Primary total hip arthroplasty: health related quality of life outcomes (original) (raw)
Abstract
Purpose
The health related quality of life (HRQoL) outcomes of total hip arthroplasty (THA) present a pertinent and clinically important problem in modern orthopaedics. Our goal was to report and compare the health-related outcomes after THA in respect to type of fixation in patients with hip osteoarthritis (H-OA) one year after operation.
Methods
A total of 145 patients with H-OA who received THA were evaluated. Uncemented and cemented subjects were evaluated using generic measures, i.e. the EQ-5D questionnaire, and the disease-specific measures designed by the authors, i.e. the Total Hip Arthroplasty Questionnaire (THAQ). Obtained data was statistically processed at the level of pain, functionality and general health perception. Patient-reported outcomes were measured differences between pre-operative measures and those at one-year follow-up visit.
Results
Significant improvement in health outcomes was reached in both groups regardless of the type of fixation (p < 0.001). Uncemented fixation exhibited better results for EQ-5DINDEX, pain (p = 0.004) and self-care on EQ-5D (p = 0.043), as well as increased magnitude of change for functionality on THAQ (p = 0.002). However, additional analysis of the subset did not reveal a significant difference between cemented vs. uncemented groups with regard to function on THAQ, but the significant difference on self-care and pain dimensions of EQ-5D remained.
Conclusions
Uncemented endoprosthesis generally achieved better short-term outcomes in some dimensions. However, painless mobility has been restored in most of the patients, regardless of the fixation type. Both methods reached good clinical outcomes in their respective domains; therefore, we would emphasise prevention of osteoarthritis and the quality of care as the more important predictors of good clinical outcomes.
Keywords: HRQoL, THA, Quality, Fixation, Hip, Osteoarthritis
Introduction
Hip osteoarthritis (H-OA) is one of the most prevalent age-related musculoskeletal disorders and the most common diagnosis that leads to total hip arthroplasty (THA) [1, 2]. Osteoarthritis of the hip may cause severe impairment which reflects pain and functional disability and strongly affects the HRQoL [3]. However, these limitations may be markedly improved by elective THA [4]. From the public health point of view, THA is one of the most effective and the most cost-effective surgical procedure [5]. However, THA is associated with undesireable, life-threatening outcomes [6, 7]. Therefore, by applying appropriate criteria, THA should be performed only on those patients in whom conservative therapy cannot achieve painless mobility [8]. in view of the medical expenses and undesireable health outcomes of this procedure, there has been a considerable effort to prevent and treat the H-OA as a primary underlying cause in recent times [9]. On the other hand, it is generally considered that the risk of arthroplasty is lower than the risk of the potential damage that the late phase of H-OA or rheumatoid arthritis (RA) [10].
There are many unclear views about THA-related health outcomes with respect to socio-economic value [11–14], medical characteristics of patients [15], hospital volume [16, 17], type of rehabilitation [18], etc. In addition to professional discrepancies towards these aspects, orthopaedic surgical practice is also not consensual on the choice of endoprosthetic fixation or the surgical access to hip [19, 20].
In the context of choice of endoprosthesis, the research on the advantage of certain fixations is mostly focused on the long-term outcomes, especially on the aspect of endoprosthesis survival [2, 21] that does not only depend on the type of fixation, but also largely depends on the lifestyle of each particular patient. Clinical parameters have been traditionally used to measure the outcomes for THA, but recently there is a consensus that patient-reported HRQoL outcomes should be primarily used in a research and clinical practice setting [22]. Although both clinical measurements and patient-report outcomes have been systematically reviewed, the optimal fixation method has not yet been defined, and further investigations have been recommended [23]. There is still a lack of data on the short-term outcomes of THA procedures, as assessed using a comprehensive approach which combines generic and disease-specific patient-reported measures [3, 24].
Until recently, cement endoprosthesis was a first choice of many surgical practices worldwide, but it has been steadily replaced by uncemented implants, although there has not been unanimous evidence presented on which method has clear advantage, if any [20, 25, 26]. The choice of endoprosthetic fixation is generally based on the characteristics of each individual patient and on the personal experience of the surgeon; however, that choice is not always determined by strict medical reasons, but rather on the availability of certain type of endoprosthesis, regardless the agreement of the surgeon.
Based on our pilot study that was conducted prior to this research, this problem is largely present and identified in Croatia and similar difficulties have been recognised internationally. Therefore, we decided to execute this research effort in order to illuminate and detect relevant determinants of hip fixation. This is the first study of this kind conducted in the Republic in Croatia and the first one that uses a uniquely designed study methodology.
Methods
This was a cross-sectional cohort study. The study design was a prospective follow-up and “before after” design with pre-operative measures and a postoperative follow-up after one-year. The study was designed in an innovative way by using two types of questionnaires: one used as a validated generic scale related to general health patient-reported outcomes, EQ-5D [27], and the other an author-designed disease-specific questionnaire, THAQ, from which the sets of questions were selected for analysis. THAQ is an author's original assessment tool that evaluates sociodemographic, functional and rehabilitation characteristics of THA patients. Our main sample consisted of 145 patients enrolled during the period of one year at the Department of Orthopaedic Surgery, University Hospital Split, Croatia. Patient inclusion criteria were the following: (1) elective primary THA, (2) patients with primary H-OA, (3) patient's age older than 18 years and (4) ability to complete self-perceived questionnaires. The data on patients with H-OA who underwent uncemented or cement THA have been evaluated prospectively to determine potential differences in HRQoL outcomes between matched groups.
All of the patients who underwent the THA surgical procedure have received: thromboprophylaxis (low molecular weight Heparin and Xlexan, pre- and postoperatively), antibiotic prophylaxis (Rocefin, pre- and postoperation), anaesthesia (epidural or general), endoprosthesis (cemented or uncemented) and one to two units of blood in addition to analgesic treatment with tramadol. The hip was surgically accessed posteriorly or laterally. Data were collected by two investigators during the pre-operative consultations and at one-year follow-up visit.
Statistical analysis included chi-squared and Mann-Whitney U tests to ascertain the significance of the cross-sectional differences between groups on our main sample. Single scale scores of the EQ-5D and the THAQ were treated as categorical outcomes. Pain and general health were continuous variables. In order to further investigate the correlation of fixation type and health related outcomes, an additional analysis of the subset of patient population was performed (n = 76) that had included primary H-OA only as the main diagnosis and that differed in age the least. This sample is also matched in terms of type of endoprosthesis so that both groups were nearly equally represented. With respect to age, the bottom two categories were exclusively isolated into all patients that were 64 years or younger and patients 65–69 of age with primary H-OA. In this way, possible age-discriminatory effects on health related outcomes were minimised. In addition, two indexes have been introduced: a PAININDEX which characterises patient's pain-related health outcomes (THAQ, items 56–60) and a FUNCTIONALITYINDEX that characterises patient's functional abilities in terms of mobility (items 61–66). Kolmogorov-Smirnov test, to determine the distribution quality, and Mann-Whitney U non-parametric test were used to detect the possible differences between cemented vs uncemented groups on a subset sample. Correlation studies have been tested via bivariate Pearson coefficient at 95 % confidence level. Significance was obtained at a 2-tailed level.
Results
Sociodemographic characteristics of our main sample (n = 145) of patients with H-OA are reported in Table 1. Most common comorbid diagnosis was hypertension in 53 (37.1 %), dyslipidemia in 27 (19.3 %), diabetes in 24 (17.1 %) and peripheral vascular disease in only eight (5.8 %) patients.
Table 1.
Characteristics and differences of uncemented and cemented patients who underwent total hip arthroplasty (THA)
| Patient data | n (%) | Uncemented | Cemented | P |
|---|---|---|---|---|
| THA | 145 (100.0) | 45 (100.0) | 100 (100.0) | |
| Uncemented | 45 (31.0) | 45 (100.0) | 0 (0.0) | |
| Cemented | 100 (69.0) | 0 (0.0) | 100 (100.0) | |
| Age at admission | 145 (100.0) | 45 (100.0) | 100 (100.0) | <0.001 |
| <64 yrs | 46 (31.7) | 33 (73.3) | 13 (13.0) | |
| 65-69 | 32 (22.1) | 5 (11.1) | 27 (27.0) | |
| 70-74 | 40 (27.6) | 3 (6.7) | 37 (37.0) | |
| 75-79 | 17 (11.7) | 3 (6.7) | 14 (14.0) | |
| ≥80 yrs | 10 (6.9) | 1 (2.2) | 9 (9.0) | |
| Sex | 145 (100.0) | 45 (100.0) | 100 (100.0) | >0.999 |
| Female | 101 (69.7) | 31 (68.9) | 70 (70.0) | |
| Male | 44 (30.3) | 14 (31.1) | 30 (30.0) | |
| Disease duration | 145 (100.0) | 44 (100.0) | 100 (100.0) | 0.258 |
| <3 yrs | 30 (20.8) | 10 (22.7) | 20 (20.0) | |
| 4-6 yrs | 102 (70.8) | 28 (63.6) | 74 (74.0) | |
| 7 or more yrs | 12 (8.3) | 6 (13.6) | 6 (6.0) | |
| Body mass index (BMI) kg/m-2 | 144 (100.0) | 45 (100.0) | 99 (100.0) | 0.248 |
| Normal mass (<25.0) | 16 (11.1) | 8 (17.8) | 8 (8.1) | |
| Overweight (25.0-30.0) | 106 (73.6) | 31 (68.9) | 75 (75.8) | |
| Obesity (>30) | 22 (15.3) | 6 (13.3) | 16 (16.2) | |
| Educational level | 145 (100.0) | 45 (100.0) | 100 (100.0) | 0.009 |
| Primary school | 89 (61.4) | 20 (44.4) | 69 (69.0) | |
| Secondary school and more | 56 (38.6) | 25 (55.6) | 31 (31.0) | |
| Preoperative employment | 142 (100.0) | 45 (100.0) | 97 (100.0) | <0.001 |
| Unemployed | 8 (5.6) | 2 (4.4) | 6 (6.2) | |
| Retired | 51 (35.9) | 11 (24.4) | 40 (41.2) | |
| Employed | 26 (18.3) | 21 (46.7) | 5 (5.2) | |
| Partially employed | 9 (6.3) | 3 (6.7) | 6 (6.2) | |
| Housewife | 48 (33.8) | 8 (17.8) | 40 (41.2) | |
| Family situation | 136 (100.0) | 44 (100.0) | 92 (100.0) | 0.021 |
| Unaccompanied | 12 (16.2) | 6 (13.6) | 16 (17.4) | |
| Married | 74 (54.4) | 32 (72.7) | 42 (45.7) | |
| With children | 33 (24.3) | 5 (11.4) | 28 (30.4) | |
| With relatives | 7 (5.1) | 1 (2.3) | 6 (6.5) | |
| Last employment | 134 (100.0) | 42 (100.0) | 92 (100.0) | 0.034 |
| Manual | 111 (82.8) | 30 (71.4) | 81 (88.0) | |
| Sedentary | 23 (17.2) | 12 (28.6) | 11 (12.0) | |
| Cigarette smoking | 145 (100.0) | 45 (100.0) | 100 (100.0) | 0.017 |
| >20 cigarettes daily | 17 (11.7) | 11 (24.4) | 6 (6.0) | |
| <20 cigarettes | 33 (22.8) | 9 (20.0) | 24 (24.0) | |
| Ex smokers | 22 (15.2) | 6 (13.3) | 16 (16.0) | |
| Non-smokers | 73 (50.3) | 19 (42.2) | 54 (54.0) | |
| Incomes | 143 (100.0) | 44 (100.0) | 99 (100.0) | – |
| Pension | 63 (44.1) | 9 (20.5) | 54 (54.5) | |
| Pension and from children | 41 (28.7) | 11 (25.0) | 30 (30.3) | |
| Salary no more than pension | 20 (14.0) | 12 (27.3) | 8 (8.1) | |
| Salary higher than pension | 12 (8.4) | 10 (22.7) | 2 (2.0) | |
| Salary more than 4000.00 kn | 1 (1.7) | 1 (2.3) | 0 (0.0) | |
| Other incomes | 6 (4.2) | 1 (2.3) | 5 (5.1) |
Cemented fixation was more commonly used than uncemented, i.e. 100 cemented (69.0 %) vs. 45 (31.0 %) uncemented implants. A direct transgluteal approach was the most commonly used in 128 H-OA patients (88.3 %) and an anterior approach in the smaller group of patients (17, 11.7 %). Significant differences in sociodemographic and vital parameters were found pre-operatively between uncemented and cemented groups of patients (Table 1) with respect to age (p ≤ 0.001). Uncemented cases were statistically younger than cemented patients (73.3 % of subjects in uncemented groups and 13.0 % of cemented patients were under 64 years; 74 % cemented and 17.8 % uncemented subjects were 65–74 years of age).
Statistical differences between the cemented and uncemented groups and relative change between preoperative measures and those measures at one-year after discharge on the EQ-5D scale are reported in Table 2. At one year after operation, not pre-operatively, statistically significant differences between the two groups (p = 0.021) in the total EQ-5DINDEX score (consisting of five dimensions: mobility, self-care, usual activities, pain/discomfort and depression/anxiety, plus EQ-5DVAS) were found; cemented subjects reached lower scores on the EQ-5DINDEX than uncemented subjects. Results show that a statistically higher number of cemented subjects exhibited persistent problems in two dimensions of the EQ-5D scale at one-year follow-up: self-care (p = 0.043) and pain/discomfort (p = 0.004).The proportion of patients with persistent, unfavourable pain/discomfort outcome at one-year postoperatively on the EQ-5D scale was 16.0 % in cemented and 0 % in the uncemented group.
Table 2.
P-values indicating differences in general health (EQ-5D) and disease-specific quality of life (THAQQ) between uncemented and cemented total hip arthroplasty (THA) after one-year follow-up
| Scales | Admission | One-year follow-up | Uncemented | Cemented |
|---|---|---|---|---|
| P-values for both uncemented (N = 45) and cemented (N = 100) | P-values at admission and one-year follow-up | |||
| EQ-5DINDEX | 0.158 | 0.021 | <0.001 | <0.001 |
| Mobility | - | 0.367 | <0.001 | <0.001 |
| Self-care | - | 0.043 | <0.001 | <0.001 |
| Usual activities | - | 0.542 | <0.001 | <0.001 |
| Pain/discomfort | 0.475 | 0.004 | <0.001 | <0.001 |
| Depression | 0.124 | 0.069 | <0.001 | <0.001 |
| EQ.5DVAS (0–100) | 0.502 | 0.196 | <0.001 | <0.001 |
| Pain | 0.300 | 0.131 | 0.013 | <0.001 |
| Pain (VAS) | 0.304 | 0.369 | <0.001 | <0.001 |
| Control by medications | 0.902 | - | - | - |
| Pain-induced insomnia | 0.999 | - | <0.001 | <0.001 |
| Disturbed daily activities | 0.999 | 0.256 | <0.001 | <0.001 |
| Functionality | <0.001 | 0.002 | <0.001 | <0.001 |
| Walking distance | - | - | <0.001 | <0.001 |
| Climbing stairs | 0.009 | - | - | <0.001 |
| Using orthopaedic devices | 0.001 | 0.401 | - | <0.001 |
| Using public transport | 0.044 | - | <0.001 | <0.001 |
| Binding shoelace | 0.106 | - | - | <0.001 |
| Getting up | - | - | <0.001 | <0.001 |
No statistical differences for EQ-5DINDEX, all five dimensions of EQ-5D and EQ-5DVAS between the two groups were found at admission, although the clear clinical differences in all five single scale scores on EQ-5D already existed pre-operatively. Self-care problems persisted in 23.0 % of cemented and 8.9 % of uncemented subjects one-year after operation. No statistical differences, but evident clinical changes were observed in mental health status between the two groups; 90.0 % of cemented subjects reported symptoms of depression/anxiety at admission and 27.0 % at one-year follow-up in contrast to 77.8 % and 13.3 % in the uncemented group. Cemented subjects exhibited worse scores in usual activities pre-operatively; 100.0 % cemented and 91.1 % uncemented patients had problems performing daily life activities as compared to 27.0 % and 22.2 % one year after THA.
Examining the dimension of functionality on THAQ, we found a significant difference between uncemented and cemented subjects pre- and postoperatively, with no significant differences for pain dimension on THAQ and THAQVAS, in contrast to pain on EQ-5D postoperatively. The mean value of pain intensity was 8 points on THAQVAS. Patients from both groups estimated pain intensity more than level 4 on VAS at referral. No statistical differences between the two groups were found for pain intensity on VAS pre-operatively, but they differed clinically. In the cemented group 33.0 %, 39.0 % and 14.0 % of patients were given 7, 8 and 9 points on VAS; in contrast to the uncemented group where 28.9 % and 46.7 % gave 7 and 8 points and only 4.4 % patients gave 9 points on VAS. Postoperatively, none of patients in the uncemented group reported pain intensity above level 3 on VAS, while 10.1 % of cemented patients reported pain intensity above level 4 on VAS. In total, 16.0 % of cemented patients experienced persistent pain at one year after operation, and 9.0 % of patients had difficulties dealing with pain while performing daily activities. All patients from both groups could control their pain with analgesia postoperatively, in contrast to 66.7 % uncemented and 64.0 % cemented at referral. The statistically significant differences between uncemented and cemented THA patients were found pre-operatively in respect to climbing the stairs; 56.0 % of cemented and only 31.1 % of uncemented patients could not climb up the stairs.
The great majority of cemented THA subjects (79.4 %) had used orthopaedic devices in contrast to 42.2 % in the uncemented group; the uncemented group scored better while using public transportation (44.4 %) as compared to the cemented subjects (26.0 %). No differences in tying shoelaces, climbing stairs, getting up from bed or using public transportation were found between groups postoperatively. None of the patients had experienced pain disturbing their sleep one year post THA. Clinical, but not statistically significant, differences were found for functional activities between groups; 88.9 % of uncemented subjects performed walking distance more than 800 metres post THA, in contrast to only 63.0 % of cemented subjects. In addition, 13 % of cemented subjects and only 6.7 % of uncemented patients still used orthopaedic devices at one year follow-up.
The rate of THA complications was recorded such that 9.7 % of patients (14) had superficial wound infection while no cases of deep wound infections occurred. Early dislocation occurred in only three cases (2 %), while there were no cases of pulmonary embolism and no fatal outcomes. Epidural anaesthesia was received by 124 patients (87.3 %) and all of the patients (100 %) received thrombolytic/antibiotic prophylaxis.
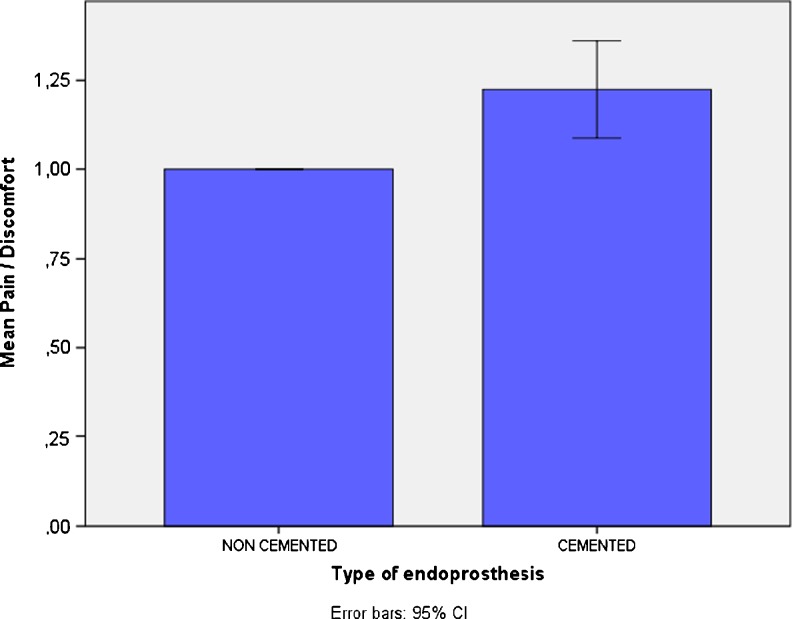
In our study of population subsets (Table 3), a total of 76 patients taken from the main sample, 36 (47 %) of them with uncemented and 40 (53 %) with cemented fixation; 44 (58 %) patients were 64 years or younger, 32 (42 %) were 65–69 years of age, while the mean age was 60.5 years. A clear statistical difference between groups for pain and discomfort (p = 0.003, Fig. 1) and a respectable difference for self-care (2-tailed p = 0.056, 1- tailed p = 0.028) were found. The uncemented group scored clinically but not significantly better results on EQ-5DINDEX and EQ-5DVAS than the cemented group, with overall health state assessment being 71.81 % for uncemented and 68.38 % for cemented subjects. In respect to THAQ dimensions, such as pain and mobility, no significant differences were found between cemented vs. uncemented groups. Perioperative dimensions of THAQ such as physical therapy and duration of hospital stay have shown significant correlation with the PAININDEX with values p = 0.006 and p = 0.005, respectively. Patients who started therapy on the bed, immediately following THA, had significantly lower pain, regardless of the type of fixation.
Table 3.
Differences on EQ-5DINDEX, EQ-5DVAS, five EQ-5D dimensions and disease specific THAQQ dimensions: PAININDEX and FUNCTIONALITYINDEX (FUNCT), between cemented and uncemented groups after total hip arthroplasty (THA) at one-year follow-up
| Test | EQ5DINDEX | PAININDEX | FUNCTINDEX | Mobility | Self-care | Usual activities | Pain | Anxiety | EQ-5DVAS |
|---|---|---|---|---|---|---|---|---|---|
| Mann–Whitney | 562.0 | 694.0 | 624.0 | 692.0 | 600.0 | 698.0 | 558.0 | 658.0 | 554.0 |
| Wilcoxon signed-rank | 1228.0 | 1360.0 | 1290.0 | 1512.0 | 1266.0 | 1364.0 | 1224.0 | 1324.0 | 1374.00 |
| −1.819 | −0.400 | −1.402 | −0.520 | −1.914 | −0.324 | −3.011 | −0.961 | −1.783 | |
| p (2-tailed) | 0.069 | 0.689 | 0.161 | 0.603 | 0.056 | 0.746 | 0.003 | 0.337 | 0.075 |
Fig. 1.
Mean pain/discomfort as one of the EQ-5D dimensions in respect to type of total hip arthroplasty (THA) fixation
Discussion
Our study of the main patient sample showed that uncemented subjects reached significantly better outcomes on pain/discomfort and self-care dimensions of EQ-5D and functionality dimension of THAQ. We argued that this could partially be influenced by the asymmetrical age distribution between the two groups, since most of the younger patients received uncemented fixation. Therefore, additional analysis of the subset with reduced age extremities showed no significant difference between the two groups regarding the functionality on THAQ, but the statistical difference on pain/discomfort and self-care dimensions of EQ-5D remained. Additionally, uncemented subjects scored better results on EQ-5DINDEX and on EQ-5DVAS, clinically, but not significantly.
Both methods, cemented and uncemented, scored significant improvements in postoperative HRQoL outcomes compared to the ones at admission, including all five dimensions of EQ-5D and pain/functionality dimensions of THAQ. Similar to other studies [28, 29], our data showed that elimination of pain, restoration of functional mobility and general state of health of the individual is generally achieved following THA, regardless of age, sex and the type of endoprosthesis [2, 3, 12, 20, 21, 30].
In our study none of our patients reported severe pain intensity on VAS scale postoperatively, which is in contrast to previous findings [31] that report that up to 30 % of patients use analgesics on a regular basis following the THA. However, a certain proportion of our patients did have persisting pain (24 % of total, out of which 7 % had pain that hindered their daily activities) which is in accordance with the findings of Beswick et al. [31] who report that a significant proportion of patients had persisting pain remaining after THA. However, in all of our cases pain could be controlled by medication and did not cause problems sleeping. A potential weakness of our study is that we did not inspect which proportion of patients were taking analgetics on a daily basis, leaving this to be further examined. In accordance with the findings in literature [21], including the Swedish Register of Arthroplasty (SHAR) [2], we did not find correlation of early complications with the type of endoprosthesis.
Cemented and uncemented fixations both excelled in their own domains—cemented being the choice in older patients that are less mobile and exhibit sedentary lifestyles, and uncemented, which has been used in younger patients with more active lifestyles [2]. However, clear and standardised criteria for choosing non-cemented fixation over cemented has not been established. Aseptic loosening and increased risk of possible revision, we assume, is the main reason why specialists choose more expensive non-cemented fixation, although there are no clear indicators that it is a superior method and pertinent literature offers no consensus on this issue [21, 32, 33]. Practical experience in the field suggests that the specialists tend to make their choice on endoprosthesis type based on availability and cost. Our data suggests that the main inclusion criteria for the type of the fixation was age.
A potential weakness of this study is the absence of randomised patient selection; however, the selection of candidates for rigorous surgical procedures such as THA is not always a simple endeavour in real-time practice. Therefore, the "gold standard" practice in orthopaedics was followed, which is supported in literature by pertinent systematic reviews, indicating that the randomised controlled trial (RCT) studies are difficult to perform and are not synonymous with the truth in orthopaedic care for patients. This could possibly mean that non-RCT trials (prospective clinical trials) with adequate follow-up and measurement could set the gold standard in orthopaedic care [21]. Our effort to resolve age-related asymmetry in respect to type of fixation resulted in the subset analysis that has been reported.
Recent literature has shown that the THA outcome results differ when different assessment instruments are used [34]. To the best of our knowledge, no previous studies have used these two HRQoL instruments with a comparable one-year period, making this exact kind of dual scoring system a methodologically original contribution to the assessment of HRQoL outcomes after THA [11, 23, 31].
Based on recent evidence, we argue that each existing questionnaire has its own strengths and limitations, and an optimal self-reporting mechanism has not yet been reached, which opens the question of instrumentation sensitivity; this should be examined in further studies [23].
In summary, we suggest that the choice of fixation should not be emphasised to the current degree in literature. Prevention of osteoarthritis and the overall health care, which will ensure elimination of undesirable outcomes, of which some are life threatening, are more important predictors of HRQoL outcomes after THA than the type of fixation alone.
Acknowledgments
We would like to thank the Department of Orthopaedic Surgery of the University Hospital Split, especially to nurse Ines Puljiz and medical technician Mladen Levačić, for providing facilities for performing the clinical evaluation of THA patients. We are frankly thankful to Žarko Bajić for technical help. Special thanks to Reuben Eldar—without him, this research would have not been possible.
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Prior to the study, the approval of University Hospital Center Split ethics committee was obtained. Written informed consent was obtained from all participants in the study. Ethical approval filed under number # 2181-147-03-01-11
Contributor Information
Ivan Bagarić, Email: ibagari1@yahoo.com.
Helena Šarac, Email: helenasarac@hi.t-com.hr.
Josip Anđelo Borovac, Phone: +385-92-1721314, Email: jborovac@mefst.hr, Email: josip.borovac@me.com.
Tonko Vlak, Email: tonko.vlak@st.t-com.hr.
Josip Bekavac, Email: josip.bekavac@inet.hr.
Andrija Hebrang, Email: andrija.hebrang1@hotmail.com.
References
- 1.Quintana JM, Arostegui I, Escobar A, Azkarate J, Goenaga JI, Lafuente I. Prevalence of knee and hip osteoarthritis and the appropriateness of joint replacement in an older population. Arch Intern Med. 2008;168(14):1576–1584. doi: 10.1001/archinte.168.14.1576. [DOI] [PubMed] [Google Scholar]
- 2.Hailer NP, Garellick G, Karrholm J. Uncemented and cemented primary total hip arthroplasty in the Swedish Hip Arthroplasty Register. Acta Orthop. 2010;81(1):34–41. doi: 10.3109/17453671003685400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ethgen O, Bruyere O, Richy F, Dardennes C, Reginster JY. Health-related quality of life in total hip and total knee arthroplasty. A qualitative and systematic review of the literature. J Bone Joint Surg Am. 2004;86-A(5):963–974. doi: 10.2106/00004623-200405000-00012. [DOI] [PubMed] [Google Scholar]
- 4.Mota RE, Tarricone R, Ciani O, Bridges JF, Drummond M. Determinants of demand for total hip and knee arthroplasty: a systematic literature review. BMC Health Serv Res. 2012;12:225. doi: 10.1186/1472-6963-12-225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lavernia CJ, Alcerro JC. Quality of life and cost-effectiveness 1 year after total hip arthroplasty. J Arthroplasty. 2011;26(5):705–709. doi: 10.1016/j.arth.2010.07.026. [DOI] [PubMed] [Google Scholar]
- 6.Senthi S, Munro JT, Pitto RP. Infection in total hip replacement: meta-analysis. Int Orthop. 2011;35(2):253–260. doi: 10.1007/s00264-010-1144-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Singh JA, Kundukulam J, Riddle DL, Strand V, Tugwell P. Early postoperative mortality following joint arthroplasty: a systematic review. J Rheumatol. 2011;38(7):1507–1513. doi: 10.3899/jrheum.110280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Quintana JM, Escobar A, Arostegui I, Bilbao A, Azkarate J, Goenaga JI, et al. Health-related quality of life and appropriateness of knee or hip joint replacement. Arch Intern Med. 2006;166(2):220–226. doi: 10.1001/archinte.166.2.220. [DOI] [PubMed] [Google Scholar]
- 9.Carr AJ, Robertsson O, Graves S, Price AJ, Arden NK, Judge A, et al. Knee replacement. Lancet. 2012;379(9823):1331–1340. doi: 10.1016/S0140-6736(11)60752-6. [DOI] [PubMed] [Google Scholar]
- 10.Culliford DJ, Maskell J, Kiran A, Judge A, Javaid MK, Cooper C, et al. The lifetime risk of total hip and knee arthroplasty: results from the UK general practice research database. Osteoarthritis Cartilage. 2012;20(6):519–524. doi: 10.1016/j.joca.2012.02.636. [DOI] [PubMed] [Google Scholar]
- 11.Jones CA, Pohar S. Health-related quality of life after total joint arthroplasty: a scoping review. Clin Geriatr Med. 2012;28(3):395–429. doi: 10.1016/j.cger.2012.06.001. [DOI] [PubMed] [Google Scholar]
- 12.Santaguida PL, Hawker GA, Hudak PL, Glazier R, Mahomed NN, Kreder HJ, et al. Patient characteristics affecting the prognosis of total hip and knee joint arthroplasty: a systematic review. Can J Surg. 2008;51(6):428–436. [PMC free article] [PubMed] [Google Scholar]
- 13.Singh JA. Smoking and outcomes after knee and hip arthroplasty: a systematic review. J Rheumatol. 2011;38(9):1824–1834. doi: 10.3899/jrheum.101221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Clement ND, Muzammil A, Macdonald D, Howie CR, Biant LC. Socioeconomic status affects the early outcome of total hip replacement. J Bone Joint Surg Br. 2011;93(4):464–469. doi: 10.1302/0301-620X.93B4.25717. [DOI] [PubMed] [Google Scholar]
- 15.Ravi B, Escott B, Shah PS, Jenkinson R, Chahal J, Bogoch E, et al. A systematic review and meta-analysis comparing complications following total joint arthroplasty for rheumatoid arthritis versus for osteoarthritis. Arthritis Rheum. 2012;64(12):3839–3849. doi: 10.1002/art.37690. [DOI] [PubMed] [Google Scholar]
- 16.Meyer E, Weitzel-Kage D, Sohr D, Gastmeier P. Impact of department volume on surgical site infections following arthroscopy, knee replacement or hip replacement. BMJ Qual Saf. 2011;20(12):1069–1074. doi: 10.1136/bmjqs.2011.051250. [DOI] [PubMed] [Google Scholar]
- 17.Shervin N, Rubash HE, Katz JN. Orthopaedic procedure volume and patient outcomes: a systematic literature review. Clin Orthop Relat Res. 2007;457:35–41. doi: 10.1097/BLO.0b013e3180375514. [DOI] [PubMed] [Google Scholar]
- 18.Khan F, Ng L, Gonzalez S, Hale T, Turner-Stokes L (2008) Multidisciplinary rehabilitation programmes following joint replacement at the hip and knee in chronic arthropathy. Cochrane Database Syst Rev 2:CD004957 [DOI] [PMC free article] [PubMed]
- 19.Jolles BM, Bogoch ER (2006) Posterior versus lateral surgical approach for total hip arthroplasty in adults with osteoarthritis. Cochrane Database Syst Rev 3:CD003828 [DOI] [PMC free article] [PubMed]
- 20.Morshed S, Bozic KJ, Ries MD, Malchau H, Colford JM. Comparison of cemented and uncemented fixation in total hip replacement: a meta-analysis. Acta Orthop. 2007;78(3):315–326. doi: 10.1080/17453670710013861. [DOI] [PubMed] [Google Scholar]
- 21.Pakvis D, van Hellemondt G, de Visser E, Jacobs W, Spruit M. Is there evidence for a superior method of socket fixation in hip arthroplasty? A systematic review. Int Orthop. 2011;35(8):1109–1118. doi: 10.1007/s00264-011-1234-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bream E, Black N. What is the relationship between patients' and clinicians' reports of the outcomes of elective surgery? J Health Serv Res Policy. 2009;14(3):174–182. doi: 10.1258/jhsrp.2009.008115. [DOI] [PubMed] [Google Scholar]
- 23.Riddle DL, Stratford PW, Bowman DH. Findings of extensive variation in the types of outcome measures used in hip and knee replacement clinical trials: a systematic review. Arthritis Rheum. 2008;59(6):876–883. doi: 10.1002/art.23706. [DOI] [PubMed] [Google Scholar]
- 24.Mariconda M, Galasso O, Costa GG, Recano P, Cerbasi S. Quality of life and functionality after total hip arthroplasty: a long-term follow-up study. BMC Musculoskelet Disord. 2011;12:222. doi: 10.1186/1471-2474-12-222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zwartele RE, Witjes S, Doets HC, Stijnen T, Poll RG. Cementless total hip arthroplasty in rheumatoid arthritis: a systematic review of the literature. Arch Orthop Trauma Surg. 2012;132(4):535–546. doi: 10.1007/s00402-011-1432-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McMinn DJ, Snell KI, Daniel J, Treacy RB, Pynsent PB, Riley RD. Mortality and implant revision rates of hip arthroplasty in patients with osteoarthritis: registry based cohort study. BMJ. 2012;344:e3319. doi: 10.1136/bmj.e3319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Brooks R. EuroQol: the current state of play. Health Policy. 1996;37(1):53–72. doi: 10.1016/0168-8510(96)00822-6. [DOI] [PubMed] [Google Scholar]
- 28.Shi HY, Chiu HC, Chang JK, Wang JW, Culbertson R, Khan MM. Evaluation and prediction of health-related quality of life replacement among Chinese in Taiwan. Int Orthop. 2008;32(1):27–32. doi: 10.1007/s00264-006-0268-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shi HY, Khan M, Culbertson R, Chang JK, Wang JW, Chiu HC. Health-related quality of life after total hip replacement: a Taiwan study. Int Orthop. 2009;33(5):1217–1222. doi: 10.1007/s00264-008-0682-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Montin L, Leino-Kilpi H, Suominen T, Lepisto J. A systematic review of empirical studies between 1966 and 2005 of patient outcomes of total hip arthroplasty and related factors. J Clin Nurs. 2008;17(1):40–45. doi: 10.1111/j.1365-2702.2007.01944.x. [DOI] [PubMed] [Google Scholar]
- 31.Beswick AD, Wylde V, Gooberman-Hill R, Blom A, Dieppe P. What proportion of patients report long-term pain after total hip or knee replacement for osteoarthritis? A systematic review of prospective studies in unselected patients. BMJ Open. 2012;2(1):e000435. doi: 10.1136/bmjopen-2011-000435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wroblewski BM, Siney PD, Fleming PA. Charnley low-frictional torque arthroplasty: follow-up for 30 to 40 years. J Bone Joint Surg Br. 2009;91(4):447–450. doi: 10.1302/0301-620X.91B4.21933. [DOI] [PubMed] [Google Scholar]
- 33.Della Valle CJ, Mesko NW, Quigley L, Rosenberg AG, Jacobs JJ, Galante JO. Primary total hip arthroplasty with a porous-coated acetabular component. A concise follow-up, at a minimum of twenty years, of previous reports. J Bone Joint Surg Am. 2009;91(5):1130–1135. doi: 10.2106/JBJS.H.00168. [DOI] [PubMed] [Google Scholar]
- 34.Alviar MJ, Olver J, Brand C, Tropea J, Hale T, Pirpiris M, et al. Do patient-reported outcome measures in hip and knee arthroplasty rehabilitation have robust measurement attributes? A systematic review. J Rehabil Med. 2011;43(7):572–583. doi: 10.2340/16501977-0828. [DOI] [PubMed] [Google Scholar]