Pulmonary edema: MedlinePlus Medical Encyclopedia (original) (raw)
Pulmonary edema is an abnormal buildup of fluid in the lungs. This buildup of fluid leads to shortness of breath.
Pulmonary edema is often caused by congestive heart failure. When the heart is not able to pump efficiently, blood can back up into the blood vessels that take blood through the lungs.
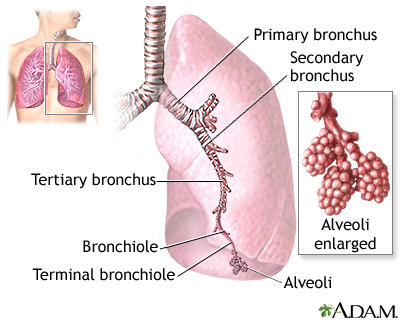
As the pressure in these blood vessels increases, fluid is pushed into the air spaces (alveoli) in the lungs. This fluid reduces normal oxygen movement through the lungs. These two factors combine to cause shortness of breath.
Congestive heart failure that leads to pulmonary edema may be caused by:
- Heart attack, or any disease of the heart that weakens or stiffens the heart muscle (cardiomyopathy)
- Leaking or narrowed heart valves (mitral or aortic valves)
- Sudden, severe high blood pressure (hypertension)
Pulmonary edema may also be caused by:
- Certain medicines
- High altitude exposure
- Kidney failure
- Narrowed arteries that bring blood to the kidneys
- Lung damage caused by burns from poisonous gas inhalation or severe infection
- Major injury
Symptoms of pulmonary edema may include:
- Coughing up blood or bloody froth
- Difficulty breathing when lying down (orthopnea)
- Feeling of "air hunger" or "drowning" (This feeling is called "paroxysmal nocturnal dyspnea" if it causes you to wake up 1 to 2 hours after falling asleep and struggle to catch your breath.)
- Grunting, gurgling, or wheezing sounds with breathing
- Problems speaking in full sentences because of shortness of breath
Other symptoms may include:
- Anxiety or restlessness
- Decrease in level of alertness
- Leg or abdominal swelling
- Pale skin
- Sweating (excessive)
The health care provider will perform a thorough physical exam.
The provider will listen to your lungs and heart with a stethoscope to check for:
- Abnormal heart sounds
- Crackles in your lungs, called rales
- Increased heart rate (tachycardia)
- Rapid breathing (tachypnea)
Other things that may be seen during the exam include:
- Leg or abdominal swelling
- Abnormalities of your neck veins (which can show that there is too much fluid in your body)
- Pale or blue skin color (pallor or cyanosis)
Possible tests include:
- Blood chemistries
- Blood oxygen levels (oximetry or arterial blood gases)
- Chest x-ray
- Complete blood count (CBC)
- Echocardiogram (ultrasound of the heart) to see if there are problems with the heart muscle
- Electrocardiogram (ECG) to look for signs of a heart attack or problems with the heart rhythm
Pulmonary edema is almost always treated in the emergency room or hospital. You may need to be in an intensive care unit (ICU).
- Oxygen is given through a face mask or tiny plastic tubes are placed in the nose.
- A breathing tube may be placed into the windpipe (trachea) so you can be connected to a breathing machine (ventilator) if you cannot breathe well on your own (only needed in severe cases).
The cause of pulmonary edema should be identified and treated quickly. For example, if a heart attack has caused the condition, it must be treated right away.
Medicines that may be used include:
- Diuretics that remove excess fluid from the body
- Medicines that strengthen the heart muscle, control the heartbeat, or relieve pressure on the heart
- Other medicines when heart failure is not the cause of the pulmonary edema
The outlook depends on the cause. The condition may get better quickly or slowly. Some people may need to use a breathing machine for a long time. If not treated, this condition can be life threatening.
Go to the emergency room or call 911 or the local emergency number if you have breathing problems.
Take all your medicines as directed if you have a disease that can lead to pulmonary edema or a weakened heart muscle.
Following a healthy diet that is low in salt and fat, and controlling your other risk factors can reduce the risk of developing this condition.
Lung congestion; Lung water; Pulmonary congestion; Heart failure - pulmonary edema
Mann DL. Management of heart failure patients with reduced ejection fraction. In: Libby P, Bonow RO, Mann DL, Tomaselli GF, Bhatt DL, Solomon SD, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 12th ed. Philadelphia, PA: Elsevier; 2022:chap 50.
Meyer NJ, Matthay MA. Pulmonary edema. In: Broaddus VC, Ernst JD, King TE, et al, eds. Murray and Nadel's Textbook of Respiratory Medicine. 7th ed. Philadelphia, PA: Elsevier; 2022:chap 133.
Rogers JG, O'Connor CM. Heart failure: epidemiology, pathobiology, and diagnosis. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 45.
Updated by: Thomas S. Metkus, MD, Assistant Professor of Medicine and Surgery, Johns Hopkins University School of Medicine, Baltimore, MD. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.