockdown resulted in reduced sprout formation in the aortic ring assay in responses to VEGF and DEA/NO (Fig. 1 E and F). However, CSE overexpression was proangiogenic; adenoviral mediated up-regulation of CSE in rat aortic ring explants significantly enhanced the outgrowth of branching microvessels (Fig. 1_G_).
H2S- and NO-Induced Angiogenesis Converges on the cGMP/PKG Pathway.
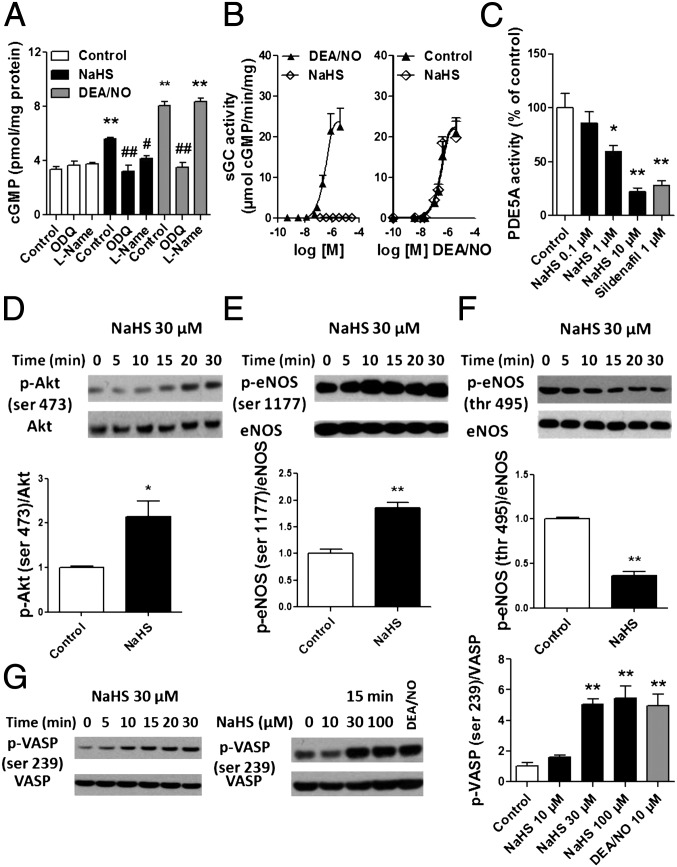
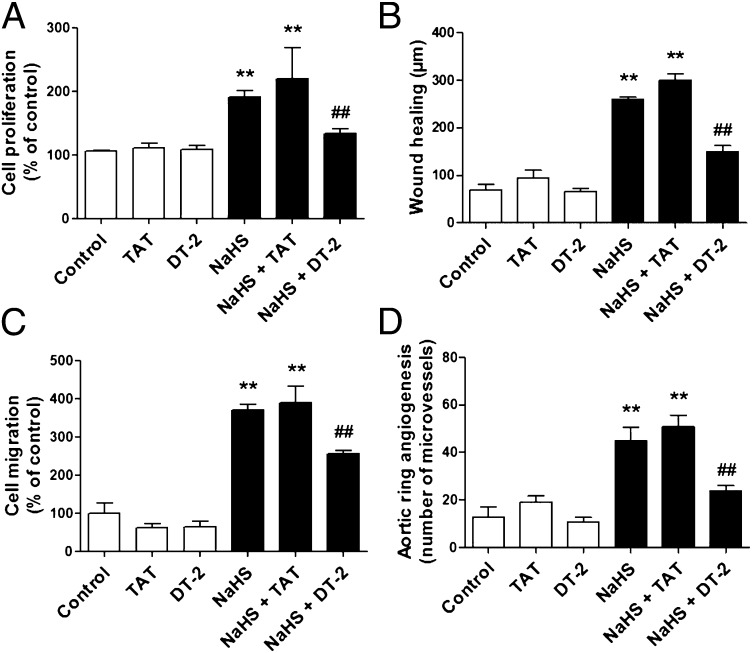
Pharmacological inhibition of sGC with ODQ prevented both the H2S- and the NO-induced angiogenic response (Fig. 1_A_) and significantly reduced the endothelial cell cGMP levels (Fig. 2_A_). H2S had no significant effect on purified human recombinant sGC activity, and did not affect DEA/NO-induced sGC activation (Fig. 2_B_). However, using purified PDE5A, sodium hydrosulfide (NaHS) was found to concentration-dependently inhibit cGMP degrading activity, with an IC50 of 1.55 μΜ (Fig. 2_C_). H2S also stimulated Akt phosphorylation at its activating site (Ser493), increased the phosphorylation of eNOS at Ser1177, and reduced the phosphorylation of eNOS at Thr495 (Fig. 2 D–F). Both H2S and NO induced the phosphorylation of VASP, a marker of PKG activation (Fig. 2_G_). These findings are consistent with a working model where H2S-mediated eNOS phosphorylation increases the catalytic activity of eNOS, whereas H2S-mediated inhibition of phosphodiesterase (PDE) amplifies the resulting intracellular cGMP response, culminating in a cooperative downstream activation of PKG. The functional importance of this cooperative PKG activation is evidenced by the fact that PKG-I inhibitor peptide DT-2 attenuated the angiogenic response to H2S (Fig. 3).
Fig. 2.
H2S and NO signaling converge on the cGMP/PKG pathway. (A) bEnd3 cells were pretreated with l-NAME (4 mM, 40 min) or ODQ (10 μM, 2 h). Following pretreatments, cells were washed twice with Hanks’ balanced salt solution and then exposed for 3 min to NaHS at the indicated concentrations. cGMP was extracted in 0.1 M HCl and measured by enzyme immunoassay. **P < 0.01 vs. control; #P < 0.05 and ##P < 0.01 vs. corresponding control. (B) sGC enzymatic activity was assayed using [α-32P]GTP to [32P]cGMP conversion assay in response to the indicated concentrations of NaHS or DEA/NO. To test whether H2S affects NO-induced sGC activation, the effect of increasing concentrations of DEA/NO on sGC activity was assessed in the presence or absence of 10 μM NaHS. (C) PDE5A activity was measured in the presence of the indicated concentrations of NaHS or 1 μM sildenafil, as a positive control. *P < 0.05 or **P < 0.01 vs. control. bEnd3 cells were exposed to NaHS at the indicated concentrations and time. Cell lysates were analyzed by SDS/PAGE. PVDF membranes were blotted by using rabbit polyclonal antibodies against phosphorylated (Ser473) or total Akt (D); phosphorylated (Ser1177) or total eNOS (E); phosphorylated (Thr495) or total eNOS (F); and phosphorylated (Ser239) or total VASP (G). Densitometric analysis was performed on three blots from three different experiments using image analysis software. *P < 0.05 and **P < 0.01 NaHS (30 min) vs. control.
Fig. 3.
PKG-I inhibition prevents H2S-induced in vitro angiogenesis. (A) bEnd3 cells were pretreated with vehicle, DT-2 peptide (1 μM, 20 min), or the control peptide (TAT) (1 μM, 20 min) and then stimulated with NaHS (30 μM) to induce cell proliferation. The effect of DT-2 on NaHS-induced response was also estimated in wound healing (B) and cell migration (C). **P < 0.01 vs. control; ##P < 0.01 vs. NaHS + TAT. (D) Aortic ring explants were embedded in collagen gel, treated with the control peptide (TAT) or DT-2 (1 μM), and cultured for 7 d in the presence or absence of NaHS (30 μM, applied every 8 h). P < 0.01 vs. control; ##P < 0.01 vs. NaHS + TAT.
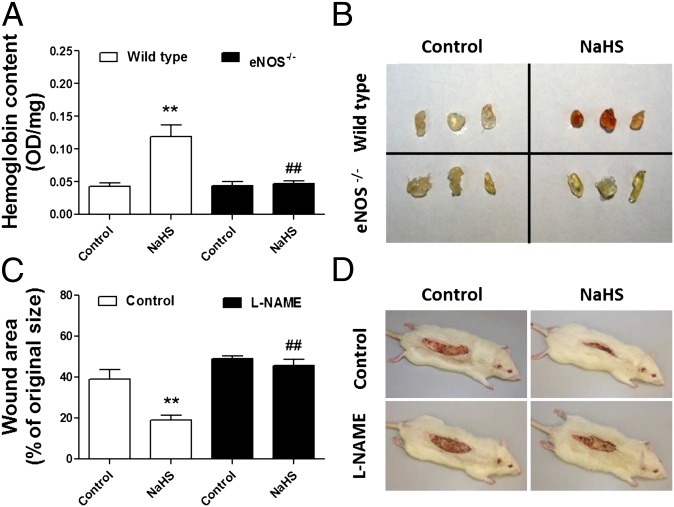
Endogenous NO Production Is Required for H2S-Induced Angiogenic Response in Vivo.
Intraperitoneal injection of NaHS caused a sustained increase in neovascularization in matrigel plugs implanted in wild-type mice, whereas this proangiogenic effect was completely absent in eNOS−/− mice (Fig. 4 A and B). Because wound healing is dependent on angiogenesis, we next assessed the ability of NaHS to facilitate wound closure in a burn wound injury. Skin wound sizes, measured by planimetry at day 28, were markedly reduced in rats receiving daily topical administrations of NaHS, and this effect was abolished by the eNOS inhibitor l-NAME (Fig. 4 C and D).
Fig. 4.
In vivo relevance for the interdependence of H2S and NO on angiogenesis. (A) The effect of H2S on angiogenesis in vivo was assessed by Matrigel plug assay in wild-type or eNOS−/− mice. Neovascularization in the matrigel plugs was quantified by measuring hemoglobin content using Drabkin’s reagent. NaHS treatments (50 μmol/kg per day) significantly promoted neovascularization in the Matrigel plugs in wild-type mice. The effect of NaHS treatment was abolished in mice lacking eNOS. **P < 0.01 vs. control; ##P < 0.01 vs. corresponding wild type. (B) Images of the Matrigel plugs immediately after collection from wild-type and eNOS−/− mice. (C) Following anesthesia and analgesia, rats were placed in a mold and subjected to burn injury by submerging the back in scalding (96–99 °C) water for 10 s. Rats were randomly divided into four groups and treated daily for 28 d either with vehicle or NaHS (300 μg/kg per day s.c.). Rats from l-NAME groups received daily s.c. injections of the eNOS inhibitor (20 mg/kg). Subcutaneous injections of NaHS were performed twice daily at four equally spaced sites in the transition zone between burn site and healthy tissue. Burn wound area was determined on day 28 by planimetry. *P < 0.05 vs. control; ##P < 0.01 vs. corresponding control. (D) Representative images of the skin wounds at 28 d.
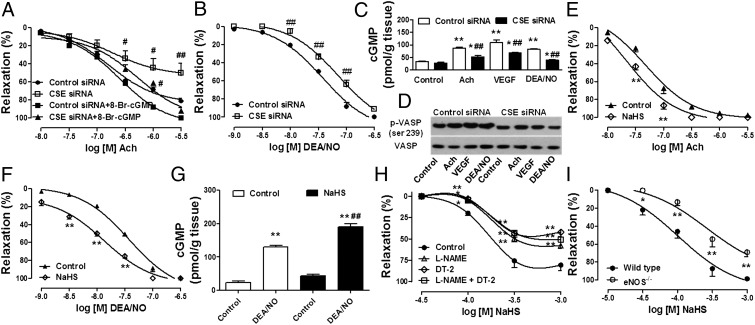
H2S- and NO-Induced Vasorelaxation Is Cooperative and Converges on the cGMP Pathway.
Silencing of CSE resulted in a significant inhibition of the vasodilatory responses of vascular rings to acetylcholine and to DEA/NO (Fig. 5 A and B and Fig. S4) and suppressed the vasorelaxant effect of VEGF (Fig. S5). Exogenously applied cell-permeable cGMP (8-Br-cGMP, 10 μM) restored endothelium-dependent relaxation responses on the background of CSE silencing (Fig. 5_A_). CSE silencing in aortic rings also resulted in reduced acetylcholine-, VEGF-, or DEA/NO-induced elevations in vascular cGMP and VASP phosphorylation (Fig. 5 C and D). H2S replacement during siRNA transfection (NaHS 30 μM, at 8-h intervals) partially restored the ability of acetylcholine to elevate cGMP levels in aortic rings subjected to CSE silencing (Fig. S6). Furthermore, pretreatment of aortic rings with a low concentration of NaHS (30 μM, 15 min) potentiated the vasorelaxant response to acetylcholine and DEA/NO (Fig. 5 E and F) and significantly increased cGMP levels in response to DEA/NO (Fig. 5_G_). Both l-NAME and DT-2 exerted a significant inhibitory effect on the NaHS-induced concentration-response curves, without having any additive effect (Fig. 5_H_ and Fig. S4). Thoracic aortic rings from eNOS−/− mice were less sensitive to the vasorelaxant action of exogenous NaHS than wild-type controls (Fig. 5_I_). Nevertheless, plasma H2S levels, as well as CSE expression and activity in thoracic aortic lysates were comparable in the two groups of mice (Fig. S7), indicating that the absence of eNOS does not induce any compensatory up-regulation of H2S production.
Fig. 5.
Requirement of simultaneous production of H2S and NO in vasorelaxation. Cumulative-concentration response curves to acetylcholine (A) or DEA/NO (B) were performed in aortic rings incubated in isolated organ baths following siRNA-mediated silencing of CSE. ##P < 0.01 vs. control siRNA. To test the effect of cGMP elevation on acetylcholine induced vasorelaxation, cell-permeable cGMP (8-Br-cGMP) was applied at 10 μM concomitantly to cumulative acetylcholine administrations. (C) Aortic rings subjected to CSE gene silencing were stimulated with acetylcholine (1 μM), DEA/NO (0.1 μM), or VEGF (50 ng/mL) for 15 min. At the end of the incubation time, cGMP was extracted and measured by enzyme immunoassay. **P < 0.01 vs. control; ##P < 0.01 vs. corresponding control siRNA. (D) Following CSE gene targeting (siRNA), aortic rings were incubated in Krebs–Henseleit buffer at 37 °C and stimulated with acetylcholine (1 μM, 15 min), DEA/NO (0.1 μM, 15 min), or VEGF (50 ng/mL, 15 min). Tissue lysates were analyzed by SDS/PAGE. PVDF membranes were blotted by using rabbit polyclonal antibodies against phosphorylated (ser 239) or total VASP. (E) Aortic rings were incubated with NaHS 30 μM on PE-induced stable tone. Concentration response curves to acetylcholine (E) or DEA/NO (F) were performed. In these settings, NaHS enhances the vasorelaxant properties of endothelium-derived or exogenously applied NO. **P < 0.01 vs. control. Similarly, 15-min exposure of aortic rings to a low concentration of NaHS (30 μM) enhanced DEA/NO-induced elevation of intracellular cGMP as assessed by enzyme immunoassay (G). (H) Aortic rings were mounted in organ baths, pretreated with vehicle, l-NAME (100 μM), DT-2 (1 μM), or l-NAME + DT-2 on basal tone for 30 min. Rings were then challenged with PE (1 μM), and concentration response curves to NaHS were performed on stable tone. *P < 0.05 and *P < 0.01 vs. control. (I) Aortic tissues were dissected from wild-type and eNOS−/− mice and placed in isolated organ baths under a resting tension of 1.5 g. Following a stabilization period, aortic rings were challenged with PE (1 μM), and cumulative concentration response curves to NaHS were performed. *P < 0.05 and **P < 0.01 vs. wild type.
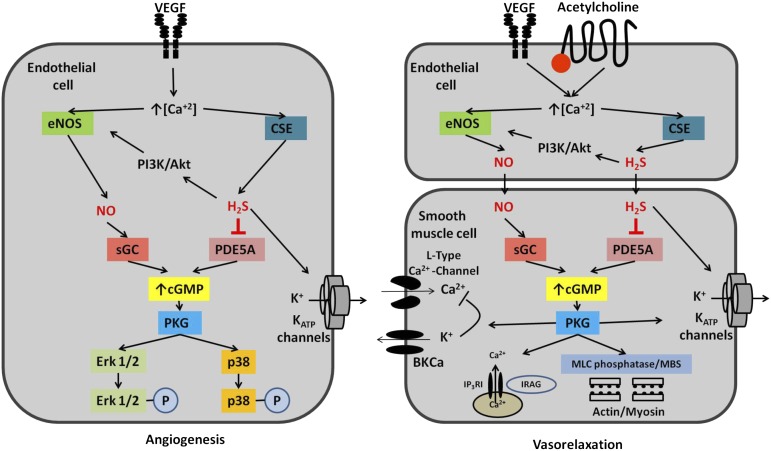
H2S and NO Interactions: Working Hypothesis.
Based on the current data, we put forward the working hypothesis that VEGF (via VEGF receptor activation) or acetylcholine (via muscarinic receptor activation) increases intracellular calcium levels, leading to eNOS activation, increased NO production, soluble guanylyl cyclase activation, and increased cGMP synthesis (Fig. 6). At the same time, VEGF and acetylcholine receptor activation triggers Ca2+/calmodulin-dependent activation of CSE. (In fact, we have observed that Ca2+/calmodulin complex induces an approximate twofold increase in l-cysteine–induced H2S production from purified human recombinant CSE; Fig. S8.) H2S production also activates the PI3K/Akt pathway, leading to eNOS phosphorylation and increased eNOS activation. Moreover, H2S inhibits cGMP-degrading phosphodiesterases, thereby leading to a stabilization of NO-induced intracellular cGMP levels. Both NO-induced sGC activation and H2S-induced inhibition of PDE is essential for the physiological control of angiogenesis and vascular relaxation. The sustained elevation in cellular cGMP levels, in turn, activates cGMP-dependent protein kinase (PKG), thereby mediating angiogenesis and endothelium-dependent vasorelaxation (Fig. 6).
Fig. 6.
Proposed pathways of H2S and NO interaction. Cooperation between NO and H2S in angiogenesis (Left) or endothelium-dependent vasorelaxation (Right). Binding of VEGF or acetylcholine to its receptor on the endothelial cell mobilizes intracellular calcium and activates eNOS as well as CSE (two calcium-dependent enzymes), resulting in a simultaneous elevation of intracellular NO and H2S levels in endothelial cells (in the context of angiogenesis) or in the smooth muscle cell (in the context of vasorelaxation). NO stimulates guanylyl cyclase, whereas endogenously produced H2S maintains a tonic inhibitory effect on PDE5, thereby delaying the degradation of cGMP and permitting physiological cGMP signaling. These two simultaneous actions ensure that cGMP has a sufficiently long half-life to activate PKG to stimulate PKG-dependent downstream signaling such as ERK1/2 and p38 in the case of angiogenesis and myosin light chain (MLC) phosphatase (via its myosin-binding subunit, MBS), large-conductance calcium- and voltage-activated potassium channels (BKCa), and IP3-R-–associated cG-kinase substrate (IRAG) in the case of smooth muscle relaxation. NO and H2S are also known to activate KATP channels, which are also involved in angiogenesis and endothelium-dependent relaxation.
Discussion
Although it is generally assumed that NO and H2S use unique signaling pathways, the current results demonstrate an unexpected level of cooperation between these signaling pathways, converging at the level of PKG to promote angiogenesis and vasorelaxation. The mutual reliance of these two gasotransmitters on each other is almost absolute in the case of angiogenesis (because blocking eNOS completely abrogates the angiogenic effects of H2S, whereas silencing of H2S markedly reduces the angiogenic effect of NO).
The functional role of cGMP in endothelial cells’ angiogenesis in response to NO and H2S is supported by the findings showing that (i) the sGC inhibitor ODQ inhibits both H2S-induced and NO-induced angiogenesis; (ii) both H2S and NO activate PKG and its cellular signaling, as evidenced by phosphorylation of VASP, a marker of PKG activation, and (iii) pharmacological blockade of PKG-I abolishes the angiogenic effects of both H2S and NO. These findings place PKG at an important junction in the regulation of angiogenesis, and suggest that pharmacological inhibition of this enzyme may be a potentially powerful approach for the therapeutic inhibition of angiogenesis.
In line with recent evidence that H2S increases cellular cGMP by inhibiting PDE activity (8), we found that NaHS concentration-dependently decreases the activity of purified PDE5A. These findings suggest that the H2S-induced increase in endothelial cell cGMP levels is due to reduced cGMP degradation. This mode of the cooperative action between H2S and NO in the control of angiogenesis is similar to the interaction between NO and the pharmacological PDE5 inhibitors (e.g., sildenafil and tadalafil), where the initial signaling of NO on soluble guanylyl cyclase is amplified as PDE5 inhibition blocks the degradation of cGMP and maintains high intracellular levels of the cyclic nucleotide (9).
The finding that l-NAME or eNOS deficiency abolishes the ability of H2S to increase cGMP levels or to induce angiogenesis in vitro or in vivo suggests that the biosynthesis of NO is an absolute requirement for H2S to exert its vascular effects. Based on the current data, we conclude that H2S, on its own (in the absence of NO), is unable to stimulate angiogenesis because it does not induce sufficient increases in cGMP levels (consistent with findings showing that it does not directly activate sGC). Another significant synergistic interaction between H2S and eNOS occurs at the level of eNOS phosphorylation. In line with previous reports (10), our data show that H2S stimulates Akt in endothelial cells, and induces eNOS activation through phosphorylation of the activating site Ser1177 and dephosphorylation at the inhibitory site Thr495. Based on our knowledge of the functional role of these amino acids in the regulation of eNOS (11, 12), the responses induced by H2S are highly consistent with the stimulation of the catalytic activity of eNOS.
Another unique finding that emerged from our angiogenesis studies is the dependence of the NO-induced responses on endogenous H2S biosynthesis. CSE silencing almost completely abrogates DEA/NO-stimulated cGMP accumulation and PKG activation, leading to an almost complete blockade of the proangiogenic effect of NO. As expected, CSE-silenced cells do not respond to l-cysteine, but maintain the expected migration and proliferation in response to NaHS, indicating that the downstream signaling pathways of H2S remain intact in CSE shRNA cells.
Studies from several laboratories have demonstrated the dependence of the prototypical angiogenic hormone VEGF responses on NO (13, 14) or H2S (15, 16) biosynthesis. The results of the current study suggest that VEGF simultaneously triggers the release of both gasotransmitters from endothelial cells, which, in turn, work in an orchestrated manner to enhance cGMP levels above a critical threshold to trigger PKG activation, thereby initiating new blood vessel growth. VEGF signaling involves intracellular calcium mobilization (14), which is an obligatory early step for the activation of both eNOS and CSE (11, 17). The finding that VEGF-stimulated in vitro sprouting is reduced in blood vessels after CSE silencing, whereas it is enhanced in vessels overexpressing CSE, indicates that endogenous H2S production by CSE is a dynamic regulator of angiogenesis. In contrast to VEGF, it has been shown that NO production does not significantly contribute to the angiogenesis-promoting effect of bFGF, whose downstream pathways are independent from NO/cGMP (18, 19). It is, therefore, consistent with our other observations that CSE knockdown does not inhibit FGF-induced proliferation and wound healing.
cGMP-dependent protein kinase (PKG) is known to contribute to the angiogenic response to NO donors, soluble guanylyl cyclase activators, PDE5 inhibitors, and VEGF (20–22). Accordingly, the present findings clearly demonstrate that H2S elicits the phosphorylation of the PKG substrate protein VASP. The finding that the PKG-I inhibitor DT-2 causes a near-complete attenuation of proliferation, migration, and sprouting suggests that activation of PKG is the final common pathway on which the actions of NO and H2S converge.
Given our findings showing the mutual requirement of NO and H2S in angiogenesis, we next investigated whether a similar relationship also exists in the control of vasorelaxation. The finding that the relaxation-response curves to NaHS are shifted to the right in vascular rings from eNOS−/− mice indicates that the vasorelaxant action of H2S, similar to its angiogenic action, requires, at least in part, the presence of endogenously produced NO. The finding that vasodilatory response to NaHS is inhibited by ODQ (23), l-NAME, or DT-2 further supports this conclusion. It is important to point out, however, that in contrast to the angiogenic response, the vasorelaxant effect of H2S is not completely blocked by NOS inhibition or PKG-I inhibition. These responses likely involve parallel pathways of H2S-induced vasorelaxation, such as KATP channels (24, 25) and other types of potassium channels and the ion exchangers (17).
The current results also point to the significant requirement of H2S to the vasorelaxant effect of NO. First, CSE silencing decreases the vasorelaxant effect of the NO donor DEA/NO. Second, CSE silencing attenuates the relaxant effect of the classical endothelium-dependent vasodilator acetylcholine. Third, addition of a low (nonvasorelaxant) concentration of NaHS potentiates the effect of DEA/NO or acetylcholine. The fact that CSE silencing attenuates the NO donor-induced cGMP accumulation and VASP phosphorylation suggests that—similar to the responses observed in the angiogenesis assays—a significant part of the cooperative effect of NO and H2S in vascular relaxation is related to H2S-mediated PDE inhibition. Again, it is important to point out that the vasorelaxant effect of NO or acetylcholine was attenuated, but not completely blocked, by CSE silencing. This finding points to the existence of parallel pathways of NO-induced vasorelaxation, either by NO-mediated activation of KATP channels or by an H2S-independent activation of PKG by NO. The latter mechanism is consistent with our findings showing that in the vascular smooth muscle cell (in contrast to the endothelial cell) the NO donor can still induce a significant degree of residual cGMP elevation even after CSE is silenced. The current findings are in line with prior findings showing that the metacholine-induced vascular relaxations were attenuated in vascular rings from the CSE−/− mice (26), but offer a different mechanism to explain this observation. The finding that the acetylcholine-induced relaxations are inhibited more by CSE deficiency than the relaxations by NO donors may be related to the fact that acetylcholine, via endothelial calcium mobilization, may stimulate endothelial H2S release, resulting in a more pronounced inhibition of PDE5 in the vascular smooth muscle. (However, NO donors do not mobilize endothelial calcium and would not be expected to stimulate endothelial H2S production.)
The biological interactions of NO and H2S are complex, involve multiple pathways, and are dependent on the vascular bed, species, and experimental condition (27–30). Nevertheless, the current results, obtained in two standard experimental models of vascular biology, suggest that (i) there is a hitherto unrecognized degree of cooperative interaction between H2S and NO in the vascular system; (ii) there is a mutual requirement of these mediators to maintain vascular homeostasis, and (iii) the interactions of NO and H2S have several levels (eNOS activity, PDE activity) that ultimately converge at the level of intracellular cGMP and, further downstream, PKG activation.
The in vivo relevance of the above interaction illustrated by the finding that the angiogenic effect of H2S, as well as its effect to promote wound healing, is completely lost in the absence of functional eNOS. The present findings may also offer a mechanistic explanation to prior observations noting that the beneficial effects of H2S during cardiac arrest are absent in eNOS-deficient mice (31). Because many cardiovascular diseases are associated with the development of the endothelial dysfunction syndrome (where both the vascular NO and H2S pathways are impaired) (32–36), supplementation of either NO or H2S alone may not be sufficient to restore vascular homeostasis. Based on the current findings, we propose that novel therapeutic approaches should focus at the simultaneous restoration of NO and H2S homeostasis in the vasculature.
Methods
Cell Culture.
The bEnd3 immortalized mouse brain microvascular endothelial cell line was cultured as described (30). For stable CSE gene silencing, shRNAs lentiviral particles were transduced at 20 multiplicity of infection, and stable clones selected via puromycin. For cell proliferation assays, cells were harvested and counted using a Neubauer hemocytometer at 48 h (15). For wound scratch assay, a scratch was made in a straight line across the diameter of each well by using a 200-μL sterile pipette tip. For cell migration assays, a modified Boyden chamber was used (15).
Aortic Ring Angiogenesis Assay.
The thin gel rat/mouse aortic ring assay was conducted as described (37–39). We stimulated vessel sprouting using NaHS (10–100 μM), DEA/NO (10 μM), or VEGF (20 ng/mL) for 7 d. To silence CSE in the endothelial cells of vascular rings, rings were transfected overnight with 30 pmol CSE siRNA (Ambion). The transfection efficiency was monitored by cotransfection of the siRNA with lacZ expression plasmid. For CSE overexpression, rings were infected with a green fluorescent protein or CSE expressing adenovirus at 3 × 108 pfu per ring (34).
Isolated Rat Aortic Ring Assay.
Isometric contraction and relaxation in aortic rings was performed as described (34).
cGMP and sGC Determination.
cGMP content in cell and vascular ring extracts was measured by a commercial EIA kit (Assay Designs) (8). For measurement of sGC activity, the recombinant α1β1 sGC was expressed in insect Sf9 cells and purified to homogeneity. Enzymatic activity was assayed using [α-32P]GTP to [32P]cGMP conversion assay described (40).
Measurement of PDE5A Activity.
PDE5A activity was measured in vitro with the PDE Assay Kit (Amsbio no. 60300).
CSE Activity Assay.
Plasma H2S and H2S production rates in mouse thoracic aorta lysates were measured as described (41).
Western Blotting Analysis.
Proteins from cells or tissues lysates were subjected to SDS/PAGE and Western blotting as described (34).
In Vivo Angiogenesis.
We performed a 30% total body surface area burn injury in Sprague–Dawley rats as described (15). We treated rats twice a day with s.c. injections of vehicle or NaHS (300 μg/kg per day) in the volume of 100 μL per injection at four equally spaced sites in the transition zone between burn site and healthy tissue. The size of lesions at day 28 was determined by planimetry. For the matrigel plug assay, wild-type or eNOS−/− C57BL/6J mice were injected s.c. with 500 μL of Matrigel. NaHS (50 μmol/kg per day) was injected s.c. in proximity of the matrigel plugs twice a day for 10 d. The Matrigel plugs were recovered by dissection and digested by Drabkin’s reagent, and angiogenesis was assessed by hemoglobin measurement.
Statistical Analysis.
All data are presented as means ± SEM. Statistical analysis was performed by one-way ANOVA followed by Bonferroni’s multiple comparison test. P < 0.05 was considered significant.
Supplementary Material
Supporting Information
Acknowledgments
This study was supported by a grant from the Shriners of North America (8661) and a grant from the Juvenile Diabetes Foundation (17-2010-542) (to C.S.), National Institutes of Health Grant R01HL088128 (to E.M.), and the European Union (Economic Social Fund) and Greek national funds through the Operational Program “Education and Lifelong Learning” of the National Strategic Reference Framework Research Funding Program ARISTEIA (Excellence) (to A.P.). The 2011 EU FP7 REGPOT CT-2011-285950 – “SEE-DRUG” project has supported this work.
Footnotes
Conflict of interest statement: C.S. is a holder of patents related to the therapeutic effects of H2S.
This article is a PNAS Direct Submission.
See Commentary on page 8801.
References
- 1.Mustafa AK, Gadalla MM, Snyder SH. Signaling by gasotransmitters. Sci Signal. 2009;2:re2. doi: 10.1126/scisignal.268re2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Szabo C. Gaseotransmitters: New frontiers for translational science. Sci Transl Med. 2010;2:59ps54. doi: 10.1126/scitranslmed.3000721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ignarro LJ. Nitric oxide: A unique endogenous signaling molecule in vascular biology. Biosci Rep. 1999;19:51–71. doi: 10.1023/a:1020150124721. [DOI] [PubMed] [Google Scholar]
- 4.Bryan NS, Bian K, Murad F. Discovery of the nitric oxide signaling pathway and targets for drug development. Front Biosci. 2009;14:1–18. doi: 10.2741/3228. [DOI] [PubMed] [Google Scholar]
- 5.Wang R. The gasotransmitter role of hydrogen sulfide. Antioxid Redox Signal. 2003;5:493–501. doi: 10.1089/152308603768295249. [DOI] [PubMed] [Google Scholar]
- 6.Szabó C. Hydrogen sulphide and its therapeutic potential. Nat Rev Drug Discov. 2007;6:917–935. doi: 10.1038/nrd2425. [DOI] [PubMed] [Google Scholar]
- 7.Mustafa AK, et al. H2S signals through protein S-sulfhydration. Sci Signal. 2009;2:ra72. doi: 10.1126/scisignal.2000464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bucci M, et al. Hydrogen sulfide is an endogenous inhibitor of phosphodiesterase activity. Arterioscler Thromb Vasc Biol. 2010;30:1998–2004. doi: 10.1161/ATVBAHA.110.209783. [DOI] [PubMed] [Google Scholar]
- 9.Francis SH, Busch JL, Corbin JD, Sibley D. cGMP-dependent protein kinases and cGMP phosphodiesterases in nitric oxide and cGMP action. Pharmacol Rev. 2010;62:525–563. doi: 10.1124/pr.110.002907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Osipov RM, et al. Effect of hydrogen sulfide in a porcine model of myocardial ischemia-reperfusion: Comparison of different administration regimens and characterization of the cellular mechanisms of protection. J Cardiovasc Pharmacol. 2009;54:287–297. doi: 10.1097/FJC.0b013e3181b2b72b. [DOI] [PubMed] [Google Scholar]
- 11.Fleming I. Molecular mechanisms underlying the activation of eNOS. Pflugers Arch. 2010;459:793–806. doi: 10.1007/s00424-009-0767-7. [DOI] [PubMed] [Google Scholar]
- 12.Förstermann U, Sessa WC. Nitric oxide synthases: Regulation and function. Eur Heart J. 2012;33:829–837. doi: 10.1093/eurheartj/ehr304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Papapetropoulos A, García-Cardeña G, Madri JA, Sessa WC. Nitric oxide production contributes to the angiogenic properties of vascular endothelial growth factor in human endothelial cells. J Clin Invest. 1997;100:3131–3139. doi: 10.1172/JCI119868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Munaron L, Fiorio Pla A. Endothelial calcium machinery and angiogenesis: Understanding physiology to interfere with pathology. Curr Med Chem. 2009;16:4691–4703. doi: 10.2174/092986709789878210. [DOI] [PubMed] [Google Scholar]
- 15.Papapetropoulos A, et al. Hydrogen sulfide is an endogenous stimulator of angiogenesis. Proc Natl Acad Sci USA. 2009;106:21972–21977. doi: 10.1073/pnas.0908047106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Szabó C, Papapetropoulos A. Hydrogen sulphide and angiogenesis: Mechanisms and applications. Br J Pharmacol. 2011;164:853–865. doi: 10.1111/j.1476-5381.2010.01191.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Li L, Rose P, Moore PK. Hydrogen sulfide and cell signaling. Annu Rev Pharmacol Toxicol. 2011;51:169–187. doi: 10.1146/annurev-pharmtox-010510-100505. [DOI] [PubMed] [Google Scholar]
- 18.Murakami M, Elfenbein A, Simons M. Non-canonical fibroblast growth factor signalling in angiogenesis. Cardiovasc Res. 2008;78:223–231. doi: 10.1093/cvr/cvm086. [DOI] [PubMed] [Google Scholar]
- 19.Ziche M, et al. Nitric oxide synthase lies downstream from vascular endothelial growth factor-induced but not basic fibroblast growth factor-induced angiogenesis. J Clin Invest. 1997;99:2625–2634. doi: 10.1172/JCI119451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pyriochou A, Vassilakopoulos T, Zhou Z, Papapetropoulos A. cGMP-dependent and -independent angiogenesis-related properties of nitric oxide. Life Sci. 2007;81:1549–1554. doi: 10.1016/j.lfs.2007.09.014. [DOI] [PubMed] [Google Scholar]
- 21.Koika V, et al. PKG-I inhibition attenuates vascular endothelial growth factor-stimulated angiogenesis. Vascul Pharmacol. 2010;53:215–222. doi: 10.1016/j.vph.2010.08.004. [DOI] [PubMed] [Google Scholar]
- 22.Pyriochou A, et al. Soluble guanylyl cyclase activation promotes angiogenesis. J Pharmacol Exp Ther. 2006;319:663–671. doi: 10.1124/jpet.106.108878. [DOI] [PubMed] [Google Scholar]
- 23.Li L, et al. Characterization of a novel, water-soluble hydrogen sulfide-releasing molecule (GYY4137): New insights into the biology of hydrogen sulfide. Circulation. 2008;117:2351–2360. doi: 10.1161/CIRCULATIONAHA.107.753467. [DOI] [PubMed] [Google Scholar]
- 24.Zhao W, Zhang J, Lu Y, Wang R. The vasorelaxant effect of H(2)S as a novel endogenous gaseous K(ATP) channel opener. EMBO J. 2001;20:6008–6016. doi: 10.1093/emboj/20.21.6008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mustafa AK, et al. Hydrogen sulfide as endothelium-derived hyperpolarizing factor sulfhydrates potassium channels. Circ Res. 2011;109:1259–1268. doi: 10.1161/CIRCRESAHA.111.240242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yang G, et al. H2S as a physiologic vasorelaxant: Hypertension in mice with deletion of cystathionine gamma-lyase. Science. 2008;322:587–590. doi: 10.1126/science.1162667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hosoki R, Matsuki N, Kimura H. The possible role of hydrogen sulfide as an endogenous smooth muscle relaxant in synergy with nitric oxide. Biochem Biophys Res Commun. 1997;237:527–531. doi: 10.1006/bbrc.1997.6878. [DOI] [PubMed] [Google Scholar]
- 28.Whiteman M, et al. Evidence for the formation of a novel nitrosothiol from the gaseous mediators nitric oxide and hydrogen sulphide. Biochem Biophys Res Commun. 2006;343:303–310. doi: 10.1016/j.bbrc.2006.02.154. [DOI] [PubMed] [Google Scholar]
- 29.Whiteman M, Moore PK. Hydrogen sulfide and the vasculature: A novel vasculoprotective entity and regulator of nitric oxide bioavailability? J Cell Mol Med. 2009;13:488–507. doi: 10.1111/j.1582-4934.2009.00645.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kajimura M, Fukuda R, Bateman RM, Yamamoto T, Suematsu M. Interactions of multiple gas-transducing systems: Hallmarks and uncertainties of CO, NO, and H2S gas biology. Antioxid Redox Signal. 2010;13:157–192. doi: 10.1089/ars.2009.2657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Minamishima S, et al. Hydrogen sulfide improves survival after cardiac arrest and cardiopulmonary resuscitation via a nitric oxide synthase 3-dependent mechanism in mice. Circulation. 2009;120:888–896. doi: 10.1161/CIRCULATIONAHA.108.833491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Szabo C. Role of nitrosative stress in the pathogenesis of diabetic vascular dysfunction. Br J Pharmacol. 2009;156:713–727. doi: 10.1111/j.1476-5381.2008.00086.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Flammer AJ, Lüscher TF. Human endothelial dysfunction: EDRFs. Pflugers Arch. 2010;459:1005–1013. doi: 10.1007/s00424-010-0822-4. [DOI] [PubMed] [Google Scholar]
- 34.Suzuki K, et al. Hydrogen sulfide replacement therapy protects the vascular endothelium in hyperglycemia by preserving mitochondrial function. Proc Natl Acad Sci USA. 2011;108:13829–13834. doi: 10.1073/pnas.1105121108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ramli J, CalderonArtero P, Block RC, Mousa SA. Novel therapeutic targets for preserving a healthy endothelium: Strategies for reducing the risk of vascular and cardiovascular disease. Cardiol J. 2011;18:352–363. [PMC free article] [PubMed] [Google Scholar]
- 36.Lynn EG, Austin RC. Hydrogen sulfide in the pathogenesis of atherosclerosis and its therapeutic potential. Expert Rev Clin Pharmacol. 2011;4:97–108. doi: 10.1586/ecp.10.130. [DOI] [PubMed] [Google Scholar]
- 37.Zhu WH, Nicosia RF. The thin prep rat aortic ring assay: A modified method for the characterization of angiogenesis in whole mounts. Angiogenesis. 2002;5:81–86. doi: 10.1023/a:1021509004829. [DOI] [PubMed] [Google Scholar]
- 38.Baker M, et al. Use of the mouse aortic ring assay to study angiogenesis. Nat Protoc. 2012;7:89–104. doi: 10.1038/nprot.2011.435. [DOI] [PubMed] [Google Scholar]
- 39.Nicosia RF. The aortic ring model of angiogenesis: A quarter century of search and discovery. J Cell Mol Med. 2009;13:4113–4136. doi: 10.1111/j.1582-4934.2009.00891.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Martin E, Berka V, Tsai AL, Murad F. Soluble guanylyl cyclase: The nitric oxide receptor. Methods Enzymol. 2005;396:478–492. doi: 10.1016/S0076-6879(05)96040-0. [DOI] [PubMed] [Google Scholar]
- 41.Brancaleone V, et al. Biosynthesis of H2S is impaired in non-obese diabetic (NOD) mice. Br J Pharmacol. 2008;155:673–680. doi: 10.1038/bjp.2008.296. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting Information