Treatment Options for Severe Epistaxis, the Experience of Coltea ENT Clinic (original) (raw)
Abstract
Objectives:
The study presents the experience of the Coltea ENT Clinic with the most common emergency in ENT pathology.
Results:
The study group comprises 51.24% women and 48.76% men with 73.14% of patients (177) coming from urban areas and the remaining 26.86% (65) from rural areas. The total number of days of hospitalization is 1411, representing an average of 5.83 days / patient. Epistaxis was anterior in 80.17% of cases (194 patients) and antero-posterior in 19.83% (48 patients). 132 patients, representing 54.55% presented elevated blood pressure whereas liver and hematological disorders are uncommon etiologies. Therapeutic interventions are mostly non-surgical 207 (85.54%), the remaining 35 cases (14.46%), requiring surgery.
Conclusions:
Epistaxis associated with high blood pressure is found in 54.55% of the study group. In 38.02% of cases the etiology cannot be determined. Pluri-factorial etiology is common. The most difficult to control were the cases with epistaxis of hepatic etiology, in which cases the surgical solution was required.
Keywords: gonarthrosis, high tibial osteotomy, tibial slope
BACKGROUND
Epistaxis is the most frequent emergency in ENT practice with a prevalence of 10-12%. It has an incidence of 30/100.000 and 60% of the general population experienced at least one episode during lifetime. Most frequently epistaxis is encountered between the ages of 10 to 50 years. Some studies report a male predominance but others consider an equal distribution between sexes. Cold weather with low humidity increases the risk of nose bleeding (1-4). Median duration of hospitalization per bleeding is approximately 3-4 days (2,5).
The source of nasal bleeding is in 80-90% of the cases anterior (6). The etiology of epistaxis may be local or systemic. Local causes of epistaxis are encountered in more than 90% of the cases. The specialist encounters the following local causes: trauma, micro strain, rhinitis, tumors, iatrogenic. Systemic causes are: hypertension, hematologic conditions, hepatic insufficiency, anticoagulant medication, rheumatic disease, diabetes, malignancies, systemic infections and intoxications.
Epistaxis is associated with physiologic conditions like physical effort, pregnancy, menstruation, puberty and menopause (2,7,8).
The treatment of epistaxis comprises general measures, local or general hemostasis, followed by surgery or embolization if the bleeding continues (9).
Local techniques for controlling the epistaxis are bipolar diathermy, balloon compression, anterior and posterior nasal packing (7,8,10).
The majority of cases are responsive to local techniques, the bleeding being stopped in 80% of the situations (5).
Postnasal packing presents a rate of failure of 52%. Vascular ligation instead of classic packing shortens the period of hospitalization, and is successful in 90% of the cases lowering the costs (6).
Surgical treatment uses vascular ligation of anterior ethmoidal artery or posterior ethmoidal artery, ligation of the internal maxillary artery or ligation of the external carotid artery (7,8).
Selective embolization is a method used in the case of failure of conservative and surgical treatment, the rate of success with embolization is around 90% (4,6). ❑
OBJECTIVES
The present study illustrates the impact of epistaxis and the possible management of this condition by the ENT specialist. Furthermore we analyze the evolution of patients with local versus systemic conditions and the rate of recurrence after the use of different treatment options. ❑
MATERIALS AND METHODS
This retrospective study comprises the patients admitted to Coltea Clinical Hospital between 01.01.2012 and 31.12.2012. We recorded 270 cases with bleeding from ENT pathology, 242 presenting both anterior and posterior. Inclusion criteria: primary diagnosis at discharge epistaxis. We did not take into consideration those patients with epistaxis that were not admitted to our ENT department. We checked for readmissions of these patients in our unit during 2012 and 2013 in order to ascertain recurrence rate. During admission all patients signed an Informed Consent that was elaborated by the Ethics Committee at Coltea Clinical Hospital in compliance with the Declaration of Helsinki and current Good Clinical Practice. ❑
RESULTS
During 2012, 2952 patients were treated in the ENT department. From these 242 patients (7.58%) presented epistaxis. A total of 1411 days of hospitalization were generated by these patients with a mean period of 5.83 days per patient.
There is an almost equal distribution per sex of the study group, 51.24% female and 48.76% male. The majority of patients come from urban areas, 73.14%, but this could be attributed to the fact that our unit serves as a 24 hours ENT emergency department for Bucharest and surrounding area.
The distribution of the cases per age groups is shown in Table 1.
Table 1.
Distribution of patients per age groups
| Age groups | Number of patients | Percentage |
|---|---|---|
| 15 - 24 | 11 | 4.55% |
| 25 - 34 | 36 | 14.88% |
| 35-44 | 31 | 12.81% |
| 45 - 54 | 41 | 16.94% |
| 55 - 64 | 63 | 26.03% |
| 65 - 74 | 37 | 15.29% |
| 75 - 84 | 16 | 6.61% |
| >85 | 7 | 2.89% |
| Total | 242 | 100% |
The source of epistaxis was anterior in 80.17% of the cases (194 patients) and combined – anterior and posterior – in 19.83% (48 patients).
Table 2 summarizes the frequency of different etiologies inside the study group.
Table 2.
Etiology of epistaxis inside the study group
| Etiology | Number of patients | Percentage |
|---|---|---|
| Idiopathic | 92 | 38.02% |
| Hypertension | 132 | 54.55% |
| Liver dysfunction | 4 | 1.65% |
| Hematologic diseases | 3 | 1.24% |
| Neoplasm | 4 | 1.65% |
| Benign tumors | 12 | 4.6% |
| Trauma | 15 | 6.20% |
| Rhinitis | 13 | 5.37% |
In 38.02% of the cases, 92 patients, the exact etiology could not be identified. Some of the patients presented multiple etiologies associating hypertension with liver, hematologic and infectious pathologies.
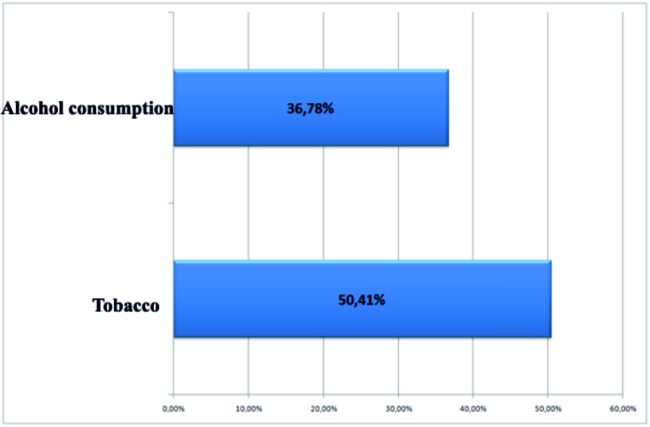
The impact of general risk factors such as tobacco and alcohol consumption is illustrated in Figure 1.
Figure 1. Risk factors.
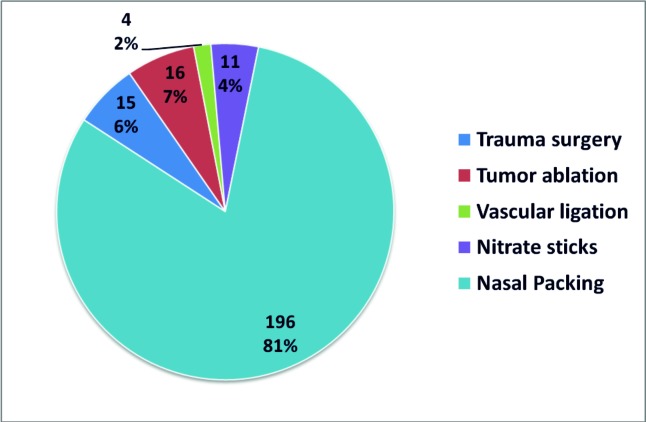
The different treatment options applied to the study group are recorded in Figure 2. Non-surgical treatment included anterior nasal packing and the use of nitrate sticks. Surgical treatment meant the management of trauma, tumor ablation (benign and malignant) and vascular ligation.
Figure 2. Treatment.
Table 3 summarizes the recurrence rate till the end of 2013 in the following subgroups: idiopathic cause, systemic cause, local cause and taking into consideration the treatment options: surgical or non-surgical. ❑
Table 3.
Recurrence rate at one year follow up
| Number of patients | Recurrence | Percentage | |
|---|---|---|---|
| Idiopathic | 92 | 24 | 26.08% |
| Systemic cause | 106 | 18 | 16.98% |
| Local cause | 44 | 6 | 13.63% |
| Surgical treatment | 35 | 6 | 17.14% |
| Non-surgical treatment | 207 | 42 | 20.28% |
DISCUSSIONS
Simultaneous anterior and posterior epistaxis is frequent in ENT practice. 7.58% of the cases treated in our ENT department during 2012 presented with nasal bleeding. Literature data are similar. The number of patients presenting with this problem is much larger because we analyzed only the cases that were hospitalized and not treated in the outpatient clinic. The number of days with hospitalization per patient is greater than data presented by other studies: 5.8 versus 3-4 days (1-5).
There were 51.24% of women and 48.76% of men, and the majority of patients were between 55 and 74 years (41.32%). These data are consistent with other studies (1-4).
The main cause for epistaxis according to our data is hypertension (54.55% of the patients). There are other studies that do not support the correlation between the two conditions (5), other state the correlation as possible (6). But the rule tends to underline the association between epistaxis and hypertension (8).
Liver dysfunctions (1.65%) and hematologic pathology (1.24%) were the most infrequent etiologies but these cases presented with the most severe bleedings. However in 38.02% of the cases epistaxis seems to be idiopathic.
Similarly to worldwide practice 85.54% of the cases were resolved through non-surgical measures (1-4,6,8).
The most difficult cases were those with hepatic etiology. In all 4 cases was used the surgical alternative of treatment, meaning the ligation of the external carotid artery (unilateral ligation in 3 patients and another one with bilateral ligation).
The 26.08% recurrence rate in the idiopathic control group suggests that many of these cases have an unknown cause due to probably insufficient investigation of the patient. ❑
CONCLUSIONS
The present study illustrates the fact that although apparently common and benign epistaxis can be a symptom of a life threatening condition requiring a team effort uniting specialists from various departments inside a tertiary medical unit. The great number of cases with systemic conditions such as hypertension underlines the fact that many of our patients either do not follow the instructions of their family doctor or do not receive annual evaluations of their health status due to low income or low accessibility to medical care.
CONFLICT OF INTEREST
none declared.
FINANCIAL SUPPORT
none declared.
References
- 1.Kucik CJ, Clenney T. Management of Epistaxis. Am Fam Physician. 2005;71:305–311. [PubMed] [Google Scholar]
- 2.Varshney S, Saxena RK. Epistaxis: A retrospective clinical study. Indian J Otolaryngol Head Neck Surg. 2005;57:125–9. doi: 10.1007/BF02907666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Faistauer M, Faistauer A, Grossi RS, et al. Clinical outcome of patients with epistaxis treated with nasal packing after hospital discharge. Braz J Otorhinolaryngol. 2009;75:857–65. doi: 10.1016/S1808-8694(15)30550-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Willems PWA, Farb RI, Agid R. Endovascular Treatment of Epistaxis. AJNR. 2009;30:1637–1645. doi: 10.3174/ajnr.A1607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hassan HR, Ali A El Solh. An Update on Otolaryngology in Critical Care. Am J Respir Crit Care Med. 2004;169:1273–1277. doi: 10.1164/rccm.200402-222UP. [DOI] [PubMed] [Google Scholar]
- 6.Douglas R, Wormald PJ. Update on epistaxis. Curr Opin Otolaryngol Head Neck Surg. 2007;15:180–3. doi: 10.1097/MOO.0b013e32814b06ed. [DOI] [PubMed] [Google Scholar]
- 7.Fuchs FD, Moreira LB, Pires CP, et al. Absence of association between hypertension and epistaxis: a population-based study. Blood Press. 2003;12:145–148. doi: 10.1080/08037050310001750. [DOI] [PubMed] [Google Scholar]
- 8.Page C, Biet A, Liabeuf S, et al. Serious spontaneous epistaxis and hypertension in hospitalized patients. Eur Arch Otorhinolaryngol. 2011;268:1749–53. doi: 10.1007/s00405-011-1659-y. [DOI] [PubMed] [Google Scholar]
- 9.Codarcea-Munteanu D. Epistaxis in emergency medical practice in ENT clinic Brasov. Bulletin of the Transilvania University of Brasov. 2012;5(54):No1–No1. [Google Scholar]
- 10.Isezuo SA, Segun-Busari S, Ezunu E, et al. Relationship between epistaxis and hypertension: a study of patients seen in the emergency units of two tertiary health institutions in Nigeria. Niger J Clin Pract. 2008;11:379–382. [PubMed] [Google Scholar]