Estimating life years lost to diabetes: outcomes from analysis of National Diabetes Audit and Office of National Statistics data (original) (raw)
Abstract
With sustained growth of diabetes numbers, sustained patient engagement is essential. Using nationally available data, we have shown that the higher mortality associated with a diagnosis of T1DM/T2DM could produces loss of 6.4 million future life years in the current UK population. In the model, the ‘average’ person with T1DM (age 42.8 years) has a life expectancy from now of 32.6 years, compared to 40.2 years in the equivalent age non diabetes mellitus population, corresponding to lost life years (LLYs) of 7.6 years/average person. The ‘average’ person with T2DM (age 65.4 years) has a life expectancy from now of 18.6 years compared to the 20.3 years for the equivalent non diabetes mellitus population, corresponding to LLY of 1.7 years/average person. We estimate that for both T1DM and T2DM, one year with HbA1c >58 mmol/mol loses around 100 life days. Linking glycaemic control to mortality has the potential to focus minds on effective engagement with therapy and lifestyle recommendation adherence.
Keywords: diabetes, HbA1C, mortality, National Diabetes Audit
Introduction
With sustained growth of diabetes numbers predicted for the future, avoiding long-term comorbidities means that effective early diagnosis and treatment of the condition is vital, along with sustained patient engagement [1–3]. With many new treatments available or in development, there are significant opportunities for intervening early to improve the longer term health outcomes for people with diabetes. In this study, we calculated the impact of suboptimal management of diabetes on overall expected lost life years (LLYs) in people with diabetes mellitus in England.
Methods
The Office for National Statistics published for 2015–2017 the actual mortality rates and projected life expectancy in years of the general population for each age year and sex [4]. The National Diabetes Audit (NDA) [5] published for 2015–2016 the mortality rates for people with Type 1 diabetes mellitus (T1DM) and Type 2 diabetes mellitus (T2DM) in five different age groups and each sex as a ratio to general population. The NDA [6] also published the number of people with T1DM and T2DM in quinary age groups by sex. The model applied relative NDA mortality rates to population rates for each age and sex, and calculated the future life expectancy for T1DM, T2DM and non diabetes mellitus populations. The difference between the total life expectancy for the reported populations by age and gender of T1DM and T2DM to an equivalent population with non diabetes mellitus gave LLYs.
LLYs are one result of suboptimal condition management, which can be viewed as poor glycaemic control measured by HbA1c. The total lost life days were allocated to the total number with higher HbA1c results and expected non diabetes mellitus life expectancy to show life days lost/life year with high HbA1c.
Results
The NDA [5] reports 57 814 deaths observed in 2015 out of the 161 871 T1DM and 1 620 784 T2DM, which is 32.1% higher than an equivalent non diabetes mellitus population. The 2015–2016 NDA [6] provides data from 6165 general practices supporting 41.34 million patients of which 217 438 were on the T1DM register and 2.50 million on the T2DM register.
In the model, the ‘average’ person with T1DM (age 42.8 years) has a life expectancy from now of 32.6 years (total population 7.1 million life years), compared to 40.2 years in the equivalent age non diabetes mellitus population, corresponding to LLY of 7.6 years/average person (1.67 million total LLY for T1DM) (Table 1). The ‘average’ person with T2DM (age 65.4 years) has a life expectancy from now of 18.6 years (total population 46 million life years) compared to the 20.3 years for the equivalent non diabetes mellitus population, corresponding to LLY of 1.7 years/average person (4.20 million total LLY for T2DM) (Table 1).
Table 1.
Total and individual life years lost in type 1 diabetes mellitus and type 2 diabetes mellitus
| Non diabetes mellitus | T1DM | T2DM | |||||
|---|---|---|---|---|---|---|---|
| Male | Female | Male | Female | Male | Female | Total | |
| Population number | 19 049 | 19 518 | 123 | 95 | 1391 | 1110 | 41 285 |
| Total normal expected life years | 846 155 | 897 512 | 4757 | 3994 | 27 480 | 23 227 | 1 803 125 |
| Projected diabetes mellitus expected life years | 3892 | 3190 | 25 533 | 20 973 | |||
| Lost life year | 864 | 804 | 1,947 | 2,253 | |||
| Average age | 37.1 | 38.9 | 43.0 | 42.7 | 64.7 | 66.3 | 39.0 |
| Normal life expectancy | 44.4 | 46.0 | 38.7 | 42.2 | 19.8 | 20.9 | 43.7 |
| Projected life expectancy | 44.4 | 46.0 | 31.7 | 33.7 | 18.4 | 18.9 | |
| Average lost life years | 7.0 | 8.5 | 1.4 | 2.0 |
Difference between sexes is also shown (Fig. 1) with the average LLY/person for women being 21% higher for T1DM and 45% higher for T2DM women versus men.
Fig. 1.
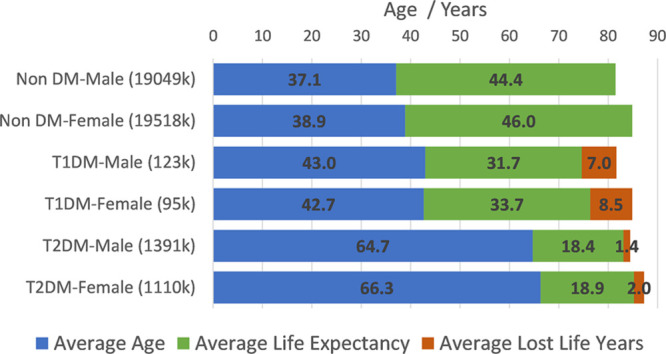
National average age, life expectancy in years for the non diabetes mellitus, T1DM and T2DM populations split by sex. The orange section reflects the LLYs corresponding to the life expectancy gap between the non diabetes mellitus population and T1DM/T2DM individuals. The longer blue bars for T2DM relate to the later age of onset than T1DM. T1DM, type 1 diabetes mellitus; T2DM, type 2 diabetes mellitus.
The NDA [6] reports that 70% of people with T1DM and 33% people with T2DM on their last check had Hba1c >58 mmol/mol which puts them at higher risk. So, for both T1DM and T2DM, one year with HbA1c >58 mmol/mol loses around 100 life days. Knowledge of this may act as an incentive for clinicians to ensure that all people are on the best therapy and for those people to engage more strongly with their therapy/lifestyle recommendations. The annual impact of suboptimal control is found to be the same for both T1DM and T2DM; the difference in T1DM comes from the higher proportion of T1DM individuals with suboptimal control and their longer duration with the condition due to onset at a younger age.
Discussion
Using nationally available data, we show that higher mortality risks associated with the diagnosis of T1DM and T2DM and their historic treatments project a future loss of over six million LLY in the current diabetes population. The consequences in terms of LLY for women with diabetes are greater than for men according to our model. We acknowledge that our article has used national-level mortality data, that is, not general practitioner practice-level data. Also, it is likely that other factors contribute such as smoking, inactivity, overweight, hypertension and taking of statins. This will be the subject of a full analysis with general practice-level data. However, it is likely that the HbA1c level will remain a strong independent determinant of mortality.
Linking poor glycaemic control to expected mortality in such a quantitative way may incentivize clinicians and people with diabetes and poor control to increase their efforts to achieve targets. Communication of life years lost from now to patients at the time of consultation with healthcare professionals and through messages publicized by Diabetes UK and other national/international patient facing organizations will be of great help in terms of disssemination of the conclusions in this article.
More work is required to understand why women are losing more life years than men.
Acknowledgements
A.H. and M.S. conceived the idea for the analysis and led on the composition of the article. M.L. (Reader in Statistics, Manchester University) supervised the data analysis. G.R. and R.G. provided editorial input. All authors contributed equally to the writing of the article.
All data used for the analysis are publicly available in the UK through NHS Digital and the Office of National Statistics.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Fisher L, Polonsky WH, Hessler D, Potter MB. A practical framework for encouraging and supporting positive behaviour change in diabetes. Diabet Med. 2017; 34:1658–1666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.The DCCT/EDIC Research Group. Epidemiology of Diabetes Interventions and Complications (EDIC). Design, implementation, and preliminary results of a long-term follow-up of the diabetes control and complications trial cohort. Diabetes Care. 1999; 22:99–111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Alva ML, Gray A, Mihaylova B, Leal J, Holman RR. The impact of diabetes-related complications on healthcare costs: new results from the UKPDS (UKPDS 84). Diabet Med. 2015; 32:459–466 [DOI] [PubMed] [Google Scholar]
- 4.ONS National life tables: UK 2015-17. https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/qmis/mortalitystatistic. [Acessed 26 July 2019]
- 5.National diabetes audit complications and mortality 2015-2016. https://digital.nhs.uk/data-and-information/publications/statistical/national-diabetes-audit/national-diabetes-audit-complications-and-mortality-2015-2016. [Accessed 25 July 2019]
- 6.National diabetes audit – 2015-2016: report 1, care processes and treatment targets. https://digital.nhs.uk/data-and-information/publications/statistical/national-diabetes-audit/national-diabetes-audit-2015-2016-report-1-care-processes-and-treatment-targets. [Accessed 26 July 2019].