Superior canal dehiscence syndrome associated with scuba diving (original) (raw)
Abstract
A 28-year-old female diver presented with dizziness and difficulty clearing her left ear whilst scuba diving. Her pure-tone audiometry and tympanometry were normal. Testing of Eustachian tube function revealed tubal stenosis. Video-oculography revealed a predominantly torsional nystagmus while the patient was in the lordotic position. Fistula signs were positive. High-resolution computed tomography (HRCT) of the temporal bone revealed a diagnosis of bilateral superior semicircular canal dehiscence (SCDS). Cervical vestibular-evoked myogenic potential (cVEMP) testing showed that the amplitude of the cVEMP measured from her left ear was larger than that from the right. In electronystagmography (ENG), nose-pinched Valsalva manoeuvres caused eye movements to be mainly directed counterclockwise with a vertical component. Tullio phenomenon was also positive for both ears. SCDS patients tend to be misdiagnosed and misunderstood; common misdiagnoses in these cases are alternobaric vertigo (AV), inner ear barotrauma, and inner-ear decompression sickness. It is difficult to diagnose vertigo attacks after scuba diving as SCDS; however, when the patient develops sound- and/or pressure-induced vertical-torsional nystagmus, HRCT should be conducted to confirm a diagnosis of SCDS.
Keywords: ENT, Scuba diving, Injuries, Inner ear, Ear barotrauma, Radiological imaging, Valsalva manoeuvre, Case report
Introduction
The dramatic ambient pressure changes that are experienced during scuba diving rarely result in sudden-onset vertigo and/or hearing loss. Rapid and strong changes in pressure within the middle ear are thought to cause alternobaric vertigo (AV) and inner ear barotrauma (IEBt).[1,2] Divers who have chronic Eustachian tube dysfunction are at higher risk of experiencing middle-ear disease.[1,2] Semicircular canal dehiscence (SCD) involving the superior canal (superior canal dehiscence syndrome [SCDS]) was first described in 1998.[3] SCDS is a rare disorder caused by the dehiscence or fracture of the temporal bone overlying the superior semicircular canal. SCDS is characterized by vertigo and vertical-torsional eye movements induced by loud sounds or stimuli that change middle ear or intracranial pressure.
We report here a case of bilateral SCDS, for which the most prominent symptom was vertigo during scuba diving, especially when a Valsalva manoeuvre was executed. To put this case in context we also include a review of the literature.
Case report
A 28-year-old woman presented to our clinic for assessment and treatment because she experienced slight dizziness and difficulty in clearing her left ear during scuba diving. Her pure tone audiometry and tympanometry results were within normal ranges, but Eustachian tube function testing revealed tubal stenosis of her left ear. Testing of fixation, positional, and positioning nystagmus revealed nothing unusual. She was diagnosed with mild alternobaric vertigo (AV) due to tubal stenosis and was treated with anti-allergy agents and nasal steroid spray. After treatment, her symptoms subsided.
Four months later, she experienced continuous dizziness, apparently being triggered not only by pressure changes during diving but also by sneezing and coughing associated with a common cold. She returned to our clinic. Up to this time, she had not experienced any equilibration disturbances during her daily routine. She also reported never having sustained head trauma or having any ear-related disease. Moreover, she reported no severe inner ear injuries, such as inner ear barotrauma (IEBt) or inner ear decompression sickness (inner-ear DCS).
To test for inner-ear hearing loss, we conducted pure tone audiometry and tympanometry, both of which yielded normal results. Eustachian tube function testing at this second visit confirmed the tubal stenosis revealed during her initial clinic visit. Nystagmus testing using an infrared CCD camera revealed a predominantly torsional nystagmus, especially while she was in the lordotic position. Slow phases were directed counterclockwise (Figure 1). Fistula signs were positive, because the patient exhibited very slight horizontal nystagmus beating to the right when positive pressure was applied to the left ear canal using a Politzer bag. These clinical findings led us to suspect a perilymph fistula in the left ear, which prompted us to carry out high-resolution computed tomography (HRCT). HRCT of the temporal bone was negative for perilymph fistula. However, it revealed bilateral dehiscence of the bone overlying the superior semicircular canals, consistent with a bilateral SCDS (Figure 2).
Figure 1.
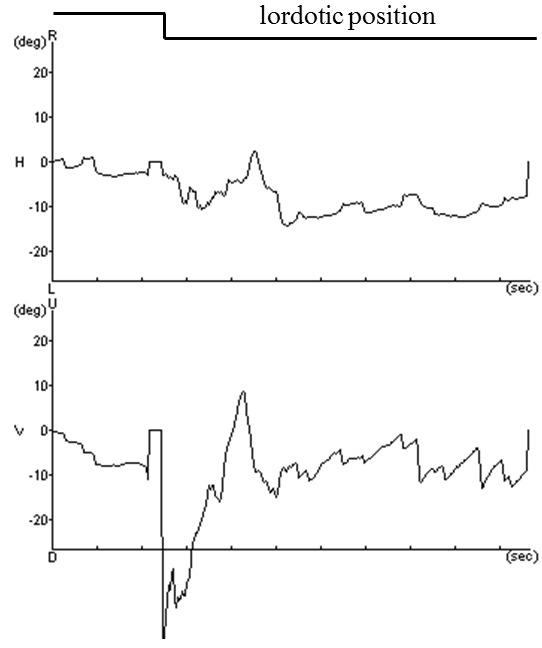
Video-oculographic recording using infrared CCD camera of horizontal and vertical eye movements in a patient with bilateral superior canal dehiscence syndrome revealed a predominantly torsional nystagmus while the patient was in the lordotic position
Figure 2.
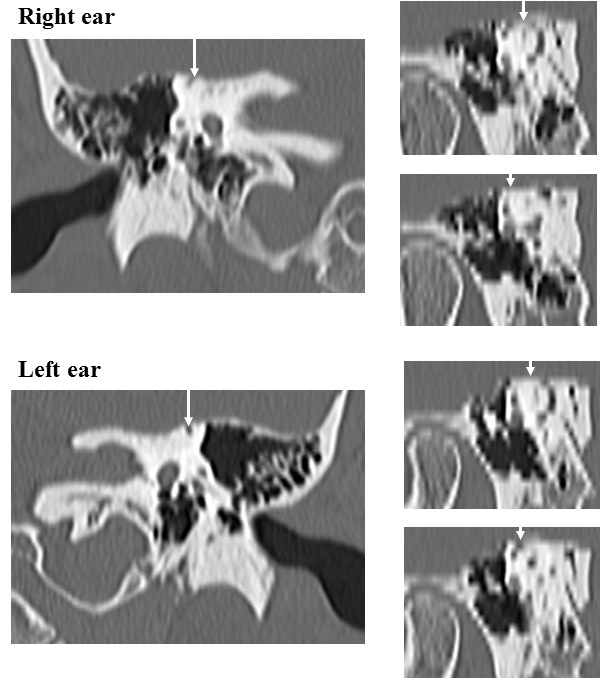
High-resolution CT images of the right and left temporal bones showing dehiscence (arrows) of the bone overlying the superior semicircular canal; coronal view (left panel) and Pöschl views (right panels, poor resolution images) through the right temporal bone
She was admitted to the Tokyo Medical University hospital for further investigations, employing cervical vestibular-evoked myogenic potential (cVEMP) and electronystagmography (ENG) testing. cVEMP revealed a peak-to-peak (p13-n23) amplitude difference between ears, with a larger peak-to-peak amplitude originating from her left ear (Figure 3). In ENG, after nose-pinched Valsalva manoeuvres, the slow phases were directed counterclockwise or clockwise, but they were mainly counterclockwise with a vertical component (Figure 4). Tullio phenomenon was positive for both ears; loud auditory stimulation (100 dB nHL at 1000 Hz) induced nystagmus (Figure 5). Taken together, these results led us to diagnose her with bilateral SCDS, dominated by the left ear.
Figure 3.
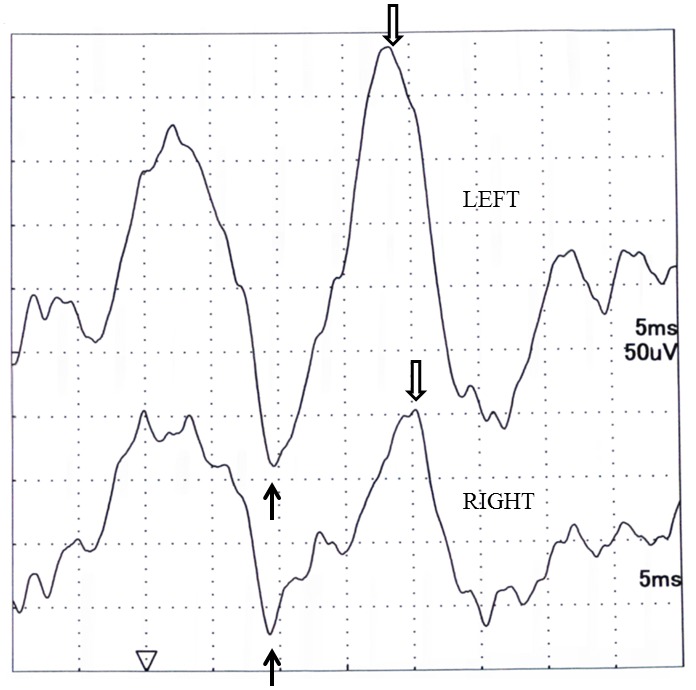
cVEMP testing results; the peak-to-peak (p13-n23) amplitude recorded from the left ear was greater than that from the right ear; the p13 peaks are indicated by black arrows, whereas n23 peaks are indicated by open arrows; the clicks were rarefactive square waves (length: 0.1 ms; intensity: 100 dB nHL)
Figure 4.
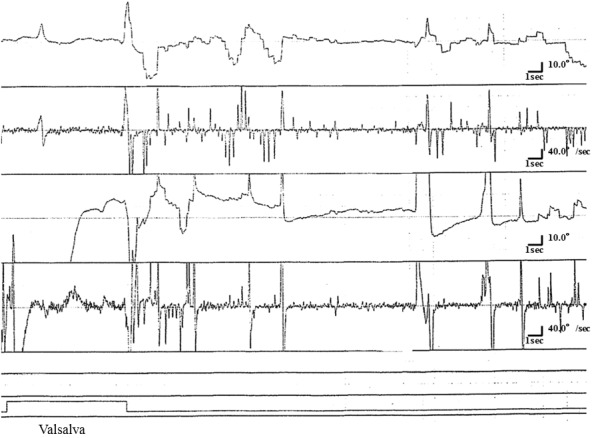
Electronystagmogram following a Valsalva manoeuvre; the manoeuvre induced nystagmus that was mainly directed counterclockwise and had a vertical component
Figure 5.
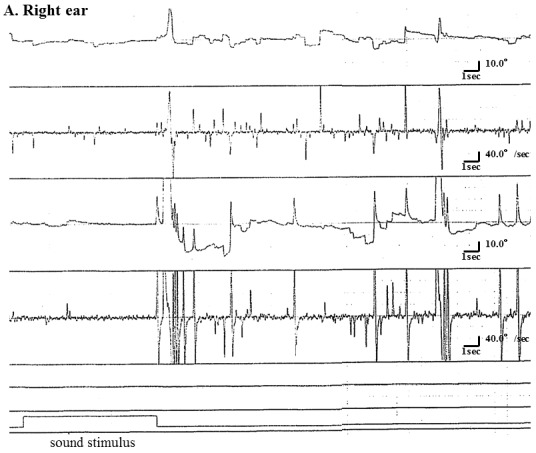
Electronystagmograms of the right (A) and left (B) ears recorded during a Tullio phenomenon; loud sound stimuli (100dB nHL at 1000 Hz) delivered to each ear induced nystagmus
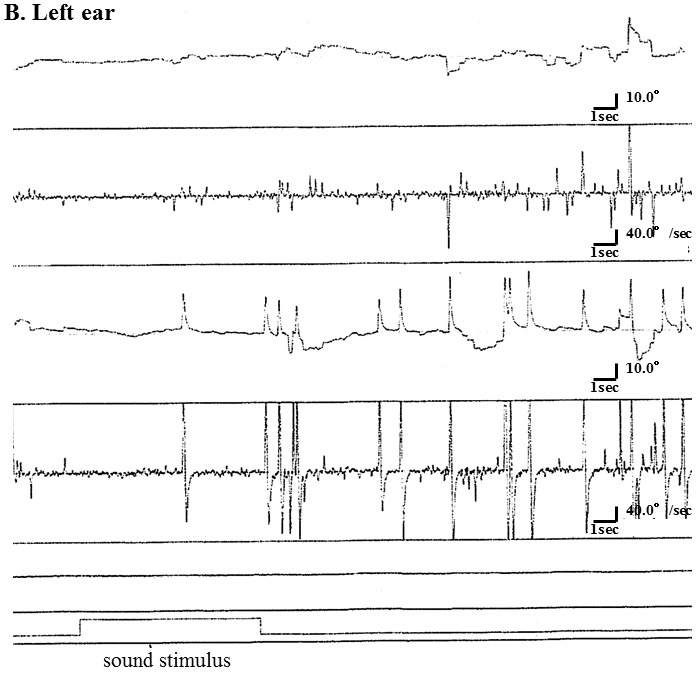
Electronystagmograms of the right (A) and left (B) ears recorded during a Tullio phenomenon; loud sound stimuli (100dB nHL at 1000 Hz) delivered to each ear induced nystagmus
The patient declined medical therapy. However, we advised her to make lifestyle changes, such as avoiding excessive exercise, including diving; ceasing performing Valsalva manoeuvres and reducing excessive straining when blowing her nose. Six months after her second visit, her ear symptoms had improved.
This study was conducted in accordance with the Declaration of Helsinki for the ethical treatment of human subjects. All procedures were carried out with the patient’s written informed consent and her consent to the publication of this case study. The review board of Tokyo Medical University approved all procedures (No. 3032).
Discussion
SCDS is diagnosed radiologically and is associated with the Tullio's phenomenon and Hennebert's sign. Tullio's phenomenon is the feeling of a spinning sensation evoked by sound. Hennebert's sign is nystagmus produced by applied pressure into the external auditory canal. These signs may arise in some cases from the development of a third mobile window within the bony labyrinth, which permits transmission of vibration into the vestibular apparatus, resulting in vertigo or dizziness.[3,4] Positive pressure applied to the external auditory canal and nose-pinched Valsalva manoeuvres cause endolymph motion with ampullofugal (excitatory) deflection of the cupula, which in turn induces a torsional-vertical nystagmus.[5] The nystagmus has slow-phase components directed upward and away from the affected labyrinth.
In the present case, the patient had bilateral SCDS. After performing nose-pinch Valsalva manoeuvres, she exhibited torsional-vertical nystagmus directed mainly away from her left side (Figure 4). In addition, cVEMP recordings revealed that cVEMP amplitude of the left ear was larger than that of the right ear (Figure 3). These findings led us to conclude that the dominantly affected ear was the left ear. Patients with a larger superior canal dehiscence show significantly more vestibulocochlear signs and symptoms and lower cVEMP thresholds compared to patients with a smaller superior canal dehiscence.[6] Thus, the results of diagnostic examinations may be associated with the size of the superior canal dehiscence as in this case.
Generally, in most SCDS patients, audiometry tests reveal low-frequency conductive hearing loss with normal or characteristically negative bone-conduction thresholds.[3,7] SCDS patients also suffer from recurrent vertigo attacks with vertical-rotational oscillopsia induced by pressure changes or loud sounds.[8] However, in our patient, audiometry test results were within normal ranges. Moreover, the patient had never experienced vertical oscillopsia, except when she was scuba diving. These findings indicate that the severity of her SCDS was mild and explains why it was difficult to diagnose her dehiscence. Our initial examination led us to believe that her vertigo attacks were triggered not only by excessive pressure changes during diving but also by Eustachian tube dysfunction, which made it difficult for her to equalize the pressure within the middle ear. The latter caused her to perform excessive Valsalva manoeuvres, which, together with rhinitis, caused her Eustachian tube function to worsen.
In a clinical setting, patients presenting with SCDS tend to be misdiagnosed and misunderstood. Vestibular signs and symptoms induced by pressure changes in the middle ear might lead to a misdiagnosis, such as AV, IEBt (including perilymph fistula) or inner-ear DCS. Table 1 presents a summary of the differential diagnosis of barotraumatic inner-ear disease related to scuba diving, including SCDS and AV. As it is difficult to distinguish SCDS from several other inner-ear diseases caused by scuba diving, we suggest performing HRCT of the temporal bone, because this is the most effective way to diagnose SCDS.
Table 1. Differential diagnosis of barotraumatic inner-ear disease due to diving; entries in the last three columns derived from Kitajima, et al.1 and Farmer and Gillespie;9 DCS − decompression sickness; PLF − perilymphatic fistula; SCDS − superior canal dehiscence syndrome.
| SCDS | Alternobaric vertigo | Inner ear barotrauma | Inner-ear DCS | |
|---|---|---|---|---|
| Frequency | Very rare | Mostly | Second most common | Rare |
| Dive exposure | Any | Any | Any | Near or exceeding decompression limits |
| Onset | Descent, ascent or post-dive | Ascent or post-dive | Descent, ascent or post-dive | At depth, ascent or post-dive |
| Inner ear symptoms | Vestibular +/- cochlear | Vestibular | Cochlear +/- vestibular | About 50% vestibular, 30% cochlear, 20% both |
| Eustachian tube dysfunction | Yes | Yes | Yes | No |
| Tullio phenomenon and Hennebert's sign | Yes | No | Yes (if with PLF) | No |
| Clinical associations | Ear barotrauma | Ear barotrauma | Ear barotrauma | Other DCS symptoms; deep or saturation dive |
| Diagnostic imaging | Semicircular canal dehiscence | No abnormality | Leak of inner ear fluid into middle ear (if with PLF) | No abnormality |
| Type of gas breathed | Mainly air | Mainly air | Mainly air | Mainly helium or hydrogen |
| Treatment | Conservative/surgery | Conservative | Conservative/surgery | Recompression/oxygen |
Conclusions
We encountered a young female patient with bilateral SCDS. She experienced dizziness correlated not only with scuba diving but also with sneezing and coughing. It is difficult to determine whether vertigo attacks that occur during diving arise from SCDS. However, when patients develop sound and/or pressure-induced vertical-torsional nystagmus, clinicians need to consider the possibility of SCDS and then perform HRCT. These conclusions will be strengthened with more similar cases, which could lead to more accurate and consistent diagnoses in the future.
Footnotes
Funding and conflicts of interest: nil
Contributor Information
N Kitajima, Kitajima ENT Clinic, Tokyo, Japan; Department of Otolaryngology, Tokyo Medical University, Tokyo, Japan.
A Sugita-Kitajima, Kitajima ENT Clinic, Tokyo, Japan; Department of Otolaryngology, St. Marianna University School of Medicine, Kanagawa, Japan.
S Kitajima, Kitajima ENT Clinic, Tokyo, Japan.
References
- Kitajima N, Sugita-Kitajima A, Kitajima S. Altered Eustachian tube function in SCUBA divers with alternobaric vertigo . Otol Neurotol. 2014;35:850–856. doi: 10.1097/MAO.0000000000000329. [DOI] [PubMed] [Google Scholar]
- Kitajima N, Sugita-Kitajima A, Kitajima S. Quantitative analysis of inner ear barotrauma using a Eustachian tube function analyzer . Diving Hyperb Med. 2016;46:76–81. [PubMed] [Google Scholar]
- Minor LB, Solomon D, Zinreich JS, Zee DS. Sound- and/or pressure-induced vertigo due to bone dehiscence of the superior semicircular canal . Arch Otolaryngol Head Neck Surg. 1998;124:249–258. doi: 10.1001/archotol.124.3.249. [DOI] [PubMed] [Google Scholar]
- Cawthorne T. Chronic adhesive otitis . J Laryngol Otol. 1956;70:559–564. doi: 10.1017/s0022215100053342. [DOI] [PubMed] [Google Scholar]
- Cremer PD, Minor LB, Carey JP, Della Santina CC. Eye movements in patients with superior canal dehiscence syndrome align with the abnormal canal . Neurology. 2000;55:1833–1841. doi: 10.1212/wnl.55.12.1833. [DOI] [PubMed] [Google Scholar]
- Pfammatter A, Darrouzet V, Gäetner M, Somers T, Dinther JV, Trabalzini F, et al. A superior semicircular canal dehiscence syndrome multicenter study: is there an association between size and symptoms . Otol Neurotol. 2010;31:447–454. doi: 10.1097/MAO.0b013e3181d27740. [DOI] [PubMed] [Google Scholar]
- Minor LB. Superior canal dehiscence syndrome . Am J Otol. 2000;21:9–19. [PubMed] [Google Scholar]
- Deutschländer A, Strupp M, Jahn K, Jäger L, Quiring F, Brandt T. Vertical oscillopsia in bilateral superior canal dehiscence syndrome . Neurology. 2004;62:784–787. doi: 10.1212/01.wnl.0000117978.13194.ed. [DOI] [PubMed] [Google Scholar]
- Farmer JC, Gillespie CA. Otologic medicine and surgery of exposures to aerospace, diving and compressed gases . In: Alberti PW, Ruben RJ, editors. Otologic medicine and surgery. New York: Churchill Livingstone; 1988. pp. 1753–1802. [Google Scholar]