Improving postpartum care for mothers and newborns in Niger and Mali: a case study of an integrated maternal and newborn improvement programme (original) (raw)
Abstract
Despite appropriate guidelines, healthcare services worldwide often fail to deliver high-impact evidence-based care. This case study describes a large-scale programme to improve integrated postpartum care for mothers and newborns in Niger and Mali. As a result of an improvement effort based on common objectives, local ownership and shared learning to accelerate implementation of best practices, 78 facilities demonstrated rapid improvement in compliance with standards for post-partum haemorrhage prevention and Essential Newborn Care as well as a reduction in estimated postpartum haemorrhage. This approach yields rapid results and can be efficiently spread to improve care in low-resource settings.
Keywords: Health systems, information systems, maternal, newborn, quality improvement, supervision, training
Description of postpartum improvement intervention in Niger and Mali
Despite the proven efficacy of high-impact clinical interventions to reduce adverse outcomes such as postpartum haemorrhage (PPH), the correct use of these practices is often limited in resource-constrained settings.1 Closing the ‘know–do gap’ between proven interventions and their reliable implementation at scale requires innovative approaches that support local actors to be change agents. We report the findings of a large-scale programme to improve the quality of maternal and newborn care in two West African countries, Niger and Mali.
Niger and Mali have some of the highest maternal (590 per 100 000 and 540 per 100 000, respectively) and newborn (32 per 1000 and 49 per 1000, respectively) mortality rates in the world with low levels of institutional delivery (30% and 50%, respectively).2–4 Women who do deliver in facilities often receive low-quality care that does not meet evidence-based standards. The United States Agency for International Development (USAID) funded the Quality Assurance Project and its successors, the USAID Health Care Improvement (HCI) and USAID Applying Science to Strengthen and Improve Systems (ASSIST) projects, to assist the Ministry of Health (MoH) of Niger from 2006 to 2008 and the MoH of Mali from 2009 to the present to improve the quality of maternal and newborn services in public sector maternities. In each country, the maternal and newborn healthcare (MNH) improvement programme was jointly designed and implemented by the MoH and project representatives.
The MNH improvement programme was implemented first in 37 maternity facilities in Niger (2006–08) and then extended to 41 maternity facilities in Mali (2009–12) (Figure 1). The programme goal was to improve quality of care for mothers and newborns with an initial focus on routine high-impact interventions needed by every mother and newborn and a subsequent focus on obstetric and neonatal complications. This case study describes the programme approach to improving adherence with routine postpartum standards of care for mothers and newborns including (1) active management of the third stage of labour (AMTSL); (2) essential newborn care (ENC) and (3) routine monitoring of mother and newborn after birth (subsequent clinical programme phases addressed or are currently addressing improved management of pre-eclampsia/eclampsia, anaemia and newborn asphyxia). AMTSL is a package of three interventions administered just after birth—administration of oxytocin, controlled cord traction and uterine massage—demonstrated to reduce PPH by over 50%.5 PPH is the leading cause of maternal mortality in Niger and Mali. ENC is a package of interventions demonstrated to reduce neonatal mortality including early and exclusive breastfeeding, thermal protection (skin-to-skin and wrapping) and clean umbilical care. Adherence to AMTSL, ENC and postpartum monitoring of mother and newborn was low in targeted maternities in Niger and Mali at the outset of the programme.
Figure 1.
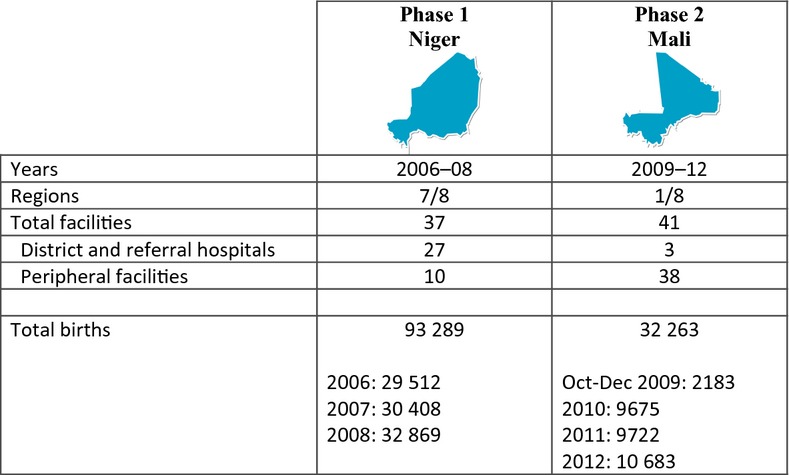
Geographic phases of the EONC programme.
The MNH programme applied a collaborative improvement strategy to improve quality of care for mothers and newborns. The programme strategy, based on an adaptation of the US Institute for Healthcare Improvement Breakthrough Series,6 combined continuous shared learning across multiple facilities with basic principles of improvement, including: (1) engaging teams of healthcare providers, managers and staff in improving care; (2) analysing how processes of care function within a system; (3) changing processes and systems of care to implement best practices; and (4) continuous analysis of data to assess results. Key improvement strategies used in the MNH improvement programme in Niger and Mali are summarised in Box 1. In Phase one in Niger (2006–08), a technical advisory group comprised of MoH and country and international experts prioritised selection and phasing of measurable improvement aims based on high-burden conditions with proven interventions. The technical advisory group decided that the programme should focus first on ‘low-hanging fruit’, routine best practices applicable for every mother and newborn, and address the more challenging management of obstetric and neonatal complications in subsequent phases. Common indicators were developed for each improvement aim to enable individual sites to track progress in real time against aims and to allow aggregation of results across all sites to assess collective progress by senior MoH managers and project staff (Box 2). A focused baseline assessment was done in Niger but not in Mali due to resource constraints. The design of the improvement work in Niger guided subsequent programme implementation in both Niger and Mali. The MNH programme in Niger built on the experience of a previous pediatric referral hospital improvement programme, accounting for the proportionally higher number of referral hospitals in Niger than in Mali (Figure 1).
Box 1. Key improvement strategies
- Upfront articulation of measurable, feasible improvement aims and indicators based on burden of MNH disease and proven clinical best practices (Phase one, Niger).
- Creation of national expert group (MoH, local experts, project and partner staff) to lead design and implementation of MNH improvement programme, including adaptation of international standards to country context (Niger and Mali).
- Focused baseline assessment (Niger) to measure quality gaps and engage local stakeholders in identifying obstacles to implementation of best practices.
- Integrated ‘implementation package’ to empower front-line facility teams to continually improve care with respect to shared objectives (on-site simultaneous clinical/improvement/data management training; monthly calculation and analysis of common indicators, supportive supervision, regular shared learning).
- Periodic supportive supervision visits to facility teams by regional MoH managers and country experts, with support of project staff.
- Monthly calculation and analysis of common indicators by all site teams (extracted from local data) with aggregation of indicator results at district, regional and national level by MOH point persons.
- Quarterly to bi-annual regional ‘learning sessions’ meetings to accelerate shared learning.
- Regular synthesis of evolving ‘best practices’ to support spread across sites within each country and from Niger to Mali.
MNH, maternal and newborn healthcare; MoH, Ministry of Health.
Box 2. Quality of care indicators tracked by sites on a monthly basis
- Percentage of births benefiting from AMTSL (10 units oxytocin within 1 minute of delivery of fetus, controlled cord traction, uterine massage)
- Estimated PPH rate (vaginal bleeding estimated at >500 ml or any bleeding with change in clinical status (e.g. tachycardia) per 100 births)
- % newborns for whom minimum ENC standards met (breastfeeding within 1 hour of birth, thermal protection, eye care (tetracycline ointment) and clean umbilical care, bacillus Calmette–Guérin vaccination)
- % mothers monitored postpartum per minimum standard (Phase 2 Mali) (assessment of uterine firmness, vaginal bleeding, blood pressure, pulse, temperature every 30 minutes for first 2 hours then twice per day)
- % newborns monitored postpartum per minimum standard (Phase 2 Mali) (assessment of temperature, colour, respirations, breastfeeding/feeding status every hour for first 4 hours then twice per day)
AMTSL, active management of the third stage of labour; ENC, essential newborn care; PPH, postpartum
Programme activities in both Niger and Mali were led by national, regional and district MoH managers working in close collaboration with project staff. A facility improvement team was formed in every maternity comprised of providers, managers, a pharmacy and laboratory representative and other staff as relevant. Facility teams were oriented on-site to the objectives and methods of the MNH improvement programme and were provided with guidelines, tools and periodic in-person and telephone support. Team role playing was used to build team capacity and troubleshoot common problems encountered by teams. On average, facility teams met on a weekly basis, maintaining meeting minutes and usually rotating the chair function.
In the first phase of implementation, priority was given to building integrated clinical, quality improvement and data skills among facility teams. On-site competency-based clinical training (1–2 days) using simulation with a mannequin linked to real-life practice during night shifts helped to build individual provider and team skills for delivery of integrated postpartum best practices for mother and newborn. Providers were taught to estimate blood loss using calibrated buckets and cloth wrappers. Certificates were awarded to individual providers meeting a minimum standard of performance.
During on-site training providers were supported to identify local obstacles to adoption of best practices in their facility and to brainstorm promising changes that they could test to overcome local barriers to achieving reliable implementation of postpartum best practices for every mother and newborn. During on-site integrated clinical and improvement training, team members analysed and modified their facility records (if needed) to permit capture of essential data for calculation of common programme quality of care indicators (Box 2). Facility teams were taught to calculate and analyse the common quality of care indicators on a monthly basis to assess their progress (or lack of progress) toward improvement aims. Indicators were calculated as ‘all or nothing adherence’ with a set of minimum standards (Box 2).
MoH managers and clinician experts with support from project staff periodically visited participating sites (usually quarterly and often as part of routine MoH supervision using MoH vehicles). Generally supervision visits lasted 2–3 hours and included a team meeting to review progress and problem-solve, refresher clinical training, and review of changes tested by teams. Supervisors spot-checked indicator results calculated by teams against primary data in facility registers and helped teams to correct any errors and to analyse their results. A written action plan was agreed at the end of every supervision visit. Teams sent their facility indicator results to a monitoring point person on the nearest regional or district health management team on a monthly basis. This point person in turn aggregated results across all sites in his or her catchment area.
During both programme phases in Niger and Mali (except during temporary suspension of activities in Mali due to the 2011 coup d'état) project staff collaborated with MoH counterparts to organise quarterly to bi-annual regional ‘learning sessions’ during which facility team representatives shared and synthesised successful changes being adopted in participating maternities to improve adherence with AMTSL, ENC and postpartum monitoring standards. As the programme evolved in Niger and Mali, emerging facility and MoH ‘improvement champions’ were recruited to help lead programme activities at regional levels, including deliberate cross-pollination of best practices from high-performing to lower-performing sites.
When the MNH programme expanded to Mali in 2009, Niger-based HCI/ASSIST staff made regular visits to Mali to build capacity of Mali MoH stakeholders and Mali-based HCI/ASSIST staff to implement the postpartum improvement intervention capitalising on learning from Niger. Successful changes adopted by Niger facility teams to improve adherence with postpartum best practices were synthesised and shared with maternity improvement teams in Mali. Successful changes in the Niger context were found to be highly relevant in neighbouring Mali and helped to accelerate improved adherence with postpartum best practices in the 41 Mali maternities. Priority was given in both countries to positioning front-line providers and managers with in-depth knowledge of their local setting to identify and test solutions to implement postpartum best practices for every mother and newborn; special priority was given to mentoring local ‘improvement champions’. Emerging best practices were continually synthesised and disseminated across sites to accelerate shared learning.
Results
Table 1 and Figure 2 show baseline values and indicator results of the MNH improvement programme in Niger (January 2006 to December 2008) and in Mali (October 2009 to December 2012). Box 3 lists successful changes tested and adopted by facility teams in Niger and Mali to improve adherence with AMTSL, ENC and routine postpartum monitoring of mothers and newborns. Participating facilities recorded rapid improvement in percentage of births benefiting from AMTSL and ENC best practices while recording a concomitant reduction in estimated PPH rate. The percentage of births benefiting from AMTSL increased from 2% at baseline to >90% in Niger and from 17% in the first month of reporting to 95–97% in Mali. The estimated PPH rate decreased by 90% from 2.2% to 0.2% of vaginal deliveries in Niger sites, and from 0.9% to less than 0.3% on average in Mali sites. The percentage of births benefiting from ENC increased from 16% in a baseline assessment to 96% in Niger and from 25% to 99% in Mali. Adherence to a set of postpartum minimum monitoring standards for mother and newborn for early detection of complications increased from 19% to 86% and from 19% to 89% in Mali, respectively (not measured as a discrete indicator in Niger). Minimum postpartum monitoring standards for mother and newborn are summarised in Box 2.
Table 1.
ENC and maternal newborn postpartum monitoring results in facilities participating in Niger and Mali MNH programme
| Baseline | 1 month | 3 months | 6 months | 12 months | 18 months | 24 months | 36 months | |
|---|---|---|---|---|---|---|---|---|
| Niger—% of newborns for whom ENC standards were met | 16% | 45 | 87 | 95 | 98 | 98 | 99 | 96 |
| Mali—% of newborns for whom ENC standards were met | N/A | 25 | 46 | 75 | 94 | 95 | 97 | 99 |
| Mali—% of newborns monitored postpartum per standards | N/A | 19 | 26 | 90 | 98 | 99 | 97 | 89 |
| Mali—% of mothers monitored postpartum per standards | N/A | 19 | 24 | 89 | 98 | 96 | 97 | 86 |
Figure 2.
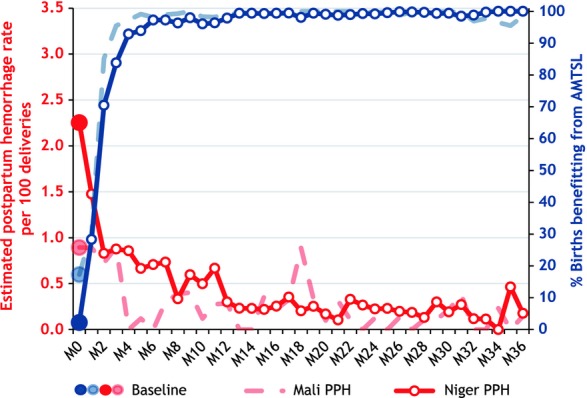
Postpartum haemorrhage rate and percentage of births benefiting from AMTSL by month of implementation in facilities participating in Niger and Mali MNH programme.
Box 3. Examples of changes implemented by quality improvement teams in Niger and Mali MNH programme
- Instituting staff-led 24-hour call schedules to ensure presence of a skilled birth attendant at all births (historically, auxiliary nurses often performed deliveries during night and weekend hours).
- Restructuring of service flow to include distinct admission/triage, labour, delivery/immediate postpartum and early postpartum care areas (e.g. curtain dividers) to improve care efficiency and privacy for women; restructuring of staff roles with specific assigned tasks for each phase of care.
- Maintenance of essential commodities in area designated for each care phase.
- Placement of locally purchased coolers in delivery area to maintain oxytocin at required cold temperatures at the bedside in a setting subject to frequent power outages.
- Preparation and placement of pre-filled oxytocin syringes and two dry cloths at the bedside during second stage of labour to facilitate immediate postpartum administration of oxytocin for mother and immediate skin-to-skin and drying and wrapping of the newborn (many deliveries attended by a single provider).
- Modest modifications of facility records and registers (as needed) to remind providers to implement and record best practices and to permit monthly calculation of quality of care indicators by facility teams (e.g. local rubber stamp to imprint AMTSL/ENC check-off boxes in partogram; insertion of columns in registers to track postpartum vital signs of mother and newborn).
- Delayed bathing of newborns (historically, newborns bathed within first two hours of birth by auxiliary maternity staff in Niger and Mali maternities to improve adherence with postpartum best practices); not placing bandage (‘pensement’) on umbilical cord.
AMTSL, active management of the third stage of labour; ENC, essential newborn care.
Strengths
The bottom-up approach used in this case study yielded rapid improvements in the adoption of a high impact, integrated postpartum package for over 100 000 mothers and newborns across 78 maternities in Niger and Mali from 2006 through 2012. A strength of the programme design was the upfront articulation of common feasible and measurable improvement aims based on high-burden conditions and a bundle of integrated interventions for mother and newborn during the high-mortality early postpartum period. The initial focus on a relatively simple clinical intervention package likely facilitated rapid results allowing teams to focus on a manageable intervention package while acquiring clinical skills (subsequent improvement work on eclampsia and newborn asphyxia in subsequent programme phases has benefited from established team improvement competencies although improvement has been more gradual for these more complex conditions).
The capacity building of local providers and managers as the ‘owners’ of improvement was likely an important contribution to the results. The emphasis on egalitarian team functioning, including shared decision making and responsibility for results, probably helped to soften institutional power hierarchies and to facilitate local innovation and continuous improvement. The strong emphasis on regular data collection and analysis of quality of care measures by facility staff and managers (facility and regional) helped to build local data management capacity and to strengthen local information systems. Over time, many facility teams and managers expressed pride in their capacity to independently improve and measure quality of care; improving care was no longer seen as the purview of ‘QI specialists’.
The focus on the system rather than on the individual provider or manager helped to sustain results despite staff turnover and to facilitate more open sharing of failures and successes essential for continuous improvement. Results suggest that gains are being sustained over time; during the coup d'état in Mali most participating sites continued to measure and report on quality indicators. A follow-up study in Niger demonstrated the sustaining of AMTSL and ENC results up to 20 months after external support ended in a sample of 20 former programme sites.7
The relatively low cost of implementation is a major strength of the MNH improvement programme described in this case study. The total cost of designing and implementing the programme in Niger was 771400(771 400 (771400(188 400 and 583400,respectively)forthefunderand583 400, respectively) for the funder and 583400,respectively)forthefunderand403 000 for the MoH.8 The average delivery cost in Niger decreased from 35.00beforeto35.00 before to 35.00beforeto28.00 after implementation of the postpartum intervention due to the decrease in PPH rate.8 Implementation in Mali was able to begin more efficiently than in Niger due to prior program design, implementation experience and learning in Niger.
Weaknesses
A weakness of the approach was the requirement for initial external technical and financial support by the USAID Quality Assurance Project and HCI projects. Another inevitable weakness was the dependence of site-specific improvement work on local leadership support; sites with strong managers generally performed at a higher level than sites with weak or disengaged managers. In Mali, baseline adherence with postpartum best practices was relatively stronger than in Niger; the presence of other partners in Mali including the United Nations Children's Fund and USAID's bilateral and Maternal and Child Health Integrated Program probably contributed to the higher baseline performance and subsequent measured gains in Mali.
The lack of independent external measurement is a weakness of this case study. Although priority was given during clinical training and site visits to building team data skills, results are based on site self-assessment and may be biased. Because the programme was designed as a quality improvement intervention in a highly resource-constrained setting it was decided early on to invest precious resources in building local capacity for continuous measurement rather than in resource-intensive external assessments. A related weakness is that PPH rates are based on provider estimates rather than on an objective measurement method. Although strong emphasis was placed on building provider capacity to correctly estimate blood loss and to diagnose PPH, more rigorous measurement (e.g. use of a calibrated drape) was beyond the means of this large-scale improvement programme. The lower than expected provider-estimated PPH rates in participating facilities suggest that providers underestimated the true incidence of PPH.
An important weakness, being addressed in the current phase (2013/14) of the Mali MNH improvement programme, is the lack of community and demand-side interventions in this case study. In a setting with low institutional delivery rates it is vital that improvement efforts address community and demand-side factors in combination with supply-side factors. Finally, a weakness is the lack of a clear mechanism to promote continuous improvement in new clinical areas after the end of the programme. An improvement collaborative is intended to be a temporary approach to bring about rapid change in a priority clinical area; other long-term strategies are probably necessary to institutionalize continuous improvement of maternal and newborn care. It is hoped, however, that the programme emphasis on building improvement competencies among MoH managers and facility staff and subsequent focus on additional clinical priority areas (eclampsia, anemia, asphyxia, post-partum family planning) will help to mitigate this weakness over time.
Opportunities
Governments and partners are keenly interested in replicable and affordable approaches to scale up and sustain improved quality of care for mothers and newborns to end preventable deaths. In many countries, decentralisation of healthcare systems is empowering local managers to choose approaches that they believe will best help them to achieve results; the approach used in this case study is readily adaptable by regional and district managers. The supervision visits and other structural meetings that occur regularly in a local health system provide a natural mechanism to implement the core components of the described approach.
Conclusions
- A multi-faceted improvement approach based on common measurable aims, local ownership and shared learning across multiple sites can yield rapid improvements in quality of care for mothers and newborns and can help strengthen local health system functions (e.g. health information system, health worker support) in resource-constrained settings.
- It is possible to close the ‘know–do’ gap between proven best practices and actual practice when front-line providers and managers are supported to test and adopt successful changes to overcome local obstacles.
- The approach described in this case study is cost-effective and can be efficiently spread to new geographic and technical areas and shows promising signs of sustainability.
Acknowledgments
The authors gratefully acknowledge the efforts of our many colleagues in Niger and Mali including MoH officials, expert clinicians and the many providers, staff and managers from participating clinics and hospitals; this case study describes the results of their collective efforts and hard work. The authors are thankful for the valuable feedback and contributions of Edward Broughton, Lani Marquez and Jorge Hermida of the USAID ASSIST project. The authors are grateful for the ongoing technical support of Lily Kak, USAID Senior Newborn Advisor, and Deborah Armbruster, Director of the former USAID Prevention of Postpartum Hemorrhage Initiative (POPPHI) and currently USAID Senior Maternal Health Advisor.
Disclosure of interests
We declare no conflicts of interest.
Contribution to authorship
MB, KH and AC conceptualised and wrote the first and subsequent drafts of the article. SH supported data analysis and presentation of data. SD, ZS, KS and EK contributed to the discussion and results sections.
Funding
This work was supported by in-kind contributions of the Niger and Mali Ministries of Health and by the American people through the United States Agency for International Development (USAID) and its Health Care Improvement (HCI) and Applying Science to Strengthen and Improve Systems (ASSIST) projects. The USAID HCI and ASSIST project are managed by University Research Co., LLC (URC).
References
- 1.Stanton C, Armbruster D, Knight R, Ariawan I, Gbangbade S, Getachew A, et al. Use of active management of the third stage of labour in seven developing countries. Bull World Health Organ. 2009;87:207–15. doi: 10.2471/BLT.08.052597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization and UNICEF. Countdown to 2015. Building a Future for Women and Children: the Countdown 2012 Report. Geneva: WHO and UNICEF; 2012. [ http://www.countdown2015mnch.org/documents/2012Report/2012-Complete.pdf]. Accessed 22 November 2013. [Google Scholar]
- 3.Institut National de la Statistique (INS) et ICF International. Enquête Démographique et de Santé et à Indicateurs Multiples du Niger 2012. Calverton: INS et ICF International Inc; 2012. MD: [Google Scholar]
- 4.INFO-STAT Cellule de Planification et de Statistique du Ministère de la Santé (CPS Institut national de la Statistique du Ministère de l'Économie, de l'Industrie et du Budget (INSTAT) et ICF International Inc. Enquête Démographique et de Santé du Mali 2012-2013. Rapport Préliminaire. Calverton, MD: CPS/DNSI et ICF International; 2013. [Google Scholar]
- 5.Begley CM, Gyte GML, Devane D, McGuire W, Weeks A. Active versus expectant management for women in the third stage of labour. Cochrane Database Syst Rev. 2011;(11):CD007412. doi: 10.1002/14651858.CD007412.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.The Breakthrough Series. IHI's Collaborative Model for Achieving Breakthrough Improvement. IHI Innovation Series white paper. Boston: Institute for Healthcare Improvement; 2003. [Google Scholar]
- 7.Boucar M, Franco LM, Sabou D, Saley Z, Jennings L, Mohan D. Sustaining Better Maternal and Newborn Care and Quality Improvement in Niger: Challenges and Successes. Research and Evaluation Report. Bethesda, MD: USAID Health Care Improvement Project; 2011. [Google Scholar]
- 8.Broughton E, Saley Z, Boucar M, Alagane D, Hill K, Marafa A, et al. Cost-effectiveness of a quality improvement collaborative for obstetric and newborn care in Niger. Int J Health Care Qual Assur. 2013;26:250–61. doi: 10.1108/09526861311311436. [DOI] [PubMed] [Google Scholar]
- 9.Frenk J. The global health system: strengthening national health systems as the next step for global progress. PLoS Med. 2010;7:e1000089. doi: 10.1371/journal.pmed.1000089. [DOI] [PMC free article] [PubMed] [Google Scholar]