Atrial fibrillation and atrial flutter: MedlinePlus Medical Encyclopedia (original) (raw)
Atrial fibrillation (Afib) and atrial flutter are common types of abnormal heart rhythms (arrhythmias) which affect the upper chambers (atria) of the heart.
In atrial flutter, the heart beats too fast, but mostly continues to contract in a regular rhythm. AFib is a closely related condition in which the atria contract in a chaotic manner, or "quivers." This creates an irregular heart rhythm that is also usually too fast. Afib and atrial flutter often occur in the same person at different times.
When working well, the 4 chambers of the heart contract (squeeze) in an organized way.
Electrical signals direct your heart to pump the right amount of blood for your body's needs. The signals begin in an area called the sinoatrial node (also called the sinus node or SA node).
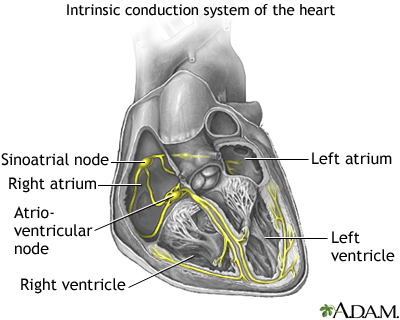
In people with AFib, the electrical impulse of the heart is not regular. This is because the sinoatrial node no longer controls the sequence of heart muscle contractions (rhythm) in the upper chambers of the heart (atria).
In AFib:
- The atria do not contract in an organized pattern.
- The lower chambers of the heart (ventricles) contract in an irregular manner that is often too fast.
- As a result, the heart cannot pump enough blood to meet the body's needs.
In people with atrial flutter, the atria beat very rapidly, but in a regular pattern.
These problems can affect both men and women. They become more common with increasing age.
Common causes of AFib include:
- Alcohol use (especially binge drinking)
- Coronary artery disease
- Heart attack or heart bypass surgery
- Heart failure or an enlarged heart
- Heart valve disease (most often the mitral valve)
- Hypertension
- Medicines
- Overactive thyroid gland (hyperthyroidism)
- Pericarditis
- Sick sinus syndrome
You may not be aware that your heart is not beating in a normal pattern. When symptoms are present, they may include one or more of the following:
- Pulse that feels rapid, racing, pounding or thumping, fluttering, irregular, or too slow.
- Sensation of feeling the heart beat (palpitations).
- Confusion.
- Dizziness, lightheadedness.
- Fainting.
- Fatigue.
- Weakness.
- Loss of ability to exercise.
- Shortness of breath and anxiety.
- Sweating.
- Chest pain or pressure, which may be a sign of a heart attack. Call 911 or the local emergency number right away if you have chest pain or pressure.
Your health care provider may hear a fast heartbeat while listening to your heart with a stethoscope. Your pulse may feel fast, uneven, or both.
The normal heart rate is 60 to 100 beats per minute. In Afib or flutter, the heart rate may be as high as 250 to 350 beats per minute and is very often over 100 beats per minute. Blood pressure may be normal or low.
An ECG (a test that records the electrical activity of the heart) may show AFib or atrial flutter.
If your abnormal heart rhythm comes and goes, you may need to wear a special monitor to diagnose the problem. The monitor records the heart's rhythms over a period of time.
- Event monitor (3 to 4 weeks)
- Holter monitor (24-hour test)
- Implanted loop recorder (extended monitoring)
Tests to find heart disease may include:
- Echocardiogram (ultrasound imaging of the heart)
- Tests to examine the blood supply of the heart muscle
- Tests to study the heart's electrical system
Cardioversion treatment may be used to get the heart back into a normal rhythm right away. There are two options for treatment:
- Electric shocks to your heart
- Medicines given through a vein
These treatments may be done as emergency methods, or planned ahead of time.
Daily medicines taken by mouth are used to:
- Slow the irregular heartbeat and maintain normal heart rhythm -- These drugs may include beta-blockers, calcium channel blockers, digoxin, and anti-arrhythmics.
- Prevent blood clots -- Blood-thinning medicines are often given to reduce the risk of blood clots that can result from ongoing irregular heart rhythms.
- Prevent AFib from coming back -- These drugs work well in many people, but they can have serious side effects. AFib returns in many people, even while they are taking these medicines.
A procedure called radiofrequency ablation can be used to scar areas in your heart where the heart rhythm problems are triggered. This can prevent the abnormal electrical signals that cause AFib or flutter from moving through your heart. You may need a heart pacemaker after this procedure. All people with AFib will need to learn how to manage this condition at home.
People with AFib will most often need to take blood thinner medicines. These medicines are used to reduce the risk of developing a blood clot that travels in the body (and that can cause a stroke, for example). The irregular heart rhythm that occurs with AFib makes blood clots more likely to form.
Blood thinner medicines include heparin, warfarin (Coumadin), apixaban (Eliquis), rivaroxaban (Xarelto), edoxaban (Savaysa) and dabigatran (Pradaxa). Antiplatelet drugs such as aspirin or clopidogrel may also be prescribed. However, blood thinners increase the chance of bleeding, so not everyone can use them.
Another stroke prevention option for people who cannot safely take these medicines is the Watchman Device, which has recently been approved by the FDA. This is a small basket-shaped implant that is placed inside the heart to block off the area of the heart where most of the clots form. This limits clots from forming.
Your provider will consider your age and other medical problems when deciding which stroke prevention methods are best for you.
Treatment can often control this disorder. Many people with AFib do very well with treatment.
AFib tends to return and get worse. It may come back in some people, even with treatment.
Clots that break off and travel to the brain can cause a stroke.
Contact your provider if you have symptoms of AFib or flutter.
Talk to your provider about steps to treat conditions that cause atrial fibrillation and flutter. Avoid binge drinking.
Auricular fibrillation; AFib; A-fib; Afib; Supraventricular arrhythmia; AF; AFL
Calkins H, Tomaselli GF, Morady F. Atrial fibrillation: clinical features, mechanisms, and management. In: Libby P, Bonow RO, Mann DL, Tomaselli GF, Bhatt DL, Solomon SD, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 12th ed. Philadelphia, PA: Elsevier; 2022:chap 66.
Jogler JA, Chung MK, Armbruster AL, et al. 2023 ACC/AHA/ACCP/HRS Guideline for the diagnosis and management of atrial fibrillation: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2024;149(1):e1–e156. PMID: 38033089 pubmed.ncbi.nlm.nih.gov/38033089/.
Zimetbaum P, Goldman L. Supraventricular ectopy and tachyarrhythmias. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 52.
Updated by: Michael A. Chen, MD, PhD, Associate Professor of Medicine, Division of Cardiology, Harborview Medical Center, University of Washington Medical School, Seattle, WA. Internal review and update on 02/19/2024 by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.