B cells – NIH Director's Blog (original) (raw)
Encouraging First-in-Human Results for a Promising HIV Vaccine
Posted on June 6th, 2023 by Lawrence Tabak, D.D.S., Ph.D.

Researchers used a customized nanoparticle (top left) to learn more about guiding the immune system to mount a desired robust response, the type needed for an effective HIV vaccine. Credit: Donny Bliss, NIH
In recent years, we’ve witnessed some truly inspiring progress in vaccine development. That includes the mRNA vaccines that were so critical during the COVID-19 pandemic, the first approved vaccine for respiratory syncytial virus (RSV), and a “universal flu vaccine” candidate that could one day help to thwart future outbreaks of more novel influenza viruses.
Inspiring progress also continues to be made toward a safe and effective vaccine for HIV, which still infects about 1.5 million people around the world each year [1]. A prime example is the recent first-in-human trial of an HIV vaccine made in the lab from a unique protein nanoparticle, a molecular construct measuring just a few billionths of a meter.
The results of this early phase clinical study, published recently in the journal Science Translational Medicine [2] and earlier in Science [3], showed that the experimental HIV nanoparticle vaccine is safe in people. While this vaccine alone will not offer HIV protection and is intended to be part of an eventual broader, multistep vaccination regimen, the researchers also determined that it elicited a robust immune response in nearly all 36 healthy adult volunteers.
How robust? The results show that the nanoparticle vaccine, known by the lab name eOD-GT8 60-mer, successfully expanded production of a rare type of antibody-producing immune B cell in nearly all recipients.
What makes this rare type of B cell so critical is that it is the cellular precursor of other B cells capable of producing broadly neutralizing antibodies (bnAbs) to protect against diverse HIV variants. Also very good news, the vaccine elicited broad responses from helper T cells. They play a critical supportive role for those essential B cells and their development of the needed broadly neutralizing antibodies.
For decades, researchers have brought a wealth of ideas to bear on developing a safe and effective HIV vaccine. However, crossing the finish line—an FDA-approved vaccine—has proved profoundly difficult.
A major reason is the human immune system is ill equipped to recognize HIV and produce the needed infection-fighting antibodies. And yet the medical literature includes reports of people with HIV who have produced the needed antibodies, showing that our immune system can do it.
But these people remain relatively rare, and the needed robust immunity clocks in only after many years of infection. On top of that, HIV has a habit of mutating rapidly to produce a wide range of identity-altering variants. For a vaccine to work, it most likely will need to induce the production of bnAbs that recognize and defend against not one, but the many different faces of HIV.
To make the uncommon more common became the quest of a research team that includes scientists William Schief, Scripps Research and IAVI Neutralizing Antibody Center, La Jolla, CA; M. Juliana McElrath, Fred Hutchinson Cancer Center, Seattle; and Kristen Cohen, a former member of the McElrath lab now at Moderna, Cambridge, MA. The team, with NIH collaborators and support, has been plotting out a stepwise approach to train the immune system into making the needed bnAbs that recognize many HIV variants.
The critical first step is to prime the immune system to make more of those coveted bnAb-precursor B cells. That’s where the protein nanoparticle known as eOD-GT8 60-mer enters the picture.
This nanoparticle, administered by injection, is designed to mimic a small, highly conserved segment of an HIV protein that allows the virus to bind and infect human cells. In the body, those nanoparticles launch an immune response and then quickly vanish. But because this important protein target for HIV vaccines is so tiny, its signal needed amplification for immune system detection.
To boost the signal, the researchers started with a bacterial protein called lumazine synthase (LumSyn). It forms the scaffold, or structural support, of the self-assembling nanoparticle. Then, they added to the LumSyn scaffold 60 copies of the key HIV protein. This louder HIV signal is tailored to draw out and engage those very specific B cells with the potential to produce bnAbs.
As the first-in-human study showed, the nanoparticle vaccine was safe when administered twice to each participant eight weeks apart. People reported only mild to moderate side effects that went away in a day or two. The vaccine also boosted production of the desired B cells in all but one vaccine recipient (35 of 36). The idea is that this increase in essential B cells sets the stage for the needed additional steps—booster shots that can further coax these cells along toward making HIV protective bnAbs.
The latest finding in Science Translational Medicine looked deeper into the response of helper T cells in the same trial volunteers. Again, the results appear very encouraging. The researchers observed CD4 T cells specific to the HIV protein and to the LumSyn in 84 percent and 93 percent of vaccine recipients. Their analyses also identified key hotspots that the T cells recognized, which is important information for refining future vaccines to elicit helper T cells.
The team reports that they’re now collaborating with Moderna, the developer of one of the two successful mRNA-based COVID-19 vaccines, on an mRNA version of eOD-GT8 60-mer. That’s exciting because mRNA vaccines are much faster and easier to produce and modify, which should now help to move this line of research along at a faster clip.
Indeed, two International AIDS Vaccine Initiative (IAVI)-sponsored clinical trials of the mRNA version are already underway, one in the U.S. and the other in Rwanda and South Africa [4]. It looks like this team and others are now on a promising track toward following the basic science and developing a multistep HIV vaccination regimen that guides the immune response and its stepwise phases in the right directions.
As we look back on more than 40 years of HIV research, it’s heartening to witness the progress that continues toward ending the HIV epidemic. This includes the recent FDA approval of the drug Apretude, the first injectable treatment option for pre-exposure prevention of HIV, and the continued global commitment to produce a safe and effective vaccine.
References:
[1] Global HIV & AIDS statistics fact sheet. UNAIDS.
[2] A first-in-human germline-targeting HIV nanoparticle vaccine induced broad and publicly targeted helper T cell responses. Cohen KW, De Rosa SC, Fulp WJ, deCamp AC, Fiore-Gartland A, Laufer DS, Koup RA, McDermott AB, Schief WR, McElrath MJ. Sci Transl Med. 2023 May 24;15(697):eadf3309.
[3] Vaccination induces HIV broadly neutralizing antibody precursors in humans. Leggat DJ, Cohen KW, Willis JR, Fulp WJ, deCamp AC, Koup RA, Laufer DS, McElrath MJ, McDermott AB, Schief WR. Science. 2022 Dec 2;378(6623):eadd6502.
[4] IAVI and Moderna launch first-in-Africa clinical trial of mRNA HIV vaccine development program. IAVI. May 18, 2022.
Links:
Progress Toward an Eventual HIV Vaccine, NIH Research Matters, Dec. 13, 2022.
NIH Statement on HIV Vaccine Awareness Day 2023, Auchincloss H, Kapogiannis, B. May, 18, 2023.
HIV Vaccine Development (National Institute of Allergy and Infectious Diseases/NIH)
International AIDS Vaccine Initiative (IAVI) (New York, NY)
William Schief (Scripps Research, La Jolla, CA)
Julie McElrath (Fred Hutchinson Cancer Center, Seattle, WA)
McElrath Lab (Fred Hutchinson Cancer Center, Seattle, WA)
NIH Support: National Institute of Allergy and Infectious Diseases
Posted In: Health, News, Science
Tags: AIDS, antibodies, B cells, bnAbs, broadly neutralizing antibodies, CD4 T cells, eOD-GT8 60mer, HIV, HIV vaccine, immune system, infectious disease, mRNA vaccine, nanoparticle, T cells
mRNA Vaccines May Pack More Persistent Punch Against COVID-19 Than Thought
Posted on July 13th, 2021 by Dr. Francis Collins

Many people, including me, have experienced a sense of gratitude and relief after receiving the new COVID-19 mRNA vaccines. But all of us are also wondering how long the vaccines will remain protective against SARS-CoV-2, the coronavirus responsible for COVID-19.
Earlier this year, clinical trials of the Moderna and Pfizer-BioNTech vaccines indicated that both immunizations appeared to protect for at least six months. Now, a study in the journal Nature provides some hopeful news that these mRNA vaccines may be protective even longer [1].
In the new study, researchers monitored key immune cells in the lymph nodes of a group of people who received both doses of the Pfizer-BioNTech mRNA vaccine. The work consistently found hallmarks of a strong, persistent immune response against SARS-CoV-2 that could be protective for years to come.
Though more research is needed, the findings add evidence that people who received mRNA COVID-19 vaccines may not need an additional “booster” shot for quite some time, unless SARS-CoV-2 evolves into new forms, or variants, that can evade this vaccine-induced immunity. That’s why it remains so critical that more Americans get vaccinated not only to protect themselves and their loved ones, but to help stop the virus’s spread in their communities and thereby reduce its ability to mutate.
The new study was conducted by an NIH-supported research team led by Jackson Turner, Jane O’Halloran, Rachel Presti, and Ali Ellebedy at Washington University School of Medicine, St. Louis. That work builds upon the group’s previous findings that people who survived COVID-19 had immune cells residing in their bone marrow for at least eight months after the infection that could recognize SARS-CoV-2 [2]. The researchers wanted to see if similar, persistent immunity existed in people who hadn’t come down with COVID-19 but who were immunized with an mRNA vaccine.
To find out, Ellebedy and team recruited 14 healthy adults who were scheduled to receive both doses of the Pfizer-BioNTech vaccine. Three weeks after their first dose of vaccine, the volunteers underwent a lymph node biopsy, primarily from nodes in the armpit. Similar biopsies were repeated at four, five, seven, and 15 weeks after the first vaccine dose.
The lymph nodes are where the human immune system establishes so-called germinal centers, which function as “training camps” that teach immature immune cells to recognize new disease threats and attack them with acquired efficiency. In this case, the “threat” is the spike protein of SARS-COV-2 encoded by the vaccine.
By the 15-week mark, all of the participants sampled continued to have active germinal centers in their lymph nodes. These centers produced an army of cells trained to remember the spike protein, along with other types of cells, including antibody-producing plasmablasts, that were locked and loaded to neutralize this key protein. In fact, Ellebedy noted that even after the study ended at 15 weeks, he and his team continued to find no signs of germinal center activity slowing down in the lymph nodes of the vaccinated volunteers.
Ellebedy said the immune response observed in his team’s study appears so robust and persistent that he thinks that it could last for years. The researcher based his assessment on the fact that germinal center reactions that persist for several months or longer usually indicate an extremely vigorous immune response that culminates in the production of large numbers of long-lasting immune cells, called memory B cells. Some memory B cells can survive for years or even decades, which gives them the capacity to respond multiple times to the same infectious agent.
This study raises some really important issues for which we still don’t have complete answers: What is the most reliable correlate of immunity from COVID-19 vaccines? Are circulating spike protein antibodies (the easiest to measure) the best indicator? Do we need to know what’s happening in the lymph nodes? What about the T cells that are responsible for cell-mediated immunity?
If you follow the news, you may have seen a bit of a dust-up in the last week on this topic. Pfizer announced the need for a booster shot has become more apparent, based on serum antibodies. Meanwhile, the Food and Drug Administration and Centers for Disease Control and Prevention said such a conclusion would be premature, since vaccine protection looks really good right now, including for the delta variant that has all of us concerned.
We’ve still got a lot more to learn about the immunity generated by the mRNA vaccines. But this study—one of the first in humans to provide direct evidence of germinal center activity after mRNA vaccination—is a good place to continue the discussion.
References:
[1] SARS-CoV-2 mRNA vaccines induce persistent human germinal centre responses. Turner JS, O’Halloran JA, Kalaidina E, Kim W, Schmitz AJ, Zhou JQ, Lei T, Thapa M, Chen RE, Case JB, Amanat F, Rauseo AM, Haile A, Xie X, Klebert MK, Suessen T, Middleton WD, Shi PY, Krammer F, Teefey SA, Diamond MS, Presti RM, Ellebedy AH. Nature. 2021 Jun 28. [Online ahead of print]
[2] SARS-CoV-2 infection induces long-lived bone marrow plasma cells in humans. Turner JS, Kim W, Kalaidina E, Goss CW, Rauseo AM, Schmitz AJ, Hansen L, Haile A, Klebert MK, Pusic I, O’Halloran JA, Presti RM, Ellebedy AH. Nature. 2021 May 24. [Online ahead of print]
Links:
COVID-19 Research (NIH)
Ellebedy Lab (Washington University, St. Louis)
NIH Support: National Institute of Allergy and Infectious Diseases; National Center for Advancing Translational Sciences
Posted In: News
Tags: antibodies, B cells, booster, coronavirus, COVID-19, COVID-19 immune response, COVID-19 vaccine, COVID-19 variants, germinal centers, immunity, lymph node, memory B cell, Moderna vaccine, mRNA vaccine, novel coronavirus, pandemic, Pfizer/BioNTech vaccine, plasmablast, SARS-CoV-2, spike protein, vaccines
On-the-Spot Gene Readouts Offer Clues to How Cells Work
Posted on March 11th, 2021 by Dr. Francis Collins

Credit: MIT and Harvard Medical School, Cambridge, MA
Just as two companies can merge to expand their capabilities, two technologies can become more powerful when integrated into one. That’s why researchers recently merged two breakthrough technologies into one super powerful new method called ExSeq. The two-in-one technology enables researchers for the first time to study an intact tissue sample and track genetic activity on the spot within a cell’s tiniest recesses, or microenvironments—areas that have been largely out of reach until now.
ExSeq, which is described in a paper in the journal Science [1], will unleash many new experimental applications. Beyond enabling more precise analysis of the basic building blocks of life, these applications include analyzing tumor biopsies more comprehensively and even unlocking mysteries of how the brain works. The latter use is on display in this colorful cross-section of a mouse’s hippocampus, a region of the brain involved in the memory of facts and events.
Here you can see in precise and unprecedented detail the areas where genes are activated (magenta) in the brain’s neurons (green). In this particular example, the genes are working within subregions of the hippocampus called the CA1 and dentate gyrus regions (white, bottom and top left).
ExSeq is a joint effort from NIH grantees Ed Boyden, Massachusetts Institute of Technology (MIT), Cambridge, and George Church, Harvard Medical School, Boston. The new method combines a technology called tissue expansion with an _in sit_u sequencing approach.
Tissue expansion swells the contents of tissue sections up to 100 times their normal size but retains their same physical structure [2]. It’s sort of like increasing the font size and line spacing on a hard-to-read document. It makes cellular details that were outside the resolution range of the light microscope suddenly accessible.
With the information inside cells now easier to see, the next step involves a technique called FISSEQ (fluorescent in situ sequencing), which generates readouts of thousands of mRNA molecules in cells [3]. FISSEQ works by detecting individual RNA molecules where they are inside cells and amplifying them into “nanoballs,” or rolled-up copies of themselves. Each nanoball can be read using standard sequencing methods and a fluorescence microscope.
Using the combined ExSeq approach, the team can analyze precisely where gene activity changes within tiny cellular microenvironments. Or, it can compile a more-comprehensive readout of gene activity within cells by analyzing as many gene readouts as detectable. When used in the hippocampus, this untargeted, “agnostic” approach led to some surprises—revealing unusual forms of RNA and, by association, genes for proteins not previously linked with communication between neurons.
Like many technology developments, the scientists envision that ExSeq can be used in many ways, including for more precise analysis of tumor biopsies. To illustrate this point, the researchers analyzed breast cancer metastases, which are cells from breast tumors that have spread to other areas in the body. Metastases contain many different cell types, including cancer cells and immune cells.
Using ExSeq, Boyden and Church learned that these distinct cell types can behave differently depending on where they are inside a tumor. They discovered, for example, that immune B cells near tumor cells expressed certain inflammatory genes at a higher level than immune B cells that were further away. Precise information about a tumor’s composition and activity may lead to development of more targeted approaches to attack it.
Many discoveries come on the heels of transformative new technologies. ExSeq shines a much brighter light on the world of the very small. And that should help us better understand how different parts of cells work together, as well as how cells work with each other in the brain, in cancer, and throughout the body.
References:
[1] Expansion sequencing: Spatially precise in situ transcriptomics in intact biological systems. Alon S, Goodwin DR, Sinha A, Wassie AT, et al. Science. 2021 Jan 29;37:eaax2656.
[2] Expansion microscopy. Chen F, Tillberg PW, Boyden ES. Science. 2015;347:543-548.
[3]. Highly multiplexed subcellular RNA sequencing in situ. Lee JH, Daugharthy ER, Scheiman J, Kalhor R, et al. Science. 2014;343:1360-1363.
Links:
Ribonucleic Acid (RNA) (National Human Genome Research Institute/NIH)
Synthetic Neurobiology Group (Massachusetts Institute of Technology, Cambridge)
George Church (Harvard Medical School, Boston)
NIH Support: National Human Genome Research Institute; National Cancer Institute; National Institute of Biomedical Imaging and Bioengineering; National Institute of Mental Health; National Institute of Neurological Disorders and Stroke
Posted In: Snapshots of Life
Tags: B cells, biotechnology, brain, brain imaging, breast cancer, cancer imaging, expansion sequencing, ExSeq, FISSEQ, fluorescence in situ sequencing of RNA, gene activity, gene expression, gene readout, genes, genomics, hippocampus, imaging, inflammatory genes, metastases, microscopy, mRNA, nanoballs, neurons, technology, tissue expansion, tissue microenvironment
Enlisting Monoclonal Antibodies in the Fight Against COVID-19
Posted on May 21st, 2020 by Dr. Francis Collins
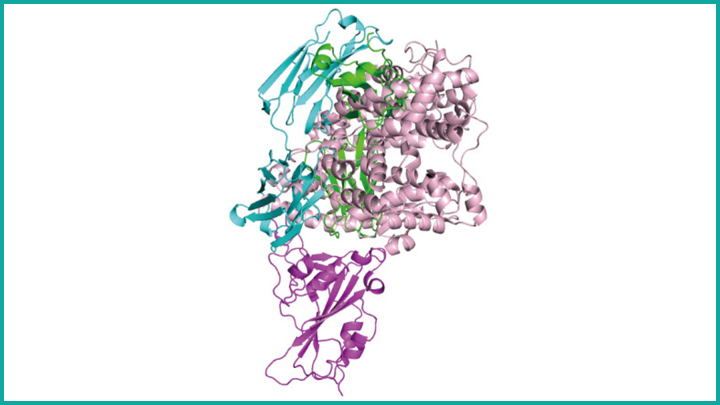
Caption: Antibody Binding to SARS-CoV-2. Structural illustration of B38 antibody (cyan, green) attached to receptor-binding domain of the coronavirus SARS-CoV-2 (magenta). B38 blocks SARS-CoV-2 from binding to the ACE2 receptor (light pink) of a human cell, ACE2 is what the virus uses to infect cells. Credit: Y. Wu et al. Science, 2020
We now know that the immune system of nearly everyone who recovers from COVID-19 produces antibodies against SARS-CoV-2, the novel coronavirus that causes this easily transmitted respiratory disease [1]. The presence of such antibodies has spurred hope that people exposed to SARS-CoV-2 may be protected, at least for a time, from getting COVID-19 again. But, in this post, I want to examine another potential use of antibodies: their promise for being developed as therapeutics for people who are sick with COVID-19.
In a recent paper in the journal Science, researchers used blood drawn from a COVID-19 survivor to identify a pair of previously unknown antibodies that specifically block SARS-CoV-2 from attaching to human cells [2]. Because each antibody locks onto a slightly different place on SARS-CoV-2, the vision is to use these antibodies in combination to block the virus from entering cells, thereby curbing COVID-19’s destructive spread throughout the lungs and other parts of the body.
The research team, led by Yan Wu, Capital Medical University, Beijing, first isolated the pair of antibodies in the laboratory, starting with white blood cells from the patient. They were then able to produce many identical copies of each antibody, referred to as monoclonal antibodies. Next, these monoclonal antibodies were simultaneously infused into a mouse model that had been infected with SARS-CoV-2. Just one infusion of this combination antibody therapy lowered the amount of viral genetic material in the animals’ lungs by as much as 30 percent compared to the amount in untreated animals.
Monoclonal antibodies are currently used to treat a variety of conditions, including asthma, cancer, Crohn’s disease, and rheumatoid arthritis. One advantage of this class of therapeutics is that the timelines for their development, testing, and approval are typically shorter than those for drugs made of chemical compounds, called small molecules. Because of these and other factors, many experts think antibody-based therapies may offer one of the best near-term options for developing safe, effective treatments for COVID-19.
So, what exactly led up to this latest scientific achievement? The researchers started out with a snippet of SARS-CoV-2’s receptor binding domain (RBD), a vital part of the spike protein that protrudes from the virus’s surface and serves to dock the virus onto an ACE2 receptor on a human cell. In laboratory experiments, the researchers used the RBD snippet as “bait” to attract antibody-producing B cells in a blood sample obtained from the COVID-19 survivor. Altogether, the researchers identified four unique antibodies, but two, which they called B38 and H4, displayed a synergistic action in binding to the RBD that made them stand out for purposes of therapeutic development and further testing.
To complement their lab and animal experiments, the researchers used a particle accelerator called a synchrotron to map, at near-atomic resolution, the way in which the B38 antibody locks onto its viral target. This structural information helps to clarify the precise biochemistry of the complex interaction between SARS-CoV-2 and the antibody, providing a much-needed guide for the rational design of targeted drugs and vaccines. While more research is needed before this or other monoclonal antibody therapies can be used in humans suffering from COVID-19, the new work represents yet another example of how basic science is expanding fundamental knowledge to advance therapeutic discovery for a wide range of health concerns.
Meanwhile, there’s been other impressive recent progress towards the development of monoclonal antibody therapies for COVID-19. In work described in the journal Nature, an international research team started with a set of neutralizing antibodies previously identified in a blood sample from a person who’d recovered from a different coronavirus-caused disease, called severe acute respiratory syndrome (SARS), in 2003 [3]. Through laboratory and structural imaging studies, the researchers found that one of these antibodies, called S309, proved particularly effective at neutralizing the coronavirus that causes COVID-19, SARS-CoV-2, because of its potent ability to target the spike protein that enables the virus to enter cells. The team, which includes NIH grantees David Veesler, University of Washington, Seattle, and Davide Corti, Humabs Biomed, a subsidiary of Vir Biotechnology, has indicated that S309 is already on an accelerated development path toward clinical trials.
In the U.S. and Europe, the Accelerating COVID-19 Therapeutic Interventions and Vaccines (ACTIV) partnership, which has brought together public and private sector COVID-19 therapeutic and vaccine efforts, is intensely pursuing the development and testing of therapeutic monoclonal antibodies for COVID-19 [4]. Stay tuned for more information about these potentially significant advances in the next few months.
References:
[1] Humoral immune response and prolonged PCR positivity in a cohort of 1343 SARS-CoV 2 patients in the New York City region. Wajnberg A , Mansour M, Leven E, Bouvier NM, Patel G, Firpo A, Mendu R, Jhang J, Arinsburg S, Gitman M, Houldsworth J, Baine I, Simon V, Aberg J, Krammer F, Reich D, Cordon-Cardo C. medRxiv. Preprint Posted May 5, 2020.
[2] A noncompeting pair of human neutralizing antibodies block COVID-19 virus binding to its receptor ACE2. Wu Y. et al., Science. 13 May 2020 [Epub ahead of publication]
[3] Cross-neutralization of SARS-CoV-2 by a human monoclonal SARS-CoV antibody. Pinto D, Park YJ, Beltramello M, Veesler D, Cortil D, et al. Nature. 18 May 2020 [Epub ahead of print]
[4] Accelerating COVID-19 therapeutic interventions and vaccines (ACTIV): An unprecedented partnership for unprecedented times. Collins FS, Stoffels P. JAMA. 2020 May 18.
Links:
Coronavirus (COVID-19) (NIH)
Monoclonal Antibodies (National Cancer Institute/NIH)
Accelerating COVID-19 Therapeutic Interventions and Vaccines (ACTIV)
NIH Support: National Institute of Allergy and Infectious Diseases; National Institute of General Medical Sciences
Posted In: News
Tags: ACE2, ACTIV, antibodies, antibody treatment, B cells, biochemistry, China, coronavirus, COVID-19, drug design, drug development, immunology, mAbs, monoclonal antibody, novel coronavirus, pandemic, SARS-CoV-2, spike protein, structural biology, synchrotron X-ray fluorescence technology
Creative Minds: Exploring the Role of Immunity in Hypertension
Posted on September 7th, 2017 by Dr. Francis Collins
Meena Madhur / Credit: John Russell
If Meena Madhur is correct, people with hypertension will one day pay as much attention to their immune cell profiles as their blood pressure readings. A physician-researcher at Vanderbilt University School of Medicine, Nashville, Madhur is one of a growing number of scientists who thinks the immune system contributes to—or perhaps even triggers—hypertension, which increases the risk of stroke, heart disease, kidney disease, and other serious health problems.
About one of every three adult Americans currently have hypertension, yet a surprising number don’t know they have it and less than half have their high blood pressure under control—leading many health experts to refer to the condition as a “silent killer”[1,2]. For many folks, blood pressure control can be achieved through lifestyle changes, such as losing weight, exercising, limiting salt intake, and taking blood pressure medicines prescribed by their health-care provider. Unfortunately, such measures don’t work for everyone, and some people continue to suffer damage to their kidneys and blood vessels from poorly controlled hypertension.
Madhur wants to know whether the immune system might be playing a role, and whether this might hold some clues for developing new, more targeted ways of treating high blood pressure. To get such answers, this practicing cardiologist will use her 2016 NIH Director’s New Innovator Award to conduct sophisticated, single-cell analyses of the immune systems of people with and without hypertension. Her goal is to produce the most comprehensive catalog to date of which human immune cells might be involved in hypertension.
Posted In: Health, Science, technology
Tags: 2016 NIH Director’s New Innovator Award, Accelerating Medicines Project, AMP, antibodies, B cells, cardiology, CyTOF, Cytometry by Time-of-Flight, flow cytometry, heart disease, high blood pressure, hypertension, immune system, inflammation, kidney disease, lupus, machine learning, mass cytometry, obesity, rheumatoid arthritis, silent killer, stroke, T cells
Regenerative Medicine: Making Blood Stem Cells in the Lab
Posted on May 23rd, 2017 by Dr. Francis Collins
Caption: Arrow in first panel points to an endothelial cell induced to become hematopoietic stem cell (HSC). Second and third panels show the expansion of HSCs over time.
Credit: Raphael Lis, Weill Cornell Medicine, New York, NY
Bone marrow transplants offer a way to cure leukemia, sickle cell disease, and a variety of other life-threatening blood disorders.There are two major problems, however: One is many patients don’t have a well-matched donor to provide the marrow needed to reconstitute their blood with healthy cells. Another is even with a well-matched donor, rejection or graft versus host disease can occur, and lifelong immunosuppression may be needed.
A much more powerful option would be to develop a means for every patient to serve as their own bone marrow donor. To address this challenge, researchers have been trying to develop reliable, lab-based methods for making the vital, blood-producing component of bone marrow: hematopoietic stem cells (HSCs).
Two new studies by NIH-funded research teams bring us closer to achieving this feat. In the first study, researchers developed a biochemical “recipe” to produce HSC-like cells from human induced pluripotent stem cells (iPSCs), which were derived from mature skin cells. In the second, researchers employed another approach to convert mature mouse endothelial cells, which line the inside of blood vessels, directly into self-renewing HSCs. When these HSCs were transplanted into mice, they fully reconstituted the animals’ blood systems with healthy red and white blood cells.
Tags: adult stem cell therapy, adult stem cells, B cells, blood, blood cells, blood disorders, blood stem cells, bone marrow transplant, bone marrow transplantation, cell reprogramming, endothelial cells, graft versus host disease, hematopoietic stem cells, HSC, HSCs, immune system, immunosuppression, induced Pluripotent Stem cells, iPS cells, iPSCs, leukemia, red blood cells, regenerative medicine, sickle cell disease, stem cells, T cells, transcription factors, white blood cells
AIDS Vaccine Research: Better By Design?
Posted on April 5th, 2016 by Dr. Francis Collins

Caption: eOD-GT8 60mer nanoparticle based on the engineered protein eOD-GT8. Yellow shows where eOD-GT8 binds antibodies; white is the protein surface outside the binding site; light blue indicates the sugars attached to the protein; dark blue is the nanoparticle core to which eOD-GT8 has been fused.
Credit: Sergey Menis and William Schief, The Scripps Research Institute
A while ago, I highlighted a promising new approach for designing a vaccine against the human immunodeficiency virus (HIV), the cause of AIDS. This strategy would “take the immune system to school” and teach it a series of lessons using several vaccine injections—each consisting of a different HIV proteins designed to push the immune system, step by step, toward the production of protective antibodies capable of fending off virtually all HIV strains. But a big unanswered question was whether most people actually possess the specific type of precursor immune cells that that can be taught to produce antibodies that kill HIV.
Now, we may have the answer [1]. In a study published in the journal Science, a research team, partly supported by NIH, found that the majority of people do indeed have these precursor cells. While the total number of these cells in each person may be low, this may be all that’s needed for the immune system to recognize a vaccine. Based in part on these findings, researchers plan to launch a Phase 1 clinical trial in human volunteers to see if their latest engineered protein can find these precursor cells and begin coaxing them through the complicated process of producing protective antibodies.
Tags: AIDS, AIDS vaccine, antibodies, B cells, bnAbs, broadly neutralizing antibodies, eOD-GT8, eOD-GT8 60mer, HIV, HIV envelope, HIV vaccine, human immunodeficiency virus, immune system, immunology, infectious disease, nanoparticle, Phase I clinical trial, protein engineering, protein modeling, retrovirus, vaccine, virology
Molecular Answers Found for a Mysterious Rare Immune Disorder
Posted on March 29th, 2016 by Dr. Francis Collins

Caption: Helping to solve a medical mystery. Top left, University of Utah’s Harry Hill; Bottom, CVID patient Roma Jean Ockler; Right, Ockler showing the medication that helps to control her CVID.
Credit: Jeffrey Allred, Deseret News
When most of us come down with a bacterial infection, we generally bounce back with appropriate treatment in a matter of days. But that’s often not the case for people who suffer from common variable immunodeficiency (CVID), a group of rare disorders that increase the risk of life-threatening bacterial infections of the lungs, sinuses, and intestines. CVID symptoms typically arise in adulthood and often take many years to diagnose and treat, in part because its exact molecular causes are unknown in most individuals.
Now, by combining the latest in genomic technology with some good, old-fashioned medical detective work, NIH-funded researchers have pinpointed the genetic mutation responsible for an inherited subtype of CVID characterized by the loss of immune cells essential to the normal production of antibodies [1]. This discovery, reported recently in The New England Journal of Medicine, makes it possible at long last to provide a definitive diagnosis for people with this CVID subtype, paving the way for them to receive more precise medical treatment and care. More broadly, the new study demonstrates the power of precision medicine approaches to help the estimated 25 to 30 million Americans who live with rare diseases [2].
Tags: B cells, common variable immunodeficiency, CVID, exome, gamma globulin, genetic counseling, genomics, IKAROS, IKAROS deficiency, immunology, passive immunity, precision medicine, primary immune deficiency, rare disease, transcription factor
Vaccine Research: New Tactics for Tackling HIV
Posted on June 30th, 2015 by Dr. Francis Collins
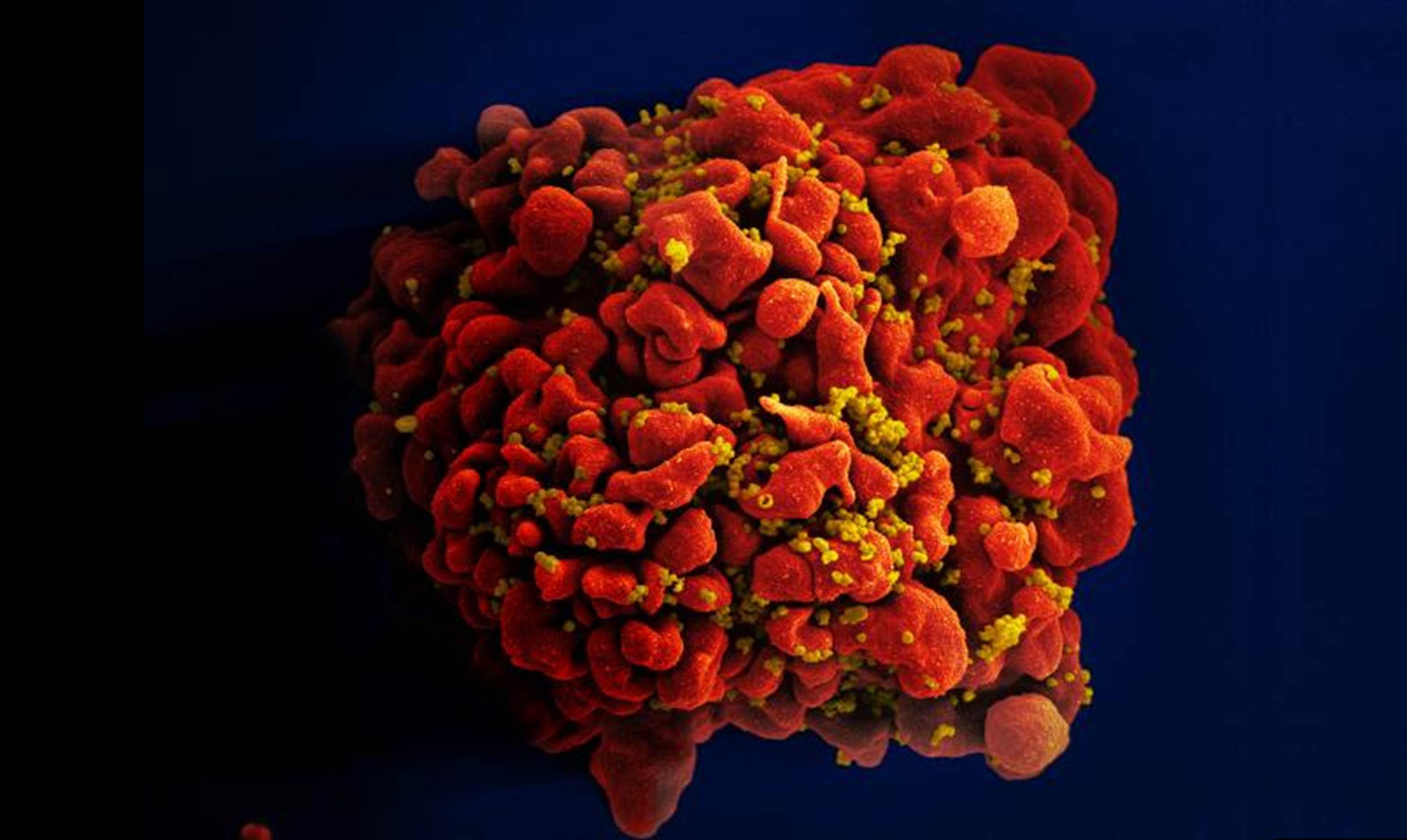
Caption: Scanning electron micrograph of an HIV-infected immune cell.
Credit: National Institute of Allergy and Infectious Diseases, NIH
For many of the viruses that make people sick—think measles, smallpox, or polio—vaccines that deliver weakened or killed virus encourage the immune system to produce antibodies that afford near complete protection in the event of an exposure. But that simple and straightforward approach doesn’t work in the case of human immunodeficiency virus (HIV), the virus that causes AIDS. In part, that’s because our immune system is poorly equipped to recognize HIV and mount an attack against the infection. To make matters worse, HIV has a habit of quickly mutating as it multiplies.That means, in order for an HIV vaccine to be effective, it must induce antibodies capable of fighting against a wide range of HIV strains. For all these reasons, the three decades of effort to develop an HIV vaccine have turned out to be enormously challenging and frustrating.
But now I’m pleased to report that NIH-funded scientists have taken some encouraging strides down this path. In two papers published in Science [1, 2] and one in Cell [3], researchers presented results of animal studies that support what most vaccine experts have come to suspect: the immune system is in fact capable of producing the kind of antibodies that should be protective against HIV, but it takes more than one step to get there. In effect, a successful vaccine strategy has to “take the immune system to school,” and it requires more than one lesson to pass the final exam. Specifically, what’s needed seems to be a series of shots—each consisting of a different engineered protein designed to push the immune system, step by step, toward the production of protective antibodies that will work against virtually all HIV strains.
Tags: AIDS, antibodies, B cells, bnAbs, broadly neutralizing antibodies, eOD-GT8 60mer, HIV, HIV envelope, HIV infection, HIV vaccine, immune response, immune system, nanoparticle, protein engineering, vaccines, virus
Taking a Snapshot of the Human Immune System
Posted on February 12th, 2013 by Dr. Francis Collins
There are numerous tests to gauge the health of your heart. But no such widely accepted test exists for the many parts of the immune system. How can we tell if the immune system is strong or weak? Or quantify how badly it’s malfunctioning when we suffer from asthma, allergies, or arthritis?
A team led by scientists at Stanford University has taken the first steps toward creating such a test—by taking “snapshots” of the immune system.
Before we talk about what they did, let me review how the immune system protects us against disease. The innate immune system is like a standing army that defends us against invading microbes. But the innate system has no memory. It doesn’t recognize the invaders more quickly if they return. This is the job of the adaptive immune system—B and T cells. These cells not only remember invaders; they’re able to adapt their weapons—antibodies and T-cell receptors—to make them more effective. Think of them as the Special Forces.
Tags: adaptive, aging, antibodies, antibody, B cells, B-cell receptors, fingerprint, flu, genomics, immune, immune system, innate, lineage, snapshots, Stanford, T cells, T-cell receptors, vaccine