Creating and Maintaining the Gastrointestinal Ecosystem: What We Know and Need To Know from Gnotobiology (original) (raw)
Abstract
Studying the cross talk between nonpathogenic organisms and their mammalian hosts represents an experimental challenge because these interactions are typically subtle and the microbial societies that associate with mammalian hosts are very complex and dynamic. A large, functionally stable, climax community of microbes is maintained in the murine and human gastrointestinal tracts. This open ecosystem exhibits not only regional differences in the composition of its microbiota but also regional differences in the differentiation programs of its epithelial cells and in the spatial distribution of its component immune cells. A key experimental strategy for determining whether “nonpathogenic” microorganisms actively create their own regional habitats in this ecosystem is to define cellular function in germ-free animals and then evaluate the effects of adding single or several microbial species. This review focuses on how gnotobiotics—the study of germ-free animals—has been and needs to be used to examine how the gastrointestinal ecosystem is created and maintained. Areas discussed include the generation of simplified ecosystems by using genetically manipulatable microbes and hosts to determine whether components of the microbiota actively regulate epithelial differentiation to create niches for themselves and for other organisms; the ways in which gnotobiology can help reveal collaborative interactions among the microbiota, epithelium, and mucosal immune system; and the ways in which gnotobiology is and will be useful for identifying host and microbial factors that define the continuum between nonpathogenic and pathogenic. A series of tests of microbial contributions to several pathologic states, using germ-free and ex-germ-free mice, are proposed.
All mammals, including humans, are adapted to life in a microbial world. Pasteur, Koch, Metchnikoff, and Escherich laid the conceptual groundwork for our present views of host-microbe interactions (51). Pasteur postulated that microbes are necessary for normal human life (176). Metchnikoff claimed that the composition of the flora is essential for the well-being of the host and stressed the importance of interactions between host and bacteria (129, 130). Escherich was convinced that accurate knowledge of the endogenous flora was essential not only for understanding the physiology of digestion but also for understanding the pathology and therapy of microbial intestinal diseases (53). Despite these early insights, scientists have only recently developed methods that allow them to directly characterize the molecular mechanisms underlying the establishment and maintenance of various microbial ecosystems located on our mucosal surfaces.
Understanding the cross talk that occurs between microorganisms and their eukaryotic hosts under nonpathogenic conditions promises to expand our views of how bacteria affect and effect cellular differentiation and function (43, 60). It should also help us understand the shifting boundary between “nonpathogenic” and “pathogenic” relationships. Characterizing the cross talk represents an experimental challenge because of its subtlety, in contrast to the often dramatic manifestations of interactions between classical pathogens and their hosts (60, 61). A key experimental strategy for defining the conversations that occur between microorganisms and their hosts is to first define cellular function in the absence of bacteria (i.e., under germ-free conditions) and then to evaluate the effects of adding a single or defined population of microbes.
Rearing mammals under germ-free conditions has developed into a scientific field of its own, termed gnotobiology from the Greek “γνωςις” (gnosis), meaning knowledge, and “βιος” (bios), meaning life (73, 74). The power of germ-free technology lies in the ability to control the composition of the environment in which a multicellular organism develops and functions. The combined use of genetically manipulatable model organisms and gnotobiotics has the potential to provide new and important information about how bacteria affect normal development, establishment and maintenance of the mucosa-associated immune system, and epithelial-cell functions. Furthermore, gnotobiology can help provide new insights about the etiologies of infectious diseases, acute and chronic inflammatory conditions (59, 170), and possibly tumorigenesis (70). This review highlights some of the contributions of gnotobiology to our present conceptualization of the dynamic, complex, and spatially diversified ecosystem which is established and maintained in the mammalian gut.
OVERVIEW OF THE GUT MICROBIOTA
The number of microbes associated with the mucosal surfaces of adult humans is estimated to exceed the number of host somatic and germ cells by at least 1 order of magnitude (171). The gastrointestinal tract contains the largest number and most complex population of these organisms. There are at least 400 different species of bacteria in the fully assembled (climax) microbial community of the gut (15, 171). Anaerobes outnumber aerobes and facultative species by a factor of 100 to 1,000 (142). Differences are found in the composition of this microbial society among different mammalian species—for example, between ruminants and nonruminants and between omnivores and carnivores (186).
How is this society assembled? Mammals are born without any microorganisms. Colonization of exposed body surfaces, including the skin, respiratory tract, genitourinary system, and gut, starts immediately at birth. Initially, when space and nutrients are not limiting, bacteria with high multiplication rates dominate. As the bacterial numbers increase and nutrient pools are depleted, habitats become populated with more specialized species and the complexity of the flora increases. The first bacteria that colonize the human gut are derived from the aerobic and anaerobic flora of the birth canal. In neonates, Escherichia coli, Clostridium spp., Streptococcus spp., Lactobacillus spp., Bacteroides spp., and Bifidobacterium spp. predominate (163). Bifidobacteria form the largest segment of the fecal flora as long as infants are breast fed (29). Distinct differences in the composition of the fecal flora are found between children from different geographic regions (1), reflecting, in part, the impact of the environment (sanitary conditions). The mode of delivery (146), feeding patterns (10, 151, 187), hospitalization (119), and antibiotic treatment (12) are other factors known to affect the composition of the gut flora in children.
Comparisons of inbred strains of rats raised under conventional conditions (i.e., with an intact microbiota), under germ-free conditions, and initially under germ-free conditions but later colonized with selected components of the microbiota (ex-germ-free conditions) have demonstrated that bacteria carry out a number of biochemical functions (133, 137). These include the deconjugation and dehydroxylation of bile acids by E. coli, Bacillus cereus, Streptococcus faecalis, Bacteroides spp., Eubacterium spp., and Clostridium spp. (132), the conversion of bilirubin to urobilinogen by Clostridium ramosum (138), and the metabolism of cholesterol to coprostanol by strains belonging to the genus Eubacterium (165). Menaquinones, i.e., vitamin K, are produced by a wide variety of intestinal bacteria, including Bacteroides, Eubacterium, Propionibacterium, Fusobacterium, Bifidobacterium, Lactobacillus, Clostridium, Enterobacterium, Veillonella, Enterococcus, Enterobacteria, and Streptococcus (75; reviewed in reference 87). Generation of short-chain fatty acids is also a common feature of the climax community, although the specific species responsible remain undefined (95).
These metabolic activities can be used as a crude signature of a functional microbiota (136). Compositional changes can be monitored as humans develop by noting changes in metabolic activities assignable to the flora. Analyses of such activities indicate that assembly of the microflora progresses over several years (131).
The climax community of microbes is never static. For example, microbiological enumeration studies and DNA fingerprinting have disclosed marked differences in the size, number, and types of Lactobacillus and Bifidobacterium subpopulations between and within adult individuals (128). A habitat in the gastrointestinal tract will, at any given time, be populated by native (resident or autochthonous) species and a variable set of transient (allochthonous) species that only temporarily fill an empty niche (171). Allochthonous bacteria can represent strains whose resident habitat is located in a more proximal region of the gut or organisms that have been ingested. The composition of the “normal” microflora in a given region of the gut is difficult to define even within a given individual, not only because of the problem of distinguishing resident from transient species but also because of the difficulty in culturing most components ex vivo. The term “microbiota” has been used to describe the collective societies of bacteria assembled on the mucosal surfaces of an individual (171). It should be possible to provide a more comprehensive description of the composition of an individual’s gastrointestinal microbiota, including societal members that cannot be cultured ex vivo, by using nucleotide sequencing strategies that target ribosomal DNAs (152a).
It is remarkable that the intestinal ecosystem is able to establish and maintain a microbiota that has functional stability (as opposed to absolute numerical or compositional stability). Several factors constantly challenge the stability of the microbial community. The intestinal epithelium and the overlying mucus layer turn over rapidly and continuously throughout life (see below). The ecosystem is open. Peristaltic activity ensures perpetual exposure of a given segment of the gut to a wide variety of allochthonous bacteria, dietary macromolecules, and gastric, pancreatic, and biliary secretions.
The factors that allow components of the microbiota to establish and maintain their regional habitats are largely unknown. Each of the intestine’s four self-renewing epithelial cell lineages maintains regional differences in its differentiation program (50, 55, 162). Components of the gut-associated immune system also have distinct distributions along both the duodenal-colonic and crypt-villus axes (64, 199). Integration of the ecosystem into the host is probably achieved in part through these preexisting regional variations in the epithelium and mucosal immune system and in part through “conversations” that allow members of the microbiota to modify the host and thus create favorable niches for themselves.
As discussed below, these conversations can be viewed as comprising a “trialogue” involving bacteria, the epithelium, and components of the gut-associated immune system. Before examining the evidence that members of the microbiota modulate differentiation of the gut mucosa, it is important to summarize the pathways for epithelial cell renewal in the adult mouse and human intestine.
EPITHELIAL CELL RENEWAL IN THE MOUSE AND HUMAN INTESTINE
Figure 1 summarizes the pathways of epithelial cell renewal in adult mice and humans. In the more thoroughly studied mouse model, the turnover time for the entire epithelial cell population averages 60 h (36, 37). Proliferation occurs in flask-shaped mucosal invaginations known as the crypts of Lieberkühn. A small intestinal crypt in the adult mouse contains an average steady-state population of 250 epithelial cells. All epithelial cells in each crypt are derived from an uncertain number of multipotent stem cells located at or near the base of the crypt (20, 21, 34, 35, 39–41, 122, 206, 207). The descendants of the stem cells are amplified through an estimated four to six rounds of cell division, forming a rapidly cycling population of transit cells located in the midportion of each crypt (159). On average, a crypt produces about 12 cells per h or 300 new cells per day. Crypts supply cells to tongue-shaped villi (Fig. 1). Several crypts surround the base of each villus; the number varies along the proximal-distal axis of the small intestine and with age (38, 212). Three of the four principal epithelial cell lineages arising from the multipotent stem cell differentiate during an upward migration from the crypt to an associated villus. These include columnar absorptive enterocytes (comprising >80% of all epithelial cells), mucus-producing goblet cells, and enteroendocrine cells. Migration from the crypt to the villus tip is completed in 2 to 5 days. The velocity of cell movement is remarkable: 0.75 to 1 cell diameter per h near the crypt-villus junction (159). The cellular migration is also remarkably well organized: studies of chimeric mice have shown that cells from each crypt migrate up an adjacent villus in coherent columns (86, 174) (Fig. 1A and B). Once the cells arrive at the villus tip, they are removed by exfoliation or apoptosis.
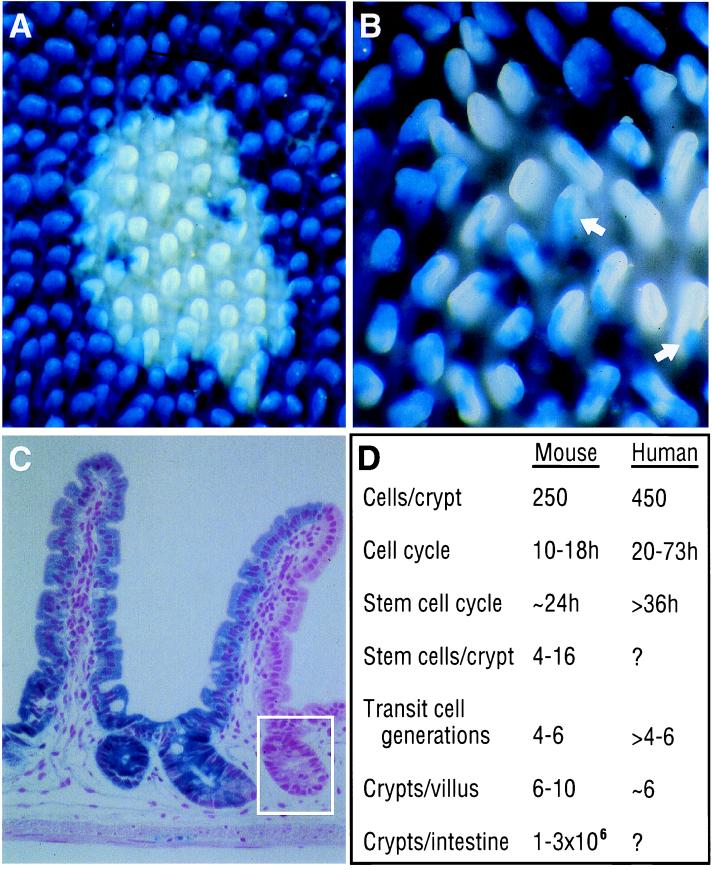
FIG. 1.
Epithelial renewal in the small intestine. (A) Whole-mount preparation of the small intestine from an adult chimeric mouse raised with a conventional microbiota. The mouse was produced by using materials from two inbred strains: embryonic stem cells from one strain (129/Sv) were introduced in blastocysts from another strain (C57BL/6; abbreviated B6). The small intestine of the resulting adult chimera is composed of patches of 129/Sv crypt-villus units and patches of B6 crypt-villus units. All B6 epithelial cells in this mouse contained a locus known as ROSA 26, which directs the production of an E. coli β-galactosidase marker (63, 210). This marker allows B6 cells to be identified with a simple histochemical stain (5-bromo-4-chloro-3-indolyl-β-d-galactopyranoside [X-Gal]). Positively stained B6 cells appear blue. None of the 129/Sv epithelial cells contain the ROSA26 locus, and their lack of β-galactosidase makes them appear white. The whole-mount is seen from above. Villi appear as tongue-like projections. The base of each villus is surrounded by crypts, which cannot be seen. Each crypt is monoclonal: it contains epithelial cells that are either all B6 or all 129/Sv but not a mixture of both. (B) Villi located near the border of patches of monoclonal B6-ROSA26 crypts and patches of monoclonal 129/Sv crypts appear striped (arrows). These villi are composed of vertical coherent columns of wholly 129/Sv (white) epithelial cells emanating from monoclonal 129/Sv crypts and adjacent columns of B6 (blue) epithelial cells emanating from monoclonal B6 crypts. The borders of these cellular columns are very distinct, illustrating the highly organized migration of epithelial cells from the base to the tip of the villus. (C) Section from the whole-mount preparation. The section has been stained with X-Gal plus nuclear fast red. The villus on the right is supplied by a B6-ROSA26 crypt that contains an entirely β-galactosidase-positive population of blue cells and by a 129/Sv crypt that contains only β-galactosidase-negative cells. One of the crypts is boxed. (D) Estimates of small-intestine epithelial cell dynamics in the crypt-villus units of mice and humans. Data from reference 157.
Paneth cells represent the fourth lineage arising from the multipotent stem cell. Members of this lineage differentiate during a downward migration to the base of the crypt, where they reside for about 20 days before being phagocytosed by neighboring cells (20, 35). A variety of functions have been attributed to Paneth cells, including modulation of the microbial flora through secretion of lysozyme and a family of antimicrobial peptides known as cryptdins (152).
A given crypt-villus unit maintains an approximate steady-state cellular census over the period required to renew its epithelium. However, when viewed over a timescale of weeks or months, it appears that this static view is unwarranted and that there is continued production of new crypts and new villi (194). The size of the mouse intestine increases with age and weight (150). The number of crypts surrounding each villus increases as the animals age (38). A crypt is a dynamic structure: it divides through bifurcation (doubling time, ∼110 days [19, 120]), apparently after its cellular population expands to a critical size (194). Some studies have estimated that as many as 3 to 10% of crypts are in the process of dividing (19, 38, 194).
The magnitude of cell renewal is impressive. One cell division occurs, on average, every 5 min in each of the approximately 106 crypts in the adult mouse small intestine (79). Each villus discharges an average of 1,400 cells per day. A total of 109 new cells (∼1 g) are produced every 5 days in the small intestine (reviewed in reference 157). Extrapolating, this means that a 25-g mouse will renew a mass of intestinal epithelial cells equal to its body weight every 4 months.
In humans, the cell number is greater in small intestinal crypts (estimated average, 450 cells), the cell division time is thought to be twice as long as in mice, and the number of amplifying transit cell generations is believed to be greater (157, 158, 211) (Fig. 1D). Croft and Cotton (47) have calculated that an adult human produces 50 × 106 intestinal epithelial cells per min. This is equivalent to ∼250 g of cells per day.
Figure 2 summarizes the differences between the epithelial cell dynamics of human versus mouse colonic crypts. The upward migration of cells from colonic crypts ends with their incorporation into a homolog of the villus—a hexagonal cuff of cells that rings the orifice of each crypt (175, 210). There are no Paneth cells in the normal colon (26).
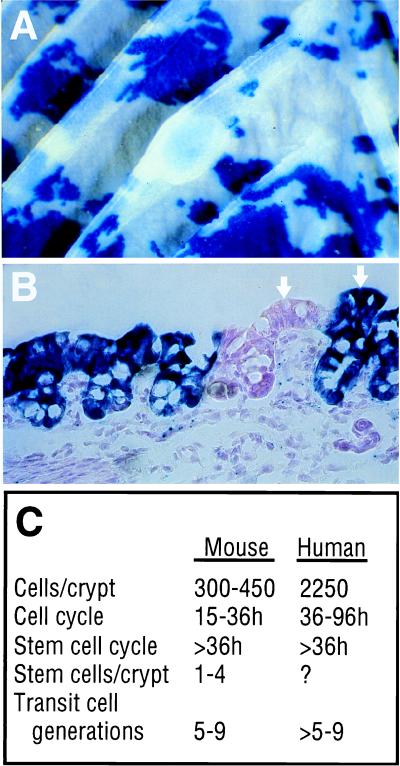
FIG. 2.
Epithelial cell renewal in the colon. (A) Whole-mount preparation of colon from the B6-_ROSA26_–129/Sv chimeric mouse in Fig. 1. The colon does not have villi. Cells emerge from colonic crypts and are incorporated into surface epithelial cuffs that surround the orifice of each crypt. These cuffs represent homologs of small-intestine villi. (B) Section from the colon that has been stained with X-Gal and nuclear fast red. Like small-intestine crypts, colonic crypts are monoclonal. Surface epithelial cuffs associated with adjacent 129/Sv and B6-ROSA26 crypts are indicated by arrows. (C) Estimated values for colonic crypt cell populations. Data from reference 157. These estimates are less accurate than the corresponding estimates for small-intestine crypts.
To appreciate host-microbe interactions in this ecosystem, it is important to consider the time course of intestinal morphogenesis. Development of the mouse intestine proceeds through the third postnatal week (31). The gut endoderm undergoes rapid remodeling from embryonic days 15 to 19, as a wave of cytodifferentiation moves proximally to distally, converting the pseudostratified epithelium to a monolayer of columnar epithelial cells. Villi first arise coincident with this cytodifferentiation. In late fetal life, villi are separated by a proliferating intervillus epithelium (175). Crypts form as this intervillus epithelium undergoes reshaping during the first two postnatal weeks. The crypts then multiply rapidly by division during the third postnatal week (153). The apical extrusion zones of villi become active at birth (31). Villi lengthen during the first 3 to 4 weeks as cell production exceeds cell loss (3, 31).
In humans, villi appear between 9 and 10 weeks of gestation. By 12 weeks, crypts have formed. At 17 weeks of gestation, all intestinal epithelial cell lineages are apparent (195).
IMPACT OF THE MICROFLORA ON THE INTESTINE
General Architectural Effects
Bacteria have a direct impact on the morphology of the gut. The responsibility for degradation of mucus glycoproteins produced by the epithelium is assigned to components of the intestinal microbiota (121), such as Peptostreptococcus micros and members of the genera Ruminococcus and Bifidobacterium, that produce a variety of glycoside hydrolases (32, 89). Germ-free animals exhibit a dramatic enlargement of their cecum—the segment of intestine interposed between the distal small bowel and proximal colon. This enlargement is due in large part to accumulation of undegraded mucus (77) and can be rapidly reversed by monoassociation with Peptostreptococcus micros (32).
Other regions of the intestine also show morphologic changes as a result of microbial colonization. The villi of the small intestine are longer in germ-free than in age-matched conventional animals. Limited morphologic studies (in rats) suggest that crypts are shorter and contain fewer cells in the germ-free state (2). Differences between germ-free and conventional animals are greatest in regions of the gut where bacterial densities are normally highest. The evolution of these differences during postnatal development and their persistence as animals age have yet to be defined by using precise morphometric methods (68). Moreover, to show definitively that bacteria are directly involved in creating these differences, components of the intestinal microbiota must be introduced into developing and adult germ-free rodents and their effects on epithelial cell dynamics determined.
Effects on Intestinal Motility
The spatial and temporal spread of migrating motor complexes in the small intestines of germ-free rats is more restricted and slower than in conventional animals. This appears to be dependent in part upon differences in the responsiveness of the germ-free and conventional intestine to enteroendocrine cell products (188). These differences can be eliminated by colonizing germ-free rats with the cecal contents of a conventionally raised animal (97).
The components of the microbiota that affect motility could be defined by using ex-germ-free animals. The results may have an important effect on our understanding of the pathogenesis of irritable bowel syndrome, especially since transient manipulations of the microbiota that lead to enteritis have been shown to lead to persistent neuromuscular dysfunction in mice (11).
The reciprocal question—whether the enteric nervous system affects the microbiota—can be examined by using mice with genetic manipulations that affect the structure and/or function of their enteric nervous systems (101, 161). For example, a recent report noted that glial cells could be ablated from the jejunum and ileum of ganciclovir-treated mice containing a transgene composed of the mouse glial fibrillary acid protein promoter linked to the herpes simplex virus thymidine kinase gene. Ganciclovir-induced ablation of glial cells was accompanied by degeneration of enteric neurons, bacterial overgrowth, and a patchy jejuno-ileitis containing foci of hemorrhagic necrosis (30). Antibiotic therapy prevented bacterial overgrowth but did not reduce the severity of the induced intestinal pathologic changes. However, as the authors point out, this selective bacterial decontamination does not rule out a role for components of the microbiota in disease pathogenesis (30).
Effects on Epithelial Differentiation
Studies of germ-free mice have shown that morphogenesis of crypt-villus units can be completed in the absence of microbes. However, comparisons of germ-free and conventionally raised animals have revealed that components of the microflora modify the differentiation programs of intestinal epithelial lineages at key points during morphogenesis.
One example of such a modification is provided by the Paneth cell lineage. This lineage emerges as crypts form (26, 49). In conventionally raised mice, cryptdin-positive Paneth cells first appear on embryonic day 15 (E15). By postnatal day seven (P7), these cells have acquired distinctive apical secretory granules. By P10, lysozyme is detectable. During the suckling-weaning transition (P21 to P28), a number of glycoconjugates containing fucose and sialic acid residues appear. In the absence of microbes, the appearance of lysozyme is delayed from P10 to P14. In addition, the expression of some fucosylated glycoconjugates is precociously induced and not suppressed subsequently during adulthood. Exposure of adult germ-free animals to a conventional flora suppresses the production of these fucosylated glycoconjugates within 2 days, restoring one aspect of the normal Paneth cell phenotype exhibited in conventionally raised adult animals (26). Given the 20-day life span of Paneth cells, this latter response represents an example of how components of the microflora can alter the state of differentiation of an existing population of mature cells.
Intestinal epithelial cell glycoconjugates represent sensitive markers of intestinal epithelial cell differentiation (27, 55). They also serve as nutrients and receptors for bacteria (98, 103, 168, 169). The ability of components of the microbiota to affect epithelial cell differentiation is illustrated by their capacity to modify host glycoconjugate production.
Transient production of a glycolipid, fucosyl-asialo-GM1, occurs in the enterocytes of adult germ-free BALB/c mice when they are exposed to an intact conventional microbiota or a component known as the segmented filamentous bacteria (199). The appearance of the fucosyl-asialo-GM1 coincides with the appearance of a fucosyltransferase that adds fucose to the acceptor molecule asialo-GM1 (197).
The NMRI strain of mice provides another example of a microbe-dependent induction of a fucosyltransferase and fucosylated glycoconjugates in enterocytes (28). During the first 3 weeks of postnatal life, both conventional and germ-free NMRI animals begin to produce Fucα1,2Galβ-containing glycoconjugates in enterocytes that populate a minor subset of villi located in the distal small intestine. These Fucα1,2Galβ epitopes can be detected with a lectin (Ulex europeaus type 1 agglutinin). In the absence of a microbiota, epitope expression is extinguished by P28 and remains suppressed throughout adult life. In the presence of a microbiota, epitope expression generalizes between P21 and P28 to involve all enterocytes located in the distal small intestine (ileum). This induction involves replacement of Fucα1,2Galβ-negative enterocytes with Fucα1,2Galβ-positive cells. Once replacement has occurred, production of the Fucα1,2Galβ epitopes is sustained for at least the first year of life. When the ileal and cecal microfloras from conventionally raised NMRI mice are inoculated into adult germ-free NMRI mice, ileal Fucα1,2Galβ-glycoconjugates are produced within 7 days. Induction is associated with the transcriptional activation of a host α1,2-fucosyltransferase gene. Production of these fucosylated glycoconjugates is maintained subsequently in the conventionalized animals.
These results suggest that the initial production of fucosylated glycoconjugates in the developing distal small intestine of germ-free NMRI mice is a marker of host preparation for life in a microbial world. Continued expression of these glycoconjugates is specified by members of the microflora through a sustainable reprogramming of enterocyte differentiation. This programming capability is not a general property of intestinal bacteria. Neither Peptostreptococcus micros nor _Bifidobacterium infantis_—an organism that secretes α-fucosidases (54, 89)—is able to specify production of fucosylated glycoconjugates in the epithelium of ex-germ-free adult NMRI mice. Bacteroides thetaiotaomicron is a member of the normal intestinal microflora of mice and humans. It can metabolize a variety of saccharides, including fucose, derived from host and dietary sources (169). When introduced into adult germ-free NMRI animals, this bacterium is able to reproduce the cellular, spatial, and temporal patterns of Fucα1,2Galβ production orchestrated by an intact microbiota (28). The induction is density dependent and does not appear to require direct binding of bacteria to the host epithelium.
B. thetaiotaomicron must be able to metabolize fucose in order for it to signal the epithelium to synthesize these fucosylated glycoconjugates. A transposon-mediated disruption of a gene required for fucose utilization blocks the ability of the organism to signal, although it does not hamper ileal colonization. However, monocontamination of a germ-free animal does not represent a sensitive or necessarily accurate index of colonization potential, since there are no competing bacteria. Bifidobacterium infantis itself is a poor colonizer of the ileum of germ-free NMRI mice. Interestingly, colonization with Bifidobacterium infantis is enhanced when it is introduced together with B. thetaiotaomicron (26a). The ability of one bacterial species to modify host epithelial differentiation in a way that supports its own growth and permits colonization by a second microbe illustrates how a microbial society may be formed (see below). In this case, the role of B. thetaiotaomicron may be to ensure the production of host fucosylated glycoconjugates that can be efficiently utilized by the α-fucosidase-producing Bifidobacterium infantis.
This genetically manipulatable, simplified ecosystem is well suited for studies of the molecular details of intestinal colonization. The response of the epithelium to colonization can be defined at one or more time points in postnatal life by using DNA microarray technology. Within the next year, the feasibility of applying this approach should improve dramatically as the number of publicly available, sequence-validated cDNA clones increases, image-processing methods improve, software for identifying temporal patterns of gene expression is developed, and ways of publicly presenting the data in user-friendly formats are devised. Although the B. thetaiotaomicron genome has not been sequenced, a global screen for bacterial genes that are induced during colonization should be possible by using the promoter trap strategy described by Valdivia and Falkow (200).
Assembly of the Diffuse Gut-Associated Lymphoid Tissue Is Modulated by the Microbiota
In humans, there are more lymphoid cells associated with the gastrointestinal mucosa than with the spleen, peripheral lymph nodes, and blood taken together (25). Gut-associated B cells account for more than 80% of all B cells in the body (25). The human gut contains 20 immunoglobulin A (IgA)-producing cells for every IgG- or IgM-producing B cell in its lamina propria. The total daily output of dimeric IgA is 0.8 g per m of intestine, an amount equivalent to the output of a lactating mammary gland (25, 67).
The gut-associated lymphoid tissue (GALT) should be considered from the perspective of both its composition and spatial complexity. Newer, more sensitive immunohistochemical methods (181) have helped define the spatial organization of the diffuse GALT (i.e., the components of the mucosal immune system that are distributed throughout the lamina propria, as opposed to the components that are organized into submucosal lymphoid aggregates, such as Peyer’s patches). For example, in conventionally raised adult mice, CD4+ T cells are distributed throughout the length of crypt-villus units and are largely confined to the lamina propria. In contrast, CD8+ T cells are largely intraepithelial and are restricted to the villus. αβ T-cell receptor (TCR)-positive cells populate the intraepithelial and lamina propria compartments of crypts and villi, unlike γδ TCR-positive cells, which are largely limited to the villus epithelium (64).
Studies of germ-free and ex-germ-free mice have shown that bacterial colonization affects the composition of the diffuse GALT. The number of αβ TCR-bearing intraepithelial lymphocytes (IELs) is increased following conventionalization of germ-free animals with an intact microbiota (99, 198). A similar expansion of αβ TCR IELs occurs when adult germ-free Agus rats are conventionalized (84). Although IELs were increased in number, flow cytometry indicated that the cephalocaudal distribution of IEL subpopulations was not affected by microbial colonization (85).
The effects of the microbiota on the spatial organization of components of the diffuse GALT must be addressed further. It is possible that establishment and maintenance of the spatial complexity of the diffuse GALT are determined, in part, by spatial differences in the distribution of components of the microbiota. It is also possible that the asymmetric distribution of components of the diffuse GALT helps define niches for various microbes.
Serum antibodies against components of the normal flora are consistently found in humans and other mammals (13). A mucosal immune response to components of the microbiota can be demonstrated in ex-germ-free mice (182). This response includes production of secretory IgAs. However, monoassociation experiments have revealed marked differences in the host humoral immune responses to different organisms (16), even though there are no constraints imposed upon the colonizing bacteria by competing indigenous microbes.
The origins of these different immune responses are undoubtedly complex, involving both host and microbial factors. These factors may include the relative spatial distributions of the organism and components of the GALT, as well as the ability of organisms to be translocated across the epithelium and delivered to regional lymph nodes or the spleen (14, 65). Such a hypothesis could be tested by using (i) germ-free inbred mice, with and without genetic manipulation of defined components of their immune systems or their epithelium; (ii) isogenic strains of a given bacterial species expressing defined endogenous or foreign epitopes; and (iii) prior or simultaneous administration of other competing organisms.
THE DIFFUSE AND ORGANIZED GUT-ASSOCIATED LYMPHOID TISSUES INFLUENCE THE EPITHELIUM
The “trialogue” referred to above views the intestinal ecosystem as being shaped by a series of interactions involving the microbiota, epithelium, and GALT. These interactions are probably dynamic, reciprocal, and combinatorial, making it difficult to separate out a dialogue from the trialogue. Nonetheless, two examples illustrate the influence of the GALT on intestinal epithelial cell biology. (i) Komano et al. used gene targeting to show that ablation of γδ TCR cells is associated with a reduction in crypt cell proliferation, the size of the crypts, and the rate of epithelial cell migration. In contrast, ablation of αβ TCR cells had no discernable effects on epithelial cell dynamics (111). (ii) Peyer’s patches are covered by a specialized follicle-associated epithelium (FAE) that contains M cells. M cells are specialized for transcytosis of macromolecules and microorganisms to professional antigen-presenting cells located in the underlying lymphoid follicle (172). A recent study has shown that M cells are derivatives of the enterocytic lineage and that they arise through a cross talk involving members of this lineage and B cells residing in the organized GALT (107). The evidence for this cross talk is as follows. First, a human intestinal adenocarcinoma-derived cell line (Caco2) normally assumes an enterocyte-like phenotype when it achieves confluency. Confluent Caco2 cells can switch to an M-cell-like phenotype when a suspension of B cells from Peyer’s patches is added to their basolateral surfaces. Second, injection of lymphocytes, recovered from mouse Peyer’s patches, into the submucosa of mouse small intestine resulted in the formation of submucosal lymphoid aggregates with an overlying FAE containing M cells. Third, the in vivo induction of an FAE with M cells requires Peyer’s patch-derived lymphocytes and cannot be reproduced with lymphocytes harvested from thymus or spleen. Moreover, in vitro differentiation of enterocytes to M cells can be programmed by B-cell-like Raj cells but not by T-cell-like Jurkat cells.
Studies in germ-free mice monoassociated with Salmonella typhimurium suggest that by inducing formation of an organized GALT, intestinal bacteria can contribute to the specification of M cell fate (173). This phenomenon should also be considered one of the factors that may determine host responsiveness to components of the microbiota (see above).
COLLABORATIONS BETWEEN THE EPITHELIUM AND THE MICROFLORA HELP CREATE AN ECOSYSTEM
Most species colonizing the mammalian intestine require fermentable carbohydrates as an energy source (168). The repertoire of saccharides that can be released into the lumen and metabolically processed by host factors and/or by microbial fermentation varies among different host species, as well as among individuals within a given species (42, 81).
Glycosidases that hydrolyze repetitive saccharide structures connected via β-linkages are produced by most members of the microbial community. Of the five principal genera present in the adult human colon—Bacteroides, Eubacterium, Bifidobacterium, Peptostreptococcus, and _Fusobacterium_—only Fusobacterium contains species that are predominantly nonsaccharolytic (168). In vitro studies of several normal components of the mouse colonic flora (E. coli, Eubacterium spp., and Fusobacterium spp.) have demonstrated that their growth in a continuous flow culture is regulated by their access to carbohydrate substrates (62). Thus, carbohydrate availability probably helps determine the niche that a given microbe is able to occupy.
The ability to degrade complex carbohydrates generated by the host epithelium is restricted to a few strains of intestinal bacteria (88, 94). Components of the colonic flora belonging to the genera Bifidobacterium and Ruminococcus produce α-glycosidases that are specific for the lacto-series core chains (Galβ1,3/4GlcNAcβ1,3Galβ1,4Glcβ1-) of glycoconjugates found in mucins and on the apical surfaces of intestinal epithelial cells (22a, 61a, 87a, 156a). There appears to be an in vivo selection for bacteria that are able to hydrolyze the oligosaccharide chains produced by the specific individual that they colonize. This was demonstrated by Hoskins and Boulding (90, 91) when they noted that the fecal flora of adult humans with the histo-blood group A phenotype degrade A but not B antigens while fecal flora recovered from adult humans with the histo-blood group B phenotype degrade B but not A antigens. These blood group antigen-degrading Bifidobacterium and Ruminococcus spp. comprise ≤1% of the cultivatable fecal microbiota (92, 139) and appear early during postnatal life, coincident with weaning. Their appearance in the microbiota can be inferred by analysis of the composition of glycosphingolipids in fecal samples. As long as an infant is breast fed, fecal glycosphingolipids resemble host epithelial cell glycosphingolipids since they are derived from exfoliated epithelial cells and have not been degraded by the microbiota. As soon as a child is no longer exclusively fed breast milk, fecal glycosphingolipids are degraded (118). This degradation process can be reproduced in vitro by incubating purified glycolipids with glycosidases recovered from the Ruminococcus or Bifidobacterium isolates (54, 93, 117).
The impact of host oligosaccharide processing on bacterial growth potential has been demonstrated in vitro (124). Addition of epithelial cell-derived mucins to an established continuous-flow culture of anaerobic isolates from human fecal flora belonging to the genera Lactobacillus, Bifidobacterium, Propionibacterium, Clostridium, and Streptococcus, as well as coliforms and Bacteroides fragilis, markedly increased the levels of secreted α- and β-glycosidases. The augmentation of soluble glycosidases was associated with enhanced growth.
Organisms that are able to metabolize complex carbohydrates should have an ecologic advantage since they have direct access to a host energy source and can also recruit a population of other organisms that utilize the released monosaccharides, further shaping the nutrient environment and the microbiological society in their intestinal habitat. Organisms that are able to induce specific host glycoconjugate production—such as B. thetaiotaomicron in NMRI mice or the segmented filamentous bacteria in BALB/c mice (see above)—may function to initiate the creation of an ecosystem by generating complex carbohydrates, thereby allowing subsequent colonization by species with the capacity to harvest monosaccharides from the induced oligosaccharides.
This hypothesis can be tested by using germ-free mice. As noted above, host complex carbohydrates represent both a marker for and a mediator of host-microbe interactions in the intestinal ecosystem. These complex carbohydrates have been defined structurally, and the genetic basis for their synthesis is known (125, 203, 214). There are several reports describing how glycoconjugates can be engineered in transgenic mice by forced expression of specific glycosyltransferases (56, 149, 160, 180). Thus, it is now possible to produce specific carbohydrate structures in the intestines of transgenic animals by using gut-specific promoters (see, e.g., references 26, 47a, 150a, and 183–185) and defined glycosyltransferases. The resulting mice can be used to study the selection of bacterial species based on their capacity to utilize the engineered host carbohydrate and to establish minimal functional model ecosystems.
It is important to point out that the capacity to metabolize complex carbohydrates may come at a price, i.e., a relative inability to metabolize other available substrates. Thus, what is most advantageous will undoubtedly depend upon the context and will differ for different organisms.
CROSSING THE CONTINUUM BETWEEN BEING A MEMBER OF THE MICROBIOTA AND BEING A PATHOGEN
Symbiotic relationships refer to those that involve mutual gain for both partners. Parasitic relationships benefit one partner but are harmful to the other. Sitting between symbiotic and parasitic are commensal relationships, where one partner gains whereas the other experiences neither gain nor loss. The relationship between a mammalian host and its intestinal microbiota is to a large extent symbiotic. However, when the components of the microflora are viewed as single entities instead of as a large polymicrobic society, many species appear to possess commensal and/or opportunistic traits. This means that given the opportunity, most intestinal bacteria will expand their habitats. The existence or expansion of commensal organisms in the ecosystem will have a variable impact on the host, depending upon factors that are expressed in either the bacterium, the given host, or both. These factors can be intrinsic properties or properties that are modified by environment. In this view, pathologic changes arise through a combinatorial mechanism where a coexistence of factors is required for initiation or progression of disease. Thus, “normal” and “pathogenic” should be viewed as relative terms when considering the microbiota.
Indigenous bacterial species can give rise to diseases in their host through a variety of mechanisms. For example, when the ecosystem is disrupted, minor components of the microbiota may expand within their normal habitat or may move to another habitat, where the host is unable to accommodate or tolerate the new colonizer. Some autoimmune responses in the host could arise as a consequence of immunodeterminants that are expressed in components of the microbiota and by host cell lineages. Potential mutagens and carcinogens could be generated through acquired or inherent metabolic activities of the microbiota. Components of the microbiota may acquire new genetic material via horizontal transfer. These gene cassettes can encode antibiotic resistance (145) and can be transferred from bacteria that only transiently reside in the gut (71). The gene cassettes can also encode virulence factors that provide growth and colonization advantages at the expense of normally beneficial host-bacterium relationships. Acquisition of these cassettes, which are known as pathogenicity islands (Pais), may represent a general mechanism by which a pathogenic strain emerges within the intestinal ecosystem (78). A variety of mechanisms may underlie the selection for Pai-containing strains in the intestine. For example, growth advantages may be imparted by enhancement of existing, or creation of novel, metabolic pathways. Acquisition of adhesion factors may favor persistence within a given niche or adaptation to a new habitat elsewhere in the gut.
Innocent until Proven Guilty
The gut microflora is an important component in the colonization resistance of the host (201). This resistance applies both to nonresident “classical” pathogens (e.g., Salmonella, Yersinia, Listeria, and Vibrio spp.) and to resident organisms. Potential pathogens and opportunistic bacteria are present in the microbiota, but their census is usually restricted unless the ecosystem is disrupted, for instance by antibiotics (7, 190). The pseudomembranous colitis caused by Clostridium difficile is a well-known example. Normal carriage of this bacterium appears to be low: 14% in healthy infants and 3% in adults as defined by fecal culture or by detection of its toxins. _C. difficile_-associated colitis appears only in conjunction with antibiotic therapy or treatment with immunosuppressive drugs (7, 123). Other examples of pathogens emerging from the normal gut microflora and placed in new environments where they are not tolerated by the host include bacteria associated with urinary tract infections (E. coli [208]), septicemia (E. coli, Klebsiella spp., members of the Enterobacteriaceae, Staphylococcus spp., and Enterococcus spp. [19]), and necrotizing enterocolitis in infants (Klebsiella spp., E. coli, and Clostridium spp. [112]).
A key event in the treatment of opportunistic enterocolitis is reconstitution of the ecological balance in the intestine (82, 201). Such a restitution can be directly curative, as has been shown when patients with relapsing pseudomembranous colitis are treated by local administration of whole fecal flora (177) or by inoculation with single bacterial strains (69, 178). These reports point to the future possibility of using probiotic rather than antibiotic strategies for treating certain infections. However, the complexity of the intact intestinal microbiota makes it very difficult to study the mechanisms of colonization resistance and the opportunistic traits of its various components. Germ-free mice represent an experimental system for simplifying the phenomenon of resistance to colonization and for defining its underlying mechanisms. For example, once a minimal functional ecosystem has been established in their intestine, these mice can be challenged with defined bacterial species.
Inflammatory Thoughts
Intestinal bacteria also play a role in development of graft-versus-host disease (GVHD) following allogenic organ transplantation (96). GVHD is mediated by donor lymphocytes that react with recipient tissue antigens. Experiments in mice have shown that GVH reactions can be completely avoided if the recipient is germ free or if the intestinal flora of conventionally raised animals is selectively reduced by antibiotics before transplantation (83). These results support the notion that GVHD involves activated donor T cells that cross-react with bacterial antigens and host endothelial epitopes. Gastrointestinal decontamination has been proven useful for preventing infection and GVHD in recipients of bone marrow transplants (204).
The origin of autoimmune diseases in humans remains elusive. A common view holds that affected individuals have an underlying genetic predisposition and that disease represents an inappropriate host response to normal environmental factors. Alternatively, these diseases may represent an appropriate host response to abnormal stimuli (see, e.g., references 155 and 156). There is accumulating evidence that host microbial populations may contribute in a significant way to the pathogenesis of these diseases (reviewed in reference 170). For example, a pathologic state resembling human inflammatory bowel disease (IBD) with associated ankylosing spondylitis occurs in transgenic rats expressing human HLA-B27 (80). These conditions do not occur in germ-free animals (191). Mice homozygous for null alleles of the interleukin-2 (IL-2), IL-10, or TCR genes develop IBD when raised under conventional conditions (114, 141, 164). In the case of IL-2- or IL-10-deficient mice, inflammation does not develop when animals are raised in a germ-free state (114, 164).
The modulating role of the microbiota in the pathogenesis of IBD is also illustrated by chemical disruption of the epithelial barrier in mice with no genetic perturbations of their immune system. The IBD induced by dextran sodium sulfate is more severe in NMRI mice reared under germ-free conditions than in conventionally raised animals but is not limited to the germ-free mice (9). This observation underscores the importance of considering the microbiota when designing and interpreting models of chronic inflammatory conditions.
The clinical and pathological similarities between postinfectious aseptic joint inflammation and rheumatoid arthritis have suggested a causative link between certain microbes and rheumatologic diseases (113). Retroviruses and enteropathogenic bacteria, such as Salmonella spp., Yersinia enterocolitica, and Shigella spp., are the most commonly invoked pathogens. However, other bacteria, including components of the indigenous human gastrointestinal flora, have been implicated (134). Pendergast et al. (154) noted that E. coli, Streptococcus spp., Staphylococcus spp., and Clostridium spp. isolated from the fecal microbiota of patients with ankylosing spondylitis express immunodeterminants similar to those produced by the host synovial cells. As with IBD, comparisons of germ-free and conventionally raised animals have shown that the severity of both chemical- and adjuvant-induced arthritis is modified by the microbiota (22, 109, 110).
Bacteria as Endogenous Risk Factors for Tumorigenesis
Intestinal bacteria may contribute to colorectal tumorigenesis (70). Analyses of germ-free and conventionally raised mice have demonstrated that indigenous intestinal bacteria produce carcinogens such as alkylating agents and nitroso compounds (104, 135, 140). Continuous exposure to these compounds could constitute an endogenous risk factor that promotes the multistep journey to neoplasia (58, 107).
Animals with a germ line mutation in the adenomatous polyposis coli gene (_Apc_Min) develop multiple intestinal adenomas (189). Conventionally raised _Apc_Min mice have a statistically significant twofold increase in tumor multiplicity in the midportion of their small intestine compared to germ-free animals. No significant differences were noted in other regions of the intestine (52). Although the magnitude of the effect is modest, the regional specificity of the response is intriguing and could reflect regional variations in the composition of the microbiota as well as the GALT. Comparisons of germ-free _Apc_Min mice and ex-germ-free _Apc_Min animals that have been colonized with known components of the microbiota represent the type of opportunity that gnotobiology can offer to help us understand the contributions of bacteria and their gene products to tumorigenesis.
THE GASTRIC ECOSYSTEM: AN OPEN WILDERNESS FOR MICROBES?
H. pylori Ecology
The human stomach has few resident microorganisms (76). Colonization represents a challenge, in part because of the harsh luminal environment. Helicobacter pylori inhabits the stomachs of more than half of the world’s population. It has probably coevolved with its human host so that it can adapt to and occupy the gastric ecosystem. In most hosts, colonization is characterized by an asymptomatic carriage that persists for decades. In a subset of hosts (∼10%) (44), colonization leads to pathologic changes: chronic active gastritis, peptic ulcer disease, and even neoplasia (147, 205).
The relationship between this bacterium and its human host cannot be readily classified as parasitic, commensal, or symbiotic (23). However, its persistent residency in an open ecosystem that contains a continuously renewing epithelium, as well as its potential for causing overt disease in some but not all hosts, is in some ways analogous to the relationship between the components of the intestinal microbiota and their host. An important advantage obtained from studying H. pylori is that the “pathogenic” state is associated with a host response that is readily detectable, assignable to this organism, and referable to a genome whose entire complement of 1,590 open reading frames is known (193). Moreover, the strategies used by this organism to induce pathologic changes in its human host may be generally applicable to other gut commensals.
Testing the Role of Attachment
Only a minor fraction of a population of colonizing H. pylori is believed to adhere to gastric epithelial cells. Mathematical modeling studies suggest that it is this adherent population that is required for persistent colonization of its human host (108). H. pylori colonizes a genetically diverse population of humans. Not surprisingly, in vitro studies indicate that this organism can express a wide variety of binding determinants that appear to recognize a wide variety of epithelial receptors (46).
A transgenic-mouse model has been developed to assess whether coexpression of a bacterial binding determinant and its host epithelial receptor affects colonization of the gastric ecosystem and the course of the host-microbe interactions. The blood group antigen Lewis b (Leb) represents one well-characterized epithelial receptor for H. pylori adhesins (24). Leb is produced in the pit and surface mucous cells of the human stomach (166). Binding to Leb appears to be determined by an _omp_-related bacterial protein known as BabA (98). The human α1,3/4 fucosyltransferase responsible for producing Leb (116) was expressed in the surface mucous cells of transgenic mice (56). Clinical isolates of H. pylori, recovered from Leb-positive patients with gastritis, were then inoculated into transgenic animals and their normal, nontransgenic, Leb-negative littermates. A high-density persistent infection occurred with high efficiency in both groups of mice (>80% after a single gavage [72]). Bacteria were found attached to the epithelium and in the mucus layer in transgenic mice, whereas they were associated only with the mucus layer in nontransgenic mice. Although attachment was not required for colonization, it did affect the host response. Attachment was associated with (i) production of antibodies to Lex carbohydrate epitopes produced by the bacteria and by acid-secreting parietal cells of the host (see below), (ii) more extensive parietal cell loss, (iii) more severe chronic gastritis, and (iv) induction of an organized GALT (72). Thus, if an H. pylori strain expressing an adhesin colonizes a host that produces a functional epithelial receptor for that adhesin, the destiny of colonization may be skewed away from a long-term commensal relationship and toward a parasitic relationship.
Significance of Molecular Mimicry
Like other gram-negative bacteria, H. pylori lipopolysaccharide (LPS) can undergo antigenic variation (48, 143). However, H. pylori LPS is less immunogenic than the LPS of other gut bacteria (18). This phenomenon appears to be related to the lipid A component of LPS. The O-specific chain of its LPS contains carbohydrate epitopes that are structurally very similar to human fucosylated histo-blood group antigens (8, 141a). Recent studies show that there is a high degree of phase variation within a given H. pylori strain due to variable expression of the fucosyltransferases responsible for synthesis of these structures (6). H. pylori contains fucosyltransferases (193) that can add α1,2- or α1,3-linked fucosyl residues to generate Lex- and Ley-containing glycoconjugates. The bacterial α1,3-fucosyltransferase responsible for Lex production has sequence similarity to orthologous human α1,3-fucosyltransferases (66, 127). Studies of clinical isolates have shown a correlation between the Lewis epitopes of H. pylori and the Lewis phenotype of its host (208). This could reflect a prior selection of strains that match the Lewis environment of their gastric niches or an adaptation initiated once a strain has entered its gastric habitat. Phase variation may underlie such an adaptation.
Molecular mimicry represents a way of evading host immune system surveillance. However, this evasive maneuver also increases the risk of “autoimmune” disease in the host. Lex and Ley epitopes are associated with mucus glycoproteins produced by mucus neck cells with the H+/K+-ATPase expressed in acid-producing parietal cells (5, 166). Circulating antibodies to this protein and parietal cells are commonly encountered in individuals with atrophic gastritis (102), including those who have evidence of exposure to H. pylori (4, 4a, 5, 41a, 115, 144). As noted above, a similar phenomenon can be reproduced in mice (5, 72).
Molecular mimicry may not only contribute to H. pylori pathogenesis but, as alluded to above, also underlie the development of inflammatory bowel diseases. The relapsing nature of these chronic inflammatory conditions could reflect periodic changes in the intestinal flora and/or epithelial barrier function in genetically predisposed hosts. This conceptualization of etiology switches the focus from autoimmunity to cross-reactivity between microbial and host immunodeterminants. Unfortunately, testing this hypothesis is complicated by the changing nature of the microbiota within and between individuals and by the genetic diversity of human hosts. Validation in germ-free animals represents an attractive possibility.
When Is H. pylori a Pathogen?
H. pylori illustrates how horizontal transmission of genetic material can change a commensal organism to a pathogen. H. pylori strains isolated from individuals with peptic ulcer disease and gastric adenocarcinoma typically produce CagA (44) and a cytotoxin known as VacA (126, 192). vacA and cagA are separated by 300 kb in the H. pylori genome, and vacA expression does not require cagA expression (196, 213). H. pylori has been divided into two major groups, type I and type II. Type I strains are cagA+ and are associated with chronic active gastritis and an increased risk for adenocarcinoma. Type II strains are generally not associated with the development of gastric pathologic findings. They lack the cagA gene, and although they contain vacA homologs, they do not produce a functional toxin (213). Thus, an arbitrary division into pathogenic and nonpathogenic isolates can be made based on the presence of cagA. This gene is part of a 40-kb cassette, termed cag (33, 45), which is believed to originate from a source other than H. pylori. cag encodes more than 40 putative proteins with sequence homologies to potential virulence factors. These factors include proteins for pilus and flagellum assembly as well as the secretion systems used by several pathogens to export virulence factors (61, 167). Similar gene fragments, the Pais, can be found in a number of pathogens, including Yersinia spp., Salmonella spp., Shigella spp., Pseudomonas aeruginosa, enteropathogenic E. coli, and several other attaching and effacing organisms. Pais usually encode proteins required for the assembly of adhesive structures and for protein secretion (78). Pais are absent or very rare in nonpathogenic variants of the same species. H. pylori attachment to epithelial cells is associated with host protein phosphorylation and pedestal formation that is dependent on an intact cag gene (179). A similar process occurs in enteropathogenic E. coli attachment to epithelial cells and is dependent upon a Pai-associated secretion system that transfers the epithelial cell receptor from the bacterium (105). Pais contain repeated sequence elements at both ends, which favor insertion and deletion. It is possible that strains of H. pylori fluctuate between a _cag_-deficient type II state that favors persistence without disease and a cag+ type I state that increases the risk of developing gastric pathologic changes.
Germ-free mice provide an opportunity for examining horizontal gene transfer under defined conditions (71). For example, monocontamination with genetically tagged isogenic H. pylori strains, with and without cag, should allow an assessment of the frequency of such an exchange and its biological consequences.
Bacteria as Therapeutic Agents—Probiotics
Germ-free mice can be used to test the feasibility of using “probiotic” therapy to prevent or abolish colonization of the gut with organisms such as H. pylori. Lactobacillus spp. are the principal bacteria found in the stomachs of normal fasting mice. The density of their colonization is low (≤103 per ml of gastric contents). Kabir et al. (100) added H. pylori to germ-free BALB/c mice and ex-germ-free BALB/c mice that had been previously monocontaminated with Lactobacillus salivarius. This organism inhibited H. pylori attachment and colonization. Moreover, addition of L. salivarius to ex-germ-free mice after they had been colonized with H. pylori eliminated H. pylori from the stomachs of these animals (100).
PROSPECTUS
The importance of understanding the relationships between humans and their resident microbial populations has been emphasized for over 100 years. The first report describing how animals could be reared under germ-free conditions appeared 102 years ago (148). The questions and the technology are old, but their applicability to understanding how the intestinal ecosystem is shaped and maintained represents an opportunity for the modern scientist. We now have the capacity to create simplified and defined model ecosystems in ex-germ-free mice. We can genetically manipulate both the host epithelium and its associated immune system, as well as potential microbial inhabitants. The ability to perform these manipulations should provide molecular insights into the factors that govern ecologic stability in the gut. The combination of gnotobiotics and molecular genetics should provide a deeper understanding of how pathogens are created, how they gain control of this habitat, and the contributions made by “normal” gut inhabitants to disease pathogenesis. Such understanding, in turn, could lead to the development of novel chemicals and microbes for use in prebiotic and probiotic strategies to prevent or cure infectious diseases and perhaps immunopathologic disorders.
REFERENCES
- 1.Adlerberth I, Carlsson B, de Man P, Jalil F, Khan S R, Larsson P, Mellander L, Svanborg C, Wold A E, Hansson L Å. Intestinal colonization of enterobacteriaceae in Pakistani and Swedish hospital delivered children. Acta Pediatr Scand. 1991;80:602–610. doi: 10.1111/j.1651-2227.1991.tb11917.x. [DOI] [PubMed] [Google Scholar]
- 2.Alam M, Midtvedt T, Uribe A. Differential cell kinetics in the ileum and colon of germ-free rats. Scand J Gastroenterol. 1994;29:445–451. doi: 10.3109/00365529409096836. [DOI] [PubMed] [Google Scholar]
- 3.Al-Nafussi A I, Wright N A. Cell kinetics in the mouse small intestine during immediate postnatal life. Virchows Arch Cell Pathol. 1982;40:51–62. doi: 10.1007/BF02932850. [DOI] [PubMed] [Google Scholar]
- 4.Appelmelk B J, Negrini R, Moran A P, Kuipers E J. Molecular mimicry between Helicobacter pylori and the host. Trends Microbiol. 1997;5:70–73. doi: 10.1016/S0966-842X(96)10084-6. [DOI] [PubMed] [Google Scholar]
- 4a.Appelmelk B J, Faller G, Claeys D, Kirchner T, Vandenbroucke-Grauls C M. Bugs on trial: the case of Helicobacter pylori and autoimmunity. Immunol Today. 1998;19:296–299. doi: 10.1016/s0167-5699(98)01281-x. [DOI] [PubMed] [Google Scholar]
- 5.Appelmelk B J, Simoons-Smit I, Negrini R, Moran A P, Aspinall G O, Forte J G, de Vries T, Quam H, Verboom T, Maaskant J J, Ghiara P, Kuipers E J, Bloemena E, Tadema T M, Townsend R R, Tyagarajan K, Crothers J M, Jr, Monteiro M A, Savio A, de Graff J. Potential role of molecular mimicry between Helicobacter pylori lipopolysaccharide and host Lewis blood group antigens in autoimmunity. Infect Immun. 1996;64:2031–2040. doi: 10.1128/iai.64.6.2031-2040.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Appelmelk B J, Shiberu B, Trinks C, Tapsi N, Zheng P Y, Verboom T, Maaskant J, Hokke C H, Schiphorst C M, Blanchard D, Simoons-Smit I M, Van den Eijnden D H, Vandenbrouche-Grauls C M. Phase variation in Helicobacter pylori lipopolysaccharide. Infect Immun. 1998;66:70–76. doi: 10.1128/iai.66.1.70-76.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Araneo B A, Cebra J J, Beuth J, Fuller R, Heidt P J, Midtvedt T, Nord C E, Nieuwenhuis P, Manson W L, Pulverer G, Rusch V C, Tanaka R, van der Waaij D, Walker R I, Wells C L. Problems and priorities for controlling opportunistic pathogens with new antimicrobial strategies: an overview of current literature. Zentbl Bakteriol. 1996;283:431–465. doi: 10.1016/s0934-8840(96)80122-8. [DOI] [PubMed] [Google Scholar]
- 8.Aspinall G O, Monteiro M A. Lipopolysaccharides of Helicobacter pylori strains P466 and MO19: structures of the O antigen and core oligosaccharide chains. Biochemistry. 1996;35:2498–2504. doi: 10.1021/bi951853k. [DOI] [PubMed] [Google Scholar]
- 9.Axelsson L G, Midtvedt T, Bylund-Fellenius A C. The role of intestinal bacteria, bacterial translocation and endotoxin in dextran sodium sulphate-induced colitis in the mouse. Microb Ecol Health Dis. 1996;9:225–237. [Google Scholar]
- 10.Balmer S E, Wharton B A. Diet and faecal flora in the newborn: breast milk and infant formula. Arch Dis Child. 1989;64:1672–1677. doi: 10.1136/adc.64.12.1672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Barbara G, Vallance B A, Collins S M. Persistent intestinal neuromuscular dysfunction after acute nematode infection in mice. Gastroenterology. 1997;113:1224–1232. doi: 10.1053/gast.1997.v113.pm9322517. [DOI] [PubMed] [Google Scholar]
- 12.Bennet R, Eriksson M, Nord C E, Zetterström R. Fecal bacterial microflora of newborn infants during intensive care management and treatment with five antibiotic regimens. Pediatr Infect Dis. 1986;5:533–539. doi: 10.1097/00006454-198609000-00009. [DOI] [PubMed] [Google Scholar]
- 13.Berg R. Host immune response to antigens of the indigenous intestinal flora. In: Hentges D, editor. Human intestinal microflora in health and disease. New York, N.Y: Academic Press, Inc.; 1983. pp. 101–126. [Google Scholar]
- 14.Berg R D. Bacterial translocation from the gastrointestinal tract. Trends Microbiol. 1995;3:149–154. doi: 10.1016/s0966-842x(00)88906-4. [DOI] [PubMed] [Google Scholar]
- 15.Berg R D. The indigenous gastrointestinal microflora. Trends Microbiol. 1996;4:430–435. doi: 10.1016/0966-842x(96)10057-3. [DOI] [PubMed] [Google Scholar]
- 16.Berg R D, Savage D C. Immune responses of specific pathogen-free and gnotobiotic mice to antigens of indigenous and nonindigenous microorganisms. Infect Immun. 1975;11:320–329. doi: 10.1128/iai.11.2.320-329.1975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bhutta Z A, Naqvi S H, Muzaffar T, Farooqui B J. Neonatal sepsis in Pakistan: presentation and pathogens. Acta Pediatr Scand. 1991;80:596–601. doi: 10.1111/j.1651-2227.1991.tb11916.x. [DOI] [PubMed] [Google Scholar]
- 18.Birkholz S, Knipp U, Nietzki C, Adamek R J, Opferkuch W. Immunological activity of lipopolysaccharide of Helicobacter pylori on human peripheral mononuclear blood cells in comparison to lipopolysaccharide of other intestinal bacteria. FEMS Immunol Med Microbiol. 1993;6:317–324. doi: 10.1111/j.1574-695X.1993.tb00344.x. [DOI] [PubMed] [Google Scholar]
- 19.Bjerknes M. A test of the stochastic theory of stem cell differentiation. Biophys J. 1986;49:1223–1227. doi: 10.1016/S0006-3495(86)83751-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bjerknes M, Cheng H. The stem cell zone of the small intestinal epithelium. I. Evidence from Paneth cells in the adult mouse. Am J Anat. 1981;160:51–63. doi: 10.1002/aja.1001600105. [DOI] [PubMed] [Google Scholar]
- 21.Bjerknes M, Cheng H. The stem cell zone of the small intestinal epithelium. III. Evidence from columnar, enteroendocrine, and mucus cells in the adult mouse. Am J Anat. 1981;160:77–91. doi: 10.1002/aja.1001600107. [DOI] [PubMed] [Google Scholar]
- 22.Björk J, Kleinau S, Midtvedt T, Klareskog L, Smedegård G. Role of the bowel flora for development of immunity to hsp65 and arthritis in three experimental models. Scand J Immunol. 1994;40:648–652. doi: 10.1111/j.1365-3083.1994.tb03518.x. [DOI] [PubMed] [Google Scholar]
- 22a.Björk S, Breimer M E, Hansson G C, Karlsson K-A, Leffler H. Structures of blood group glycosphingolipids of human small intestine. A relation between the expression of fucolipids of epithelial cells and the ABO, Le and Se phenotype of the donor. Biol Chem. 1987;262:6758–6765. [PubMed] [Google Scholar]
- 23.Blaser M J. Ecology of Helicobacter pylori in the human stomach. J Clin Invest. 1997;100:1–4. doi: 10.1172/JCI119588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Borén T, Falk P, Roth K A, Larson G, Normark S. Attachment of Helicobacter pylori to human gastric epithelium mediated by blood group antigens. Science. 1993;262:1892–1895. doi: 10.1126/science.8018146. [DOI] [PubMed] [Google Scholar]
- 25.Brandtzaeg P, Halstensen T S, Kett K, Krajci P, Kvale D, Rognum T O, Scott H, Sollid L M. Immunology and immunopathology of human gut mucosa: humoral immunity and intraepithelial lymphocytes. Gastroenterology. 1989;97:1562–1584. doi: 10.1016/0016-5085(89)90406-x. [DOI] [PubMed] [Google Scholar]
- 26.Bry L, Falk P, Huttner K, Ouellette A, Midtvedt T, Gordon J I. Paneth cell differentiation in the developing intestine of normal and transgenic mice. Proc Natl Acad Sci USA. 1994;91:10335–10339. doi: 10.1073/pnas.91.22.10335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26a.Bry, L., P. Falk, T. Midtvedt, and J. I. Gordon. Unpublished data.
- 27.Bry L, Falk P G, Gordon J I. Genetic engineering of carbohydrate biosynthetic pathways in transgenic mice demonstrates cell-cycle-associated regulation of glycoconjugate production in small intestinal epithelial cells. Proc Natl Acad Sci USA. 1996;93:1161–1166. doi: 10.1073/pnas.93.3.1161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bry L, Falk P G, Midtvedt T, Gordon J I. A model for host-microbial cross-talk in an open mammalian ecosystem. Science. 1996;273:1380–1383. doi: 10.1126/science.273.5280.1380. [DOI] [PubMed] [Google Scholar]
- 29.Bullen C L, Tearle P V, Willis A T. Bifidobacteria in the intestinal tract of infants: an in vivo study. J Med Microbiol. 1976;9:325–333. doi: 10.1099/00222615-9-3-325. [DOI] [PubMed] [Google Scholar]
- 30.Bush T G, Savidge T C, Freeman T C, Cox H J, Campbell E A, Mucke L, Johnson M H, Sofroniew M V. Fulminant jejuno-ileitis following ablation of enteric glia in adult transgenic mice. Cell. 1998;93:189–201. doi: 10.1016/s0092-8674(00)81571-8. [DOI] [PubMed] [Google Scholar]
- 31.Calvert R, Porthier P. Migration of fetal intestinal intervillous cells in neonatal mice. Anat Rec. 1990;227:199–206. doi: 10.1002/ar.1092270208. [DOI] [PubMed] [Google Scholar]
- 32.Carlstedt-Duke B, Midtvedt T, Nord C E, Gustafsson B E. Isolation and characterization of a mucin degrading strain of Peptostreptococcus from rat intestinal tract. Acta Pathol Microbiol Immunol Scand Sect B. 1986;94:292–300. doi: 10.1111/j.1699-0463.1986.tb03056.x. [DOI] [PubMed] [Google Scholar]
- 33.Censini S, Lange C, Xiang Z, Crabtree J E, Ghiara P, Borodovsky M, Rappuoli R, Covacci A. Cag, a pathogenicity island of Helicobacter pylori, encodes type I-specific and disease-associated virulence factors. Proc Natl Acad Sci USA. 1996;93:14648–14653. doi: 10.1073/pnas.93.25.14648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cheng H. Origin, differentiation and renewal of the four main epithelial cell types in the mouse small intestine. II. Mucous cells. Am J Anat. 1974;141:481–502. doi: 10.1002/aja.1001410404. [DOI] [PubMed] [Google Scholar]
- 35.Cheng H. Origin, differentiation and renewal of the four main epithelial cell types in the mouse small intestine. IV. Paneth cells. Am J Anat. 1974;141:521–536. doi: 10.1002/aja.1001410406. [DOI] [PubMed] [Google Scholar]
- 36.Cheng H, Bjerknes M. Whole population cell kinetics of mouse duodenal, jejunal, ileal and colonic epithelial as determined by radioautography and flow cytometry. Anat Rec. 1982;203:251–264. doi: 10.1002/ar.1092030207. [DOI] [PubMed] [Google Scholar]
- 37.Cheng H, Bjerknes M. Cell production in mouse intestinal epithelium measured by stathmokinetic flow cytometry and Coulter particle counting. Anat Rec. 1983;207:427–434. doi: 10.1002/ar.1092070305. [DOI] [PubMed] [Google Scholar]
- 38.Cheng H, Bjerknes M. Whole population kinetics and postnatal development of the mouse intestinal epithelium. Anat Rec. 1985;211:420–426. doi: 10.1002/ar.1092110408. [DOI] [PubMed] [Google Scholar]
- 39.Cheng H, Leblond C P. Origin, differentiation and renewal of the four main epithelial cell types in the mouse small intestine. I. Columnar cells. Am J Anat. 1974;141:461–480. doi: 10.1002/aja.1001410403. [DOI] [PubMed] [Google Scholar]
- 40.Cheng H, Leblond C P. Origin, differentiation and renewal of the four main epithelial cell types in the mouse small intestine. III. Enteroendocrine cells. Am J Anat. 1974;141:503–520. doi: 10.1002/aja.1001410405. [DOI] [PubMed] [Google Scholar]
- 41.Cheng H, Leblond C P. Origin, differentiation and renewal of the four main epithelial cell types in the mouse small intestine. V. Unitarian theory of the origin of the four epithelial cell types. Am J Anat. 1974;141:537–561. doi: 10.1002/aja.1001410407. [DOI] [PubMed] [Google Scholar]
- 41a.Claeys D, Faller G, Appelmelk B J, Negrini R, Kirchner T. The gastric H+K+ ATPase is a major autoantigen in chronic Helicobacter pylori gastritis with body mucosa atrophy. Gastroenterology. 1998;115:340–347. doi: 10.1016/s0016-5085(98)70200-8. [DOI] [PubMed] [Google Scholar]
- 42.Clausen H, Hakomori S I. ABH and related histoblood group antigens: immunochemical differences in carrier isotypes and their distribution. Vox Sang. 1989;56:1–20. doi: 10.1111/j.1423-0410.1989.tb03040.x. [DOI] [PubMed] [Google Scholar]
- 43.Cossart P, Boquet P, Normark S, Rappuoli R. Cellular microbiology emerging. Science. 1996;271:315–316. doi: 10.1126/science.271.5247.315. [DOI] [PubMed] [Google Scholar]
- 44.Covacci A, Censini S, Bugnoli M, Petracca R, Burroni D, Macchia G, Massone A, Papini E, Xiang Z, Figura N, Rappuoli R. Molecular characterization of the 128-kD immunodominant antigen of Helicobacter pylori associated with cytotoxicity and duodenal ulcer. Proc Natl Acad Sci USA. 1993;90:5791–5795. doi: 10.1073/pnas.90.12.5791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Covacci A, Falkow S, Berg D E, Rappuoli R. Did the inheritance of a pathogenicity island modify the virulence of Helicobacter pylori? Trends Microbiol. 1997;5:205–208. doi: 10.1016/S0966-842X(97)01035-4. [DOI] [PubMed] [Google Scholar]
- 46.Cover T L, Blaser M J. Helicobacter pylori infection, a paradigm for chronic mucosal inflammation: pathogenesis and implications for eradication and prevention. Adv Intern Med. 1996;42:85–117. [PubMed] [Google Scholar]
- 47.Croft C N, Cotton P B. Gastrointestinal cell loss in man. Digestion. 1973;8:144–160. doi: 10.1159/000197310. [DOI] [PubMed] [Google Scholar]
- 47a.Crossman M W, Hauft S M, Gordon J I. The mouse ileal lipid binding protein gene: a model for studying axial patterning during gut morphogenesis. J Cell Biol. 1994;126:1547–1564. doi: 10.1083/jcb.126.6.1547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Danaher R J, Levin J C, Arking D, Burch C L, Sandlin R, Stein D C. Genetic basis of Neisseria gonorrhoeae lipooligosaccharide antigenic variation. J Bacteriol. 1995;177:7275–7279. doi: 10.1128/jb.177.24.7275-7279.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Darmoul D, Brown D, Selsted M E, Ouellette A J. Cryptdin gene expression in developing mouse small intestine. Am J Physiol (Gastrointest Liver Physiol) 1997;272:G197–G206. doi: 10.1152/ajpgi.1997.272.1.G197. [DOI] [PubMed] [Google Scholar]
- 50.Darmoul D, Ouellette A J. Positional specificity of defensin gene expression reveals Paneth cell heterogeneity in mouse small intestine. Am J Physiol (Gastrointest Liver Physiol) 1996;271:G68–G74. doi: 10.1152/ajpgi.1996.271.1.G68. [DOI] [PubMed] [Google Scholar]
- 51.De Kruif P. Microbe hunters. New York, N.Y: Harcourt & Brace Co.; 1926. [Google Scholar]
- 52.Dove W F, Clipson L, Gould K A, Luongo C, Marshall D J, Moser A R, Newton M A, Jacoby R F. Intestinal neoplasia in the APCMin mouse: independence from microbial and natural killer (beige locus) status. Cancer Res. 1997;57:812–814. [PubMed] [Google Scholar]
- 53.Escherich T. The intestinal bacteria of the neonate and breast-fed infant. Forschritte der Medizin, vol. 3. Featured in. Rev Infect Dis. 1885;10:1220–1225. doi: 10.1093/clinids/10.6.1220. , 1988. [DOI] [PubMed] [Google Scholar]
- 54.Falk P, Hoskins L C, Larson G. Bacteria of the human intestinal microbiota produce glycosidases specific for lacto-series glycosphingolipids. J Biochem. 1990;108:466–474. doi: 10.1093/oxfordjournals.jbchem.a123223. [DOI] [PubMed] [Google Scholar]
- 55.Falk P, Roth K A, Gordon J I. Lectins are sensitive tools for defining the differentiation programs of mouse gut epithelial cell lineages. Am J Physiol (Gastrointest Liver Physiol) 1994;266:G987–G1003. doi: 10.1152/ajpgi.1994.266.6.G987. [DOI] [PubMed] [Google Scholar]
- 56.Falk P G, Bry L, Holgersson J, Gordon J I. Expression of a human α-1,3/4 fucosyltransferase in the pit cell lineage of FVB/N mouse stomach results in production of Lewisb-containing glycoconjugates: a potential transgenic mouse model for studying Helicobacter pylori infection. Proc Natl Acad Sci USA. 1995;92:1515–1519. doi: 10.1073/pnas.92.5.1515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Faller G, Steininger H, Eck M, Hensen J, Hann E G, Kirchner T. Antigastric autoantibodies in Helicobacter pylori gastritis: prevalence, in situ binding sites and clues for clinical relevance. Virchows Arch. 1996;427:483–486. doi: 10.1007/BF00199508. [DOI] [PubMed] [Google Scholar]
- 58.Fearon E R, Vogelstein B. A genetic model for colorectal tumorigenesis. Cell. 1990;61:759–767. doi: 10.1016/0092-8674(90)90186-i. [DOI] [PubMed] [Google Scholar]
- 59.Fedorak R N. Naturally occurring and experimental models of inflammatory bowel disease. In: Kirstner J B, Shorter R G, editors. Inflammatory bowel disease. 4th ed. Baltimore, Md: The Williams & Wilkins Co.; 1995. pp. 71–95. [Google Scholar]
- 60.Finlay B B, Cossart P. Exploitation of mammalian host cell functions by bacterial pathogens. Science. 1997;276:718–725. doi: 10.1126/science.276.5313.718. [DOI] [PubMed] [Google Scholar]
- 61.Finlay B B, Falkow S. Common themes in bacterial pathogenesis revisited. Microbiol Mol Biol Rev. 1997;61:136–169. doi: 10.1128/mmbr.61.2.136-169.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61a.Finne J, Breimer M E, Hansson G C, Karlsson K A, Leffler H, Vliegenthart J F, van Halbeek H. Novel polyfucosylated N-linked glycopeptides with blood group A, H, X, and Y determinants from human small intestinal epithelial cells. J Biol Chem. 1989;264:5720–5735. [PubMed] [Google Scholar]
- 62.Freter R, Brickner H, Botney M, Cleven D, Aranki A. Mechanisms that control bacterial populations in continuous-flow culture models of mouse large intestinal flora. Infect Immun. 1983;39:686–703. doi: 10.1128/iai.39.2.676-685.1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Friedrich G, Soriano P. Promoter traps in embryonic stem cells: a genetic screen to identify and mutate developmental genes in mice. Genes Dev. 1991;5:1513–1523. doi: 10.1101/gad.5.9.1513. [DOI] [PubMed] [Google Scholar]
- 64.Garabedian E M, Roberts L J J, McNevin M S, Gordon J I. Examining the role of Paneth cells in the small intestine by lineage ablation in transgenic mice. J Biol Chem. 1997;272:23729–23740. doi: 10.1074/jbc.272.38.23729. [DOI] [PubMed] [Google Scholar]
- 65.Gautreaux M, Gelder F, Deitch E, Berg R. Adoptive transfer of T lymphocytes to T-cell-depleted mice inhibits Escherichia coli translocation from the gastrointestinal tract. Infect Immun. 1995;63:3827–3834. doi: 10.1128/iai.63.10.3827-3834.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Ge Z M, Chan N W C, Palcic M M, Taylor D E. Cloning and heterologous expression of an α-1,3-fucosyltransferase gene from the gastric pathogen Helicobacter pylori. J Biol Chem. 1997;272:21357–21363. doi: 10.1074/jbc.272.34.21357. [DOI] [PubMed] [Google Scholar]
- 67.Goldblum R M, Hansson L Å, Brandtzaeg P. The mucosal defense system. In: Stiehm E R, editor. Immunologic disorders in infants and children. Philadelphia, Pa: The W. B. Saunders Co.; 1996. pp. 159–199. [Google Scholar]
- 68.Goodlad R A, Wright N A. Quantitative studies on epithelial replacement in the gut. In: Tichen T A, editor. Techniques in life sciences. Digestive physiology. Dublin, Ireland: Elsevier Biomedical Press; 1982. pp. 212/1–212/23. [Google Scholar]
- 69.Gorbach S L, Chang T W, Goldin B. Successful treatment of relapsing Clostridium difficile colitis with Lactobacillus GG. Lancet. 1987;ii:1519. doi: 10.1016/s0140-6736(87)92646-8. [DOI] [PubMed] [Google Scholar]
- 70.Gorbach, S. L., and B. R. Goldin. 1990. The intestinal microflora and the colon cancer connection. Rev. Infect. Dis. 12(Suppl. 2):S252–S261. [DOI] [PubMed]
- 71.Gruzza M, Fons M, Ouriet M F, Duval-Iflah Y, Ducluzeau R. Study of gene transfer in vitro and in the digestive tract of gnotobiotic mice from Lactococcus lactis strains to various strains belonging to human intestinal flora. Microb Releases. 1994;2:183–189. [PubMed] [Google Scholar]
- 72.Guruge J L, Falk P G, Lorenz R G, Dans M, Wirth H P, Blaser M J, Berg D E, Gordon J I. Epithelial attachment alters the outcome of Helicobacter pylori infection. Proc Natl Acad Sci USA. 1998;95:3925–3930. doi: 10.1073/pnas.95.7.3925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Gustafsson, B. E. 1948. Germ-free rearing of rats, general techniques. Acta Pathol. Microbiol. Immunol. Scand. 111(Suppl. LXX).
- 74.Gustafsson B E. Lightweight stainless steel systems for rearing germfree animals. Ann N Y Acad Sci. 1959;78:17–28. doi: 10.1111/j.1749-6632.1959.tb53092.x. [DOI] [PubMed] [Google Scholar]
- 75.Gustafsson B E. Vitamin K deficiency in germfree rats. Ann N Y Acad Sci. 1959;78:166–173. doi: 10.1111/j.1749-6632.1959.tb53101.x. [DOI] [PubMed] [Google Scholar]
- 76.Gustafsson B E. The physiological importance of the colonic microflora. Scand J Gastroenterol. 1982;77:117–133. [PubMed] [Google Scholar]
- 77.Gustafsson B E, Midtvedt T, Strandberg K. Effects of microbial contamination on the cecum enlargement of germ-free rats. Scand J Gastroenterol. 1970;5:309–314. [PubMed] [Google Scholar]
- 78.Hacker J, Blumoehler G, Muhldorfer I, Tschape H. Pathogenicity islands of virulent bacteria—structure, function and impact on microbial evolution. Mol Microbiol. 1997;23:1089–1097. doi: 10.1046/j.1365-2958.1997.3101672.x. [DOI] [PubMed] [Google Scholar]
- 79.Hagemann R F, Sigdestad C P, Lesher S. A quantitative description of the intestinal epithelium of the mouse. Am J Anat. 1971;129:41–51. doi: 10.1002/aja.1001290104. [DOI] [PubMed] [Google Scholar]
- 80.Hammer R E, Maika S D, Richardson J A, Tang J P, Taurog J D. Spontaneous inflammatory disease in transgenic rats expressing HLA-B27 and human beta 2m: an animal model of HLA-B27-associated human disorders. Cell. 1990;63:1099–1112. doi: 10.1016/0092-8674(90)90512-d. [DOI] [PubMed] [Google Scholar]
- 81.Hansson G C. Structural aspects of blood group glycosphingolipids in the gastrointestinal tract. Adv Exp Med Biol. 1988;228:465–494. doi: 10.1007/978-1-4613-1663-3_17. [DOI] [PubMed] [Google Scholar]
- 82.Heidt P J, van der Waaij D, Vossen J M, Hendriks W D H. Recontamination following antibiotic decontamination: restoration of colonization resistance. Microecol Ther. 1981;11:71–82. [Google Scholar]
- 83.Heidt P J, Vossen J M. Experimental and clinical gnotobiotics: influence of the microflora on graft-versus-host disease after allogenic bone marrow transplantation. J Med. 1992;23:161–173. [PubMed] [Google Scholar]
- 84.Helgeland L, Vaage J T, Rolstad B, Midtvedt T, Brandtzaeg P. Microbial colonization influences composition and T-cell receptor Vβ repertoire of intraepithelial lymphocytes in rat intestine. Immunology. 1996;89:494–501. doi: 10.1046/j.1365-2567.1996.d01-783.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Helgeland L, Vaage J T, Rolstad B, Halstensen T S, Midtvedt T, Brandtzaeg P. Regional phenotypic specialization of intraepithelial lymphocytes in the rat intestine does not depend on microbial colonization. Scand J Immunol. 1997;46:349–357. doi: 10.1046/j.1365-3083.1997.d01-133.x. [DOI] [PubMed] [Google Scholar]
- 86.Hermiston M L, Wong M H, Gordon J I. Forced expression of E-cadherin in the mouse intestinal epithelium slows cell migration and provides evidence for non-autonomous regulation of cell fate in a self-renewing system. Genes Dev. 1996;10:985–996. doi: 10.1101/gad.10.8.985. [DOI] [PubMed] [Google Scholar]
- 87.Hill M J. Intestinal flora and endogenous vitamin synthesis. Eur J Cancer Prev. 1997;6:S43–S45. doi: 10.1097/00008469-199703001-00009. [DOI] [PubMed] [Google Scholar]
- 87a.Holgersson J, Strömberg N, Breimer M E. Glycolipids of human large intestine: difference in glycolipid expression related to anatomical localization, epithelial/non-epithelial tissue and the ABO, Le and Se phenotypes of the donors. Biochimie. 1988;70:1565–1574. doi: 10.1016/0300-9084(88)90292-1. [DOI] [PubMed] [Google Scholar]
- 88.Hoskins L C. Bacterial degradation of gastrointestinal mucins. II. Bacterial origin of fecal ABH(O) blood group antigen-destroying enzymes. Gastroenterology. 1968;54:218–224. [PubMed] [Google Scholar]
- 89.Hoskins L C, Augustines M, McKee W B, Boulding E T, Kriaris M, Niedermeyer G. Mucin degradation in human colon ecosystems. Isolation and properties of fecal strains that degrade ABH blood group antigens and oligosaccharides from mucin glycoproteins. J Clin Invest. 1985;75:944–953. doi: 10.1172/JCI111795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Hoskins L C, Boulding E T. Degradation of blood group antigens in human colon ecosystems. I. In vitro production of ABH blood group-destroying enzymes by enteric bacteria. J Clin Invest. 1976;57:63–73. doi: 10.1172/JCI108270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Hoskins L C, Boulding E T. Degradation of blood group antigens in human colon ecosystems. II. A gene interaction in man that affects the fecal population density of certain enteric bacteria. J Clin Invest. 1976;57:74–82. doi: 10.1172/JCI108271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Hoskins L C, Boulding E T. Mucin degradation in human colon ecosystems. Evidence for the existence and role of bacterial subpopulations producing glycosidases as extracellular enzymes. J Clin Invest. 1981;67:163–172. doi: 10.1172/JCI110009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Hoskins L C, Boulding E T, Larson G. Purification and characterization of blood group A-degrading isoforms of α-N-acetylgalactosaminidase from Ruminococcus torques strain IX-70. J Biol Chem. 1997;272:7932–7939. doi: 10.1074/jbc.272.12.7932. [DOI] [PubMed] [Google Scholar]
- 94.Hoskins L C, Zamcheck N. Bacterial degradation of gastrointestinal mucins. I. Comparison of mucus constituents in stools of germfree and conventional rats. Gastroenterology. 1968;54:210–217. [PubMed] [Google Scholar]
- 95.Høverstad T. The normal microflora and short chain fatty acids. In: Grubb R, Midtvedt T, Norin E, editors. The regulatory and protective role of the normal microflora. London, England: Macmillan Press; 1989. pp. 89–108. [Google Scholar]
- 96.Hunter, A. E., A. P. Haynes, and N. H. Russell. 1995. Bone marrow transplantation: current situation, complications and prevention. J. Antimicrob. Chemother. 36(Suppl. B):119–133. [DOI] [PubMed]
- 97.Huseby E, Hellström P M, Midtvedt T. Intestinal microflora stimulates myoelectric activity of rat intestinal wall by promoting cyclic initiation and aboral propagation of migrating myoelectric complexes. Dig Dis Sci. 1994;39:946–956. doi: 10.1007/BF02087542. [DOI] [PubMed] [Google Scholar]
- 98.Ilver D, Arnqvist A, Ögren J, Frick I M, Kersulyte D, Incecik E T, Berg D E, Covacci A, Engstrand L, Borén T. Helicobacter pylori adhesin binding fucosylated histo-blood group antigens revealed by retagging. Science. 1998;279:373–377. doi: 10.1126/science.279.5349.373. [DOI] [PubMed] [Google Scholar]
- 99.Imaoka A, Matsumoto S, Setoyama H, Okada Y, Umesaki Y. Proliferative recruitment of intestinal epithelial lymphocytes after microbial colonization of germ-free mice. Eur J Immunol. 1996;26:945–948. doi: 10.1002/eji.1830260434. [DOI] [PubMed] [Google Scholar]
- 100.Kabir A M A, Aiba Y, Takagi A, Kamiya S, Miwa T, Koga Y. Prevention of Helicobacter pylori infection by lactobacilli in a gnotobiotic murine model. Gut. 1997;41:49–55. doi: 10.1136/gut.41.1.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Kapur R P, Livingston R, Doggett B, Sweetser D A, Siebert J R, Palmiter R D. Abnormal microenvironmental signals underlie intestinal agangliosis in Dominant megacolon mutant mice. Dev Biol. 1996;174:360–369. doi: 10.1006/dbio.1996.0080. [DOI] [PubMed] [Google Scholar]
- 102.Karlsson F A, Burman P, Lööf L, Mårdh S. Major parietal cell antigen in autoimmune gastritis with pernicious anemia is the acid-producing H+,K+-adenosine triphosphatase of the stomach. J Clin Invest. 1988;81:475–479. doi: 10.1172/JCI113344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Karlsson K A. Animal glycosphingolipids as membrane attachment sites for bacteria. Annu Rev Biochem. 1989;58:309–350. doi: 10.1146/annurev.bi.58.070189.001521. [DOI] [PubMed] [Google Scholar]
- 104.Kautiainen A, Midtvedt T, Törnqvist M. Intestinal bacteria and endogenous production of malonaldehyde and alkylators in mice. Carcinogenesis. 1993;14:2633–2636. doi: 10.1093/carcin/14.12.2633. [DOI] [PubMed] [Google Scholar]
- 105.Kenny B, DeVinney R, Stein M, Reinscheid D J, Frey E A, Finlay B B. Enteropathogenic E. coli transfers its receptor for intimate adherence into mammalian cells. Cell. 1997;91:511–520. doi: 10.1016/s0092-8674(00)80437-7. [DOI] [PubMed] [Google Scholar]
- 106.Kernéis S, Bogdanova A, Kraehenbuhl J P, Prignault E. Conversion by Peyer’s patch lymphocytes of human enterocytes into M cells that transport bacteria. Science. 1997;277:949–952. doi: 10.1126/science.277.5328.949. [DOI] [PubMed] [Google Scholar]
- 107.Kinzler K W, Vogelstein B. Lessons from hereditary colorectal cancer. Cell. 1996;87:159–170. doi: 10.1016/s0092-8674(00)81333-1. [DOI] [PubMed] [Google Scholar]
- 108.Kirschner D E, Blaser M J. The dynamics of Helicobacter pylori infection of the human stomach. J Theor Biol. 1995;176:281–290. doi: 10.1006/jtbi.1995.0198. [DOI] [PubMed] [Google Scholar]
- 109.Kohashi O, Kuwata J, Umehara K, Umeura F, Takahashi T, Ozawa A. Susceptibility to adjuvant-induced arthritis among germ-free, specific-pathogen-free, and conventional rats. Infect Immun. 1979;26:791–794. doi: 10.1128/iai.26.3.791-794.1979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Kohashi O, Kohashi Y, Takahashi T, Ozawa A, Shigematsu N. Suppressive effect of Escherichia coli on adjuvant-induced arthritis in germ free rats. Arthritis Rheum. 1986;29:547–553. doi: 10.1002/art.1780290413. [DOI] [PubMed] [Google Scholar]
- 111.Komano H, Fujiura Y, Kawaguchi M, Matsumoto S, Hashimoto Y, Obana S, Mombaerts P, Tonegawa S, Yamamoto H, Itohara S, Nanno M, Ishikawa H. Homeostatic regulation of intestinal epithelia by intraepithelial gamma delta T cells. Proc Natl Acad Sci USA. 1995;92:6147–6151. doi: 10.1073/pnas.92.13.6147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Kosloske A M. Epidemiology of necrotizing enterocolitis. Acta Pediatr Suppl. 1994;396:S2–S7. doi: 10.1111/j.1651-2227.1994.tb13232.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Krause A, Kamradt T, Burmester G R. Potential infectious agents in the induction of arthritides. Curr Opin Rheumatol. 1996;8:203–209. doi: 10.1097/00002281-199605000-00007. [DOI] [PubMed] [Google Scholar]
- 114.Kühn R, Löhler J, Rennick D, Rajewski K, Müller W. Interleukin-10-deficient mice develop chronic enterocolitis. Cell. 1993;75:263–274. doi: 10.1016/0092-8674(93)80068-p. [DOI] [PubMed] [Google Scholar]
- 115.Kuipers E J, Appelmelk B J. Helicobacter pylori and atrophic gastritis. Biomed Pharmacother. 1997;51:150–155. doi: 10.1016/s0753-3322(97)85582-5. [DOI] [PubMed] [Google Scholar]
- 116.Kukowska-Latallo J F, Larsen R D, Nair R P, Lowe J B. A cloned human cDNA determines expression of a mouse stage-specific embryonic antigen and Lewis blood group α(1,3/1,4) fucosyltransferase. Genes Dev. 1990;4:1288–1303. doi: 10.1101/gad.4.8.1288. [DOI] [PubMed] [Google Scholar]
- 117.Larson G, Falk P, Hoskins L C. Degradation of human intestinal glycosphingolipids by extracellular glycosidases from mucin-degrading bacteria of the human fecal flora. J Biol Chem. 1988;263:10790–10798. [PubMed] [Google Scholar]
- 118.Larson G, Falk P, Hynsjö L, Midtvedt A C, Midtvedt T. Fecal excretion of glycosphingolipids of breast-fed and formula-fed infants. Microb Ecol Health Dis. 1990;3:305–319. [Google Scholar]
- 119.LeFrock J, Ellis C, Weinstein L. The impact of hospitalization on the aerobic fecal microflora. J Med Sci. 1979;277:269–274. doi: 10.1097/00000441-197905000-00004. [DOI] [PubMed] [Google Scholar]
- 120.Li Y Q, Roberts S A, Paulus A, Loeffler M, Potten C S. The crypt cycle in mouse small intestinal epithelium. J Cell Sci. 1994;107:3271–3279. doi: 10.1242/jcs.107.12.3271. [DOI] [PubMed] [Google Scholar]
- 121.Lindstedt G, Lindstedt S, Gustafsson B G. Mucus in intestinal contents of germfree rats. J Exp Med. 1965;121:201–213. doi: 10.1084/jem.121.2.201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Loeffler M, Bratke T, Paulus U, Li Y Q, Potten C S. Clonality and life cycles of intestinal crypts explained by a state dependent stochastic model of epithelial stem cell organization. J Theor Biol. 1997;186:41–54. doi: 10.1006/jtbi.1996.0340. [DOI] [PubMed] [Google Scholar]
- 123.Lyerly D M, Krivan H C, Wilkins T D. Clostridium difficile: its disease and toxins. Clin Microbiol Rev. 1988;1:1–18. doi: 10.1128/cmr.1.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Macfarlane G T, Hay S, Gibson G R. Influence of mucin on glycosidase, protease and arylamidase activities of human gut bacteria grown in a 3-stage continuous culture system. J Appl Bacteriol. 1989;66:407–417. doi: 10.1111/j.1365-2672.1989.tb05110.x. [DOI] [PubMed] [Google Scholar]
- 125.Mandel U, White T, Karkov J, Hakomori S, Clausen H, Dabelsteen E. Expression of histo-blood group ABO gene defined glycosyltransferases in epithelial tissues. J Oral Pathol Med. 1990;19:251–256. doi: 10.1111/j.1600-0714.1990.tb00836.x. [DOI] [PubMed] [Google Scholar]
- 126.Marchetti M, Arico B, Burroni D, Figura N, Rappuoli R, Ghiara P. Development of a mouse model for Helicobacter pylori infection that mimics human disease. Science. 1995;267:1655–1658. doi: 10.1126/science.7886456. [DOI] [PubMed] [Google Scholar]
- 127.Martin S L, Edbrooke M R, Hodgman T C, van den Eijnden, Bird M I. Lewis x biosynthesis in Helicobacter pylori—molecular cloning of an α-1,3-fucosyltransferase gene. J Biol Chem. 1997;272:21349–21356. doi: 10.1074/jbc.272.34.21349. [DOI] [PubMed] [Google Scholar]
- 128.McCartney A L, Wenzhi W, Tannock G W. Molecular analysis of the composition of the bifidobacterial and lactobacillus microflora of humans. Appl Environ Microbiol. 1996;62:4608–4613. doi: 10.1128/aem.62.12.4608-4613.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Metchnikoff E. Études sur la flore intestinale. Ann Inst Pasteur Paris. 1908;22:929–955. [Google Scholar]
- 130.Metchnikoff E. Études sur la flore intestinale—Deuxième mémoire. Ann Inst Pasteur Paris. 1910;24:755–770. [Google Scholar]
- 131.Midtvedt A C, Carlstedt-Duke B, Norin E, Saxerholt H, Midtvedt T. Development of five metabolic activities associated with the intestinal microflora of healthy infants. J Pediatr Gastroenterol Nutr. 1988;7:559–567. doi: 10.1097/00005176-198807000-00014. [DOI] [PubMed] [Google Scholar]
- 132.Midtvedt T. Microbial bile acid transformation. Am J Clin Nutr. 1974;27:1341–1347. doi: 10.1093/ajcn/27.11.1341. [DOI] [PubMed] [Google Scholar]
- 133.Midtvedt T. Intestinal microflora-associated characteristics. Microecol Ther. 1986;16:121–130. [Google Scholar]
- 134.Midtvedt T. Intestinal bacteria and rheumatoid disease. Scand J Rheumatol. 1987;64:49–54. doi: 10.3109/03009748709096721. [DOI] [PubMed] [Google Scholar]
- 135.Midtvedt T. Germfree animals and carcinogenesis. Biosci Microflora. 1997;16:9–12. [Google Scholar]
- 136.Midtvedt T, Carlstedt-Duke B, Höverstad T, Lingaas E, Norin K E, Saxerholt H, Steinbakk M. Influence of peroral antibiotics upon the biotransformatory activity of the intestinal microflora in healthy subjects. Eur J Clin Invest. 1986;16:11–17. doi: 10.1111/j.1365-2362.1986.tb01300.x. [DOI] [PubMed] [Google Scholar]
- 137.Midtvedt T, Carlstedt-Duke B, Höverstad T, Midtvedt A C, Norin K E, Saxerholt H. Establishment of a biochemically active intestinal ecosystem in ex-germfree rats. Appl Environ Microbiol. 1987;53:2866–2871. doi: 10.1128/aem.53.12.2866-2871.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Midtvedt T, Gustafsson B E. Microbial conversion of bilirubin to urobilins in vitro and in vivo. Acta Pathol Microbiol Scand Sect B. 1981;89:57–60. doi: 10.1111/j.1699-0463.1981.tb00152_89b.x. [DOI] [PubMed] [Google Scholar]
- 139.Miller R S, Hoskins L C. Mucin degradation in human colon ecosystems. Fecal population densities of mucin-degrading bacteria estimated by “most probable number” method. Gastroenterology. 1981;81:759–765. [PubMed] [Google Scholar]
- 140.Möller L, Zeisig M, Midtvedt T, Gustafsson J Å. Intestinal microflora enhances formation of DNA adducts following administration of 2-NF and 2-AAF. Carcinogenesis. 1994;15:857–861. doi: 10.1093/carcin/15.5.857. [DOI] [PubMed] [Google Scholar]
- 141.Mombaerts P, Mizoguchi E, Grusby M J, Glimcher L H, Bhan A K, Tonegawa S. Spontaneous development of inflammatory bowel disease in T cell receptor mutant mice. Cell. 1993;75:275–282. doi: 10.1016/0092-8674(93)80069-q. [DOI] [PubMed] [Google Scholar]
- 141a.Monteiro M A, Chan K H, Rasko D A, Taylor D E, Zheng P Y, Appelmelk B J, Wirth H P, Yang M, Blaser M J, Hynes S O, Moran A P, Perry M B. Simultaneous expression of type 1 and type 2 Lewis blood group antigens by Helicobacter pylori lipopolysaccharides. Molecular mimicry between H. pylori lipopolysaccharides and human gastric epithelial cell surface glycoforms. J Biol Chem. 1998;273:11533–11543. doi: 10.1074/jbc.273.19.11533. [DOI] [PubMed] [Google Scholar]
- 142.Moore W E C, Holdeman L V. Human fecal flora: the normal flora of 20 Japanese-Hawaiians. Appl Microbiol. 1974;27:961–979. doi: 10.1128/am.27.5.961-979.1974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Moran, A. P. 1996. The role of lipopolysaccharide in Helicobacter pylori pathogenesis. Aliment. Pharmacol. Ther. 10(Suppl. 1):39–50. [DOI] [PubMed]
- 144.Negrini R, Lisato L, Zanella I, Cavazzini L, Guillini S, Villanacci V, Poiesi C, Albertini A, Ghielmi S. Helicobacter pylori infection induces antibodies cross-reacting with human gastric mucosa. Gastroenterology. 1991;101:437–445. doi: 10.1016/0016-5085(91)90023-e. [DOI] [PubMed] [Google Scholar]
- 145.Neu H C. The crisis of antibiotic resistance. Science. 1992;257:1064–1073. doi: 10.1126/science.257.5073.1064. [DOI] [PubMed] [Google Scholar]
- 146.Neut C, Bezirtzoglou E, Romond C, Beerens H, Delcroix M, Noel A M. Bacterial colonization of the large intestine in newborns delivered by caesarian section. Zentbl Bakteriol Mikrobiol Hyg Ser A. 1987;266:330–337. doi: 10.1016/s0176-6724(87)80213-4. [DOI] [PubMed] [Google Scholar]
- 147.NIH Consensus Conference. Helicobacter pylori in peptic ulcer disease. JAMA. 1994;272:63–69. [PubMed] [Google Scholar]
- 148.Nuttal G H F, Thierfelder H. /1896. Thieresches Leben ohne Bakterien im Verdauungskanal. Z Physiol Chem. 1895;21:109–121. [Google Scholar]
- 149.Obama H, Kuname T, Sudo A, Yanagida T, Ikematsu S, Ozawa M, Yoshida H, Kannagi R, Yamamura K I, Muramatsu T. A transgenic mouse line with α-1,3/4-fucosyltransferase cDNA: production and characteristics. Glycoconj J. 1995;12:795–801. doi: 10.1007/BF00731241. [DOI] [PubMed] [Google Scholar]
- 150.O’Connor T M. Cell dynamics in the intestine of the mouse from late fetal life to maturity. Am J Anat. 1996;118:525–536. doi: 10.1002/aja.1001180212. [DOI] [PubMed] [Google Scholar]
- 150a.Ogata H, Inoue N, Podolsky D K. Identification of a goblet cell-specific enhancer element in the rat intestinal trefoil factor gene promoter bound by a goblet cell nuclear protien. J Biol Chem. 1998;273:3060–3067. doi: 10.1074/jbc.273.5.3060. [DOI] [PubMed] [Google Scholar]
- 151.Örskov F, Biering-Sörensen K. Escherichia coli serogroups in breast fed and bottle fed infants. Acta Pathol Microbiol Scand Sect B. 1975;83:25–30. [PubMed] [Google Scholar]
- 152.Ouellette A J, Selsted M E. Paneth cell defensins: endogenous peptide components of intestinal host defense. FASEB J. 1996;10:1280–1289. doi: 10.1096/fasebj.10.11.8836041. [DOI] [PubMed] [Google Scholar]
- 152a.Pace N R. New perspective on the natural microbial world: molecular microbial ecology. ASM News. 1996;62:463–470. [Google Scholar]
- 153.Park H S, Goodlad R A, Wright N A. Crypt fission in the small intestine and colon. A mechanism for the emergence of G6PD locus-mutated crypts after treatment with mutagens. Am J Pathol. 1995;147:1416–1427. [PMC free article] [PubMed] [Google Scholar]
- 154.Pendergast J K, McGuigan L E, Geczy A F, Kwong Y D L, Edmonds J P. Persistence of HLA-B27 cross reactive bacteria in the bowel flora of patients with ankylosing spondylitis. Infect Immun. 1984;46:686–689. doi: 10.1128/iai.46.3.686-689.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Podolsky D K. Inflammatory bowel disease (1) N Engl J Med. 1991;325:928–937. doi: 10.1056/NEJM199109263251306. [DOI] [PubMed] [Google Scholar]
- 156.Podolsky D K. Inflammatory bowel disease (2) N Engl J Med. 1991;325:1008–1016. doi: 10.1056/NEJM199110033251406. [DOI] [PubMed] [Google Scholar]
- 156a.Podolsky D K. Oligosaccharide structures of isolated human colonic mucin species. J Biol Chem. 1985;260:15510–15515. [PubMed] [Google Scholar]
- 157.Potten C S. The significance of spontaneous and induced apoptosis in the gastrointestinal tract of mice. Cancer Metast Rev. 1992;11:179–195. doi: 10.1007/BF00048063. [DOI] [PubMed] [Google Scholar]
- 158.Potten C S, Kellet M, Roberts S, Rew D, Wilson G. The in vivo measurement of proliferation in normal human colorectal mucosa using bromodeoxyuridine. Gut. 1992;33:71–78. doi: 10.1136/gut.33.1.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Potten C S, Loeffler M. Stem cells: attributes, cycles, spirals, pitfalls and uncertainties. Lessons for and from the crypt. Development. 1990;110:1001–1020. doi: 10.1242/dev.110.4.1001. [DOI] [PubMed] [Google Scholar]
- 160.Prieto P A, Mukerji P, Kelder B, Erney R, Gonzales D, Yun J S, Smith D F, Moremen K W, Nardelli C, Pierce M, Li Y, Chen X, Wagner T E, Cummings R D, Kopchick J J. Remodeling of mouse milk glycoconjugates by transgenic expression of a human glycosyltransferase. J Biol Chem. 1995;270:29515–29519. doi: 10.1074/jbc.270.49.29515. [DOI] [PubMed] [Google Scholar]
- 161.Robertson K, Mason I, Hall S. Hirschsprung’s disease: genetic mutations in mice and men. Gut. 1997;41:436–441. doi: 10.1136/gut.41.4.436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Roth K A, Hertz J W, Gordon J I. Mapping enteroendocrine cell populations in transgenic mice reveals an unexpected degree of complexity in cellular differentiation within the gastrointestinal tract. J Cell Biol. 1990;110:1791–1801. doi: 10.1083/jcb.110.5.1791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Rotimi V O, Duerden B I. The development of the bacterial flora in normal neonates. J Med Microbiol. 1981;14:51–62. doi: 10.1099/00222615-14-1-51. [DOI] [PubMed] [Google Scholar]
- 164.Sadlack B, Merz H, Schorle H, Schimpl A, Feller A C, Horak I. Ulcerative colitis-like disease in mice with a disrupted interleukin-2 gene. Cell. 1993;75:253–261. doi: 10.1016/0092-8674(93)80067-o. [DOI] [PubMed] [Google Scholar]
- 165.Sadzikowski M R, Sperry J F, Wilkins T D. Cholesterol reducing bacterium from human feces. Appl Environ Microbiol. 1977;34:355–362. doi: 10.1128/aem.34.4.355-362.1977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Sakamoto J, Watanabe T, Tokumaru T, Tagaki H, Nakazato H, Lloyd K O. Expression of Lewisa, Lewisb, Lewisx, Lewisy, sialyl-Lewisa and sialyl-Lewisx blood group antigens in human gastric adenocarcinoma and in normal gastric tissue. Cancer Res. 1989;49:745–752. [PubMed] [Google Scholar]
- 167.Salmond G P C. Pili, peptidases and protein secretion: curious connections. Trends Microbiol. 1996;4:474–476. doi: 10.1016/s0966-842x(97)82907-1. [DOI] [PubMed] [Google Scholar]
- 168.Salyers A A, West S E H, Vercelotti J R, Wilkins T D. Fermentation of mucins and plant polysaccharides by anaerobic bacteria from the human colon. Appl Environ Microbiol. 1977;34:529–533. doi: 10.1128/aem.34.5.529-533.1977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Salyers A A, Pajeau M. Competitiveness of different polysaccharide utilization mutants of Bacteroides thetaiotaomicron in the intestinal tracts of germ-free mice. Appl Environ Microbiol. 1989;55:2572–2578. doi: 10.1128/aem.55.10.2572-2578.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Sartor R B. Microbial factors in Crohn’s disease, ulcerative colitis, and experimental intestinal inflammation. In: Kirstner J B, Shorter R G, editors. Inflammatory bowel disease. 4th ed. Baltimore, Md: The Williams & Wilkins Co.; 1995. pp. 96–124. [Google Scholar]
- 171.Savage D C. Microbial ecology of the gastrointestinal tract. Annu Rev Microbiol. 1977;31:107–133. doi: 10.1146/annurev.mi.31.100177.000543. [DOI] [PubMed] [Google Scholar]
- 172.Savidge T C. The life and times of an intestinal M cell. Trends Microbiol. 1996;4:301–306. doi: 10.1016/0966-842x(96)10052-4. [DOI] [PubMed] [Google Scholar]
- 173.Savidge T C, Smith M W, James P S, Aldred P. Salmonella-induced M-cell formation in germ-free mouse Peyer’s patch tissue. Am J Pathol. 1991;139:177–184. [PMC free article] [PubMed] [Google Scholar]
- 174.Schmidt G H, Wilkinson M M, Ponder B A J. Cell migration pathway in the intestinal epithelium: an in situ marker system using mouse aggregation chimeras. Cell. 1985;40:425–429. doi: 10.1016/0092-8674(85)90156-4. [DOI] [PubMed] [Google Scholar]
- 175.Schmidt G H, Winton D J, Ponder B A J. Development of the pattern of cell renewal in the crypt-villus unit of chimeric mouse intestine. Development. 1988;103:785–790. doi: 10.1242/dev.103.4.785. [DOI] [PubMed] [Google Scholar]
- 176.Schottelius M. Die Bedeutung der Darmbakterien für die Ehrnährung. II. Arch Hyg. 1902;42:48–70. [Google Scholar]
- 177.Schwan A, Sjölin S, Trottestam U, Aronsson B. Relapsing Clostridium difficile colitis cured by rectal infusion of normal faeces. Scand J Infect Dis. 1984;16:211–215. doi: 10.3109/00365548409087145. [DOI] [PubMed] [Google Scholar]
- 178.Seal D V, Boriello S P, Barclay F, Welch A, Piper M, Bonnycastle M. Treatment of relapsing Clostridium difficile diarrhoea by administration of a non-toxigenic strain. Eur J Clin Microbiol. 1987;6:51–53. doi: 10.1007/BF02097191. [DOI] [PubMed] [Google Scholar]
- 179.Segal E D, Lange C, Covacci A, Tompkins L S, Falkow S. Induction of host signal transduction pathways by Helicobacter pylori. Proc Natl Acad Sci USA. 1997;94:7595–7599. doi: 10.1073/pnas.94.14.7595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Sharma A, Okabe J, Birch P, McLellan S B, Martin M J, Platt J L, Logan J S. Reduction in the level of Gal(α1,3)Gal in transgenic mice and pigs by the expression of an α(1,2) fucosyltransferase. Proc Natl Acad Sci USA. 1996;93:7190–7195. doi: 10.1073/pnas.93.14.7190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Shindler K S, Roth K A. Double immunofluorescent staining using two unconjugated primary antisera raised in the same species. J Histochem Cytochem. 1996;44:1331–1335. doi: 10.1177/44.11.8918908. [DOI] [PubMed] [Google Scholar]
- 182.Shroff K E, Meslin K, Cebra J J. Commensal enteric bacteria engender a self-limiting humoral mucosal immune response while permanently colonizing the gut. Infect Immun. 1995;63:3904–3913. doi: 10.1128/iai.63.10.3904-3913.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Simon T C, Cho A, Tso P, Gordon J I. Suppressor and activator functions mediated by a repeated heptad sequence in the liver fatty acid binding protein gene (Fabpl): effects on renal, small intestinal and colonic gene expression in transgenic mice. J Biol Chem. 1997;272:10652–10663. doi: 10.1074/jbc.272.16.10652. [DOI] [PubMed] [Google Scholar]
- 184.Simon T C, Roberts L J J, Gordon J I. A 20 nucleotide element in the intestinal fatty acid binding protein gene modulates its cell lineage-specific, differentiation-dependent, and cephalocaudal patterns of expression in transgenic mice. Proc Natl Acad Sci USA. 1995;92:8685–8689. doi: 10.1073/pnas.92.19.8685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Simon T C, Roth K A, Gordon J I. Use of transgenic mice to map cis-gut elements in the liver fatty acid-binding protein gene (Fabpl) that regulate its cell lineage-specific, differentiation-dependent, and spatial patterns of expression in the intestinal epithelium and in the liver acinus. J Biol Chem. 1993;268:18345–18358. [PubMed] [Google Scholar]
- 186.Smith H W, Crabb W E. The faecal bacterial flora of animals and man: its development in the young. J Pathol Bacteriol. 1961;82:53–66. [Google Scholar]
- 187.Stark P L, Lee A. The microbial ecology of the large bowel of breast-fed and formula-fed infants during the first year of life. J Med Microbiol. 1982;15:189–203. doi: 10.1099/00222615-15-2-189. [DOI] [PubMed] [Google Scholar]
- 188.Strandberg K, Sedvall G, Midtvedt T, Gustafsson B E. Effect of some biologically active amines on the cecum wall of germ-free rats. Proc Soc Exp Biol Med. 1966;121:699–702. doi: 10.3181/00379727-121-30864. [DOI] [PubMed] [Google Scholar]
- 189.Su L K, Kinzler K W, Vogelstein B, Preisinger A C, Moser A R, Luongo C, Gould K A, Dove W F. Multiple intestinal neoplasia caused by a mutation in the murine homolog of the APC gene. Science. 1992;256:668–670. doi: 10.1126/science.1350108. [DOI] [PubMed] [Google Scholar]
- 190.Tannock G W. The normal microflora: new concepts in health promotion. Microbiol Sci. 1988;5:4–8. [PubMed] [Google Scholar]
- 191.Taurog J D, Richardson J A, Croft J T, Simmons W A, Zhou M, Fernandez-Sueiro J L, Balish E, Hammer R E. The germfree state prevents development of gut and joint inflammatory disease in HLA-B27 transgenic rats. J Exp Med. 1994;180:2359–2364. doi: 10.1084/jem.180.6.2359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Telford J L, Ghiara P, Dell’Orco M, Comanducci M, Burroni D, Bugnoli M, Tecce M F, Censini S, Covacci A, Xiang Z, Papini E, Montecucco C, Parente L, Rappuoli R. Gene structure of the Helicobacter pylori cytotoxin and evidence of its key role in gastric disease. J Exp Med. 1994;179:1653–1658. doi: 10.1084/jem.179.5.1653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Tomb J F, White O, Kerlavage A R, Clayton R A, Sutton G G, Fleischmann R D, Ketchum K A, Klenk H P, Gill G, Dougherty G A, Nelson K, Quackenbush J, Zhou L, Kirkness E F, Peterson S, Loftus B, Richardson D, Dodson R, Khalak H G, Glodek A, McKenney K, Fitzegerald L M, Lee N, Adams M D, Hickey D K, Berg D E, Gocayne J D, Utterback T R, Peterson J D, Kelley J M, Cotton M D, Weidman J M, Fujii C, Bowman C, Watthey L, Wallin E, Hayes W S, Borodovsky M, Karp P D, Smith H D, Fraser C M, Venter J C. The complete genome sequence of the gastric pathogen Helicobacter pylori. Nature. 1997;388:539–547. doi: 10.1038/41483. [DOI] [PubMed] [Google Scholar]
- 194.Totafurno J, Bjerknes M, Cheng H. The crypt cycle: crypt and villus production in the adult intestinal epithelium. Biophys J. 1987;52:279–294. doi: 10.1016/S0006-3495(87)83215-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Trier J S, Moxey P C. Morphogenesis of the small intestine during fetal development. Ciba Found Symp. 1979;70:3–29. doi: 10.1002/9780470720530.ch2. [DOI] [PubMed] [Google Scholar]
- 196.Tummuru M K, Cover T L, Blaser M J. Mutation of the cytotoxin-associated cagA gene does not affect the vacuolating cytotoxin activity of Helicobacter pylori. Infect Immun. 1994;62:2609–2613. doi: 10.1128/iai.62.6.2609-2613.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Umesaki Y, Sakata T, Yajima T. Abrupt induction of GDP-fucose:asialo GM1 fucosyltransferase in the small intestine after conventionalization of germ-free mice. Biochem Biophys Res Commun. 1982;105:439–443. doi: 10.1016/0006-291x(82)91453-x. [DOI] [PubMed] [Google Scholar]
- 198.Umesaki Y, Setoyama H, Matsumoto S, Okada Y. Expansion of aβ T-cell receptor-bearing intestinal intraepithelial lymphocytes after microbial colonization in germ-free mice and its independence from thymus. Immunology. 1993;79:32–37. [PMC free article] [PubMed] [Google Scholar]
- 199.Umesaki Y, Okada Y, Matsumoto S, Imaoka A, Setoyama H. Segmented filamentous bacteria are indigenous intestinal bacteria that activate intraepithelial lymphocytes and induce MHC class II molecules and fucosyl GM1 glycolipids on the small intestinal epithelial cell in the ex-germ-free mouse. Microbiol Immunol. 1995;34:555–562. doi: 10.1111/j.1348-0421.1995.tb02242.x. [DOI] [PubMed] [Google Scholar]
- 200.Valdivia, R. H., and S. Falkow. 1997. Fluorescence-based isolation of bacterial genes expressed within host cells. Science 2007–2011. [DOI] [PubMed]
- 201.van der Waaij D. The ecology of the human intestine and its consequences for overgrowth by pathogens such as Clostridium difficile. Annu Rev Microbiol. 1989;43:69–87. doi: 10.1146/annurev.mi.43.100189.000441. [DOI] [PubMed] [Google Scholar]
- 202.van der Waaij D, van der Waaij B D. The colonization resistance of the digestive tract in different animal species and in man: a comparative study. Epidemiol Infect. 1990;105:237–243. doi: 10.1017/s0950268800047841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Varki A. Biological roles of oligosaccharides. All the theories are correct. Glycobiology. 1993;3:97–130. doi: 10.1093/glycob/3.2.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Vossen J M, Heidt P J, van den Berg H, Gerritsen E J, Hermans J, Dooren L J. Prevention of infection and graft-versus-host disease by suppression of intestinal microflora in children treated with allogeneic bone marrow transplantation. Eur J Clin Microbiol Infect Dis. 1990;9:14–23. doi: 10.1007/BF01969527. [DOI] [PubMed] [Google Scholar]
- 205.Webb P M, Forman D. Helicobacter pylori as a risk factor for cancer. Baillière’s Clin Gastroenterol. 1995;9:563–582. doi: 10.1016/0950-3528(95)90049-7. [DOI] [PubMed] [Google Scholar]
- 206.Winton D J, Blount M A, Ponder B A J. A clonal marker induced by mutation in mouse intestinal epithelium. Nature. 1988;333:463–466. doi: 10.1038/333463a0. [DOI] [PubMed] [Google Scholar]
- 207.Winton D J, Ponder B A J. Stem cell organization in mouse small intestine. Proc R Soc Lond Ser B. 1990;241:13–18. doi: 10.1098/rspb.1990.0059. [DOI] [PubMed] [Google Scholar]
- 208.Wirth H P, Yang M, Peek R M, Jr, Tham K T, Blaser M J. Helicobacter pylori Lewis expression is related to the host Lewis phenotype. Gastroenterology. 1997;113:1091–1098. doi: 10.1053/gast.1997.v113.pm9322503. [DOI] [PubMed] [Google Scholar]
- 209.Wold A E, Caugant D A, Lidin-Jansson G, de Man P, Svanborg C. Resident colonic E. coli strains frequently display uropathogenic characteristics. J Infect Dis. 1992;165:46–52. doi: 10.1093/infdis/165.1.46. [DOI] [PubMed] [Google Scholar]
- 210.Wong M H, Hermiston M L, Syder A J, Gordon J I. Forced overexpression of the tumor suppressor adenomatous polyposis coli protein induces disordered cell migration in the intestinal epithelium. Proc Natl Acad Sci USA. 1996;93:9588–9593. doi: 10.1073/pnas.93.18.9588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Wright N A, Alison M. The biology of epithelial cell populations. Oxford, England: Clarendon Press; 1984. The control of cell proliferation in the gastrointestinal tract; pp. 843–869. [Google Scholar]
- 212.Wright N A, Irwin M. The kinetics of villus cell populations in the mouse small intestine: normal villi—the steady state requirement. Cell Tissue Kinet. 1982;15:595–609. doi: 10.1111/j.1365-2184.1982.tb01066.x. [DOI] [PubMed] [Google Scholar]
- 213.Xiang Z, Censini S, Bayeli P F, Telford J L, Figura N, Rappuoli R, Covacci A. Analysis of expression of cagA and vacA virulence factors in 43 strains of Helicobacter pylori reveals that clinical isolates can be divided into two major types and that cagA is not necessary for expression of the vacuolating cytotoxin. Infect Immun. 1995;63:94–98. doi: 10.1128/iai.63.1.94-98.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Yamamoto F, Clausen H, White T, Marken J, Hakomori S. Molecular genetic basis for histo-blood group ABO system. Nature. 1990;345:229–233. doi: 10.1038/345229a0. [DOI] [PubMed] [Google Scholar]