bone (original) (raw)
Bone is a connective tissue consisting of three types of cell that contribute to bone homeostasis. These are bone-building osteoblasts, stationary osteocytes (mature bone cells), and bone-destroying osteoclasts, embedded in a mineralized matrix infused with spaces and canals. An equilibrium between osteoblasts and osteoclasts maintains bone tissue.
There are two types of bone tissue: compact and spongy. As the names imply, these types of differ in density, or how tightly the tissue is packed together.
Compact bone
 |
|---|
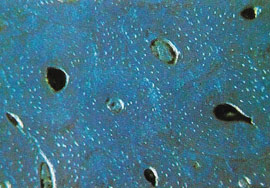
| This cross-section through the compact bone tissue of a long bone shows the concentric layers of several Haversian canal systems. At the center of each is a blood vessel surrounded by bone-forming cells. |
Compact bone is bone that consists of closely packed osteons or haversian systems. The osteon consists of a central canal called the osteonic (haversian) canal, which is surrounded by concentric rings (lamellae) of matrix. Between the rings of matrix, the bone cells (osteocytes) are located in spaces called lacunae. Small channels (canaliculi) radiate from the lacunae to the osteonic (haversian) canal to provide passageways through the hard matrix. In compact bone, the haversian systems are packed tightly together to form what appears to be a solid mass. The osteonic canals contain blood vessels that are parallel to the long axis of the bone. These blood vessels interconnect, by way of perforating canals, with vessels on the surface of the bone.
Spongy (cancellous) bone
Spongy bone is bone that is lighter and less dense than compact bone. Spongy bone consists of plates (trabeculae) and bars of bone adjacent to small, irregular cavities that contain red bone marrow. The canaliculi connect to the adjacent cavities, instead of a central haversian canal, to receive their blood supply. It may appear that the trabeculae are arranged in a haphazard manner, but in fact they are organized to provide maximum strength similar to braces that are used to support a building. The trabeculae of spongy bone follow the lines of stress and can realign if the direction of stress changes.
Bone formation
The terms osteogenesis and ossification are often used synonymously to indicate the process of bone formation. Parts of the skeleton form during the first few weeks after conception. By the end of the eighth week after conception, the skeletal pattern is formed in cartilage and connective tissue membranes and ossification begins.
Bone development continues throughout adulthood. Even after adult stature is attained, bone development continues for repair of fractures and for remodeling to meet changing lifestyles. Osteoblasts, osteocytes and osteoclasts are the three cell types involved in the development, growth and remodeling of bones. Osteoblasts are bone-forming cells, osteocytes are mature bone cells, and osteoclasts break down and reabsorb bone.
There are two types of ossification: intramembranous and endochondral.
Intramembranous
Intramembranous ossification involves the replacement of sheet-like connective tissue membranes with bony tissue. Bones formed in this manner are called intramembranous bones. They include certain flat bones of the skull and some of the irregular bones. The future bones are first formed as connective tissue membranes. Osteoblasts migrate to the membranes and deposit bony matrix around themselves. When the osteoblasts are surrounded by matrix they are called osteocytes.
Endochondral ossification
Endochondral ossification involves the replacement of hyaline cartilage with bony tissue. Most of the bones of the skeleton are formed in this manner. These bones are called endochondral bones. In this process, the future bones are first formed as hyaline cartilage models. During the third month after conception, the perichondrium that surrounds the hyaline cartilage "models" becomes infiltrated with blood vessels and osteoblasts and changes into a periosteum. The osteoblasts form a collar of compact bone around the diaphysis. At the same time, the cartilage in the center of the diaphysis begins to disintegrate. Osteoblasts penetrate the disintegrating cartilage and replace it with spongy bone. This forms a primary ossification center. Ossification continues from this center toward the ends of the bones. After spongy bone is formed in the diaphysis, osteoclasts break down the newly formed bone to open up the medullary cavity.
The cartilage in the epiphyses continues to grow so the developing bone increases in length. Later, usually after birth, secondary ossification centers form in the epiphyses. Ossification in the epiphyses is similar to that in the diaphysis except that the spongy bone is retained instead of being broken down to form a medullary cavity. When secondary ossification is complete, the hyaline cartilage is totally replaced by bone except in two areas. A region of hyaline cartilage remains over the surface of the epiphysis as the articular cartilage and another area of cartilage remains between the epiphysis and diaphysis. This is the epiphyseal plate or growth plate.
Bone growth
Bones grow in length at the epiphyseal plate by a process that is similar to endochondral ossification. The cartilage in the region of the epiphyseal plate next to the epiphysis continues to grow by mitosis. The chondrocytes, in the region next to the diaphysis, age and degenerate. Osteoblasts move in and ossify the matrix to form bone. This process continues throughout childhood and the adolescent years until the cartilage growth slows and finally stops. When cartilage growth ceases, usually in the early twenties, the epiphyseal plate completely ossifies so that only a thin epiphyseal line remains and the bones can no longer grow in length. Bone growth is under the influence of growth hormone (GH) from the anterior pituitary gland and sex hormones from the ovaries and testes.
Even though bones stop growing in length in early adulthood, they can continue to increase in thickness or diameter throughout life in response to stress from increased muscle activity or to weight. The increase in diameter is called appositional growth. Osteoblasts in the periosteum form compact bone around the external bone surface. At the same time, osteoclasts in the endosteum break down bone on the internal bone surface, around the medullary cavity. These two processes together increase the diameter of the bone and, at the same time, keep the bone from becoming excessively heavy and bulky.
Classification of bones
All bones have surface markings and characteristics that make a specific bone unique. There are holes, depressions, smooth facets, lines, projections and other markings. These usually represent passageways for vessels and nerves, points of articulation with other bones or points of attachment for tendons and ligaments.
The bones of the body come in a variety of sizes and shapes. The four principal types of bones are long, short, flat and irregular.
Long bones
Bones that are longer than they are wide are called long bones. They consist of a long shaft with two bulky ends or extremities. They are primarily compact bone but may have a large amount of spongy bone at the ends or extremities. Long bones include bones of the thigh, leg, arm, and forearm.
Short bones
Short bones are roughly cube shaped with vertical and horizontal dimensions approximately equal. They consist primarily of spongy bone, which is covered by a thin layer of compact bone. Short bones include the bones of the wrist and ankle.
Flat bones
Flat bones are thin, flattened, and usually curved. Most of the bones of the cranium are flat bones.
Irregular bones
Bones that are not in any of the above three categories are classified as irregular bones. They are primarily spongy bone that is covered with a thin layer of compact bone. The vertebrae and some of the bones in the skull are irregular bones.
How to maintain healthy bones
Eat a diet high in calcium, which is found in nuts, seeds (especially sesame), soya produce, whole grains, vegetables, fish and dairy produce.
Increase your intake of essential fatty acids (EFAs) as these facilitate calcium absorption and may slow down calcium excretion and bone loss. EFAs are found in oily fish and various nut and seed oils.
Limit your intake of fizzy drinks, tea, coffee, sugar and bran, which can all inhibit calcium absorption. Animal protein and salt can also increase calcium loss in urine.
Calcium absorption requires the presence of other minerals, especially vitamin D, magnesium, and phosphorous. These are abundant in nuts, seeds, soya produce and whole grains. If taking a calcium supplement, check that other minerals (especially magnesium) are also present.
Include lots of phytoestrogens in your diet. These plant estrogens help to slow bone loss and are found in soya produce, sesame, sunflower and pumpkin seeds, chickpeas, linseeds, alfalfa and the herb red clover.
If you're taking a calcium supplement, take it in the evening. Calcium has a soporific effect and the uptake of calcium into the bones is greater at night.
Get regular exposure to sunlight. This increases production of vitamin D, which aids calcium absorption (but remember to use protection against UV rays). Vitamin D is also found in whole grains, nuts and seeds, eggs and dairy produce.
Take regular weight-bearing exercise. Walking, skipping, rebounding, racket sports and jogging are ideal. Swimming increases flexibility and tones muscles, thereby improving bone support, but doesn't build bone strength as no weight bearing is involved. Make sure you don't overexercise, though.
Limit alcohol intake and stop smoking, as both contribute to nutrient loss.